Abstract
Various studies have pointed to the great importance of subjective health as an indicator for mortality in older age, while less is known about factors that contribute to changes of subjective (self-rated) health over time. Based on a nationwide longitudinal survey (German Ageing Survey, N = 1,286; initial age 40–85), two major findings emerged: first, the incidence of a serious health event caused greater changes in subjective health and life satisfaction in middle compared to older age. This was as expected because serious health events are less common in middle age and are correspondingly experienced more often as an “off-time event”. Secondly, the study extended previous findings on the impact of a positive view of ageing on health by showing that this optimistic view positively affects subjective health and life satisfaction even in the face of a serious health event. Overall, the study indicates that a positive view on ageing is an important psychological resource in the case of a serious health event, both when it occurs on-time or off-time from a developmental perspective.
Keywords: Subjective (self-rated) health, Positive view on ageing, Serious health event, Life satisfaction, Longitudinal study
Introduction
Just over 25 years ago, Mossey and Shapiro (1982) showed that a single question on subjective (self-rated) health is a better predictor for mortality in later life than measures on physical health status. This meant not only that people with poorer health appraisals are at higher risk for mortality but also that those who maintain good subjective health despite poor physical health may reduce their risk of mortality (Chipperfield 1993). Numerous subsequent studies came to the same conclusion (for reviews see Benyamini and Idler 1999; Idler and Benyamini 1997).
These findings stimulated interest in the relationship between physical and subjective health, but studies on the subject came to diverging results (e.g. Goldstein et al. 1984; Jang et al. 2004; Linn and Linn 1980). This heterogeneity is partly due to the varying health indicators used in different studies (Pinquart 2001). Additionally, psychological factors contribute to the explanation of why individuals with equivalent levels of disease have varying levels of subjective health (Benyamini et al. 2000; Quinn et al. 1999).
One way to a better understanding of the impact of physical diseases on subjective health of older adults is to examine how much the incidence of a serious health event affects changes in subjective health, a question that has only been addressed in a few studies (Diehr et al. 2001). The present longitudinal study considers this question and examines furthermore whether psychological resources moderate the impact of a serious health event. The findings may contribute to a better understanding of the relationship between physical diseases and subjective health and indicate how people can maintain good subjective health despite a serious medical event. Given the strong relationship between subjective health and mortality, this would appear to be an important task.
The impact of a serious health event on subjective health
The occurrence of a serious health event such as a stroke, cancer or a hip fracture often marks a turning point in life. Unlike acute illnesses such as influenza, these illnesses are more often life-threatening and are often also accompanied by long-term consequences such as pain or functional limitations. At least two studies have examined how the subjective health of older adults (aged 65 and over) changes using observations before and after a serious health event; the analyses were based on the Cardiovascular Health Study (Diehr et al. 2001) and the Epidemiologic Study of the Elderly (Wilcox et al. 1996). These studies observed that the occurrence of a serious health event did not adversely affect the subjective health of all people; on the contrary, some people maintained or even improved their subjective health.
Why people assess their health as similar or even better after a serious health event can be explained by an adaptation process referred to as “response shift” (Sprangers and Schwarz 1999). This response shift implies that the meaning of self-evaluation of health has changed, e.g. due to a change in the individual’s standards or values, or a redefinition (i.e. re-conceptualisation) of health. One considerable factor for the occurrence and extent of this response shift is the age at which a health event occurs.
Age as a moderator in the relationship between a serious health event and subjective health
Studies that have analysed the relationship of physical illnesses or functional limitations and subjective health have repeatedly shown that this correlation is stronger for younger age groups, while it decreases in older age groups (e.g. Idler 1993; Jang et al. 2004; Rakowski and Cryan 1990). One essential cause for this age-related divergence presumably lies in the biological, societal and age-normative structuring of the life course. The fact that ageing is accompanied by worsening health is well known and the adjustment to decreasing physical strength and health is therefore regarded as a major developmental task in later life (Havighurst 1981). Accordingly, the worsening of health is a normatively expected life change in later life and older people are prepared for it (see also Heckhausen and Krüger 1993). This is reflected in the finding that older adults are more likely than younger ones to define lower levels of functioning as a concomitant phenomenon of ageing but not of deteriorating health (Leventhal and Prohaska 1986). Older adults may therefore maintain good subjective health despite illness or disability because they apply a different standard for their health perception. This standard often refers to a comparison with most other age peers (Krause and Jay 1994), in which older people often perceive their peers as less healthy than themselves (Heckhausen and Brim 1997). But an individual’s awareness that he or she has reached a great age as well as the recognition that a wide range of (even painful) experiences has been overcome may also contribute to good subjective health (Martin et al. 2001).
These considerations argue in favour of the assumption that older adults perceive a serious health event more as normal and expectable, that is, as an “on-time event” (Neugarten 1996), than middle-aged adults, for whom the same event is comparatively “off-time” and therefore presumably more of a crisis. This should also be reflected in changes after a serious health event: with increasing age, subjective health should be less affected by a serious health event.
However, even if this was empirically established, the following alternative explanation makes a clear-cut interpretation of the result more difficult. Subjective health decreases with age (Idler 1993). This means that middle-aged and older adults could differ in their response to a serious health event simply because a further decrease of subjective health is less likely for older adults. On this account, life satisfaction should be additionally considered. While subjective health reflects a domain-specific satisfaction, general life satisfaction is more a trait component of subjective well-being and does not decrease with age (e.g. Diener 1994). In the present study, we therefore included both subjective health and life satisfaction to compare whether the findings for both measures point in the same direction.
There is still lack of studies on the age-related importance of serious health events because the majority of studies focus either on younger or older adults. For this reason, the present study considers this question by examining the impact of a serious health event on changes in subjective health and life satisfaction for individuals aged 40–85, that is, for middle-aged and older adults.
Is a positive view on ageing beneficial in the case of a serious health event?
Age is not a psychological indicator, but it seems to be a proxy for dealing with physical losses and the importance attributed to these physical losses. Does this mean conversely that an optimistic view of ageing is detrimental to subjective health and life satisfaction because these expectations are contrary to actual development?
