Abstract
Objective
To estimate the prevalence of extreme obesity in a large, multiethnic contemporary cohort of children and adolescents.
Study design
In a cross-sectional study, measured weight and height were extracted from electronic medical records of 710 949 patients aged 2 to 19 years (87.8% of eligible patients) who were enrolled in an integrated prepaid health plan in 2007 and 2008. Prevalence of extreme obesity was defined as body mass index (BMI)-for-age ≥1.2 times 95th percentile or BMI ≥35 kg/m2.
Results
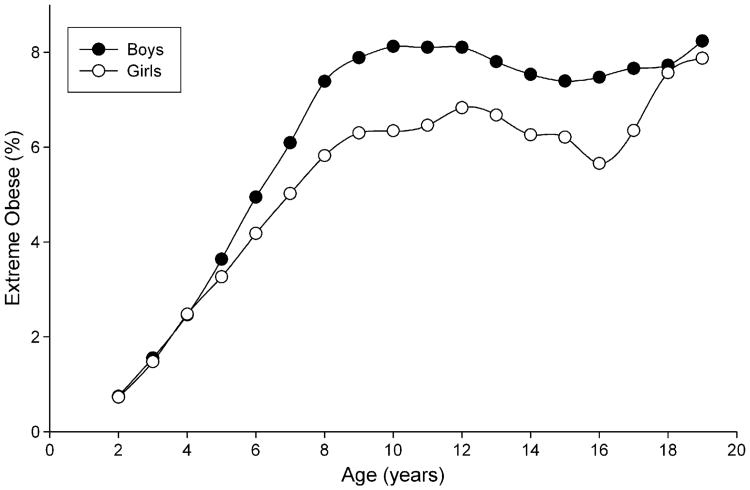
Extreme obesity was observed in 7.3% of boys and 5.5% of girls. The prevalence peaked at 10 years of age in boys and at 12 years of age with a bimodal distribution in girls (second peak at 18 years; P value for sex × age interaction = .036). The prevalence of extreme obesity varied in ethnic/racial and age groups, with the highest prevalence in Hispanic boys (as high as 11.2%) and African-American girls (as high as 11.9%).
Conclusion
Extreme obesity in Southern California youth is frequently observed at relatively young ages. The shift toward extreme body weights is likely to cause an enormous burden of adverse health outcomes once these children and adolescents grow older.
The American Medical Association and the Centers for Disease Control and Prevention (CDC) recommendations on prevention, assessment, and treatment of childhood obesity are based on relatively limited knowledge about extreme childhood obesity at the population level1. Data from National Health and Nutrition Examination Survey 1999 to 2004 suggest that extreme obesity, defined as a body mass index (BMI) ≥99th percentile, is prevalent in 3.8% of children and adolescents aged 2 to 19 years, with the highest prevalence in African-American girls and Hispanic boys.2,3 Newer data on recent trends are not available. The present economic burden and health consequences are largely unknown and ill defined.
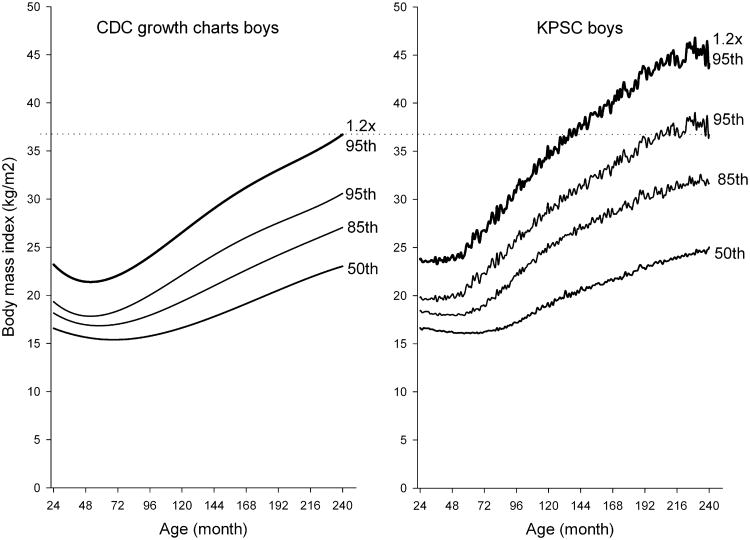
The assessment of extreme obesity in children is complicated by the lack of a standard definition. Because the 2000 CDC growth charts lack the precision necessary to calculate percentiles <3rd and >97th,4 multiples of other percentiles corresponding to adulthood obesity classes at 18 years of age can be used to define extreme obesity in children. Adulthood obesity class 2 (BMI ≥35 kg/m2) corresponds approximately to 1.2 times the 95th percentile of BMI-for-age after 18 years of age. Therefore, the new definition of extreme childhood obesity proposed by the CDC is a BMI-for-age ≥1.2 times the 95th percentile or a BMI ≥35 kg/m2.5
To provide current insight into the prevalence of extreme obesity, we performed a cross-sectional study in >710 000 children and adolescents in Southern California who were actively enrolled in a large pre-paid integrated managed health care system in 2007 and 2008. By taking advantage of the large and diverse population and the resultant precision, we sought to describe the empirical distributions of BMI-for-age and estimates of the prevalence of extreme pediatric obesity.
