Abstract
Disability-free life expectancy estimates (DFLE) are summary measures to monitor whether a longer life expectancy (LE) is associated with better health or whether additional years of life are years of poor health or disability. Disability is a generic term defined as the impact of disease or injury on the functioning of individuals. It covers various situations from the rather common functional limitations to restrictions in daily activities and finally dependency. Disentangling these dimensions is essential to monitor future needs of care and assistance; but this is not always feasible since surveys do not systematically cover a large range of disability dimensions in their questionnaires. This study aims to cover different disability dimensions by using data from different French population surveys. We computed ten disability-free life expectancies, based on both specific and generic disability indicators from four population health surveys, in order to describe and compare trends and patterns for France over the 1980s and the 1990s. We used the Sullivan method to combine prevalence of disability and life tables. In 2000, two thirds of total LE at age 65 are years with physical or sensory functional limitations and 10% are years with restrictions in personal care activities. Trends in DFLE over the two last decades seem to have remained stable for moderate levels of disability and to have increased for more severe levels of disability or activity restrictions. We found that patterns are consistent from one survey to the other when comparing indicators reflecting similar disability situations.
Keywords: Disability-free life expectancy, Trends, France, Disability concepts
Introduction
The last few decades have been marked by a continuing decline in mortality in many countries, associated with an increasing chance of surviving to very old ages and/or of living with chronic conditions. This demographic pattern raises questions regarding the health status of populations and, more specifically, functional health and disability, which are frequently associated with both old age and chronic diseases. In this context, life expectancy (LE) indicators are no longer sufficient to monitor and qualify the dynamics of the population. Health expectancy indicators, such as disability-free life expectancy (DFLE), are computed to combine mortality and health data and to determine the average number of years to be lived in a given health status within total LE. These estimates shed light on whether longer life goes along with healthier life or whether additional years of life are years of poor health or of poor quality of life and disability.
Research on DFLE has been conducted worldwide since the 1980 s. The first studies showed favorable trends in disability in many developed countries (Robine et al. 2003). But many concepts and situations are grouped together under the overused term of disability: from basic functional limitations (poor vision, walking difficulties, etc.), to activity restrictions at work or at home, and ultimately “dependency”, when people require assistance for usual activities, like for personal care (bathing, feeding, etc.). Each of these dimensions corresponds to specific needs of care and assistance. Research has progressively highlighted the need to disentangle these different concepts and dimensions in order to better describe disability worldwide (Robine and Michel 2004). Clarifications of concepts and measures also provide a means to interpret apparently diverging trends between or within countries.
In recent years, studies have defined more clearly the underlying disability concepts used, more often making the distinction between levels of severity of disability or, when possible, providing various and complementary indicators. The distinction allowed researchers to show different trends according to the disability concept under consideration. Several studies have shown a decline in the prevalence among older people of need of assistance with personal care activities during the 1990s. For instance, in the US, a decline in ADL disability has been shown to be consistent across datasets (Freedman et al. 2004; Wolf et al. 2005). Meanwhile, a recent study in Sweden shows trends that contrast with previous findings: no improvement in the prevalence of activity restriction at old ages over the 1990s and a worsening of functional limitations (Parker et al. 2005). In the UK, over the 1980s and 1990s, LE without limiting long standing illness or disability increased less than total LE for men and increased equally for women (ONS 2006). Similarly, the share of LE with minor disability increased in the Netherlands over the 1990s while the share of LE with moderate and severe disability decreased (Perenboom et al. 2004). In Spain, DFLE has increased more than LE in recent years (Sagardui-Villamor et al. 2005). Thus, except in Sweden, the share of life expectancy with activity restrictions has usually decreased, while the share of life with moderate disability has remained stable or even increased.
In France, DFLE estimates available so far have shown that the increase in LE at age 65 between 1981 and 1991 (+1.8 years for women and +1.6 for men) was associated with an increase in DFLE for women (+2.3 years) and for men (+1.3 years) (Robine and Mormiche 1994). Both severe and moderate DFLE increased as LE increased. But, in the light of the patterns described above, it is obvious that two time point estimates are not sufficient to adequately monitor disability, especially when based on just one question. While a single survey does not provide enough information to document trends and patterns for various disability indicators, this study aims to mobilize all the available population data on disability in order to produce a set of DFLE indicators to better describe the situation for France.
We used four French surveys to compute a set of ten different DFLE estimates (three surveys allowing trends to be documented). We deliberately decided not to pool the data: first, because of heterogeneity in survey designs, questionnaires and quality or limits of the data that make meta-analysis impossible; second, because we wanted to benefit from the full range of information provided by these various data sources. A similar exercise was performed in the US with the aim of analyzing apparently divergent disability trends documented through various surveys (Freedman et al. 2004). In this paper, we (1) briefly review the disability models and conceptual frameworks that enabled us to organize and interpret our findings; (2) introduce the various French population surveys and the available disability indicators in reference to the models; and (3) present the corresponding DFLE estimates and discuss their limits and scope.
Definitions, methods and data
The definitions of disability and models
Disability is a generic term which can be defined as the consequences of illness and injury on an individual’s body functions, daily activities and social integration. Many models and definitions have been proposed to organize research since the late 1960s (Robine et al. 1997). In 1965, Nagi proposed one of the first instruments and models to measure individual functioning and assess need of care (Nagi 1965). It was followed by the research stream on the international classification of disability, introducing the idea of a functional decline and progressive loss of autonomy due to illness and health problems (Wood and Badley 1978; WHO 1980): impairments (deteriorated organs, structures or tissues) can translate into functional limitations, defined as body function alterations (vision, hearing, walking, etc.); these alterations can make it difficult for people to adequately and independently perform usual activities (at work or at home), resulting eventually in social disadvantage (job loss, isolation, need for help, need for pension etc.). Environmental and individual resources intervene in the process, influencing the capacity to cope with altered functions and to prevent possible repercussions on activities (Fougeyrollas and Majeau 1991; Verbrugge and Jette 1994). The revised version of the first classification of disability by the WHO, the International Classification of Functioning (ICF), also recommends recognizing the role of environment and determining how disability situations and factors are linked (WHO 2001). Even though the existing models of disability are based on a variety of definitions or classification systems (Hendershot 2006), they all advocate presenting indicators of disability in a way that allows disentangling the specific needs to which they correspond and interpreting apparently diverging trends.