This conclusion was drawn by Bultena and Powers (1978), who stated that “Ironically, the negative stereotypes about older persons . . . may be functional in the sense of providing a sufficiently dreary picture of old age that many aged persons, by comparison, feel advantaged” (Bultena and Powers 1978, p. 753). A study by Isaacowitz and Seligman (2001) points to the same conclusion. In their study of older people, they found that optimists experienced more depressive symptoms as a result of negative life events than pessimists. They did not expect this finding, however, because optimism had emerged as an adaptive strategy for younger adults they concluded that with increasing age overestimating competence becomes more and more maladaptive.
On the other hand, recent longitudinal studies have shown a beneficial effect of a positive view on ageing for physical and functional health, health behaviour and longevity (e.g. Levy and Myers 2004; Levy et al. 2002; Maier and Smith 1999; Wurm et al. 2007). Hence, these studies argue more in favour of the assumption that older people who hold a positive view on ageing have good psychological resources at their disposal and that such a positive view does not therefore pose a risk, even in old age. However, these studies did not consider any negative events. Thus, it is possible that the majority of older adults who had not experienced a negative life event (at least not during the period of the study) obscured the adverse impact of a positive view on ageing for those who actually have experienced a negative event (e.g. a serious illness). Studies that have focused on optimism and the course of diseases or recovery argue in turn against this thesis by showing that optimism, even unrealistic optimism, promotes recovery after a serious disease (e.g. Borkan and Quirk 1992; Scheier et al. 1989; Taylor et al. 2000). Accordingly, Aspinwall and her colleagues (2001) suggest that optimism and other positive beliefs serve as resources that allow people to use their skills in coping and problem-solving flexibly and successfully. Although the previous findings point to contradictory conclusions, the majority tend to argue in favour of a beneficial effect of a positive view on ageing even if a serious health event occurs. But none of these studies has examined this question directly.
The present study thus addressed two major hypotheses. First, we expected that the impact of a serious health event on changes in subjective health and life satisfaction would depend on age; that is, a serious health event should affect middle-aged adults more strongly than older adults, reflecting its status as an on-time or off-time event. Secondly, we expected that a positive view on ageing would positively affect subjective health and life satisfaction independently of whether a serious health event occurred or not (main effect). Additionally, we explored the question of whether a positive view on ageing would moderate the negative impact of a serious health event on subjective health and life satisfaction (buffer effect).
Method
Sample
The current study is based on longitudinal data from 1,286 non-institutionalised Germans aged 40–85 at baseline. In-home interviews and questionnaires were used initially in 1996 and again in a follow-up study 6 years later in 2002. The longitudinal sample is part of the German Ageing Survey, an ongoing nationwide population-based study, which uses a longitudinal and sequential design with several samples (Engstler and Wurm 2006).
The baseline sample was drawn by means of national probability sampling. About 50% of the persons contacted completed an interview (N = 4,838), 83.4% of whom additionally completed a questionnaire (N = 4,034; Table 1a). The response rate corresponds to that of other large survey studies in Germany (Neller 2005). The sample was stratified by three age groups (40–54, 55–69, 70–85 years), gender and place of residence (Eastern or Western Germany). In 1996 the survey participants were asked whether they were willing to be re-interviewed at a later point in time and 61% (N = 2,972) agreed to this. The addresses of the other participants were deleted in accordance with the regulations of the German data protection law. Six years after the first interview, 16.3% of the 2,972 respondents had died or moved to unknown addresses, which reduced the sample that could be contacted for a second time to N = 2,478. 63.8% of persons from this reduced sample were in fact re-interviewed, while 36.2% refused (due to illness, or without giving any reason). Considering only those people who completed both the interview and the questionnaire in both waves of the survey, the longitudinal sample consists of N = 1,286 participants (Table 1b). Compared to the baseline sample, the longitudinal sample was about 3 years younger (M AgeT1 = 57.07; SD = 10.81), but hardly differed in gender (47.5% female, n = 611) and the place of residence (63.5% from Western Germany, n = 816). As can be seen in Table 1, the follow-up participants of the German Ageing Survey have a higher education and income, rated their heath better and were more likely to live with a partner (Engstler and Wurm 2006). Moreover, follow-up participants had significantly higher life satisfaction, and a more positive view on ageing. The selective attrition applies more to older adults than to middle-aged adults.
Table 1.
Sample characteristics
| (a) Baseline sample (N = 4,034) | (b) Longitudinal sample (N = 1,286)a | |
|---|---|---|
| Age (years) | 60.05 (12.18) | 57.07 (10.81) |
| Female | 48.8% | 47.5% |
| Western Germany | 66.1% | 63.5% |
| Education | 1.49 (0.71) | 1.64 (0.76) |
| Income (Euro) | 1243.09 (730.87) | 1335.78 (725.01) |
| Prestige | 45.93 (11.62) | 48.27 (11.89) |
| With partner | 78.4% | 83.8% |
| Physical illnesses | 2.57 (1.90) | 2.32 (1.78) |
| No functional limitations | 67.0% | 73.3% |
| Serious health eventb | – | 23.0% |
| Positive view on ageingc | 50.00 (10.00) | 52.71 (8.67) |
| Life satisfaction Tc1 | 50.00 (10.00) | 48.77 (9.39) |
| Life satisfaction Tc2 | – | 50.00 (10.00) |
| Subjective health T1 | 3.47 (0.85) | 3.63 (0.78) |
| Subjective health T2 | – | 3.49 (0.78) |
All data refer to the first wave of the survey (T1) unless otherwise noted. Percentage or mean and standard deviations in brackets
aLongitudinal sample comprises a share of the baseline sample
bSerious health events that occurred between the first and second wave of the survey were assessed retrospectively at T2
cLatent variable scores, T-standardised (cf. “Data analysis”)
These findings reflect the established fact of selective attrition in longitudinal research on ageing (e.g. Baltes et al. 1971; Chatfield et al. 2005; Norris 1985). We return to the implications of sample selectivity in the “Discussion” section.
Measures
Subjective health
On both measurement occasions a single standard item was used, asking “How would you rate your health at the present time?” This item could be answered on a 5-point Likert scale ranging from 1 = very good to 5 = very bad. For the analyses, the responses were reverse coded so that a high score refers to good subjective health. This simple global question is one of the most frequently used measures of self-rated health (Fayers and Sprangers 2002). The Pearson correlation between subjective health and age was r T1 = −0.22, r T2 = −0.24 (P < 0.001), i.e. subjective health in fact decreased with age.
