Abstract
Disruptive behavior disorders (DBDs) are chronic, impairing, and costly behavioral health conditions that are four times more prevalent among children of color living in impoverished communities as compared to the general population. This disparity is largely due to the increased exposure to stressors related to low socioeconomic status including community violence, unstable housing, under supported schools, substance abuse, and limited support systems. However, despite high rates and greater need, there is a considerably lower rate of mental health service utilization among these youth. Accordingly, the current study aims to describe a unique model of integrated health care for ethnically diverse youth living in a New York City borough. With an emphasis on addressing possible barriers to implementation, integrated models for children have the potential to prevent ongoing mental health problems through early detection and intervention.
Keywords: Child mental health, early detection and treatment, integrated care pathway
Introduction
Children of color who live in urban, poverty-impacted communities are at high risk for mental health problems due in large part to their exposure to stressors related to low socioeconomic status such as community violence, unstable housing, under supported schools, substance abuse, and limited support systems (McKay, Hibbert, Hoagwood, Rodriguez, & Murray, 2004; Tolan & Henry, 1996). As a case in point, disruptive behavior disorders (DBDs), which are chronic, impairing, and costly behavioral health conditions (Foster & Jones, 2005; Loeber, Green, Lahey, Frick, & McBurnett, 2000; Washburn et al., 2008), are up to four times more prevalent among children of color living in impoverished communities than rates within the general population (Cauce et al., 2002; Dubay & Lebrun, 2012; Tolan, Gorman-Smith, & Loeber, 2000).
Despite a greater need, there is a considerable disparity in the utilization of mental health services among these youth (Freedenthal, 2007; Garland et al., 2005; Lopez, 2002; Miller, Southam-Gerow, & Allin, 2008; Zimmerman, 2005). Specifically, up to 80% of children and adolescents in need of treatment who reside in poverty-impacted, urban communities never access the mental health system, while among those who attend an appointment, 50% end up dropping out of treatment prematurely (U.S. Public Health Service, 1999, 2000a, 2000b, 2001).
Families are impeded from accessing mental health services due to logistical barriers (e.g., transportation, financial, and childcare difficulties), and often more potent perceptual obstacles such as negative perceptions about mental health and treatment, mistrust of the mental health system, and stigma (Garcia & Weisz, 2002; Gopalan, Goldstein, Klingenstein, Sicher, & McKay, 2010; Kazdin, Holland, & Crowley, 1997; MacNaughton & Rodrigue., 2001; McKay & Bannon, 2004; Nock & Kazdin, 2001). One study, for example, found that parents were six times less likely to see the utility of mental health treatment and overcome structural and contextual barriers to care when having a past experience of feeling disrespected by their child’s mental health provider (Kerkorian et al., 2006). Perceptual obstacles such as mistrust toward the mental health system and concerns regarding stigma, which are thought to be more potent among persons of color, also play a significant role in perception of mental health, providers, and treatment, and has been implicated in service underuse (Alegria et al., 2010; Godoy & Carter, 2013).
Over a decade ago, the Surgeon General’s National Action Agenda for Children’s Mental Health proposed integrating the primary and behavioral health care systems in order to enhance access and utilization of treatment for children in need (U.S. Public Health Service, 2001a). This call was in response to a persistent problem in children’s mental health services; service silos, administratively separate agencies serving the population of children with mental health needs and their families. Numerous reports over at least three decades have underscored the segmentation of the system responsible for serving children and families (Garland et al., 2000; Garland, Landsverk, Hough, & Ellis-MacLeod, 1996; Institute of Medicine, 2001; Stroul & Friedman, 1994).
The asymmetry created by separate service systems (i.e., pediatric and mental health clinics) responsible for providing care to children with mental health needs creates difficult challenges for caregivers seeking services for their children. This includes lengthy waitlists delaying service initiation (Koppelman, 2004; McKay & Bannon, 2004), poorly coordinated care (Heflinger, 1996; Saxe, Cross, & Silverman, 1988), a poorly trained workforce providing ineffective services (Huang, Macbeth, Dodge, & Jacobstein, 2004; Weissman et al., 2006), piecemeal service plans (Vernberg, Roberts, & Nyre, 2002), and other significant barriers to access and continuity (Kataoka, Zhang, & Wells, 2002).
