Abstract
IMPORTANCE
Health care spending on children in the United States continues to rise, yet little is known about how this spending varies by condition, age and sex group, and type of care, nor how these patterns have changed over time.
OBJECTIVE
To provide health care spending estimates for children and adolescents 19 years and younger in the United States from 1996 through 2013, disaggregated by condition, age and sex group, and type of care.
EVIDENCE REVIEW
Health care spending estimates were extracted from the Institute for Health Metrics and Evaluation Disease Expenditure 2013 project database. This project, based on 183 sources of data and 2.9 billion patient records, disaggregated health care spending in the United States by condition, age and sex group, and type of care. Annual estimates were produced for each year from 1996 through 2013. Estimates were adjusted for the presence of comorbidities and are reported using inflation-adjusted 2015 US dollars.
FINDINGS
From 1996 to 2013, health care spending on children increased from $149.6 (uncertainty interval [UI], 144.1–155.5) billion to $233.5 (UI, 226.9–239.8) billion. In 2013, the largest health condition leading to health care spending for children was well-newborn care in the inpatient setting. Attention-deficit/hyperactivity disorder and well-dental care (including dental check-ups and orthodontia) were the second and third largest conditions, respectively. Spending per child was greatest for infants younger than 1 year, at $11 741 (UI, 10 799–12 765) in 2013. Across time, health care spending per child increased from $1915 (UI, 1845–1991) in 1996 to $2777 (UI, 2698–2851) in 2013. The greatest areas of growth in spending in absolute terms were ambulatory care among all types of care and inpatient well-newborn care, attention-deficit/hyperactivity disorder, and asthma among all conditions.
CONCLUSIONS AND RELEVANCE
These findings provide health policy makers and health care professionals with evidence to help guide future spending. Some conditions, such as attention-deficit/hyperactivity disorder and inpatient well-newborn care, had larger health care spending growth rates than other conditions.
In 2014, the United States spent $2.9 trillion on health care, comprising more than 17% of US gross domestic product, or $9255 per person.1 More than 1 in 4 Americans is a child or adolescent younger than 20 years, representing more than 80 million individuals and potential users of health care.2 Because children and adolescents receive a disproportionately small percentage of health care spending, and because health care investments at this age can be integral in ensuring a healthy life, it is important that resources are allocated efficiently across age groups, health conditions, and types of care. To determine if the allocation is efficient, a basic understanding of current spending allocations is essential—how much is being spent on children’s health care, which conditions are leading to health care, and how trends evolve over time.
Several studies have estimated US children’s health care or medical spending by age, but most lack national representativeness, focus on one type of insurance status, or only cover a few years.3–9 Moreover, few have split spending across both health condition and type of care.3,10–13 The Health Care Cost Institute has produced 4 annual reports that assess health care spending for children, but their focus was on children who are covered by employer-based insurance. Thus, the reports excluded children covered by state and federally funded health insurance programs, which have expanded since the introduction of the State Children’s Health Insurance Program in 1997.3 In addition to these, the bulk of health care spending and utilization research were cost of illness studies that focused on 1 or a few specific health conditions.14–18 While these studies are useful to policy makers to assess focused trends over time, they do not provide an overall view of total health care spending on children, allow for comparisons across diseases, or ensure that the total spending across all conditions reflects official US health care spending estimates.
The objective of this study was to estimate annual health care spending from 1996 to 2013 for children in the United States, regardless of payer or health care professional, by splitting estimates into 10 age and sex groups, 150 conditions, and 6 types of care.
Methods
Conceptual Framework and Data Sources
Data were extracted from the Institute for Health Metrics and Evaluation (IHME) Disease Expenditure 2013 project database.19 The estimates generated by this project have been used, to our knowledge, for only 1 research article prior to this one.19 These estimates split US health care spending by condition age, sex, and type of care, for each year from 1996 to 2013 (eAppendix 1 in the Supplement). This project generates estimates from 183 sources of data, including household surveys, insurance claims, administrative records, and government budgets and reports. Together, these sources of data contain more than 2.9 billion records (eAppendix 2 in the Supplement). This project received review and approval from the University of Washington Institutional Review Board, and because data were used from a deidentified database, informed consent was waived.
The overarching strategy of the IHME Disease Expenditure 2013 project was to use nationally representative encounter-level data to estimate spending by condition, age, and sex for each type of care. An encounter is an interaction with the medical system, such as an inpatient or nursing facility admission; an emergency department, ambulatory, or dental care visit; or the purchase of a prescribed pharmaceutical.20 Encounter-level data reporting health care spending, patient age and sex, type of care, and patient diagnoses and comorbidities were extracted from insurance claims, facility surveys, and household surveys. Spending on encounters with the same primary diagnosis, age, sex, year, and type of care were aggregated. Sampling weights were used to ensure that the estimates remained nationally representative.
These data are scaled to reflect the official US government estimate of personal health care spending for each type of care from 1996 to 2013. These official estimates are made by the US Centers for Medicare and Medicaid Services and are reported in the National Health Expenditure Accounts (NHEA). Personal health care spending, which excludes public health activities, investment, and 2 categories tracking administrative costs associated with government health insurance such as Medicare and Medicaid, comprised 89.5% of total health care spending in 2013.21
The NHEA divides total personal health care spending into 10 mutually exclusive types of care, which include hospital care, physician and clinical services, nursing facility care, and pharmaceutical spending, among others. To better align the NHEA personal health care spending accounts with patients’ encounter-level data, spending fractions from the Medical Expenditure Panel Survey and methods described by Roehrig22 were used to split these 10 categories into the 6 types of personal health care tracked in this study: inpatient care, ambulatory care, emergency departments, nursing facilities care, dental care, and retail pharmaceuticals.23 Ambulatory care included health care in urgent care facilities, and pharmaceuticals only included prescribed medicine that was purchased in a retail setting rather than that provided during an inpatient or ambulatory care visit. Together, health care spending incurred through these 6 types of care constituted between 84.0% and 85.2% of annual personal health care spending from 1996 to 2013.21 Spending on over-the-counter pharmaceuticals, nondurable and durable medical devices, and home health made up the remainder of the personal health care spending.
