Abstract
Homeless African Americans with serious mental illness experience higher rates of morbidity and mortality than adults with severe mental illness alone. Peer navigators, individuals with similar lived experiences, may help these individuals navigate the healthcare system to improve healthcare utilization. This study examined whether the Peer Navigator Program (PNP) improved scheduling and achieving healthcare appointments compared to treatment as usual (TAU) over the course of 12 months, including three periods within that timeframe: engagement (first three months), impact (middle six months), and maintenance (final six months). Results indicated no change during the first three months of the study, a significantly greater improvement in scheduled and achieved appointments for PNP compared to TAU during the middle six months, and maintenance of appointment change improvements over the final three months of the study. This research suggests peer navigators may offer a promising solution to barriers in utilizing the healthcare system for people with severe mental illness, especially those who may be homeless or from minority racial groups.
Keywords: healthcare utilization
1. Introduction
Adults with serious mental illness get sick and die 10 to 15 years younger than same age adults (World Health Organization, 2005; Mai et al., 2011). Morbidity and mortality are even worse when the adult is African American and/or homeless (Lanouette et al., 2009; Lee, O’Neill et al., 2012). Findings from a qualitative study of this population uncovered several reasons for this problem (Corrigan et al., 2015). Participants believed poor health resulted from healthcare having lower priority on a homeless person’s list of needs (with exposure to the elements and criminal victimization ranked more pressing), lack of available and accessible services, being stigmatized by the health care system, and being disoriented as a result of recurring psychiatric symptoms. One of the solutions identified by the group was strategic assistance navigating the healthcare system. In particular, focus group respondents reflected on the ideas of patient navigators, paraprofessionals who assist people in traversing a complex health system to meet their individual needs. Respondents said peers would be especially beneficial as navigators; individuals with similar lived experiences are perceived as having better empathy for members of the target population and are likely to have street smarts in addressing health needs.
Peers have been incorporated into programs meant to enhance the physical health goals of people with serious mental illness in previous research. Four randomized clinical trials (RCT) showed people who received versions of psychiatric case management services from peers demonstrated the same level of improvement in functional and symptom outcomes as those provided by professional or paraprofessional staff (Davidson et al., 2004). More recently, people with serious mental illness in hospitals receiving peer mentoring had significantly fewer hospitalizations and inpatient days during nine months of a study (Sledge et al., 2011). For the most part, these studies did not examine benefits on health needs per se, though they frequently examined overall improvements in quality of life. Hence, results were used from the earlier qualitative study (Corrigan et al., 2015) by a community-based participatory research (CBPR) team to adapt navigator guidelines for the needs and priorities of African Americans with serious mental illness who were homeless. Elsewhere findings from a randomized controlled trial showed participants in a yearlong Peer Navigator Program (PNP), compared to treatment as usual (TAU) showed significant improvement in self-perceptions of mental health, physical health, recovery and quality of life (Corrigan et al., in review). Unclear was whether these gains corresponded with similar improvement in engagement in health care services. We would expect those in the PNP would show significantly more scheduled appointments in health care services, as well as subsequent achievement of those appointments (e.g., the person actually attended the scheduled appointment).
This paper reports on appointment change over the one year PNP participation compared to the TAU group. We expect to show people participating in PNP would report more frequent monthly scheduled and achieved appointments during the yearlong study. In addition, we examine change in scheduled and achieved appointments over three periods of the 12 month study reflecting how PN is experienced and leads to change during the course of the study. The first three months represent engagement where we expect no significant changes because participants were first comprehending the breadth and depth of services and their potential impact. The second six months impact where successful impact was expect to show significant interactions in effects; i.e., those in the PNP showing significant gains in scheduled and achieved appointments compared to TAU. The final three months represents maintenance where the interaction effect is no longer significant but PNP gains from impact are still evident as significant group effects.
