Abstract
Objective
To prospectively examine vaping as a predictor of future cigarette smoking among youth with and without previous cigarette smoking experience. A secondary aim is to investigate whether vaping may desensitize youth to the dangers of smoking.
Methods
Analysis of prospective longitudinal panel data from the nationally-representative Monitoring the Future study. The analysis is based on 347 12th grade students who were part of a randomly-selected subsample that completed in-school surveys in 2014 and were resurveyed one year later.
Results
Among youth who had never smoked a cigarette by 12th grade, baseline, recent vapers were more than four times [RR=4.78] more likely to report past-year cigarette smoking at follow-up, even among youth who reported the highest possible level of perceived risk for cigarette smoking at baseline. Among 12th grade students who had smoked in the past but had not recently smoked at baseline, recent vapers were twice [RR=2.15] as likely to report smoking in the past 12 months at the follow-up. Vaping did not predict cessation of smoking among recent smokers at baseline. Among never-smokers at baseline, recent vapers were more than four times [RR=4.73] more likely to move away from the perception of cigarettes as posing a “great risk” of harm, a finding consistent with a desensitization process.
Conclusions
These results contribute to the growing body of evidence supporting vaping as a one-way bridge to cigarette smoking among youth. Vaping as a risk factor for future smoking is a strong, scientifically-based rationale for restricting youth access to e-cigarettes.
Keywords: electronic nicotine delivery devices, harm reduction, priority/special populations
INTRODUCTION
Use of e-cigarettes (vaping) among U.S. high school students has increased rapidly in recent years. Any vaping in the past 30 days as of 2015 was 16% among 12th graders, 14% among 10th graders, and 10% among 8th graders.1 This is rapid growth from a 30-day prevalence of near 1% among secondary school students in 2011.2 As prevalence has increased so too has concern that vaping among school-aged adolescents may be a bridge to future use of traditional combustible cigarettes.
Evidence is building to bolster this concern. Prospective observational studies provide some of the strongest possible scientific evidence to assess vaping as a risk factor for smoking. To date, five such studies based on U.S. samples have examined the issue and all find vaping to be an independent predictor of smoking initiation. Among youth who had never smoked at baseline, the odds of incident smoking were 1.75 to 2.87 times higher among youth who vaped compared to those who did not among 9th and 10th grade students,3–5 and odds were greater than six among 12th grade students.6 Among a panel of Hispanic youth at mean age 23, odds of incident smoking one year later were more than 3 times higher among vapers.7
This finding is robust across research designs. The studies noted above are all school-based samples that originally surveyed respondents in schools and then followed them longitudinally. An analysis that used random digit dialing to recruit subjects nationally throughout the U.S. found odds of incident smoking to be more than eight times higher for vapers among a sample aged 16 to 26.8
Importantly, in all these studies vaping remains a significant predictor of smoking incidence after taking into account potential confounders such as baseline smoking susceptibility. In fact, a recent analysis indicates that vaping had the greatest predictive power for incident smoking among adolescents who had the lowest propensity to smoke at baseline.9
This study focuses on vaping as a risk factor for smoking among 12th grade students originally surveyed in schools in 2014 and contributes to the field in three ways. First, to our knowledge we report the first results on this topic from a sample of schools selected to be nationally-representative. All current school-based samples on the topic sample a specific U.S. state or city, and replication of results from existing studies with a national, school-based sample strengthens the case for all these studies to directly inform national policy and regulation.
Second, the analysis examines perceived risk of harm from cigarette use as both a baseline confounder and also a possible intervening mechanism connecting vaping with future smoking. Perceived risk of harm predicts use of a wide variety of substances10–12 and is substantially associated with cigarette smoking.13 Evidence that baseline levels of perceived risk from cigarette smoking do not “explain away” the finding of vaping as an independent predictor of future smoking would show that the finding is robust across different, major measures of smoking propensity. In addition, evidence that vaping predicts later reductions in perceived risk of smoking would be an important step toward the identification of a possible desensitization process that would help explain how vaping is connected to later smoking. Lastly, we examine vaping as a predictor of future smoking among youth with past cigarette smoking experience, a group that has received relatively less attention than never-smokers. This is a preliminary step to consider whether vaping leads this group of youth away from smoking or not.