Estimating Spending by Age, Sex, and Condition
After the type of care was determined, the encounter-level data were split by sex and age. Spending was placed into 5 age groups: younger than 1 year, 1 to 4 years, 5 to 9 years, 10 to 14 years, and 15 to 19 years. Finally, these data were also split across 150 health conditions (eAppendix 3 in the Supplement). Of the 150 conditions, 135 were based on the disease categories used in the Global Burden of Disease 2013 study.24 The remaining 15 conditions are associated with large amounts of health care spending but are not underlying causes of health burden and are thus excluded from the Global Burden of Disease study.24 Examples of these additional categories include well-person visits, routine dental visits, and pregnancy and postpartum care.
The spending estimates for each type of care were scaled to reflect the adjusted annual health care spending reported by the NHEA. This procedure is common among health care spending researchers, as no single data source offers a census of spending in all health care settings.22,25 This scaling procedure assumes that the spending captured in the data used for this study was representative of spending in the total population. The encounter-level spending estimates were adjusted so that all spending estimates are reported in inflation-adjusted 2015 US dollars.26
Addressing Data Nonrepresentativeness
On average, comorbidities make health care more complicated and moreexpensive.27–29 Attributing all of the resources used in a health care encounter to the primary diagnosis biases the estimates and ignores type and intensity of care provided.20 To account for the presence of comorbidities, a regression-based method was used to adjust health care spending.19 As a consequence, conditions that are routinely accompanied by costly comorbidities coded as secondary diagnoses decreased after the comorbidity adjustment, while conditions routinely considered comorbidities increased after adjustment. Thus, the adjusted spending estimates reflect the spending attributed to each condition, rather than simply tracking spending attributed to primary diagnoses (eAppendix 4 in the Supplement).
In addition to this comorbidity adjustment, several other adjustments were performed to improve the accuracy of spending estimates (eAppendix 4 in the Supplement). First, health care charges, rather than spending, were reported in a primary data source used to measure inpatient care spending.30 Because actual spending is generally a fraction of the charge, charge data were adjusted to reflect spending using a regression-based adjustment.30 Second, to address concerns associated with undersampled rare conditions, a Bayesian hierarchical model was applied. For most types of care, 2 data sources were combined to generate spending estimates with complete time and age trends and to leverage the strength of each data source. This method allows us to make more granular estimates than what would be possible with a single data source, such as the Medical Expenditure Panel Survey.23 The model was used independently for each condition, sex, and type of care combination. The third adjustment addressed the fact that ambulatory and inpatient care data sources used for this study underestimate spending at specialty mental health and substance abuse facilities. To address this problem, spending on these types of care was split into portions that reflect mental health and substance abuse spending and scaled to an appropriate total estimated using spending reported by the US Substance Abuse and Mental Health Services Administration.31 This adjustment ensured that the total spending on mental health and substance abuse in these settings was commensurate with official US records.
Quantifying Uncertainty
Uncertainty intervals were quantified by bootstrapping the underlying encounter-level data 1000 times. The estimation process was completed for each bootstrap sample independently, and 1000 estimates were generated for each condition, age, sex, year, and type. The estimates reported in this article are the mean of these 1000 estimates. An uncertainty interval was constructed using the 2.5th and 97.5th percentiles. The intervals were not calibrated to reflect 95% CIs and are included only as an indicator of relative confidence. eAppendix 1 and eAppendix 5 in the Supplement provide additional information about all the methods used for this analysis.
Statistical Analysis
We compared spending estimates by condition, age, and sex, across 6 types of care. We then summarized spending by focusing on (1) the largest 20 conditions leading to children’s healthcare spending in 2013; (2) aggregated spending by age, type of care, and condition categories for 2013; (3) spending per child by age and type for 2013; and (4) changes and percent changes in spending per child by condition, type, and age between 1996 and 2013. Stata version 13.1 (StataCorp), R version 3.3.1, and Python version 3.5.1 were used for these analyses.
