Abstract
The Disablement Process model proposes a pathway for how chronic diseases in late life can lead to disability, with the variables in the main pathway designated as pathology, impairment, functional limitations, and disability. The model also suggests that psychosocial and contextual variables in the periphery of the model affect disability outcomes. The current study included 149 Swedish adults aged 86, 90, or 94 living in the community or in institutions who answered questions and performed tasks of physical and cognitive ability. A series of regressions were used to test the mediating role of variables within the main pathway of the model, as well as the ability of psychosocial variables to mediate main pathway relationships. Results indicated that physical limitations accounted for between 31 and 52% of the direct effects between impairments and disability, but delayed recall did not mediate these relationships. For the tests of psychosocial variables, mastery was a consistent mediator between impairments and functional limitations, and also mediated several relationships between functional limitations and disability variables. Depression and loneliness also mediated some of the relationships within the main pathway, but explained a smaller percentage of the total effects than mastery. The study concludes that the Disablement Process model is an effective biopsychosocial approach in describing and predicting disability in the oldest-old. In addition, the course of disability seems to be buffered by certain psychosocial variables, particularly feelings of mastery.
Keywords: Disability, Functional ability, Disablement Process model, Oldest-old, Mastery
Introduction
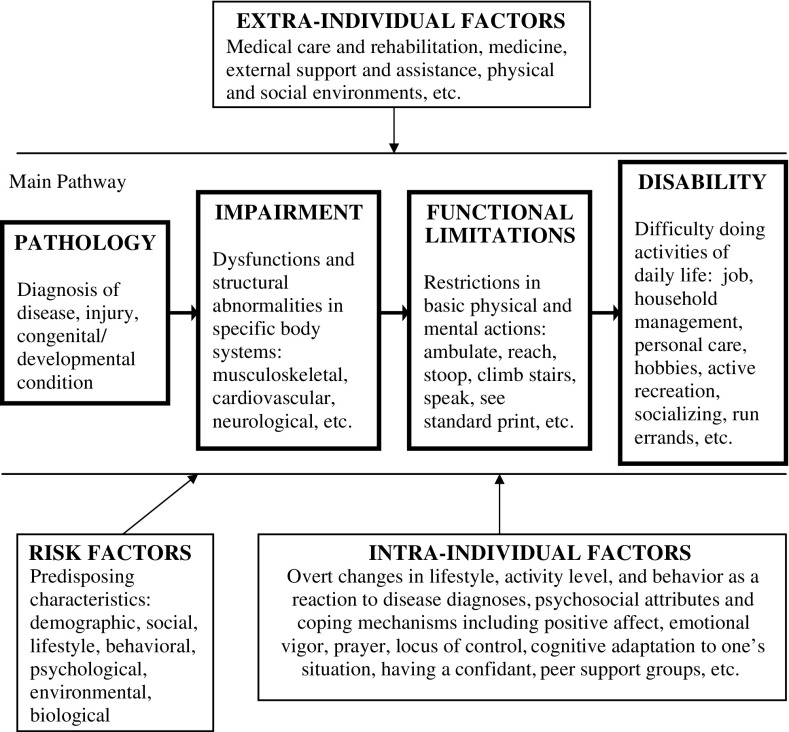
The Disablement Process model (Verbrugge and Jette 1994; Fig. 1) describes how chronic diseases develop into disability, and suggests that contextual and psychological variables affect the course of disablement. Thus, the model helps explain why there is variability in disability outcomes. Because of its biopsychosocial framework, the Disablement Process model is one that is especially useful in gerontology—a field which often requires a multidisciplinary approach.
Fig. 1.
Schematic representation of the Disablement Process model (adapted from Verbrugge and Jette 1994)
A “full” Disablement Process model, incorporating all possible variables discussed by Verbrugge and Jette (1994) has not yet been tested. There have, however, been partial tests published in three noteworthy studies (Femia et al. 2001; Lawrence and Jette 1996; Peek et al. 2003). Using longitudinal analyses, Lawrence and Jette’s (1996) study supported the causal directionality of the relationships between impairments, functional limitations, and disability. Femia et al. (2001) and Peek et al. (2003) found evidence for mediation between variables within the main pathway, as well as evidence that the main pathway variables have indirect effects on disability through various psychosocial factors (depression, subjective health, and social integration in Femia’s study, and perceived support in Peek’s study). In fact, Femia concluded that the results “suggest disability to be as much a function of an individual’s psychosocial characteristics as the degree of functional limitations and functional impairments” (2001, p. 20). Thus, there is support for the organization of the main pathway, and support that functional limitations act as mediators between impairment and disability. In addition, Femia’s study, in particular, illustrates the importance of intra-individual factors as potential buffers to disablement.