Methods
Between Jan 1, 2007, and Dec 31, 2008, Kaiser Permanente Southern California (KPSC) provided health care service to >3.2 million patients, including 816 204 children aged 2 to 19 years. Members received their care in medical offices and hospitals owned by KPSC throughout the 7-county region. After exclusion of pregnant members (n = 6475), 809 729 patients were eligible for participation in this cross-sectional study. Of these patients, 710 949 patients (87.8% of eligible patients) had made at least one medical office visit in the 2-year study period and were included in the final cohort. The study protocol was reviewed and approved by the institutional review board of KPSC before implementation.
Body weight and height is routinely measured during medical office visits. For the final study cohort of 710 949 patients, we extracted data on weight and height from electronic medical charts that detailed 1 849 256 inpatient and outpatient encounters. Biologically implausible values for weight and height data were excluded (data from 39 648 encounters). The procedures are described in detail elsewhere.6 A validation study including a random subsample of 15 000 patients with 45 980 medical encounters indicated an error rate <0.6% after deleting implausible weight and height values.
After deleting implausible weight and height values, the average number of medical encounters was 2.6 ± 0.1 per child per year. For the most recent available year (2007 or 2008), the median BMI and median BMI-for-age percentile of all encounters for a patient were calculated and used for this analysis. When only 1 height and weight were available, BMI and median BMI-for-age percentile was calculated and included in the study.
Race and ethnicity information was obtained from administrative records and birth certificate information. For unknown race and ethnicity information (52.5%), administrative records were supplemented by an imputation algorithm on the basis of surname lists and address information derived from the US Census Bureau.7-9 The optimal probability cutoff points were chosen on the basis of receiver operating curve analysis in patients with known race ethnicity when the specificity rate was >98%. Asian/Pacific Islander race was assigned when the probability cutoff point for surname was >50% for Asian/Pacific Islander race. Hispanic ethnicity was assigned when the probability cutoff point for surname was >50% for Hispanic ethnicity. For African-American subjects and non-Hispanic Caucasian subjects, members' addresses were geocoded to the US Census block level. Race and ethnicity were assigned on the basis of the composition of the block, applying a probability cutoff point >75% for African-American race and >45% for Caucasian race. Race/ethnicity was assigned in the specified order for Asian/Pacific Islander, Hispanic, African-Amerian, and Caucasian when no other assignment could be made before. In patients with known race/ethnicity, the specificity and positive predictive values of this hierarchical algorithm were >98% for all races/ethnicities. We categorized race/ethnicity as non-Hispanic Caucasian, Hispanic Caucasian, African-American (regardless of ethnicity), Asian or Pacific Islander, other or multiple race/ethnicity, and unknown because of missing information. The distribution of the population remained essentially unaltered after race imputation.
The distributions of age, sex, and race/ethnicity of KPSC members aged 2 through 19 years were compared with the California Census population from 2000 (accessed on Oct 29, 2008 at http://wonder.cdc.gov/population.html).
