Abstract
Objectives
Because children with medical complexity (CMC) display very different health trajectories, needs, and resource utilization than other children, it is unclear how well traditional conceptions of population health apply to CMC. We sought to identify key health outcome domains for CMC as a step toward determining core health metrics for this distinct population of children.
Methods
We conducted and analyzed interviews with 23 diverse national experts on CMC to better understand population health for CMC. Interviewees included child and family advocates, health and social service providers, and research, health systems, and policy leaders. We performed thematic content analyses to identify emergent themes regarding population health for CMC.
Results
Overall, interviewees conveyed that defining and measuring population health for CMC is an achievable, worthwhile goal. Qualitative themes from interviews included: (1) CMC share unifying characteristics that could serve as the basis for population health outcomes; (2) optimal health for CMC is child specific and dynamic; (3) health of CMC is intertwined with health of families; (4) social determinants of health are especially important for CMC; and (5) measuring population health for CMC faces serious conceptual and logistical challenges.
Conclusions
Experts have taken initial steps in defining the population health of CMC. Population health for CMC involves a dynamic concept of health that is attuned to individual, health-related goals for each child. We propose a framework that can guide the identification and development of population health metrics for CMC.
Keywords: children with medical complexity, children with special health care needs, complex chronic conditions, health outcomes, population health
INTRODUCTION
Improving the health of populations is a national priority codified by the Triple Aim.1 Children with medical complexity (CMC), a sub-set of children with special health care needs (CSHCN), are a particularly important population due to their high needs and disproportionate use of resources. Comprising less than 3% of United States (US) children, CMC generate substantial costs, including 40% of child Medicaid expenditures.2,3 This population of children is most commonly conceptualized as having a combination of significant family-identified service needs; chronic, severe conditions; functional limitations; and high healthcare use.2
Given the outsize importance of CMC to the child health system, an appropriate framework for population health is important. General definitions of population health vary but, as established by Kindig and Stoddart, typically involve the aggregated health outcomes of a group of individuals, with special consideration of the distribution of those outcomes4 and factors that contribute to variability in that distribution.5 Because CMC are generally on one extreme end of the health distribution for all children, more general conceptions of population health—such as the Healthy People 2020 framework,6 the Institute for Healthcare Improvement model for population health,7 the Institute of Medicine Framework for Indicator Development,8 and even the 6 Core Outcomes for Children with Special Health Care Needs9—and the metrics that serve them may fail to adequately capture important health differences among CMC themselves.
Furthermore, important domains relevant primarily to CMC may be missing from existing frameworks. For example, the recognized impact of caregiving for CMC on the physical and mental health of families,10,11 which may in turn affect the health of CMC, is largely absent from existing models of population health.
Previous efforts have explored what population health might mean more broadly for CSHCN,9,12 but consensus outcomes for CMC, whose problems are simultaneously more severe and more heterogeneous than those of other CSHCN, remain elusive.12,13 Although aspects of the outcomes applied to CSHCN are likely relevant to CMC, such as access to a medical home and adequate health insurance, they likely do not fully capture the nuances of the CMC population. Numerous outcomes have been included in research among CMC;14 however, the validity of these measures and their applicability to the population are often unknown.
Qualitative research with CMC experts around the US could supplement the current literature to fill these gaps and provide a more comprehensive conceptualization of population health for CMC. Although the importance of family members,15–17 providers,17 and systems leaders in comprehending and shaping outcomes related to CMC is readily acknowledged, previous work has not synthesized these experts’ perspectives on population health for CMC. The purpose of this study was to interview a diverse national stakeholder group to identify key population health outcome domains for CMC as a step toward determining core health metrics for this distinct population of children.
METHODS
We performed an in-depth qualitative analysis of interview data collected from a diverse group of experts on CMC to better understand population health for CMC. This study was conducted as Phase 2 of a larger project that combines systematic literature review (Phase 1)14 and group concept mapping18 (Phase 3) to propose candidate population health outcomes for CMC.