METHODS
Data
Data come from the annual Monitoring the Future (MTF) study, which since 1975 has used questionnaires administered in classrooms to survey nationally-representative samples of U.S. 12th graders in the 48 contiguous states.12,14 The project has been approved by the University of Michigan Institutional Review Board. The target sample is all schools in the contiguous United States that enroll 25 or more 12th grade students, and in 2014 the study surveyed 122 schools (105 public and 17 private). In 2014, 13,015 12th grade students completed questionnaires, for a response rate of 82%. Almost all non-response was due to school absences. This non-response did not lead to a substantial upward or downward bias of the study’s prevalence estimates for smoking and vaping in comparison to other nationally-representative, school-based surveys.15,16
The geographic areas sampled included the 28 largest metropolitan areas containing about one third of the nation’s population, as well as 136 other primary areas. In 2014, either an original school or a replacement school was obtained in 92% of the sample units.
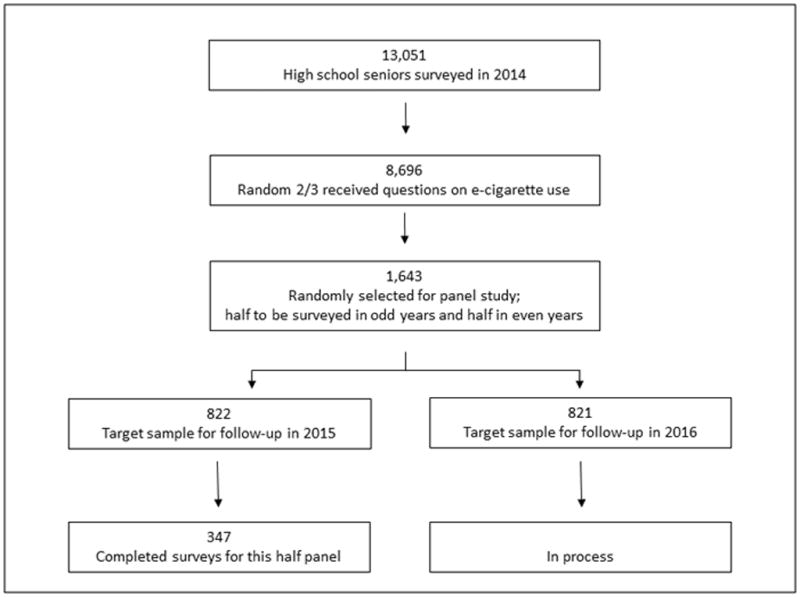
This analysis uses information from 347 follow-up participants in 2015. Figure 1 presents information on how they were selected. Every year a random subsample of 2,450 members of the 12th grade class is selected to participate in a panel that receives follow-up surveys. Questions on vaping were included on four of the six forms of the survey (the forms are randomly distributed in equal proportions). Consequently, 1,643 (~2/3) of the 2,450 respondents selected for follow-up were eligible for the analyses. To reduce respondent burden the panel is split into two random halves, with one half receiving questionnaires in even years and the other in odd years. In 2015 out of the 822 target panel respondents 347 provided sufficient information to be included in the analyses, for a response rate of 42% at modal age 19. Only respondents who had complete information on their 2015 cigarette smoking status were retained in the final analyses (97% of responders). Of these, the average length of the follow up period was 13.40 months (with a 95% confidence interval of 13.23–13.57). Tables A1 and A2 in the Appendix provide more detailed information on the sample size of the analysis pool.
Figure 1.
Statistical Analysis
We developed and used attrition weights to control the potential influence of panel attrition. The attrition weight was the inverse of the predicted probability of follow-up response, based on a regression equation modeling panel retention as a function of respondents’ baseline characteristics, which are defined in Table 1. Final weights were calculated as this attrition weight multiplied by a weight used to control the panel’s intentional oversampling of individuals with higher levels of illicit drug use at baseline.17
Table 1.