Results
Aggregated Results by Age, Type of Care, and Condition
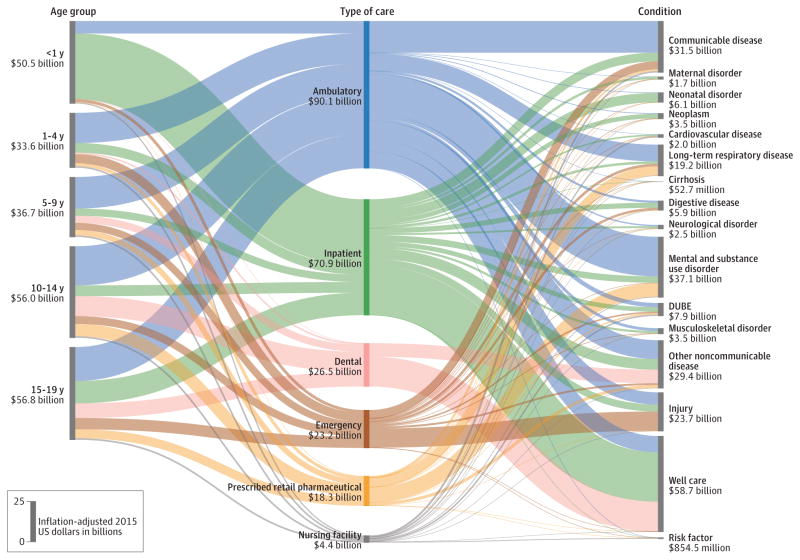
In 2013, $233.5 (uncertainty interval [UI], 226.9–239.8) billion was spent on children’s personal health care. (All spending estimates are reported in inflation-adjusted 2015 US dollars.) Figure 1 shows how spending on children’s health care was simultaneously split by age, condition, and type of care. In 2013, 30.4% (UI, 28.8–32.4) of total children’s personal health care spending was spent on in patient care, while 38.6% (UI, 37.1–40.3) and 7.8% (UI, 6.8–8.7) was spent on ambulatory care and retail pharmaceuticals, respectively. Spending on infants younger than 1 year was the largest portion of spending on children’s personal health care, comprising 21.6% (UI, 19.9–23.5) of the total amount spent on children’s health care. Spending on non-communicable and long-term diseases was $111.0 (UI, 106.7–114.5) billion, amounting to 3.5-fold more than the $31.5 (UI, 29.7–33.9) billion spent on communicable, infectious, and nutritional disorders. Nearly $23.7 (UI, 22.4–25.2) billion was spent on injuries and $58.7 (UI, 54.9–63.8) billion on nonillness conditions, such as well newborn care, well-child care, and preventative dental care.
Figure 1. Personal Health Care Spending in the United States by Age Group, Aggregated Condition Category, and Type of Care in 2013.
Each of the 3 columns reflect the $233.5 billion of children’s health care spending disaggregated in this study. The length of each bar reflects the relative share of the $233.5 billion attributed to that age group, condition category, or type of care. Spending estimates are reported using inflation-adjusted 2015 US dollars. Communicable diseases include nutrition deficiencies. DUBE indicates diabetes, urogenital, blood, and endocrine diseases.
Largest Health Conditions Leading to Children’s Personal Health Care Spending
The Table highlights the top 20 health conditions leading to children’s personal health care spending. In 2013, spending for these 20 most costly conditions accounted for 78.0% (UI, 74.9–81.1) of all personal health care spending on children. Well-newborn care, with $27.9 (UI, 24.2–32.2) billion spent on infants younger than 1 year in inpatient settings, received the most health care spending. Attention deficit/hyperactivity disorder (ADHD) was the second largest condition causing children’s health care spending, with $20.6 (UI, 17.3–23.5) billion in 2013. Of this spending, 60.6% (UI, 55.4–63.9) was spent on boys aged 5 to 14 years. Of total ADHD spending, 63.9% (UI, 51.0–76.1) was spent on ambulatory care, while 35.4% (UI, 26.3–44.4) was spent on retail pharmaceuticals. Well-dental care, which includes general examinations, x-rays, and orthodontia, was the third largest condition.
Table.
Largest 20 Conditions of Personal Health Care Spending for Children and Adolescents 19 Years and Younger in the United States in 2013
| Rank | Condition | 2013 Spending (US$ in Billions) | 2013 Spending per Child (US$ in Thousands) | 2013 Spending per GDP, % | 2013 Spending, % | |||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Ambulatory Care | Inpatient Care | Retail Pharmaceuticals | Age <1y | |||||
| All conditions | 233.5 | 2.78 | 1.42 | 38.6 | 30.4 | 7.8 | 21.6 | |
| 1 | Well-newborn | 27.9 | 6.49a | 0.17 | 0 | 100 | 0 | 100 |
| 2 | ADHD | 20.6 | 0.24 | 0.13 | 63.9 | 0.7 | 35.4 | 0 |
| 3 | Well-dental (eg, general examination and cleaning, x-rays, and orthodontia) | 18.2 | 0.22 | 0.11 | NA | NA | NA | 0 |
| 4 | Asthma | 9.0 | 0.11 | 0.05 | 35.6 | 7.7 | 47.1 | 0 |
| 5 | Oral disorders (eg, oral surgery and caries, including fillings, crowns, extraction, and dentures) | 8.7 | 0.10 | 0.05 | 0.8 | 2.1 | 0.2 | 0 |
| 6 | Well-child | 8.5 | 0.10 | 0.05 | 100 | 0 | 0 | 39.0 |
| 7 | Upper respiratory tract infections | 8.4 | 0.10 | 0.05 | 71.0 | 4.0 | 2.1 | 15.3 |
| 8 | Other long-term respiratory diseases (eg, sleep apnea, allergic rhinitis, and chronic sinusitis) | 8.1 | 0.10 | 0.05 | 76.8 | 2.7 | 16.3 | 0 |
| 9 | Skin and subcutaneous diseases (eg, cellulitis, sebaceous cyst, acne, and eczema) | 8.0 | 0.10 | 0.05 | 60.3 | 9.3 | 20.9 | 2.4 |
| 10 | Exposure to mechanical forces (eg, falling object, striking other object, cuts, and being crushed) | 7.8 | 0.09 | 0.05 | 40.5 | 4.0 | 0.4 | 0.9 |
| 11 | Falls | 7.8 | 0.09 | 0.05 | 33.9 | 6.9 | 0.1 | 3.2 |
| 12 | Congenital anomalies | 7.4 | 0.09 | 0.05 | 27.8 | 71.7 | 0 | 59.0 |
| 13 | Otitis media | 7.4 | 0.09 | 0.05 | 84.1 | 0.8 | 5.5 | 14.9 |
| 14 | Lower respiratory tract infections | 6.1 | 0.07 | 0.04 | 32.6 | 46.3 | 3.1 | 28.4 |
| 15 | Other infectious diseases (eg, viral and chlamydial infection and streptococcal) | 5.9 | 0.07 | 0.04 | 69.5 | 5.9 | 3.7 | 12.4 |
| 16 | Sense organ diseases (eg, cataracts, vision correction, adult hearing loss, and macular degeneration) | 5.3 | 0.06 | 0.03 | 86.4 | 3.7 | 2.1 | 6.7 |
| 17 | Depressive disorders | 5.0 | 0.06 | 0.03 | 58.7 | 23.1 | 15.2 | 0 |
| 18 | Preterm birth complications (eg, respiratory distress and extreme immaturity) | 4.9 | 1.14a | 0.03 | 6.0 | 93.8 | 0.1 | 100 |
| 19 | Pregnancy and postpartum care (eg, normal pregnancy, including cesarean delivery) | 3.5 | 0.17b | 0.02 | 33.0 | 64.7 | 0.3 | 0 |
| 20 | Anxiety disorders | 3.4 | 0.04 | 0.02 | 82.1 | 8.3 | 3.8 | 0 |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; GDP, gross domestic product; NA, not applicable.