Sex-specific BMI-for-age growth charts developed by the CDC were used to define overweight and obesity for children and adolescents.4 Overweight was defined as BMI-for-age ≥85th percentile or a BMI ≥25 kg/m2, obesity as ≥95th percentile or a BMI ≥30 kg/m2, and extreme obesity ≥1.2 times the 95th percentile or a BMI ≥35 kg/m2.4,5,10 Adolescents aged 12 to 19 years who were classified as having extreme obesity (≥1.2 × 95th percentile or a BMI ≥35 kg/m2) were further subdivided into obesity class 2 (BMI 35.0-39.9 kg/m2), obesity class 3 (BMI 40.0-49.9 kg/m2), and obesity class 4 (BMI ≥50 kg/m2).11 Each child was assigned to a specific age group (2-5, 6-11, or 12-19 years) according to the child's mid-year age. The empiric percentiles of BMI (50, 85, 95, and 1.2 × 95) were summarized by age (months) and plotted for boys and girls. Each data point (month of age) consisted of an average of 1602 for boys and 1586 for girls.
Differences in the distribution of extreme obesity across sex and race/ethnicity specific-categories were assessed with the χ2 test. Multiple logistic regression models were generated to estimate the association between extreme obesity and sex, age and race/ethnicity simultaneously, and the interactions between these characteristics. The associations are expressed as odds ratios and their corresponding 95% CIs. All analyses were conducted with SAS software version 9.1 (SAS Institute, Cary, North Carolina).
Results
The study sample comprised 357 205 boys and 353 744 girls, approximately half of whom were Hispanic Caucasian (Table I). Children and adolescents enrolled in the KPSC health plan represent approximately 12.3% of the population in the counties of Southern California served by KPSC. Compared with the Southern California population, KPSC patients were similar in their sex distribution, but slightly older than the underlying population. Ethnic/racial distribution differed slightly, with more Hispanic and fewer non-Hispanic Caucasian members in the health plan than in the California population of the same age.
Table I. Characteristics of patients aged 2 through 19 years in Southern California compared with Southern California Census* data.
| Variable | Patients | Southern Calfornia Census | ||
|---|---|---|---|---|
|
|
|
|||
| Boys | Girls | Boys | Girls | |
| n (% of total population) | 357 205 (50.2) | 353 744 (49.8) | 2 973 090 (51.3) | 2 822 021 (48.7) |
| Age group, % | ||||
| 2-5 years | 24.6 | 23.4 | 22.4 | 22.2 |
| 6-11 years | 29.9 | 28.4 | 35.4 | 35.6 |
| 12-19 years | 45.5 | 48.2 | 42.2 | 41.8 |
| Race/ethnicity†,‡,% | ||||
| Non-Hispanic Caucasian | 28.5 | 28.6 | 32.8 | 32.7 |
| Hispanic Caucasian | 50.5 | 51.1 | 47.1 | 47.0 |
| African-American | 8.8 | 8.7 | 8.9 | 9.0 |
| Asian or Pacific Islander | 8.1 | 7.7 | 9.6 | 9.6 |
| Other§ | 4.1 | 3.9 | 1.6 | 1.6 |
On the basis of 2000 California Census data of the counties covered by Kaiser Permanente Southern California (Kern, Los Angeles, Orange, Riverside, San Bernardino, San Diego, San Louis Obispo, Santa Barbara, Tulare, Ventura).
In patients with known race/ethnicity. Race/ethnicity was missing in 52.5% of patients before imputation and in 12.4% of patients after imputation.
Southern California Census information is based on bridged-race estimates.
Other race for KPSC also comprises patients of multiple race.
The empirical percentiles of BMI-for-age of KPSC boys and girls (Figures 1 and 2; available at www.jpeds.com) assessed in 2007/2008 are higher than in the 2000 CDC growth charts, with larger differences at higher percentiles and small differences at and below the median.
Figure 1.
Comparison of the percentiles of BMI for boys from CDC growth charts with empiric percentiles of Southern California patients aged 2 to 19 years.
Figure 2.
Comparison of the percentiles of BMI for girls from 2000 CDC growth charts empiric percentiles of Southern California patients aged 2 to 19 years.