Definitions and Sample Proportions for Analysis Variables (standard errors in brackets)a
| Variable | % of follow-up subsample n=347 |
|---|---|
| Variables Measured at Baseline in 2014 | |
| Recently vaped | 15.60 |
| coded 1 for response of at least one to the question “During the LAST 30 DAYS, on how many days (if any) have you used electronic cigarettes (e-cigarettes)?” | [1.97] |
| See “great risk” in smoking | 80.88 |
| coded 1 for the response of “great risk” to the question “How much do you think people risk harming themselves (physically or in other ways) if they smoke one or more packs of cigarettes per day?” | [2.28] |
| Never smoked a cigarette | 71.05 |
| coded 1 for the response “never” to the question “Have you ever smoked cigarettes?” | [2.49] |
| Recently smoked | 10.13 |
| coded 1 for a response of “less than one cigarette a day” or more to the question “How frequently have you smoked cigarettes in the past 30 days? | [1.68] |
| Female | 56.26 |
| coded 1 for female respondents | [2.80] |
| Non-whiteb | 39.89 |
| coded 1 for respondents who did not report that they were “White (Caucasian).” | [2.77] |
| Binge drinking in past two weeks | 16.12 |
| coded 1 for a response of at least one to the question “Think back over the LAST TWO WEEKS. How many times (if any) have you had five or more drinks in a row?” | [2.00] |
| Recently smoked marijuana | 18.93 |
| Coded 1 for a response of at least one to the question “On how many occasions (if any) have you used marijuana (weed, pot) or hashish (hash, hash oil) during the last 30 days?” | [2.09] |
| Variables Measured at Follow-Up in 2015 | |
| See “great risk” in smoking | 83.05 |
| coded 1 for the response of “great risk” to the question “How much do you think people risk harming themselves (physically or in other ways) if they smoke one or more packs of cigarettes per day?” | [2.13] |
| Changed perception of risk of smoking away from “great risk” | 11.12 |
| coded 1 for respondents who saw “great risk” in smoking at baseline but not at follow-up. | [1.82] |
| Smoked in last 12 months at one-year follow-up | 21.75 |
| coded 1 for respondents who responded “smoked once or twice”, or more, to the question “What best describes your cigarette smoking in the last 12 months?” | [2.27] |
Estimates weighted for oversample of 12th grade students with high levels of drug use and for attrition
More detailed measures of race/ethnicity are precluded by small sample size
Note: Baseline questions on cigarettes ask about lifetime and past 30-day smoking, but not smoking in the past year.
Table A3 in the Appendix shows that with use of the attrition weights none of the baseline variables differed for the follow-up responders as compared to the target sample. The attrition weights took into account a higher likelihood of response for females and Whites, as well as respondents with lower levels of substance use.
To control for missing item-level data among follow-up respondents the analysis used multiple imputation with 20 imputed data sets,18 in conjunction with the survey weights. The imputation process had little effect on the study results because item-level missing data were uncommon (92% of the 347 respondents had complete information on all analysis variables). In a parallel analysis that used listwise deletion instead of multiple imputation all statistically significant differences remained, in the same direction, across the two analyses. Likewise, all significant differences remained and were in the same direction when the attrition weights were not used, both in analyses with and without multiple imputation.
The main analyses consist of two main components. First, Tables 2 and 3 examine vaping as a predictor of future smoking (detailed results presented in Tables A4 and A5). The predictive power of vaping may differ by respondents’ past level of smoking experience and/or perceived risk of harm from smoking cigarettes, and consequently the analyses are stratified by these factors. Stratification also controls any potential differential sample attrition by these factors. The multivariable models include additional controls for demographics as well as baseline levels of marijuana use and binge drinking, which serve as measures of proclivity for general substance use. The second component of the analyses examines vaping as a predictor of decreases in perceived risk of smoking, to examine whether vaping desensitizes youth to the dangers of smoking cigarettes.
Table 2.