Integrated care is the systematic coordination of primary and behavioral health care used to produce the best possible outcomes for patients with both general health and behavioral health needs (SAMHSA-HRSA Center for Integrated Health Solutions, 2013). Integrated care has been purported to address these obstacles to treatment access by providing a unified service delivery system, which in turn reduces fragmentation and enhances interdisciplinary collaboration. Additionally, integrated care is believed to enhance the quality of services by having a mental health professional on site in pediatric clinics, which can provide staff the time and the access to each other to consult on the immediate needs of patients, thereby allowing for appropriate referrals and treatment (Brunelle & Porter, 2013). Families may feel less stigmatized accessing care by offering mental health services at a primary medical location as opposed to a secondary location distinctly providing specialized mental health treatment.
SAMHSA-HRSA Center for Integrated Health Solutions (2013) describes three models of integrated care for children with varying levels of integration: (1) a facilitated referral model, in which a referral will be provided if screening uncovers a potential mental health problem, (2) a co-located model, in which health and mental health providers are housed in the same facility but work separately and consult about shared clients, and (3) an in-house model, in which both mental health services are integrated within the primary care setting and part of the clinic’s workflow. They also note five core competencies associated with integrated care models for children with behavioral health problems. The competencies, which are based on the chronic care model (National Initiative for Children’s Healthcare Quality, 2011; Wagner et al., 2001) and a system-of-care approach for involving community services and supports for children with mental health problems (Pires, 2002; Stroul, Blau, & Friedman, 2010), include the following: (1) developing a child and family-driven team in which family members have input, (2) creating an individualized care plan for the child, (3) using screening and assessment measures that are evidence-based, (4) forging relationships with other child-serving systems, and (5) having data systems that serve a platform for planning and decision making activities (The SAMHSA-HRSA Center for Integrated Health Solutions, 2013). While the model of focus in the current paper shares elements of all three SAMHSA-HRSA models presented above, it was developed to fit the needs of service systems using a bottom up approach that will be explained further below.
There is a growing effort to integrate mental health detection and/or treatment in primary care settings (Godoy & Carter, 2013). Although numerous positive outcomes are associated with these interventions, such as increased likelihood to access and complete treatment, improved child outcomes, increased consumer satisfaction, and improved provider practices (Kolko et al., 2014), there are significant barriers to implementation. Some physicians report not having enough time to screen (Sand et al., 2005) and express concerns that they lack the knowledge and training to adequately treat mental health problems (Williams, Klinepeter, Palmes, Pulley, & Foy, 2004). However, these issues can be overcome if addressed through education, additional manpower, and other supports (Godoy & Carter, 2013).
The purpose of this article is to describe a unique model of integrated health care for ethnically diverse children living in a New York City borough, with an emphasis on addressing potential barriers to implementation. Considering that approximately 50% of pediatric office visits involve behavioral issues and nearly 75% of children exhibiting psychiatric symptoms are initially seen by a pediatrician (Martini et al., 2012), integrated models for children have the potential to prevent ongoing mental health problems through early detection and intervention. A subsequent paper, which is in preparation, will examine outcomes associated with this innovative model.
Integrated health care project
Project description
In 2014, the Institute for Family Health, an established New York City–based federally qualified health center network that provides primary care and mental health services, was the recipient of a one-year catalyst grant from a private foundation to create an integrated health care service delivery system for children between 5 and 18 years of age at high risk for mental health problems who were living in the Bronx, a diverse borough composed primarily of residents of color of low socioeconomic status. According to the U.S. Census Bureau (2015), 43.3% of Bronx residents identified as African-American, and 54.6% identified as Hispanic and Latino in 2013; in contrast, 17.5% and 18.4% of residents across New York identified as African-American or Latino, respectively. Between 2009 and 2013, the median household income for Bronx residents was $34,388, and 29.8% of residents lived below the poverty level; in comparison, the median income across New York State was $58,003, and the poverty rate 15.3% (U.S. Census Bureau, 2015).
The grant’s aims were to reach projected benchmarks (e.g., provide routine screening for behavioral health problems in the primary care workflow), and augment supports in the primary care setting to facilitate the integrated model through the provision of trainings on topics including evidence-based engagement strategies and treatments for children and adolescents.