Measurement instruments
The available data sets and measurement instruments have not necessarily followed the developments of the models and classifications. In surveys, disability is often assessed through detailed question modules to assess functional limitations and difficulties in performing activities. Questions on functional limitations aim to assess the body function alterations as described in the disablement process (difficulties in walking a certain distance, clearly hearing a conversation, seeing newspaper print, etc.). People reporting functional limitations are in various disability situations. Most of them can cope with their functional limitations, which do not impact their activity at work, at home or for personal care; they remain independent in their daily life. But for a number of others, the functional limitations translate into restrictions in specific activities. Activity restrictions correspond to the next step of the disablement process and help to specify disability situations. In most surveys, they are addressed by modules of questions dealing with a selection of activities which can be considered as essential to live independently (Lawrence and Jette 1996). The most common module assesses the difficulties with some personal care activities (getting dressed and undressed, bathing, etc.), as originally proposed by Katz with a selection of six “activities of daily living” or ADL (Katz et al. 1963). Surveys also contain questions referring to other activities related to daily management at home (preparing meals, shopping, taking medication, etc.), as proposed by Lawton and Brody with the “instrumental activity of daily living” or IADL (Lawton and Brody 1969). Studies based on these indicators have demonstrated that most people reporting functional limitations do not report activity restrictions. Nevertheless, people with functional limitations are more at risk for reporting activity restrictions. Longitudinal datasets confirm that functional limitations can be seen as a predictor of further restrictions (Jagger et al. 2001; Barberger-Gateau et al. 2000). The risk is modulated according to a number of individual social and demographic characteristics (see literature in Cambois et al. 2005). There are indeed factors that help compensate for functional limitations and allow older adults to remain independent. For example, studies have also highlighted that the use of technical devices can influence the capacity to maintain basic activity for people with functional limitations (Agree 1999; Freedman et al. 2006; Verbrugge et al. 1997).
These disability indicators depict a gradient in the severity of disability that can be defined as the impact on the independence of the people in their daily life: moderate levels of disability correspond to situations in which functional limitations do not impact usual activities and people remain independent in their daily life; severe levels correspond to situations in which people have difficulties in their usual activities. Activity restrictions for personal care can be considered as the most severe level of disability and difficulties in performing such activities usually require daily assistance. They concern a very small part of the general population, and occur late within the disablement process. People keep performing such activities until their body functions prevent them from taking care of them. Other activities such as shopping or preparing meals are more commonly delegated to relatives or professionals.
Survey questionnaires also contain single questions on disability (through which people report, in different ways, being limited or hampered in their daily life), aiming to depict the full range of disability situations (Verbrugge 1997). Cross-tabulations of these single questions with the modules on functional limitations and activity restrictions show that reporting severe functional problems or limitation correspond to situations in which people report activity restriction rather than simply functional problems (Cambois et al. 2007). This confirms the connection between the disability situation described via functional limitations and activity restrictions and the level of severity of disability.
Trends and patterns observed with these indicators can be interpreted in light of these definitions. The literature indicates more years lived with functional limitations and moderate levels of disability, probably linked to increased survival with chronic diseases or mild dysfunctions. But it also indicates a reduction in the years lived with activity restriction, with need for help in personal care activities or severe levels of disability. It can mean that the most common functional limitations may be increasing with the decrease in mortality risks, but that they less systematically translate into activity restrictions. A better acknowledgement and management of the functional limitations in recent years may have counterbalanced the associated risk of becoming restricted in daily activities.
A number of French surveys contain questions on disability that can be used to apply this conceptual approach. Altogether, we came up with ten disability indicators from the four surveys: three indicators of activity restrictions for personal care; two indicators of functional limitations (physical and sensory); five general questions on disability. We provide the corresponding disability prevalence for persons aged 65 years and older for recent years (standardized on the age structure of the French population in the beginning of the 2000s).
The surveys and the specific disability measurement instruments used
The health and medical care surveys (ESSM)
The ESSM is conducted every 10 years by the National Institute for Statistics and Economic Studies (INSEE), on a representative sample of French households. It collects information on self-reported health, health care consumption and health behavior over a several-week period. In the most recent survey 2002–2003 (conducted from the last term of 2002 to the third term of 2003), information was gathered over a 1-month period, during which an interviewer visited the households three times. The sample was based on 25,000 addresses randomly selected in the census database (with a 78% response rate among the households in the scope of the survey). Within the sample, a total of 6,237 persons aged 65 years and older completed the questionnaire of the first visit and 5,226 did so for all three visits (a weighting system is used to adjust the final sample in accordance with the characteristics of persons who dropped out). Among those who dropped out, 2.6% of the initial sample was designated as “not capable of participating in the survey” through a direct question addressed to the main respondent of the household (see Sect. “Discussion” for assessment of the associated bias). We used two general questions on disability asked during the first visit and the question modules on functional limitations and activity restrictions asked during the third visit.
General question on “Disability or discomfort” The general question (“Is there anyone in the household who is disabled or who simply has difficulties or discomfort in daily life? excluding temporary limitations or disabilities, such as a broken leg in plaster”) was asked in the ESSM 1980–1981, 1991–1992, 2002–2003 to the main respondent for the whole household, who designated household members in such a situation so that this information could be linked to their individual characteristics. The wording of this question covers a wide range of situations from “simple discomfort” to “being disabled”. This question was used to compute the 1981 and 1991 DFLE estimates presented in the Sect. “Introduction”. Unfortunately, due to a change in the survey design and positioning of the question in the interview in the 2002–2003 survey, the way of responding to this question seems to have changed, with greater focus on activity restrictions or recognized impairments and handicaps, while in previous surveys it surely included more people with moderate disability (Cambois et al. 2007); after some analysis, it was concluded that the question could not reliably be used to document most recent trends. We still display the three DFLE, indicating the break in the series, to keep the most complete information. The age-standardized prevalence for the 65+ age group in the household population is 16% in 2002–2003 (and was much larger in the two previous surveys).