Smoking Incidence at One-Year Follow Up among 12th Grade Students Who Had Never Smoked Traditional, Combustible Cigarettes, by Baseline Vaping (Standard Errors and 95% Relative Risk Confidence Intervals in Brackets)a
| Model | (1) | (2) |
|---|---|---|
| All | See “great risk” in smoking cigarettes | |
| n (weighted) | 246 | 204 |
| Recently vaped at time of 12th grade survey: | ||
| No | 6.75 [1.70] | 7.15 [1.96] |
| Yes | 31.07 [14.00] | 32.92 [14.99] |
| Bivariate Relative Riskb | 4.60** [1.71–12.34] | 4.59** [1.67–12.63] |
| Adjusted Relative Riskb | 4.78** [1.91–11.96] | 4.64** [1.66–12.93] |
p<.01
Estimates weighted.
Differences across e-cigarette use groups modeled in a binomial regression with a log link. See Table A4 for detailed presentation of the controls in the models for adjusted relative risk.
Table 3.
Prevalence of Past 12-Month Smoking at One-Year Follow Up among 12th Grade Students Who Had Ever Smoked, by Baseline Vaping Status (Standard Errors and 95% Relative Risk Confidence Intervals in Brackets)a
| n (weighted) | All | Non-Recent Smoking at 12th Grade Surveyc | Recent Smokers at 12th Grade Surveyc |
|---|---|---|---|
| 101 | 66 | 35 | |
| Recently vaped at time of 12th grade survey | |||
| No | 37.44 [6.73] | 27.45 [6.78] | 76.93 [13.72] |
| Yes | 80.18 [5.78] | 62.70 [10.62] | 94.86 [3.69] |
| Bivariate Relative Riskb | 2.14** [1.46–3.14] | 2.28** [1.27–4.10] | 1.23 [.87–1.73] |
| Adjusted Relative Riskb | 2.15* [1.49–3.12]* | 2.26** [1.22–4.18] | 1.32 [.89–1.96] |
p<.05;
p<.01
Estimates weighted.
Differences across e-cigarette use groups modeled in a binomial regression with a log link. Not all controls could be included in each adjusted model due to convergence issues; see Table A4 for detailed presentation of multivariable models.
Non-recent smoking defined as youth who smoked at some time in the past but not in 30 days prior to the 12th grade survey, and recent smokers defined as those who smoked in the 30 days prior to the 12th grade survey
RESULTS
Table 1 presents the proportions and definitions of the study variables. The prevalence of vaping ranked among the highest of all substance use,19 and prevalence of recent vaping (in the past 30 days) was about 50% higher than prevalence of recent smoking (smoked combustible cigarettes in the past 30 days). Cigarette smoking was considered harmful by most, with the percentage seeing great risk in smoking one or more packs of cigarettes per day over 80% at both the baseline and follow-up surveys.
Table 2 presents incidence of cigarette smoking among respondents who had never smoked a cigarette up to the time of the 12th grade survey. For this group, the incidence of smoking within the past 12 months in 2015 was about four times higher for youth who vaped at baseline as compared to those who did not, at 31% and 7%, respectively (Model 1). This difference remained after statistically controlling the potential confounders of sex, race, and parental education. Among the group of new smokers at follow-up who had recently vaped at baseline, all reported that they had smoked cigarettes at the level of “once or twice” in the past 12 months at follow-up.
Model 2 of Table 2 presents results for the subgroup of never-smokers who at baseline saw great risk in cigarette smoking. This group would presumably be the least likely to consider cigarette smoking in the future. Even among this group, recent vaping at baseline strongly predicted incidence of cigarette smoking in the following year.
Table 3 presents prevalence of any cigarette smoking in the past 12 months among respondents who had ever smoked a cigarette by the time of the 12th grade survey. For this group the prevalence of past 12-month smoking at follow-up was more than twice as high for baseline recent vapers compared to non-vapers at baseline, at 80% and 37%, respectively. This difference was statistically significant in bivariate and multivariable analyses.