2. Methods
African Americans with serious mental illness who were homeless were recruited for and randomized to a one-year trial of the PNP compared to TAU. Strategies for recruitment and group assignment, as well as specification of the PNP, were described elsewhere (Corrigan et al., 2016). Research participants were 39% female (N=26) and 52.9 ± 8.0 years old on average. The group was 87% (N=58) heterosexual and somewhat varied in education with 64% (N= 43) having a high school diploma or less. Thirteen percent (N=10) reported some kind of employment. Diagnoses included major depression (N=33, 49%), bipolar disorder (N=11, 17%), anxiety disorder (N=8, 12%), PTSD (N=7, 10 %) and schizophrenia (N=8, 10%). The two groups did not differ significantly on any demographic characteristics nor on primary diagnosis.
Developed by the CBPR team, the PNP was governed by eight basic values (e.g., accepting, empowering, recovery focused, and available), seven qualities of being part of a team (e.g., networked, accessed, informed, resourced, and supervised), and six fundamental approaches (e.g., proactive, broad focused, active listener, shared decision making, and problem focused). PNs used these skills in face-to-face meetings with service recipients in places and times that were convenient to the recipient. Three peer navigators were fully trained on the program. Treatment-as-usual included services provided by the Together for Health system (T4H), a coordinated care entity funded by the state of Illinois’ Medicaid Authority to engage and manage care for individuals with multiple chronic illnesses. T4H was a network of more than 30 mental and/or physical health care programs in Chicago to provide integrated care to people with serious mental illness. One of the goals of T4H (and for the PNP, for that matter) was to engage and enroll people with disabilities into its network.
2.1 Counting appointments
Towards the beginning of each week during the yearlong study, a research assistant (RA) telephoned research participants to obtain a list of their specific appointments for the previous week using the Weekly Contact Report (WCR). The WCR asked research participants to report dates of all health-related appointments from the previous week, clinic and provider name, reason for appointment, and whether appointment was missed or achieved. The research participant was familiar with the RA and generally had a cordial relationship. In addition, the research participant was paid $5 for completing each weekly interview. All aspects of the protocol were approved by the IRB at the Illinois Institute of Technology and Heartland Alliance.
2.2 Data analyses
Four weekly assessments of scheduled and achieved appointments were summed to total twelve monthly appointments. Omnibus 2×12 ANOVAs (group by trial), separately completed for scheduled and achieved appointments, represent whether change in PN appointments were significantly greater than TAU appointments during the overall course of the study. Post hoc tests were then complete by examining change in three segments: during the first three months of the study (engagement), middle six months (impact), and final three months (maintenance). We expect interaction effects for 2×3 ANOVAs for the first three months to be nonsignificant because PN benefits have not yet been realized while engagement occurs. We expect the middle six months to show significant interaction effects. We expect interactions for the final three months to be nonsignificant because increase in appointments due to PNP have maximized and therefore leveled off. However, we expect a significant group effect showing appointments for the PN group to be significantly larger than TAU.
3. Results
Skew, kurtosis, and distribution of dependent variables were examined and seemed satisfactory such that we opted not to transform data. Means of scheduled and achieved appointments per month are graphed separately for PN and TAU groups in Figure 1. Results of The interaction effect for 2×12 ANOVA for scheduled appointments was not significant (F(11,54)=1.72; ns). However, post hoc analyses seem to support gradual engagement in PNs over the course of the study leading to significant increase in scheduled appointments maintained during the final three months. Scheduled appointments did not significantly differ across groups at the beginning of the study, month 1 (F(1,66)=1.43, ns). Moreover, no significant interaction was observed in scheduled appointments during, engagement, the first three months of study participation (F(5,65)=2.95; ns).
Figure 1.