Life satisfaction
Life satisfaction was measured on both measurement occasions by three items (“I am satisfied with my life”, “In most ways my life is close to my ideal”, “The conditions of my life are excellent”), which could be answered on a 4-point scale ranging from 1 = definitely true to 4 = definitely false; again, for the analyses the items were reverse coded.
Based on these three items at baseline (T1) and follow-up (T2), we computed a longitudinal measurement model using LISREL 8.5 (cf. “Data analysis”). Subjective health and life satisfaction were the only indicators assessed at both measurement occasions; they were correlated to a moderate extent (T1: r = 0.24, T2: r = 0.35). The correlation between life satisfaction and age was r T1 =0.07 (P < 0.01), r T2 = −0.01 (P = 0.62), i.e. as expected and unlike subjective health, life satisfaction did not decrease with age.
Serious health events
In the year 2002 (T2), survey participants were asked retrospectively: “Have you had a serious illness or an accident in the last 6 years?” In cases where not only one but several illnesses or accidents had occurred, the interviewer asked the respondent to report on the most serious one only. About a quarter (25.7%, n = 330) of the respondents reported on a serious illness or accident such as cancer, heart attack, serious fall or traffic accident. Participants who reported a serious health event were additionally asked to what extent this event was stressful for them: “If you think back, how would you describe the extent to which this illness or injury was stressful to you?” This question was answered on a 5-point scale ranging from “not at all stressful” to “very stressful”. The data collection of the first wave was carried out from February to June 1996. This means serious health events could happen both before or after the interview was held in 1996. On this account, we only considered health events from the years 1997–2002 (n = 296; 78% of these were illnesses), to ensure that the reported health events did not occur before the first interview in 1996. In additional analyses, however, we included serious health events that happened in 1996; the results remained largely the same.1
Positive view on ageing
We used the “Ongoing Development” scale, which we had already applied in previous studies (Wurm et al. 2007). This scale refers to the view of ageing as a time of personal development and was assessed by four items (“Ageing means to me that I continue to make plans”, “Ageing means to me that my capabilities are increasing”, “Ageing means to me that I can still learn new things”, “Ageing means to me that I can still put my ideas into practice”), developed by Dittmann-Kohli and her colleagues (1997). Participants could endorse the items on a scale ranging from 1 = definitely true to 4 = definitely false that were reverse coded for the analyses. As for life satisfaction, we computed the scale based on a latent measurement model (cf. “Data analysis”).
Age
We included chronological age (in years) for the analysis of age differences in the experience of a serious health event.
Socio-demographic characteristics
Indicators of socio-demographic characteristics were considered as control variables. These were the variables gender, living arrangement (with or without partner), place of residence (Eastern or Western Germany), and level of education (1 = less than 10 years school education, 2 = 10 or 11 years of school education, 3 = at least 12 years of school education). Additionally, we considered the equivalent household income (OECD scale on net household income in Euro, weighted by the number of people sharing the household, cf. Figini 1998) and a measure of occupational prestige ranging from 14 (=e.g. agricultural worker) to 78 (=e.g. medical doctor; Treiman 1977). For individuals who have never been part of the labour force, the occupational prestige of the spouse was used instead. All socio-demographic characteristics were collected at T1.
Physical illnesses and limitations
Indicators on physical illnesses and functional limitations were used as additional control variables. Physical illnesses were measured by a symptom checklist of 11 health problems (heart and circulatory complaints, perfusion problems, back or joint diseases, diabetes, cancer, gastro-intestinal diseases, respiratory diseases, bladder complaints, liver or kidney diseases, eye problems, ear complaints). For each person a sum score was computed based on the number of reported illnesses. Summary scores on self-reported physical illnesses have shown a considerably better accordance with medical reports than self-reports on single physical illnesses (Katz et al. 1996). Functional limitations were assessed by a question on difficulties with day-to-day tasks (“Are you hampered by health impairments in carrying out routine tasks, i.e. household chores?”) which could be responded to with 1 = not at all, 2 = a little, 3 = a great deal. The correlation of physical illnesses and functional limitations with subjective health were of medium extent (r ill-sh = 0.47, r limit-sh = 0.53, Ps < 0.001), which made these indicators strong control variables.
Data analysis
We computed latent variable scores and scale reliabilities for life satisfaction and positive view on ageing by testing latent measurement models using LISREL 8.5 (Jöreskog and Sörbom 1996) as our computer programme and maximum likelihood (ML) as our estimation method. This approach offers the possibility of accounting for measurement errors in the manifest indicators (observed measures) and testing the assumed measurement model empirically.
Latent measurement model for life satisfaction
First, we computed a longitudinal measurement model for life satisfaction, based on the three items at baseline (T1) and follow-up (T2) described above. A longitudinal measurement model allows us to test whether the observed measures load on the same latent variable on both occasions (configural invariance) and whether the observed variables have the same loadings on this latent variable on both occasions (metric invariance; Horn and McArdle 1992). Hence, a longitudinal measurement model allows us to test whether a latent variable (here: life satisfaction) is measured identically on both occasions. Allowing a correlation between the error terms of each item over T1 and T2 (De Shon et al. 1998) significantly improved the model fit. The longitudinal measurement model fitted the data very well [χ 2(7) = 17.76, P = 0.01, root mean square error of approximation (RMSEA) = 0.035, nonnormed fit index (NNFI) = 0.99, standardised root mean residual (SRMR) = 0.022]. This model showed both configural invariance and metric invariance. We created a scale by calculating the latent variable scores (“factor scores”) from this longitudinal measurement model. The factor loadings ranged between 0.72 and 0.87 resulting in a reliability of ρ = 0.86 at T1 and ρ = 0.84 at T2 according to Raykov (2004).
Latent measurement model for positive view on ageing
Secondly, we computed a measurement model for positive view on ageing (at T1). The scale was obtained by calculating the latent variable score from a congeneric measurement model with two error terms allowed to correlate. This model fitted the data well [χ 2(1) = 0.54, P = 0.46, RMSEA = 0.000, NNFI = 1.00, SRMR = 0.002]. The factor loadings ranged between 0.43 and 0.77 resulting in a reliability of ρ = 0.67 (Raykov 2004). Finally, the latent factor scores for life satisfaction and positive view on ageing were T-standardised (M = 50, SD = 10) in order to obtain an established scaling.
