Hydrophilic polymers are widely used as surface coatings on vascular medical devices including guidewires, introducer and delivery sheaths, implantable stents and coils as well as cardiac, central and peripheral catheters. These surface coatings have unique properties that enhance biocompatibility and maneuverability of endovascular technologies, while decreasing friction and reducing trauma to vessel walls. Select polymers also enable targeted intravascular drug delivery while decreasing systemic toxicity and improving compliance. With increasing trends towards minimally invasive procedures and novel drug delivery systems, applications of polymer coatings on vascular devices are gradually increasing. Despite their advantages, unanticipated biological reactions and coating delamination from vascular device surfaces have been recognized worldwide and associated with significant morbidity over recent years1–4.
Non-healing ulcers and painful access site nodules were first recognized over ten years ago in patients who underwent transradial catheterization using hydrophilic coated vascular sheaths 2. Biopsies of these superficial lesions revealed localized inflammation resulting from intradermal deposits of polymeric foreign bodies. These reports established polymer coatings as a potential iatrogenic cause of inflammation and led to warning labels on specific Cook branded vascular sheaths (Cook Medical, Inc., Bloomington, IN). More significant reactions have subsequently been documented due to mechanical abrasion and embolization of polymer particles from the surfaces of various branded devices to sites downstream from areas of intravascular insertion or implantation (Fig 1A). This phenomenon of hydrophilic polymer embolization has steadily gained attention following initial reports of fatality in 20093,4.
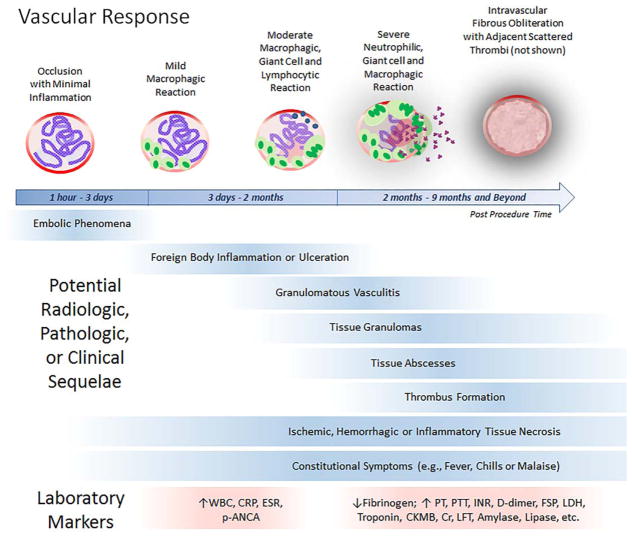
Figure 1. Hydrophilic Polymer Embolism Formation and Histologic Appearances.
Schematic depiction showing polymer coating delamination from vascular device surface (A), with localized foreign body deposition at access site (single arrow) or associated embolic phenomena (double arrows). Histologic findings in a patient with pulmonary hydrophilic polymer embolism include non-refractile, basophilic, granular, lamellated intravascular foreign bodies (B,C) with associated congestion (B,C), inflammation (C,D), vasculitis (D), adjacent thrombi (E) and pulmonary infarct (not shown).
The 2015 U.S. FDA safety communication pertaining to lubricious coating separation from intravascular medical devices (http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm473794.htm) disclosed approximately 500 Medical Device Reports of this phenomenon over a two-year period5. In this statement, the FDA acknowledged a rising clinical concern pertaining to polymer coating phenomena and reported 11 device recalls and 9 deaths associated primarily with peeling or flaking of interventional guidewire coatings since the start of 2010. Furthermore, the FDA acknowledged existing gaps in current national and international device standards and stated that the agency will work with stakeholders to further evaluate surface integrity and safety of coated vascular medical devices. Despite FDA acknowledgment, polymer complications remain clinically under-recognized by healthcare providers who routinely manage and treat patients using coated intravascular medical technologies.