Many additional researchers have tested the relationships between specific “main pathway” variables (e.g. disability) and the associations with selected risk, intra-individual, and extra-individual factors. For example, gender (Bauco 1996; Rogers et al. 1992), marital status and ethnicity (Camacho et al. 1993), cognitive abilities (Smits et al. 1997), mastery and neuroticism (Kempen et al. 1999) self-efficacy (Kempen et al. 1999), hardiness (Kobasa et al. 1994), the built environment (Clarke and George 2005) and various aspects of social networks and social support (Camacho et al. 1993; House et al. 1988; Mendes de Leon et al. 1999; Wilcox et al. 1994) have all been found to be related to functional ability and disability in late life (for a more extensive review, see Stuck et al. 1999). Although not all of these studies cite the Disablement Process model, per se, they add additional empirical support for associations between the main pathway and peripheral factors.
Because disablement is a process that occurs over time, there is an inherent directionality to the organization of the model (with the model in Fig. 1 reading from left to right). When the relationships in the model are tested longitudinally, it is possible to capture this time process by allowing variables such as pathology and impairment to be measured at an earlier point in time than outcome variables, such as disability. It is also possible, however, to test the relationships in the model cross-sectionally, as long as the assumptions about directionality are made (that is, we should work from left to right in the model). Both cross-sectional and longitudinal analyses of the Disablement Process model are important in helping us better understand how the factors in the main pathway are related to each other, as well as how the variables in the periphery of the model (such as psychosocial variables) may act as risk or protective factors in the Disablement Process. In addition, although we can use multiple analytic strategies to observe the relationships between these variables in the model (e.g., bivariate tests, multivariate tests, tests of direct effects, tests of moderation) mediation tests, either cross sectional or longitudinal, offer a logical strategy for better understanding the relationships in the Disablement Process model. Mediation allows us to ask whether variable A affects variable C, largely through their relationships to variable B. That is, by testing mediation of the main pathway variables we can see if the effects of impairments on disability seem to work through functional limitations. We can also ask if people’s level of functional limitations are directly associated with their level of disability, and/or if this relationship is explained all, or in part, by the presence of psychosocial risk and protective factors.
The current study uses a cross-sectional design to partially replicate past findings on the mediating relationships between main pathway variables in the Disablement Process model, as well as observe how intra-individual factors mediate main pathway components. Although this is a partial replication of previous research, it uses a sample of Swedish adults who are older than individuals sampled in prior studies. All three previous partial tests of the Disablement Process model have included people over 85, however, in each study, the majority of the sample contained younger-old adults. Lawrence and Jette’s (1996) sample had an average age of 74.18 (sd = 3.73), and was a US sample of non-institutionalized older adults. Only those participants who reported having no functional limitations and no disability at baseline were retained for analyses. In comparison to the current study, their sample is much younger, excludes institutionalized adults, and therefore is potentially less disabled. Peek et al. (2003) study of Mexican American adults had an average aged sample of 72.3 (sd = 6.0), and mostly tested younger-old adults. Femia et al. (2001) studied a Swedish sample with a mean age of 83.4, however, only 27.4% of the sample was over the age of 85. The current study’s sample has an average age of 89.5 (sd = 3.26) and 100% of the sample is over the age of 85. Therefore, from the current data we can test the Disablement Process model specifically in the oldest-old population.
Statement of the problem
The oldest-old (aged 85+), are the group at the highest risk for developing chronic illness and disability. Estimates among those aged 64–74 indicate that 10% of the population experience disability, however, over age 85, the percentage of disability prevalence rises to over 50% (Beckett et al. 1996; Kunkel and Appelbaum 1992). The Disablement Process model is a promising approach for understanding the ways in which older adults may become physically impaired and dependent as a result of their chronic conditions. Only a few studies, however, have tested the Disablement Process model exclusively in samples of people at the most risk for disablement, namely, the oldest-old. The current analyses test the mediating relationships within the Disablement Process (with external factors excluded) to observe whether the relationships presented in the model are supported in this at-risk sample, at one point in time.
Methods
Participants
Participants came from NONA, a longitudinal study of the oldest-old living in the municipality of Jönköping, Sweden. The study utilized a cohort sequential design of individuals aged 86, 90, and 94. This design was chosen to target the oldest-old, while specifically oversampling for nonagenarians. The Swedish population registry was used to identify 100 individuals in each of the three age groups, with a target sample of n = 300. When difficulties arose in finding 94 year olds, several individuals aged 93 and 95 were contacted as well. Of those 300 people contacted, 62 (20.7%) refused participation, 54 (18.0%) were unable to be interviewed due to cognitive or physical impairment(s), 18 (6.0%) died before the initial interview, 8 (2.7%) started but were unable to complete the interview due to frailty, and 11 (3.7%) were unable to participate for other reasons. Therefore the final sample size for the current analysis was n = 149; 40% aged 86 (n = 60), 32% aged 90 (n = 47), 6% aged 93 (n = 9), 19% aged 94 (n = 28), and 3% aged 95 (n = 5). The majority of participants were women (69.8%), and participants had a mean age of 89.5. They reported having an average of 6.79 years of formal schooling which is typical of Swedes in this age cohort. Only 22.1% were currently married, and almost half (47.0%) lived alone. Approximately one-third (32.3%) of participants lived in institutional housing, including nursing homes and service apartments, which are institutional residences similar to assisted living facilities found in countries like the United States.