Further analyses
We carried out further analyses using SPSS 15.0. Intercorrelations among study variables and variance inflation factors (VIF) were assessed to determine multicollinearity. Sequential multiple regressions [i.e. independent variables (IVs) enter the equation in an order specified by the researcher; Tabachnik and Fidell 2007] were used to predict changes in subjective health and life satisfaction. IVs entered the equation in an order that we specified according to the hypotheses. Hence, the first IV that entered the equation was subjective health or life satisfaction at T1 to adjust the longitudinal analyses for the baseline values of the dependent variables. Subsequently, the main effects and interaction effects were included. In order to check the robustness of the regression, control variables were included in the last step. We calculated the interaction terms by multiplying the respective variables.
Missing values treatment
Single missing values were supplemented by data imputation with the Expectation-maximisation algorithm originally introduced by Dempster and colleagues (1977). This algorithm iteratively estimates the missing values (expectation step) by maximising the likelihood of the data (maximisation step). Imputing missing values offers the advantage that there is no loss of participants who missed single items. The amount of missing values was not systematic and negligible in size; n = 873 subjects (67.9%) had no missing values on all 75 variables, another n = 365 subjects (28.3%) had between one and ten missing values, and only n = 48 subjects (3.8%) had more than ten missing values. In no case were more than 35 out of 75 variables missing.
Results
Age and serious health event
On examining our first hypothesis that the impact of a serious health event on subjective health and life satisfaction depends on age, we conducted two sequential multiple regression analyses, one for changes in subjective health and one for changes in life satisfaction. For the prediction of subjective health at T2, subjective health at T1 was entered in the first step of the analyses (M1, β = 0.48; see Table 2a). In the second step, the main effects of serious health event and age were entered into the regression equation (M2). The occurrence of a serious health event had a significant and substantial impact on subjective health (β = −0.21), the effect of age was smaller but also significant (β = −0.12). In the next step (M3), the interaction term was entered into the equation and turned out to be highly significant (β = 0.37). This effect remained stable after controlling for socio-demographic characteristics (education, income, prestige, gender, place of residence, partnership) as well as physical illnesses and limitations (M4, β = 0.34). Similar results pertained to the prediction of life satisfaction, which has about the same stability as subjective health (M1, β = 0.45; see Table 2b). The main effect (M2) of a serious health event (β = −0.08) was smaller; as expected, chronological age could not predict changes in life satisfaction (β = 0.00). However, the interaction term “age × serious health event” was also significant for life satisfaction (M3, β = 0.30). After controlling for the covariates, the interaction coefficient remained significant (M4, β = 0.30) (cf. Note 1).
Table 2.
Sequential regression analysis predicting subjective health and life satisfaction by serious health event, age and the interaction between serious health event and age
| Predictors | (a) Subjective health (T2; six-year follow-up) | (b) Life satisfaction (T2; six-year follow-up) | ||||||
|---|---|---|---|---|---|---|---|---|
| βM1 | βM2 | βM3 | βaM4 | βM1 | βM2 | βM3 | βaM4 | |
| Subjective health (T1) | 0.48** | 0.43** | 0.43** | 0.33** | – | – | – | – |
| Life satisfaction (T1) | – | – | – | – | 0.45** | 0.45** | 0.45** | 0.39** |
| Serious health event | −0.21** | −0.52** | −0.49** | −0.08** | −0.33** | −0.32** | ||
| Age | −0.12** | −0.28** | −0.21** | 0.00 | −0.14* | −0.07 | ||
| Event × age | 0.37** | 0.34* | 0.30* | 0.30* | ||||
| Adjusted R² | 0.228 | 0.289 | 0.292 | 0.311 | 0.206 | 0.211 | 0.213 | 0.235 |
Dashes in cells indicate that the construct was not considered in the regression analysis
* P < 0.05 one-tailed; ** P < 0.01
aBeta coefficients controlled for gender, place of residence, partner, socio-economic status (education, income, prestige), physical illnesses, and functional limitations
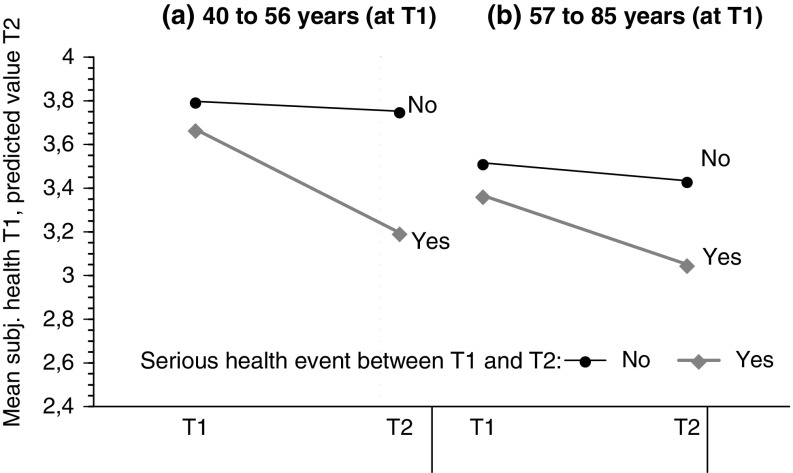
The significant interaction effects, both with regard to subjective health as well as to life satisfaction, are in line with the hypothesis. Figure 1 illustrates this finding for subjective health. The figure reveals that the impact of a serious health event on subjective health depends on age; as expected, younger individuals show stronger decreases in their subjective health after a serious health event than older individuals. Additional analyses showed that this finding could not be explained by a different evaluation of the event’s seriousness by young and old.
Fig. 1.