Participants
We used purposive sampling to create a sample of key stakeholders that was diverse in terms of geography, gender, race/ethnicity, and expertise related to CMC. Initially, the research team generated a list of potential nominees for interviews based on personal knowledge of individuals and organizations involved in the care of CMC, subsequent snowball sampling, and our previous literature review. That list was supplemented and refined during a 4-month process; emailed invitations for interview participation were then sent to 28 individuals. Our goal was to interview a broad array of prominent stakeholders within each of 3 main categories of expertise (child and family advocate; provider; and systems, research, or policy leader). Twenty-three invitees (82%) agreed to be interviewed. Their primary categorization, as determined by our research team and interviewee responses to a question asking about their role with CMC, was: 5 child and family advocates; 6 child healthcare and social service providers; and 12 healthcare systems, research, or policy leaders. Several of the 23 participants spanned multiple categories of stakeholders. All participants granted their permission to report their names and titles (Appendix 1).
Data Collection
We developed a semi-structured interview guide that was informed by our preceding systematic literature review14 and refined after pilot testing. Interviews queried participants about their perspectives on population health for CMC, including unifying features of CMC, definitions of health for CMC, and challenges in measuring the population health of CMC (for sample interview questions, see Appendix 2). Approximately one day prior to interviews, interview participants were emailed the interview guide. Qualitative methods using one-on-one, semi-structured confidential interviews were employed. Interviews took place via telephone and lasted 30 to 60 minutes. Interviews were conducted by 3 team members trained in qualitative methods.
Data Analysis
We used 6-step thematic content analysis to identify themes representative of participants’ views on population health of CMC.19 Interviews were audio-recorded and transcribed by a transcription service. Using ATLAS.ti software (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany), 3 coders independently reviewed the transcripts to discuss codes. These initial codes were discussed with our entire research team at a research meeting. After a subsequent round of independent coding, the entire research team met again to compare initial themes and reach consensus. Two coders then independently coded the interview transcripts. A third coder resolved any disagreements between coders. Kappa statistics were calculated to measure consistency between the 2 main coders based on examination of a random sample of transcripts. We continued interviews until we reached saturation of themes, as assessed during discussions during weekly research team meetings. In total, we conducted 23 interviews, which passed and then confirmed saturation of themes.20
RESULTS
Overall, participants across all the stakeholder groups expressed that defining and measuring population health for CMC is an achievable, worthwhile goal. The experts’ perspectives on population health for CMC were categorized into the following five themes: (1) CMC share unifying characteristics that could serve as the basis for population health outcomes; (2) optimal health for CMC is child specific and dynamic; (3) health of CMC is intertwined with health of families; (4) social determinants of health are especially important for CMC; and (5) measuring population health for CMC faces serious conceptual and logistical challenges. Kappa ranged from 0.52 (moderate agreement) to 0.81 (near perfect agreement). Representative quotations from participants, divided thematically, can be found in Table 1.
TABLE 1.
Thematic Quotations from In-Depth Interviews with Experts on Children with Medical Complexity
| Theme 1: CMC share unifying characteristics that could serve as the basis for population health outcomes |
| Intensive health service utilization: “They all universally share the fact that they need healthcare and other service provisions from many people and many different places over prolonged periods of time.” |
| Essential role of families and high caregiver burden and stress: “These parents [of CMC] and sometimes grandparents and other extended family are just doing the best job they can possibly do but they are working to the brink of complete exhaustion and it’s all consuming for them financially, socially, and physically.” |
| Social isolation: “One of the challenges that children with complex needs face is broader acceptance by those individuals that don’t have complex needs. Because a child is a child first and foremost. They’re human beings and they should not be defined by their condition. ” |
| Social isolation: “What I see with our children—at least those who are a bit older and able to verbalize—is that they feel different, they feel separate from their peers. They fear that they will be looked down upon because of their disease. They feel they don’t fit in.” |
| Challenges with community integration: “They [CMC] share the interface of their disease with the community and how they can adapt to living with their condition in the community.” |
|
|
| Theme 2: Optimal health for CMC is child specific and dynamic |
| “I think what it [health for CMC] means is living as well as possible for as long as possible.” |
| “Healthy means that they [CMC] are functioning at the highest ability, the highest and most stable ability given the medical complexities they’re dealing with.” |
| “I think being healthy means that you’re trying to minimize acute illnesses [for CMC] and maximize their growth and potential.” |
| “Health means being home and staying out of the hospital and being able to participate in activities appropriate for that child’s age or developmental level. I think it means being able to be in school on days when school is in session. And participating in kind of a social life.” |
|
|
| Theme 3: Health of CMC is intertwined with health of families |