Procedures
Nurses were trained by the research team in Jönköping to conduct the interviews of NONA participants based on a standard protocol used in prior studies. Initial interviews were monitored carefully to assure that the nurses followed all procedures accurately, and that subjective ratings (vision and hearing) were consistent with the established rating criteria. Participants were interviewed in their residences (both private homes and institutional settings), and they were assessed with measures that used “question and answer” format, as well as via performance-based tasks.
Measures
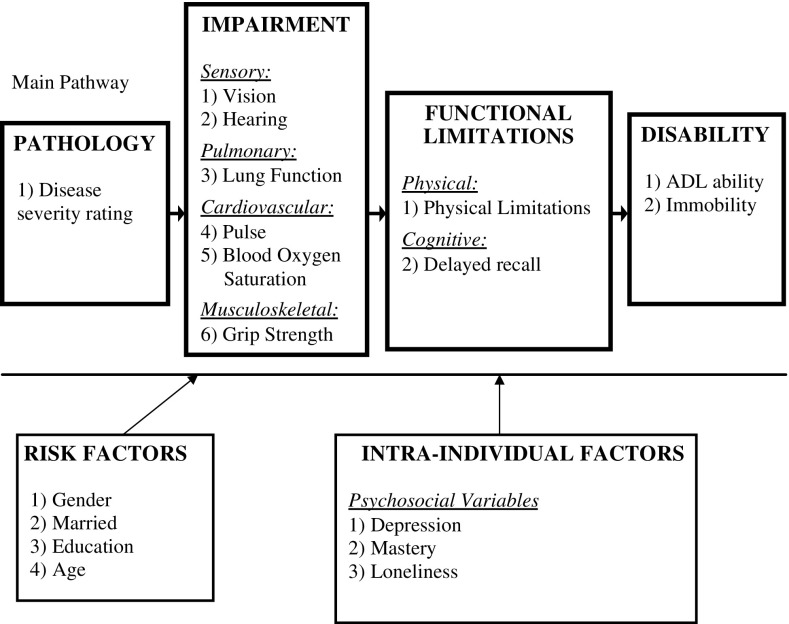
Figure 2 describes how variables used in NONA correspond to constructs in the Disablement Process model. As demonstrated in this figure, extra-individual variables were excluded from analyses because they were not assessed in the interview. Similarly, intra-individual factors were limited to questions about psychosocial attributes, and did not include questions about lifestyle and behavioral changes due to disease and disability, or levels and type of physical activities and exercise.
Fig. 2.
Variables included in analyses
Pathology
Verbrugge and Jette (1994) describe pathology as a “diagnosis of disease, injury, or congenital/developmental condition” (p. 2). In a meta-analysis of functional impairment or disability variables as outcomes, Stuck et al. (1999) found support for significant associations between specific medical conditions and impairment or disability. NONA contained a list of 40 diseases and symptoms, and participants self-reported whether each condition was 1 “currently present” or 0 “not currently present”. Gold et al. (2002) disease severity rating (created by a panel of two MD’s and two MD/PhD’s) was used to code the diseases and symptoms into categories: (1) very life-threatening; (2) somewhat life-threatening; and (3) non life-threatening. In Gold’s research (Gold et al. 2002), the inter-rater reliability of this classification system was 0.78. The current study first coded all 40 conditions using Gold’s classification system, and then, in order to collapse these ratings into one final scale, the participants were assigned a final score of disease severity as: 0 (no diseases were present), 1 (one or more non life-threatening diseases but no somewhat or very life-threatening diseases were present), 2 (one or more somewhat life-threatening diseases but no very life-threatening diseases were present), and 3 (one or more very life threatening conditions were present).
Impairments
Impairments are defined in the Disablement Process model as “dysfunctions and structural abnormalities in specific body systems: musculoskeletal, cardiovascular, neurological, etc.” (Verbrugge and Jette 1994, p. 2). NONA included one or more assessments of ability and dysfunction in the visual, auditory, cardiovascular, pulmonary and muscular systems. Tests and instruments were chosen based on their portability (ease of being brought to the patient’s home and still remaining standardized across homes), and their representativeness of the function of that bodily system.