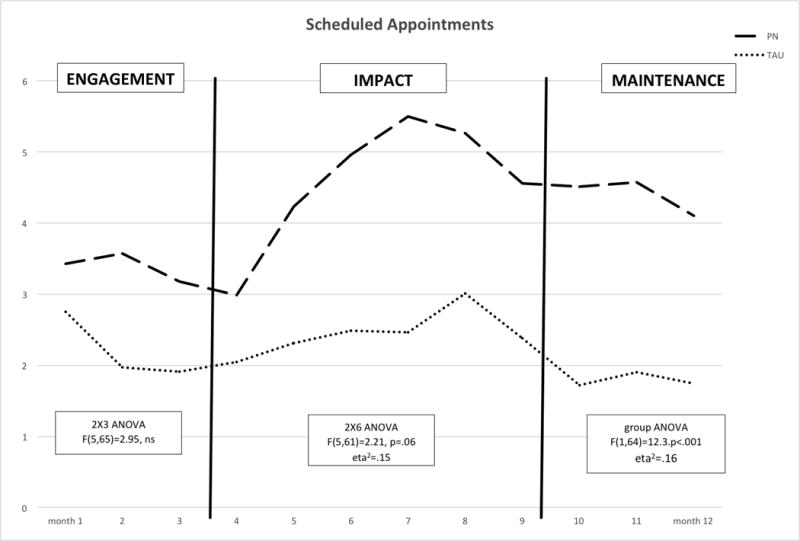
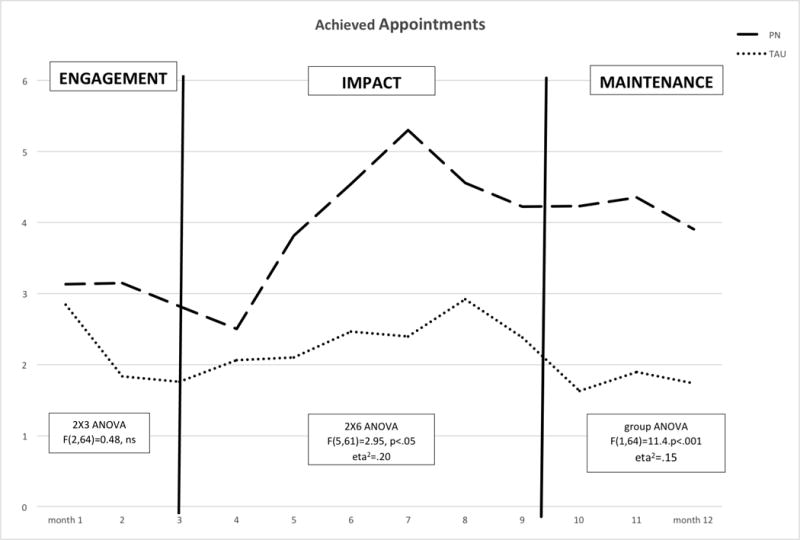
Mean number of scheduled and achieve appointments per month for peer navigator and TAU groups.
A 2×6 ANOVA yielded nonsignificant trends for impact, the middle six months (F(5,61)=2.21, p=.06). Review of the figure shows the last month (month 9) of the middle six showed a slight dip as number of appointments seemed to be leveling off. Hence, a 2×5 ANOVA representing months 4 through 8 did yield a significant interaction (F(5,61)=2.21, p<.05) with small effect size (eta2=.15). As expected, relative increase of PN group appointments, compared to the TAU group, leveled off so no significant interaction was found during maintenance (F(2,63)=0.15, ns). However a significant group effect was observed for the final three months (F(1,64)=12.3, p<.001; eta2=.16) showing that increases in scheduled appointments remained over time.
Changes in achieved appointments showed a similar pattern. Once again, the interaction effect representing relative change in achieved appointments for the 2×12 ANOVA was nonsignificant (F(11,54)=1.63, ns). Number of achieved appointments did not differ across groups at baseline (F(1,66)=1.30, ns) nor was a significant interaction found for the 2×3 ANOVA represent engagement (F(2,64)=0.48, ns). However, achieved appointments increased significantly for the PN, compared to TAU, groups during the middle six months of impact (F(1,64)=12.3, p<.001; eta2=.16). Achieved appointments leveled off so the interaction effect for the 2×3 ANOVA for the final three maintenance months was nonsignificant (F(2,63)=0.15, ns). The group effect, however, was significant (F(1,64)=11.4, p<.001; eta2=.15) showing that increases in appointments due to PN maintained during the last three months of the study.
