Abstract
Background:
Studies have shown that distress and accompanying neuroendocrine stress responses as important predictor of survival in advanced breast cancer patients. Some psychotherapeutic intervention studies have shown have modulation of neuroendocrine-immune responses in advanced breast cancer patients. In this study, we evaluate the effects of yoga on perceived stress, sleep, diurnal cortisol, and natural killer (NK) cell counts in patients with metastatic cancer.
Methods:
In this study, 91 patients with metastatic breast cancer who satisfied selection criteria and consented to participate were recruited and randomized to receive “integrated yoga based stress reduction program” (n = 45) or standard “education and supportive therapy sessions” (n = 46) over a 3 month period. Psychometric assessments for sleep quality were done before and after intervention. Blood draws for NK cell counts were collected before and after the intervention. Saliva samples were collected for three consecutive days before and after intervention. Data were analyzed using the analysis of covariance on postmeasures using respective baseline measure as a covariate.
Results:
There was a significant decrease in scales of symptom distress (P < 0.001), sleep parameters (P = 0.02), and improvement in quality of sleep (P = 0.001) and Insomnia Rating Scale sleep score (P = 0.001) following intervention. There was a decrease in morning waking cortisol in yoga group (P = 0.003) alone following intervention. There was a significant improvement in NK cell percent (P = 0.03) following intervention in yoga group compared to control group.
Conclusion:
The results suggest modulation of neuroendocrine responses and improvement in sleep in patients with advanced breast cancer following yoga intervention.
Keywords: Cortisol, immune, natural killer cell, sleep, yoga
INTRODUCTION
The advancement and progression of breast cancer impose severe psychologic distress. There follows a sequel of dejection, depression anxiety, and fear of dying and thoughts of impending treatments-related side effects that are known to cause distress, impair sleep, and normal functioning.[1,2] Metastatic breast cancer patients often have to cope with uncertainty about their future which is known to cause severe stress.[3] This chronic stress is known to impair sleep and circadian rhythms. Impairment in sleep in cancer patients could be due to pain, electrolyte disturbances, infection, or psychologic distress and mood states.[4] Sleep is an important buffer of stress response. Both sleep quality and duration are important attributes of sleep.[5] While good sleep acts as a buffer of stress response, impaired sleep is known to exacerbate symptoms, distress, and fatigue.[6] Alteration in circadian patterns of sleep with daytime sleepiness and fatigue is one of the early signs of sleep impairment.[4,6] This impairment in sleep is primarily caused due to elevated stress hormones such as cortisol and change in circadian rhythms of cortisol due to perceived stress.[7] This triad of stress, sleep impairment, and altered diurnal cortisol rhythm is known exacerbate symptom distress, pain, fatigue, and lower antitumor immune response in patents.[8]
This treatment-related distress coupled with daily hassles is intense enough to cause elevated cortisol levels and hypothalamopituitary axes dysregulation.[8,9] Most distressed patients have had flat or upward cortisol slopes that have shown to be an important predictor for survival.[7,8]
Moreover, the effects of this intense stressor are known to affect psychoneuroendocrine and psychoneuroimmune axes causing maladaptive neuroendocrine responses and immunosuppression.[10,11] This is evident in earlier studies wherein advanced breast cancer patients had low natural killer (NK) cell counts due to their psychologic distress.[8,11] The study of changes in these pathways has intrigued scientists to try psychologic and mind-body interventions that can modulate these pathways and help patients cope with this stressor.
Several studies have shown that psychotherapeutic interventions modulate abnormal rhythms and morning salivary cortisol peaks and improve sleep quality and reduce distress. Cognitive behavior therapy,[12,13] supportive therapy,[14] and other mind-body therapies such as mindfulness-based stress reduction,[15] Yoga, Tai Chi,[16] etc., have shown to reduce morning cortisol levels. In our earlier study with stage I–III breast cancer patients undergoing radiotherapy, our integrated yoga program showed decrease in cortisol levels following radiotherapy.[17] However, most of these studies have shown changes in early cancer patients with exception of few on metastatic breast cancer patients using psychotherapeutic interventions.[16]
METHODS
In this study, 91 patients with metastatic breast cancer were recruited to participate in a trial comparing an integrated yoga program versus education and supportive therapy sessions on stress, sleep, diurnal salivary cortisol rhythms, and NK cell counts. The recruitments were carried out from January 2004 to June 2007 with referrals from medical and radiation oncology outpatient departments of a comprehensive cancer care center. The Institutional Review Board of the participating institution approved the study. The subjects were recruited if they satisfied the selection criteria and gave written consent to participate in the study.
Selection criteria
Patients were included if they met the following criteria:
Women diagnosed with stage IV breast cancer within 6 months–2 years after diagnosis either recurrent disease or progressive disease
Age between 30 and 70 years
Zubrod's performance status 0–2 (ambulatory >50% of time)
Minimum high school education
Willingness to participate in the study.