| “If families need regional center services or California Children’s Center services, the hours are 9 to 5. That’s not family centered. If I need to see a doctor on the weekend, I have to go to urgent care or I have to go to the emergency room… And when you’re thinking about somebody who’s got multiple complexities, it’s like the family is at the end of the width as opposed to being the center.” |
| “Living with and caring for a child with complex medical conditions–the amount of stress and anxiety that comes along with that is a lot. Not only for the parents and for the child but also for siblings and other family members. I think the benefits of having psychological support within the home and having a medical team you trust are exponential in terms of the overall health of everyone within that family unit, including the child.” |
| “Let’s face it—these kids are a huge responsibility for the family to take care of. Unless we support the family, we’re going to see these kids in emergency rooms in our hospitals over and over again.” |
| “I think they [CMC] need a functional, strong family, right? It’s really a burden to the family. So we need to think of not just the child but what do we do with the families to make them resilient and support them through this process of caring for a child with medically complex disease.” |
|
|
| Theme 4: Social determinants of health are especially important for CMC |
| Socio-demographics and family functioning: “If we look at the national survey of children’s health and the national survey of children with special health needs, we know the children living in poverty have poor symptom outcomes based on the surveys. Race and ethnicity, a proxy for discrimination, contributes to that. Family instability—we know that, unfortunately, children, with complex conditions have more family disruption than the typically developing child. So a child can have access to the best health in the world and still have poor health outcomes because of all the other social factors that are going on in his or her life. You cannot separate those [social factors] from a child’s health.” |
| Parental employment: “If you ask an economist, you say you had a billion dollars to invest in child wellbeing what would they do? They would all hire parents for jobs. Because parents who work have healthier kids. Period.” |
| Poverty: “If you’re poor and you have spina bifida or acute lymphoblastic leukemia or whatever else, your mortality is actually increased. And despite getting the best possible care, mortality and morbidity go up with poverty in all of the conditions in the CMC group.” |
| Geography and access: “There’s the transportation issue, especially when you’re dealing with a children’s hospital that’s 50 to 100 to 200 miles away… We have parents that cannot afford to come here because they just don’t have the gas money.” |
| Immigration and citizenship issues: “You have the [immigration] checkpoints in the southern part of the state. For children that are medically complex that live that other side of the checkpoint, they can’t access the care that they need. Many families are mixed citizenship status so the client may be documented, but the parents are of mixed citizenship so it creates a barrier. They’re afraid to cross that checkpoint.” |
|
|
| Theme 5: Measuring population health for CMC faces serious conceptual and logistic challenges |
| Difficulty defining health for CMC: “I think it’s hard for the group [CMC community] as a whole to say what health [for CMC] means.” |
| Needs for measures specific to CMC: “Really great measures for typically developing kids exist for all the different age groups but they really do not work very well for atypically developing kids. I’d have to say there are no great measures [of development] for CMC. ‘Cause, boy, I’ve looked.” |
| Needs for measures specific to CMC: “Has the parent been able to go to work, has the child been able to go to school, is the family eating meals together? Those are important measures of being healthy from the family perspective. Population health really is about quality of life and we really need to develop a good tool to assess quality of life for a child with a complex need.” |
| Need for greater emphasis on measures related to mental health: “I don’t see much [in the literature] about psychiatric stuff [outcomes] … I think you ought to look at it because I think it [psychiatric problems in CMC and parents] is pretty prevalent.” |
| Difficulty incentivizing measurements relevant to CMC health outcomes: “If you don’t address work and school attendance and cost, you might as well not even sit at the table… Because frankly, for the business payers, Medicaid, the governor, decision makers, the rest of the stuff is irrelevant to them.” |
| Difficulty incentivizing measurements of any health outcomes: “Often times, there’s not systems in place to get measures. Hospitals don’t like to be measured and compared on quality. Doctors don’t like to be objectively measured and compared on quality. Those things [comparative reports of outcome measures] are difficult to get to, particularly when you get into the battles of market share and money is involved.” |
Overarching Concepts Regarding Population Health of CMC
CMC share unifying characteristics that could serve as the basis for population health outcomes
When asked to identify any common features CMC share, interviewees expressed that the heterogeneity of these children can make it difficult to find unifying characteristics. However, there was a strong consensus that unifying characteristics exist that transcend differences in factors such as diagnoses, age, developmental stage, functional ability, and social settings. Identification of unifying characteristics of CMC seemed to be an important question to the interviewees and one that was difficult to answer. Examples given of common features shared by CMC included 1) intensive health service utilization, 2) an essential role of families in the care of CMC, and 3) high caregiver burden and stress. Participants also reported that many CMC and their families share similar challenges related to social isolation and exclusion, including difficulty integrating CMC into educational systems and broader community social networks, and difficulty integrating parents of CMC into traditional family and societal roles. There was broad consensus, for instance, that two key health indicators for many CMC were 1) children’s school participation or attendance and 2) parents’ not reducing or missing scheduled work hours.
