Abstract
The purpose of the current study was to predict concurrent levels of problem behaviors from young children’s baseline cortisol and attachment classification, a proxy for the quality of caregiving experienced. In a sample of 58 children living at or below the federal poverty threshold, children’s baseline cortisol levels, attachment classification, and problem behaviors were assessed at 17 months of age. We hypothesized that an interaction between baseline cortisol and attachment classification would predict problem behaviors above and beyond any main effects of baseline cortisol and attachment. However, based on limited prior research, we did not predict whether or not this interaction would be more consistent with diathesis-stress or differential susceptibility models. Consistent with diathesis-stress theory, the results indicated no significant differences in problem behavior levels among children with high baseline cortisol. In contrast, children with low baseline cortisol had the highest level of problem behaviors in the context of a disorganized attachment relationship. However, in the context of a secure attachment relationship, children with low baseline cortisol looked no different, with respect to problem behavior levels, then children with high cortisol levels. These findings have substantive implications for the socioemotional development of children reared in poverty.
Keywords: Diathesis-stress, Cortisol, Attachment, Problem behaviors
1. Introduction
In 2015, an estimated 13.5% of all U.S. citizens, including over one in five children, were living below the federal poverty threshold (U.S. Census Bureau, 2016). Children growing up in conditions of poverty are at increased risk for impaired socioemotional functioning compared to their counterparts living above the poverty threshold (Duncan and Brooks-Gunn, 2000). Parents with low socioeconomic status, compared to parents with high socioeconomic status, tend to report more withdrawal, inattentiveness, and aggression in their children (Brooks-Gunn & Duncan, 1997; Meins, Centifanti, Fernyhough, & Fishburn, 2013; van Oort, van der Ende, Wadsworth, Verhulst, & Achenbach, 2011). These problems tend to persist and also place children on trajectories to experience disadvantages throughout the life course (McLeod & Fettes, 2007; Turney, 2012).
Although the specific pathways linking poverty to problem behaviors are still coming into focus, researchers have suggested biological mechanisms for this prospective relation. The biological embedding framework suggests that the early chronic stress associated with poverty may get “under the skin” and become “embedded” in biological systems, leading to individual differences in physiology, development, and health (Evans, Chen, Miller, & Seeman, 2012; McEwen & Stellar, 1993; Propper, 2012). Compelling evidence from animal and human studies support this framework and indicate that early stress exposure can indeed have lasting effects on multiple stress response systems (Alkon, Wolff, & Boyce, 2012; Evans et al., 2012; Levine, 2005; Lupien, King, Meaney, & McEwen, 2000). These alterations in biological processes are hypothesized to influence physical and mental health early in life and across the lifespan (Hertzman, 2012). As such, contextually mediated alterations in children’s stress physiology may be one mechanism through which poverty influences socioemotional development (Engle & Black, 2008; Mills-Koonce & Towe-Goodman, 2012; Obradović, Bush, & Boyce, 2011).
One principal psychobiological stress system that has been the focus of such research is the hypothalamic-pituitary-adrenocortical (HPA) axis. Cortisol, a marker of HPA output, contributes to the modulation of numerous systems, including cardiovascular and immune system functioning (Sapolsky, Romero, & Munck, 2000; Takahashi et al., 2004). Researchers have frequently linked low baseline cortisol levels to higher rates of externalizing behaviors, including oppositional and aggressive behavior (Shirtcliff, Granger, Booth, & Johnson, 2005; van Goozen, Matthys, Cohen-Kettenis, Buitelaar, & Van Engeland, 2000). High baseline cortisol, on the other hand, may also be problematic and has been regularly associated with internalizing behaviors (Granger, Stansbury, & Henker, 1994; Granger, Weisz, McCracken, Ikeda, & Douglas, 1996) and less effective executive functioning (Blair et al., 2011). However, there are conflicting findings on the links between baseline cortisol levels and childhood problem behaviors, with some researchers finding non-significant, or opposite relations (Alink et al., 2008; Dahl et al., 1989). As such, it is not entirely clear how baseline cortisol might act as a risk factor for problem behaviors among children reared in poverty.
A number of researchers have argued that the quality of caregiving a child receives is a factor that likely moderates the relations between children’s stress physiology and problem behaviors (Boyce and Ellis, 2005; Eisenberg et al., 2012; Luecken & Lemery, 2004). Supportive parenting encourages socioemotional competence by fostering the development of self-regulation and prosocial behaviors (Barnett, Gustafsson, Deng, Mills-Koonce, & Cox, 2012; Spinrad et al., 2007). In particular, the early development of emotion regulation is highly dependent on the responsiveness and patterns of regulation provided by attachment figures (Halligan et al., 2013). Studies have consistently demonstrated that sensitive and responsive caregiving promotes the development of secure attachment (Ainsworth, Blehar, Waters, & Wall, 1978; De Wolff & van IJzendoorn, 1997) whereas frightening/frightened, unpredictable, and extremely insensitive parenting is thought to contribute to the development of disorganized attachment (Hesse & Main, 2006). As such, secure and disorganized attachment reflect a history of caregiving extremes (Conradt, Measelle, & Ablow, 2013). Although researchers have identified caregiving quality as important determinants of children’s problem behaviors, relatively few efforts have been made to study these links in relation to children’s baseline cortisol levels.
Given these findings, it is likely that the interplay between caregiving experience and children’s cortisol levels influences early socioemotional outcomes among children living in the context of poverty. The differential susceptibility theory offers one potential mechanism through which contextual and caregiving influences moderate the relations between children’s HPA activity and socioemotional development (Belsky, Bakermans-Kranenburg, & Van IJzendoorn, 2007; also see Boyce & Ellis, 2005). According to differential susceptibility theory, children who would be considered more vulnerable to contextual risk within a traditional diathesis-stress framework (Zuckerman, 1999), such as children with physiological hyperreactivity, may also reap the benefits of supportive environments in a “for-better-and-for-worse” fashion (Belsky & Pluess, 2009). That is, susceptibilities may predispose children to maladaptation when paired with stressful, unsupportive contexts. However, according to differential susceptibility theory, this type of susceptibility may also predispose these children to the most successful outcomes when paired with supportive and positive contexts. In other words, susceptibilities can moderate the effect of context on adaptation such that sensitive children, compared with less sensitive peers, are more negatively affected by harmful rearing environments and more positively affected by supportive rearing environments (Boyce & Ellis, 2005). Thus, the essential difference between diathesis-stress and differential susceptibility models is that the former emphasizes the exclusive susceptibility to negative environments for some individuals, while the latter highlights susceptibility to both negative and positive environments in the same individuals (Belsky & Pluess, 2012).
Several studies have provided initial evidence suggesting that physiological reactivity may act as a marker of differential susceptibility (Belsky & Pluess, 2009). For example, in a sample of 5- to 6-year old children, Obradović. Bush, Stamperdahl, Adler, and Boyce (2010) found that children with high respiratory sinus arrhythmia (RSA; a measure of parasympathetic stress response related to respiration-linked heart rate) and high cortisol reactivity had more maladaptive outcomes (e.g., more externalizing and less prosocial behavior) in the context of high adversity but better adaptation in the context of low adversity. Similarly, in a sample of mothers and infants living in poverty, Conradt et al. (2013) found that infants with high baseline RSA exhibited the highest levels of problem behavior in the context of a disorganized relationship, but the lowest levels of problem behaviors in the context of a secure attachment relationship. Together, these studies offer evidence that stress-related physiology may act as a marker of differential susceptibility. At present, physiological susceptibilities have figured prominently in the growing differential susceptibility literature. However, relatively little of this work has focused on very young children, limiting our ability to identify susceptibilities earlier in life when they may be most sensitive to initial rearing conditions and, ideally, to intervention effects.