Exclusion criteria were
Duration of metastasis more than 1 year
Brain metastasis
Those undergoing chemotherapy/radiotherapy during the study except for treatment of bone metastases with bisphosphonates/zoledronic acid
Those on hydrocortisone medications
A concurrent medical condition likely to interfere with yoga intervention or survival
Any major psychiatric, neurological illness, or autoimmune disorders
Those who are on hydrocortisone medications or have HIV
Pregnant and lactating mothers or planning to conceive during the study period
Those who are recruited for clinical trials involving investigational new drugs
Prior practice of yoga in the last 6 months
Prior chemotherapy other than treatment of bone metastases mentioned above in the last 2 weeks
History of any pathologic fractures.
In this study, 257 patients with advanced metastatic breast cancer patients were screened over a 3-year period. One hundred and fifty-three patients were eligible, and 91 patients consented to participate in this study. Patients were recruited to participate in a two-arm prospective randomized controlled trial comparing the effects of an “integrated yoga based stress reduction program” (n = 45) versus standard “education and supportive therapy sessions” (n = 46).
Sample size
Earlier study with Mindfulness-Based Stress Reduction Program (MBSR) had shown a modest effect size (ES = 0.38) on EORTC QLC30 global quality of life measure.[18] We used G power to calculate the sample size with α = 0.05 and β = 0.2 and an ES of 0.38 for repeated measures ANOVA between factor effects. The sample size thus required was (n = 44) in each group. Second, earlier studies were only on stage I–III breast cancer patients and not on metastatic breast cancer patients.
Randomization
A person who had no part in the trial randomly allocated consenting participants to either yoga or supportive therapy groups using random numbers generated by a random number table at a different site. Randomization was performed using opaque envelopes with group assignments, which were opened sequentially in the order of assignment during recruitment with names and registration numbers written on their covers.
Masking and blinding
Being a popular intervention, it was not possible to mask the yoga intervention from the subjects. However, the investigators (treating oncologists) were blind to the intervention and subjects were asked not to disclose the type of intervention (yoga or supportive therapy) to them. Second, the saliva and blood samples were blinded from the technicians who analyzed the coded samples at a site different from the study center. The samples and data were unblinded only at the conclusion of the study.
Outcome measures
Pittsburgh Insomnia Rating Scale is a widely used instrument in clinical and research practice.[19] It is a scale with 65-items. It was designed to assess severity of insomnia in clinical settings. It is known to assess subjective distress score (46 items) related to sleep, subjective sleep parameters (10 items) and sleep-related quality-of-life (9 items). The items have to be scored according to symptoms experienced in the previous week. The test-retest reliability and internal consistency for the scale was 0.93 (Veqar and Hussain, 2016).[20]
Diurnal salivary cortisol measures
Saliva collection and storage: participants were trained to collect their saliva by chewing on a cotton swab and dribble the saliva to a plastic holder resting inside a sterile centrifuge tube. Samples were collected at 0600 h, 0900 h, and 2100 h for 3 consecutive days. The samples were stored in refrigerator and delivered to study personnel after 3 days. Samples were then centrifuged to remove mucous, freeze, and stored at −70°C in Eppendorf tubes for analysis.
Quantifications of salivary cortisol
Salivary cortisol levels were assessed using enzyme immunoassay method using kits manufactured by Salimetrics Inc., USA. The test samples were run in duplicates and readings taken on a microplate reader (Bio-Rad, USA). The tests were standardized under controlled laboratory conditions using standards, positive, and negative controls provided along with the kit by the manufacturer. The plates were read at 450 nm, and a standard curve was plotted on a graph for each run by plotting the log of cortisol concentrations on “y” axis and log of optical density (O.D) reading on “x” axes and best fit line determined by regression analyses. The values were then extrapolated with the graph using the mean O.D readings of the duplicate wells and plotting their corresponding concentration on the graph. The detection range with these kits was 0.012–3.0 Hgm/dl. The intra-assay coefficient ranged from 3.35% to 3.65% and inter-assay coefficient from 3.75% to 6.41% with these samples. Mean cortisol levels for specific time points over a 3-day period were extrapolated.
Natural killer cells (CD56%) measures
Blood sample collection: all subjects in metastatic breast cancer study were asked to provide blood samples at the study start and at the end of intervention. About 5 ml of heparinized blood sample was collected in vacuettes under sterile conditions. All the blood samples were collected between 8 am to 12 am to reduce diurnal variability.