Optimal health for CMC is child specific and dynamic
When asked how to define health for CMC, nearly all participants conveyed that optimal health for CMC should be defined as the degree to which each child meets his or her potential. Optimal health was expressed as a dynamic “baseline” status unique to each child that might differ widely from baseline statuses of children without medical complexity and even of other CMC. Health providers were more likely than other stakeholders to describe health by emphasizing traditional medical indicators, such as frequency of acute infections. Several participants expressed that quality of life for CMC—as assessed by child and family ability to meet their own stated goals—was at least as important as longevity. Participants also expressed that markers of social and community integration, an important and often overlooked aspect of health for CMC, should constitute additional health outcomes for CMC.
Health of CMC is intertwined with health of families
All participants agreed that a family-centered conceptualization of health outcomes is essential. Although some felt that health systems were making progress in adopting a family-centered approach, many cited this as a critical gap. The most common rationale for a family-centered approach was that families play the most critical role in caring for CMC, including logistical, supportive, and direct medical care responsibilities. In addition, participants reported that caring for CMC intensely affects family health—it can be strengthening and empowering but can also strain caregiver physical and mental health and family functioning. Many participants asserted that the health of CMC in turn depends on the health of their families, and that families need additional supports to effectively meet the needs of CMC. Examples of supports that might be measurable included assisting families with overcoming logistical barriers, such as transportation, as well as broader supports such as assistance finding 1) appropriate housing, 2) jobs that provide adequate caregiver leave, and 3) community resources for CMC and their siblings and parents.
Social determinants of health are especially important for CMC
Participants generally agreed that social factors—especially race, ethnicity, socioeconomic status, immigration status, and geographic proximity to medical care—have strong influences on the health of CMC. Participants reported that factors such as belonging to a racial minority, poverty, and geographic isolation strongly affected health outcomes for CMC, mainly through decreased access to care and higher levels of parental stress. Several participants reported that, since CMC have such intensive need for health services, social factors that cause differential access to care may impact CMC more sharply compared to the non-complex population. A few participants expressed the view that CMC from traditionally underserved groups also receive lower quality of care, not just less access.
Measuring population health for CMC faces serious conceptual and logistical challenges
Participants across all stakeholder groups described that significant challenges exist in accurately measuring the population health of CMC. Participants conveyed that conceptual challenges, such as how to define CMC, as well as logistical and financial barriers, make it difficult to measure population health of CMC. Key challenges included difficulty developing outcome measures specific for CMC and difficulty incentivizing measurement for less traditional outcome measures such as family functioning and parent mental health, versus more easily obtained metrics of utilization and cost. Nevertheless, these leaders expressed that the identification and implementation of key measures of population health for CMC was an achievable, useful goal. Participants also generally agreed that important gaps in existing measurement tools exist that hinder our ability to adequately measure the population health of CMC. Participants across all stakeholder groups specifically suggested that greater attention needed to be paid to the measurement of 1) mental health and 2) quality of life in both CMC and their families, both in regards to developing or refining existing measures and addressing implementation challenges. Participants also conveyed that new measurement tools specific for CMC were needed, such as measures capturing child’s health status relative to family goals for that child. In contrast to this majority viewpoint, one participant conveyed that existing population health measures applicable to a general pediatric population could simply be applied to CMC, especially because movement between the population of CMC and the general pediatric population may be more common than is typically believed. Finally, the lack of measures to quantify social and community integration of CMC was described as an important gap in existing measurement tools.
DISCUSSION
As an initial step toward establishing core population health measures, we synthesized perspectives of a diverse national stakeholder group around key concepts of health for CMC. Our findings identified concepts that have received limited attention to date, but nonetheless have important implications for defining health within this distinct population.
A Goals-Based Approach to Outcomes
Because of the chronicity, severity, and dynamic nature of CMC health conditions, achievement of optimal health might be most appropriately measured as progress on health-related goals, which should be assessed explicitly and regularly. Moreover, achievable goals may differ across groups of CMC or change within individual children as their underlying condition waxes and wanes. Across this population, uniform static measures of health are likely to be misleading.
