Abstract
Background:
Head and neck cancer pain is intractable and difficult to manage. Many a times it is difficult to treat with oral opioids and adjuvants.
Aim:
This study aims to study the effects of transnasal sphenopalatine ganglion block (SPGB), administered using cotton swab/ear bud by patients’ caretaker, at home, for pain management.
Study Design:
This is a prospective, single-arm observational study conducted on 100 head and neck cancer patients, from January 2014 to December 2015. Patients and caretaker were given a demonstration of the procedure using sterile cotton swab/ear buds. They were advised to repeat the procedure when their visual analog score (VAS) was more than 5. They continued with the oral analgesics. They kept the records of pre- and post-procedure pain score (VAS), the frequency of repetition, ease of performance of procedure, and morphine requirement. A paired t-test (SPSS software) was used for statistical analysis.
Results:
A significant reduction in pain was noted by a decrease in mean VAS from 8.57 ± 1.31 to 2.46 ± 1.23 (P < 0.0001), immediately on first administration. The mean duration of analgesia was 4.95 ± 3.43 days. Pre- and post-procedure mean morphine requirement were 128.2 ± 84.64 and 133.8 ± 81.93 (P > 0.05) mg per day, at the end of 2 months. Ease of performance was observed in 88 patients.
Conclusion:
The home-based application of SPGB is an easy, safe, and cost-effective method to manage cancer pain. It provides excellent immediate pain relief with a minimum side effect. It can be performed bilaterally, repeatedly and even with a feeding tube in place.
Keywords: Head and neck cancer, pain management, palliative care, sphenopalatine ganglion block
INTRODUCTION
Head and neck cancers are common cancers, with a prevalence rate of 57.5% in India. It accounts for 30% of all cancers in India.[1] Due to high consumption of tobacco, these types of cancers are significantly prevalent in Gujarat. Pain[2] in patients with head and neck cancer is most frequent symptom; it is severe, intractable and sometimes difficult to treat with pharmacological therapy. Hence, the need for intervention rises.[3]
Sphenopalatine ganglion is one of the four ganglion in head and neck area, situated in pterygopalatine fossa found outside the cranium.[4,5] It is mainly a parasympathetic ganglion and is exposed to the environment through our nasal cavity. Science has proved that sphenopalatine ganglion block (SPGB) provides excellent analgesia in various types of acute and chronic orofacial pain.[4,5,6,7] There are various approaches[4,5,6,7,8] described for this procedure, of which transnasal approach using local anesthetic agent is a less invasive, easy and safe method of pain relief but provides temporary analgesia, hence, needs to be performed repeatedly. Conventional methods of transnasal block require the use of endoscope,[9] image guidance,[10,11,12] or special catheter like Tx360[10] Spinocath, or[11] Allevio.[12] We modified the technique using cotton swab/ear buds so that it can be performed at home.
We used various devices such as intravenous cannula, cotton swab sticks, and ear buds during our pilot study of SPGB in head and neck cancer pain management on 385 patients at our institute and developed a standard technique using ear buds to be inserted transnasal.
This study was undertaken with the primary aim of providing immediate pain relief to head and neck cancer patients attending our outpatient department (OPD) with moderate to severe pain. It was also aimed to study effects of SPGB, its duration of analgesia, morphine requirement, ease of performance of procedure at home.
METHODS
This was a prospective, single-arm, observational study performed at State Cancer Institute. The study duration was 2 years, i.e., from January 2014 to December 2015 for 100 patients. The study was approved by the Institutional Review Board. Patients were reviewed for detailed history, pain assessment, investigations, and examination including examination of both nostrils. Patients and caretakers were explained the procedure thoroughly. Those who expressed willingness to participate in the study were enrolled in this study, and their written informed consent was obtained.
Inclusion criteria
The inclusion criteria were (1) Patients with moderate to severe pain (visual analog score [VAS] >5). (2) Patient whose pain is not well controlled on oral morphine. (3) Good pain relief with previous SPGB. (4) Patients and caretakers who can comprehend what we explain or understand the procedure demonstration.
Exclusion criteria
Patients with bleeding diathesis and/or nasal obstruction, nasopharyngeal growth, carcinoma maxilla, intracranial extension of disease, recent nasal, or sinus surgery were excluded from the study.