Per infant younger than 1 year.
Per adolescent aged 15 to 19 years.
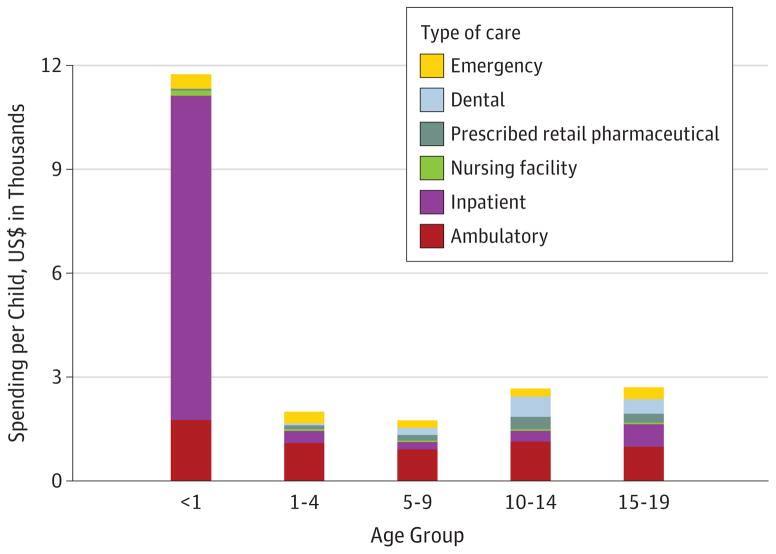
Children’s Spending by Age Group
Figure 2 highlights personal health care spending per child by age group and type of care. Spending per infant younger than 1 year was much larger than spending on all other age groups, at $11 741 (UI, 10 799–12 765). Of this spending, 79.8% (UI, 72.2–88.3) took place in inpatient care facilities. Of inpatient care spending, 69.3% (UI, 60.1–79.9) was spent on well-newborn care, while 15.1% (UI, 12.4–17.6) was spent on neonatal conditions. The remaining 4 age groups each received roughly 15% to 25% of the amount spent on infants younger than 1 year, and most of this spending was for ambulatory care rather than inpatient care.
Figure 2. Spending per Child on Personal Health Care for Children and Adolescents in the United States by Type of Care in 2013.
Health care spending per child reported using inflation-adjusted 2015 US dollars. Emergency care excludes emergency visits that resulted in an inpatient stay admission. Inpatient care includes spending in emergency departments for patients who transferred to inpatient care and includes pharmaceuticals provided while in inpatient care. Ambulatory care includes urgent care clinics and pharmaceuticals provided as part of a visit.
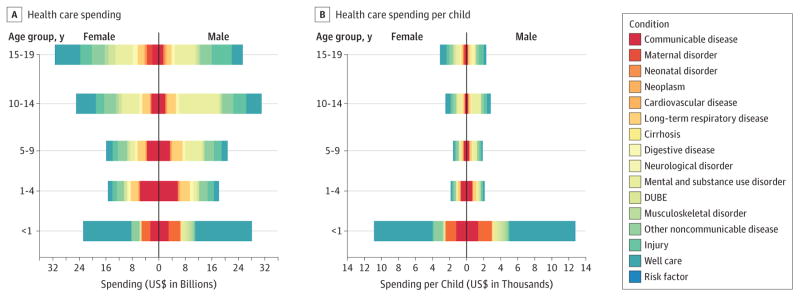
Figure 3 shows personal health care spending for children and spending per child by age, sex, and condition, highlighting the substantial amount of health care spending in 3 key areas: (1) communicable diseases and well-newborn care during the first year of life; (2) mental health and behavioral disorders—primarily ambulatory care and pharmaceuticals for ADHD—for boys aged 5 to 14 years; and (3) reproductive health care for girls aged 15 to 19 years, which was included in well-care.
Figure 3. Children’s Personal Health Care Spending in the United States by Age, Sex, and Condition in 2013.
Spending estimates are reported using inflation-adjusted 2015 US dollars. Increases in spending along the x-axis indicate more spending. Communicable diseases include nutrition deficiencies. DUBE indicates diabetes, urogenital, blood, and endocrine diseases.
