Abstract
Introduction
The development of precision approaches for customized health interventions is a promising application of genomic discovery. To optimize such weight management interventions, target audiences will need to be engaged in research and implementation efforts. Investigation into approaches that engage these audiences will be required to ensure that genomic information, particularly with respect to genomic influences on endophenotypes like eating behavior, is understood and accepted, and not associated with unintended adverse outcomes. We took steps to characterize healthy individuals’ beliefs about genetic influences on eating behavior.
Methods
Data were collected via online survey from 261 participants selected at random from a database.
Results
Respondents infrequently spontaneously identified eating behavior-related factors as running in families. However, those who perceived themselves as overweight and perceived a family history of overweight were more likely to attribute eating behavior to genetics on closed-ended assessments, β=.252, p=.039. Genetic attributions for eating behaviors were associated with lower confidence in ability to control eating and weight, β=−.119, p=.035.
Conclusions
These exploratory findings shed light on beliefs about genetic influences on eating, a behavioral trait (rather than a disease). This investigation can inform future health intervention efforts.
Keywords: eating behaviors, genetics, beliefs, body weight, behavioral interventions
Introduction
It has long been understood that body weight is highly heritable.1–3 Estimates suggest that between 40 and 70% of one’s weight is inherited.4 Research efforts have also uncovered several specific genes that influence weight.5–6 A growing literature further supports the existence of genetic underpinnings for several weight-related behaviors. Central among these are eating behaviors. Indeed, specific genes have been implicated in behaviors like eating in the absence of hunger, food preferences, taste perception, and willingness to try new foods.7–11
Key among the anticipated applications of ongoing genomic discovery is the development of genomics-informed approaches for customized health interventions.4 Such personalized approaches will require better understanding of gene-environment and gene-gene interactions that influence health and disease. The high profile Precision Medicine Initiative is the latest,15 most ambitious effort in this regard. However, to make personalized weight management interventions a reality, target audiences will need to be engaged in research and implementation efforts. At present, there is little information available to guide the integration of genomic information into weight management approaches. Investigation into optimal approaches will be required to ensure that genomic information is understood and accepted, and is not associated with unintended adverse outcomes among target populations.
Theory and evidence suggest that individuals’ response to the integration of genomic information into weight management programs will be governed in part by their causal beliefs regarding the role of genetics in weight and eating.16–18 This encompasses not only the extent to which individuals believe that genetic factors are operational, but also their understanding of how, or the mechanism through which, these influences operate.19 In general, most people agree that in addition to behavioral factors, genetic factors are at least partially responsible for one’s body weight.20–21 Importantly, however, genetic factors are frequently discussed as operating primarily on biological processes like metabolism, as opposed to influencing one’s food preferences, taste perceptions and other drivers of weight-related behaviors.22 Thus, the extent to which the public endorses genetic underpinnings of eating behaviors is almost entirely unknown.
Eating behaviors are frequently conceptualized as the causal aspects of weight that are under one’s volitional control, and are often pitted against genetic causal explanations. Individuals tend to most strongly attribute genetic causes to physical and appearance-related characteristics, and less frequently associate them with mental or behavioral characteristics.23 For example, surveys have demonstrated low endorsement of the notion that genes influence smoking behavior.24–25 In addition, studies investigating perceptions of social influences on food intake have found that individuals are often unaware of or unwilling to acknowledge influences on their eating behavior that fall outside common-sense, experiential explanations like hunger and perceptions of how food tastes.26 It is therefore possible that genetic explanations for eating behavior may not be salient, or may even be rejected to the extent that they are perceived to contradict personal experience or notions of personal control.27 Determining whether this is the case will be essential for optimally communicating genomic influences of eating behavior in future interventions.
It has been suggested that genomics-based personalization of behavior change interventions might add value to current intervention approaches.28 Such suggestions have raised concerns that deterministic misunderstandings of genetic influences on health may lead target audiences to become discouraged or fatalistic about the value of behavior change. However, research has typically shown that attribution of weight to genetic factors does not decrease self-efficacy for weight management.29 The veracity of these concerns when considering the genetic underpinnings of eating behaviors has not yet been assessed. Research by Cameron and colleagues demonstrated that understanding the mechanisms through which behavior can reduce genetically-conferred risk for health conditions is important for undercutting potential fatalistic responses.19 However, it is unclear how self-efficacy might be influenced when target audiences are told that the very behaviors required to lower obesity risk are also genetically influenced.