Table 3 also presents results stratified by smoking activity in the 30 days prior to the 12th grade survey. Vaping significantly predicted cigarette smoking in the past 12 months at follow-up among youth who had smoked in the past but not recently (63% vs. 27%), but did not reach significance among youth who had smoked recently (95% vs. 77%). To test whether the predictive power of vaping was significantly different across these two groups of youth we modeled past-12-month prevalence at follow-up as a function of baseline recent vaping, baseline recent smoking, and the multiplicative interaction between these two dichotomies. The significance level of the interaction term was p<.062, which meets criteria as “statistically significant” to the extent that multiplicative interaction terms warrant higher probability cutoffs.20
Among youth with past smoking experience the analysis examined potential differences by level of past cigarette use (analyses not presented in the Tables). About half (50.73%, se=5.06) of non-recent smokers in 12th grade were experimental smokers who reported that they had smoked a cigarette just “once or twice” in their life. For this subgroup vaping was a significant predictor of past-year smoking at the follow-up survey (bivariate relative risk=2.75; 95% confidence interval=1.17–6.76). The other half of youth with past smoking experience reported that before 12th grade they smoked “occasionally but not regularly” or “regularly in the past.” For this subgroup vaping was not a significant predictor of past-year smoking in the follow-up survey (bivariate relative risk=1.60; 95% confidence interval=.88–2.91). However, the relative risk estimates did not significantly differ across the two groups, making these differences across the two groups only suggestive (relative risk differences tested with a multiplicative interaction term in a model that included all past smokers).
Table 4 presents baseline recent vaping as a predictor of changes in perception of cigarette smoking away from “great risk” to a lower level during the study period. Among respondents who had never smoked a cigarette by the 12th grade survey, recent vapers compared to non-vapers were four times more likely to move away from the view that cigarette smoking poses a “great risk.” This predictive association was statistically significant in bivariate and multivariable models both of all never-smokers as well as never-smokers who saw “great risk” in cigarette smoking at the baseline survey. No predictive association for recent vaping on risk perception was present among respondents who had ever smoked cigarettes at the baseline survey.
Table 4.
Percentage Who Changed Their Perceived Risk of Smoking Away from “Great Risk” at Follow-up Wave (Standard Errors and 95% Relative Risk Confidence Intervals in Brackets)a
| Smoking status: | --- Never smoked by 12th grade --- | Smoked by 12th grade | |
|---|---|---|---|
| All | See “great risk” in smoking cigarettes | All | |
| n (weighted) | 246 | 204 | 101 |
| Recently vaped at time of 12th grade survey: | |||
| No | 9.01 [2.04] | 10.92 [2.44] | 14.12 [5.05] |
| Yes | 41.27 [16.58] | 41.73 [16.68] | 11.65 [5.70] |
| Bivariate Relative Riskb | 4.56** [1.87–11.11] | 3.81** [1.57–9.21] | 0.82 [.29–2.83] |
| Adjusted Relative Riskb | 4.73** [2.07–10.82] | 3.74** [1.57–8.89] | 0.69 [.19–2.49] |
p<.01
Estimates weighted
differences across e-cigarette use groups modeled in a binomial regression with a log link. Adjusted relative risk controls sex, parental education, and race (white v. non-white).
Note: Analysis includes five cases with imputed data for the dependent variable. Results changed only trivially when these five cases were removed from the analysis. See Table A5 for detailed presentation of multivariable models.
DISCUSSION
Two aims motivated this study. The first was to examine vaping in 12th grade as a predictor of future smoking of traditional combustible cigarettes, among youth with and without smoking experience at baseline. The second was to examine whether youth who vaped later downgraded their perception of the risks of smoking. Study participants were drawn from a nationally-representative sample of students in U.S. private and public schools in 2014 and followed up one year later in 2015.
Among 12th grade students who had never smoked combustible cigarettes, vaping strongly predicted smoking initiation a year later. First use of a combustible cigarette at follow-up was reported by 31% of those who had recently vaped at the baseline survey, as compared to 7% among those who not. The analysis also examined the group of non-smokers who at baseline reported the highest level of perceived risk for smoking; these adolescents would be expected to have the lowest predisposition to start smoking cigarettes. Even among this group, recent vaping was a strong predictor of smoking initiation, which was 33% for vapers as compared to 7% among non-vapers.