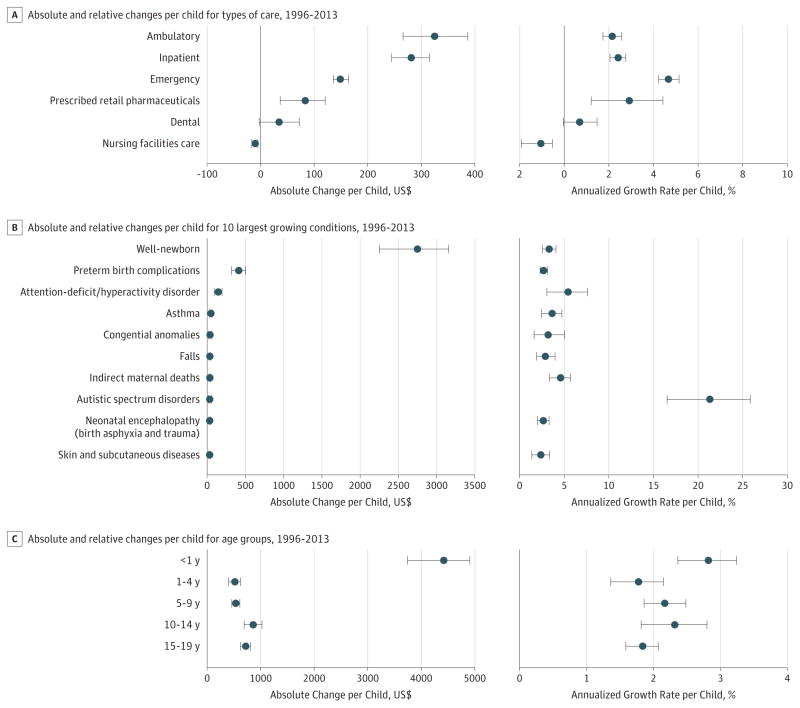
Trends in Personal Health Care Spending on Children
Personal health care spending on children and adolescents 19 years and younger grew 56.2% (UI, 49.5–62.3) from $149.6 (UI, 144.1–155.5) billion in 1996 to $233.5 (UI, 226.9–239.8) billion in 2013. Per child, this was an annualized growth of 2.5% (UI, 2.1–2.7). Figure 4 highlights the types of care, conditions, and age groups with the greatest increases per child. Among types of care, ambulatory care and inpatient care increased the most during this period. Together, these 2 types of care accounted for 70.0% (UI, 62.6–76.5) of all increases in health care spending on children between 1996 and 2013. Among all conditions, well-newborn care, preterm birth complications, and ADHD increased the most in absolute terms per child during this period. Well-newborn care alone added $12.9 (UI, 10.8–14.7) billion to the children’s health care spending total. In relative terms, though, autism spectrum disorder grew substantively more than all other conditions, with an annualized growth rate of 21.8% (UI, 17.0–26.4). Finally, annualized growth in spending per child across all age groups was roughly the same, with growth rates ranging from 2.8% (UI, 2.4–3.2) for infants younger than 1 year to 1.8% (UI, 1.4–2.1) for children aged 1 to 4 years. Because infant spending was much greater than the other age groups in 1996, the spending growth per child was much greater in absolute terms for this age group.
Figure 4. Changes in Spending per Child on Personal Health Care in the United States by Condition From 1996 to 2013.
Each panel reports the absolute change in spending (left) reported using inflation-adjusted 2015 US dollars and the annualized rate of change in spending (right) reported as an annualized growth rate. For all panels and axes, change is the difference in spending between 1996 and 2013. A, Changes in spending for all 7 types of care. Emergency care excludes emergency visits that resulted in an inpatient stay admission. Inpatient care includes spending in emergency departments for patients that transferred to inpatient care and includes pharmaceuticals provided to these patients. Ambulatory care includes urgent care clinics and pharmaceuticals provided as part of a visit. B, Changes for the 10 conditions with the greatest absolute increases in spending. C, Changes in spending for the 5 age groups. Error bars indicate uncertainty intervals.
Discussion
Summary of Key Findings
To our knowledge, this is the most comprehensive study to date that produces national estimates of personal health care spending for the general population of children in the United States. These estimates describe patterns of spending by condition, age and sex group, type of care, and time. Children’s health care spending accounted for 8.4% (UI, 8.2–8.6) of total health care spending in 2013, amounting to $233.5 (UI, 226.9–239.8) billion.19 The largest health conditions leading to health care spending include well-newborn, ADHD, and well-dental care, together accounting for $66.7 (UI, 72.2–61.0) billion spent in 2013. Between 1996 and 2013, annual health care spending on children overall grew by 56.2% (UI, 49.5–62.3) or $83.9 (UI, 75.9–90.7) billion, fueled by growth in ambulatory and inpatient spending and by growth in well newborn and ADHD care spending.
Comparison With Past Research and Contribution
Previous studies have proposed estimates for children’s health care spending, but to our knowledge, none have provided such granular estimates over a long period for all major payers. The Centers for Medicare and Medicaid Services estimates spending on the population 18 years and younger to be $276 billion in 2012, compared with our estimate of $233.5 (UI, 226.9–239.8) billion in 2013.32 The Health Care Cost Institute provides health care spending estimates for those covered by employer-based insurance but excludes all other payers, including government insurance, such as Medicaid. Furthermore, these estimates do not allow for granular condition-level comparisons. McCormick et al33 have produced 11 annual reports of health care on children in the United States between 2000 and 2015, but they do not report a comprehensive set of estimates by condition.34 Our total and condition-specific spending estimates are an improvement on previous studies and move the field forward for several reasons. We combine information from 183 data sources rather than relying on a single data source and scale spending estimates (across all ages) to reflect official US estimates. This results in a complete time series of granular spending estimates for 150 conditions, disaggregated by age, sex, and type of care from 1996 to 2013.