The current report takes initial steps in characterizing healthy individuals’ beliefs about the notion that there are genetic influences on eating behavior in comparison with beliefs about genetic influences on body weight. We gathered data on eating behavior causal attributions and their correlates as part of a larger survey assessing individuals’ eating behavior traits.30 Given the exploratory nature of this project, we developed several research questions:
How salient is the concept that factors influencing one’s eating behaviors are passed down in the family?
To what extent do individuals perceive eating behaviors to be caused by genetics, and how does this compare with perceptions of the extent to which a) eating behaviors are caused by the environment, and b) body weight is caused by genetics?
What factors (demographic and perceptual) are associated with individuals’ genetic and environmental causal beliefs regarding eating behaviors?
How do genetic attributions for eating behaviors relate to variables relevant to future interventions including: confidence in dietary intake and weight control and interest in eating behavior-related genetic testing?
Methods
Procedure and participants
These data were collected as part of a larger survey effort related to assessing eating behavior phenotypes in 2014–2015.30 Participants represented all weight categories and were not selected on the basis of participation in a weight management program. The study was introduced to participants as an effort to better understand individuals’ eating behaviors and habits. Participants were contacted from a database of individuals who had indicated previous interest in participating in clinical research though the Patient Recruitment and Public Liaison Office of the National Institutes of Health. Individuals were randomly chosen from the database, and an email introduction was sent with an opportunity to opt out from study material mailings. A week later, a packet including login information for the online survey was sent to the mailing address on file for each participant who did not opt out. Participants were given online access via a unique user ID and password to the survey that they could choose to complete following informed consent procedures. Surveys were incentivized with check or gift card. Two hundred sixty-one participants completed the survey that contained the information reported here. This is indicative of a 23% response rate. This research was approved by the IRB of the National Human Genome Research Institute.
Measures
Demographics and predictor variables
We collected participants’ age, self-reported height and weight (from which we calculated BMI), gender, marital status (dichotomized as married/partnered versus single), parental status (dichotomized as parent versus non-parent), race (collapsed categories into White, or nonwhite), education (dichotomized as college versus no college), perceived weight (collapsed into overweight versus not overweight), and perceived family history of overweight (dichotomized as yes versus no).
Spontaneous beliefs
Participants were asked to respond to the following prompt by generating a list: “Please give examples of health conditions or other characteristics that you think might run in your family”; five response slots were provided. These responses were grouped into five categories by two trained coders who met to resolve discrepancies and achieved kappa levels greater than 0.6.
Prompted beliefs
Participants were asked to indicate their causal beliefs about the influence of genes and of environment on eating behaviors and on body weight with four items: “How much do you think (body weight/eating behavior) is influenced by (a person’s genes/the environment we live in)?”. Responses were collected on a four-point scale (not at all, a little, some, or a lot). A “don’t know” option was also included.
Intervention-Relevant Attitudes
We assessed participants’ interest in eating behavior-related genetic testing with a single item assessing how interested individuals would be in having a genetic test related to eating habits (1–7 scale from not at all interested to extremely interested; a “don’t know” option was also included). Self-efficacy was assessed by averaging two items, one assessing confidence in weight control and the other assessing confidence in controlling dietary intake (1–5 scale, not at all confident to extremely confident; a “don’t know” option was also included). These two items were correlated (r = 0.73, p<.0001, n=259).
Statistical Analysis
All analyses were conducted using the statistical software package SPSS. We ran two sets of linear regressions to test our primary research questions. The first set of analyses examined associations between relevant demographic and predictor variables with causal beliefs about eating behavior and weight. The second set of analyses investigated associations of relevant demographic variables and genetic and environmental causal beliefs with two primary outcomes: confidence in one’s ability to manage weight/eating and interest in eating behavior-related genetic testing.
Results
Demographics
Demographic characteristics of the sample are available in Table 1.
