Abstract
The convention of prescribing hemodialysis on a thrice weekly schedule began empirically when it seemed that this frequency was convenient and likely to treat symptoms for a majority of patients. Later, when urea was identified as the main target and marker of clearance, studies supported the prevailing notion that thrice weekly dialysis provided appropriate clearance of urea. Today, national guidelines on hemodialysis from most countries recommend patients receive at least thrice weekly therapy. However resource constraints in low- and middle-income countries have resulted in a substantial proportion of patients using less frequent hemodialysis in these settings. Observational studies of patients on twice weekly dialysis show that twice weekly therapy has non-inferior survival rates compared with thrice weekly therapy. In fact, models of urea clearance also show that twice weekly therapy can meet urea clearance “targets” if patients have significant residual function or if they follow a protein-restricted diet, as may be common in low- and middle-income countries. Greater reliance on twice weekly therapy, at least at the start of hemodialysis, therefore has potential to reduce health care costs and increase access to renal replacement therapy in low-resource settings; however, randomized control trials are needed to better understand long-term outcomes of twice versus thrice weekly therapy.
Keywords: renal replacement therapy, frequency of hemodialysis, low- and middle-income countries, health care costs
The overwhelming majority of persons with end-stage renal disease in the U.S., Western Europe, Australia or Japan initiate in-center hemodialysis for 3–4 hours per session, three sessions a week. Why is thrice weekly hemodialysis “conventional”?
History of thrice weekly hemodialysis
Schribner et al. provide a narrative rationale.1 In the early 1960s, nephrologists at the Seattle Kidney Center had been customizing the dose and frequency of hemodialysis to treat persons’ uremic symptoms (among the most recalcitrant was peripheral neuropathy). In 1966, they reported success in treating 22 persons, mostly via a twice weekly schedule [Table 1].2 Of note, they asked patients on dialysis to follow a 400 mg sodium, 40 g protein restricted diet.
Table 1. Dialysis Duration and Frequency for some of the first persons on dialysis at the Seattle Kidney Center.
Adapted from Pendras et al. The original table lists creatinine clearance, body weight, dialysis duration, and dialysis frequency for each patient. Average time per dialysis session was calculated based on the reported dialysis duration and frequency.
| Person | Creatinine Clearance (ml/min) | Body Weight (kg) | Dialysis Duration (Hours/Week) | Dialysis Frequency (Sessions/Week) | Average Time per Dialysis Session (Hours/Session) |
|---|---|---|---|---|---|
| DB | 0 | 42.6 | 28 | 2 | 14 |
| LO | 0 | 53 | 32 | 2 | 16 |
| CY | 0 | 53.8 | 28 | 2 | 14 |
| FW | 0 | 61.1 | 40 | 3 | 13.3 |
| MM | 0 | 62.7 | 32 | 2 | 16 |
| PF | 0 | 63 | 32 | 2 | 16 |
| FS | 0 | 65.1 | 36 | 3 | 12 |
| JA | 0 | 65.2 | 36 | 3 | 12 |
| SS | 0 | 66 | 32 | 2 | 16 |
| JM | 0 | 66.3 | 32 | 2 | 16 |
| KH | 0 | 80.3 | 32 | 2 | 16 |
| JM | 0 | 93 | 40 | 3 | 13.3 |
| FT | 0.4 | 62 | 28 | 2 | 14 |
| MM | 0.5 | 51 | 28 | 2 | 14 |
| ES | 0.9 | 69.3 | 36 | 3 | 12 |
| DD | 1.4 | 74 | 32 | 2 | 16 |
| ML | 2 | 46.9 | 28 | 2 | 14 |
| CL | 2.1 | 86.3 | 32 | 2 | 16 |
| NO | 2.1 | 86.5 | 36 | 3 | 12 |
| SA | 2.2 | 51 | 26 | 2 | 13 |
| BF | 3.7 | 75.6 | 24 | 2 | 12 |
| GG | 5.2 | 70.1 | 32 | 2 | 16 |
Average value for three most recent months of dialysis.