Five performance metrics were outlined in the grant proposal: (1) to screen 3,000 children receiving primary care for a mental health condition, (2) to conduct at least one documented case conference or behavioral health consultation every 3 months for youth who screened positive for the mental health condition, (3) to demonstrate at least 30% of youth who received care coordination (children who received a case conference) improved after 6 months via a condition-specific standardized measure, (4) to report the percentage of children treated for a mental health condition at specialty care clinics, and (5) to demonstrate that at least 30% of children referred to specialty care clinics for a behavioral health condition improved after 6 months as determined by a condition-specific standardized measure
Collaborative partners
Primary care
BronxCare Pediatrics Practice at Concourse (BronxCare) is embedded within Bronx-Lebanon Hospital Center, the largest hospital serving the South and Central Bronx (http://www.bronxcare.org/our-services/pediatrics/). In 2014, BronxCare provided more than 44,000 visits for 14,000 children and adolescents, and was the health care home for more than 18,000 youth insured by Medicaid, Medicare, or other safety net insurance (http://www.bronxcare.org/our-services/pediatrics/). Typically, families seen at the Practice experience a range of psychosocial and environmental stressors, including poverty, child welfare involvement, community violence, and parental mental illness.
Behavioral health provider
The IFH is one of the largest primary health care organizations in New York State, serving over 94,000 patients yearly. IFH has 26 centers, seven of which are licensed mental health centers and the remaining are primary care sites with on-site mental health services. Five of the centers are located in the Bronx (both primary care and mental health clinics) and IFH services are available to all patients, regardless of insurance status or ability to pay. IFH also operates two free clinics, one of which is located in the Bronx, that offers free health and behavioral health care services for persons in need (http://www.institute.org/health-care/services/free-clinics-for-the-uninsured).
Procedure
Over the course of 9 months, the collaborative partners in conjunction with academic researchers, who served as the evaluation team, convened to meet the objectives of the grant project. These meetings occurred bimonthly for 8 months and focused on developing the integrated care pathway, addressing potential obstacles to implementation (e.g., integrating a licensed clinical social worker as a screener into the pediatric setting, space, and time constraints), and creating a data collection system so that the five performance metrics that were initially outlined in the grant proposal were tracked.
Project implementation
Screening
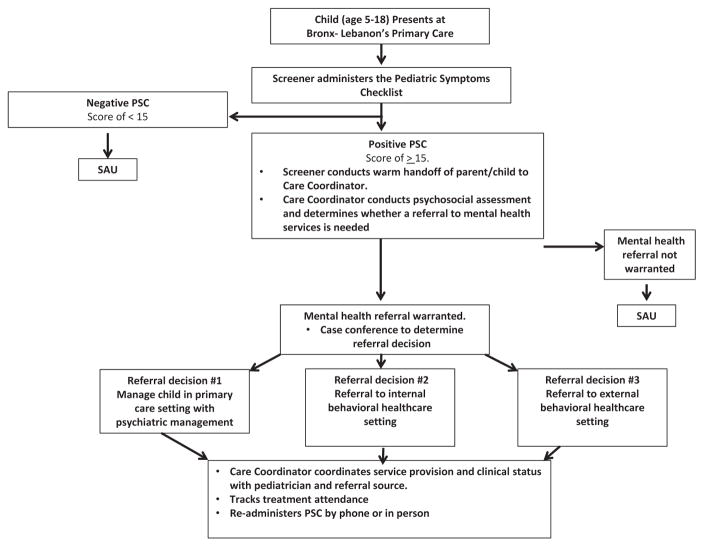
As pictured in Figure 1, the first step of the pathway is to screen for mental health problems in the primary care setting. Although the initial focus of this project was on disruptive behavior problems, pediatricians from the pediatric site reported depression and attention deficit hyper-activity disorder were also common problems among the children they saw in the practice. Therefore, the screening instrument would optimally need to assess for externalizing, internalizing, and attention-related issues.
Figure 1.
Integrated care pathway.
An additional set of considerations for choosing the screening instrument was that the measure be psychometrically validated (consistent with one of the core competencies stated by SAMHSA-HRSA’s Center for Integrated Health Solutions), free or low cost in order to enhance sustainability, easy to administer, and short in length so as not to burden families. Further, as a high percentage of families who attend the ambulatory center are Spanish-speaking, it was necessary that the instrument be validated in both Spanish and English.