The procedure was performed in the presence of caretaker. The patients were placed in supine position, and their affected side (ipsilateral) of nostril was anesthetized with Lignocaine jelly. After 5 min, a sterile cotton swab stick, soaked in Lignocaine jelly was inserted in anesthetized nostril, in upward and backward direction[13] till resistance was felt or for a maximum of 5 cm. Injection bupivacaine 0.5%, one ml was instilled along the side of stick, so that the drug can reach at the base of the medial turbinate. After 5 min, the stick was redirected upward, lateral, and backward[13] to cover wide area. Again one ml of injection bupivacaine was instilled in a similar fashion. Patients were kept in the same position for 6–8 min. The procedure was demonstrated and explained to caretaker at the same time. We also made the caretaker practice the procedure in our presence [Figure 1]. If they could perform it easily, then they were allowed to perform the procedure at home. For preparing a cotton swab at home, ear buds were used as shown in [Figure 2].
Figure 1.

Patient's relative performing sphenopalatine block
Figure 2.
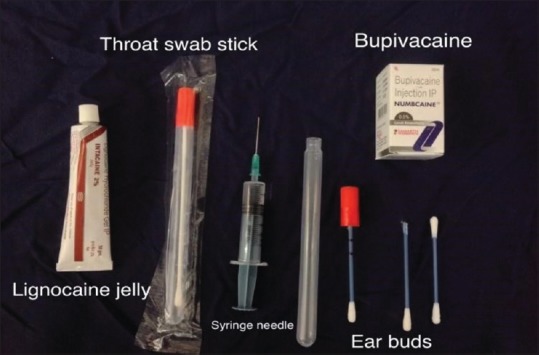
Material used for sphenopalatine block at home
Caretakers were asked to repeat the procedure at home when patient's VAS was more than 5. They also maintained a diary for pre- and post-procedure pain score (VAS), frequency of repetition of the procedure and ease of performance, which was described as follows.
Easy = caretaker can insert the ear bud and instilled medicine in the first attempt.
Not easy = caretaker can insert the ear bud and instilled medicine in more than two attempts.
Difficult = Caretaker is not able to insert the ear bud in nostril.
This was checked during follow-up visits, every 2 weeks, for next 2 months. Immediate pain relief was noted by an immediate reduction in pain score and duration of analgesia was noted by the frequency of repetition of the procedure. All other pharmacological therapy including morphine and adjuvant were continued. The requirement of morphine, side effects, and any untoward effects was noted. Statistical analysis was done using paired t-test using SPSS 20, software (IBM, Armonk, NY, USA).
RESULTS
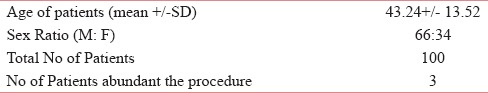
A total of hundred patients of head and neck cancer were enrolled in this study. There were 66 males and 34 females. Three patients were excluded from study either due to difficult procedure or due to procedure related complication [Table 1].
Table 1.
Demographic details of patients
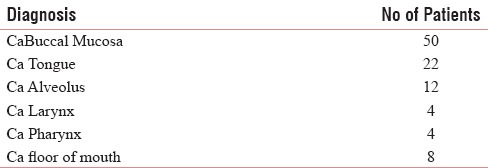
The diagnosis of patients was carcinoma of buccal mucosa (50), tongue (22), alveolus (12), larynx (4), pharynx (4), and floor of mouth (8) [Table 2].
Table 2.
Diagnosis of Patients
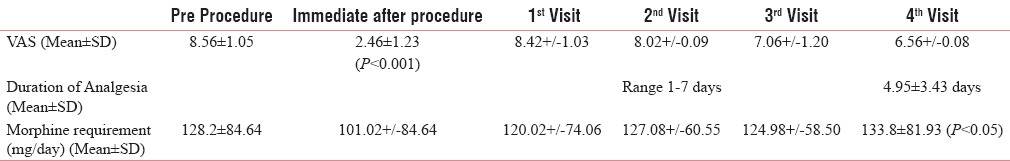
Immediate pain relief was observed by a reduction in VAS score after the procedure, which was reduced from 8.56 ± 1.05 to 2.46 ± 1.23 (P < 0.0001). The mean duration of analgesia was 4.95 ± 3.43 days, (range 1–7 days).