Longitudinal interaction effect of a serious health event × age (two-way interaction) on subjective health over a six-year period. The figure depicts the values for mean subjective health at T2 as predicted by subjective health at T1, age, serious health event (yes/no) and the interaction term age × serious health event. For reasons of visual clarity, age was separated by median split in two age groups
Positive view on ageing and serious health event
The second hypothesis referred to the question of whether a positive view on ageing is beneficial even if a serious health event occurs. After entering subjective health at T1 in the regression analysis (M1, β = 0.48), serious health event (M2, β = −0.22) and positive view of ageing (M3, β = 0.13) were considered (cf. Table 3a). The impact of a positive view on ageing remained significant after controlling for the covariates (M4, β = 0.10). Next, we computed the same regression analyses including consideration of the interaction effect between serious health event and positive view on ageing. The interaction term was not significant after consideration of all control variables (β = −0.03; P = 0.73). Thus, a positive view on ageing was beneficial independent of whether a serious health event occurs or not, but it did not additionally buffer the effect of a serious health event. Similar conclusions can be made for the change in life satisfaction as the outcome variable (Table 3b). Here, the main effect of a positive view on ageing was slightly stronger (M3: β = 0.16; M4: β = 0.15). But again there was no interaction effect between a serious health event and a positive view on ageing after all control variables entered the equation (β = −0.07; P = 0.36).2
Table 3.
Sequential regression analysis predicting subjective health and life satisfaction by serious health event and positive view on ageing
| Predictors | (a) Subjective health (T2; six-year follow-up) | (b) Life satisfaction (T2; six-year follow-up) | ||||||
|---|---|---|---|---|---|---|---|---|
| βM1 | βM2 | βM3 | βaM4 | βM1 | βM2 | βM3 | βaM4 | |
| Subjective health (T1) | 0.48** | 0.46** | 0.43** | 0.32** | – | – | – | – |
| Life satisfaction (T1) | – | – | – | – | 0.45** | 0.45** | 0.40** | 0.34** |
| Serious health event | −0.22** | −0.22** | −0.21** | −0.08** | −0.07** | −0.07** | ||
| Positive view on ageing | 0.13** | 0.10** | 0.16** | 0.15** | ||||
| Adjusted R² | 0.228 | 0.277 | 0.292 | 0.317 | 0.206 | 0.212 | 0.235 | 0.253 |
Dashes in cells indicate that the construct was not considered in the regression analysis
** P < 0.01
aBeta coefficients controlled for age, gender, place of residence, partner, socio-economic status (education, income, prestige), physical illnesses, and functional limitations
Age, positive view on ageing and serious health event
In a last step, we investigated whether a positive view on ageing only serves as a buffer in case of a serious health event in older age. With increasing age, a positive view on ageing becomes less common (r age × PVA = −0.25, P < 0.001), partly due to the age-related increase of losses. Thus, whether individuals have a positive view on ageing could become more and more crucial with age; i.e. in old age, a positive view on ageing could reflect high psychological resilience. To examine this buffer effect, we computed the same analyses as before, but additionally considered all two-way interactions between age, a positive view on ageing and a serious health event and finally the three-way interaction of the variables. The two-way interaction “age × serious health event” could significantly predict changes in subjective health (β = 0.39; P < 0.05), while the other two-way interactions were not significant after the adjustment of all control variables. However, the three-way interaction only marginally predicted changes in subjective health after the control variables in the regression analysis (β = 0.84; P = 0.05) were entered. Finally, we examined the three-way interaction effect with regard to life satisfaction, but the interaction term was not significant (β = 0.31; P = 0.49). Altogether, the findings support the second hypothesis that a positive view on ageing is beneficial even in the wake of a serious health event.
Discussion
The present longitudinal study tested two major hypotheses about the impact of a serious health event on changes in subjective health and life satisfaction. First, we had hypothesised that a serious health event would affect subjective health and life satisfaction to a decreasing extent with higher age because older adults perceive a serious health event more as normal and expectable, i.e. as an “on-time event”, which was supported by the present findings. Secondly, we had hypothesised that a positive view on ageing would promote subjective health and life satisfaction even if a serious health event occurs, which was corroborated as well.
Before discussing the findings of the present study, we would like to mention some limitations relating to the interpretation and generalisation of the present findings. The sample of the present study included non-institutionalised persons only and was biased toward better-educated and healthier people, particularly in older age. The selective attrition may have reduced our ability to detect decline in subjective health, since individuals with poorer health perceptions and those with a serious health event were less likely to participate in the follow-up interview because they were too ill or had died. A recent longitudinal study on multi-morbidity in old age which included institutionalised and cognitively impaired older people as well as proxy interviews has pointed to diverging results for more versus less strongly selected samples in respect of the prevalence rates of health problems (Meinow et al. 2006). This relates to the fact that surveys with non-institutionalised individuals are in general positively selected, particularly in favour of healthier people. Some researchers suggest “ . . . that attrition may affect the descriptive, representative outcomes of aging studies, particularly when such studies are focused on health and function, but that attrition not always seems to be a serious problem when associations between variables are analysed.” (Kempen and van Sonderen 2002, pp. 227–228).
This has been shown by several longitudinal ageing studies that have examined the question of how much the findings differ between a selected longitudinal sample and the corresponding original baseline sample. For this, follow-up data were estimated for those people in the baseline sample who dropped out (Kempen and van Sonderen 2002; Wurm et al. 2007). The studies report converging findings between the different samples. Although these findings qualify the impact of selective attrition in the present study, we should keep in mind the sample selectivity (both at baseline and follow-up), especially with regard to older adults.
A second limitation refers to the design of the present study. All variables were collected in the years 1996 and 2002, while serious health events occurred at any time in between both measures. Thus, with these data we could not consider whether older adults are more resilient with respect to a serious health event or whether they have a faster recovery than younger adults. More information around the time of a serious health event would be desirable in future studies to enable a differentiation between resilience and recovery (Bonnano 2004) and the role therein of a positive view on ageing.
However, the present study also has its methodological strengths, which lie in the large community sample, the longitudinal design as well as the large age range from middle to old age that allowed for age comparisons. In the following two sections we will go into the contributions of the present study to the existing field of research.
The age-related decrease in the importance of a serious health event for subjective health
Previous studies have repeatedly pointed to the lack of information about how subjective health changes over time and in particular, how it changes around the time of a serious health event (Diehr et al. 2001; Quinn et al. 1999). Moreover, it has been emphasised that consideration of older adults should be more differentiated instead of treating them as one single group that often spans 40 or more years (Jang et al. 2004).
We therefore included age as one key variable to examine changes in subjective health and life satisfaction after a serious health event. Our findings on age differences in experiencing a serious health event (Hypothesis 1) contribute to the explanation of why objective and subjective health increasingly diverge with age (e.g. Pinquart 2001). In fact, the present findings support our assumption that older people are more prepared for a worsening of health. They often regard health-related losses as a concomitant phenomenon of ageing (i.e. as “on-time event”) and not as a reason to change their subjective health perception after a serious health event. In contrast, middle-aged adults are comparably less prepared and therefore experience such an event more often as “off-time” (Neugarten 1996). Thus, age can serve as buffer in the experience of a serious health event.