Measurement strategies may be most effective if they are flexible enough to account for the health-related goals set by individuals and families, against which a trajectory can be assessed (i.e., progress towards or away from their goals). Although health-related quality of life can be measured among CMC,21 absolute scale scores may be less informative than determining whether a family has moved closer to their own critical goal, e.g., their child has less difficulty with sleep. While health-related goals also apply to the broader pediatric population, what comprises optimal health for CMC may, in some cases, differ greatly from what comprises optimal health in the non-complex population, and may change radically over time. We speculate that, compared to reliance on established and predictable central tendencies, distributions, and developmental trajectories for outcomes in a general pediatric population, incorporation of individual health-related goals into benchmarks may prove to be the key distinguishing feature of a population health approach for CMC.
Child Health and Family Health Are Inseparable
In order to build a population health framework attuned to the goals that define optimal health for CMC, it may be essential to adopt an approach in which child health cannot be measured outside the context of family health. The health care system’s enormous dependence on caregivers to deliver essential and often sophisticated health care is unique to CMC, which makes health – especially mental health – of caregivers paramount. Previous qualitative work among families of CMC has identified caregiver self-efficacy to manage their child’s care as a major determinant of the child’s outcomes.16
Beyond caregiver efficacy to deliver complex care at home, our interviewees conveyed that one of the main commonalities that CMC share is the intense vulnerability of families. Related to this observation, past research has described the extensive challenges faced by caregivers of CMC across the US.22 Furthermore, inadequately supported caregivers delivering complex care at home can experience wide-ranging mental health or socioeconomic consequences.10,11,23,24 Conversely, when going well, caring for CMC at home can be beneficial for families, inducing positive physical, psychological, and social impacts.10 Interviewees from our study repeatedly emphasized the importance of optimizing family functioning and family health as an integral part of improving CMC health outcomes. Examples of key family outcomes include parental missed days of work, parent depressive symptoms, sibling depressive symptoms, family connectedness, and other measures that capture family/caregiver health. Although not yet well-established, our work suggests a link between CMC health and the health of their caregivers. Compared to other populations, the effect of this potentially cyclical relationship is likely exaggerated for CMC, where positive and negative caregiver experiences directly influence family, which then directly influences CMC health, and vice versa.
In summary, we propose that CMC health is not completely represented when we interpret our results in the context of existing population health models.4,6–8 Most notably, the concepts of dynamic, individualized health-related goals and the influence of family health are not reflected in these models. Therefore, to integrate our findings,14 we propose adaptations to the existing Institute of Medicine (IOM) framework for developing core metrics of population health for CMC, as discussed below.8
CMC Health Outcomes Development Framework
We synthesized results from the qualitative thematic analysis and applied these results to create a framework for developing core metrics of health for CMC (Figure 1). We examined existing population health models and found that our results best fit the broad Institute of Medicine (IOM) “Framework for Indicator Development,” which was designed to guide the future selection of 20 core health metrics applicable to the general population.8 The IOM framework suggests that factors related to three broad categories—1) social and physical environment, 2) health-related behavior, and 3) health systems—be considered when developing indicator measures for population health outcomes. Although we maintained the basic structure of the IOM framework, based on our interviews with our diverse group of national experts, we modified the IOM indicator development framework to create a health outcomes framework for CMC. Our outcomes framework for CMC differs from the IOM’s in several respects.
FIGURE 1.