Beyond the immediate caregiving context, children living in poverty face a broad range of ecological stressors known to compromise socioemotional development (Chang, Shelleby, Cheong, & Shaw, 2012; Shonkoff, Boyce, & McEwen, 2009). Greater risk for adverse outcomes has been linked to low maternal education and low income (Baharudin & Luster, 1998; McLoyd, 1998), marital status (Bachman, Coley, & Carrano, 2011), infant negative emotionality (Gartstein & Rothbart, 2003), caregiver depression (Gross, Shaw, Burwell, & Nagin, 2009), and other measures of ecological risk. Typically, these risks are scored as present or absent and summed into a cumulative score (Conradt et al., 2013; Kochanska, Kim, & Koenig Nordling, 2012). Given that these stressors tend to be overrepresented in low-income families and are important predictors of development (Raver, 2004), we examined whether children’s cortisol levels interacted with attachment classifications to explain variance in problem behaviors beyond the variance explained by cumulative risk.
In sum, while many studies recognize that early caregiving is critical for successful socioemotional development and normative physiological development early in life, there is a paucity of studies, especially in contexts of poverty, examining how caregiving quality may moderate the relations between young children’s resting cortisol levels and early problem behaviors. Moreover, given the differing perspectives (e.g., diathesis-stress vs. differential susceptibility) regarding the nature of this moderation, it is unknown whether baseline cortisol levels may diminish or amplify the effects of attachment classification on problem behaviors. By examining this interplay, we can better understand how early problem behaviors are shaped among children with low-income backgrounds.
1.1. The present investigation
The overarching goal of this study was to predict 17-month problem behavior levels from the interaction between concurrent measures of baseline cortisol and attachment status. Specifically, we were interested in whether this interplay was more reflective of a diathesis-stress or differential susceptibility account. The 17-month time point provides an optimal opportunity to examine how attachment classification interacts with potential biomarkers of risk or susceptibility because it represents a period when children’s relationship with the primary caregiver are more clearly patterned and the effects of caregiving quality on stress physiology are more readily discernable compared to earlier ages (Bernard & Dozier, 2010; Gunnar & Quevedo, 2007; Tryphonopoulos, Letourneau, & Azar, 2014). Additionally, recent studies have also used attachment as an index of the quality of early rearing to test for differential susceptibility effects (Bakermans-Kranenburg & van Ijzendoorn, 2011; Conradt et al., 2013). We hypothesized an interaction between baseline cortisol and attachment classification when predicting concurrent problem behaviors above and beyond any main effects of baseline cortisol and attachment. Based on limited prior research, it was difficult to predict, with confidence, whether or not this interaction would be more consistent with diathesis-stress or differential susceptibility models.
2. Method
2.1. Participants
Participants were drawn from a prospective longitudinal study that followed 105 women at risk for parenting problems and their infants across the perinatal period. At the time of enrollment, all women were living below the federal poverty threshold. Of the original 105 women, 95 continued in the study are in our 5-month postnatal assessment, and of these, 86 dyads returned to the laboratory when infants were 17 months (mean rate of attrition = 9.2% between assessment periods). We examined data from 86 of the dyads that participated in the 17-month laboratory visit (M = 17.56 months, SD = 1.73; 48 female, 38 male). As there were too few children classified as avoidant (8%) and resistant (5%), our analyses were restricted to 70 dyads with secure and disorganized attachment classifications. Additionally, secure and disorganized attachment classifications represent positive and negative rearing extremes, providing a context through which to examine how physiological factors may confer adaptation and maladaptation. Finally, the analysis was limited to 58 dyads with complete physiological data (i.e., at least one baseline cortisol sample). There were no significant differences between dyads included or excluded in the present sample on a variety of demographic and risk variables including household income, maternal education, child negative emotionality, caregiver depression, and problem behaviors (all ps > 0.09).
There were no mean differences in baseline cortisol among children classified as avoidant and resistant and among those classified as secure and disorganized (all ps > 0.21). In addition, there were no significant differences in demographics, risk indices, problem behavior scores, or attachment classification among dyads with complete physiological and attachment data and those with missing physiological data or whose infants were classified as avoidant and resistant.
At the prenatal assessment, mothers’ mean age was 24.11 years (SD = 4.77, range = 18–38). Mothers were primarily European American (81.0%), with 2.9% African American, 5.8% Hispanic, 3.8% American Indian, 1% Asian, and 5.7% identifying themselves as “another group”.
2.2. Procedure
2.2.1. Baseline cortisol
Mothers and their children participated in two laboratory visits when children were 17 months of age. All sessions were conducted in the afternoon (M start time = 3:17 p.m.; SD = 47 min) to minimize diurnal rhythm effects. Participants were asked to refrain from eating or drinking (except water) for one hour before the session. For each session, a saliva sample was collected soon after the dyad arrived to index baseline cortisol levels. Samples were assayed for salivary cortisol by enzyme immunoassay (Salimetrics, State College, PA). The test used 25 μl of saliva, lower limit of sensitivity was 0.007 μg/dl, range = 0.007–3.0 μg/dl, average intra- and inter-assay coefficients of variation were <5% and <10%. The correlation between baseline cortisol across the two sessions was strong and significant (r = 0.42, p = 0.01); correspondingly, we found a non-significant difference between the absolute values of the two sessions, t(54) = −1.06, p = 0.20. Finally, there was no significant difference in the actual time-of-day that the two baseline samples were collected for each infant, t(54) = 0.80, p = 0.43. We therefore combined the two measures by averaging them together to create a single index of children’s baseline cortisol.
2.2.2. Attachment measures at 17 months
During the first 17-month laboratory session, dyads completed the strange situation procedure (Ainsworth et al., 1978). The procedure is designed to activate the child’s attachment system through a series of mother-child separation and reunion episodes (see Ainsworth et al., 1978; for a full description). This procedure was videotaped, and the tapes were coded by E. Carlson and L. A. Sroufe at the University of Minnesota. Overall agreement for the major attachment classifications was 90% (κ = 0.83). In our sample, 8% of infants were classified as avoidant, 67% as secure, 5% as resistant, and 20% as disorganized. Of the infants classified as disorganized, 44% received a secondary classification of avoidant, 38% received a secondary classification of secure, and 19% received a secondary classification of resistant. Although a lower percentage of infants (13%) in the present low-income sample were classified as insecure (resistant or avoidant) compared to a normative low-risk population (24%; van IJzendoorn, Schuengel, & Bakermans-Kranenburg, 1999), these rates are comparable to those reported in other samples of non-maltreated, low SES samples (e.g., Barnett, Ganiban, & Cicchetti, 1999; Crittenden, 1988). Consistent with the high-risk nature of our sample, this helps to explain the increased number of infants classified as disorganized rather than avoidant or resistant.
2.2.3. Average cumulative risk
Guided by cumulative risk research, which has consistently demonstrated that the accumulation of multiple risk factors explain more variance in developmental outcomes than do individual risk factors (Sameroff, Seifer, Barocas, Zax, & Greenspan, 1987; Sheinkopf et al., 2007), an average cumulative risk index was created to characterize the range of risk factors experienced by the sample. Mothers and their children were assessed on a wide range of measures of development, behavior, home environment, and caregiver characteristics chosen a priori based on developmental theory (Table 1). These indicators included premature birth (birth before 37 weeks gestational age), any perinatal medical complications, single mother status, less than a college education, low household income (less than an annual household income of $20,000), child negative emotionality (Infant Behavior Questionnaire-Revised; Garstein & Rothbart, 2003), maternal depression (score greater than clinical cutoff of 16 on Center for Epidemiologic Studies Depression Scale; Radloff, 1977), low family resources (Family Resource Scale; Dunst & Leet, 1987), and high level of confusion and disorganization in the home environment (Confusion, Hubbub, and Order Scale; Wachs, Ludwig, & Phillips, 1995). For measures with a dichotomous risk status (present vs. absent) or with a clinical cutoff score, one point was assigned for each risk item present. For more continuous measures (i.e., Family Resource Scale and Confusion, Hubbub, and Order Scale), “risk present” was identified as have scores one standard deviation below the mean. Risk for child negative emotionality was defined as present for scores greater than one standard deviation above the mean. Thus, nine measures were each dichotomized to reflect high vs. low risk (see Conradt et al., 2013 and Sheinkopf et al., 2007 for similar approaches) with one point assigned for each risk item present. These risk items were averaged to create an average cumulative risk index.
Table 1.