Overall, the prevalence of overweight, obesity, and extreme obesity were 37.1%, 19.4%, and 6.4% of patients, respectively (Table II). The highest prevalence was observed in Hispanic Caucasian patients, followed by African-Amerian patients, and other or multiple races/ethnicities. The prevalence was higher in boys than in girls and lowest in 2- to 5-year-old patients. In boys, the prevalence of overweight, obesity, and extreme obesity was highest in Hispanic Caucasian patients. In girls, the prevalence of overweight and obesity was similarly high for Hispanic Caucasian and African-American patients, and extreme obesity was highest in African-American girls.
Table II. Prevalence of overweight, obesity, and extreme obesity in 710 949 patients aged 2 through 19 years in Southern California*.
| Total n | Weight class | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Overweight | Obese | Extremely obese | |||||
|
|
|
|
|||||
| ≥85th percentile of the CDC Growth Charts or ≥25 kg/m2 | ≥95th percentile of the CDC Growth Charts or ≥30 kg/m2 | ≥1.2 × 95th percentile of the CDC Growth Charts or ≥35 kg/m2 | |||||
|
|
|
|
|||||
| n† | % | n† | % | n | % | ||
| All | 710 949 | 263 902 | 37.1 | 138 026 | 19.4 | 45 394 | 6.4 |
| Sex | |||||||
| Boys | 357 205 | 139 459 | 39.0 | 77 365 | 21.7 | 25 922 | 7.3 |
| Girls | 353 744 | 124 443 | 35.2 | 60 661 | 17.2 | 19 472 | 5.5 |
| Age, years | |||||||
| 2-5 | 170 453 | 46 126 | 27.1 | 22 358 | 13.1 | 4216 | 2.5 |
| 6-11 | 207 284 | 84 506 | 40.8 | 47 638 | 23.0 | 15 398 | 7.4 |
| 2-19 | 333 212 | 133 270 | 40.0 | 68 030 | 20.4 | 25 780 | 7.7 |
| Race/ethnicity | |||||||
| Non-Hispanic Caucasian | 177 862 | 51 806 | 29.1 | 23 021 | 12.9 | 6725 | 3.8 |
| Hispanic Caucasian | 316 394 | 135 611 | 42.9 | 74 372 | 23.5 | 25 126 | 7.9 |
| African-American | 54 491 | 21 207 | 38.9 | 11 249 | 20.6 | 4476 | 8.2 |
| Asian or Pacific Islander | 49 229 | 13 262 | 26.9 | 6142 | 12.5 | 1676 | 3.4 |
| Other | 24 772 | 9489 | 38.3 | 5364 | 21.6 | 1689 | 6.8 |
| Unknown | 88 201 | 32 527 | 36.9 | 16 442 | 18.6 | 5702 | 6.5 |
| Boys | |||||||
| Age, years | |||||||
| 2-5 | 87 839 | 24 491 | 27.9 | 12 324 | 14.0 | 2334 | 2.7 |
| 6-11 | 106 744 | 46 110 | 43.2 | 27 299 | 25.6 | 9392 | 8.8 |
| 12-19 | 162 622 | 68 858 | 42.3 | 37 742 | 23.2 | 14 196 | 8.7 |
| Race/ethnicity | |||||||
| Non-Hispanic Caucasian | 89 648 | 27 555 | 30.7 | 13 269 | 14.8 | 3793 | 4.2 |
| Hispanic Caucasian | 158 533 | 71 938 | 45.4 | 42 423 | 26.8 | 14 887 | 9.4 |
| African-American | 27 553 | 10 227 | 37.1 | 5440 | 19.7 | 2025 | 7.3 |
| Asian or Pacific Islander | 25 372 | 7979 | 31.4 | 4072 | 16.0 | 1152 | 4.5 |
| Other | 12 830 | 5217 | 40.7 | 3076 | 24.0 | 1018 | 7.9 |
| Unknown | 43 269 | 16 543 | 38.2 | 8960 | 20.7 | 3047 | 7.0 |
| Girls | |||||||
| Age, years | |||||||
| 2-5 | 82 614 | 24 491 | 27.9 | 10 034 | 12.2 | 1882 | 2.3 |
| 6-11 | 100 540 | 46 110 | 43.2 | 20 339 | 20.2 | 6006 | 6.0 |
| 12-19 | 170 590 | 68 858 | 42.3 | 30 288 | 17.8 | 11 584 | 6.8 |
| Race/ethnicity | |||||||
| Non-Hispanic Caucasian | 88 214 | 24 251 | 27.5 | 9752 | 11.1 | 2932 | 3.3 |
| Hispanic Caucasian | 157 861 | 63 673 | 40.3 | 31 949 | 20.2 | 10 239 | 6.5 |
| African-American | 26 938 | 10 980 | 40.8 | 5809 | 21.6 | 2451 | 9.1 |
| Asian or Pacific Islander | 23 857 | 5283 | 22.1 | 2070 | 8.7 | 524 | 2.2 |
| Other | 11 942 | 4272 | 35.8 | 2276 | 19.1 | 671 | 5.6 |
| Unknown | 44 932 | 15 984 | 35.6 | 7482 | 16.7 | 2655 | 5.9 |
Pregnant girls were excluded.