Our study was not designed to examine whether the increases have been appropriate or whether the proportion of child to adult health care spending was equitable. Instead, this study explained spending and changes in spending in order to elucidate important health system patterns and to provide evidence for policy makers who plan children’s health care and pediatric health systems. Addressing the lack of an integrated child health care data system focused on financing could be an important aspect of improving the American pediatric health care infrastructure.35 Through a wide ranging set of data that splits health care spending into granular categories, researchers, policy makers, and health care clinicians have a foundation to explore important associations among trends in health care spending, use, and disease burden.
Implications for Research and Policy
Newborn Care
On average, $11 741 (UI, 10 799–12 765) was spent on health care per infant younger than 1 year in 2013. Most health care spending for these infants occurred in the inpatient setting. Well-newborn care, which was almost exclusively associated with uncomplicated delivery, accounted for 69.3% (UI, 60.1–79.9) of inpatient spending for infants younger than 1 year, while 14.2% (UI, 11.5–16.6) of spending was for neonatal conditions, including preterm birth complications, neonatal encephalopathy, and other neonatal disorders. Well-newborn care spending has increased $12.9 (UI, 10.8–14.7) billion from 1996 to 2013, while spending on neonatal conditions has increased $2.6 (UI, 2.0–3.1) billion. These findings align with past research indicating that newborn care was one of the top 5 conditions in terms of total hospitalization costs across all age groups.36 Pediatric health researchers should investigate what factors are driving increased costs of newborn care and whether these increases are efficiently or effectively improving outcomes.
Reproductive Health
Health care spending on adolescents aged 15 to 19 years was spurred by spending related to reproductive health, including pregnancy and postpartum care, maternal conditions, and family planning. Three hundred fifty-five dollars (UI, 330–382) per girl aged 15 to 19 years was spent on pregnancy and postpartum care, $163 (UI, 144–183) was spent on maternal conditions, and $13 (UI, 11–15) was spent on family planning. Following a decline in adolescent pregnancy since 2008, inpatient spending on pregnancy and postpartum care for these girls dropped slightly from 2008 through 2013. Despite these modest reductions, pregnancy and postpartum care remains the largest condition leading to health care spending for girls aged 15 to 19 years and the 19th largest condition across all ages and sexes.
ADHD and Behavioral Health
Increased spending on mental health and behavioral disorders caused 24.8% (UI, 19.9–29.4) of the increases in children’s personal health care spending, and 15.4% (UI, 12.9–17.5) was due to increases in well-newborn care. Within the mental health and behavioral disorders category, spending on ADHD pharmaceuticals, especially for boys aged 5 to 14 years, was the largest source of spending increases. This aligns with past research that indicated a growth in diagnostics and treatments of ADHD among this age group since the early 2000s.37 These findings call for greater research on increased costs associated with ADHD care, effectiveness of ADHD interventions, and cost-effective strategies for children with ADHD.
Ambulatory Well-Child Care
Growth in spending on ambulatory well-child care has been much slower than growth in spending on inpatient well-newborn care. Despite being the presumptive cornerstone of pediatric health care, well-child care was still only the sixth largest condition in 2013. Well child care in the ambulatory setting amounted to $8.5 (UI, 7.1–10.4) billion spent across all ages, representing 3.7% (UI, 3.0–4.4) of total children’s health care spending. This translates to an average of $101.5 (UI, 84.5–123.3) per child that was spent on well-child care in ambulatory care settings. Preventing adult disease and establishing environments and patterns that promote lifelong health are the primary purposes of pediatric health care. Whether well-child care is currently constructed and funded at levels that allow effective pursuit of these goals remains unclear.
Moreover, it is also unclear whether increases in pediatric health care spending have occurred in ways that are strategically or rationally designed to contribute to lifelong health on a population level. Increases in spending have flowed to inpatient well-newborn care for reasons that should be investigated further, but increases have also flowed to relatively common and long-term physical and developmental issues (eg, ADHD, asthma, and autism) that are likely to have some population-level importance for adult health. Data elucidating which areas have not yet benefited from increases such as these may be helpful in evaluating the societal usefulness of spending trends and allocation of resources.
Limitations
While the IHME Disease Expenditure 2013 project produces granular spending estimates using standardized methods across time, these data have important limitations. First, the survey data underlying some of the spending estimates were not fully representative of the US population, as they excluded some small segments of the population, such as incarcerated persons. Second, reliance on survey data means that data on rare conditions or exceptionally expensive health system encounters were underreported. Similarly, administrative data are dependent on coding and diagnosis patterns that are popular among physicians and hospital administrators. To address these concerns, the IHME Disease Expenditure 2013 project leveraged multiple data sets to build on the strengths of each data source. Still, these methods do not eliminate the need for amore representative and comprehensive health care surveillance system. Third, the underlying data prevented stratification by race, socioeconomic status, payer, geographic region, or medical complexity. Complex medical cases that are sometimes covered by Medicaid comprise a large fraction of children’s health care spending.37 A small percentage of children make up the vast majority of health care spending in inpatient settings.12 While it is clinically and politically relevant to understand the differences between medically complex and nonmedically complex health care spending, this study was unable to do so. Ongoing research is encouraged to understand how health care spending varies across these dimensions.