Descriptive data for individual risk items and the cumulative risk score.
| Risk-score item | M | SD | Range | Risk present (%) | Criterion for risk considered present |
|---|---|---|---|---|---|
| Prematurity | – | – | – | 4.3 | <37 weeks GA |
| Perinatal medical complications | – | – | – | 12.7 | Any medical complication |
| Marital status | – | – | – | 25.4 | Single mother status |
| Maternal education | – | – | <high school–<grad. degree | 20.3 | <College education |
| Household income | – | – | <$4999–>$200,000 | 33.8 | <$20,000 |
| Child negative emotionality | 2.53 | 1.95 | 0–8 | 35.6 | >1 SD above mean |
| Caregiver depression | 11.79 | 9.38 | 0–44 | 30.1 | CES-D score >16 (clinical cutoff) |
| Family resources | 134.08 | 16.75 | 86–174 | 15.1 | <1 SD below mean |
| Chaos | 13.52 | 3.93 | 6–24 | 17.1 | >1 SD above mean |
| Average cumulative risk scorea | 0.21 | 0.18 | 0–0.67 | – | – |
Note. GA = gestational age. CES-D = Center for Epidemiologic Studies Depression Scale.
Each dyad received 1 point for each risk item for which the criterion was met. The average of these values comprised the average cumulative risk score.
2.2.4. Problem behavior at 17 months
The Brief Infant-Toddler Social and Emotional Assessment (BITSEA; Briggs-Gowan & Carter, 2002) is a 42-item measure designed to evaluate symptoms of social and emotional problems and competence in children one to three years old. The BITSEA has demonstrated acceptable test-retest reliability (αs = 0.85–.87; Briggs-Gowan, Carter, Irwin, Wachtel, & Cicchetti, 2004). We used children’s total problem scores on the BITSEA, completed by mothers when their child was approximately 17 months old, to measure individual differences in levels of social and emotional problems. Cronbach’s alpha was greater than 0.81 for the present study.
3. Results
3.1. Preliminary analyses
The means and standard deviations of variables of interest appear in Table 2. In all analyses, baseline cortisol was centered around the sample mean to reduce nonessential multicollinearity among interaction terms (Aiken & West, 1991). Sex (0 = male, 1 = female) and major attachment classification (0 = secure, 1 = disorganized) were dummy coded.
Table 2.
Intercorrelations and descriptive statistics (N = 58).
| Measures | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. | Child gender | 0.55 | 0.50 | – | |||||
| 2. | Child age | 17.30 | 1.36 | 0.04 | – | ||||
| 3. | Cumulative risk | 0.21 | 0.16 | −0.18 | 0.15 | – | |||
| 4. | Baseline cortisol | 0.62 | 0.66 | −0.05 | −0.05 | −0.07 | – | ||
| 5. | Attachment status | 0.19 | 0.40 | −0.10 | 0.09 | 0.23* | 0.02 | – | |
| 6. | Problem behaviors | 16.83 | 8.32 | −0.36** | −0.18 | 0.24 | −0.14 | 0.25 | – |
Note. The mean for Child gender represents the proportion of participants who were female. The mean for Attachment status represents the proportion of participants who were disorganized, as opposed to secure.
p < 0.05.
p < 0.01.
We tested relations between baseline cortisol and additional covariates. There was no significant relation between baseline cortisol and gender (r = −0.05, p = 0.69), age (r = 0.03, p = 0.82), or time of saliva collection (r = 0.19, p = 0.11 for the first session and r = 0.13, p = 0.29 for the second session). Next, a simple linear regression was used to analyze the association between baseline cortisol and attachment classification. There were no significant differences in baseline cortisol between children with secure and disorganized attachment classifications, b = 0.01, p = 0.89. Importantly, this lack of association enabled our test of the diathesis-stress and susceptibility hypotheses (Belsky et al., 2007; Kraemer, Stice, Kazdin, Offord, & Kupfer, 2001).
3.2. Diathesis-stress and differential susceptibility analyses
A linear regression was used to test the main effects of cumulative risk, gender, 17-month baseline cortisol, and attachment classification (secure vs. disorganized) on 17-month problem behaviors (assessed using the BITSEA). The regression revealed no significant association between problem behavior and average cumulative risk, baseline cortisol, or attachment classification (Table 3). There was a significant association between problem behavior and gender (b = −5.43, p = 0.02), with females showing lower levels of problem behaviors. Although gender was not associated with baseline cortisol or attachment, it was retained as a covariate in the model.
Table 3.
Results of the hierarchical regression predicting problem behavior at 17 months.
| Step and predictor | b | b SE | β | t | p |
|---|---|---|---|---|---|
| Step 1: F(4,53) = 3.03, p = 0.03, R2 = 0.19 | |||||
| Intercept | 17.88 | 2.19 | 8.18 | ||
| Cumulative risk | 7.67 | 6.55 | 0.15 | 1.17 | 0.25 |
| Child gender | −5.43 | 2.10 | −0.33 | −2.59 | 0.01 |
| Attachment classification | 1.83 | 2.68 | 0.09 | 0.68 | 0.50 |
| Baseline cortisol | −1.28 | 1.07 | −0.15 | −1.19 | 0.24 |
| Step 2: F(5,52) = 3.87, p = 0.01, R2 = 0.27 | |||||
| Intercept | 17.21 | 2.11 | 8.17 | ||
| Cumulative risk | 9.90 | 6.33 | 0.20 | 1.57 | 0.12 |
| Child gender | −4.95 | 2.01 | −0.30 | −2.46 | 0.02 |
| Attachment classification | 1.84 | 2.56 | 0.09 | 0.72 | 0.48 |
| Baseline cortisol | 0.01 | 1.15 | 0.00 | 0.01 | 0.99 |
| Attachment × Baseline cortisol | −6.45 | 2.62 | −0.33 | −2.46 | 0.02 |
Next, a hierarchical linear regression was run to determine if the interaction between baseline cortisol and attachment classification predicted concurrent problem behavior at 17 months. Average cumulative risk, child gender, 17-month baseline cortisol, and attachment classification were entered on Step 1 of the regression model, and the interaction between baseline cortisol (natural-log-transformed and grand mean centered) and attachment classification (dummy coded) was entered in Step 2 (Table 3). With all predictors entered simultaneously, gender (b = −4.95, p = 0.02) and the interaction between 17-month baseline cortisol and attachment classification significantly predicted variability in 17-month problem behavior (b = −6.45, p = 0.02), ΔR2 = 0.09, p = 0.02.1
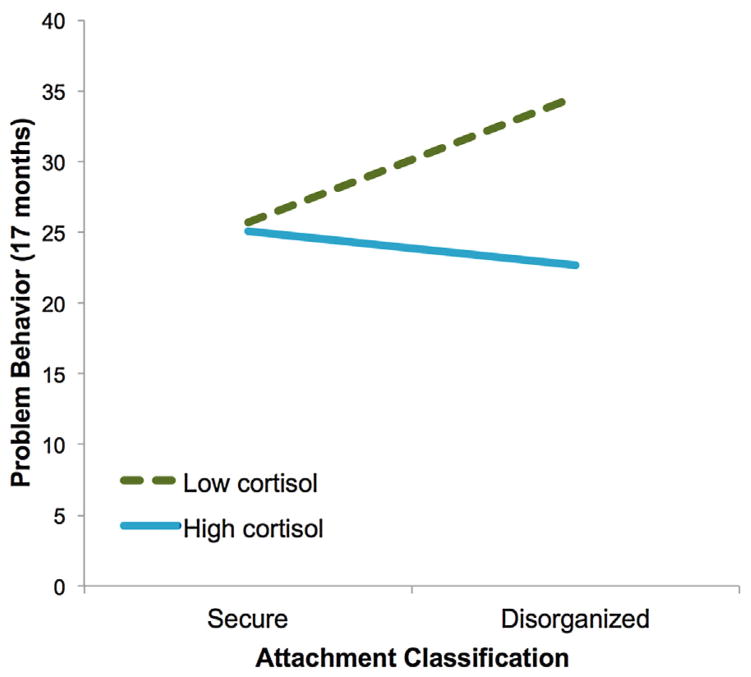
Online computational tools were used to clarify the nature of this interaction (Preacher et al., 2006; http://www.quantpsy.org/interact/mlr2.htm). These tools follow established methods for testing and probing interactions (Aiken & West, 1991; Bauer & Curran, 2004; and Cohen et al., 2003) and were used to calculate the simple slopes of baseline cortisol at 1 standard deviation above and below the mean and to compute specific values for plotting significant two-way interactions. There was no significant difference in problem behavior between children with high baseline cortisol who had secure attachment classifications or disorganized attachment classifications, b = −1.79, p = 0.38 (Fig. 1). In contrast, among children with low baseline cortisol, there was a significant difference in problem behavior depending on attachment classification such that children with a disorganized attachment classification (M = 23.00, SD = 21.21) had significantly higher problem behavior scores than children with a secure attachment classification (M = 16.10, SD = 6.38), b = 8.87, p < 0.001. Of note, the group means for children with low cortisol and disorganized attachment classification had problem-behavior scores that were above the community norms of 19 for girls and 21 for boys (Briggs-Gowan & Carter, 2002) for unselected community samples.