Table 1.
Demographics and characteristics of the sample (n=261)
| Characteristic | Mean (95% CI) or frequency (%) |
|---|---|
| Age | 34 (33–35) years old |
| BMI (kg/m2) | 26 (25–27) |
| Gender: | |
| Female | 150 (58%) |
| Male | 111 (43%) |
| Marital status1: | |
| Married/Partnered | 71 (27%) |
| Single | 189 (73%) |
| Parental status: | |
| Yes | 87 (33%) |
| No | 174 (67%) |
| Race1: | |
| White | 108 (42%) |
| Nonwhite | 146 (58%) |
| Education1: | |
| No college | 43 (17%) |
| College or more | 217 (83%) |
| Perceived weight: | |
| Not overweight | 132 (51%) |
| Overweight | 129 (49%) |
| Perceived family history of overweight: | |
| Yes | 122 (44.7%) |
| No | 137 (50.2%) |
Indicates that there are missing values for this variable
Spontaneous Beliefs
In response to the open ended question asking participants to provide a list of health conditions or other characteristics that run in their family, participants gave a mean of 3.82 responses (95% CI, 3.65 to 3.98). A medical condition (e.g., diabetes, high blood pressure) was named by 94% of participants, 26% indicated that elements of body weight run in their family (e.g., overweight), a physical trait (e.g., eye color) was named by 19% of participants, 11% named a personality trait (e.g., humor), and factors that influence eating or dietary behaviors (e.g., a tendency toward overeating, preference for fatty foods) was named by 8%.
Prompted Beliefs
For eating behaviors, participants’ genetic attributions averaged 2.86 (95% CI, 2.75 to 2.96), and their environmental attributions averaged 3.64 (95% CI, 3.55 to 3.72). Environmental attributions were significantly higher than genetic attributions, t(254)=−12.05, p<.0001. These variables were not significantly correlated, r=.059, p>.05.
For body weight, participants’ genetic attributions averaged 3.21 (95% CI, 3.12 to 3.30), and their environmental attributions averaged 3.59 (95% CI, 3.51 to 3.68). Again, environmental attributions were significantly higher than genetic ones, t(252)=−6.34, p<.0001. These variables were also not significantly correlated, r=.032, p>.05.
Genetic attributions for body weight were higher than genetic attributions for eating behaviors [t(251)=6.72, p<.001], whereas environmental attributions did not differ between body weight and eating behaviors, t(256)=−1.50, p>.05.
Associations between predictor variables and causal attributions
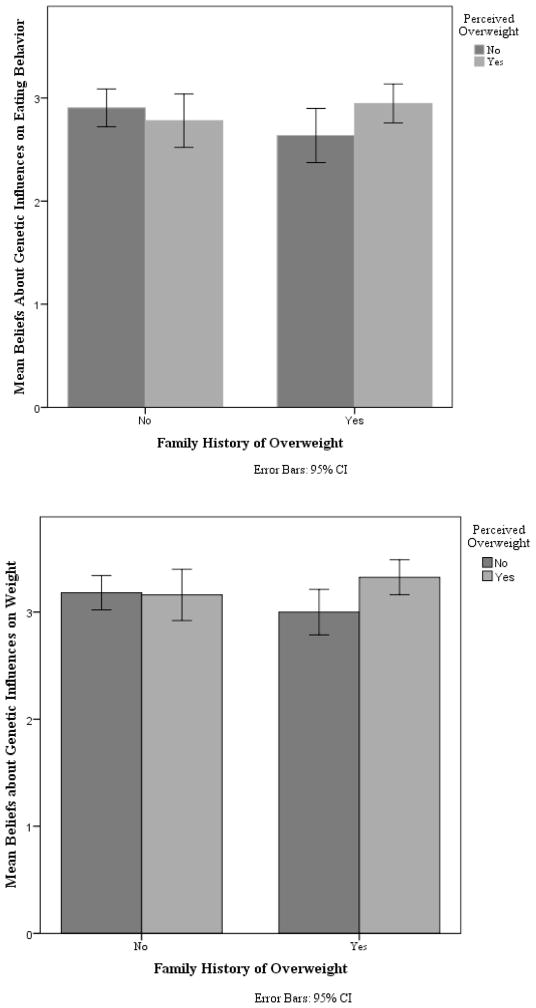
Linear regression results are available in Table 2. Participants’ genetic attributions for eating behaviors were associated solely with an interaction between their perceived weight status and their perceived family history of overweight, such that participants who perceived themselves to be overweight had higher genetic attributions for eating behavior, but only when they also perceived a family history of overweight (β=.247, p=.044). See Figure 1. None of the predictors were significantly associated with participants’ environmental attributions for eating behaviors.