Quantification of natural killer cells (CD56%)
The NK cell assay was done using reagents and antibodies from DAKO Corporation, USA in a Becton Dickinson Flow Cytometer. Flow cytometer measures and analyses optical properties of single cells passing through a focused laser beam, analysis of hundreds of cells per second provides a statistically significant picture, when the cells pass through the laser beam they disrupt and scatter the laser light which is detected as forward scatter (FSC) and side scatter (SSC). While FSC is related to cell size, the SSC is an indicator of cells internal complexity. Cells are stained with monoclonal antibodies coupled with fluorescent dye FITC, and the conjugated samples were acquired using flow cytometer, when acquiring, blood cells are segregated into different populations-lymphocytes, monocytes, and erythrocytes using cell quest pro software version 3.1. The cytometer processes the electronic signals resulting from each cell and creates numeric value for each parameter. Each cell count acquired is taken as one event. Before acquiring this is set based on the availability of the cells in the sample (it is set for 10,000 events). Once acquisition is done, the cells segregated are analyzed by encircling the cell population in FSC/SSC plot. Stained cells are separated from the unstained cells by gating. The cytometer processes the electronic signals resulting from each cell and creates numeric value for each parameter thereby total number of NK cells and percentage NK cells are calculated. Absolute lymphocyte count (ALC) was also estimated using this procedure.
Interventions
The intervention group received “integrated yoga program” and the control group received “supportive counseling sessions” both imparted as individual sessions. The objectives of this yoga intervention as described to participants were as follows: (i) to develop an opportunity to understand one's personal responses to daily stress and explore ways and means to cope with them, (ii) to learn concepts and techniques which bring about stress reduction and change in appraisal, and (iii) to enable the participants to take an active part in their self-care and healing.
The yoga practices consisted of a set of asanas (postures done with awareness) breathing exercises, pranayama (voluntarily regulated nostril breathing), meditation, and yogic relaxation techniques with imagery. These practices were based on principles of attention diversion, awareness and relaxation to cope with stressful experiences.
The sessions began with didactic lectures and interactive sessions on philosophical concepts of yoga and importance of these in managing day-to-day stressful experiences (10 min) beginning every session. This was followed by a preparatory practice (20 min) with few easy yoga postures, breathing exercises, and pranayama and yogic relaxation. The subjects were then guided through any one of these meditation practices for next 30 min which included focusing awareness on sounds and chants from Vedic texts,[21] or breath awareness and impulses of touch emanating from palms and fingers while practicing yogic mudras, or a dynamic form of meditation (cyclic meditation) which involved practice with eyes closed of four yoga postures interspersed with relaxation while supine, thus achieving a combination of both “stimulating” and “calming,” practice.[22] In meditation, participants try to develop clarity in their thinking, learn to observe their own mind, decrease negative mind states and develop positive mind states, and maintain equipoise in their emotions. These sessions were followed by informal individual counseling sessions that focused on problems related to impediments in home practice, clarification of participant's doubts, motivation, and supportive interaction with spouses. The participants were also informed about practical day-to-day application of awareness and relaxation to attain a state of equanimity during stressful situations and were given homework in learning to adapt to such situations by applying these principles.
The subjects were given booklets and instructions on these practices and were encouraged to pursue relevant themes and gain greater depth through proficiency in practice. Subjects were provided audiotapes of these practices for home practice using the instructor's voice so that a familiar voice could be heard on the cassette. Subjects were asked to attend yoga intervention at least two times/week for 12 weeks. The control groups were imparted supportive counseling during their hospital visits. Patients were exposed to at least 24 in person sessions with home practice on the remaining days. Patients were asked to maintain a diary noting their daily activity, daily yoga schedule, duration of practice, intake of medications, and distressing symptoms if any, etc.
Their homework was monitored on a day-to-day basis by their instructor who conducted weekly house visits, and participants were also encouraged to maintain a daily log listing the yoga practices done, use of audiovisual aids, duration of practice, experience of distressful symptoms, and diet history. There were two instructors in all one being a physician in naturopathy and yoga and other a trained and certified therapist in yoga from the yoga institute. They together supervised and imparted the yoga intervention while trained social workers and counselors at the cancer hospital imparted supportive therapy intervention.
Control intervention-supportive counseling sessions
Supportive counseling sessions as control intervention included two important components “education and reinforcing social support.” The reasons why we chose to have education and supportive therapy sessions as control intervention are 3-fold.
This was used as a control intervention to control for the nonspecific effects of the program that may be associated with adjustments such as attention, support, and a sense of control. In fact, these didactic educational interventions are known to improve quality of life of women with breast cancer[23,24] and serve as an effective coping preparation in controlling chemotherapy-related side effects.[25]
Even though the use of education and supportive therapy is a form of enhanced usual care, if yoga program does not provide any benefit over this intervention, then we will know that didactic educational programs should be integrated within the standard of care.