Fig. 1.
Problem behavior at 17 months as a function of attachment classification (secure vs. disorganized) and baseline cortisol (low = 1 SD below the mean, high = 1 SD above the mean).
Following recommendations by Roisman et al. (2012), further “regions of significance” testing (Hayes & Matthes, 2009) was conducted in order to test whether the significant interaction was more consistent with a diathesis-stress or differential susceptibility model. The region of significance defines the specific value of baseline cortisol at which the slope between attachment classification and problem behaviors moves from significance to nonsignificance. There was a lower bound of significance such that the relation between attachment classification and problem behaviors proved significant only when baseline cortisol levels were 0.70 SD below the mean for baseline cortisol levels. Stated differently, significant differences in problem behavior scores between children with secure vs. disorganized attachment emerge at baseline cortisol levels 0.70 SD below the mean. As a differential-susceptibility pattern would yield both upper and lower bounds of the region of significance within the range of baseline cortisol levels (Roisman et al., 2012), the significant interaction between baseline cortisol and attachment classification in the present sample was more consistent with diathesis-stress than differential-susceptibility models.
4. Discussion
The overarching goal of this study was to predict 17-month problem behavior levels from the interaction between baseline cortisol and attachment. Specifically, we were interested in whether this interplay was more reflective of a diathesis-stress or differential susceptibility account. Our pattern of findings is more consistent with a diathesis-stress model than a differential susceptibility model because low baseline cortisol functioned principally as a risk factor, and not also as an enhancement factor. For the differential susceptibility model to have been supported empirically, children with low baseline cortisol, compared to their peers with high baseline cortisol, would have needed to have the highest levels of problem behaviors (“for worse”) in the context of a disorganized attachment relationship and the lowest levels of problem behaviors (“for better”) in the context of a secure attachment relationship. However, our analysis reflected diathesis-stress alone because children with low baseline cortisol only fared worse than their high baseline cortisol counterparts when in a disorganized attachment context and did not evidence enhanced outcomes in the context of secure attachment. Stated differently, children with low cortisol levels at 17 months had the most concurrent problem behaviors in the context of a disorganized attachment relationship; in the context of a secure attachment relationship, children with low cortisol levels looked no different than children with high cortisol levels. Children with high cortisol levels had similar levels of problem levels in either attachment context.
Consistent with the finding that low cortisol is related to problem behavior levels, previous empirical work has linked low baseline cortisol to increased rates of externalizing behaviors (Shirtcliff et al., 2005; van Goozen et al., 2000). According to stimulation-seeking theory, persistently low cortisol levels may be experienced as an aversive physiological state (Raine, 1996). Consequently, children with low cortisol may be motivated to seek out additional stimulation, for example, by being overactive or acting out, in order to raise physiological arousal to more desired levels. In the related fearlessness theory, physiological underarousal is hypothesized to reflect low levels of fear such that children with low cortisol engage in maladaptive behaviors because they are less responsive to fear-evoking cues that should inhibit problem behaviors (Raine, 2002). In line with both stimulation-seeking and fearlessness theories, researchers have also found initial evidence that low cortisol is associated with increased sensation-seeking behaviors (Rosenblitt, Soler, Johnson, & Quadagno, 2001) and impaired fear reactivity (Kagan, Reznick, & Snidman, 1988), which may present as problem behaviors. We found that children with low cortisol levels had lower levels of problem behaviors in the context of a secure attachment relationship compared to a disorganized attachment relationship, suggesting that these children were responsive to a history of interactions with caregivers.
Importantly, our results suggest that low cortisol levels may not always be problematic. For example, for very young children with low cortisol levels, problem behaviors might not manifest when caregivers are supportive, warm, and sensitive to the child’s needs. In these secure caregiving experiences, children can rely on external resources, such as caregiver responsiveness, for socioemotional regulation. In contrast, in the context of a disorganized attachment relationship, children have less reliable external resources for regulation and support. As such, a secure attachment relationship may help buffer against the harmful effects of low cortisol levels on socioemotional behaviors.
The finding that attachment security moderates the relations between low baseline cortisol and problem behaviors may also help reconcile prior null findings of the relations between low baseline cortisol and problem behaviors (e.g., see Dahl et al., 1989; Kruesi, Schmidt, Donnelly, Hibbs, & Hamburger, 1989; Ouellet-Morin et al., 2010). For example, Ouellet-Morin et al. (2010) did not find relations between low baseline cortisol levels and externalizing or internalizing problems in a low-risk sample of toddlers. A potential source of this discrepant finding is the lack of consideration of children’s early rearing, which has been shown to be critical for both HPA and socioemotional development (Gunnar & Quevedo, 2007; Mills-Koonce & Towe-Goodman, 2012). Supportive caregiving, which may be more prevalent in lower-risk samples with more resource availability, may protect children with low cortisol levels from engaging in problem behaviors.
In contrast to children with low cortisol, children with high cortisol showed no difference in problem behavior levels in the context of a secure or disorganized attachment relationship. Although researchers have previously linked high cortisol with internalizing problems in older children (Hastings, Fortier, Utendale, Simard, & Robaey, 2009; Lopez-Duran, Kovacs, & George, 2009), we did not find evidence of this relation. One reason for the inconsistent finding may be related to the very young age group of the current sample. At 17 months of age, internalizing behaviors are less likely to be detected and identified as problematic than externalizing behaviors (Tandon, Cardeli, & Luby, 2009). So, although we attempted to survey a constellation of early problem behaviors, it is conceivable that externalizing behaviors, compared to internalizing behaviors, were more frequently reported (and/or more frequently identified as problematic). As such, relations between high cortisol levels and problem behaviors may have been more difficult to detect.
It is important to note that while the nature of the reported interaction is reflective of a diathesis-stress model, the nature of this interaction may differ in samples of differing risk, in particular, lower risk. For example, in this low-income sample, a secure attachment relationship may not have been supportive enough to detect differential susceptibility effects in children with low cortisol baseline cortisol. Children in low-income families are disproportionately exposed to abuse, neglect, household dysfunction, and other adversities (Evans, 2004). Thus, even with a secure attachment relationship, children from the present sample likely face additional adverse childhood experiences such as parental history of psychopathology and parental marital distress that mask potentially beneficial effects of low baseline cortisol. Additionally, studies on adverse childhood experiences have consistently found that multiple forms of adversity co-occur (Dong, Anda, Dube, Giles, & Felitti, 2003; Dong et al., 2004). For example, Dong et al. (2004) found that approximately 87% of individuals exposed to one adverse childhood experience reported being exposed to one additional adverse childhood experience. These studies suggest that many children with low-income backgrounds are likely exposed to multiple adverse childhood experiences. Future studies should replicate the current study in samples of lower risk to see if the diathesis-stress effects hold, or if differential susceptibility effects are detected.