Table 2.
Associations between predictor variables and causal attributions; data are presented as standardized Betas and significance
| Eating behavior attributions | Body weight attributions | |||
|---|---|---|---|---|
| Genetic | Environmental | Genetic | Environmental | |
| Demographics | ||||
| Age | −0.081 | −0.093 | −0.205 * | −0.222 ** |
| Gender (Female) | 0.094 | −0.090 | 0.015 | −0.081 |
| Race (White) | −0.096 | 0.125 | −0.037 | 0.054 |
| Education (some college or more) | −0.019 | 0.094 | 0.049 | 0.047 |
| Parental status (Parent) | −0.011 | −0.140 | 0.158 * | 0.005 |
| Perceptions | ||||
| Perception of being overweight (Yes) | −0.036 | 0.065 | −0.020 | 0.071 |
| Perceived family history of overweight (Yes) | −0.161 | 0.076 | −0.138 | 0.071 |
| Perception of overweight x Perceived family history interaction | 0.247 * | −0.085 | 0.252 * | −0.041 |
p<.05,
p<.01
Figure 1.
Interactions between perceived overweight and perceived family history of overweight on endorsement of genetic attributions in 1) Eating behavior and 2) Body weight. Interactions are significant in both models.
In comparison, participants’ genetic attributions for body weight were associated with their age such that younger individuals had stronger genetic attributions for body weight, β=−.205, p=.005. Parents were also significantly more likely to endorse genetic attributions for weight, β=.158, p=.035. There was also a significant interaction between perceived overweight and perceived family history of overweight on genetic attributions for weight (β=.252, p=.039) such that participants who perceived themselves to be overweight had higher genetic attributions for weight, but only when they also perceived a family history of overweight. Participants’ environmental attributions for body weight were only associated with their age, such that younger individuals endorsed stronger environmental attributions for body weight (β=−.222, p=.002).
Associations between causal attributions and intervention-relevant attitudes
Participants’ genetic attributions for eating behaviors and their genetic attributions for body weight were both associated with their confidence in their ability to control their dietary intake and their weight (β=−.119, p=.035 and β=−.121, p=.031, respectively), such that higher genetic attributions were associated with lower confidence. In both models, gender and perceived weight status were also statistically significant, such that men and those who do not report being overweight also indicate more confidence (β=.210, p<.000 and β=−.405, p<.000 respectively for gender and weight status in the eating behaviors model; β=.190, p<.000 and β=−.429, p<.000 respectively for gender and weight status in the body weight model). Environmental causal attributions were not related to confidence in either analysis. See Table 3.
Table 3.
Association between genetic and environmental causal attributions for eating behavior and body weight, and intervention-relevant attitudes; data are presented as standardized Betas and significance.
| Confidence in weight/dietary control | Interest in eating behavior-related genetic testing | |||
|---|---|---|---|---|
| Eating behaviors | Body weight | Eating behaviors | Body weight | |
| Age | .046 | .035 | .030 | .475 |
| Gender (1=male) | .210 ** | .190 ** | .093 | .079 |
| Race (1=white) | −.010 | −.000 | −.100 | −.121 |
| Education | −.116 | −.107 | .129 | .108 |
| Parental status | .036 | .041 | −.043 | −.079 |
| Overweight (1=yes) | −.405 ** | −.429 ** | .253 ** | .259 ** |
| Genetic attributions | −.119 * | −.121* | .163 * | .094 |
| Environmental attributions | −.038 | −.017 | .046 | .008 |
p <.05,
p <.01
Genetic attributions for eating behaviors were associated with interest in an eating behavior-related genetic test, such that higher genetic attributions were associated with more interest in the test (β=.163, p=.013). Genetic attributions for body weight and both types of environmental attributions were not related to participants’ interest in the genetic test. Weight status was significant in both models, in that there was an association of higher perceived weight status with participants’ interest in eating behavior-related genetic testing (β β=.253, p<.000 for the eating behaviors model; β=.259, p<.000 in the body weight model). See Table 3.