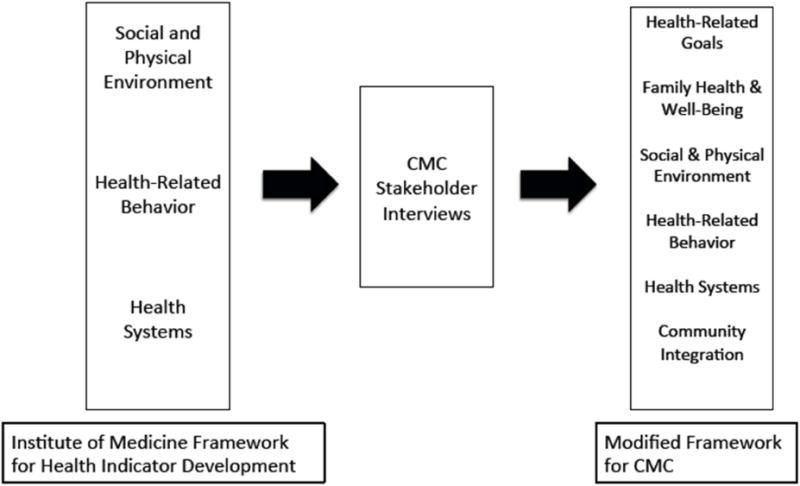
Health Indicator Development Framework for Measuring the Health of Children with Medical Complexity (CMC)
First, we retained the 3 IOM categories “Social and Physical Environment,” “Health-Related Behavior,” and “Health Systems.” Related to these categories, our data notably suggests that social determinants of health may impact CMC more intensely than the general pediatric population. We also added “Health-Related Goals” as an additional concept to include when devising a health outcome measurement strategy for CMC. The “Health-Related Goals” category for CMC must extend beyond traditional measures such as longevity or absence of morbidity to include a broader, more dynamic, and more individualized conception of health. For CMC, each child should have their own health measurements tailored to the current capacities, future potentials, and goals of the children, their families, and their providers. These iterative goals should be developed through ongoing dialogue, characterized by trust and mutual respect, between families and providers. For CMC, both health and health-related goals may unpredictably shift over time.
Second, we added a “Family Health & Well-Being” category to the health indicator development framework. This reflects the expert perspective that among CMC, family health outcomes including family functioning and parent mental health and well-being are inextricably linked with child health outcomes and therefore deserve separate consideration from “Social & Physical Environment.” Additional family well-being outcomes should assess financial, logistical and self-efficacy barriers experienced by families caring for CMC, as well as access to programs that support the physical and mental health and well-being of caregivers.
Finally, we added a “Community Integration” category to the framework. The expert participants expressed that CMC and their families face many complexity-related challenges with community integration (e.g., schools, public activities, workplaces) that seem to go beyond usual conceptions of “Social & Physical Environment” and rise to the level of a health indicator domain.
Limitations
As with all qualitative studies, the generalizability of our study is limited to the experiences of the experts we interviewed. To minimize this, we aimed to reach a diverse, experienced group of national experts on CMC across the US who represent multiple stakeholder perspectives. Despite these efforts, however, selection bias may have been an issue. Finally, we employed a sampling frame that spanned the country and interviews were conducted by telephone, which may have influenced the dynamics and fluidity of conversation.
CONCLUSION
Adopting a population health approach for development of core health metrics for CMC may be more feasible than currently suggested by the existing literature. Defining population health for CMC entails a dynamic concept of health attuned to health-related goals for each child. A better understanding of the impact of caring for CMC on the health of families and the subsequent impact of family health on the health of CMC is needed. Identifying a more comprehensive set of core population health metrics for CMC may be achievable using the CMC health indicator development framework from this study. Population health metrics for CMC likely include those relevant to both the general and CSHCN pediatric populations, such as oral health status, nutritional status, and immunization rates, and also extend beyond the traditional conceptions of health for children. This framework considers health-related goals, family heath & well-being, social and physical environment, health-related behavior, health system, and community integration as key concepts to guide the selection of core population health metrics for CMC. Ultimately, capturing these outcomes for CMC may help reveal opportunities to improve health measurement for all children.
WHAT’S NEW.
A consensus approach to population health for children with medical complexity (CMC) does not yet exist. Based on interviews with experts on CMC, we developed a population health framework for CMC that can help guide policies and programs for CMC.
Acknowledgments
Thank you to our interview participants and to Dr. Edward Schor for his visionary and conceptual contributions. This work was supported by a grant from the Lucile Packard Foundation for Children’s Health and by the UCLA Children’s Discovery and Innovation Institute.
Project support: This work was supported by a grant from the Lucile Packard Foundation for Children’s Health and by the UCLA Children’s Discovery & Innovation Institute.