The finding that a serious health event affects the subjective health of younger and older age groups differently raises the question of what such a global self-rated health item in fact measures. Subjective health perceptions cannot be disproved because they do not refer to any external reality; thus, they clearly differ from self-reports of conditions (e.g. self-reports on diabetes or arthritis), which are in principle verifiable, because they can theoretically be checked against medical records. Idler (1992) supposes the following process:
One interpretation is that the self-assessment of health is the end result of a complicated cognitive process in which respondents review the data available to them about their own health, select from it that which seems relevant, and then evaluate this information according to some set of criteria (p. 41).
These criteria, which form a framework of reference for providing a subjective health assessment, vary according to age. While the subjective health of younger individuals often refers to their health behaviour (Krause and Jay 1994), the health perception of older individuals more often includes health problems as such and comparisons to their age peers and includes the awareness that numerous age peers have been outlived (Eriksson et al. 2001). The different frame of reference for the health perception of younger and older adults cannot, however, prevent an age-related decrease of subjective health in general. However, the present study showed that the subjective health of older adults was less affected than that of younger adults if a serious health event occurred. Together, this suggests that the present findings on age differences cannot be solely explained by different frames of reference for the health perception of middle-aged and older adults; rather, the findings suggest that the age differences are dependent on whether an event was experienced as “on-time” or “off-time” in life.
An alternative explanation for the lower impact of a serious health event on the subjective health of older adults is that a further decrease of their subjective health is less probable because older adults already have lower subjective health than middle-aged adults. We therefore tested the hypothesis not only for subjective health (i.e. domain-specific satisfaction), but for general life satisfaction as well. Life satisfaction is more a trait component of subjective well-being and does not decrease with age (e.g. Diener 1994). The finding that the analyses for life satisfaction showed the same results as for subjective health militates against this alternative explanation. Finally, the present findings could not only be due to age-related differences but to cohort differences as well. However, other studies that have also pointed to an age-related divergence between subjective and physical health considered other birth cohorts but came to similar results (e.g. Idler 1993; Jang et al. 2004).
Thus, a serious health event has a lower impact on the subjective health of older adults, presumably because they are prepared for illness as an inevitable part of ageing. But several studies have pointed to the finding that people who attribute health problems to ageing (i.e. not to illnesses) have worse health behaviour (e.g. Leventhal and Prohaska 1986; Sarkisian et al. 2002) and higher mortality (Rakowski and Hickey 1992). This suggests that we have to differentiate between the expectation (and experience) that illnesses increase with age and the attribution of health problems to ageing; the former means that people are prepared for illness, the latter means, however, that age is equated with illness.
The importance of a positive view on ageing in the case of a serious health event
Previous studies have pointed to the finding that a positive view on ageing is beneficial for health, health behaviour and longevity in old age (e.g. Levy and Myers 2004; Levy et al. 2002; Maier and Smith 1999). Although we expected the same beneficial effect in the case of a serious health event (Hypothesis 2), we also considered the converse effect as possible; the positive view of ageing as an ongoing development could also hamper coping, because a serious health event could place limits on further development.
As expected, a positive view on ageing was also beneficial in the wake of a serious health event. This supports the assumption that optimistic beliefs can serve as a resource up to old age, independently of whether a negative life event occurs or not. The finding is thus in line with those of Levy and colleagues described above; correspondingly, it does not support the finding that pessimistic beliefs are more advantageous than optimistic ones if a negative life event occurs in old age (Isaacowitz and Seligman 2001).
The finding that a positive view on ageing affected subjective health and life satisfaction up to old age is noteworthy, in particular as a positive view on ageing referred in the present study to the expectation of ongoing personal development; personal development, however, primarily characterises the goal orientation of younger and middle-aged adults, while older adults focus more strongly on maintenance and loss avoidance (Heckhausen 1997; Ryff 1989). Although the perception of ongoing personal development is less common in old age, this view on ageing seems nevertheless to be important. Presumably this view implies that a person still has a meaningful purpose in life and can learn and grow from both positive and negative life experiences. Such positive beliefs are known as psychological resources that contribute to resilience, even if they are unrealistic or overly positively biased (Taylor et al. 2000). Because a positive view on ageing is less common in old age, it is probable that mainly those older adults who are particularly resilient still view ageing as ongoing development.
We thus additionally explored whether a positive view on ageing also serves as a buffer in old age. However, the three-way interaction between age, positive view on ageing and serious health event just failed the significance level to predict changes in subjective health (β = 0.84; P = 0.05). Given the difficulty to find significant higher-order interactions in unselected samples and the fact that age already buffers the negative impact of a serious health event in old age (cf. Hypothesis 1), it would seem worthwhile examining this finding in future studies with old and very old adults.
Conclusions
The present findings showed that a serious health event affects subjective health and life satisfaction to a lesser extent when perceived as on-time in life. This suggests that it is beneficial to be prepared for illnesses and disabilities, bearing in mind that illnesses become more common with age. At the same time, it seems important to view ageing as an ongoing development, that is, to have a positive future outlook with a meaningful purpose in life, even if it might be unrealistically optimistic.
Footnotes
We additionally computed the regression analyses including serious health events in 1996 (N = 34 or 2.64% of the sample reported on a serious health event in 1996), although we cannot distinguish events in 1996 that occurred before the interview from those after the interview. The results of the analyses were similar to those reported above; however, the interaction effect of serious health event × age was no more significant in the prediction of life satisfaction (β = 0.19, P =0.254). This might be due to the fact that serious health events that occurred before the first interview were also included.
Here too, we additionally computed the regression analyses including serious health events in 1996. The results of the analyses were similar to those reported above including only serious health events from 1997 to 2002.