Column numbers include numbers of columns to the right.
In boys and girls, extreme obesity was observed early in life (Figure 3). In boys, the prevalence of extreme obesity was greater in increasingly older age groups until approximately 10 years of age. In girls, the distribution of extreme obesity over age was bimodal, with peaks at 12 and 18 years of age. The prevalence of extreme obesity in boys and girls was similar after 18 years of age. This interaction between sex and age remained significant after adjustment for race/ethnicity (P = .036).
Figure 3.
Percentage of extremely obese boys and girls according to age. In boys, extreme obesity develops at an earlier age than in girls, but girls catch up later, with a similar prevalence at age 18 to 19 years (P for sex × age interaction = .036).
The odds of extreme obesity for races/ethnicities differed by age group (P for interaction <.001 for both sexes; Table III). Relatively consistent in almost all age groups, the odds of extreme obesity were highest for Hispanic Caucasian patients, African-American patients, and patients os other races. For boys, the highest prevalence of extreme obesity was observed in 6- to 11-year-old and 12- to 19-year-old Hispanic Caucasian patients and patients of other races/ethnicities. For girls, the highest prevalence of extreme obesity was observed in African-American girls aged 12 to 19 years. The lowest prevalence of extreme obesity was generally found in non-Hispanic and in Asian/Pacific Islander girls.
Table III. Odds of extreme obesity* in 710 949 patients aged 2 to 19 years in Southern California by sex, race/ethnicity, and age group.
| Boys | Girls | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| n | % | OR (95% CI) | n | % | OR (95% CI) | |
| Races/ethnicities by age | ||||||
| 2-5 years | ||||||
| Non-Hispanic Caucasian | 260 | 1.3 | 1.00 (reference) | 146 | 1.1 | 1.00 (reference) |
| Hispanic Caucasian | 1388 | 3.6 | 2.96 (2.59-3.38) | 522 | 2.8 | 2.96 (2.55-3.44) |
| African-American | 132 | 2.1 | 1.68 (1.36-2.08) | 147 | 2.6 | 2.46 (1.99-3.05) |
| Asian or Pacific Islander | 131 | 1.8 | 1.42 (1.45-1.75) | 60 | 1.1 | 1.01 (0.77-1.32) |
| Other | 186 | 3.6 | 2.97 (2.46-3.60) | 128 | 2.6 | 2.49 (2.00-3.12) |
| Unknown | 237 | 2.4 | 1.93 (1.62-2.31) | 879 | 2.5 | 1.96 (1.61-2.39) |
| 6-11 years | ||||||
| Non-Hispanic Caucasian | 1141 | 4.8 | 1.00 (reference) | 465 | 3.4 | 1.00 (reference) |
| Hispanic Caucasian | 5576 | 11.2 | 2.52 (2.36-2.69) | 1376 | 7.6 | 2.31 (2.13-2.51) |
| African-American | 699 | 8.6 | 1.87 (1.69-2.06) | 666 | 9.5 | 3.13 (2.81-3.48) |
| Asian or Pacific Islander | 436 | 5.8 | 1.23 (1.10-1.38) | 119 | 2.5 | 0.72 (0.60-0.85) |
| Other | 506 | 10.6 | 2.37 (2.12-2.64) | 291 | 6.7 | 2.15 (1.87-2.47) |
| Unknown | 1034 | 8.2 | 1.79 (1.64-1.95) | 3089 | 5.9 | 1.99 (1.79-2.21) |
| 12-19 years | ||||||
| Non-Hispanic Caucasian | 2392 | 5.3 | 1.00 (reference) | 1242 | 4.9 | 1.00 (reference) |
| Hispanic Caucasian | 7923 | 11.3 | 2.26 (2.16-2.37) | 1646 | 8.2 | 1.87 (1.77-1.96) |
| African-American | 1194 | 9.1 | 1.79 (1.67-1.92) | 1550 | 11.9 | 2.95 (2.76-3.16) |
| Asian or Pacific Islander | 585 | 5.6 | 1.05 (0.96-1.56) | 217 | 3.4 | 0.66 (0.58-0.74) |
| Other | 326 | 11.1 | 2.22 (1.97-2.51) | 252 | 9.4 | 2.30 (2.00-2.64) |
| Unknown | 1776 | 8.6 | 1.66 (1.56-1.77) | 6677 | 6.5 | 1.75 (1.64-1.87) |
OR, Odds ratio.