Appendix 1: Participants in Key Informant Interviews on the Population Health of Children with Medical Complexity (CMC)
| Interviewee Name | Interviewee Title and Position |
|---|---|
| Jori Bogetz, MD | Assistant Professor, Pediatrics, University of California, San Francisco |
| Gertrude Carter, MD | Chief Medical Officer, LA Care Health Plan |
| Susan Chacon, MSW | CSHCN Director New Mexico, New Mexico Department of Health, Children’s Medical Services |
| Eyal Cohen, MD, MSc, FRCP(C) | Pediatrician, The Hospital for Sick Children Associate Professor of Pediatrics and Health Policy, Management & Evaluation, University of Toronto |
| W. Carl Cooley, MD | Clinical Professor of Pediatrics, Geisel School of Medicine at Dartmouth |
| Devon Dabbs | Vice President of Pediatric Programming and Education, Children’s Hospice and Palliative Care Coalition |
| Robert Dimand, MD | Chief Medical Officer, California Children’s Services |
| Juno Duenas | Executive Director, Support for Families Family Voices of California Council Member Agency |
| Amy Houtrow, MD, PhD, MPH | Associate Professor and Vice Chair, Department of Physical Medicine and Rehabilitation, University of Pittsburg |
| Siem Ia, NP | Nurse Practitioner, Pediatric Medical Home Program, University of California, Los Angeles |
| Ivan J. Kamil, MD | Pediatrician and Medical Director |
| Kelly Kelleher, MD, MPH | Vice President, Health Services Research; Director, Center for Innovation in Pediatric Practice; The Research Institute, Nationwide Children’s Hospital Professor of Psychiatry, Pediatrics, The Ohio State University |
| Dennis Kuo, MD, MHS | Pediatrician, Arkansas Children’s Hospital Associate Professor, Pediatrics, University of Arkansas for Medical Sciences College of Medicine |
| Stacey Lihn | President and Co-Founder, Sisters by Heart |
| Rita Mangione-Smith, MD, MPH | Professor and Chief, Division of General Pediatrics and Hospital Medicine, University of Washington |
| Josefina Martinez | Parent of Child with Medical Complexity |
| Fernando Mendoza, MD, MPH | Professor, Pediatrics, Lucile Salter Packard Children’s Hospital |
| James M. Perrin, MD | John C. Robinson Chair in Pediatrics, Mass General Hospital for Children, Harvard Medical School |
| Jean Raphael, MD, MPH | Associate Professor, Pediatrics, Baylor College of Medicine |
| Matthew Sadof, MD | Pediatrician, Baystate Health |
| Edward Schor, MD | Senior Vice President for Programs and Partnerships, Lucile Packard Foundation for Children’s Health |
| Debra Waldron, MD, MPH | Director, Division of Services for Children with Special Health Care Needs, Maternal Child Health Bureau, Health Resources and Services Administration |
| Rosella Yousef, LMFT | Manager, Medical Case Management Services, Department of Children and Family Services, Los Angeles |
Appendix 2: Sample Semi-Structured Interview Questions for Interviews with National Experts on CMC
I. Demographics
What is your role in caring for children with medical complexity (CMC)?
Do you have a specific focus area (e.g., specific diseases, specific clinical setting, or other specific focus?
II. Defining the Population Health of Children with Medical Complexity
When thinking about a child with medical complexity, especially one who will be dealing with potentially lifelong serious medical challenges, what does being healthy mean now and in the future?
Are there key health concerns and challenges that most children with medical complexity share, regardless of their specific disease?
Do you have specific thoughts about the role of social factors (e.g., poverty, living conditions, family instability, and race/ethnicity) on the ability of CMC to stay healthy?
III. Population Health Metrics for Children with Medical Complexity
For each component of the healthy life you described earlier [list them], and for each key shared health challenge you mentioned [list them], what are the two or three most important outcomes to measure for children with medical complexity?
We conducted a systematic literature review on outcome measures of health for medically complex children. We synthesized these results into a list of key outcome categories for medically complex children and emailed you with the list. These items are also listed at the end of this document.
Based on both your own experience and our discussion thus far, what do you think about the current list?
What major outcomes or domains are missing?
Which of these key outcomes do you think are the most feasible and impactful to measure?
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: The authors have no conflicts of interest relevant to this article to disclose.