Furthermore, although children with low cortisol levels and disorganized attachment status had higher levels of problem behaviors than all other groups, these results do not permit causal conclusions. In other words, we cannot infer that increasing attachment security among children with low cortisol will decrease engagement in problem behaviors because neither condition was randomly assigned. While it is certainly possible that a causal relationship lies behind the current findings, further experimental study is required to determine if this is the case or if other factors such as maternal sensitivity serve as a better explanation for differences in problem behavior levels.
Consistent with the broader literature on gender differences and problem behaviors, boys had higher levels of problem behaviors than girls (Baillargeon et al., 2007). Although gender differences in problem behaviors before two years of age are not typically examined, recent research suggest that at least some of these behaviors emerge before two years, and subsequently increase in magnitude (Baillargeon et al., 2007; Keenan & Shaw, 1997). It is likely that gender-differentiated socialization efforts by caregivers contribute to these gender differences in problem behavior levels. In any case, the detection of gender differences in problem behaviors at 17 months suggest that toddlerhood may represent an important period in which gender differences in socioemotional problems of potentially clinical significance may begin to emerge (Baillargeon et al., 2007; DelCarmen-Wiggins & Carter, 2004).
Surprisingly, our measure of cumulative risk did not directly predict problem behavior levels. This discrepancy with existing research may be partly explained by the relatively high education level (79.7% had some college education, or greater) of mothers in the current study. This type of educational background may support socioemotional competence despite exposure to other risk factors (Obradović et al., 2010). In addition, data for this study was collected in the early to mid-2000’s before the serious U.S. economic downturn beginning in 2008. Despite low household income, our somewhat more educated sample may have been benefitting from still available social services resources. Alternatively, the lack of associations between cumulative risk and behavior problems may reflect a narrower rather than broader range of risk given that our samples was generally high risk (i.e., very low income, history of maternal psychopathology, and risk for parenting problems).
Even as this research begins to answer some questions about factors shaping problem behaviors, it also raises future questions and directions to be pursued. One question is whether the effects found here are stable. For example, the predictive accuracy of very early problem behaviors is somewhat limited such that toddlers who engage in frequent problem behavior at 17 months of age often do not behave the same way one year later (Baillargeon et al., 2007). As such, it is important to examine whether the nature of interaction found in this study holds as children age. Additionally, as toddlers acquire more self-regulation skills with age, it will be important to examine whether disorganized attachment classifications still confer harm among children with lower cortisol levels. Although the stability of these interactive effects is unknown, a strength of its current study is examination of this interaction at 17-months. This time point may represent a critical period in which problem behaviors of clinical significance may begin to emerge (Baillargeon et al., 2007). As such, this time point is ideal for examining the early origins of problem behaviors and can contribute knowledge to early intervention efforts aimed at promoting socioemotional development by targeting early caregiving.
In the future, it will also be important to look at how cortisol functions with other parameters of stress physiology, including the sympathetic and parasympathetic nervous system. Recent research has begun to suggest that the specific patterns of interactions across multiple stress response systems may create discrete forms of vulnerability or susceptibility (Hinnant & El-Sheikh, 2013; Laurent, Ablow, & Measelle, 2012; Obradovicí, 2012). For example, findings from two empirical investigations of the interactions between the different stress systems suggest that symmetrical activity in the two systems resulting in hypoarousal (e.g., low sympathetic nervous system and HPA activity, or coinhibition) or hyperarousal (high sympathetic nervous system and HPA activity, or coactivation) leaves children most susceptible to behavior problems (El-Sheikh, Erath, Buckhalt, Granger, & Mize, 2008; Gordis, Granger, Susman, & Trickett, 2006). Children least at risk for behavioral problems had moderate activity in both systems, or asymmetrical activity in the two systems (e.g., reciprocal activation). Thus, future studies should examine measures of autonomic and HPA activity, both alone and in combination, as possible sources of risk or protection in high-risk samples.
Limitations of the current study include the moderate sample size, limited racial/ethnic heterogeneity in the sample, and reliance on single reporters of problem behaviors. Additionally, twelve children were missing baseline cortisol data, raising the possibility that there could be systematic differences in children with and without cortisol data. However, comparison of children with and without baseline cortisol data on a variety of demographic, risk, and problem behavior variables revealed no significant differences between these groups. Furthermore, although we attempted to control for potential confounds for cortisol and to increase reliability by averaging initial saliva samples across two days, we acknowledge that multiple baseline samples, both at home and in the laboratory, would give a more stable estimate of what we are calling baseline cortisol. Future research should collect multiple measures of cortisol across the day to more fully characterize children’s resting cortisol levels. Finally, attachment was used as a proxy for the interaction history between child and parent because of prospective research indicating that early parenting quality is predictive of attachment (see meta-analysis by Wolff & Ijzendoorn, 1997; Grossman, Grossmann, Spangler, Suess, & Unzner, 1985; Isabella, 1993). However, given somewhat inconsistent associations found between measures of early caregiving and later attachment security (Bigelow et al., 2010; Goldsmith & Alansky, 1987), findings from the present study should be interpreted cautiously and future work should also how examine the interaction between baseline cortisol and other measures of caregiving quality, such as maternal sensitivity relate to early problem behaviors.
The present study begins to identify physiological and contextual factors that influence a child’s behavior. Low baseline cortisol was identified as a risk factor for problem behaviors under conditions of disorganized attachment. However, secure attachment relationships appeared to buffer these children from problem behaviors. Given that early problem behaviors set children on poor trajectories throughout the lifespan, identification of children most vulnerable to developing problem behaviors gives us the potential to foster more successful development.
Footnotes
As suggested by a reviewer, we completed additional analyses combining resistant and avoidant children (i.e., secure vs. resistant and avoidant). A hierarchical linear regression revealed no significant association between problem behavior or any variables of interest. The interaction between 17-month baseline cortisol and attachment classification (secure vs. resistant and avoidant) did not significantly predict variability in 17-month problem behavior (b = −2.39, p = 0.44), though the effect size suggests that this effect might have reached significance in a larger sample.