General question on “Long term activity limitations” In the first visit, all household members reported individually if they were “limited for at least 6 months in activities people usually do, because of health problems”; a question widely used now in Europe (Van Oyen et al. 2006). This indicator also corresponds to various disability situations, from simple functional limitations to activity restrictions, with a slightly larger representation of the latter (Cambois et al. 2007). The age-standardized prevalence for the 65+ age group in the household population is 31% in 2002–2003.
Activity restrictions (personal care) Respondents reported having difficulty or being unable to perform, without someone’s help, activities related to personal care (getting dressed, feeding him/herself, getting into/out of bed, washing/bathing, going to the toilet). Persons reporting difficulties in at least one of these activities are considered restricted in personal care activities. The age-standardized prevalence for the 65+ age group in the household population is 11% in 2002–2003.
Functional limitations Respondents reported difficulty in walking, climbing stairs, kneeling, picking up an object, lifting and carrying a package, clearly hearing a conversation, seeing newspaper print, recognizing someone’s face across a street. Among persons reporting such functional limitations, we focus on those with residual functional limitations (i.e., persisting even with the use of their regular assistive or corrective device such as glasses or lenses, walking stick, etc.), in order to select limitations most linked to the risk of restrictions in activities. The age-standardized prevalence for the 65+ age group in the household population is 61% in 2002–2003.
Health and social protection survey (ESPS)
The ESPS survey, conducted annually since 1988 by the Institute for Research and Information on Health Economics (IRDES), aims to measure and analyze health and healthcare consumption of households in France. The ESPS concerns households in which at least one person is registered with one of the three main health insurance schemes, and which represent around 95% of persons living in households in 2000 (Auvray et al. 2003). Within the sample of households contacted by telephone, the non-response rate is high (56% of usable addresses supplied). Furthermore, it has increased over time, due to changes in the design (combination of an increased sample size and increased contact failures) (Doussin et al. 2002). The telephone contact provides preliminary information on socio-demographic characteristics and health insurance. A self-administered questionnaire, which contains the questions on disability, is then addressed to the household or administered face-to-face for the population above age 65. The non-response rate is generally high for the self-administered questionnaire (30% in 2002), but smaller in face-to-face administration. Due to these limitations, the level of disability and comparisons over time based on the ESPS should be interpreted with caution. However, these DFLE series are presented here to flesh out the all too scarce information on trends available for France. In this study, we used data from four periods: 1988–1991; 1992–1995; 1996–1998; 2000–2002. In 2002, a total of 4,650 persons aged 65 and older were contacted. To calculate DFLE, we used the mid-period life tables (1990, 1994, 1997, 2001). Two questions from this series of surveys are used to compute disability-free life expectancies:
Activity restrictions (washing/bathing) People were asked if they have difficulties washing/bathing themselves. This question is used to cover the domain of restriction for personal care activities. Most studies show that people reporting such problems generally cumulate difficulties in other personal care activities. At the same time, it should be more selective than a complete module, as the higher the number of items proposed, the higher the number of persons concerned (Rodgers and Miller 1997). The age-standardized prevalence for the 65+ age group in the household population is 11% in 2000–2002.
General question on “Mobility difficulties” People report if they have “difficulties moving around”. Response categories distinguish two severity levels. We consider “all levels of mobility difficulties” and among them we focus on “severe mobility difficulties” by excluding those who report “only difficulties that cause minor limitations”. People with severe mobility difficulties are in very poor functional health, as illustrated by the fact that 63% of them report also washing/bathing difficulties (vs. 11% in the total household population). In 2000–2002, the age-standardized prevalences for the 65+ age group in the household population are 18% for mobility difficulties of any level and 9% for severe mobility difficulties.
The disability and dependence survey (HID)
The HID survey aims to assess the disability situations of people with various types of disabilities living in households and in institutions. In order to remain consistent with the other surveys of our study, we focused on the household sample conducted in 1999, a stratified sample based on a preliminary screening survey “Vie quotidienne et santé” (a supplement to the 1999 population census questionnaire addressed to 360,000 respondents). This procedure resulted in the selection and over-representation of people with different types of disability for HID. The response rate was 78%. The sample of persons aged 65 and older totaled 7,560 individuals. Proxy responses were allowed to avoid exclusion of people unable to answer for health reasons (9.4% of the sample among the 65+ age group were helped during the interview and 8.4% were replaced by proxies). We used the question modules on functional limitations and activity restrictions.
Activity restrictions (personal care) People were asked if they had severe difficulties or were unable to eat without help (when food is ready); dress without help; wash/bathe without help; use the toilet without help; get into or out of bed without help. We focus on similar items in HID and in ESSM to facilitate comparison, despite different wordings. The age-standardized prevalence for the 65+ age group in the household population is 14% in 1999.
Functional limitations The respondents report difficulties walking, going up and down stairs, using their hands, cutting their toenails, bending down to pick up an object, poor near vision, poor distant vision, poor hearing. The wording of these questions makes no distinction between functional limitations with or without the use of a technical aid for physical limitations, but asks about residual limitations for sensory limitations (when people use their regular devices and aids), which makes it possible to compute an indicator similar to the one from ESSM 2002–2003. This survey contains a question related to time disorientation (cognitive limitations) which was not used also to remain closer to ESSM 2002–2003 indicators. The age-standardized prevalence of functional limitations for the 65+ age group in the household population is 62% in 1999.
The European Community Household Panel (ECHP)
The European Community Household Panel (ECHP) was a survey conducted by Eurostat and based on a standardized questionnaire that involved annual interviewing of a representative panel of households and individuals in each European country, covering a wide range of socio-economic topics including a couple of questions on health. It was run from 1994 to 2001. The response rate was 79% in 1994 (90% of non-responses were due to failure to contact households and 10% due to health problems). We use the 1995–2001 survey data (in 1994, the health questions were different). The French sample comprised around 12,600 community-dwelling people aged over 20 in 1995, and around 9,500 in 2001 (2,000 for those aged 65 and older) (Eurostat 1997).