References
- Aspinwall LG, Richter L, Hoffman RRI. Understanding how optimism works: an examination of optimists adaptive moderation of belief and behavior. In: Chang E, editor. Optimism and pessimism: implications for theory, research, and practice. Washington, DC: American Psychological Association; 2001. pp. 217–238. [Google Scholar]
- Baltes PB, Schaie KW, Nardi AH. Age and experimental mortality in a 7-year longitudinal study of cognitive behavior. Dev Psychol. 1971;5:18–26. doi: 10.1037/h0031085. [DOI] [Google Scholar]
- Benyamini Y, Idler EL. Community studies reporting association between self-rated health and mortality: additional studies, 1995–1998. Res Aging. 1999;21:392–401. doi: 10.1177/0164027599213002. [DOI] [Google Scholar]
- Benyamini Y, Idler EL, Leventhal H, Leventhal EA. Positive affect and function as influences on self-assessments of health: expanding our view beyond illness and disability. J Gerontol Psychol Sci. 2000;55B:P107–P116. doi: 10.1093/geronb/55.2.p107. [DOI] [PubMed] [Google Scholar]
- Bonnano GA. Loss, trauma, and human resilience. Am Psychol. 2004;59:20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- Borkan JM, Quirk M. Expectations and outcomes. Int J Aging Hum Dev. 1992;34:339–350. doi: 10.2190/4KLB-5CM4-1RRX-3U4U. [DOI] [PubMed] [Google Scholar]
- Bultena GL, Powers EA. Denial of aging: age identification and reference group orientations. J Gerontol. 1978;33:748–754. doi: 10.1093/geronj/33.5.748. [DOI] [PubMed] [Google Scholar]
- Chatfield MD, Brayne CE, Matthews FE. A systematic literature review of attrition between waves in longitudinal studies in the elderly shows a consistent pattern of dropout between differing studies. J Clin Epidemiol. 2005;58:13–19. doi: 10.1016/j.jclinepi.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Chipperfield JG. Incongruence between health perceptions and health problems. J Aging Health. 1993;5:475–496. doi: 10.1177/089826439300500404. [DOI] [Google Scholar]
- De Shon RP, Ployhart RE, Sacco JM. The estimation of reliability in longitudinal models. Int J Behav Dev. 1998;22:493–515. doi: 10.1080/016502598384243. [DOI] [Google Scholar]
- Dempster AP, Laird NM, Rubin DB. Maximum likelihood from incomplete data via the EM algorithm. J R Stat Soc [Ser B] 1977;39:1–22. [Google Scholar]
- Diehr P, Williamson J, Patrick DL, Bild DE, Burke GL. Patterns of self-rated health in older adults before and after sentinel health events. J Am Geriatr Soc. 2001;49:36–44. doi: 10.1046/j.1532-5415.2001.49007.x. [DOI] [PubMed] [Google Scholar]
- Diener E. Assessing subjective well-being: progress and opportunities. Soc Indic Res. 1994;31:103–157. doi: 10.1007/BF01207052. [DOI] [Google Scholar]
- Dittmann-Kohli F, Kohli M, Künemund H, Motel A, Steinleitner C, Gerben Westerhof in Zusammenarbeit mit infas-Sozialforschung (1997) Lebenszusammenhänge, Selbst- und Lebenskonzeptionen. Erhebungsdesign und Instrumente des Alters-Survey (Life contexts, conceptions of self and life. Design and instruments of the German Aging Survey). Freie Universität (Report 61), Berlin
- Engstler H, Wurm S (2006) Datengrundlagen und Methodik (Data base and method). In: Tesch-Römer C, Engstler H, Wurm S (eds) Sozialer Wandel und individuelle Entwicklung in der zweiten Lebenshälfte (Social change and individual development in the second half of life). VS Verlag für Sozialwissenschaften, Wiesbaden, pp 47–83
- Eriksson I, Unden A-L, Elofsson S. Self-rated health. comparisons between three different measures. Results from a population study. Int J Epidemiol. 2001;30:326–333. doi: 10.1093/ije/30.2.326. [DOI] [PubMed] [Google Scholar]
- Fayers PM, Sprangers MAG. Understanding self-rated health. Lancet. 2002;359:187–188. doi: 10.1016/S0140-6736(02)07466-4. [DOI] [PubMed] [Google Scholar]
- Figini P (1998) Inequality Measures, Equivalence Scales and Adjustment for Household Size and Composition. Luxembourg Income Study (Working Paper 185), Luxembourg
- Goldstein MS, Siegel JM, Boyer R. Predicting changes in perceived health status. Am J Public Health. 1984;74:611–614. doi: 10.2105/ajph.74.6.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havighurst RJ. Developmental tasks and education. New York: Longman; 1981. [Google Scholar]
- Heckhausen J. Developmental regulation across adulthood: primary and secondary control of age-related challenges. Dev Psychol. 1997;33:176–187. doi: 10.1037/0012-1649.33.1.176. [DOI] [PubMed] [Google Scholar]
- Heckhausen J, Brim OG. Perceived problems for self and others: self-protection by social downgrading throughout adulthood. Psychol Aging. 1997;12:610–619. doi: 10.1037/0882-7974.12.4.610. [DOI] [PubMed] [Google Scholar]
- Heckhausen J, Krüger J. Developmental expectations for the self and most other people: age grading in three functions of social comparison. Dev Psychol. 1993;29:539–548. doi: 10.1037/0012-1649.29.3.539. [DOI] [Google Scholar]
- Horn JL, McArdle JJ. A practical and theoretical guide to measurement invariance in aging research. Exp Aging Res. 1992;18:117–144. doi: 10.1080/03610739208253916. [DOI] [PubMed] [Google Scholar]
- Idler EL. Self-assessed health and mortality: a review of studies. Int Rev Health Psychol. 1992;1:33–54. [Google Scholar]
- Idler EL. Age differences in self-assessments of health: age changes, cohort differences, or survivorship? J Gerontol Soc Sci. 1993;48:S289–S300. doi: 10.1093/geronj/48.6.s289. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- Isaacowitz DM, Seligman MEP. Is pessimism a risk factor for depressive mood among community-dwelling older adults? Behav Res Ther. 2001;39:255–272. doi: 10.1016/S0005-7967(99)00178-3. [DOI] [PubMed] [Google Scholar]