When the Center began a home hemodialysis program, persons expressed an interest in shorter sessions while sleeping at night. Thus, the nephrologists split the approximately 24–30 hours of total dialysis time in 8–10 hours three times weekly. As the authors put it: “It soon became obvious that dialysis 8 to 10 hr three times weekly seemed to control all the major life-threatening complications. As a result, this became the usual dialysis schedule and we stopped our crude efforts to adjust the treatment schedule based on patient symptoms.1” With the advent of higher surface area dialyzers, session length gradually shortened but the thrice weekly frequency became embedded in the conventional hemodialysis prescription, and, when Medicare began funding dialysis in 1973, in the reimbursement lexicon.
Around the same time, the National Cooperative Dialysis Study (NCDS), the first large-scale clinical trial focused on hemodialysis dose, evaluated the frequency of uremia-associated hospitalization among patients randomized to higher versus lower time-average urea targets, and longer (4.5–5 hours) versus shorter (3 hours) session length; the latter was used as a proxy for middle molecule clearance.3 Subsequent trials have studied whether higher Kt/Vurea targets, longer session lengths, or more frequent treatment schedules improve outcomes, but none have studied whether less frequent hemodialysis might be sufficiently therapeutic. Current guidelines from nephrology societies based in the U.S., Europe, and Japan generally assume at least a thrice weekly frequency; only two describe a less frequent strategy in the presence of significant residual function (Table 2).
Table 2.
Society guidelines for conventional and alternate hemodialysis prescriptions.
| Society | Conventional hemodialysis prescription | Alternate hemodialysis Prescriptions | Single pool Kt/V |
|---|---|---|---|
| National Kidney Foundation Kidney Disease Outcomes Quality Initiative (NKF/KDOQI) 201525 | 3–4 sessions/wk; minimum of 3 h/session | Persons may opt for in-center, short, frequent hemodialysis (<3 h/session, 5–7 sessions/wk). Persons with sufficient residual renal function may opt for a lower dose of hemodialysis. However, residual function should be measured regularly to ensure that the prescribed dose is not sub-therapeuic. Persons not on a thrice weekly schedule should have a target standard Kt/V of 2.3 and a minimum standard Kt/V of 2.1; measurement of Kt/V should account for ultrafiltration and endogenous kidney function. |
Target: 1.4; Minimum: 1.2 |
| European Renal Association/European Dialysis and Transplant Association (ERA/EDTA)26 | 3 sessions/wk, 12 h/wk | Increase dialysis time/frequency in persons with hemodynamic instability, cardiovascular instability, persistent hypertension, and reduced phosphate control | Target: ≥ 1.4 |
| Japanese Society for Dialysis Therapy (JSDT) 201527 | 4 h/session minimum if person gets 3 sessions/wk | Minimum: 1.4; but 1.2 is acceptable in persons with a large body size | |
| Canadian Society of Nephrology (CSN) 200628 | 3 sessions/wk, 4 h/session | Frequent or sustained hemodialysis can be used for persons with poorly controlled blood pressure. | Minimum: 1.2 |
| Kidney Health Australia-Caring for Australasians with Renal Impairment (KHA-CARI) 200517,29 | 3 sessions/wk, 4 h/session; Optimal: 6–8 h/session, 5–6 sessions/wk, nighttime | Persons with cardiovascular comorbidities or hemodynamic instability and the elderly can consider a hemodialysis regimen with increased treatment time or frequency. | Target: 1.4; Minimum: 1.2 |
| UK Renal Association 201130 | 3 sessions/wk, 4 h/session | Twice weekly hemodialysis without an increase in session duration may be acceptable temporarily in persons with adequate residual renal function (eGFR > 5 ml/min/1.73m2) | Minimum: 1.3 |
Prevalence of twice weekly dialysis and associated outcomes
Prevalence
Resource constraints in middle-income countries with burgeoning numbers of patients with ESRD—such as India, China, and Iran—now translates into a substantial proportion of the persons able to access hemodialysis undertaking fewer than three sessions per week (Figure 1).
Figure 1. Available data on distribution of persons receiving <3 vs. ≥3 sessions of hemodialysis per week by country.