General question on “Discomfort due to illness or disability” Since 1995, ECHP respondents have been asked “are you hampered in your daily activities by a physical or mental health problem, illness or disability; yes severely; yes, to some extent; no”. As with other general questions, the wording includes a wide range of situations; the use of “hampered” at the beginning of the question could contribute to the reporting of moderate problems only. The age-standardized prevalence for the 65+ age group in the household population is 55% in 2001.
Statistical analyses
The DFLE is defined as the mean length of time that individuals can expect to live free of disability if current health conditions continue to apply. Various methods exist to combine the risks of disability and mortality but for cross-sectional data corresponding to the above described surveys, the Sullivan method should be used (Sullivan 1971); it combines the disability prevalence and the usual period life table. The person-years of the life table for each age group are multiplied by the age-specific prevalence of disability, providing within the total number of years, the years lived with and without disability. The table then provides the total life expectancy (TLE), and its two components, the disability-free life expectancy (DFLE) and life expectancy with disability (LED). The confidence intervals take account of the survey sample size (Jagger et al. 2006). However, the surveys used only concern community-dwelling adults, excluding people living in institutions, who are considered to be less healthy than people living in a household. As proposed in the Sullivan’s method, we reintroduced the years spent in an institution, considering them as years with disability. The rate of residence in institutions is provided by the censuses and extrapolated for the period of interest of the study. Person-years in life tables are first decomposed into years lived in an institution and years lived in a household. Person-years in an institution are considered as lived with disability and added to person-years in households lived with disability. We discuss the implication of this assumption in the discussion section.
We also compared the trends obtained by the different time series that were available. We needed to estimate comparable rates of change based on the observed data, while surveys had different periodicities and covered different dates. We first estimated the disability-free life expectancy for each survey and each date. We then estimated the parameter of progression of the age-standardized prevalence between two dates based on a log-linear regression for each series (enabling to link the rate of change to the observed level of disability). We derived yearly prevalence from the parameters and estimated annual rates of change for the series.
Results
DFLE in France over the period 1999–2003
Table 1 gives the values of the ten DFLE calculated using the most recent survey data and ranked in decreasing order. Due to large survey samples, confidence intervals are small (hardly exceeding 1 year around the DFLE value). The order of DFLE is the same for men and for women, and the estimates obtained from indicators based on similar definitions are in the same range, even when the data sources are different.
Table 1.
Disability free life expectancies (DFLE) for men and women at age 65 years based on different disability indicators available in four recent household population health surveys, France 1999 to 2003 (% DFLE/LE and confidence intervals)
| Men | Women | |||
|---|---|---|---|---|
| Life expectancy at age 65 in 1999 | 16.5 | – | 21.0 | – |
| Life expectancy at age 65 in 2003 | 17.1 | – | 21.5 | – |
| Life expectancy | ||||
| Without severe mobility difficulties (ESPS 2000–2002) | 15.5 (91%) | 15.4–15.6 | 18.8 (88%) | 18.5–19.0 |
| Without washing difficulties(ESPS 2000–2002) | 15.4 (91%) | 15.3–15.5 | 18.3 (86%) | 18.0–18.5 |
| Without personal care activity restrictions (ESSM 2002–2003) | 14.8 (87%) | 14.7–14.9 | 17.1 (80%) | 16.9–17.3 |
| Without personal care activity restrictions (HID 1999) | 14.2 (86%) | 14.1–14.3 | 17.0 (81%) | 16.9–17.1 |
| Without disability or discomfort in daily life (ESSM 2002–2003) | 13.5 (79%) | 13.3–13.6 | 16.1 (75%) | 15.8–16.3 |
| Without mobility difficulties. all levels of severity (ESPS 2000–2002) | 12.9 (76%) | 12.6–13.1 | 14.7 (69%) | 14.3–15.2 |
| Without long-term activity limitations (ESSM 2002–2003) | 11.7 (69%) | 11.5–11.9 | 13.1 (61%) | 12.7–13.5 |
| Without discomfort due to illness or disability (ECHP 2001) | 7.8 (46%) | 7.1–8.5 | 8.3 (39%) | 7.4–9.2 |
| Without physical and sensory functional limitations (ESSM 2002–2003) | 6.8 (40%) | 6.4–7.3 | 6.9 (32%) | 6.3–7.5 |
| Without physical and sensory functional limitations (HID 1999) | 5.2 (32%) | 4.8–5.6 | 5.8 (28%) | 5.4–6.3 |
Sources: ESSM, INSEE 2002–2003; ESPS, IRDES 2000–2002; ECHP, Eurostat/INSEE 2001; HID, INSEE 1999
At the bottom of the gradient, we found the LE without physical or sensory functional limitations from HID in 1999 and ESSM in 2003; they are, respectively, 5.2 and 6.8 years for men and 5.8 and 6.9 years for women, being around one-third of LE at age 65. LE without personal care activity restrictions computed from HID and ESSM are located at the top of the gradient and also close to each other: 14.2 and 14.8 years for men and 17 and 17.1 years for women. They are also very close to the LE without washing/bathing difficulties based on ESPS 2000–2002. Altogether, men can expect to live around 10–15% of their LE free of such activity restrictions and women between 15 and 20%.
LE without discomfort due to illness or disability based on the French version of ECHP is quite low: 7.8 and 8.3 years for men and women, respectively. It clearly encompasses a broad range of situations including common moderate functional limitations beside more severe difficulties. Conversely, LE without disability or discomfort based on ESSM in 2003 is quite high, as expected, due to the impact of the new survey design that restricts the responses to severe or recognized disability (13.5 and 16.1 years for men and women, respectively). LE without long-term activity limitations lies in between. Finally, persons aged 65 can expect to spend around 75% of their remaining LE without mobility difficulties (all levels of severity) and around 90% without severe mobility difficulties. Women can expect to live more years with mobility difficulties than men, especially severe difficulties.
Change in DFLE over time
Over the 1990s, LE at age 65 increased by 1.35 years for men and 1.44 years for women. Fig. 1 displays the 10 DFLE for recent years as well as the DFLE obtained with earlier surveys. The corresponding figures are shown in Tables 2, 3, and 4.
Fig. 1.