For these reasons, the Pediatric Symptom Checklist (PSC)-35 was chosen as the screening instrument. The PSC is a publicly available instrument that contains items targeting emotional and behavioral problems. The instrument has three subscales: (1) externalizing problems, which consists of seven items, (2) internalizing problems, which consists of five items, and (3) attentional problems, consisting of five items. Caregivers rate how much of a problem each item is (e.g., “complains of aches/pains,” “acts as if driven by a motor”), from 0, indicating it is never a problem, to 2, which indicates it is often a problem. Each subscale is calculated separately depending on a specific set of items; however, a total score of 28 or higher is indicative of the presence of psychosocial impairment and the need for an assessment to further evaluate the child’s mental health status.
This scale, which was specifically designed to be used in primary care settings, is highly reliable (test retest reliability ranges from .84 to .91) and valid instrument (studies suggest 68% of children who screen positive on the PSC will be identified as impaired, and 95% of children who are negative are identified as unimpaired by a mental health professional) (http://www.massgeneral.org/psychiatry/services/psc_scoring.aspx). In order to reduce time constraints, a bilingual screener with a master’s degree in a mental health field was embedded within the primary care site to administer the PSC-35 to youth. The screener received training in the administration and scoring of the PSC.
Comprehensive assessment
The screener then presents the results to the family. Children who screen negative receive services as usual, which consists of ongoing routine pediatric primary care. Children who obtain a positive screen are referred to the care coordinator, a licensed clinical social worker who is also bilingual and based in the pediatric setting. The care coordinator answers any questions and obtains permission to conduct a psychosocial assessment that is based upon the specific symptoms the child is experiencing (e.g., children who screen positive on the internalizing problems subscale receive the Spence Children’s Anxiety Scale; Spence, 1998). The care coordinator received a series of trainings in the administration of the screening and assessment tools, as well as care coordination.
Initial care coordination
After the comprehensive assessment, the screener, care coordinator, and pediatrician convene to discuss the results and referral to one of three venues: (1) managing the child’s mental health within the primary care setting, (2) referring the child to Bronx Lebanon’s behavioral health clinic, or (3) referring the child to specialty care clinics. Cases that are straightforward (e.g., ADHD without comorbidity) are referred to the primary care setting, and supports were brought in to prepare pediatric staff to manage mental health problems in primary care, including trainings in childhood mental health and treatment conducted by a psychiatrist and on call psychiatric consultation. Cases that are more complex, such as comorbid mental health problems or mental health/substance abuse problems, are first referred to Bronx Lebanon’s behavioral health care clinic, or if at capacity, referred to the specialty care clinic.
To enhance engagement in treatment, both pediatric staff and the care coordinator were trained in evidence-based engagement strategies developed by McKay and colleagues specifically for children and families of color living in impoverished communities. These brief, engagement strategies derived from prior research on engaging children with substance abuse difficulties and families into services clarify expectations about mental health treatment and providers and address concrete and logistical obstacles (see McKay et al., 2004; McKay & Bannon, 2004 for a more thorough description).
Ongoing initial care coordination
After presenting the family with the referral recommendation, the care coordinator coordinates service provision between the primary and behavioral care site. Coordination includes a series of case conferences between the primary care pediatrician, mental health professional (if applicable), and care coordinator every 3 months. Guiding the case conference is the results of the condition-specific standardized measure, which is re-administered every three months, as well as treatment attendance and any other factors that are relevant to the child’s emotional health and receipt of treatment. In the cases in which a family is not engaged in care, the care coordinator utilizes the engagement strategies referenced above to optimally facilitate service use.