References
- Aiken LS, West SG. Multiple regression: testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Ainsworth MD, Blehar MC, Waters E, Wall S. Patterns of attachment: A psychological study of the strange situation. Hillsdale, NJ: Erlbaum; 1978. [Google Scholar]
- Alink LR, van IJzendoorn MH, Bakermans-Kranenburg MJ, Mesman J, Juffer F, Koot HM. Cortisol and externalizing behavior in children and adolescents: Mixed meta-analytic evidence for the inverse relation of baseline cortisol and cortisol reactivity with externalizing behavior. Developmental Psychobiology. 2008;50:427–450. doi: 10.1002/dev.20300. http://dx.doi.org/10.1002/dev.20300. [DOI] [PubMed] [Google Scholar]
- Alkon A, Wolff B, Boyce WT. Poverty, stress, and autonomic reactivity. In: Maholmes V, King RB, editors. Oxford handbook on child development and poverty. New York, NY: Oxford University Press; 2012. pp. 221–239. [Google Scholar]
- Baharudin R, Luster T. Factors related to the quality of the home environment and children’s achievement. Journal of Family Issues. 1998;19:375–403. http://dx.doi.org/10.1177/019251398019004002. [Google Scholar]
- Baillargeon RH, Normand CL, Séguin JR, Zoccolillo M, Japel C, Pérusse D, et al. The evolution of problem and social competence behaviors during toddlerhood: A prospective population-based cohort survey. Infant Mental Health Journal. 2007;28:12–38. doi: 10.1002/imhj.20120. http://dx.doi.org/10.1002/imhj.20120. [DOI] [PubMed] [Google Scholar]
- Bakermans-Kranenburg MJ, van Ijzendoorn MH. Differential susceptibility to rearing environment depending on dopamine-related genes: New evidence and a meta-analysis. Development and Psychopathology. 2011;23:39–52. doi: 10.1017/S0954579410000635. http://dx.doi.org/10.1017/S0954579410000635. [DOI] [PubMed] [Google Scholar]
- Bachman HJ, Coley RL, Carrano J. Maternal relationship instability influences on children’s emotional and behavioral functioning in low-income families. Journal of Abnormal Child Psychology. 2011;39:1149–1161. doi: 10.1007/s10802-011-9535-1. http://dx.doi.org/10.1007/s10802-011-9535-1. [DOI] [PubMed] [Google Scholar]
- Barnett D, Ganiban J, Cicchetti D. Maltreatment, negative expressivity, and the development of type D attachments from 12 to 24 months of age. Monographs of the Society for Research in Child Development. 1999;64(Serial No. 258):97–118. doi: 10.1111/1540-5834.00035. [DOI] [PubMed] [Google Scholar]
- Barnett MA, Gustafsson H, Deng M, Mills-Koonce WR, Cox M. Bidirectional associations among sensitive parenting, language development, and social competence. Infant and Child Development. 2012;21:374–393. doi: 10.1002/icd.1750. http://dx.doi.org/10.1002/icd.1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer DJ, Curran PJ. The integration of continuous and discrete latent variable models: Potential problems and promising opportunities. Psychological Methods. 2004;9:3–29. doi: 10.1037/1082-989X.9.1.3. http://dx.doi.org/10.1037/1082-989X.9.1.3. [DOI] [PubMed] [Google Scholar]
- Belsky J, Bakermans-Kranenburg MJ, Van IJzendoorn MH. For better and for worse differential susceptibility to environmental influences. Current Directions in Psychological Science. 2007;16:300–304. http://dx.doi.org/10.1111/j.1467-8721.2007.00525.x. [Google Scholar]
- Belsky J, Pluess M. Beyond diathesis stress: Differential susceptibility to environmental influences. Psychological Bulletin. 2009;135:885–908. doi: 10.1037/a0017376. http://dx.doi.org/10.1037/a0017376. [DOI] [PubMed] [Google Scholar]
- Belsky J, Pluess M. Differential susceptibility to long-term effects of quality of child care on externalizing behavior in adolescence? International Journal of Behavioral Development. 2012;36:2–10. http://dx.doi.org/10.1177/0165025411406855. [Google Scholar]
- Bernard K, Dozier M. Examining infants’ cortisol responses to laboratory tasks among children varying in attachment disorganization: Stress reactivity or return to baseline? Developmental Psychology. 2010;46:1771–1778. doi: 10.1037/a0020660. http://dx.doi.org/10.1037/a0020660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bigelow AE, MacLean K, Proctor J, Myatt T, Gillis R, Power M. Maternal sensitivity throughout infancy: Continuity and relation to attachment security. Infant Behavior and Development. 2010;33:50–60. doi: 10.1016/j.infbeh.2009.10.009. [DOI] [PubMed] [Google Scholar]
- Blair C, Granger DA, Willoughby M, Mills-Koonce R, Cox M, Greenberg MT, Fortunato CK. Salivary cortisol mediates effects of poverty and parenting on executive functions in early childhood. Child Development. 2011;82:1970–1984. doi: 10.1111/j.1467-8624.2011.01643.x. http://dx.doi.org/10.1111/j.1467-8624.2011.01643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyce WT, Ellis BJ. Biological sensitivity to context: An evolutionary-developmental theory of the origins and functions of stress reactivity. Development and Psychopathology. 2005;13:271–301. doi: 10.1017/s0954579405050145. http://dx.doi.org/10.1017/S0954579405050145. [DOI] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS. Brief Infant-Toddler Social and Emotional Assessment (BITSEA) manual (Version 2.0) New Haven, CT: Yale University; 2002. [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Irwin JR, Wachtel K, Cicchetti DC. The Brief Infant-Toddler Social and Emotional Assessment: Screening for social-emotional problems and delays in competence. Journal of Pediatric Psychology. 2004;29:133–155. doi: 10.1093/jpepsy/jsh017. http://dx.doi.org/10.1093/jpepsy/jsh017. [DOI] [PubMed] [Google Scholar]
- Brooks-Gunn J, Duncan GJ. The effects of poverty on children. The Future of Children. 1997:55–71. http://dx.doi.org/10.2307/1602387. [PubMed]
- Chang H, Shelleby EC, Cheong J, Shaw DS. Cumulative risk, negative emotionality, and emotion regulation as predictors of social competence in transition to school: A mediated moderation model. Social Development. 2012;21:780–800. http://dx.doi.org/10.1111/j.1467-9507.2011.00648.x. [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3. Mahwah, NJ: Erlbaum; 2003. [Google Scholar]
- Conradt E, Measelle J, Ablow JC. Poverty, problem behavior, and promise: Differential susceptibility among infants reared in poverty. Psychological Science. 2013;24:235–242. doi: 10.1177/0956797612457381. http://dx.doi.org/10.1177/0956797612457381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crittenden PM. Relationships at risk. In: Belsky J, Nezworski T, editors. Clinical implications of attachment. Hillsdale, NJ: Erlbaum; 1988. pp. 136–174. [Google Scholar]
- Dahl RE, Puig-Antich J, Ryan N, Nelson B, Novacenko H, Twomey J, et al. Cortisol secretion in adolescents with major depressive disorder. Acta Psychiatrica Scandinavia. 1989;80:18–21. doi: 10.1111/j.1600-0447.1989.tb01295.x. http://dx.doi.org/10.1111/j.1600-0447.1989.tb01295.x. [DOI] [PubMed] [Google Scholar]
- De Wolff MS, van IJzendoorn MH. Sensitivity and attachment: A meta-analysis on parental antecedents of infant attachment. Child Development. 1997;68:571–591. [PubMed] [Google Scholar]
- Dong M, Anda RF, Dube SR, Giles WH, Felitti VJ. The relationship of exposure to childhood sexual abuse to other forms of abuse, neglect and household dysfunction during childhood. Child Abuse & Neglect. 2003;27:625–639. doi: 10.1016/s0145-2134(03)00105-4. [DOI] [PubMed] [Google Scholar]
- Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, et al. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect. 2004;28:771–784. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Duncan GJ, Brooks-Gunn J. Family poverty, welfare reform, and child development. Child Development. 2000;71:188–196. doi: 10.1111/1467-8624.00133. http://dx.doi.org/10.1111/1467-8624.00133. [DOI] [PubMed] [Google Scholar]
- Dunst CJ, Leet HE. Measuring the adequacy of resources in households with young children. Child: Care Health and Development. 1987;13:111–125. doi: 10.1111/j.1365-2214.1987.tb00528.x. http://dx.doi.org/10.1111/j.1365-2214.1987.tb00528.x. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Sulik MJ, Spinrad TL, Edwards A, Eggum ND, Liew J, et al. Differential susceptibility and the early development of aggression: Interactive effects of respiratory sinus arrhythmia and environmental quality. Developmental Psychology. 2012;48:755–768. doi: 10.1037/a0026518. http://dx.doi.org/10.1037/a0026518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Erath SA, Buckhalt JA, Granger DA, Mize J. Cortisol and children’s adjustment: the moderating role of sympathetic nervous system activity. Journal of Abnormal Child Psychology. 2008;36:601–611. doi: 10.1007/s10802-007-9204-6. http://dx.doi.org/10.1007/s10802-007-9204-6. [DOI] [PubMed] [Google Scholar]