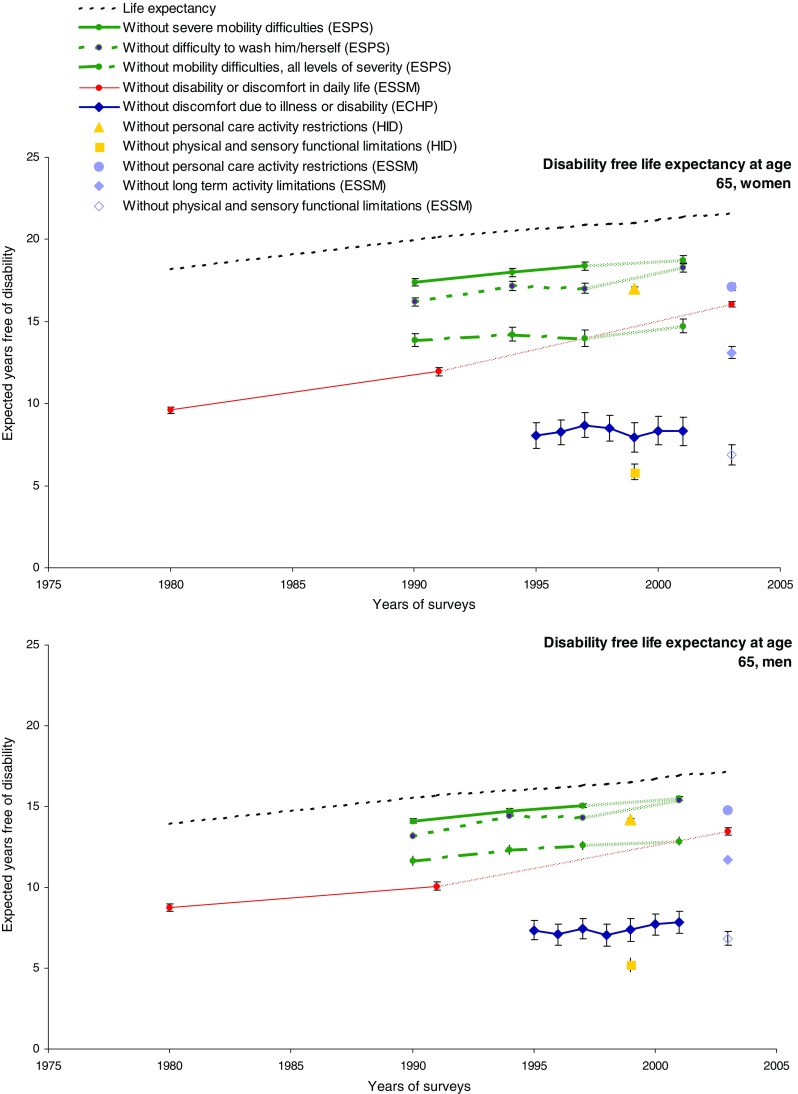
Disability-free life expectancy estimates at age 65 for France between 1980 and 2003 based on ten disability indicators and four surveys (see detailed figures in Tables 1, 2, 3, 4); men and women [Changes in the survey design of the EESM 2002-2003 caused a break in the series for these estimates (Cambois et al. 2007); change in the response rate in the ESPS surveys in 2002 leads to caution in interpretation of trends over time (Auvray et al. 2003)]
Table 2.
Life expectancy (LE) and life expectancy without disability or discomfort in daily life (DFLE) for men and women at age 65 based on ESSM (1980–1981; 1991–1992; 2002–2003), and confidence intervals at 95% (CI)
| Men | Women | |||||
|---|---|---|---|---|---|---|
| 1980–1981 | 1990–1991 | 2002–2003 | 1980–1981 | 1990–1991 | 2002–2003 | |
| LE | 14.1 | 15.7 | 17.1 | 18.3 | 20.1 | 21.52 |
| DFLE | 8.8 | 10.1 | 13.5 | 9.8 | 12.1 | 16.1 |
| CI | 8.5–9.0 | 9.8–10.3 | 13.3–13.7 | 9.4–9.8 | 11.7–12.2 | 15.9–16.2 |
| %DFLE/LE | 62 | 64 | 79 | 54 | 60 | 75 |
Changes in the survey design of the EESM 2002–2003 caused a break in the series for these estimates (Cambois et al. 2007)
Table 3.
Life expectancy (LE) and life expectancy without discomfort due to illness or disability (DFLE) for men and women at age 65 based on ECHP (1995–2001), and confidence intervals at 95% (CI)
| 1995 | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | |
|---|---|---|---|---|---|---|---|
| Men | |||||||
| LE | 16.09 | 16.12 | 16.32 | 16.39 | 16.50 | 16.72 | 16.91 |
| DFLE | 7.3 | 7.1 | 7.4 | 7.0 | 7.4 | 7.7 | 7.8 |
| CI | 6.7–7.9 | 6.4–7.7 | 6.8–8.1 | 6.3–7.7 | 6.7–8.1 | 7.0–8.4 | 7.1–8.5 |
| %DFLE/LE | 46 | 44 | 46 | 43 | 45 | 46 | 46 |
| Women | |||||||
| LE | 20.64 | 20.72 | 20.88 | 20.94 | 20.99 | 21.22 | 21.37 |
| DFLE | 8.1 | 8.3 | 8.7 | 8.5 | 7.9 | 8.4 | 8.3 |
| CI | 7.3–8.8 | 7.5–9.0 | 7.9–9.5 | 7.7–9.3 | 7.0–8.9 | 7.5–9.2 | 7.4–9.2 |
| %DFLE/LE | 39 | 40 | 42 | 41 | 38 | 39 | 39 |
Table 4.