Desensitization to the dangers of smoking may play a role in explaining how vaping can progress to smoking among youth who have no history of cigarette use. Youth who begin to vape primarily to experiment and because they taste good (the most common reasons for vaping21) may detect no immediate health consequences and conclude that the dangers of smoking are exaggerated. Empirical support for a desensitization process comes from this study’s finding that youth who vaped were significantly more likely to change their perception of the dangers of smoking away from “great risk,” among those who had never smoked at baseline.
The analysis also examined vaping as a predictor of cigarette smoking among students with smoking experience by 12th grade. Among those who had not recently smoked at the baseline survey, vaping strongly predicted any cigarette smoking in the past 12 months at the follow-up. In contrast, among students who were recent smokers at the baseline survey, the prevalence of past 12 month smoking at the follow-up did not differ significantly by vaping at baseline.
Health Policy Implications
Developing a rationale to regulate youth access to e-cigarettes will require more than a simple extension of the arguments used to regulate combustible cigarettes. Currently lacking for e-cigarettes is a developed body of scientific evidence documenting their health dangers, a body of evidence that exists for combustible cigarettes and plays a central role in the rationale for their regulation. The development of such evidence for the direct effects of e-cigarettes may require many years or even decades (as it did for regular cigarettes), and once this body is developed e-cigarette manufacturers could change their ingredients and the process may need to start all over again. In addition, recent research shows that the majority of youth who vape report that they vape “just flavoring” and not nicotine.22 Consequently, regulations and policies based on a rationale of nicotine regulation may not necessarily apply to youth e-cigarette use in a straightforward way.
One important rationale to regulate e-cigarettes is that they lead to use of combustible cigarettes among youth. This rationale builds on the already-existing consensus and political will to reduce youth cigarette smoking, given that most people would favor age restrictions on sale of devices that lead youth to smoke.
This study strengthens the evidence that vaping is a risk factor for cigarette smoking among youth in three ways. First, it contributes the first findings based on a sample of schools selected to be nationally-representative of the U.S. to the growing body of evidence linking vaping to later smoking incidence among youth who had never smoked at baseline. Now four studies have used school-based samples of adolescents to investigate this topic longitudinally, and all support vaping as an independent predictor of smoking incidence, taking into account predisposition to smoke at baseline.3,4,6 These findings are particularly important given that vaping is one of the most common forms of substance use among youth who have never smoked, with a current prevalence of 4% for this group.
Second, the study’s evidence for a potential role for perceived risk is an important step in the identification of mechanisms that link vaping to later smoking incidence among never smokers. The intervening mechanisms at work may not necessarily be linked to chemical addiction and may operate even if the substance vaped in e-cigarettes is not addictive or physically harmful. Other candidate intervening mechanisms include smoking expectancies, peer smoker affiliations, and attitudes toward smokers.23 The planned, future addition of a third wave of data will allow testing of a formal mediation model.
Finally, this study is one of few to consider the possibility that vaping may lead youth with past smoking experience to return to smoking. Among youth who had smoked in the past but had not recently smoked at the time of survey, those who vaped were about twice as likely to have smoked at least one cigarette in the past 12 months at the follow-up. Vaping did not divert this group away from smoking.
We note four limitations of this study. First, the analyses do not take into account what substances youth vaped in their e-cigarettes. Such questions were asked in more recent surveys, so in the future it will be possible to test if the overall predictive power of vaping for future smoking incidence differs among subgroups who vape different types of substances.
A second limitation is that the sample size of the analysis did not allow detailed examination of important subgroups. For example, analysis of racial/ethnic categories beyond white and non-white led to groupings that were too small to support statistical analysis. The sample size also did not allow analysis by different frequency of vaping in the past 30 days at baseline. In future years, the sample size will grow considerably with the addition of new cohorts that can be combined with this one, which will allow more detailed analysis of possible differences in the overall findings across specific subgroups.