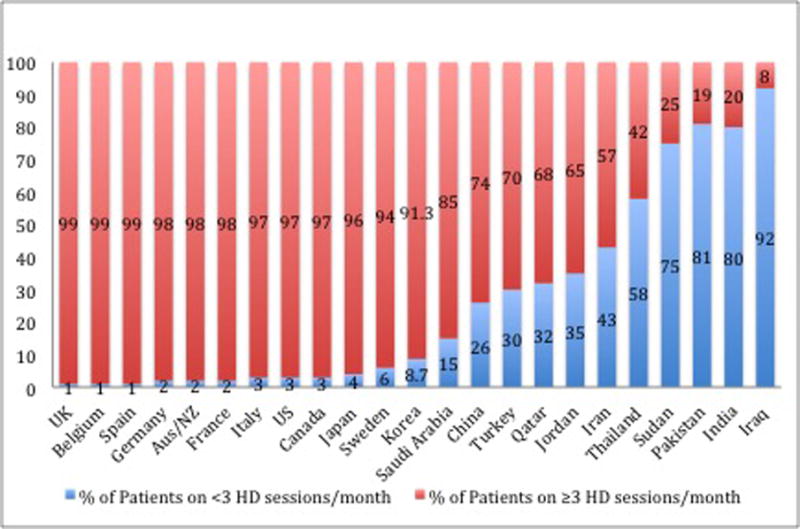
Adapted from Bieber et al.9 We added data from Saudi Arabia, Turkey, Qatar, Jordan, Iran, Thailand, Sudan, Pakistan, India, and Iraq. 3,20–24 Data from Jordan, Qatar, Iran, and Turkey are drawn from national registries, data from Pakistan, Iraq and Saudi Arabia are drawn from from multi-center studies, and data from India, Thailand, and Sudan are drawn from single-center studies.3,20–24
Survival
While high quality data are sparse, most observational data show no difference in survival among persons on thrice or more versus twice weekly hemodialysis. Table 3 summarizes the available observational data on survival on twice versus thrice weekly hemodialysis.
Table 3.
Review of clinical studies assessing mortality of patients on twice- vs. thrice-weekly hemodialysis.
| Author | Setting | Incident | Prevalent | Residual function | Mortality | |
|---|---|---|---|---|---|---|
|
| ||||||
| N | N | HR or RR | 95% CI | |||
| Lin, X | China | _ | 2572 | N/A | 0.8 | 0.6–1.1 |
| Obi, Y | U.S. | 8419 | Y | 1 | 0.8–1.3 | |
| N | 1.6 | 1.0–2.5 | ||||
| Hanson, J | U.S. | 4888 | 10179 | Y | 1 | |
| N | 0.8 | |||||
| Hwang | Korea | 113 | Y | 4.20 | 1.02–17.32 | |
Lin et al. studied a cohort of 2,572 persons receiving maintenance hemodialysis from the Shanghai Renal Registry and found that survival rates of persons receiving twice weekly dialysis were non-inferior to those of persons receiving thrice weekly dialysis.4 In certain subgroups, including persons starting dialysis or those extended dialysis vintage (longer than five years), persons on less frequent hemodialysis experienced better survival. While data on residual kidney function were not available, it is reasonable to assume that most patients whose vintage was five or more years had negligible residual kidney function—but also important to consider that the patients who survived for 5 years likely enjoyed greater health at the start of dialysis.4
Obi et al. performed a retrospective analysis of patients receiving hemodialysis at facilities operated by DaVita, Inc., a large for-profit dialysis provider in the U.S. Among 23,645 prevalent patients, roughly 2% (n=351) were prescribed twice weekly hemodialysis regimen for at least 52 weeks at the start of their dialysis experience.5 Patients on twice weekly dialysis with little to no residual kidney function experienced higher all-cause mortality compared with those with similarly low residual kidney function on the thrice weekly schedule. In contrast, among patients with substantial residual kidney function (i.e., residual urea clearance >3ml/min/1.73m2, matching the thresholds recommended by the Kidney Disease Outcomes Quality Initiative [KDOQI] when considering less frequent dialysis), there was no difference in survival by frequency (twice versus thrice weekly).