Implementation barriers and recommendation
It is important to note both provider and logistic barriers that were faced during model development and implementation. At the provider level, physicians were concerned that they lacked knowledge and training to treat and manage pharmacology as part of mental health treatment. To address this concern, two training sessions were set up with a leading psychiatrist at a major medical center in New York City to improve knowledge and skills in pediatric pharmacology, mental health conditions, and evidence-based treatment. Further, the training psychiatrist agreed to remain on call as an ongoing consulting psychiatrist. Aside from physicians, the care coordinator and screener, who are both licensed clinical social workers, received a training session led by a child psychologist and National Institutes of Health (NIH)-funded researcher to describe the model in detail and deliver knowledge and skills of pediatric mental health symptoms, diagnoses, and comprehensive assessment procedures. Lastly, a training session was provided across disciplines in the pediatric clinic to provide knowledge and skills pertaining to evidence based engagement strategies. At the logistic level, there were concerns that the primary care setting would not allow for physicians to do screenings or allocate enough staff to effectively screen children and coordinate their care. As a result, we boosted their internal resources by adding our own licensed clinical social workers to the primary care setting to administer screening and provide care coordination. To promote sustainability once the grant ends, the licensed clinical social workers will begin billing for services to support their roles as care coordinator and screener.
Given the barriers that were faced, it is important to share an important recommendation for implementation of a model such as this. Before undertaking development and implementation, we found it very important to complete an organizational assessment to determine the needs, strengths, and weaknesses of the clinic that we ultimately wanted to work with as described by Glisson and Williams (2015). Accordingly, we recommend this as the first step in the model development and implementation process since the issues presented above will likely vary based on location and context.
Discussion
The purpose of this article was to present an integrated health model linking children receiving services at a major pediatric center located in one of the poorest communities in New York to mental health services. Primary care has become the de facto provider for many child mental health conditions, such as ADHD and depression (Godoy & Carter, 2013), yet pediatricians feel they lack the training and knowledge to adequately address mental health problems (Williams et al., 2004). Integrated care models have the potential to compliment pediatric services, provide a central behavioral health home, and decrease fragmentation (Godoy & Carter, 2013). It also provides support for pediatricians as they navigate what can be unfamiliar territory and reduce logistical, perceptual, and provider-level obstacles to service receipt.
The model presented here attempted to address these issues; trainings were conducted to enhance provider knowledge about engaging families into services, and evidence based pharmacological and psychological treatments for internalizing, externalizing, and attention-related problems. A psychiatrist was also available for consultation for pediatricians managing the child’s mental health symptoms and pharmacology in house. Further, we embedded a screener and care coordinator into the practice to reduce potential time-related issues related to assessment and care coordination, and optimally enhance the clinical sustainability of the model.
In addition to clinical sustainability, The SAMHSA-HRSA Center for Integrated Health Solutions (2013) emphasizes integrated care systems also need to be financially sustainable in order to be adopted and embedded within practice over time. To this end, we chose a free, publicly available screening instrument, and employed staff who would be able to bill for services once the grant ended. Additionally, a cost–benefit analysis of the pathway and whether it reduces high-cost expenditures including emergency room visits, which was the main objective of the project, is currently underway. It is important to highlight that social workers were integral to this project, involved in the development of the model, screening, care coordination, and providing therapeutic services. It is imperative for the social work field to be more involved in the development and implementation of integrated care models to better link primary and behavioral health care, such as this one, since social workers provide the majority of mental health care in the United States (Duffy et al., 2004; Hodge et al., 2007).
In sum, integrated care pathways offer much promise for children at risk for undetected and untreated mental health problems. Early detection and treatment can prevent the perpetuation of mental health problems into adolescence and adulthood, reducing individual, familial, and societal burden, and enhancing the lives of children and their families. The hope for this innovative model is that it improves the identification of mental health problems and access to services among a high-risk population, streamlines service systems, and reduces high-cost expenditures due to unmanaged mental health conditions and disconnection from a regular source of mental health care.