Similar supportive sessions have been used successfully as a control comparison group to evaluate psychotherapeutic interventions.[26,27] These sessions aimed at enriching the patient's knowledge of their disease and treatment options, thereby reducing any apprehensions and anxiety regarding their treatment and involved interaction with the patient's spouses. Subjects and their caretakers were invited to participate in an introductory session lasting 60 min before starting any conventional treatment wherein they were given information about each conventional treatment and management of its related side effects, dietary advice, providing information about a variety of common questions and showing a patient coping successfully. This counseling was extended over the course of their intervention during their hospital visits (once in 10 days, 15 min sessions), and participants were encouraged to meet their counselor whenever they had any concerns or issues to discuss. Subjects in the supportive therapy group also completed daily logs or dairies on treatment-related symptoms, medication, and diet while the goals of yoga intervention were stress reduction and appraisal change, the goals of supportive therapy were education, reinforcing social support, and coping preparation.
Baseline assessments were done on 91 patients in case of metastatic breast cancer patients. A total of 66 patients contributed data to the current analyses. The reasons for dropouts were attributed to migration to other hospitals, use of other complementary therapies (e.g., homeopathy or ayurveda), lack of interest, time constraints, and other concurrent illness [Figure 1]. Among the 66 study completers, 46 out of 66 completers gave the saliva samples as per protocol. Fifteen subjects (yoga n = 5, control, n = 10) in the study were not comfortable in giving saliva samples. Subjects who missed collecting saliva sample on consecutive days at the same time were excluded from the analysis (n = 5).
Figure 1.
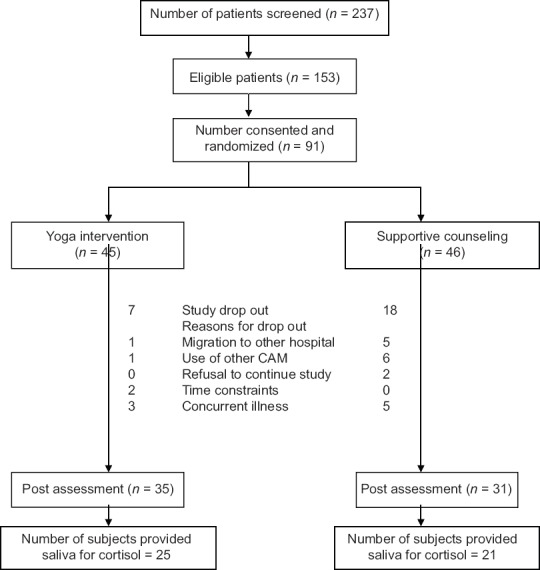
Trial profile
Data analysis
Statistical procedures were conducted using SPSS version 10 (Sun Micro solutions, Gujarat, India) for PC Windows 2000. The data of baseline and follow-up of both the groups were assessed with tests for normality and homogeneity using Shapiro–Wilks test and one-way ANOVA. We used the analysis of covariance (ANCOVA) to study the effects of intervention on outcome measures at follow-up assessments using their respective baseline measure as a covariate. Paired samples’ t-test was done to see within-group changes. All analyses were carried out with intention to treat principle to account for missing values and dropouts.
Diurnal salivary cortisol
Mean cortisol levels for specific time points over a 3-consecutive days were extrapolated at 0600, 0900, 2100 hrs. The diurnal cortisol response was evaluated by calculating the area under curve for time 0600, 0900 and 2100 h. This helps to limit the amount of statistical comparisons between groups to minimize the correction of the α-error probability. With the AUC variables, the number of repeated measurements is irrelevant and thus, the number of statistical comparisons only depends on the number of groups to be compared. With the two AUC formulas, AUCg for baseline diurnal cortisol measurements and AUCi increase in the AUC with respect to AUCg for postmeasure using trapezoidal method,[28] different aspects of the time course of the repeated measurements could be assessed. The slope of diurnal cortisol rhythm was analyzed using random coefficient modeling (i.e., “linear mixed models”), which has been advocated by some researchers.[29] Slopes were compared at baseline and at postmeasurements in both the groups. Alternatively, nonparametric Mann–Whitney U-test and Wilcoxon-signed rank test were also done for variables with skewed distribution.
RESULTS
Sociodemographic and medical characteristics of the study sample
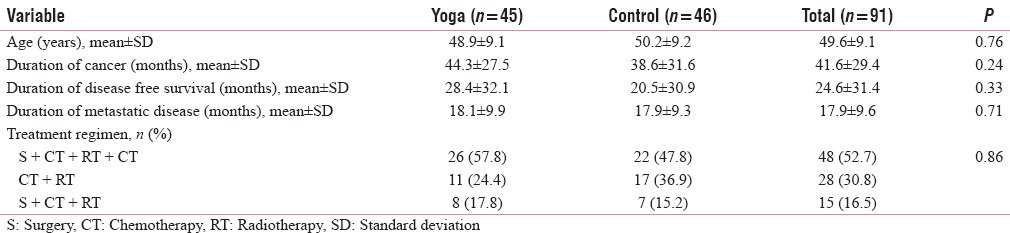
The mean age of participants was 48.9 ± 9.1 years in yoga and 50.2 ± 9.2 years in control groups. Twenty-Six subjects underwent surgery, chemotherapy, radiotherapy and chemotherapy, 11 subjects received chemotherapy and radiotherapy and eight subjects underwent surgery and radiotherapy as primary treatment. Participants in both groups were comparable with respect to sociodemographic and medical characteristics. A goodness of fit test run on all these demographic variables did not show any significant changes between yoga and supportive therapy groups (P > 0.05) [Table 1].