In contrast, a prospective study by Hwang et al. found that the cohort on twice weekly hemodialysis had a higher mortality rate compared with the cohort on a thrice weekly schedule when both groups had some residual kidney function (defined as urine output of at least 100 ml/day).6 While the study was well designed with rigorous ascertainment of residual kidney function, the number of events in each group was small (11 deaths in total), so that confidence in the validity and precision of the result is limited. Of note, the exact volume of urine output is unknown, as patients reported whether or not the output was at least one cup. Another study in the U.S. conducted by Hanson et al. found prevalent patients on a twice weekly schedule had a 24% lower mortality risk, but there was no difference in mortality among incident patients after adjustment for residual kidney function.7
Other outcomes: residual kidney function, nutrition, and quality of life
Evidence is fairly consistent that less frequent dialysis is associated with preserved residual kidney function – the key question is whether preserved residual kidney function facilitates success on twice weekly hemodialysis (which we believe to be likely), twice (relative to thrice) weekly hemodialysis preserves residual kidney function, or both. In the study by Obi et al., regardless of the initial level of residual kidney function, patients on the ‘incremental’ (twice weekly hemodialysis at initiation) schedule experienced more sustained residual kidney function relative to patients on a conventional thrice weekly schedule.5 A Taiwanese study corroborates the notion that less frequent hemodialysis might help to preserve residual kidney function. Patients receiving thrice weekly hemodialysis experienced a faster decline in residual kidney function than patients receiving twice weekly hemodialysis, although these results were likely confounded by patient age (as younger patients tend to have more rapid progression of CKD, and were also more likely to be on thrice weekly hemodialysis).8 At the end of the study, the twice weekly cohort had lower B2-microglobulin levels and pre- and post-HD mean arterial pressures. Even in the study by Hwang et al., which showed overall poorer survival in the twice weekly group, loss of residual kidney function loss was more rapid in the thrice weekly group. Whether these findings reflect a true “protective” effect of less frequent hemodialysis, or an “effect-cause” phenomenon made evident by the definition of incremental therapy, is unknown.
Data linking the frequency of hemodialysis and dietary intake are mixed. In the study by Obi et al., patients on the twice weekly schedule had similar normalized patient catabolic rate (nPCR) (1.0 vs. 1.1 g/kg/d) and serum albumin concentrations, compared with those on the conventional thrice weekly schedule.5 In contrast, Bieber et al. found that Chinese patients dialyzing twice weekly schedule had an nPCR which was lower (0.68 versus 0.83 g/kg/day) but a serum albumin concentration which was similar to that of patients dialyzing thrice weekly.9 This indicates that protein intake was lower in the patients on twice weekly treatment.
Effects of twice versus thrice weekly hemodialysis on health-related quality of life and hospitalization are largely unknown. In their study of twice versus thrice weekly hemodialysis in China, Beiber et al. utilized the Medical Outcomes Study Short-form-12 (SF-12) to assess health-related quality of life and found that patients on twice weekly hemodialysis had slightly lower scores in both the physical and mental domains of health-related quality of life, when adjusted for differences by age and sex.9 Although one might expect a higher rate of hospitalization due to fluid overload with less frequent hemodialysis, patients in the Hwang et al. study and on the less frequent schedule did not have a substantially higher rate of hospitalization due to cardiovascular events during the course of the study.6 Assuming that hospitalization rates and costs are comparable to thrice weekly hemodialysis—e.g., because the greater risk for fluid overload and/or electrolyte imbalance on less frequent therapy is overcome either by residual kidney function or by stricter diet restrictions—less frequent hemodialysis would be expected to lower health care costs.10
Sources of bias in available data
Since all available data on twice weekly hemodialysis and outcomes are from non-randomized studies, they are first and foremost subject to confounding by indication (in other words, patients assigned to twice weekly rather than thrice weekly hemodialysis are likely to be different in ways that are not measured). Physicians are likely prescribing twice-weekly hemodialysis to patients whom they think can withstand the less frequent schedule, and perhaps enjoy greater overall health. For example, in the studies from China and Taiwan, patients on twice weekly hemodialysis were more likely to be female and had lower rates of diabetes.4,8,9 In the U.S. study by Hanson et al., patients in the twice weekly cohort were more likely to be female, Caucasian, employed, and have graduated from high school.7 In the study by Obi et al. from DaVita, patients prescribed twice-weekly hemodialysis were older and also more likely to be female and Caucasian.5 In contrast, in the Korean cohort—the only study to so far demonstrate poorer survival in association with the lower frequency of dialysis—patients on twice weekly hemodialysis were generally less healthy at baseline: slightly older, more likely to have cardiovascular disease, and had worse baseline nutritional status (as indicated by nPCR) compared to patients receiving thrice-weekly therapy – factors that may have influenced the regimen to which patients were assigned and may be related to outcomes.6
Another potential source of bias in a majority of available studies is survival bias (Table 2). Since enrollment at the start of dialysis was not mandated, persons who may have died relatively early will be missed; it is conceivable that persons assigned the less frequent therapy are more likely to die early than persons assigned the conventional therapy. Even the study from Obi et al. which examined data from the start of dialysis required persons in their cohort to be alive at one year post start of dialysis.5
Despite the limitations in current data, the preponderance of evidence suggests that twice weekly hemodialysis is safe for patients with modest residual kidney function. In fact, many patients starting dialysis likely have this degree of residual function (e.g., in the quarter prior to start of dialysis, median eGFR was 11.7 ml/min/1.73m2 in 5,989 patients at Kaiser Permanente of Southern California),11 and some experts suggest an ‘incremental’ approach, whereby patients with sufficient residual function would initiate less frequent dialysis and gradually increase treatments per week as residual function declined.10 Further they argue that such a strategy would prolong presence of residual function, the loss of which is a key determinant of mortality among patients on hemodialysis.5,12,13
Can we employ a lower frequency in absence of residual kidney function?