Extreme obesity is defined as BMI ≥1.2 × 95th percentile of the CDC growth charts or ≥35 kg/m2.
A wide range of BMI was observed, with some patients qualifying for adulthood obesity class 3 (BMI 40.0-49.9 kg/m2) and class 4 (BMI ≥50 kg/m2). The overall prevalence of obesity class 3 and class 4 in 12- to 19-year-old patients was 1.8% and 0.2%, respectively. African-American patients had the highest prevalence of obesity class 3 and class 4 (3.0% and 0.5 %, respectively), and Asian/Pacific Islanders had the lowest prevalence of obesity class 3 and 4 (0.8% and 0.1%, respectively; P for race difference <.001).
Estimates on the basis of patients with known race/ethnicity remained largely unaltered, but with wider confidence intervals because of a significantly reduced sample size in some subgroups.
Discussion
This Southern California population-based cross-sectional study provides valuable information on the extent of extreme childhood obesity on the basis of 2007 to 2008 estimates. The extremely large sample size affords a much more precise estimate than has been possible in other settings.2,12 These data suggest that >6% of boys and girls can be classified as extremely obese, translating to an estimated 560 000 children and adolescents in California. Extreme obesity occurs already at a young age, especially in boys, indicating that extreme childhood obesity is a serious issue for pediatric care. Moreover, it appears that some ethnic/racial minorities are particularly affected, showing both a high rate of extreme obesity and a shift in the body weight distribution toward extreme body weights qualifying for adult obesity class 3 or higher.
Childhood obesity is related to an increased risk for a number of adverse health conditions that can occur in childhood or later in adulthood.13-23 Analogous to the concept of “pack-years” for smoking patients, extremely obese children may suffer cumulative effects of their “pound-years.”24 Thus, a better understanding of the health consequences of extreme obesity is an important public health issue.
Only 2 studies12,13 have addressed potential additional health consequences of extreme obesity compared with moderate obesity in children. Data from the Bogalusa Heart Study suggest that the number of cardiovascular risk factors increases with increasing degree of obesity in children aged 5 to 17 years. In that study, 59% of children at or above the 99th percentile of BMI-for-age had at least 2 cardiovascular risk factors, compared with 39% of children at or above the 95th percentile.12 Another study categorized children and adolescents as moderately obese (BMI z-score of 2.0-2.5, corresponding to the 97th-99.5th percentile of BMI-for-age) and extremely obese (BMI z-score >2.5, corresponding to the 99.5th percentile).13 Higher severity of obesity was associated with higher prevalence of components of the metabolic syndrome, and some race groups were more affected than others. The prevalence of the metabolic syndrome was approximately 30% in moderately obese children and approximately 50% in extremely obese children; symptoms worsened in a relatively short follow-up time.13 The overall public health impact and the magnitude of potential adverse health risks associated with extreme childhood obesity cannot be estimated from those studies12,13 and are largely unknown. Considering these potential health consequences as shown by the studies aforementioned and the relatively high numbers of patients with extreme obesity with marked variance across racial and ethnic groups as shown in our study, robust and validated risk stratification schemes are needed to address the variability in risks for adverse health outcomes.