Discussion
This exploratory study provides preliminary evidence that adults may generally view eating behaviors as ‘less genetic’ than body weight. Unprompted, participants infrequently (8%) mentioned the factors that underlie eating behaviors as a condition or characteristic that runs in their family. This stands in contrast to how often participants listed body weight as running in families (26%). It is therefore unlikely that genomic or familial underpinnings of eating behaviors are salient to the public, since participants rarely mentioned this concept even in the context of the present eating behavior-related research study. As such, we may find that providing basic information to the public about the influence of genes on eating behavior is necessary in the course of developing related programs.
In all, we found participants to be somewhat accepting of the notion that eating behaviors have genetic underpinnings. Notably, this level of endorsement was lower than endorsement of environmental underpinnings of eating behaviors, and lower than endorsement of both genetic and environmental factors in body weight. One group was somewhat more willing to make the link between genetics and eating behaviors, i.e., individuals who perceived they were overweight and also perceived a family history of overweight. Although many individuals who are overweight more frequently report low perceived control in this arena,31 they may be reluctant to endorse genetic factors. This is because overweight and obesity are highly stigmatized, and individuals who are perceived as failing to take responsibility for their condition are viewed even more negatively.32 Individuals who have a family history of overweight, however, may perceive that there is evidence to support this connection. These results highlight the importance of considering how life experiences and social context can underlie beliefs about causal factors in eating behaviors and other traits.
The current results furthermore suggest that we may need to be cautious in introducing notions that genetic factors can or do influence eating behaviors to the public due to links we found in this study between endorsement of genetic causes and reduced self-efficacy. It is notable that the current findings differ from systematic reviews showing that genetic/genomic information rarely leads to fatalistic beliefs about the ability to control one’s weight.29 These findings also differ from the one study that has looked at the influence of describing a behavioral mechanism for the influence of genes on weight.33 However, the latter study focused on genetic influences on binge eating as the behavioral mechanism. In general, introducing the notion that genes directly influence eating behaviors may be more likely to trigger fatalistic beliefs and perceived loss of control than the generalized notions of genetic influence on body weight that have been studied previously. This is because individuals often believe they can ‘fight’ or ‘overcome’ a genetic predisposition for overweight through more careful control of their lifestyle behaviors.34 The idea that these very behaviors are themselves genetically influenced could make them seem impervious to change, and could make a genetic predisposition for overweight seem more difficult to overcome.
These findings suggest the need for additional research on how and under what circumstances new knowledge regarding the heritability of eating traits might be best used in behavior change interventions. This includes anticipating the characteristics of those who might be drawn to these interventions. For example, as we saw in this study, those who are most interested in seeking eating behavior-related genetic testing may also be most susceptible to fatalistic interpretations of those results. This has implications for how we might target eating behavior-related genetic testing and the potential importance of educating the public about these topics before offering such testing.
Limitations
The current study had several limitations. Many of the concepts studied here were measured with single or two-item measures given their inclusion in a longer survey. We were also able to assess only limited predictors and intervention-relevant outcomes. We also assessed open-ended beliefs about things that run in families using the word “characteristics”. Participants tended to list predispositions or tendencies that underlie eating behaviors (e.g., having a sweet tooth), similarly to responses in other categories (e.g., humor as a personality trait). Questioning participants about “behaviors” that run in families may have made spontaneous mention of eating behaviors more likely. In addition, this sample represents the full spectrum of weight status which gives a fuller picture of beliefs among healthy adults and allows assessment of the role of weight status and related variables on these beliefs without problems of restricted range. However, future work should also investigate these beliefs among people engaged in weight loss or weight gain-prevention efforts. In addition, although invitations were issued at random to volunteers, response rate was fairly low suggesting self-selection. Furthermore, this information was collected in the course of a study related to eating behaviors and as such the sample may have been more thoughtful about eating behaviors and their causes than the average individual. While detected associations were small, they were based on naturally-occurring beliefs. Understanding the nature and direction of these patterns can help counteract misconceptions and capitalize on areas of understanding as they related to emerging scientific findings about genetics and eating behavior. Finally, this survey was cross-sectional and therefore no casual relationships can be inferred.