- Engle PL, Black MM. The effect of poverty on child development and educational outcomes. Annals of the New York Academy of Sciences. 2008;1136:243–256. doi: 10.1196/annals.1425.023. http://dx.doi.org/10.1196/annals.1425.023. [DOI] [PubMed] [Google Scholar]
- Evans GW. The environment of childhood poverty. American Psychologist. 2004;59:77–92. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]
- Evans GW, Chen E, Miller G, Seeman T. How poverty gets under the skin: A life course perspective. In: Maholmes V, King RB, editors. Oxford handbook on child development and poverty. New York, NY: Oxford University Press; 2012. pp. 13–36. [Google Scholar]
- Gartstein MK, Rothbart MK. Studying infant temperament via the revised Infant Behavior Questionnaire. Infant Behavior & Development. 2003;26:64–86. http://dx.doi.org/10.1016/S0163-6383(02)00169-8. [Google Scholar]
- Gordis EB, Granger DA, Susman EJ, Trickett PK. Asymmetry between salivary cortisol and alpha-amylase reactivity to stress: Relation to aggressive behavior in adolescents. Psychoneuroendocrinology. 2006;31:976–987. doi: 10.1016/j.psyneuen.2006.05.010. http://dx.doi.org/10.1016/j.psyneuen.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Granger DA, Stansbury K, Henker B. Preschoolers’ behavioral and neuroendocrine responses to social challenge. Merrill-Palmer Quarterly. 1994;40:190–211. [Google Scholar]
- Granger DA, Weisz JR, McCracken JT, Ikeda SC, Douglas P. Reciprocal influences among adrenocortical activation, psychosocial processes, and the behavioral adjustment of clinic-referred children. Child Development. 1996;67:3250–3262. [PubMed] [Google Scholar]
- Gross H, Shaw DS, Burwell RA, Nagin DS. Transactional processes in child disruptive behavior and maternal depression: A longitudinal study from early childhood to adolescence. Development and Psychopathology. 2009;21:139–156. doi: 10.1017/S0954579409000091. http://dx.doi.org/10.1017/S0954579409000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman K, Grossmann KE, Spangler G, Suess G, Unzner L. Maternal sensitivity and newborns’ orientation responses as related to quality of attachment in northern Germany. In: Bretherton I, Waters E, editors. Growing point of attachment theory and research. 1985. pp. 233–256. 50: Monographs of the Society for Research in Child Development. [PubMed] [Google Scholar]
- Gunnar M, Quevedo K. The neurobiology of stress and development. Annual Review of Psychology. 2007;58:145–173. doi: 10.1146/annurev.psych.58.110405.085605. http://dx.doi.org/10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- Halligan SL, Cooper PJ, Fearon P, Wheeler SL, Crosby M, Murray L. The longitudinal development of emotion regulation capacities in children at risk for externalizing disorders. Development and Psychopathology. 2013;25:391–406. doi: 10.1017/S0954579412001137. http://dx.doi.org/10.1017/S0954579412001137. [DOI] [PubMed] [Google Scholar]
- Hastings PD, Fortier I, Utendale WT, Simard LR, Robaey P. Adrenocortical functioning in boys with attention-deficit/hyperactivity disorder: examining subtypes of ADHD and associated comorbid conditions. Journal of Abnormal Child Psychology. 2009:565–578. doi: 10.1007/s10802-008-9292-y. http://dx.doi.org/10.1007/s10802-008-9292-y. [DOI] [PubMed]
- Hayes AF, Matthes J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behavior Research Methods. 2009;41:924–936. doi: 10.3758/BRM.41.3.924. http://dx.doi.org/10.3758/BRM.41.3.924. [DOI] [PubMed] [Google Scholar]
- Hertzman C. Putting the concept of biological embedding in historical perspective. Proceedings of the National Academy of Sciences. 2012;109:17160–17167. doi: 10.1073/pnas.1202203109. http://dx.doi.org/10.1073/pnas.1202203109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesse E, Main M. Frightened, threatening, and dissociative parental behavior in low-risk samples: Description, discussion, and interpretations. Development and Psychopathology. 2006 doi: 10.1017/S0954579406060172. [DOI] [PubMed] [Google Scholar]
- Hinnant JB, El-Sheikh M. Co-development of externalizing and internalizing symptoms in middle to late childhood: Sex, baseline respiratory sinus arrhythmia, and respiratory sinus arrhythmia reactivity as predictors. Development and Psychopathology. 2013;25:419–436. doi: 10.1017/S0954579412001150. http://dx.doi.org/10.1017/S0954579412001150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isabella RA. Origins of attachment: Maternal interactive behavior across the first year. Child Development. 1993;64:605–621. doi: 10.1111/j.1467-8624.1993.tb02931.x. http://dx.doi.org/10.1111/j.1467-8624.1993.tb02931.x. [DOI] [PubMed] [Google Scholar]
- Kagan J, Reznick JS, Snidman N. Biological bases of childhood shyness. Science. 1988;240:167–171. doi: 10.1126/science.3353713. http://dx.doi.org/10.1126/science.3353713. [DOI] [PubMed] [Google Scholar]
- Keenan K, Shaw D. Developmental and social influences on young girls’ early problem behavior. Psychological Bulletin. 1997;121:95–113. doi: 10.1037/0033-2909.121.1.95. http://dx.doi.org/10.1037/0033-2909.121.1.95. [DOI] [PubMed] [Google Scholar]
- Kochanska G, Kim S, Koenig Nordling J. Challenging circumstances moderate the links between mothers’ personality traits and their parenting in low-income families with young children. Journal of Personality and Social Psychology. 2012;103:1040–1049. doi: 10.1037/a0030386. http://dx.doi.org/10.1037/a0030386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. http://dx.doi.org/10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Kruesi MJP, Schmidt ME, Donnelly H, Hibbs ED, Hamburger SP. Urinary free cortisol output and disruptive behavior in children. Journal of the American Academy of Child and Adolescent Psychiatry. 1989;28:441–443. doi: 10.1097/00004583-198905000-00024. [DOI] [PubMed] [Google Scholar]
- Laurent HK, Ablow JC, Measelle J. Taking stress response out of the box: Stability, discontinuity, and temperament effects on HPA and SNS across social stressors in mother-infant dyads. Developmental Psychology. 2012;48:1–8. doi: 10.1037/a0025518. http://dx.doi.org/10.1037/a0025518. [DOI] [PubMed] [Google Scholar]
- Levine S. Developmental determinants of sensitivity and resistance to stress. Psychoneuroendocrinology. 2005;30:939–946. doi: 10.1016/j.psyneuen.2005.03.013. http://dx.doi.org/10.1016/j.psyneuen.2005.03.013. [DOI] [PubMed] [Google Scholar]
- Lopez-Duran NL, Kovacs M, George CJ. Hypothalamic-pituitary-adrenal axis dysregulation in depressed children and adolescents: A meta-analysi. Psychoneuroendocrinology. 2009;34:1272–1283. doi: 10.1016/j.psyneuen.2009.03.016. http://dx.doi.org/10.1016/j.psyneuen.2009.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luecken LJ, Lemery KS. Early caregiving and physiological stress responses. Clinical Psychology Review. 2004;24:171–191. doi: 10.1016/j.cpr.2004.01.003. http://dx.doi.org/10.1016/j.cpr.2004.01.003. [DOI] [PubMed] [Google Scholar]
- Lupien SJ, King S, Meaney MJ, McEwen BS. Child’s stress hormone levels correlate with mother’s socioeconomic status and depressive state. Biological Psychiatry. 2000;48:976–980. doi: 10.1016/s0006-3223(00)00965-3. http://dx.doi.org/10.1016/S0006-3223(00)00965-3. [DOI] [PubMed] [Google Scholar]
- Matheny AP, Jr, Wachs TD, Ludwig JL, Phillips K. Bringing order out of chaos: Psychometric characteristics of the confusion, hubbub, and order scale. Journal of Applied Developmental Psychology. 1995;16:429–444. http://dx.doi.org/10.1016/0193-3973(95)90028-4. [Google Scholar]
- McEwen BS, Stellar E. Stress and the individual: mechanisms leading to disease. Archives of Internal Medicine. 1993;153:2093–2101. http://dx.doi.org/10.1001/archinte.1993.00410180039004. [PubMed] [Google Scholar]