References
- Alegría M, Canino G, Lai S, Ramirez RR, Chavez L, Rusch D, Shrout PE. Understanding caregivers’ help-seeking for Latino children’s mental health care use. Medical Care. 2004;42(5):447–455. doi: 10.1097/01.mlr.0000124248.64190.56. [DOI] [PubMed] [Google Scholar]
- Alegría M, Atkins M, Farmer E, Slaton E, Stelk W. One size does not fit all: Taking diversity, culture and context seriously. Administration and Policy in Mental Health and Mental Health Services Research. 2010;37(1–2):48–60. doi: 10.1007/s10488-010-0283-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunelle J, Porter R. Integrating care helps reduce stigma. Health Progress. 2013;24:26–29. [PubMed] [Google Scholar]
- Cauce AM, Domenech-Rodríguez M, Paradise M, Cochran BN, Shea JM, Srebnik D, Baydar N. Cultural and contextual influences in mental health help seeking: A focus on ethnic minority youth. Journal of Consulting and Clinical Psychology. 2002;70(1):44–55. doi: 10.1037/0022-006X.70.1.44. [DOI] [PubMed] [Google Scholar]
- Dubay LC, Lebrun LA. Health behavior and health care disparities: Disentangling the effects of income and race in the United States. International Journal of Health Services. 2012;42(4):607–625. doi: 10.2190/HS.42.4.c. [DOI] [PubMed] [Google Scholar]
- Duffy FF, West JC, Wilk J, Narrow WE, Hales D, Thompson J, Manderscheid RW. Mental health, United States, 2002. Rockville, MD: US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services; 2004. Mental health practitioners and trainees; pp. 327–368. [Google Scholar]
- Foster EM, Jones DE. The high costs of aggression: Public expenditures resulting from conduct disorder. American Journal of Public Health. 2005;95(10):1767–1772. doi: 10.2105/AJPH.2004.061424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedenthal S. Racial disparities in mental health service use by adolescents who thought about or attempted suicide. Suicide and Life-Threatening Behavior. 2007;37(1):22–34. doi: 10.1521/suli.2007.37.issue-1. [DOI] [PubMed] [Google Scholar]
- Garcia JA, Weisz JR. When youth mental health care stops: Therapeutic relationship problems and other reasons for ending youth outpatient treatment. Journal of Consulting and Clinical Psychology. 2002;70:439–443. doi: 10.1037/0022-006X.70.2.439. [DOI] [PubMed] [Google Scholar]
- Garland AF, Hough RL, Landsverk J, McCabe KM, Yeh M, Ganger WC, Reynolds BJ. Racial and ethnic variations in mental health care utilization among children in foster care. Children’s Services: Social Policy, Research and Practice. 2000;3(3):133–146. doi: 10.1207/S15326918CS0303_1. [DOI] [Google Scholar]
- Garland AF, Landsverk JA, Hough RL, Ellis-MacLeod E. Type of maltreatment as a predictor of mental health service use in foster care. Child Abuse and Neglect. 1996;20:675–688. doi: 10.1016/0145-2134(96)00056-7. [DOI] [PubMed] [Google Scholar]
- Garland AF, Lau AS, Yeh M, McCabe KM, Hough RL, Landsverk JA. Racial and ethnic differences in utilization of mental health services among high-risk youths. The American Journal of Psychiatry. 2005;162(7):1336–1343. doi: 10.1176/appi.ajp.162.7.1336. [DOI] [PubMed] [Google Scholar]
- Glisson C, Williams NJ. Assessing and changing organizational social contexts for effective mental health services. Annual Review of Public Health. 2015;36:507–523. doi: 10.1146/annurev-publhealth-031914-122435. [DOI] [PubMed] [Google Scholar]
- Godoy L, Carter AS. Identifying and addressing mental health risks and problems in primary care pediatric settings: A model to promote developmental and cultural competence. American Journal of Orthopsychiatry. 2013;83(1):73–88. doi: 10.1111/ajop.12005. [DOI] [PubMed] [Google Scholar]
- Gopalan G, Goldstein L, Klingenstein K, Sicher C, McKay M. Engaging families into child mental health treatment: Updates and special considerations. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2010;19(3):182–196. [PMC free article] [PubMed] [Google Scholar]
- Heflinger CA. Measuring service system coordination in managed mental health care for children and youth. Evaluation and Program Planning. 1996;19(2):155–163. doi: 10.1016/0149-7189(96)00006-7. [DOI] [Google Scholar]
- Hodge MA, Morris JA, Daniels AS, Stuart GW, Huey LY, Adams N. Action plan for behavioral health workforce development: A framework for discussion. Report prepared for the Substance Abuse and Mental Health Services Administration (SAMHSA) by The Annapolis Coalition on the Behavioral Health Workforce. 2007 Retrieved from http://annapoliscoalition.org/wp-content/uploads/2013/11/action-plan-full-report.pdf.