Residual kidney function is certainly a key consideration in nephrologists’ acceptance of the less frequent therapy; theoretically, a patient on hemodialysis with substantial residual kidney function can easily reach the same time averaged urea clearance on twice weekly hemodialysis as a patient with little or no residual kidney function on thrice weekly hemodialysis (Figure 2a). Residual kidney function can also protect persons on hemodialysis from complications associated with volume overload, with or without diuretic therapy.
Figure 2a. Predicted BUN concentration profiles for a patient on thrice weekly schedule without residual function and on a twice weekly schedule with residual function.
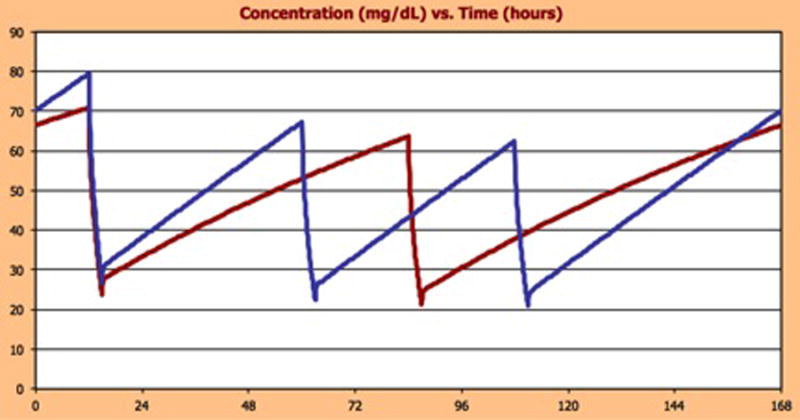
The plots show the predicted BUN concentrations for a patient receiving hemodialysis on a thrice weekly (blue line) or twice weekly (red line) schedule, with each session being 3 hours in duration. The plots are made assuming a dialytic urea clearance of 234 ml/min, urea volume of distribution of 36 liters, fluid gain of 1 liter/day and urea generation rate of 7200 mg/day. The patient’s hematocrit is assumed to be 33%. For a patient on thrice weekly dialysis with no residual renal function (blue line) the predicted average peak BUN concentration is 70 mg/dl and the time-averaged BUN is 49 mg/dl. Similar BUN values would be achieved with a twice-weekly dialysis in a patient who had a residual urea clearance of 3.7 mL/min (red line), assuming all other parameters were the same.