References
- 1.Berwick D, Nolan T, Whittington J. The Triple Aim: Care, Health, and Cost. Health Affairs. 2008;27(3):759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 2.Cohen E, Kuo DZ, Agrawal R, et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529–538. doi: 10.1542/peds.2010-0910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berry J, Agrawal R, Cohen E, Kuo K. The Landscape of Medical Care for Children with Medica Complexity. Overland Park: Children’s Hospital Association; p. 2013. [Google Scholar]
- 4.Kindig D, Stoddart G. What is population health? Am J Public Health. 2003;93(3):380–383. doi: 10.2105/ajph.93.3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Evans R, Barer M, Marmor T. Why are some People Healthy and Others Not?: The Determinants of Health of Populations. New York: Aldine de Gruyter; 1994. [Google Scholar]
- 6.Koh HK, Piotrowski JJ, Kumanyika S, Fielding JE. Healthy people: a 2020 vision for the social determinants approach. Health Educ Behav. 2011;38(6):551–557. doi: 10.1177/1090198111428646. [DOI] [PubMed] [Google Scholar]
- 7.Steifel M, Nolan K. A Guide to Measuring the Triple Aim: Population Health, Experience of Care, and Per Capital Cost. Cambridge, Massachusetts: Institute for Healthcare Improvement; 2012. [Google Scholar]
- 8.Institute of Medicine Committee on the State of the USA Health Indicators. State of the USA Health Indicators–Letter Report. Washington DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- 9.Health Resources and Services Administration. National Agenda for Children With Special Health Care Needs: Achieving the Goals 2000. Washington DC: Health Resources and Services Administration; 1997. [Google Scholar]
- 10.Wang KW, Barnard A. Technology-dependent children and their families: a review. J Adv Nurs. 2004;45(1):36–46. doi: 10.1046/j.1365-2648.2003.02858.x. [DOI] [PubMed] [Google Scholar]
- 11.Aday LA, Wegener DH. Home care for ventilator-assisted children: implications for the children, their families, and health policy. Child Health Care. 1988;17(2):112–120. doi: 10.1207/s15326888chc1702_9. [DOI] [PubMed] [Google Scholar]
- 12.Ghandour RM, Grason HA, Schempf AH, et al. Healthy People 2010 Leading Health Indicators: How Children With Special Health Care Needs Fared. American Journal of Public Health. 2013;103(6):E99–E106. doi: 10.2105/AJPH.2012.301001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schor E, Bergman D. A Triple Aim Practice for Children with Special Health Care Needs. Palo Alto: Lucile Packard Foundation for Children’s Health, Issue Brief; 2013. [Google Scholar]
- 14.Coller R, Barnert ES, Nelson BB, Thompson LR, Chan V, Padilla C, Klitzner TS, Szilagyi M, Chung PJ. Defining Population Health for Children with Medical Complexity: A Systematic Review; Pediatric Academic Societies Annual Meeting; Baltimore, MD. 2015. [Google Scholar]
- 15.Solan LG, Beck AF, Brunswick SA, et al. The Family Perspective on Hospital to Home Transitions: A Qualitative Study. Pediatrics. 2015;136(6):e1539–1549. doi: 10.1542/peds.2015-2098. [DOI] [PubMed] [Google Scholar]
- 16.Desai AD, Durkin LK, Jacob-Files EA, Mangione-Smith R. Caregiver Perceptions of Hospital to Home Transitions According to Medical Complexity: A Qualitative Study. Acad Pediatr. 2016;16(2):136–144. doi: 10.1016/j.acap.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 17.Hudson SM, Newman SD, Hester WH, Magwood GS, Mueller M, Laken MA. Factors influencing hospital admissions and emergency department visits among children with complex chronic conditions: a qualitative study of parents′ and providers’ perspectives. Issues in comprehensive pediatric nursing. 2014;37(1):61–80. doi: 10.3109/01460862.2013.855844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Trochim W. Special issue: Concept mapping for evaluation and planning. Evaluation and Program Planning. 1989;12(1):1–111. [Google Scholar]
- 19.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. [Google Scholar]
- 20.Francis JJ, Johnston M, Robertson C, et al. What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Health. 2010;25(10):1229–1245. doi: 10.1080/08870440903194015. [DOI] [PubMed] [Google Scholar]
- 21.Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care. 1999;37(2):126–139. doi: 10.1097/00005650-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Kuo DZ, Cohen E, Agrawal R, Berry JG, Casey PH. A national profile of caregiver challenges among more medically complex children with special health care needs. Arch Pediatr Adolesc Med. 2011;165(11):1020–1026. doi: 10.1001/archpediatrics.2011.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kirk S. Families' experiences of caring at home for a technology-dependent child: a review of the literature. Child Care Health Dev. 1998;24(2):101–114. doi: 10.1046/j.1365-2214.1998.00043.x. [DOI] [PubMed] [Google Scholar]
- 24.Thyen U, Kuhlthau K, Perrin JM. Employment, child care, and mental health of mothers caring for children assisted by technology. Pediatrics. 1999;103(6 Pt 1):1235–1242. doi: 10.1542/peds.103.6.1235. [DOI] [PubMed] [Google Scholar]