- Huang L, Macbeth G, Dodge J, Jacobstein D. Transforming the workforce in children’s mental health. Administration and Policy in Mental Health and Mental Health Services Research. 2004;32(2):167–187. doi: 10.1023/B:APIH.0000042745.64582.72. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: The National Academies Press; 2001. [PubMed] [Google Scholar]
- Kataoka S, Zhang L, Wells KB. Unmet need for mental health care among U.S. children: Variation by ethnicity and insurance status. American Journal of Psychiatry. 2002;159:1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Holland L, Crowley M. Family experience of barriers to treatment and premature termination from child therapy. Journal of Consulting and Clinical Psychology. 1997;65(3):453–463. doi: 10.1037/0022-006X.65.3.453. [DOI] [PubMed] [Google Scholar]
- Kerkorian D, Bannon WM, McKay M. Seeking help a second time: Parents’/ caregivers’ characterizations of previous experiences with mental health services for their children and perceptions of barriers to future use. American Journal of Orthopsychiatry. 2006;76(2):161–166. doi: 10.1037/0002-9432.76.2.161. [DOI] [PubMed] [Google Scholar]
- Kolko DJ, Campo J, Kilbourne AM, Hart J, Sakolsky D, Wisniewski S. Collaborative care outcomes for pediatric behavioral health problems: A cluster randomized trial. Pediatrics. 2014;133(4):e981–92. doi: 10.1542/peds.2013-2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koppelman J. The provider system for children’s mental health: Workforce capacity and effective treatment. Washington, DC: National Health Policy Forum; 2004. Oct, [PubMed] [Google Scholar]
- Loeber R, Green SM, Lahey BB, Frick PJ, McBurnett K. Findings on disruptive behavior disorders from the first decade of the Developmental Trends Study. Clinical Child and Family Psychology Review. 2000;3(1):37–60. doi: 10.1023/A:1009567419190. [DOI] [PubMed] [Google Scholar]
- Lopez SR. Mental health care for Latinos: A research agenda to improve the accessibility and quality of mental health care for Latinos. Psychiatric Services. 2002;53(12):1569–1573. doi: 10.1176/appi.ps.53.12.1569. [DOI] [PubMed] [Google Scholar]
- MacNaughton KL, Rodrigue JR. Predicting adherence to recommendations by parents of clinic-referred children. Journal of Consulting and Clinical Psychology. 2001;69:262–270. doi: 10.1037/0022-006X.69.2.262. [DOI] [PubMed] [Google Scholar]
- Martini R, Hilt R, Marx L, Chenven M, Naylor M, Sarvet B, Ptakowski KK. Best principles for integration of child psychiatry into the pediatric health home. Washington, DC: American Academy of Child & Adolescent Psychiatry; 2012. Retrieved from https://www.aacap.org/App_Themes/AACAP/docs/clinical_practice_center/systems_of_care/best_principles_for_integration_of_child_psychiatry_into_the_pediatric_health_home_2012.pdf. [Google Scholar]
- McKay M, Hibbert R, Hoagwood K, Rodriguez J, Murray L. Integrating evidence-based engagement interventions into ‘real world’ child mental health settings. Journal of Brief Treatment and Crisis Intervention. 2004;4:177–186. doi: 10.1093/brief-treatment/mhh014. [DOI] [Google Scholar]
- McKay MM, Bannon WM. Engaging families in child mental health services. Child and Adolescent Psychiatric Clinics of North America. 2004;13:905–921. doi: 10.1016/j.chc.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Miller LM, Southam-Gerow MA, Allin RBJ. Who stays in treatment? Child and family predictors of youth client retention in a public mental health agency. Child & Youth Care Forum. 2008;37(4):153–170. doi: 10.1007/s10566-008-9058-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Initiative for Children’s Healthcare Quality. Care Model for Child Health. 2011 Retrieved from www.nichq.org/how_we_work/care_model_for_child_health.html.