Life expectancy (LE) and life expectancy without mobility difficulties and without difficulty washing oneself (DFLE) for men and women at age 65 based on ESPS (1988–1991; 1992–1995; 1996–1998; 2000–2002), and confidence intervals at 95% (CI)
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| 1988–1991 | 1992–1995 | 1996–1998 | 2000–2002 | 1988–1991 | 1994–1995 | 1996–1998 | 2000–2002 | |
| LE | 15.6 | 16.2 | 16.3 | 16.9 | 19.9 | 20.7 | 20.9 | 21.4 |
| Without mobility difficulties. all levels of severity | ||||||||
| DFLE | 11.6 | 12.3 | 12.6 | 12.9 | 13.9 | 14.2 | 14.0 | 14.7 |
| CI | 11.4–11.9 | 12.1–12.6 | 12.4–12.9 | 12.6–13.1 | 13.5–14.3 | 13.8–14.7 | 13.5–14.5 | 14.3–15.2 |
| %DFLE/LE | 75 | 76 | 77 | 76 | 70 | 69 | 67 | 69 |
| Without severe mobility difficulties | ||||||||
| DFLE | 14.1 | 14.7 | 15.1 | 15.5 | 17.4 | 18.0 | 18.4 | 18.8 |
| CI | 14.0–14.2 | 14.6–14.9 | 14.9–15.2 | 15.4–15.6 | 17.2–17.6 | 17.8–18.2 | 18.1–18.6 | 18.5–19.0 |
| %DFLE/LE | 91 | 91 | 92 | 92 | 87 | 87 | 88 | 88 |
| Without washing difficulties | ||||||||
| DFLE | 13.2 | 14.4 | 14.3 | 15.4 | 16.2 | 17.1 | 17.0 | 18.3 |
| CI | 13.0–13.4 | 14.3–14.6 | 14.2–14.5 | 15.3–15.5 | 16.0–16.5 | 16.9–17.4 | 16.7–17.3 | 18.0–18.5 |
| %DFLE/LE | 85 | 89 | 88 | 91 | 81 | 83 | 82 | 86 |
Change in the response rate in the ESPS surveys in 2002 leads to caution in interpretation of trends over time (Auvray et al. 2003)
LE without disability or discomfort increased between 1981 and 1991, as described in the Sect. “Introduction” (Table 2): men at age 65 gained 1.3 years and women 2.3 years, representing an annual rate of increase in DFLE—computed using a log-linear regression—of 1.3 and 2.0% which is greater than the increase in total LE. Due to the break in the series, we cannot compare without caution figures for 1991 and 2003; the most recent estimate fits in the range of the three estimates of LE without personal care activity restrictions (in previous surveys, the DFLEs based on this question were relatively low).
The ECHP data for the period 1995–2001 indicate that LE without discomfort due to illness or disability levelled off for women at age 65 and rose slightly for men (Table 3); in view of the sample size, the confidence intervals are larger than the variations. The proportion of LE without discomfort due to illness or disability remains stable at around 46% for men and 40% for women, indicating that the years of life gained over the period are accompanied by such disability.
The ESPS data were used to build three DFLE time series from 1988–1991, 1992–1995, 1996–1998 to 2000–2002 (Table 4). The increase in LE without mobility difficulties, for all levels of severity, is 1.3 years for men and +0.8 years for women; the increase in LE without severe mobility difficulties is 1.4 years for both sexes. LE without difficulty washing/bathing increased faster than total LE (+2.2 years for men and +2.1 years for women), corresponding to an annual rate of increase of +1.3% for men and +1% for women. The confidence intervals do not enable us to draw definite conclusions, but it seems that years of life gained are not years with difficulties in personal care activities, even though the most common mobility limitations occupy a stable proportion of LE at age 65.
Discussion
This study brings together for the first time all the available sets of population data that can be used to estimate DFLE in France over the last two decades, and covering a wide range of disability situations. The DFLE estimates computed from these data reveal several compelling facts. At age 65, years lived with the most common functional limitations account for almost two thirds of the total LE and years lived with personal care activity restrictions for about 10% of total LE. Whatever the disability indicator, women spend a smaller proportion of their LE free of disability; but the more severe the difficulties, the smaller the gender gap, with almost no difference regarding disability or discomfort in 2003. Gains in LE over the last decades may have been years with moderate difficulties expressed by discomfort due to illness or disability (ECHP), but not years with severe disability expressed by difficulties in washing/bathing (ESPS).
The study also highlights the consistency of the patterns observed with similar measurement instruments coming from different surveys; the age-specific prevalence, and consequently the DFLE, appear to be quite stable while applied to the same population and for closely spaced periods of time: physical and sensory functional limitations and personal care activity restrictions from HID and ESSM are very similar (as well as the question on “washing” in ESPS even if a single item is slightly more selective than modules with several personal care items). These question modules appear to be quite robust when similar items are used.
Beside these findings, this study also points out some weaknesses in the data sets or in the computation method. But in most cases, complementary analysis showed that these only slightly influence our conclusions.
First, the computation method imposed by the cross-sectional nature of the datasets may tend to under-estimate DFLE, because it is based on prevalence of disability (stock data) rather than incidence (flow data). The prevalence-based estimates do not correspond literally to “period” indicators as they should; prevalence data do not concentrate on the current risk of disability but represent situations that are influenced by both current and past conditions of life, which the older part of the population have undergone over their life course. The past disabling conditions, due to eradicated disease for instance, that contribute to present disability situations would not be accounted for in current risk of disability onset under the health and life conditions at the beginning of the 2000s. However, the size of the discordance is hard to assess due to contradictory effects, and a recent study on this topic did not find much variation in the final DFLE estimate using incidence or prevalence (Imai and Soneji 2007).
Another limit of the method is to consider the years lived in institution as years of disability, whatever the type of disability, therefore considering a prevalence of 100%. This assumption is motivated by the fact that people are living in an institution because they cannot care for themselves. When considering precise disability situations, this assumption is less acceptable as the persons living in institutions would not all report disability, especially at the most severe levels. The HID survey was designed to be representative of the whole population and so was also conducted in medical institutions and nursing homes in 1998. The prevalence of functional limitation is above 90% for the institutionalized population over age 65, so it is close to the assumption adopted in our calculations. The prevalence of personal care activity restrictions is smaller even at this age (63% for men and 55% for women). These data can be used to assess the size of the error induced by considering that all years in an institution are years of disability; LE without personal care activity restriction at age 65 gains almost 3 months for men and 5 months for women. LE without functional limitations remains practically unchanged due to the very high prevalence of functional limitations among residents of institutions (less than one month’s difference for men and women alike). These differences of a few months are, in most cases, smaller than the confidence intervals presented in the tables which take account of the sample size. We conclude that the impact of this assumption does not change the conclusions.