4. Discussion
This study examined the effects of yearlong participation in a peer navigator program on scheduling and achieving healthcare appointments. We assessed relative change in PNP and TAU during the overall 12 months as well as three periods during the time: engagement (the first three months), impact (the middle six months), and maintenance (final six months). Results mostly supported our hypotheses for both scheduled and achieved appointments. Namely, no change was noted during the first three months of the project when participants were being introduced and engaging in the program. The middle six months seemed to show significantly greater improvement in scheduled and achieved appointments for PNP compared to TAU groups. Interactions were significant for the six month analysis for achieved appointments and approached significance for scheduled appointments. Benefits maintained over the final three months of the study.
There are several limitations to this study. Results represent a relatively small group of participants and we lost about 10% of participants to follow-up, though this is fairly strong retention for research participants who are homeless at program entry. We assumed that increases in scheduled and achieved appointments would correspond with improved health. However, the link between appointments and health was not assessed in this paper. Finally, we hypothesized that navigator services provided by peers would enhance the quality of navigation in healthcare services. However, this study does not examine peer influences per se. Future research will need to directly compare navigator interventions provided by peers with those offered by paraprofessionals without lived experience.
Should the various questions listed above be answered affirmatively, peer navigators have promise for generally addressing the health care needs of people with serious mental illness, especially those who are most disconnected or disenfranchised from healthcare such as people who are homeless or from minority racial groups. In this light, navigators join the growing ranks of jobs which peer support specialists might add to their service portfolio.
References
- Corrigan P, Pickett S, Kraus D, Burks R, Schmidt A. Community- based participatory research examining the health care needs of African Americans who are homeless with mental illness. Journal of health care for the poor and underserved. 2015;26(1):119–133. doi: 10.1353/hpu.2015.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan P, Kraus D, Pickett S, Schmidt A, Stellon E, Hantke E. Peer navigators that address the integrated healthcare needs of African Americans with serious mental illness who are homeless. Manuscript submitted for review to Psychiatric Services. doi: 10.1176/appi.ps.201600134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson L, Shahar G, Stayner DA, Chinman MJ, Rakfeldt J, Tebes JK. Supported socialization for people with psychiatric disabilities: Lessons from a randomized controlled trial. Journal of Community Psychology. 2004;32(4):453–477. [Google Scholar]
- Lanouette NM, Folsom DP, Sciolla A, Jeste DV. Psychotropic medication nonadherence among United States Latinos: a comprehensive literature review. Psychiatric Services. 2015 doi: 10.1176/appi.ps.60.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, O’Neill A, Park J, Scully L, Shenassa E. Health insurance moderates the association between immigrant length of stay and health status. Journal of Immigrant and Minority Health. 2012;14(2):345–349. doi: 10.1007/s10903-010-9411-z. [DOI] [PubMed] [Google Scholar]
- Mai Q, Holman CDAJ, Sanfilippo FM, Emery JD, Preen DB. Mental illness related disparities in diabetes prevalence, quality of care and outcomes: a population- based longitudinal study. BMC medicine. 2011;9(1):1. doi: 10.1186/1741-7015-9-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sledge WH, Lawless M, Sells D, Wieland M, O’Connell MJ, Davidson L. Effectiveness of peer support in reducing readmissions of persons with multiple psychiatric hospitalizations. Psychiatric Services. 2011;62(5):541–544. doi: 10.1176/ps.62.5.pss6205_0541. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Dept. of Mental Health and Substance Abuse. Mental health atlas 2005. World Health Organization; 2005. [Google Scholar]