The prevalence of obesity in children is high. Nationwide, 17.1% of boys and 15.5% of girls aged 2 to 19 years are obese as defined by using a BMI-for-age ≥95th percentile.25 On the basis of National Health and Nutrition Examination Survey data from 1999 to 2004, an estimated 3.8% of children and adolescents have BMI-for-age ≥99th percentile.26 Results from our study on the basis of 2007 to 2008 data suggest that we also face a shift toward extreme obesity. Some segments of the population were more affected than others, with a prevalence approaching 12% for specific groups. The slight differences in the definition of extreme obesity used for these studies (99th percentile versus 1.2 × 95th percentile) cannot account for this difference. The shift toward extreme body weight compared with national reference data from CDC growths charts as shown in our study is unlikely to be explained by a difference in time alone. This large population-based study in Southern California differs significantly in its racial and ethnic distribution from national studies and includes larger numbers of minority children with a high prevalence of extreme obesity. However, the 50th percentile of BMI-for-age is strikingly similar between our population and national reference data, whereas the differences between BMI-for-age percentiles get more pronounced at the growing tail of extreme body weights. This indicates that our study does not reflect a right shift of an entire population, but a right shift of obesity toward extreme obesity.
Boys were more affected by extreme obesity than girls in our study, in whom a high prevalence of extreme obesity was observed throughout childhood. In contrast, girls showed a second peak at 18 years, resulting in similar prevalence of extreme obesity for boys and girls at the beginning of adulthood, but potentially longer exposure to extreme obesity for boys. These findings have to be interpreted with caution because they are based on cross-sectional data. The results of our study also suggest that the higher prevalence of extreme obesity in boys was relatively consistent for almost all subgroups defined by age and race/ethnicity. This finding is in agreement with other reports suggesting a higher prevalence of obesity-related health conditions such as the metabolic syndrome in boys than in girls27 and supports the theory of cumulative effects of “pound-years.”
Ethnic/racial minorities were not evenly affected by extreme obesity. In our study, the prevalence of extreme obesity was highest in Hispanic Caucasian and African-American patients, and the lowest prevalence was found in Asian/Pacific Islander and non-Hispanic Caucasian patients. However, the heaviest patients were found in the African-American Black adolescent group, with >3.5% classified as adulthood obesity class 3 or higher (BMI ≥40 kg/m2). These high rates of adult obesity class 3 and higher among African-American adolescents are alarming.
Race and ethnicity are subject to potential misclassification because of imputation of missing race/ethnicity information for more than half of the study population. However, results did not differ when only children with known race/ethnicity information from administrative records were analyzed. Moreover, prevalence estimates from children with missing race/ethnicity information were comparable with the total prevalence in almost all subgroups, suggesting that the racial/ethnic distribution of children with missing race/ethnicity was comparable with children whose race/ethnicity was known.
This study benefits from measured weight and height from medical office visits as opposed to self-reported weight and height. All children were members of a large pre-paid managed care system, and standardized screening guidelines for weight and height in all children in the health plan were routine. However, no general calibration protocol for scales has been followed, data are manually entered into a computer system, and inaccurate measurements may occur because of seasonal differences in clothing or measurements taken with shoes. Although this issue has been partially addressed by a BMI based on an average of 2.6 encounters per child, the large sample size, and careful cleaning of implausible weight and height data, potential misclassifications cannot entirely be ruled out and may limit interpretability.
Acknowledgments
This research was supported by Kaiser Permanente Direct Community Benefit Funds.
Glossary
- BMI
Body mass index
- CDC
Centers for Disease Control and Prevention
- KPSC
Kaiser Permanente Southern California
Footnotes
The authors declare no conflicts of interest.
References
- 1.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120:S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 2.Freedman DS, Khan LK, Serdula MK, Ogden CL, Dietz WH. Racial and ethnic differences in secular trends for childhood BMI, weight, and height. Obesity (Silver Spring) 2006;14:301–8. doi: 10.1038/oby.2006.39. [DOI] [PubMed] [Google Scholar]
- 3.Skelton JA, Cook SR, Auinger P, Klein JD, Barlow SE. Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr. 2009;9:322–9. doi: 10.1016/j.acap.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002;11:1–190. [PubMed] [Google Scholar]
- 5.Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR. Characterizing extreme values of body mass index for age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr. 2009;90:1314–20. doi: 10.3945/ajcn.2009.28335. [DOI] [PubMed] [Google Scholar]
- 6.Smith N, Coleman KJ, Lawrence JM, Quinn VP, Getahun D, Reynolds K, et al. Body weight and height data in electronic medical records of children. Int J Pediatr Obes. 2009 doi: 10.3109/17477160903268308. In press. [DOI] [PubMed] [Google Scholar]
- 7.Bureau of the Census. Census 2000 surname list. [Accessed 11, 2009]; Available at http://www.census.gov/genealogy/www/freqnames2k.html.