Limits to our study are also due to the various survey designs and differences in the response rates, as indicated in the literature (Wiener et al. 1990). On the one hand, ill health might be one of the explanatory factors for not participating in surveys, leading to under-estimation of the disability prevalence; on the other hand, being active can also increase the risk of not being contacted or refusing to participate, resulting in over-estimation of the prevalence due to exclusion of healthy people. Our results implicitly assume that those who are excluded have, on average, the same health characteristics as those who participated, whereas they might actually be more or less exposed to disability. We cannot determine to what extent this assumption impacts the results for each survey, in which specific respondent selection processes may occur. This is one of the reasons why we preferred not to pool the data sets. This bias cannot be assessed but can be approached with ESSM by analyzing drop-out from the sample over the 1-month period of data collection (16% of the initial sample for the 65+ age group). In our estimates, we consider implicitly that the drop-outs had the same prevalence of disability as the rest of the sample. We computed DFLE considering that the drop-outs were in fact all experiencing “disability”: under this assumption, LE without functional limitations at age 65 is reduced by 1.5 months for men and women and LE without personal care activity restrictions by 4.5 months for men and 5.5 months for women.
These data rely solely on self-reported information. Changes over time or differences in DFLE also depend on how disability is perceived and reported. This is partly influenced by the respondents level of knowledge about their health in general. The growing desire among older people to remain independent may also have an incentive effect on the reporting of difficulties and need of assistance (Spillman 2004; Wolf et al. 2005), thus increasing the inclination to report disability. Moreover, the reporting variation might depend on the severity of the disability situation; the literature tends to show that the more severe and evident the disability situation, such as personal care activity restrictions, the lower the sensitivity to self-reporting variations (Smith et al. 1990; Tager et al. 1998). Therefore, the stagnation or slight increase in LE with moderate disability in ECHP can be partly explained by an increase in the inclination to report difficulties, due to increased knowledge of respondents on their health status and their higher expectation of good health and functioning.
Our findings not only show consistency between datasets, but they are also congruent with some international results presented in the introduction section. Even if we need to be cautious about trends, France seems to follow the pattern of an increase in LE free of personal care activity restrictions rather than a worsening as found recently in Sweden. No time series are yet available in France to monitor trends in functional limitations and to compare with international findings on this specific dimension; our figures only show an increase in LE with discomfort due to illness or disability in the ECHP, reflecting moderate disability. Trends and patterns in France may be explained by increased knowledge about health in general and about existing services which could make people more aware of their own condition and of how to cope with it. Both individual and environmental resources can contribute to maintaining activity in spite of functional limitations (Cambois et al. 2005). Therefore, even if age-related functional limitations have not been significantly reduced, the diverging patterns of functional limitations and activity restrictions may be explained by better equipment to cope with functional limitation today than 10 years ago. Meanwhile, this change at the individual level could translate at the population level into a trade-off between the need for human assistance for daily activities and the need for special equipment. In any case, whatever the trends observed at the individual levels, increasing needs should be anticipated at the population level due to the ever increasing number of people concerned by these various disability situations in our ageing population.
Acknowledgements
This study was funded by the Research and Statistics Department of the French Ministry of Health (DREES).
References
- Agree E. The influence of personal care and assistive devices on the measurement of disability. Soc Sci Med. 1999;48(4):427–443. doi: 10.1016/S0277-9536(98)00369-4. [DOI] [PubMed] [Google Scholar]
- Auvray L, Doussin A, Le Fur P (2003) Santé, soins et protection sociale en 2002: Enquête Santé et Protection Sociale (ESPS), France [Health, care and social protection in 2002: survey on health and social protection, France]. Rapport IRDES 1509 (2003/12), Paris, pp 181
- Barberger-Gateau P, Rainville C, Letenneur L, Dartigues J-F. A hierarchical model of domains of disablement in the elderly: a longitudinal approach. Disabil Rehabil. 2000;22(7):308–317. doi: 10.1080/096382800296665. [DOI] [PubMed] [Google Scholar]
- Cambois E, Robine J-M, Mormiche P. Did the prevalence of disability in France really fall in the 1990s? A discussion of questions asked in the French health survey. Population E. 2007;62(2):313–326. [Google Scholar]
- Cambois E, Robine JM, Romieu I. Risks of restrictions in personal care activities at older ages: determining the concurrent role of functional limitations, age, sex and place of residence. Disabil Rehabil. 2005;27(15):871–883. doi: 10.1080/09638280500030860. [DOI] [PubMed] [Google Scholar]
- Doussin A, Le Fur P, Dumesnil S (2002) Enquête Santé et Protection Sociale (ESPS) : méthode et déroulement de l’enquête. [“Health, health care and insurance survey” (ESPS): methodology and process of the survey”] Rapport IRDES 1401, (2002/12), Paris, pp 190
- Eurostat (1997) ECHP working group: response rates for the first three waves of the ECHP Doc PAN 92/97
- Fougeyrollas P, Majeau P (1991) Le processus de production des handicaps: comment utiliser le modèle conceptuel: exemple. Réseau international CIDIH 4(3)