- Nock MK, Kazdin AE. Parent expectancies for child therapy: Assessment and relation to participation in treatment. Journal of Child and Family Studies. 2001;10:155–180. doi: 10.1023/A:1016699424731. [DOI] [Google Scholar]
- Pires S. Building Systems of Care: A Primer. National Technical Assistance Center for Children’s Mental Health; 2002. Retrieved from https://gushare.georgetown.edu/ChildHumanDevelopment/CENTER%20PROJECTS/WebSite/PRIMER_CompleteBook.pdf. [Google Scholar]
- Sand N, Silverstein M, Glascoe FP, Gupta VB, Tonniges TP, O’Connor KG. Pediatricians’ reported practices regarding developmental screening: Do guidelines work? Do they help? Pediatrics. 2005;116:174–179. doi: 10.1542/peds.2004-1809. [DOI] [PubMed] [Google Scholar]
- Saxe L, Cross T, Silverman N. Children’s mental health: The gap between what we know and what we do. American Psychologist. 1988;43(10):800–807. doi: 10.1037/0003-066X.43.10.800. [DOI] [PubMed] [Google Scholar]
- Spence SH. A measure of anxiety symptoms among children. Behaviour Research and Therapy. 1998;36(5):545–566. doi: 10.1016/S0005-7967(98)00034-5. [DOI] [PubMed] [Google Scholar]
- Stroul B, Blau G, Friedman R. Updating the system of care concept and philosophy. Washington, DC: Georgetown University Center for Child and Human Development, National Technical Assistance Center for Children’s Mental Health; 2010. [Google Scholar]
- Stroul BA, Friedman RM. A system of care for children and youth with severe emotional disturbances. Washington, DC: Georgetown University Child Development Center, CASSP Technical Assistance Center; 1994. Revised edition. [Google Scholar]
- The SAMHSA-HRSA Center for Integrated Health Solutions. Integrating Behavioral Health and Primary Care for Children and Youth: Concepts and Strategies was developed for the SAMHSA-HRSA Center for Integrated Health Solutions. 2013 Retrieved from http://www.integration.samhsa.gov/integrated-care-models/13_June_CIHS_Integrated_Care_System_for_Children_final.pdf.
- Tolan PH, Gorman-Smith D, Loeber R. Developmental timing of onsets of disruptive behaviors and later delinquency of inner-city youth. Journal of Child and Family Studies. 2000;9(2):203–220. doi: 10.1023/A:1009471021975. [DOI] [Google Scholar]
- Tolan PH, Henry D. Patterns of psychopathology among urban poor children: Comorbidity and aggression effects. Journal of Consulting and Clinical Psychology. 1996;64(5):1094–1099. doi: 10.1037/0022-006X.64.5.1094. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. State and County QuickFacts. Bronx County, NY: 2015. Retrieved from http://quickfacts.census.gov/qfd/states/36/36005.html. [Google Scholar]
- U.S. Public Health Service. Mental Health: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; 1999. [Google Scholar]
- U.S. Public Health Service. Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda. Washington, DC: Department of Health and Human Services; 2000a. [Google Scholar]
- U.S. Public Health Service. Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda. Washington, DC: Department of Health and Human Services; 2000b. [Google Scholar]
- U.S. Public Health Service. Youth Violence: A report of the surgeon general. Washington, DC: Department of Health and Human Services; 2001. [Google Scholar]
- Vernberg EM, Roberts MC, Nyre JE. School-based intensive mental health treatment. In: Marsh DT, Fristad MA, editors. Handbook of serious emotional disturbance in children and adolescents. New York, NY: John Wiley & Sons; 2002. pp. 412–427. [Google Scholar]
- Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: Translating evidence into action. Health Affairs. 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- Washburn J, Teplin L, Voss L, Simon C, Abram K, McClelland G. Psychiatric disorders among detained youths: A comparison of youths processed in juvenile court and adult criminal court. Psychiatric Services. 2008;59(9):965–973. doi: 10.1176/ps.2008.59.9.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Verdeli H, Gameroff MJ, Bledsoe SE, Betts K, Mufson L, … Wickramaratne P. National survey of psychotherapy training in psychiatry, psychology, and social work. Archives of General Psychiatry. 2006;63:925–934. doi: 10.1001/archpsyc.63.8.925. [DOI] [PubMed] [Google Scholar]
- Williams J, Klinepeter K, Palmes G, Pulley A, Foy JM. Diagnosis and treatment of behavioral health disorders in pediatric practice. Pediatrics. 2004;114:601–606. doi: 10.1542/peds.2004-0090. [DOI] [PubMed] [Google Scholar]
- Zimmerman FJ. Social and economic determinants of disparities in professional help-seeking for child mental health problems: Evidence from a national sample. Health Services Research. 2005;40(5p1):1514–1533. doi: 10.1111/hesr.2005.40.issue-5p1. [DOI] [PMC free article] [PubMed] [Google Scholar]