Table 1.
Demographic and medical characteristics of the initially randomized sample
Insomnia Rating Scale
Insomnia Rating Scale symptom distress
ANCOVA on postmeasures using baseline symptom distress scores as a covariate showed a significant difference between groups with better decrease in symptom distress scores in yoga compared to control group [F (1,61) = 21.23, P < 0.001, ES-1.2, Percentage change (PC) - 91.31%]. Paired-sample t-test done to assess within group change showed a significant decrease in symptom distress scores in yoga group only (t = 3.1, P = 0.004) and not in the control group (t = −1.32, P = 0.19) [Table 2].
Table 2.
Comparison of Insomnia Rating Scale scores using analysis of covariance between yoga and control groups with the respective baseline measure as a covariate
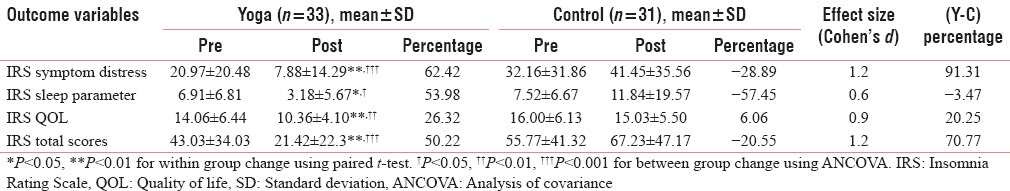
Insomnia Rating Scale sleep parameters
ANCOVA on postmeasures using baseline sleep distress parameter scores as a covariate showed a significant difference between groups with better decrease in sleep distress parameter scores in yoga compared to control group [F (1,61) = 5.75, P = 0.02, ES - 0.6, PC - 111.43%]. Paired-sample t-test done to assess within group change showed a significant decrease in sleep distress parameter scores in yoga group only (t = 2.5, P = 0.01) and not in the control group (t = −1.30, P = 0.20) [Table 2].
Insomnia Rating Scale quality of life
ANCOVA on postmeasures using baseline sleep quality of life scores as a covariate showed a significant difference between groups with better decrease in sleep quality of life scores in yoga compared to control group [F (1,61) = 13.03, P = 0.001, ES - 0.9, PC - 20.25%]. Paired-sample t-test done to assess within group change showed a significant decrease in sleep quality of life scores in yoga group only (t = 2.9, P = 0.006) and not in the control group (t = 0.78, P = 0.44) [Table 2].
Insomnia Rating Scale total scores
ANCOVA on postmeasures using baseline sleep total distress scores as a covariate showed a significant difference between groups with better decrease in sleep total distress scores in yoga compared to control group [F (1,61) = 22.40, P = 0.001, ES - 1.2, PC - 70.77%]. Paired-sample t-test done to assess within group change showed a significant decrease in sleep total distress scores in yoga group only (t = 3.3, P = 0.002) and not in the control group (t = −1.33, P = 0.19) [Table 2].
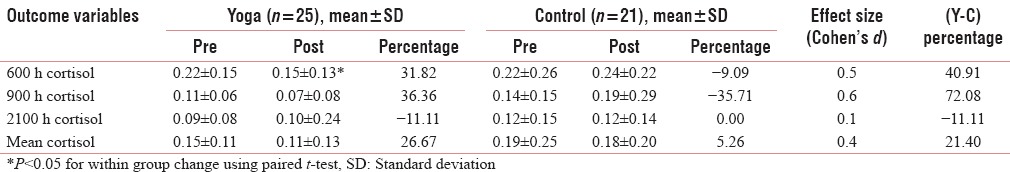
Diurnal salivary cortisol levels
ANCOVA was used to assess between-group differences using baseline cortisol value (for the corresponding time) as a covariate did not show any significant change. A liner mixed effects model using R software showed no difference in precortisol slopes (P = 0.67, t = 0.41) and postcortisol slopes (post: P =0.42, t = 0.8) between groups [Table 3]. Paired-samples t-test to assess within group change following intervention showed a significant decrease in 0600 h. Cortisol (t = 2.28, P = 0.031) in yoga group alone but not in the control group (t = −0.31, P = 0.76) [Table 3].
Table 3.