However, in settings where patients pay for a large share of their therapy out-of-pocket, financial constraints can influence decisions regarding prescribed hemodialysis frequency. For example, in China, patients on a twice weekly hemodialysis schedule were less likely to have national health insurance or to have completed at least twelve years of schooling.9 Fewer than 20% of patients on in-center hemodialysis are working in high-income countries. But without a social safety net, many more patients on dialysis in low- and middle-income countries are likely under obligation to work, and this may in turn lead to significant time and travel constraints as well.14,15 In such settings, even patients without substantial residual kidney function routinely undertake twice weekly hemodialysis.9
It has been assumed (but not proved) that patients on twice weekly hemodialysis with no residual kidney function do not receive “adequate” hemodialysis, based on the traditional, “urea-centric” approach to assessing dialysis dose. However, a twice weekly regimen may be acceptable if it adequately controls the levels of toxic solutes.16 A major problem in addressing this question is that we have not identified the entire range of solutes that cause uremia.17 Studies performed before dialysis became widely available showed, however, that reducing protein intake could ameliorate uremic symptoms. This suggests that the production of toxic solutes can be reduced by reducing protein intake, in which case the combination of twice weekly dialysis and protein restriction might control solute levels as effectively as thrice weekly dialysis without protein restriction (Figure 2b). In their NCDS paper that has since led to the development of Kt/V and urea clearance standards, Lowrie et al. also make this important caveat about how patients on a protein-restricted diet may behave differently than those studied.16 Additional considerations in attempting twice weekly dialysis in patients without residual function are restriction of sodium, fluid, potassium, and phosphate intake.
Figure 2b. Predicted BUN concentration profiles for a patient without residual function on a thrice weekly with an unrestricted diet and on a twice weekly schedule with dietary protein restriction.
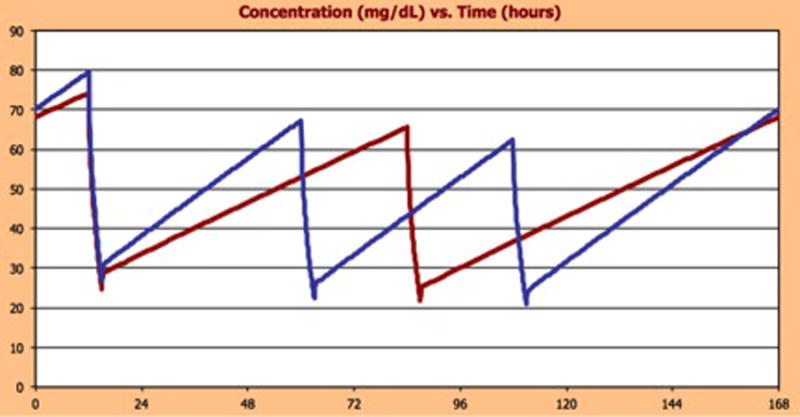
The plots show the predicted BUN concentrations for patients with no residual renal function receiving hemodialysis on thrice weekly (blue line) or twice weekly (red line) schedules, with each session being 3 hours in duration. The plots are made assuming a dialytic urea clearance of 234ml/min, fluid gain of 1 liter/day, and urea volume of distribution of 36 liters. The patient’s hematocrit is assumed to be 33%. For patients on thrice weekly dialysis with urea generation rates of 7200 mg/day (blue line) the predicted average peak concentration is 70 mg/dl and the time-averaged BUN is 49 mg/dl. Similar BUN values would be achieved on a twice weekly dialysis schedule in patient who restricted protein intake such that the urea generation rate was 4810 mg/day (red line), assuming all other parameters were the same. That protein restriction can lower BUN levels is well established. The proposition that it reduces the production of toxic solutes sufficiently to allow twice-weekly dialysis to be clinically effective in patients without residual function remains to be tested.
Financial implications of twice weekly hemodialysis in an international context
The vast majority of patients with ESRD in low- and middle-income countries (LMIC) are unable to afford any hemodialysis. For example, in South Africa, only fifty percent of the patients with ESRD can initiate government-sponsored hemodialysis.18 In India, nine out of ten patients with ESRD are unable to afford long-term renal replacement therapy.
Rather than exhausting the national budget on patients who can afford thrice weekly hemodialysis but have sufficient residual kidney function to do well on twice weekly, implementing an incremental strategy for dialysis frequency can extend dialysis therapy to more patients. In India, the total cost of hemodialysis (including the cost of the facility, therapy, and physician and staff salary) is approximately $16–21 per session.19 Hence, one year on a twice weekly schedule costs $1,733 – $2,196 whereas one year on a thrice weekly schedule costs $2,600 – $3,293. In Jordan, the cost of one session of hemodialysis is roughly $72; thus, it would cost $7,488 for one patient to be on twice weekly dialysis and $11,232 for the patient to be on thrice weekly dialysis for one year of therapy.14 In simple qualitative terms, for every two patients who spend their first year of dialysis on twice weekly rather than thrice weekly therapy, one patient could receive a year of dialysis at no additional cost to the health care system.