Pre- and post-procedure mean morphine requirements were 128.2 ± 84.64 and 133.8 ± 81.93 (P > 0.05), mg per day, at the end of 2 months [Table 3].
Table 3.
Pre & Post-procedure VAS, Duration of Analgesia and Morphine Requirement
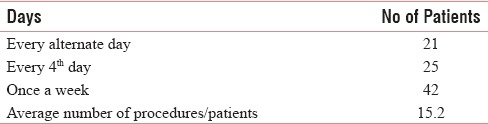
Totally, 42 patients required it to be performed every week, 25 patients, once in 4 days, while 21 patients received SPGB every alternate day [Table 4].
Table 4.
No of Procedures done at home
The ease of performance was observed in 88 patients, and it was found to not easy to perform in nine patients. Two patients did not receive SPGB at home as their caretaker found difficulty in administration.
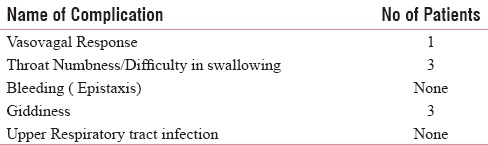
No serious complications were observed in any patients except giddiness in three patients and temporary numbness in throat in three patients which resulted in temporary difficulty in swallowing. All patients felt the bitter taste of drugs [Table 5].
Table 5.
Complications
The cost of the materials used in the procedure is 22 Rs. per procedure.
DISCUSSION
Although sphenopalatine ganglion[4,5,6,7,8] is considered mainly as a parasympathetic ganglion, it also has sympathetic and sensory innervations. Its parasympathetic preganglionic fibers arise from superior salivatory nucleus of facial nerve in medulla which traverses as a greater petrosal nerve. These parasympathetic fibers along with sympathetic from deep petrosal nerve create nerves to viridian canal and enter sphenopalatine ganglion. The postganglionic parasympathetic fibers supply to nasal gland, palatine gland, and lacrimal gland. The sympathetic fibers projecting to sphenopalatine ganglion arise from upper thoracic spinal cord T1–T2. The postganglionic fibers synapse in superior cervical ganglion. Postganglionic sympathetic fibers from superior cervical ganglion entries in sphenopalatine ganglion via deep pterosal nerve which are an extension of carotid plexus. Superior cervical ganglion is connected with upper cervical nerve roots (C1, C2, and C3) and so cervical ganglion has connection with sphenopalatine ganglion. Sensory innervations of sphenopalatine ganglion are through the maxillary nerve of trigeminal nerve. Hence, the pain from upper cervical and back gets referred to head and facial area and vice versa. This might explain why SPGB would relieve a headache, facial pain, and pain in the neck as well as upper back.
Approximately, 67%–91% of patients with head and neck cancer have relatively high prevalence of pain.[1,2] About 80%–90% of cancer pain can be eliminated by pharmacological method according to the WHO Analgesic Ladder, but nearly half of all these patients receive less than optimum care[1] and require intervention for their pain management.[3]
Sphenopalatine block[6,16] alone or as an adjuvant has been utilized by many authors for management of wide varieties of orofacial pain such as Sluder's neuralgia, trigeminal neuralgia, cluster headache, migraine, complex regional pain syndrome of head and neck and pain due to advanced malignancy of head and neck. Saade and Paige,[14] Varghese and Koshy,[9] and Prasanna A[15] have reported its role in immediate pain relief in head and neck cancer pain management.
For sphenopalatine block, various techniques,[6] superficial to highly invasive have been described such as transnasal, endoscope-guided transnasal, intraoral and infrazygomatic lateral approach. SPGB by transnasal approach[6,7,8,9,10,11,12,13,14,15] is a very easy and safe method of pain relief.[16] Cotton tipped applicator dipped in topical anesthetic agent is placed on nasopharyngeal mucosa posterior to middle turbinate in the conventional method.[13] Several modifications of transnasal technique have been published which includes Mingi's modification[7] of technique using an intratracheal cannula. Intranasal device such as Sphenocath,[11] Allevio,[12] and have been used to block the ganglion. Windsor and Jahnke[8] and Cady et al.[10] have modified the techniques to minimize drug requirement.