Finally, spending data reported in this study reflect only direct health care spending and do not account for indirect societal costs associated with care, such as parental forgone earnings or child care costs. Spending data in this study are based on health system payments, except for inpatient spending, where charges are used as the data input. While this study uses a charge-to-payment ratio to adjust these charges, the development of a nationally comprehensive database of health care payments would improve the accuracy of these estimates.38
Conclusions
Describing health care spending and changes in health care spending is an essential first step in elucidating health system patterns and providing evidence for policy makers who plan children’s health care and pediatric health systems. The next step should be analyzing the factors driving increased health care spending and determining whether changes in particular subcategories of spending have been associated with improvements in processes or outcomes. It is crucial to understand whether spending increases have been appropriate or misguided and how we might target spending increases and reductions now and in the future.
Supplementary Material
Acknowledgments
Funding/Support: Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under award P30AG047845 and by the Vitality Institute.
Footnotes
Conflict of Interest Disclosures: None reported.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Vitality Institute.
Additional Contributions: We acknowledge all members of the Institute for Health Metrics and Evaluation Disease Expenditure 2013 research team. In particular, for their ideas during the conception of this research, we thank Ranju Baral, PhD (Global Health Sciences, University of California, San Francisco); Anne Bulchis, MPH (Global Health Sciences, University of California, San Francisco); Madeline Campbell, BS, Elizabeth Johnson, BA, and Jonathan Joseph, BS (Institute for Health Metrics and Evaluation, Seattle, Washington); and Liya Lomsadze, BS (Northwell Health, New Hyde Park, New York). None of the contributors were compensated for their work.
Author Contributions: Dr Dieleman had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Mr Bui and Dr Dieleman are co–first authors of this article.
Concept and design: Bui, Dieleman, Birger, Chapin, Duber, Murray.
Acquisition, analysis, or interpretation of data: Bui, Dieleman, Hamavid, Birger, Duber, Horst, Reynolds, Squires, Chung.
Drafting of the manuscript: Bui, Dieleman, Chapin, Duber, Reynolds, Murray.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Bui, Dieleman, Birger, Horst, Reynolds, Squires.
Obtained funding: Dieleman, Chapin.
Administrative, technical, or material support: Bui, Dieleman, Chapin, Murray.
Supervision: Bui, Dieleman, Chapin, Duber, Chung, Murray.
References
- 1.Hartman M, Martin AB, Lassman D, Catlin A National Health Expenditure Accounts Team. National health spending in 2013: growth slows, remains in step with the overall economy. Health Aff (Millwood) 2015;34(1):150–160. doi: 10.1377/hlthaff.2014.1107. [DOI] [PubMed] [Google Scholar]
- 2.United States Census Bureau. [Accessed June 4, 2015];Age and sex composition in the United States. http://www.census.gov/population/age/data/2012comp.html.
- 3.Health Care Cost Institute. [Accessed July 26, 2016];Children’s health spending: 2010–2014. http://www.healthcostinstitute.org/files/2016%20Kids%20Report%205.16.16.pdf.
- 4.Lassman D, Hartman M, Washington B, Andrews K, Catlin A. US health spending trends by age and gender: selected years 2002–10. Health Aff (Millwood) 2014;33(5):815–822. doi: 10.1377/hlthaff.2013.1224. [DOI] [PubMed] [Google Scholar]
- 5.Simpson L, Zodet MW, Chevarley FM, Owens PL, Dougherty D, McCormick M. Health care for children and youth in the United States: 2002 report on trends in access, utilization, quality, and expenditures. Ambul Pediatr. 2004;4(2):131–153. doi: 10.1367/1539-4409(2004)4<131:HCFCAY>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Halfon N, DuPlessis H, Inkelas M. Transforming the U.S. child health system. Health Aff (Millwood) 2007;26(2):315–330. doi: 10.1377/hlthaff.26.2.315. [DOI] [PubMed] [Google Scholar]
- 7.Liem O, Harman J, Benninga M, Kelleher K, Mousa H, Di Lorenzo C. Health utilization and cost impact of childhood constipation in the United States. J Pediatr. 2009;154(2):258–262. doi: 10.1016/j.jpeds.2008.07.060. [DOI] [PubMed] [Google Scholar]
- 8.Guevara J, Lozano P, Wickizer T, Mell L, Gephart H. Utilization and cost of health care services for children with attention-deficit/hyperactivity disorder. Pediatrics. 2001;108(1):71–78. doi: 10.1542/peds.108.1.71. [DOI] [PubMed] [Google Scholar]
- 9.Kuo DZ, Hall M, Agrawal R, et al. Comparison of health care spending and utilization among children with medicaid insurance. Pediatrics. 2015;136(6):e1521–e1529. doi: 10.1542/peds.2015-0871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hartman M, Catlin A, Lassman D, Cylus J, Heffler S. U.S. health spending by age, selected years through 2004. Health Aff (Millwood) 2008;27(1):w1–w12. doi: 10.1377/hlthaff.27.1.w1. [DOI] [PubMed] [Google Scholar]
- 11.Swinburn AT, Matthew DM. Health status-adjusted life excpectancy and health care spending for different age groups in the United States. [Accessed July 26, 2016];Mich J Public Aff. 2013 10:30–43. http://mjpa.umich.edu/files/2014/08/2013-DavisSwinburn-LifeExpectancy.pdf. [Google Scholar]