Reported Adverse Events
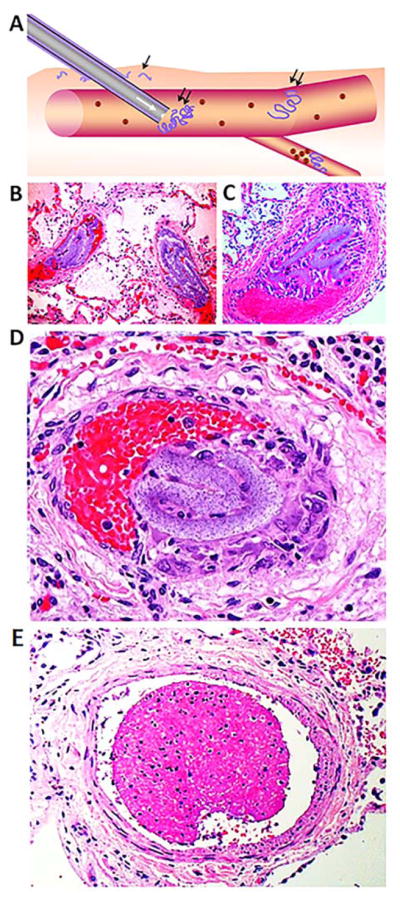
Polymer-induced vascular effects may include luminal occlusion, intra- and peri-vascular inflammation and fibrous obliteration following embolism to small, intermediate, and large-sized vessels throughout the body (Fig 1B–F). Reported tissue injuries have most commonly involved the brain1,3,4,6–8 and lungs1,4,9, however involvement of the heart10–13, kidneys11,12, skin14–16, arteriovenous grafts11, transplanted organs4,11, colon17, small intestine17, liver, and pancreas have also been documented, along with multisystem involvement and systemic effects in rare cases (Mehta, unpublished observations). Sequelae may include focal or multifocal hemorrhage, inflammation, arteritis, vasculopathy, thrombosis, transient ischemia or tissue infarcts, and fever among other effects1–4. The majority of polymer reactions are subclinical. However complications are often long-lasting and may lead to serious irreversible injuries. Outcomes have been shown to vary with embolic burden, site(s) of involvement, co-existing morbidities and severity of secondary reactions1–4. Symptom onset may occur during the acute, subacute or delayed post-procedure periods8, with onset as late as 9 months post-procedure7 and recurrence or persistence of reactive inflammation in some cases for over 3 years11. While sequelae are heterogeneous and organ specific, predictable vascular reaction patterns have been recognized (Fig 2)1,8. Postmortem data reveal a hospital autopsy frequency of at least 13%, although the clinical incidence of polymer embolism is unknown1.
Figure 2. Summary of Vascular Changes Induced by Hydrophilic Polymer Emboli, with Diagnostic Features.
Abbreviations: CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; FSP, fibrin split products; INR, international normalised ratio; LDH, lactate dehydrogenase; LFT, liver function tests; p-ANCA, perinuclear anti-neutrophil cytoplasmic antibodies; PT, prothrombin time; PTT, Partial thromboplastin time; WBC, white blood cell
Diagnosis and Management
A heightened index of suspicion is required for clinical diagnosis of polymer coating embolism. Recognition of specific presenting patterns during the acute, subacute and delayed post-procedure intervals may facilitate empiric diagnosis of this iatrogenic phenomenon (Fig 2, upper panels)1,8. Preliminary data suggest the utility of routine serum markers as supportive evidence of the diagnosis (Fig 2, lower panel)1,8. Tissue sampling (e.g., biopsy, autopsy, or evaluation of evacuated embolic or clot material) is necessary for histologic confirmation, although sampling errors occur and negative biopsies do not exclude the diagnosis1,3. On standard pathologic preparations, polymer emboli generally appear as nonrefractile, nonpolarizable, basophilic, granular lamellated foreign bodies (Fig 1B–D). For accurate diagnosis, infection and alternate causes of embolism or vasculitis should be ruled out. Recognition of this iatrogenic event may prevent misdiagnosis of unrelated medical disease (e.g., transplant organ rejection, parasitic infection or sarcoidosis)12,17. In some cases, steroids and immunomodulatory therapies have been effective in mitigating inflammatory reactions, although optimal dosages are unreported and risks of immunosuppression should be considered with long-term use. Antiplatelet therapy has additionally been reported to alleviate symptoms in some patients, while surgical resection may be necessary in others to exclude treatable conditions or to debride secondary necrotic wounds9. As no specific therapies are currently available, additional supportive measures should be implemented, as needed.