Results of diurnal cortisol levels after intervention using paired t-test and analysis of covariance
Natural killer cell count and percentage
ANCOVA was used to assess between-group differences using baseline NK cell % value as a covariate showed significant improvement in NK cell % in yoga group compared to control group [F (1, 31) = 5.43, P = 0.03, ES - 0.5, PC - 32.43%]. Other parameters such as NK cell count did not show any significant difference between groups. Paired-samples t-test to assess within group change following intervention showed a significant increase in NK cell % (t = −3.10, P < 0.01) in yoga group alone but not in the control group (t = 1.03, P = 0.32) [Table 4].
Table 4.
Comparison of mean values of natural killer cell and absolute lymphocyte count levels using paired t-test and analysis of covariance
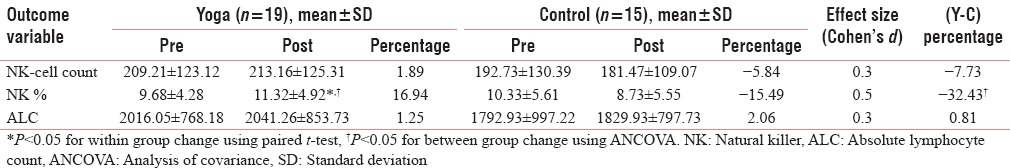
Absolute lymphocyte count
The baseline values of ALC were different in the two groups. There was no significant change within or between groups in ALC [Table 4].
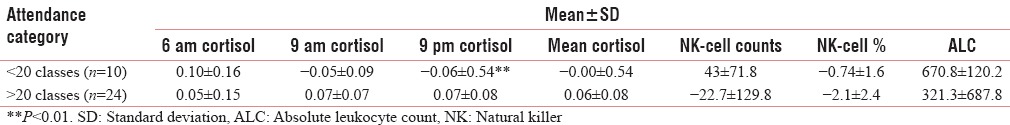
Adherence to intervention
In this study, the adherence was good with 80% attending 24 supervised sessions. There was a significant decrease in 9 am salivary cortisol levels (t = −3.6, P = 0.001) in those who attended >20 classes as compared to those attending <20 classes on independent samples t-test [Table 5].
Table 5.
Comparison of change scores on salivary cortisol and natural killer cell counts using independent samples t-test between those attending yoga classes (>20/<20 classes) in yoga group
DISCUSSION
Sleep on Pittsburg Insomnia Rating Scale
In this study, there was a significant decrease in symptom distress (91.3%, ES = 1.2), sleep parameters (111.4%, ES = 0.6), quality of life (20.3%, ES = 0.9), and overall insomnia score (70.8%, ES = 1.2). Our results are consistent with earlier findings with mindfulness-based stress reduction intervention that has shown improvement in overall sleep quality by 20.4%.[30] Insomnia has been related to poor NK cell function, higher morning cortisol levels and abnormal diurnal rhythms in breast cancer patients.[8] This is an important problem as it seems to worsen with age and psychological distress.[5] This is also one of the important symptoms in the cancer care continuum expressed often by patients.[4] Improving sleep duration, quality, and restoring the normal sleep rhythms are important to preserve immune homeostasis and quality of life. The improvements seen with our intervention suggests that yoga could be used as an adjunct to manage sleep disorders in cancer patients.
Diurnal salivary cortisol level
There was also a significant decrease in early morning salivary cortisol levels in the advanced breast cancer study in yoga group only (40.9%, ES = 0.5). The decrease in morning salivary cortisol levels suggests possible stress-reducing benefits of yoga intervention. Our results are similar to earlier studies that have shown similar decreases in cortisol in early breast cancer study undergoing adjuvant radiotherapy.[17] Our results are also similar to changes (16%–45%) in cortisol seen with behavioral interventions in cancer populations.[13,31,32] While these earlier studies have measured one time plasma cortisol, we chose to assess both morning and evening levels of free salivary cortisol as changes in the rate of cortisol secretion over a day (diurnal cortisol rhythm) is considered as a robust measure compared to onetime cortisol assessment.[8,33] Earlier studies with similar stress reduction interventions such as MBSR have also shown decrements in cortisol in breast cancer patients who had initially high cortisol levels suggesting that more distressed patients tend to benefit with stress reduction intervention.[18] However, there was no difference in both high and low basal cortisol groups in our study.
One of the major limitations in this study is the inequality in contact duration of interventions. Supportive therapy interventions were used with an intention of negating the confounding variables such as instructor-patient interaction, education, and attention.[27] However, inequality in contact duration of this intervention could have affected its effectiveness as successes of such interventions depend mainly on contact duration and content. Similar supportive sessions have been used successfully as a control comparison group to evaluate psychotherapeutic interventions[26,27] and have been effective in controlling chemotherapy-related side effects.
CONCLUSION
Future studies should unravel the putative mechanisms and aspects of hypothalamic-pituitary-adrenal axes dysregulations and assess neuroendocrine responses to artificially induced stressors in the laboratory. Future studies should use more sophisticated measurements of immune function such as NK cell cytotoxicity, DNA repair mechanism, etc., to understand the psychoneuroimmune mechanisms underlying such interventions. Larger randomized controlled studies using more structured psychiatric and behavioral intervention as controls are needed.