Other strategies to increase the proportion of patients who need hemodialysis to be able to access it include encouraging living donation and starting all (or most) patients who qualify for peritoneal dialysis on this less expensive renal replacement therapy.
Conclusion
Hemodialysis is rarely prescribed on a twice weekly schedule for those seeking optimal therapy. Internationally, patients are typically on this regimen if they cannot afford conventional, thrice weekly therapy. In the United States, patients on twice weekly hemodialysis either have ample residual kidney function or do not seek aggressive therapy for quality of life reasons. Hence, data available on the twice weekly hemodialysis regimen are sparse and are drawn from observational studies. However, available data suggest that twice weekly hemodialysis may be effective. This seems certainly true for patients with residual kidney function and may be true for patients without residual function who are able to adhere to dietary restrictions. To better assess the therapeutic efficacy of the twice weekly hemodialysis schedule, we recommend a randomized control trial examining long-term survival, hospitalizations, and health-related quality of life for patients on twice versus thrice weekly hemodialysis therapy among patients with careful ascertainment of residual kidney function.
Acknowledgments
Disclosures of Grants and Other Sources of Funding:
Dipal Savla is supported by Arnhold Institute for Global Health Research Fellowship
Dr. Chertow is supported by National Institute for Diabetes and Digestive and Kidney Health [grant # K24 DK085446].
Dr. Anand is supported by National Institute for Diabetes and Digestive and Kidney Health [grant # K23 DK101826].
Footnotes
Conflict of Interest: None
References
- 1.Scribner BH, Cole JJ, Ahmad S, Blagg CR. Why thrice weekly dialysis? 2004:188–192. doi: 10.1111/j.1492-7535.2004.01094.x. [DOI] [PubMed] [Google Scholar]
- 2.Pendras JP, Erickson RV. Hemodialysis: a successful therapy for chronic uremia. Ann Intern Med. 1966;64:293–311. doi: 10.7326/0003-4819-64-2-293. [DOI] [PubMed] [Google Scholar]
- 3.Rhee CM, et al. Infrequent Dialysis: A New Paradigm for Hemodialysis Initiation. Semin Dial. 2013;26:720–727. doi: 10.1111/sdi.12133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin X, et al. Clinical Outcome of Twice-Weekly Hemodialysis Patients in Shanghai. 2014;200001:66–72. doi: 10.1159/000334634. [DOI] [PubMed] [Google Scholar]
- 5.Obi Y, et al. Incremental Hemodialysis, Residual Kidney Function, and Mortality Risk in Incident Dialysis Patients: A Cohort Study. Am J Kidney Dis. 2016:1–10. doi: 10.1053/j.ajkd.2016.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hwang HS, et al. Comparison of Clinical Outcome Between Twice-Weekly and Thrice-Weekly Hemodialysis in Patients With Residual Kidney Function. Medicine (Baltimore) 2016;95:e2767. doi: 10.1097/MD.0000000000002767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hanson JA, et al. Prescription of twice-weekly hemodialysis in the USA. Am J Nephrol. 1999;19:625–33. doi: 10.1159/000013533. [DOI] [PubMed] [Google Scholar]
- 8.Lin YF, et al. Comparison of residual renal function in patients undergoing twice-weekly versus three-times-weekly haemodialysis. Nephrology. 2009;14:59–64. doi: 10.1111/j.1440-1797.2008.01016.x. [DOI] [PubMed] [Google Scholar]
- 9.Bieber B, et al. Two-times weekly hemodialysis in China: frequency, associated patient and treatment characteristics and Quality of Life in the China Dialysis Outcomes and Practice Patterns study. Nephrol Dial Transplant. 2014;29:1770–7. doi: 10.1093/ndt/gft472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalantar-Zadeh K, et al. Twice-weekly and incremental hemodialysis treatment for initiation of kidney replacement therapy. Am J Kidney Dis. 2014;64:181–6. doi: 10.1053/j.ajkd.2014.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chapter 8: Transition of Care in CKD. Am J Kidney Dis. 2016;67:S85–S98. [Google Scholar]