Conclusion
Taken together, this exploratory work requires replication, particularly among a sample of individuals selected on the basis of likely recruitment into weight management programs. However, these initial findings shed light on healthy individuals’ beliefs about genomic influences on behavioral traits (rather than diseases) in a context of high public health importance (i.e., eating behavior and obesity). Additional qualitative and quantitative research could offer valuable insight for the formative development of a new generation of genomics-informed behavior change interventions related to weight management. For example, the beliefs of health care providers who are likely to administer interventions should also be examined. In addition, future research should examine the influence of these concepts on additional intervention-relevant factors that can be intervened upon, and are conceptually linked to intervention outcomes. It will also be crucial to understand whether communication about the heritability of behaviors adds value over current approaches for achieving promised benefits of genomic discovery.
Highlights.
Individuals infrequently spontaneously identified eating behaviors as characteristics that run in families
Genetic influence on eating behaviors was moderately endorsed in closed-ended assessments
Life experience factors were most influential on endorsement of genetic influence on eating behaviors in closed-ended assessments
Genetic attributions for eating behaviors were associated with lower confidence in ability to control eating and weight
Acknowledgments
This research was supported by the Intramural Research Program of the National Human Genome Research Institute, National Institutes of Health. The authors thank Deanna Wilson for assistance with data collection. Clinical trial registration number: NCT02015078
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bouchard C, Perusse L. Heredity and body fat. Annu Rev Nutr. 1988;8(1):259–77. doi: 10.1146/annurev.nu.08.070188.001355. http://dx.doi.org/10.1146/annurev.nu.08.070188.001355. [DOI] [PubMed] [Google Scholar]
- 2.Maes HH, Neale MC, Eaves LJ. Genetic and environmental factors in relative body weight and human adiposity. Behav Genet. 1997;27(4):325–51. doi: 10.1023/a:1025635913927. http://dx.doi.org/10.1023/A:1025635913927. [DOI] [PubMed] [Google Scholar]
- 3.Wardle J, Carnell S, Haworth CM, Plomin R. Evidence for a strong genetic influence on childhood adiposity despite the force of the obesogenic environment. Am J Clin Nutr. 2008;87(2):398–404. doi: 10.1093/ajcn/87.2.398. [DOI] [PubMed] [Google Scholar]
- 4.Bray MS, Loos RJ, McCaffery JM, Ling C, Franks PW, Weinstock GM, Snyder MP, Vassy JL, Agurs-Collins T. NIH working group report—using genomic information to guide weight management: From universal to precision treatment. Obes. 2016;24(1):14–22. doi: 10.1002/oby.21381. http://dx.doi.org/10.1002/oby.21381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Early Growth Genetics (EGG) Consortium. A genome-wide association meta-analysis identifies new childhood obesity loci. Nat Genet. 2012;44(5):526–31. doi: 10.1038/ng.2247. http://dx.doi.org/10.1038/ng.2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Speliotes EK, Willer CJ, Berndt SI, Monda KL, Thorleifsson G, Jackson AU, Allen HL, Lindgren CM, Luan JA, Mägi R, Randall JC. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat Genet. 2010;42(11):937–48. doi: 10.1038/ng.686. http://dx.doi.org/10.1038/ng.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wardle J, Llewellyn C, Sanderson S, Plomin R. The FTO gene and measured food intake in children. Int J Obes. 2009;33(1):42–5. doi: 10.1038/ijo.2008.174. http://dx.doi.org/10.1038/ijo.2008.174. [DOI] [PubMed] [Google Scholar]
- 8.Wardle J, Cooke L. Genetic and environmental determinants of children’s food preferences. Br J Nutr. 2008;99(S1):S15–21. doi: 10.1017/S000711450889246X. http://dx.doi.org/10.1017/S000711450889246X. [DOI] [PubMed] [Google Scholar]