Financial support and sponsorship
This Study was funded with grants from the Central Council for research in Yoga and Naturopathy, Ministry of AYUSH, Government of India.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Central Council for Research in Yoga and Development, Ministry of AYUSH, Government of India.
REFERENCES
- 1.Cleeland CS, Mayer M, Dreyer NA, Yim YM, Yu E, Su Z, et al. Impact of symptom burden on work-related abilities in patients with locally recurrent or metastatic breast cancer: Results from a substudy of the VIRGO observational cohort study. Breast. 2014;23:763–9. doi: 10.1016/j.breast.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Kenne Sarenmalm E, Ohlén J, Odén A, Gaston-Johansson F. Experience and predictors of symptoms, distress and health-related quality of life over time in postmenopausal women with recurrent breast cancer. Psychooncology. 2008;17:497–505. doi: 10.1002/pon.1258. [DOI] [PubMed] [Google Scholar]
- 3.Hagen KB, Aas T, Lode K, Gjerde J, Lien E, Kvaløy JT, et al. Illness uncertainty in breast cancer patients: Validation of the 5-item short form of the Mishel Uncertainty in Illness Scale. Eur J Oncol Nurs. 2015;19:113–9. doi: 10.1016/j.ejon.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 4.Berger AM. Update on the state of the science: Sleep-wake disturbances in adult patients with cancer. Oncol Nurs Forum. 2009;36:E165–77. doi: 10.1188/09.ONF.E165-E177. [DOI] [PubMed] [Google Scholar]
- 5.Fetveit A. Late-life insomnia: A review. Geriatr Gerontol Int. 2009;9:220–34. doi: 10.1111/j.1447-0594.2009.00537.x. [DOI] [PubMed] [Google Scholar]
- 6.Berger AM, Farr L. The influence of daytime inactivity and nighttime restlessness on cancer-related fatigue. Oncol Nurs Forum. 1999;26:1663–71. [PubMed] [Google Scholar]
- 7.Abercrombie HC, Giese-Davis J, Sephton S, Epel ES, Turner-Cobb JM, Spiegel D. Flattened cortisol rhythms in metastatic breast cancer patients. Psychoneuroendocrinology. 2004;29:1082–92. doi: 10.1016/j.psyneuen.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Sephton SE, Sapolsky RM, Kraemer HC, Spiegel D. Diurnal cortisol rhythm as a predictor of breast cancer survival. J Natl Cancer Inst. 2000;92:994–1000. doi: 10.1093/jnci/92.12.994. [DOI] [PubMed] [Google Scholar]
- 9.Giese-Davis J, Sephton SE, Abercrombie HC, Durán RE, Spiegel D. Repression and high anxiety are associated with aberrant diurnal cortisol rhythms in women with metastatic breast cancer. Health Psychol. 2004;23:645–50. doi: 10.1037/0278-6133.23.6.645. [DOI] [PubMed] [Google Scholar]
- 10.Baltrusch HJ, Stangel W, Titze I. Stress, cancer and immunity. New developments in biopsychosocial and psychoneuroimmunologic research. Acta Neurol (Napoli) 1991;13:315–27. [PubMed] [Google Scholar]
- 11.Levy S, Herberman R, Lippman M, d’Angelo T. Correlation of stress factors with sustained depression of natural killer cell activity and predicted prognosis in patients with breast cancer. J Clin Oncol. 1987;5:348–53. doi: 10.1200/JCO.1987.5.3.348. [DOI] [PubMed] [Google Scholar]
- 12.Granath J, Ingvarsson S, von Thiele U, Lundberg U. Stress management: A randomized study of cognitive behavioural therapy and yoga. Cogn Behav Ther. 2006;35:3–10. doi: 10.1080/16506070500401292. [DOI] [PubMed] [Google Scholar]
- 13.Cruess DG, Antoni MH, McGregor BA, Kilbourn KM, Boyers AE, Alferi SM, et al. Cognitive-behavioral stress management reduces serum cortisol by enhancing benefit finding among women being treated for early stage breast cancer. Psychosom Med. 2000;62:304–8. doi: 10.1097/00006842-200005000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Spiegel D, Bloom JR, Kraemer HC, Gottheil E. Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet. 1989;2:888–91. doi: 10.1016/s0140-6736(89)91551-1. [DOI] [PubMed] [Google Scholar]
- 15.Lengacher CA, Kip KE, Barta M, Post-White J, Jacobsen PB, Groer M, et al. A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers. J Holist Nurs. 2012;30:170–85. doi: 10.1177/0898010111435949. [DOI] [PubMed] [Google Scholar]