A third limitation is that not all target follow-up respondents returned surveys, which introduces the possibility of response bias. Subgroups that are more likely to respond may exert a larger influence than their size warrants on the study results. In particular, for this study any differential sampling response by groups with high predisposition to smoke cigarettes at baseline or smoking experience at baseline have potential to confound the results. To address this possibility the analyses stratify by these factors, with perceived risk of smoking as an indicator of predisposition to smoke. Stratification of analyses by key groups takes into account both substantive confounding as well as any confounding that results from their potentially different levels of survey response. Confidence that response bias does not seriously confound the study results is strengthened both by the stratification procedure as well as the finding from the attrition analyses that the stratified subgroups showed no major difference in proportionate size among follow-up responders as compared to the target panel sample. To be thorough, the study’s attrition weighting addresses the small differences in response rates by groups, and this attrition weighting did not change the study’s substantive results or conclusions.
A fourth limitation is that the data do not contain specific questions related to tobacco use such as smoking susceptibility, smoking expectations, rebelliousness, affiliation with smokers in the community, and perception of friends’ attitudes toward smoking. Such questions would allow more comprehensive, statistical control of the predisposition of youth to smoke cigarettes. The analyses control for these influences in part by controlling general substance use at baseline, through which many of these influences would act, and still find support for vaping as an independent predictor of future smoking. These results are consistent with other school-based studies in this literature that include controls for these factors3,4,6 and still find that vaping significantly predicts future smoking. Taken together, existing studies suggest that it is unlikely that predisposition to smoke can “explain away” the association of vaping with future cigarette smoking.
In conclusion, these results bolster findings for vaping as a one-way bridge to cigarette smoking among adolescents. To our knowledge, the risk for future cigarette smoking is currently one of the strongest, scientific-based rationales for restricting youth access to e-cigarettes.
Supplementary Material
What this paper adds.
This paper contributes to the growing body of evidence that e-cigarette use is an independent risk factor for future smoking, both among youth who are non-smokers and also youth with past smoking experience. Results support a desensitization process, whereby youth who vape lower their perceived risk of cigarette smoking.
Acknowledgments
Funding This study was supported by the National Institute on Drug Abuse, part of the National Institutes of Health, by grants # R01DA001411 and R01DA016575.
Footnotes
Competing interests None.
Contributors: LJ is the Principal Investigator of the Monitoring the Future Study, and the other authors are all co-Investigators. RM developed the paper plan, performed the data analysis, and drafted the manuscript, assisted by MP. All authors contributed to drafts of the manuscript.
Ethics approval University of Michigan Institutional Review Board, approval #HUM00063656
Data sharing statement The data are drawn from a wider survey that examines trends in the use of a variety of substances among adolescents, as well as trends in many substance use related variables. Each year a de-identified version of the previous year’s data is made publicly available and can be downloaded for no charge at: http://www.icpsr.umich.edu/icpsrweb/NAHDAP/index.jsp. Researchers wishing to use sensitive data that cannot be publicly released should send a request to mtfinformation@umich.edu to start the application process.
References
- 1.Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use: 1975–2015: Overview of Key Findings on Adolescent Drug Use. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2016. [Google Scholar]
- 2.Singh T. Tobacco Use Among Middle and High School Students—United States, 2011–2015. MMWR Morbidity and mortality weekly report. 2016:65. doi: 10.15585/mmwr.mm6514a1. [DOI] [PubMed] [Google Scholar]