Clinical Implications
Post-procedural embolic phenomena have generally been attributed to air, septic, atheromatous, thrombotic or other foreign body embolism, however, polymer embolism is now a well-documented iatrogenic event attributed to catheterization and other vascular procedures. A recent analysis of material captured through use of an embolic protection device during mitral valve repair showed that polymer embolism occurred as frequently as acute thromboembolism (86%), with native tissue emboli (64%) and organizing thrombi (29%) noted less often18. Frequent polymer coating emboli have also been affiliated with other percutaneous procedures19,20. Thus, polymer embolism should be included in the differential of unanticipated ischemic or inflammatory complications as well as unexplained vasculopathies occurring during the post-procedural clinical setting. Iatrogenic polymer effects may be transient and self-limiting, as polymer emboli eventually biodegrade in vivo, although the time course is variable1,4. Unanticipated inflammation, particularly if persistent or associated with delayed onset following catheterization or endovascular treatment should raise clinical suspicion for this potential complication8. Onset of constitutional symptoms in the setting of temporally evolving vascular phenomena (eg., transient elevation of p-ANCA, with subsequent thrombosis, coagulopathy, sterile abscess or granulomata) should also prompt consideration for biodegrading polymeric reactions1,3,8,9. In cases with unclear embolic etiology, tissue evaluation may be considered if accurate detection will influence the need for medical or invasive therapies.
Future Directions
Given the millions of endovascular and catheter-based interventions performed worldwide each year as well as increasing trends toward polymer-based nanotherapies, there is an urgent need to better understand the effects of intravascular polymers in live patients. In large part, a lack of awareness on this subject and limitations of conventional diagnostic tools have hindered accurate assessments of polymer effects in the clinical setting1,3,4. However, methodologies such as use of embolic protection devices illustrate the feasibility of systematically analyzing particulates retrievable from the human bloodstream18. Heightened awareness and empiric diagnosis of this phenomenon would yield critical information regarding the incidence of polymer embolism in different contexts. Investigations into novel biomarkers and alternative methods of analyzing blood particulates may allow for more sensitive and specific methods of noninvasive clinical detection. Moreover, examination of distinct populations such as patients with immunosuppression (e.g., cancer or chronic steroid use), hyperinflammation (e.g., sepsis or autoimmune disease), acidosis (e.g., impaired renal function), vascular risk factors (e.g., diabetes or hypertension), chronic indwelling devices (e.g., implanted stents or prolonged dialysis) or potential toxicological interactions (e.g., various therapeutic regimens) may elucidate effects of intravascular polymers in patient subsets. Large-scale prospective studies and investigations into patient specific factors may further clarify the natural evolution, specific biodegradative profiles and long-term consequences of polymer deposition within the distal vasculature. Further work in this area will help stratify risks and improve the safety and design of modern devices and therapies, while impacting beneficially on vascular health and patient outcome.
Acknowledgments
R.I.M. is supported by a grant from the National Institute of Neurological Disorders and Stroke (K08NS089830).
Footnotes
Conflicts of Interest: All authors declare no conflicts of interest
Verification: All authors had access to the data and a role in writing this manuscript
References
- 1.Mehta RI, Mehta RI, Choi JM, Mukherjee A, Castellani RJ. Hydrophilic polymer embolism and associated vasculopathy of the lung: prevalence in a retrospective autopsy study. Hum Pathol. 2015;46:191–201. doi: 10.1016/j.humpath.2014.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kozak M, Adams DR, Ioffreda MD, et al. Sterile inflammation associated with transradial catheterization and hydrophilic sheaths. Cathet Cardiovasc Intervent. 2003;59:207–213. doi: 10.1002/ccd.10522. [DOI] [PubMed] [Google Scholar]