- McLeod JD, Fettes DL. Trajectories of failure: The educational careers of children with mental health problems. American Journal of Sociology. 2007;113:653–701. doi: 10.1086/521849. http://dx.doi.org/10.1086/521849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLoyd VC. Socioeconomic disadvantage and child development. American Psychologist. 1998;53:185–204. doi: 10.1037//0003-066x.53.2.185. http://dx.doi.org/10.1037/0003-066X.53.2.185. [DOI] [PubMed] [Google Scholar]
- Meins E, Centifanti LCM, Fernyhough C, Fishburn S. Maternal mind-mindedness and children’s behavioral difficulties: Mitigating the impact of low socioeconomic status. Journal of Abnormal Child Psychology. 2013;41:543–553. doi: 10.1007/s10802-012-9699-3. http://dx.doi.org/10.1007/s10802-012-9699-3. [DOI] [PubMed] [Google Scholar]
- Mills-Koonce WR, Towe-Goodman N. The effects of poverty on children’s HPA functioning. In: Maholmes V, King RB, editors. Oxford handbook on child development and poverty. New York, NY: Oxford University Press; 2012. pp. 387–403. [Google Scholar]
- Obradovicí J. How can the study of physiological reactivity contribute to our understanding of adversity and resilience processes in development? Development and Psychopathology. 2012;24:371–387. doi: 10.1017/S0954579412000053. http://dx.doi.org/10.1017/S0954579412000053. [DOI] [PubMed] [Google Scholar]
- Obradović J, Bush NR, Boyce WT. The interactive effect of marital conflict and stress reactivity on externalizing and internalizing symptoms: The role of laboratory stressors. Development and Psychopathology. 2011;23:101–114. doi: 10.1017/S0954579410000672. http://dx.doi.org/10.1017/S0954579410000672. [DOI] [PubMed] [Google Scholar]
- Obradović J, Bush NR, Stamperdahl J, Adler NE, Boyce WT. iological sensitivity to context: The interactive effects of stress reactivity and family adversity on socioemotional behavior and school readiness. Child Development. 2010;81:270–289. doi: 10.1111/j.1467-8624.2009.01394.x. http://dx.doi.org/10.1111/j.1467-8624.2009.01394.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouellet-Morin I, Tremblay RE, Boivin M, Meaney M, Kramer M, Côté SM. Diurnal cortisol secretion at home and in child care: A prospective study of 2-year-old toddlers. Journal of Child Psychology and Psychiatry. 2010;51:295–303. doi: 10.1111/j.1469-7610.2009.02167.x. http://dx.doi.org/10.1111/j.1469-7610.2009.02167.x. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31:437–448. [Google Scholar]
- Propper C. The early development of vagal tone: Effects of poverty and elevated contextual risk. In: Maholmes V, King RB, editors. Oxford handbook on child development and poverty. New York, NY: Oxford University Press; 2012. pp. 103–123. [Google Scholar]
- Radloff LS. The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurements. 1977;1:385–401. http://dx.doi.org/10.1177/014662167700100306. [Google Scholar]
- Raine A. Autonomic nervous system activity and violence. In: Stoff DM, Cairns RF, editors. The neurobiology of clinical aggression. Hillsdale, NJ: Earlbaum; 1996. [Google Scholar]
- Raine A. Biosocial studies of antisocial and violent behavior in children and adults: A review. Journal of Abnormal Child Psychology. 2002;30:311–326. doi: 10.1023/a:1015754122318. [DOI] [PubMed] [Google Scholar]
- Raver CC. Placing emotional self-regulation in sociocultural and socioeconomic contexts. Child Development. 2004;75:346–353. doi: 10.1111/j.1467-8624.2004.00676.x. [DOI] [PubMed] [Google Scholar]
- Roisman GI, Newman DA, Fraley RC, Haltigan JD, Groh AM, Haydon KC. Distinguishing differential susceptibility from diathesis-stress: Recommendations for evaluating interaction effects. Development and Psychopathology. 2012;24:389–409. doi: 10.1017/S0954579412000065. http://dx.doi.org/10.1017/S0954579412000065. [DOI] [PubMed] [Google Scholar]
- Rosenblitt JC, Soler H, Johnson SE, Quadagno DM. Sensation seeking and hormones in men and women: exploring the link. Hormones and Behavior. 2001;40:396–402. doi: 10.1006/hbeh.2001.1704. http://dx.doi.org/10.1006/hbeh.2001.1704. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, Seifer R, Barocas R, Zax M, Greenspan S. Intelligence quotient scores of 4-year-old children: social-environmental risk factors. Pediatrics. 1987;79:343–350. [PubMed] [Google Scholar]
- Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocrine Reviews. 2000;21:55–89. doi: 10.1210/edrv.21.1.0389. http://dx.doi.org/10.1210/er.21.1.55. [DOI] [PubMed] [Google Scholar]
- Sheinkopf SJ, Lagasse LL, Lester BM, Liu J, Seifer R, Bauer CR, Das A. Vagal tone as a resilience factor in children with prenatal cocaine exposure. Development and Psychopathology. 2007;19:649–673. doi: 10.1017/S0954579407000338. http://dx.doi.org/10.1017/S0954579407000338. [DOI] [PubMed] [Google Scholar]
- Shirtcliff EA, Granger DA, Booth A, Johnson D. Low salivary cortisol levels and externalizing behavior problems in youth. Development and Psychopathology. 2005;17:167–184. doi: 10.1017/s0954579405050091. http://dx.doi.org/10.1017/S0954579405050091. [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities. Journal of the American Medical Association. 2009;301:2252–2259. doi: 10.1001/jama.2009.754. http://dx.doi.org/10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- Spinrad TL, Eisenberg N, Gaertner B, Popp T, Smith CL, Kupfer A, Hofer C. Relations of maternal socialization and toddlers’ effortful control to children’s adjustment and social competence. Developmental Psychology. 2007;43:1170–1186. doi: 10.1037/0012-1649.43.5.1170. http://dx.doi.org/10.1037/0012-1649.43.5.1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi T, Ikeda K, Ishikawa M, Tsukasaki T, Nakama D, Tanida S, Kameda T. Social stress-induced cortisol elevation acutely impairs social memory in humans. Neuroscience Letters. 2004;363:125–130. doi: 10.1016/j.neulet.2004.03.062. http://dx.doi.org/10.1016/j.neulet.2004.03.062. [DOI] [PubMed] [Google Scholar]
- Tandon M, Cardeli E, Luby J. Internalizing disorders in early childhood: A review of depressive and anxiety disorders. Child and Adolescent Psychiatric Clinics of North America. 2009;18:593–610. doi: 10.1016/j.chc.2009.03.004. http://dx.doi.org/10.1016/j.chc.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tryphonopoulos PD, Letourneau N, Azar R. Approaches to salivary cortisol collection and analysis in infants. Biological Research for Nursing. 2014;16:398–408. doi: 10.1177/1099800413507128. http://dx.doi.org/10.1177/1099800413507128 [Advance online publication] [DOI] [PubMed] [Google Scholar]
- Turney K. Pathways of disadvantage: Explaining the relationship between maternal depression and children’s problem behaviors. Social Science Research. 2012;41:1546–1564. doi: 10.1016/j.ssresearch.2012.06.003. http://dx.doi.org/10.1016/j.ssresearch.2012.06.003. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Income and Poverty in the United States: 2015. 2016 [Retrieved from: November 21 2016]. http://www.census.gov/library/publications/2016/demo/p60-256.html.
- van Goozen SHM, Matthys W, Cohen-Kettenis PT, Buitelaar JK, Van Engeland H. Hypothalamic-pituitary-adrenal axis and autonomic nervous system activity in disruptive children and matched controls. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:1438–1445. doi: 10.1097/00004583-200011000-00019. http://dx.doi.org/10.1097/00004583-200011000-00019. [DOI] [PubMed] [Google Scholar]
- van IJzendoorn MH, Schuengel C, Bakermans-Kranenburg MJ. Disorganized attachment in early childhood: Meta-analysis of precursors, concomitants, and sequelae. Development and Psychopathology. 1999;11:225–250. doi: 10.1017/s0954579499002035. [DOI] [PubMed] [Google Scholar]
- van Oort FVA, van der Ende J, Wadsworth ME, Verhulst FC, Achenbach TM. Cross-national comparison of the link between socioeconomic status and emotional and behavioral problems in youths. Social Psychiatry and Psychiatric Epidemiology. 2011;46:167–172. doi: 10.1007/s00127-010-0191-5. http://dx.doi.org/10.1007/s00127-010-0191-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff MS, Ijzendoorn MH. Sensitivity and attachment: A meta-analysis on parental antecedents of infant attachment. Child Development. 1997;68:571–591. http://dx.doi.org/10.1111/j.1467-8624.1997.tb04218.x. [PubMed] [Google Scholar]
- Zuckerman M. Vulnerability to psychopathology: A biosocial model. Washington, DC: American Psychological Association; 1999. http://dx.doi.org/10.1037/10316-000. [Google Scholar]