- 3.Leventhal AM, Strong DR, Kirkpatrick MG, et al. Association of Electronic Cigarette Use With Initiation of Combustible Tobacco Product Smoking in Early Adolescence. JAMA. 2015;314(7):700–707. doi: 10.1001/jama.2015.8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wills TA, Knight R, Sargent JD, Gibbons FX, Pagano I, Williams RJ. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tobacco control. doi: 10.1136/tobaccocontrol-2015-052705. Published Online First: January 25, 2016:tobaccocontrol-2015-052705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leventhal AM, Stone MD, Andrabi N, et al. Research Letter: Association of e-Cigarette Vaping and Progression to Heavier Patterns of Cigarette Smoking. JAMA. 2016;316(18):1918–1919. doi: 10.1001/jama.2016.14649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barrington-Trimis JL, Urman R, Berhane K, et al. E-Cigarettes and Future Cigarette Use. Pediatrics. 2016 doi: 10.1542/peds.2016-0379. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Unger JB, Soto DW, Leventhal A. E-cigarette use and subsequent cigarette and marijuana use among Hispanic young adults. Drug and alcohol dependence. 2016;163:261–264. doi: 10.1016/j.drugalcdep.2016.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Primack BA, Soneji S, Stoolmiller M, Fine MJ, Sargent JD. Progression to traditional cigarette smoking after electronic cigarette use among US adolescents and young adults. JAMA pediatrics. 2015;169(11):1018–1023. doi: 10.1001/jamapediatrics.2015.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wills TA, James D. Sargent, Frederick X. Gibbons, Ian Pagano, and Rebecca Schweitzer. E-Cigarette Use is Differentially Related to Smoking Onset Among Lower Risk Adolescents. Tobacco control. 2016 doi: 10.1136/tobaccocontrol-2016-053116. (Published Online First, 9/9/2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bachman JG, Johnston LD, O’Malley PM. Explaining recent increases in students’ marijuana use: Impacts of perceived risks and disapproval. American Journal of Public Health. 1998;88:887–892. doi: 10.2105/ajph.88.6.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bachman JG, Johnston LD, O’Malley PM, Humphrey RH. Explaining the recent decline in marijuana use: Differentiating the effects of perceived risks, disapproval, and general lifestyle factors. Journal of Health and Social Behavior. 1988;29:92–112. [PubMed] [Google Scholar]
- 12.Miech RA, Johnston L, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Survey Results on Drug Use, 1975–2015: Volume I, Secondary School Students. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2016. [Google Scholar]
- 13.Bachman JG, O’Malley PM, Schulenberg JE, Johnston L, Bryant AL, Merline AC. The Decline of Substance Use in Young Adulthood: Changes in Social Activities, Roles, and Beliefs. Mahwah, New Jersey: Lawrence Erlbaum; 2002. [Google Scholar]
- 14.Bachman JG, Johnston LD, O’Malley PM, Schulenberg JE, Miech RA. The Monitoring the Future Project after Four Decades: Design and Procedures. Occasional Paper #82. 2015 http://monitoringthefuture.org/pubs/occpapers/mtf-occ82.pdf.
- 15.Arrazola RA, Singh T, Corey CG, et al. Tobacco use among middle and high school students—United States, 2011–2014. MMWR Morbidity and mortality weekly report. 2015;64(14):381–385. [PMC free article] [PubMed] [Google Scholar]
- 16.Kann L. Youth Risk Behavior Surveillance—United States, 2015. MMWR Surveillance Summaries. 2016:65. doi: 10.15585/mmwr.ss6506a1. [DOI] [PubMed] [Google Scholar]
- 17.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Miech RA. Monitoring the Future National Survey Results on Drug Use, 1975–2013: Volume 1, Secondary School Students. Ann Arbor: Institute for Social Research, The University of Michigan; 2014. [Google Scholar]
- 18.Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A Multivariate Technique for Multiply Imputing Missing Values Using a Sequence of Regression Models. Survey Methodology. 2001;27:85–95. [Google Scholar]
- 19.Miech RA, Johnston L, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Survey Results on Drug Use, 1975–2014: Volume I, Secondary School Students. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2015. [Google Scholar]
- 20.Selvin S. Statistical analysis of epidemiologic data. Oxford University Press; 2004. [Google Scholar]
- 21.Patrick ME, Miech RA, Carlier C, O’Malley P, Johnston LD, Schulenberg JE. Self-Reported Reasons for Vaping among 8th, 10th, and 12th Graders in the US: Nationally-Representative Results. Drug and Alcohol Dependence. doi: 10.1016/j.drugalcdep.2016.05.017. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miech RA, Patrick ME, O’Malley PM, Johnston LD. What Are Kids Vaping? Results from a National Sample of U.S. Adolescents. Tobacco control. doi: 10.1136/tobaccocontrol-2016-053014. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wills T, Gibbons F, Sargent J, Schweitzer R. How Is the Effect of Adolescent E-Cigarette Use on Smoking Onset Mediated: A Longitudinal Analysis. Psychology of addictive behaviors: journal of the Society of Psychologists in Addictive Behaviors. 2016 doi: 10.1037/adb0000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