We used sterile cotton swab stick or sterile ear bud instead of a cotton-tipped applicator. It makes the procedure more easy, safe, and cost-effective so that caretaker can perform it at home.
Various agents,[6] for example, local anesthetic such as 4% cocaine, 2%–4% lignocaine,[7,13,11] or 0.5% bupivacaine,[7,8] depot steroids and neurolytic agent[9] had been tried for SPGB. An injection of neurolytic agent is not always easy and safe, without the use of an endoscope. Repeated use of steroid has its own complications. Cady et al.[10] used 0.5% bupivacaine, 0.3 ml while We used 0.5% injection bupivacaine 2 ml in each nostril.
Cancer is a dynamic process in which as the disease progresses; one can never get optimal pain relief with time. Furthermore, it requires a different treatment plan as time passes an increase in opioids requirement and needs to the repetition of the procedure frequently. The use of local anesthetic agent provides excellent immediate pain relief but only temporary in nature. Varghese and Koshy[9] used 6% phenol for transnasal block under endoscopic guidance in 22 patients. He found immediate pain relief was good but had to repeat the procedure in four patients. Prasanna and Morphy[15] also found good immediate pain relief. In our study, immediate pain relief was excellent in all the patients, but the rate of repetition of the procedure greatly varied between every alternate day to 7 days.
Our additional observations were SPGB caused mood elevation, relieved insomnia in all patients; patients were able to swallow without pain which helped in the improvement of food intake. Schaffer et al.[17] utilized SPGB for the management of an acute headache in the emergency department and he found that along with a headache it also controls nausea.
The top four symptoms[18] (2014) in head and neck cancer are pain, insomnia, loss of appetite and fatigue. SPGB provides analgesia and adequate sleep. The aim of cancer pain management in palliative care is to relieve pain with less adverse effects thereby improving the quality of life of patients.[1,2,3]
SPGB using local anesthetic agent have no serious side effects except temporary bitter taste, temporary difficulty in breathing and swallowing, lightheadedness, and sometimes epistaxis.[3,4,5,6,7] One of our patients had vasovagal response, in whom the procedure was abandoned. Three patients had temporary difficulty in swallowing. Bitter taste was complained by almost all patients.
According to the American Institute of Medicine[19] (2011) and American Pain Society[20] (2005) psychological interventions such as patient's education, communication, and involvement of caretaker in management reduce psychological distress while improving the quality of life of cancer patients.[1] The home-based application of SPGB improves both patients’ and caretakers’ confidence in managing difficult situations.
Saade and Paige[14] utilized the same method, i.e., self-administration of SPGB in patients with lethal midline granuloma requiring high dose of morphine. He taught patients to administer 4% lignocaine 1.5 ml into each nostril three times a day as well as to follow-up after 3 months. There was a substantial pain relief and reduction of morphine dose without any complication. With 6% aqueous phenol, Varghese, and Koshy[9] could stop analgesics in two patients and adjuvant in eight patients but only for 1 week. In our study, all our patients were already on oral morphine immediate release, having partial pain relief. Their morphine requirement did not change significantly.
Eighty-eight patients were able to perform the procedure easily at home. All had optimum control of pain while their morphine requirements either remained stable or increased.