- 16.Banasik J, Williams H, Haberman M, Blank SE, Bendel R. Effect of Iyengar yoga practice on fatigue and diurnal salivary cortisol concentration in breast cancer survivors. J Am Acad Nurse Pract. 2011;23:135–42. doi: 10.1111/j.1745-7599.2010.00573.x. [DOI] [PubMed] [Google Scholar]
- 17.Vadiraja HS, Raghavendra RM, Nagarathna R, Nagendra HR, Rekha M, Vanitha N, et al. Effects of a yoga program on cortisol rhythm and mood states in early breast cancer patients undergoing adjuvant radiotherapy: A randomized controlled trial. Integr Cancer Ther. 2009;8:37–46. doi: 10.1177/1534735409331456. [DOI] [PubMed] [Google Scholar]
- 18.Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29:448–74. doi: 10.1016/s0306-4530(03)00054-4. [DOI] [PubMed] [Google Scholar]
- 19.Moul D, Pilkonis P, Miewald J. Preliminary study of the test-retest reliability and concurrent validities of the Pittsburgh Insomnia Rating Scale (PIRS) Sleep Abstract Supplement. 2002:A246–7. [Google Scholar]
- 20.Veqar Z, Hussain ME. Validity and reliability of insomnia severity index and its correlation with pittsburgh sleep quality index in poor sleepers among Indian university students. Int J Adolesc Med Health. 2017 doi: 10.1515/ijamh-2016-0090. pii:/j/ijamhahead-of-print/ijamh-2016-0090/ijamh-2016-0090xml. [DOI] [PubMed] [Google Scholar]
- 21.Telles S, Nagarathna R, Nagendra HR. Autonomic changes while mentally repeating two syllables – One meaningful and the other neutral. Indian J Physiol Pharmacol. 1998;42:57–63. [PubMed] [Google Scholar]
- 22.Telles S, Reddy SK, Nagendra HR. Oxygen consumption and respiration following two yoga relaxation techniques. Appl Psychophysiol Biofeedback. 2000;25:221–7. doi: 10.1023/a:1026454804927. [DOI] [PubMed] [Google Scholar]
- 23.Helgeson VS, Cohen S, Schulz R, Yasko J. Long-term effects of educational and peer discussion group interventions on adjustment to breast cancer. Health Psychol. 2001;20:387–92. doi: 10.1037//0278-6133.20.5.387. [DOI] [PubMed] [Google Scholar]
- 24.Helgeson VS, Cohen S, Schulz R, Yasko J. Education and peer discussion group interventions and adjustment to breast cancer. Arch Gen Psychiatry. 1999;56:340–7. doi: 10.1001/archpsyc.56.4.340. [DOI] [PubMed] [Google Scholar]
- 25.Burish TG, Snyder SL, Jenkins RA. Preparing patients for cancer chemotherapy: Effect of coping preparation and relaxation interventions. J Consult Clin Psychol. 1991;59:518–25. doi: 10.1037//0022-006x.59.4.518. [DOI] [PubMed] [Google Scholar]
- 26.Greer S, Moorey S, Baruch JD, Watson M, Robertson BM, Mason A, et al. Adjuvant psychological therapy for patients with cancer: A prospective randomised trial. Br Med J. 1992;304:675–80. doi: 10.1136/bmj.304.6828.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Telch CF, Telch MJ. Group coping skills instruction and supportive group therapy for cancer patients: A comparison of strategies. J Consult Clin Psychol. 1986;54:802–8. doi: 10.1037//0022-006x.54.6.802. [DOI] [PubMed] [Google Scholar]
- 28.Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28:916–31. doi: 10.1016/s0306-4530(02)00108-7. [DOI] [PubMed] [Google Scholar]
- 29.Rogosa D, Saner H. Longitudinal data analysis examples with random coefficient models. J Educ Behav Statistics. 1995;20:149–70. [Google Scholar]
- 30.Carlson LE, Garland SN. Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med. 2005;12:278–85. doi: 10.1207/s15327558ijbm1204_9. [DOI] [PubMed] [Google Scholar]
- 31.Schedlowski M, Jung C, Schimanski G. Effects of behavioral intervention on plasma cortisol and lymphocytes in breast cancer patients: An exploratory study. Psychooncology. 1994;3:181–7. [Google Scholar]
- 32.van der Pompe G, Duivenvoorden HJ, Antoni MH, Visser A, Heijnen CJ. Effectiveness of a short-term group psychotherapy program on endocrine and immune function in breast cancer patients: An exploratory study. J Psychosom Res. 1997;42:453–66. doi: 10.1016/s0022-3999(96)00393-5. [DOI] [PubMed] [Google Scholar]
- 33.Turner-Cobb JM, Sephton SE, Koopman C, Blake-Mortimer J, Spiegel D. Social support and salivary cortisol in women with metastatic breast cancer. Psychosom Med. 2000;62:337–45. doi: 10.1097/00006842-200005000-00007. [DOI] [PubMed] [Google Scholar]