- 9.de Krom M, Bauer F, Collier D, Adan RA, La Fleur SE. Genetic variation and effects on human eating behavior. Annu Rev Nutr. 2009;29:283–304. doi: 10.1146/annurev-nutr-080508-141124. http://dx.doi.org/10.1146/annurev-nutr-080508-141124. [DOI] [PubMed] [Google Scholar]
- 10.Cooke LJ, Haworth CM, Wardle J. Genetic and environmental influences on children’s food neophobia. Am J Clin Nutr. 2007;86(2):428–33. doi: 10.1093/ajcn/86.2.428. [DOI] [PubMed] [Google Scholar]
- 11.Grimm ER, Steinle NI. Genetics of eating behavior: established and emerging concepts. Nutr Rev. 2011;69(1):52–60. doi: 10.1111/j.1753-4887.2010.00361.x. http://dx.doi.org/10.1111/j.1753-4887.2010.00361.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenkranz RR, Dzewaltowski DA. Model of the home food environment pertaining to childhood obesity. Nutr Rev. 2008;66(3):123–40. doi: 10.1111/j.1753-4887.2008.00017.x. http://dx.doi.org/10.1111/j.1753-4887.2008.00017.x. [DOI] [PubMed] [Google Scholar]
- 13.Headland M, Clifton PM, Carter S, Keogh JB. Weight-Loss Outcomes: A Systematic Review and Meta-Analysis of Intermittent Energy Restriction Trials Lasting a Minimum of 6 Months. Nutrients. 2016;8(6):354. doi: 10.3390/nu8060354. http://dx.doi.org/10.3390/nu8060354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mann T, Tomiyama AJ, Westling E, Lew AM, Samuels B, Chatman J. Medicare’s search for effective obesity treatments: diets are not the answer. Am Psychol. 2007;62(3):220. doi: 10.1037/0003-066X.62.3.220. http://dx.doi.org/10.1037/0003-066X.62.3.220. [DOI] [PubMed] [Google Scholar]
- 15.Collins FS, Varmus H. A new initiative on precision medicine. N Engl J Med. 2015;372(9):793–5. doi: 10.1056/NEJMp1500523. http://dx.doi.org/10.1056/NEJMp1500523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cameron LD, Muller C. Psychosocial aspects of genetic testing. Curr Opin Psychiatry. 2009;22(2):218–23. doi: 10.1097/YCO.0b013e3283252d80. http://dx.doi.org/10.1097/YCO.0b013e3283252d80. [DOI] [PubMed] [Google Scholar]
- 17.Müller M, Kersten S. Nutrigenomics: goals and strategies. Nat Rev Genet. 2003;4(4):315–22. doi: 10.1038/nrg1047. http://dx.doi.org/10.1038/nrg1047. [DOI] [PubMed] [Google Scholar]
- 18.Senior V, Marteau TM, Peters TJ. Will genetic testing for predisposition for disease result in fatalism? A qualitative study of parents responses to neonatal screening for familial hypercholesterolaemia. Soc Sci Med. 1999;48(12):1857–60. doi: 10.1016/s0277-9536(99)00099-4. http://dx.doi.org/10.1016/S0277-9536(99)00099-4. [DOI] [PubMed] [Google Scholar]
- 19.Cameron LD, Marteau TM, Brown PM, Klein WM, Sherman KA. Communication strategies for enhancing understanding of the behavioral implications of genetic and biomarker tests for disease risk: the role of coherence. J Behav Med. 2012;35(3):286–98. doi: 10.1007/s10865-011-9361-5. http://dx.doi.org/10.1007/s10865-011-9361-5. [DOI] [PubMed] [Google Scholar]
- 20.Waters EA, Muff J, Hamilton JG. Multifactorial beliefs about the role of genetics and behavior in common health conditions: prevalence and associations with participant characteristics and engagement in health behaviors. Genet Med. 2014;16(12):913–21. doi: 10.1038/gim.2014.49. http://dx.doi.org/10.1038/gim.2014.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sanderson SC, Diefenbach MA, Streicher SA, Jabs EW, Smirnoff M, Horowitz CR, Zinberg R, Clesca C, Richardson LD. Genetic and lifestyle causal beliefs about obesity and associated diseases among ethnically diverse patients: a structured interview study. Public Health Genomics. 2012;16(3):83–93. doi: 10.1159/000343793. http://dx.doi.org/10.1159/000343793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. [Accessed August 2, 2016];Genetic influences on weight. WebMD website. http://www.webmd.com/diet/tc/genetic-influences-on-weight-topic-overview.