CONCLUSION
Home-based application of SPGB is an easy, safe, and cost-effective method of management of acute, chronic, and breakthrough pain. It provides excellent immediate pain relief with a minimum side effect. It can be performed bilaterally, repeatedly and even with a feeding tube in place. It can be taught to caregivers so that it can be performed safely as well as effectively at home. Home-based application of SPGB with local anesthetic agent will fulfill the aim of palliation and symptoms management at home. It will eliminate frequent visits to hospitals or doctors.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kulkarni MR. Head and neck cancer Burden in India. Review article. Int J Head Neck Surg. 2013;4:29–35. [Google Scholar]
- 2.Chiara B, Francesco M, Laura C, Mariasole M, Andrea C. Pain in head and neck cancer: Prevalence and possible predictive factors - Review article. J BUON. 2014;19:592–7. [PubMed] [Google Scholar]
- 3.Joshi M, Chambers WA. Pain relief in palliative care: A focus on interventional pain management. Expert Rev Neurother. 2010;10:747–56. doi: 10.1586/ern.10.47. [DOI] [PubMed] [Google Scholar]
- 4.Khonsary SA, Ma Q, Villablanca P, Emerson J, Malkasian D. Clinical functional anatomy of the pterygopalatine ganglion, cephalgia and related dysautonomias: A review. Surg Neurol Int. 2013;4(Suppl 6):S422–8. doi: 10.4103/2152-7806.121628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Campbell EH. Affections of the sphenopalatine ganglion. Ann Surg. 1935;101:429–37. doi: 10.1097/00000658-193501000-00046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piagkou M, Demesticha T, Troupis T, Vlasis K, Skandalakis P, Makri A, et al. The pterygopalatine ganglion and its role in various pain syndromes: From anatomy to clinical practice. Pain Pract. 2012;12:399–412. doi: 10.1111/j.1533-2500.2011.00507.x. [DOI] [PubMed] [Google Scholar]
- 7.Mingi C, Seng J, Wang Y, Martin S. Sphenopalatine ganglion block - A simple but underutilized therapy for pain control. J Pain. 1996;6:97–104. [Google Scholar]
- 8.Windsor RE, Jahnke S. Sphenopalatine ganglion blockade: A review and proposed modification of the transnasal technique. Pain Physician. 2004;7:283–6. [PubMed] [Google Scholar]
- 9.Varghese BT, Koshy RC. Endoscopic transnasal neurolytic sphenopalatine ganglion block for head and neck cancer pain. J Laryngol Otol. 2001;115:385–7. doi: 10.1258/0022215011907938. [DOI] [PubMed] [Google Scholar]
- 10.Cady R, Saper J, Dexter K, Manley H. A double blind, placebo controlled study of repetitive transnasal sphenopalatine ganglion blockade with Tx360® as acute treatment for chronic migraine - Research submission. Headache. 2015;55:101–16. doi: 10.1111/head.12458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dolor Technologies, LLC; 2015. 2015. [Cited on 2017 March 06]. Available from: http://www.Sphenocath.com .
- 12.Jet Medical. 2015. [Last accessed 2017 Mar 06]. Available from: http://www.Alleviospg.com .
- 13.Serdar E. Sympathetic block of the head and neck. In: Prithvi Raj P, editor. Interventional Pain Management: Image Guided Procedure. 2nd ed. Philadelphia: Saunders Elsevier; 2008. pp. 288–91. [Google Scholar]
- 14.Saade E, Paige GB. Patient-administered sphenopalatine ganglion block. Reg Anesth. 1996;21:68–70. [PubMed] [Google Scholar]
- 15.Prasanna A, Murthy PS. Sphenopalatine ganglion block and pain of cancer. J Pain Symptom Manage. 1993;8:125. doi: 10.1016/0885-3924(93)90139-m. [DOI] [PubMed] [Google Scholar]
- 16.Peterson JN, Schames J, Schames M, King E. Sphenopalatine ganglion block: A safe and easy method for the management of orofacial pain. Cranio. 1995;13:177–81. doi: 10.1080/08869634.1995.11678065. [DOI] [PubMed] [Google Scholar]
- 17.Schaffer JT, Hunter BR, Ball KM, Weaver CS. Noninvasive sphenopalatine ganglion block for acute headache in the emergency department: A randomized placebo-controlled trial. Ann Emerg Med. 2015;65:503–10. doi: 10.1016/j.annemergmed.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 18.Gandhi AK, Roy S, Thakar A, Sharma A, Mohanti BK. Symptom burden and quality of life in advanced head and neck cancer patients: AIIMS study of 100 patients. Indian J Palliat Care. 2014;20:189–93. doi: 10.4103/0973-1075.138389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 20.Gordon DB, Dahl JL, Miaskowski C, McCarberg B, Todd KH, Paice JA, et al. American pain society recommendations for improving the quality of acute and cancer pain management: American Pain Society Quality of Care Task Force. Arch Intern Med. 2005;165:1574–80. doi: 10.1001/archinte.165.14.1574. [DOI] [PubMed] [Google Scholar]