- 12.Peltz A, Hall M, Rubin DM, et al. Hospital utilization among children with the highest annual inpatient cost. Pediatrics. 2016;137(2):e20151829. doi: 10.1542/peds.2015-1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gray SH, Trudell EK, Emans SJ, Woods ER, Berry JG, Vernacchio L. Total direct medical expenses and characteristics of privately insured adolescents who incur high costs. JAMA Pediatr. 2015;169(10):e152682. doi: 10.1001/jamapediatrics.2015.2682. [DOI] [PubMed] [Google Scholar]
- 14.Kenney G, Yee J. SCHIP at a crossroads: experiences to date and challenges ahead. Health Aff (Millwood) 2007;26(2):356–369. doi: 10.1377/hlthaff.26.2.356. [DOI] [PubMed] [Google Scholar]
- 15.Hudson JL, Selden TM. Children’s eligibility and coverage: recent trends and a look ahead. Health Aff (Millwood) 2007;26(5):w618–w629. doi: 10.1377/hlthaff.26.5.w618. [DOI] [PubMed] [Google Scholar]
- 16.Currie J, Decker S, Lin W. Has public health insurance for older children reduced disparities in access to care and health outcomes? J Health Econ. 2008;27(6):1567–1581. doi: 10.1016/j.jhealeco.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 17.Dubay L, Kenney G. The impact of CHIP on children’s insurance coverage: an analysis using the National Survey of America’s Families. Health Serv Res. 2009;44(6):2040–2059. doi: 10.1111/j.1475-6773.2009.01040.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ringel JS, Sturm R. National estimates of mental health utilization and expenditures for children in 1998. J Behav Health Serv Res. 2001;28(3):319–333. doi: 10.1007/BF02287247. [DOI] [PubMed] [Google Scholar]
- 19.Dieleman JL, Baral R, Birger M, et al. US spending on personal health care and public health, 1996–2013. JAMA. 2016;316(24):1–20. doi: 10.1001/jama.2016.16885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosen AB, Cutler DM. Challenges in building disease-based national health accounts. Med Care. 2009;47(7, suppl 1):S7–S13. doi: 10.1097/MLR.0b013e3181a23e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Medicare and Medicaid Services. [Accessed December 16, 2015];National health expenditure data: historical. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountshistorical.html.
- 22.Roehrig C. Mental disorders top the list of the most costly conditions in the United States: $201 billion. Health Aff (Millwood) 2016;35(6):1130–1135. doi: 10.1377/hlthaff.2015.1659. [DOI] [PubMed] [Google Scholar]
- 23.Medical Expenditure Panel Survey. [Accessed September 27, 2016];Agency for Healthcare Research and Quality. https://meps.ahrq.gov/mepsweb/
- 24.GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roehrig C, Miller G, Lake C, Bryant J. National health spending by medical condition, 1996–2005. Health Aff (Millwood) 2009;28(2):w358–w367. doi: 10.1377/hlthaff.28.2.w358. [DOI] [PubMed] [Google Scholar]
- 26.International Monetary Fund. [Accessed May 28, 2016];World Economic Outlook database. http://www.imf.org/external/pubs/ft/weo/2016/01/weodata/index.aspx.
- 27.Hodgson TA, Cohen AJ. Medical care expenditures for diabetes, its chronic complications, and its comorbidities. Prev Med. 1999;29(3):173–186. doi: 10.1006/pmed.1999.0534. [DOI] [PubMed] [Google Scholar]
- 28.Fortin M, Soubhi H, Hudon C, Bayliss EA, van den Akker M. Multimorbidity’s many challenges. BMJ. 2007;334(7602):1016–1017. doi: 10.1136/bmj.39201.463819.2C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162(20):2269–2276. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- 30.Healthcare Cost and Utilization Project. [Accessed September 27, 2016];Agency for Healthcare Research and Quality. https://www.hcup-us.ahrq.gov/
- 31.Levit K, Frankel S, Mark T, Coffey R, Ivanova E, Pfuntner A. National Expenditures for Mental Health Services & Substance Abuse Treatment: 1986–2009. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Accessed July 26, 2016]. https://store.samhsa.gov/shin/content/SMA13-4740/SMA13-4740.pdf. [Google Scholar]
- 32.Centers for Medicare and Medicaid Services. [Accessed May 29, 2016];National health expenditure data: age and gender. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Age-and-Gender.html.
- 33.McCormick MC, Kass B, Elixhauser A, Thompson J, Simpson L. Annual report on access to and utilization of health care for children and youth in the United States: 1999. Pediatrics. 2000;105(1 pt 3):219–230. [PubMed] [Google Scholar]
- 34.Torio CM, Encinosa W, Berdahl T, McCormick MC, Simpson LA. Annual report on health care for children and youth in the United States: national estimates of cost, utilization and expenditures for children with mental health conditions. Acad Pediatr. 2015;15(1):19–35. doi: 10.1016/j.acap.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 35.Halfon N, Wise PH, Forrest CB. The changing nature of children’s health development: new challenges require major policy solutions. Health Aff (Millwood) 2014;33(12):2116–2124. doi: 10.1377/hlthaff.2014.0944. [DOI] [PubMed] [Google Scholar]
- 36.Torio CM, Andrews RM. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: Agency for Health Care Policy and Research; 2006. [Accessed June 27, 2016]. National inpatient hospital costs: the most expensive conditions by payer, 2011: statistical brief #160. http://www.ncbi.nlm.nih.gov/books/NBK169005/ [PubMed] [Google Scholar]
- 37.Berry JG, Hall M, Neff J, et al. Children with medical complexity and Medicaid: spending and cost savings. Health Aff (Millwood) 2014;33(12):2199–2206. doi: 10.1377/hlthaff.2014.0828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hamavid H, Birger M, Bulchis AG, et al. Assessing the complex and evolving relationship between charges and payments in US hospitals: 1996 – 2012. PLoS One. 2016;11(7):e0157912. doi: 10.1371/journal.pone.0157912. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.