- 8.Fiscella K, Holt K, Meldrum S, Franks P. Disparities in preventive procedures: comparisons of self-report and Medicare claims data. BMC Health Serv Res. 2006;6:122. doi: 10.1186/1472-6963-6-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Word DL, Perkins RC. Technical Working paper no 13. Washington, DC: US Bureau of the Census; 1996. Building a Spanish surname list for the 1990s—a new approach to an old problem. [Google Scholar]
- 10.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Technical Report Series 894: obesity: preventing and managing the global epidemic. Gemeva: World Health Organization; 2000. [PubMed] [Google Scholar]
- 12.Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150:12–7. doi: 10.1016/j.jpeds.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 13.Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350:2362–74. doi: 10.1056/NEJMoa031049. [DOI] [PubMed] [Google Scholar]
- 14.Rocchini AP. Childhood obesity and a diabetes epidemic. N Engl J Med. 2002;346:854–5. doi: 10.1056/NEJM200203143461112. [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez MA, Winkleby MA, Ahn D, Sundquist J, Kraemer HC. Identification of population subgroups of children and adolescents with high asthma prevalence: findings from the Third National Health and Nutrition Examination Survey. Arch Pediatr Adolesc Med. 2002;156:269–75. doi: 10.1001/archpedi.156.3.269. [DOI] [PubMed] [Google Scholar]
- 16.Angulo P. Obesity and nonalcoholic fatty liver disease. Nutr Rev. 2007;65:S57–63. doi: 10.1111/j.1753-4887.2007.tb00329.x. [DOI] [PubMed] [Google Scholar]
- 17.Dunn W, Schwimmer JB. The obesity epidemic and nonalcoholic fatty liver disease in children. Curr Gastroenterol Rep. 2008;10:67–72. doi: 10.1007/s11894-008-0011-1. [DOI] [PubMed] [Google Scholar]
- 18.Coviello AD, Legro RS, Dunaif A. Adolescent girls with polycystic ovary syndrome have an increased risk of the metabolic syndrome associated with increasing androgen levels independent of obesity and insulin resistance. J Clin Endocrinol Metab. 2006;91:492–7. doi: 10.1210/jc.2005-1666. [DOI] [PubMed] [Google Scholar]
- 19.Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, Stewart L, et al. Health consequences of obesity. Arch Dis Child. 2003;88:748–52. doi: 10.1136/adc.88.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Visser M. Higher levels of inflammation in obese children. Nutrition. 2001;17:480–1. doi: 10.1016/s0899-9007(01)00509-3. [DOI] [PubMed] [Google Scholar]
- 21.Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB. Low-grade systemic inflammation in overweight children. Pediatrics. 2001;107:E13. doi: 10.1542/peds.107.1.e13. [DOI] [PubMed] [Google Scholar]
- 22.Wills M. Orthopedic complications of childhood obesity. Pediatr Phys Ther. 2004;16:230–5. doi: 10.1097/01.PEP.0000145911.83738.C6. [DOI] [PubMed] [Google Scholar]
- 23.Tauman R, Gozal D. Obesity and obstructive sleep apnea in children. Paediatr Respir Rev. 2006;7:247–59. doi: 10.1016/j.prrv.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 24.Xanthakos SA, Inge TH. Extreme pediatric obesity: weighing the health dangers. J Pediatr. 2007;150:3–5. doi: 10.1016/j.jpeds.2006.11.040. [DOI] [PubMed] [Google Scholar]
- 25.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003-2006. JAMA. 2008;299:2401–5. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 26.Skelton JA, Cook SR, Auinger P, Klein JD, Barlow SE. Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr. 2009;9:322–9. doi: 10.1016/j.acap.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2003;157:821–7. doi: 10.1001/archpedi.157.8.821. [DOI] [PubMed] [Google Scholar]