- Freedman VA, Agree EM, Martin LG, Cornman JC. Trends in the use of assistive technology and personal care for late-life disability 1992–2001. Gerontologist. 2006;46:124–127. doi: 10.1093/geront/46.1.124. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Crimmins E, Schoeni RF, Spillman BC, Aykan H, Kramarow E, Land K, Lubitz J, Manton K, Martin LG, Shinberg D, Waidman T. Resolving inconsistencies in trends in old-age disability: report from a technical working group. Demography. 2004;41(3):417–441. doi: 10.1353/dem.2004.0022. [DOI] [PubMed] [Google Scholar]
- Hendershot GE. Survey measurement of disability: a review of international activities and recommendations. In: Altman B, Barnartt S, editors. International views on disability measures: moving toward comparative measurement. Oxford: Elsevier; 2006. pp. 17–40. [Google Scholar]
- Imai K, Soneji S. On the estimation of disability-free life expectancy: Sullivan’s method and its extension. J Am Stat Assoc. 2007;102(480):1199–1211. doi: 10.1198/016214507000000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagger C, Arthur A, Spiers N, Clarke M. Patterns of onset of disability in activities of daily living with age. J Am Geriatr Soc. 2001;49(4):404–409. doi: 10.1046/j.1532-5415.2001.49083.x. [DOI] [PubMed] [Google Scholar]
- Jagger C, Cox B, Le Roy S, EHEMU group (2006) Health expectancy calculation by the Sullivan method, 3rd edn. EHEMU Technical Report [downloaded from http://www.ehemu.eu/; training material and calculation guide]
- Katz S, Ford A, Moskowitz R, Jackson B, Jaffe M. Studies of illness in the aged. The Index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185(12):914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Lawrence R, Jette A. Disentangling the disablement process. J Gerontol Soc Sci. 1996;51B(4):S173–S182. doi: 10.1093/geronb/51b.4.s173. [DOI] [PubMed] [Google Scholar]
- Lawton M, Brody E. Assessment of older people: self-maintenance and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- Nagi S. Some conceptual issues in disability and rehabilitation. In: Sussman M, editor. Sociology and rehabilitation. Washington: American Sociological Association; 1965. pp. 100–113. [Google Scholar]
- Office for National Statistics (ONS) Report: health expectancies in the UK, 2002. Health Stat Q. 2006;29:59–62. [PubMed] [Google Scholar]
- Parker MG, Ahacic K, Thorslund M. Health changes among Swedish oldest old: prevalence rates from 1992 and 2002 show increasing health problems. J Gerontol Med Sci. 2005;60(10):1351–1355. doi: 10.1093/gerona/60.10.1351. [DOI] [PubMed] [Google Scholar]
- Perenboom RJ, Van Herten LM, Boshuizen HC, Van Den Bos GA. Trends in disability-free life expectancy. Disabil Rehabil. 2004;26(7):377–386. doi: 10.1080/0963828032000174098. [DOI] [PubMed] [Google Scholar]
- Robine J-M, Michel J-P. Looking forward for a general theory on population aging. J Gerontol A Biol Sci Med Sci. 2004;59:590–597. doi: 10.1093/gerona/59.6.m590. [DOI] [PubMed] [Google Scholar]
- Robine JM, Mormiche P. Estimation de la valeur de l’espérance de vie sans incapacité en France en 1991 [Estimation of the value of disability-free life expectancy in France in 1991] Solidarité Santé. 1994;1:17–36. [Google Scholar]
- Robine JM, Ravaud J-F, Cambois E. General concepts of disablement. In: Hamerman D, editor. Osteoarthritis: public health implication for an aging population. Baltimore: John Hopkins University Press; 1997. pp. 63–83. [Google Scholar]
- Robine JM, Romieu I, Michel JP. Trends in health expectancies. In: Robine JM, Jagger C, Mathers C, Crimmins E, Suzman R, editors. Determining health expectancies. Chichester: Wiley; 2003. pp. 75–101. [Google Scholar]
- Rodgers W, Miller B (1997) A comparative analysis of ADL questions in surveys of older people. J Gerontol B 52B (special issue):21–36 [DOI] [PubMed]
- Sagardui-Villamor J, Guallar-Castillon P, Garcia-Ferruelo M, Banegas JR, Rodriguez-Artalejo F. Trends in disability and disability-free life expectancy among elderly people in Spain: 1986–1999. J Gerontol A Biol Sci Med Sci. 2005;60:1028–1034. doi: 10.1093/gerona/60.8.1028. [DOI] [PubMed] [Google Scholar]
- Smith LA, Branch LG, Scheer PA, Wetle T, Evans DE, Hebert L, Taylor JO. Short-term variability of measures of physical function in older people. J Am Geriatr Soc. 1990;38:993–998. doi: 10.1111/j.1532-5415.1990.tb04422.x. [DOI] [PubMed] [Google Scholar]
- Spillman BC. Changes in elderly disability rates and the implications for health care utilization and cost. Milbank Q. 2004;82(1):157–194. doi: 10.1111/j.0887-378X.2004.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan DF. A single index of mortality and morbidity. HSMHA Health Rep. 1971;86(4):347–354. [PMC free article] [PubMed] [Google Scholar]
- Tager IB, Swanson A, Satariano WA. Reliability of physical performance and self-reported functional measures in an older population. J Gerontol Med Sci. 1998;53A(4):M295–M300. doi: 10.1093/gerona/53a.4.m295. [DOI] [PubMed] [Google Scholar]
- Van Oyen H, van der Heyden J, Perenboom RC, Jagger C. Monitoring population disability: evaluation of a new Global Activity Limitation Indicator (GALI) Soz Praventivmed. 2006;51:153–161. doi: 10.1007/s00038-006-0035-y. [DOI] [PubMed] [Google Scholar]
- Verbrugge L. A global disability indicator. J Aging Stud. 1997;11:337–362. doi: 10.1016/S0890-4065(97)90026-8. [DOI] [Google Scholar]
- Verbrugge L, Jette A. The disablement process. Soc Sci Med. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Verbrugge L, Rennert C, Madans J. The great efficacy of personal and equipment assistance in reducing disability. Am J Public Health. 1997;87(3):384–392. doi: 10.2105/AJPH.87.3.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiener JM, Hanley RJ, Clark R, Van Nostrand JF. Measuring the activity of daily living: comparison across national surveys. J Gerontol Soc Sci. 1990;45(6):S229–S237. doi: 10.1093/geronj/45.6.s229. [DOI] [PubMed] [Google Scholar]
- Wolf DA, Hunt K, Knickman J. Perspectives on the recent decline in disability at older ages. Milbank Q. 2005;83:365–395. doi: 10.1111/j.1468-0009.2005.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood P, Badley E. An epidemiological appraisal of disablement. In: Bennett A, editor. Recent advances in community medicine. Edinburgh: Churchill Livingstone; 1978. pp. 149–173. [Google Scholar]
- World Health Organization (WHO) International classification of impairments, disabilities, and handicaps. Geneva: WHO; 1980. [Google Scholar]
- World Health Organization (WHO) International classification of functioning, disability and health: ICF. Geneva: WHO; 2001. [Google Scholar]