- Jang Y, Poon LW, Martin P. Individual differences in the effects of disease and disability on depressive symptoms: The role of age and subjective health. Int J Aging Hum Dev. 2004;59:125–137. doi: 10.2190/RT1W-2HD7-KG5X-K1FB. [DOI] [PubMed] [Google Scholar]
- Jöreskog K, Sörbom D. Lisrel 8: User’s reference guide. Chicago: SSI Scientific Software; 1996. [Google Scholar]
- Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- Kempen GIJM, van Sonderen E. Psychological attributes and changes in disability among low-functioning older persons. Does attrition affect the outcomes? J Clin Epidemiol. 2002;55:224–229. doi: 10.1016/S0895-4356(01)00474-7. [DOI] [PubMed] [Google Scholar]
- Krause NM, Jay GM. What do global self-rated health items measure? Med Care. 1994;32:930–942. doi: 10.1097/00005650-199409000-00004. [DOI] [PubMed] [Google Scholar]
- Leventhal EA, Prohaska TR. Age, symptom interpretation and health behavior. J Am Geriatr Soc. 1986;34:185–191. [PubMed] [Google Scholar]
- Levy BR, Myers LM. Preventive health behavior influenced by self-perceptions of aging. Prev Med. 2004;39:625–629. doi: 10.1016/j.ypmed.2004.02.029. [DOI] [PubMed] [Google Scholar]
- Levy BR, Slade MD, Kasl SV. Longitudinal benefit of positive self-perceptions of aging on functional health. J Gerontol. 2002;57B:P409–P417. doi: 10.1093/geronb/57.5.p409. [DOI] [PubMed] [Google Scholar]
- Linn BS, Linn MW. Objective and self-assessed health in the old and very old. Soc Sci Med. 1980;14A:311–315. doi: 10.1016/0160-7979(80)90112-5. [DOI] [PubMed] [Google Scholar]
- Maier H, Smith J. Psychological predictors of mortality in old age. J Gerontol Psychol Sci. 1999;54B:P44–P54. doi: 10.1093/geronb/54b.1.p44. [DOI] [PubMed] [Google Scholar]
- Martin P, Rott C, Poon LW, Courtenay B, Lehr U. A molecular view of coping behavior in older adults. J Aging Health. 2001;13:72–91. doi: 10.1177/089826430101300104. [DOI] [PubMed] [Google Scholar]
- Meinow B, Parker MG, Kareholt I, Thorslund M. Complex health problems in the oldest old in Sweden 1992–2002. Eur J Ageing. 2006;3:98–106. doi: 10.1007/s10433-006-0027-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossey JM, Shapiro E. Self-rated health: a predictor of mortality among the elderly. Am J Public Health. 1982;72:800–808. doi: 10.2105/AJPH.72.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neller K. Kooperation und Verweigerung: Eine Non-Response-Studie (Cooperation and refusal: a non-response study) ZUMA-Nachr. 2005;57:9–36. [Google Scholar]
- Neugarten BL. The meanings of age. Chicago: The University of Chicago Press; 1996. [Google Scholar]
- Norris FH. Characteristics of older nonrespondents over 5 years of a panel study. J Gerontol. 1985;40:627–636. doi: 10.1093/geronj/40.5.627. [DOI] [PubMed] [Google Scholar]
- Pinquart M. Correlates of subjective health in older adults: a meta-analysis. Psychol Aging. 2001;16:414–426. doi: 10.1037/0882-7974.16.3.414. [DOI] [PubMed] [Google Scholar]
- Quinn ME, Johnson MA, Poon LW, Martin P. Psychosocial correlates of subjective health in sexagenarians, octogenarians, and centenarians. Issues Ment Health Nurs. 1999;20:151–171. doi: 10.1080/016128499248727. [DOI] [PubMed] [Google Scholar]
- Rakowski W, Cryan CD. Associations among health perceptions and health status within three age groups. J Aging Health. 1990;2:58–80. doi: 10.1177/089826439000200105. [DOI] [Google Scholar]
- Rakowski W, Hickey T. Mortality and the attribution of health problems to aging among older adults. Am J Public Health. 1992;82:1139–1142. doi: 10.2105/ajph.82.8.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raykov T. Estimation of maximal reliability: a note on a covariance structure modelling approach. Br J Math Stat Psychol. 2004;57:21–27. doi: 10.1348/000711004849295. [DOI] [PubMed] [Google Scholar]
- Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57:1069–1081. doi: 10.1037/0022-3514.57.6.1069. [DOI] [Google Scholar]
- Sarkisian CA, Hays RD, Mangione CM. Do older adults expect to age successfully? The association between expectations regarding aging and beliefs regarding healthcare seeking among older adults. J Am Geriatr Soc. 2002;50:1837–1843. doi: 10.1046/j.1532-5415.2002.50513.x. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Matthews KA, Owens JF, Magovern GJ, Lefebvre RC, Abbott AR, et al. Dispositional optimism and recovery from coronary artery bypass surgery: the beneficial effects on physical and psychological well-being. J Pers Soc Psychol. 1989;57:1024–1040. doi: 10.1037/0022-3514.57.6.1024. [DOI] [PubMed] [Google Scholar]
- Sprangers MAG, Schwartz CE. Integrating response shift into health-related quality of life research: a theoretical model. Soc Sci Med. 1999;48:1507–1515. doi: 10.1016/S0277-9536(99)00045-3. [DOI] [PubMed] [Google Scholar]
- Tabachnik BG, Fidell LS. Using multivariate statistics. 5th edn. Boston: Allyn and Bacon; 2007. [Google Scholar]
- Taylor SE, Kemeny ME, Reed GM, Bower JE, Gruenewald TL. Psychological resources, positive illusions, and health. Am Psychol. 2000;55:99–109. doi: 10.1037/0003-066X.55.1.99. [DOI] [PubMed] [Google Scholar]
- Treiman DJ. Occupational prestige in comparative perspective. New York: Academic Press; 1977. [Google Scholar]
- Wilcox VL, Kasl SV, Idler EL. Self-rated health and physical disability in elderly survivors of a major medical event. J Gerontol Soc Sci. 1996;51B:S96–S104. doi: 10.1093/geronb/51b.2.s96. [DOI] [PubMed] [Google Scholar]
- Wurm S, Tesch-Roemer C, Tomasik MJ. Longitudinal findings on aging-related cognitions, control beliefs and health in later life. J Gerontol Psychol Sci. 2007;62B:P156–P164. doi: 10.1093/geronb/62.3.p156. [DOI] [PubMed] [Google Scholar]