- 3.Mehta RI, Mehta RI, Fishbein MC, et al. Intravascular polymer material following coil embolization of a giant cerebral aneurysm. Hum Pathol. 2009;40:1803–1807. doi: 10.1016/j.humpath.2009.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehta RI, Mehta RI, Solis OE, Jahan R, Salamon N, Tobis JM, Yong WH, Vinters HV, Fishbein MC. Hydrophilic polymer emboli: an under-recognized iatrogenic cause of ischemia and infarct. Mod Pathol. 2010;23:921–30. doi: 10.1038/modpathol.2010.74. [DOI] [PubMed] [Google Scholar]
- 5.U.S. Food and Drug Administration. Lubricious coating separation from intravascular medical devices FDA Safety Communication. FDA; Silver Spring MD: 2015. [Accessed 20 November 2016]. Available at: http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm473794.htm. [Google Scholar]
- 6.Barnwell SL, D’Agostino AN, Shapiro SL, et al. Foreign bodies in small arteries after use of an infusion microcatheter. Am J Neuroradiol. 1997;18:1886–1889. [PMC free article] [PubMed] [Google Scholar]
- 7.Fealey ME, Edwards WD, Giannini C, et al. Complications of endovascular polymers associated with vascular introducer sheaths and metallic coils in 3 patients, with literature review. Am J Surg Pathol. 2008;32:1310–1316. doi: 10.1097/PAS.0b013e318165582a. [DOI] [PubMed] [Google Scholar]
- 8.Mehta RI, Mehta RI. Polymer-induced central nervous system complications following vascular procedures: spectrum of iatrogenic injuries and review of outcomes. Hum Pathol. 2016 Jul;53:178–90. doi: 10.1016/j.humpath.2016.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allan RW, Alnuaimat H, Edwards WD, et al. Embolization of hydrophilic catheter coating to the lungs: report of a case mimicking granulomatous vasculitis. Am J Clin Pathol. 2009;132:794–797. doi: 10.1309/AJCPH2PGCCPA0ZJF. [DOI] [PubMed] [Google Scholar]
- 10.El-Najjar V, Robinson M. Autopsy demonstration of intramyocardial polymer gel emboli associated with a giant-cell reaction following cardiac catheterization: a case report. Cardiovasc Pathol. 2012;21:59–61. doi: 10.1016/j.carpath.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Sequeira A, Parimoo N, Wilson J, Traylor J, Bonsib S, Abreo K. Polymer embolization from minimally invasive interventions. Am J Kidney Dis. 2013;61:984–987. doi: 10.1053/j.ajkd.2012.12.021. [DOI] [PubMed] [Google Scholar]
- 12.Chen CL, Chen NC, Wang JS. Acute hydrophilic-polymer nephropathy and acute renal failure. N Engl J Med. 2015;372:1775–6. doi: 10.1056/NEJMc1414822. [DOI] [PubMed] [Google Scholar]
- 13.Sanon S, Maleszewski JJ, Rihal CS. Hydrophilic polymer embolism induced acute transcatheter aortic valve thrombosis: a novel complication. Catheter Cardiovasc Interv. 2014;83:1152–1155. doi: 10.1002/ccd.25353. [DOI] [PubMed] [Google Scholar]
- 14.Danowski KM, Morrison M, Ghaferi J, Cotton J. Hydrophilic polymer embolization: an emerging cause of livedo reticularis. J Cutan Pathol. 2014;41:813–5. doi: 10.1111/cup.12434. [DOI] [PubMed] [Google Scholar]
- 15.Thompson AK, Peters MS, El-Azhary RA, Gibson LE, Chang MB, Griffin JR, Davis MD, McEvoy MT, Camilleri MJ, Bridges AG. Cutaneous microemboli from hydrophilic polymer after endovascular procedures. J Am Acad Dermatol. 2015;73:666–71. doi: 10.1016/j.jaad.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 16.Hardy CL, Glass JS, Sorrells T, Nicholas LC. Hemorrhagic panniculitis caused by delayed microemboli from intravascular device. JAMA Dermatol. 2015;151:204–7. doi: 10.1001/jamadermatol.2014.2393. [DOI] [PubMed] [Google Scholar]
- 17.Chavez JA, Chen W, Frankel WL, Arnold CA. Hydrophilic Polymer-associated Ischemic Enterocolitis. Am J Surg Pathol. 2016 Nov 4; doi: 10.1097/PAS.0000000000000765. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 18.Frerker C1, Schlüter M2, Sanchez OD3, Reith S4, Romero ME3, Ladich E3, Schröder J4, Schmidt T5, Kreidel F5, Joner M3, Virmani R3, Kuck KH5. Cerebral Protection During MitraClip Implantation: Initial Experience at 2 Centers. JACC Cardiovasc Interv. 2016;9:171–9. doi: 10.1016/j.jcin.2015.09.039. [DOI] [PubMed] [Google Scholar]
- 19.Grundeken MJ, Li X, Kurpershoek CE, et al. Distal embolization of hydrophilic-coating material from coronary guidewires after percutaneous coronary interventions. Circ Cardiovasc Interv. 2015;8:e001816. doi: 10.1161/CIRCINTERVENTIONS.114.001816. [DOI] [PubMed] [Google Scholar]
- 20.Schmidt T, Akdag O, Wohlmuth P, Thielsen T, Schewel D, Schewel J, Alessandrini H, Kreidel F, Bader R, Romero M, Ladich E, Virmani R, Schäfer U, Kuck KH, Frerker C. Histological Findings and Predictors of Cerebral Debris From Transcatheter Aortic Valve Replacement: The ALSTER Experience. J Am Heart Assoc. 2016;5:e004399. doi: 10.1161/JAHA.116.004399. [DOI] [PMC free article] [PubMed] [Google Scholar]