- 12.Mathew AT, Fishbane S, Obi Y, Kalantar-Zadeh K. Preservation of residual kidney function in hemodialysis patients: reviving an old concept. Kidney Int. 2016 doi: 10.1016/j.kint.2016.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shafi T, et al. Association of residual urine output with mortality, quality of life, and inflammation in incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for End-Stage Renal Disease (CHOICE) Study. Am J Kidney Dis. 2010;56:348–358. doi: 10.1053/j.ajkd.2010.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kutner N, Bowles T, Zhang R, Huang Y, Pastan S. Dialysis facility characteristics and variation in employment rates: a national study. Clin J Am Soc Nephrol. 2008;3:111–116. doi: 10.2215/CJN.02990707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Helanterä I, Haapio M, Koskinen P, Grönhagen-Riska C, Finne P. Employment of patients receiving maintenance dialysis and after kidney transplant: a cross-sectional study from Finland. Am J Kidney Dis. 2012;59:700–706. doi: 10.1053/j.ajkd.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 16.Lowrie EG, Laird NM, Parker TF, Sargent JA. Effect of the hemodialysis prescription of patient morbidity: report from the National Cooperative Dialysis Study. N Engl J Med. 1981;305:1176–81. doi: 10.1056/NEJM198111123052003. [DOI] [PubMed] [Google Scholar]
- 17.Kerr P, Perkovic V, Petrie J, Agar J, Disney A. Dialysis adequacy (HD) guidelines: Dose of haemodialysis. Nephrology. 2005;10 doi: 10.1111/j.1440-1797.2005.00464_1.x. [DOI] [PubMed] [Google Scholar]
- 18.Anand S, Bitton A, Gaziano T. The Gap between Estimated Incidence of End-Stage Renal Disease and Use of Therapy. PLoS One. 2013;8 doi: 10.1371/journal.pone.0072860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khanna U. The Economics of Dialysis in India. Indian J Nephrol. 2009;19:1. doi: 10.4103/0971-4065.50671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chauhan R, Mendonca S. Adequacy of twice weekly hemodialysis in end stage renal disease patients at a tertiary care dialysis centre. Indian J Nephrol. 2015;25:329–333. doi: 10.4103/0971-4065.151762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anees M, Hameed F, Mumtaz A, Ibrahim M, Khan MNS. Dialysis-related factors affecting quality of life in patients on hemodialysis. Iran J Kidney Dis. 2011;5:9–14. [PubMed] [Google Scholar]
- 22.Shdaifat EA, Manaf MRA. Haemodialysis in Jordan: Socio-demographic data, clinical analysis and projecting burden. Middle East J Sci Res. 2013;14:624–632. [Google Scholar]
- 23.Mohammed FA. Prediction of Malnutrition Using Modified Subjective Global Assessment-Dialysis Malnutrition Score in Patients on Chronic Hemodialysis. J Community Med Health Educ. 2014;04:4–11. [Google Scholar]
- 24.Supasyndh O, et al. Nutritional status of twice and thrice-weekly hemodialysis patients with weekly Kt/V > 3.6. J Med Assoc Thai. 2009;92:624–31. [PubMed] [Google Scholar]
- 25.Daugirdas JT, et al. KDOQI Clinical Practice Guideline for Hemodialysis Adequacy: 2015 Update. Am J Kidney Dis. 2015;66:884–930. doi: 10.1053/j.ajkd.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 26.Tattersall J, et al. European Best Practice Guidelines on haemodialysis – part 2. Nephrol Dial Transplant. 2007;22(supplem) [Google Scholar]
- 27.Watanabe Y, et al. Japanese Society for Dialysis Therapy Clinical Guideline for ‘Maintenance Hemodialysis: Hemodialysis Prescriptions’. Ther Apher Dial. 2015;19:67–92. doi: 10.1111/1744-9987.12294. [DOI] [PubMed] [Google Scholar]
- 28.Culleton BF. Introduction. J Am Soc Nephrol. 2006;17:S1–S3. doi: 10.1681/ASN.2005121372. [DOI] [PubMed] [Google Scholar]
- 29.Kerr P, Perkovic V, Petrie J, Agar J, Disney A. Duration and frequency of haemodialysis therapy. Nephrology. 2005;10:S71–S74. [Google Scholar]
- 30.Mactier R, et al. Summary of the 5th edition of the Renal Association Clinical Practice Guidelines (2009–2012) Nephron Clin Pract. 2011;118(Suppl):c27–70. doi: 10.1159/000328060. [DOI] [PubMed] [Google Scholar]