- 23.Condit CM. Public understandings of genetics and health. Clin Genet. 2010;77(1):1–9. doi: 10.1111/j.1399-0004.2009.01316.x. http://dx.doi.org/10.1111/j.1399-0004.2009.01316.x. [DOI] [PubMed] [Google Scholar]
- 24.Houfek JF, Atwood JR, Wolfe RM, Agrawal S, Reiser GM, Schaefer GB, Rennard SI. Knowledge and beliefs about genetics and smoking among visitors and staff at a health care facility. Public Health Nurs. 2008;25(1):77–87. doi: 10.1111/j.1525-1446.2008.00682.x. http://dx.doi.org/10.1111/j.1525-1446.2008.00682.x. [DOI] [PubMed] [Google Scholar]
- 25.Quaak M, Smerecnik C, van Schooten FJ, de Vries H, van Schayck CP. Knowledge, attitudes and preferences regarding genetic testing for smoking cessation. A cross-sectional survey among Dutch smokers. BMJ Open. 2012;2(1):e000321. doi: 10.1136/bmjopen-2011-000321. http://dx.doi.org/10.1136/bmjopen-2011-000321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vartanian LR, Herman CP, Wansink B. Are we aware of the external factors that influence our food intake? Health Psychol. 2008;27(5):533. doi: 10.1037/0278-6133.27.5.533. http://dx.doi.org/10.1037/0278-6133.27.5.533. [DOI] [PubMed] [Google Scholar]
- 27.Dar-Nimrod I, Heine SJ. Genetic essentialism: on the deceptive determinism of DNA. Psychol Bull. 2011;137(5):800. doi: 10.1037/a0021860. http://dx.doi.org/10.1037/a0021860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McBride CM, Bryan AD, Bray MS, Swan GE, Green ED. Health behavior change: can genomics improve behavioral adherence? Am J Public Health. 2012;102(3):401–5. doi: 10.2105/AJPH.2011.300513. http://dx.doi.org/10.2105/AJPH.2011.300513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheera EK, Klarich DS, Hong MY. Psychological and behavioral effects of genetic risk testing for obesity: a systematic review. Per Med. 2016;13(3):265–77. doi: 10.2217/pme-2015-0013. http://dx.doi.org/10.2217/pme-2015-0013. [DOI] [PubMed] [Google Scholar]
- 30.Bouhlal S, McBride CM, Trevedi NS, Agurs-Collins T, Persky S. Identifying eating behavior phenotypes and their correlates: A novel direction toward improving weight management interventions. Appetite. 2017;111:142–150. doi: 10.1016/j.appet.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ferrante JM, Piasecki AK, Ohman-Strickland PA, Crabtree BF. Family physicians’ practices and attitudes regarding care of extremely obese patients. Obesity. 2009;17(9):1710–6. doi: 10.1038/oby.2009.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9(12):788–805. doi: 10.1038/oby.2001.108. http://dx.doi.org/10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 33.Sanderson SC, Persky S, Michie S. Psychological and behavioral responses to genetic test results indicating increased risk of obesity: does the causal pathway from gene to obesity matter? Public Health Genomics. 2009;13(1):34–47. doi: 10.1159/000217794. http://dx.doi.org/10.1159/000217794. [DOI] [PubMed] [Google Scholar]
- 34.Meisel SF, Wardle J. ‘Battling my biology’: psychological effects of genetic testing for risk of weight gain. J Genet Couns. 2014;23(2):179–86. doi: 10.1007/s10897-013-9628-9. http://dx.doi.org/10.1007/s10897-013-9628-9. [DOI] [PubMed] [Google Scholar]