After interacting with participants during the interview, including asking participants to read text presented in font sized 16, 12, and 8, nurses subjectively rated participants’ vision using a 4-point scale (1 indicating blindness, through 4, indicating no vision problems). Nurse’s ratings of vision and the objective results from the font test were significantly correlated r(126) = 0.75, P < 0.001, and only the 4-point subjective ratings were used in the current study. No objective hearing tests were conducted, however, based on the nurse’s interaction with the participant, hearing was subjectively rated by nurses on a similar 4-point scale (with 1 indicating deafness through 4 indicating no hearing problems).
To measure cardiovascular impairments, a pulse oximeter was placed on the participant’s finger, and two readings were taken while the participant was sitting. An average of these two readings was computed for each individual. This device measures pulse per minute and oxygen saturation in the blood. Low readings of blood oxygen saturation (Potter 2007) and an elevated heart rate (Palatini 2007) indicate problems in the cardiovascular system.
Pulmonary function is often measured via peak expiratory flow, or PEF. PEF is used as a biomarker of overall lung health, and in elderly populations is associated with general physical health, cognition, disability, and death (Cook et al. 1989). PEF was measured by having participants blow forcefully into a spirometer while seated, which measured the maximum liters of air expelled per second. Three trials were performed, and the maximum lung function score was recorded.
Muscular function was assessed via measuring grip strength. Grip strength is an established biomarker of general muscular function, and losses in grip strength are significantly correlated with losses in other muscle groups (Lauretani et al. 2003). In the current study it was measured by having participants squeeze a dynamometer separately with both their right and left hands, for three trials on each hand. The grip strength score was the maximum amount of force participants were able to apply on either hand.
Functional limitations
Measures of functional limitation can include either cognitive limitations or physical limitations. Cognitive limitations were assessed via the delayed recall portion of the Memory in Reality test (or MIR; Johansson 1988/1989). The test asks participants to memorize 10 everyday household objects, and then asks them to place the objects in a replica of an apartment according to the correct room that the objects would be used in. After 30 min, the participants are asked to recall the items, and are scored by the number of items they can correctly recall.
In the current study, physical limitations were measured via a battery of eight tasks used in previous research to assess physical limitations within the Disablement Process model (Femia et al. 2001). These tasks included having participants (1) lift a 1 kg weight with their dominant hand, (2) pick up a pen from the floor, (3) bring their right hand around the back of their head to touch their left ear, (4) bring their left hand around the back of their head to touch their right ear, (5) walk 3 m, turn around and walk back, (6) bring their right finger down to touch their left toe while seated, (7) bring their left finger down to touch their right toe while seated, and (8) cross their arms and try to stand up from a chair. The nurses administering the interview coded the participants on a scale of 1 (no difficulty) to 4 (not able to do at all). Although past studies (Femia et al. 1997, 2001) reduced these tasks into two scales of physical functional limitations, namely, upper body ability and lower body ability, this distinction was less prevalent in the current study. A factor analysis was conducted using principle axis factoring, with VARIMAX rotation, and Eigenvalues over 1 were extracted. The “touching right ear with left hand” task was excluded from these factor analyses because it was highly correlated with the “touching left ear with right hand” task, r(147) = 0.72, P < 0.001). In addition, the “left hand toe touch” task was excluded from the factor analysis because it was highly correlated with the “right hand toe touch” task, r(146) = 0.86, P < 0.001. Results indicated that only one factor could be extracted. Factor loadings on this factor ranged from 0.61 to 0.89, and the Eigenvalue captured 65.36% of the variance. Therefore, based on the factor analyses, a generalized physical limitations scale (α = 0.915) was created for the current study that averaged the participants’ abilities on all eight functional tests.
Disability
Disability was measured using participants’ self-reported ability to perform personal and instrumental activities of daily living, as well as reports of their own general mobility. Personal activities of daily living (PADL; Katz et al. 1963) were measured by asking participants how much of a problem it was for them to bathe or shower, dress/undress, use the toilet, transfer from bed to chair, and feed themselves. Disability in instrumental activities of daily living (IADL; Lawton 1971) included their self-rated ability to clean their home, shop for food, manage transportation, and prepare meals. Possible responses ranged from 0 “cannot do at all” to 3 “no problem”. An overall ADL ability score combined the PADL and IADL items into one scale, with a higher score indicating better ADL functioning.
Immobility was measured by asking participants to describe their ability to get around (1) indoors, (2) outside, and (3) on stairs. Possible responses ranged from 1 “very good ability” to 6 “wholly unable to do”. Ability on these three items was combined, with a higher score indicating more mobility impairment.
Risk factors
Risk factors included: gender, age, marital status (married vs. unmarried/divorced/widowed), and education (in years). Originally whether or not people lived alone was to be included as a risk factor, however, there was a high degree of overlap between marital status and living alone (95% of the sample was either living alone and not married (71%) or not living alone and married (24%)). Therefore, of the two variables, only marital status was used as a risk variable.
Intra-individual factors
Several psychosocial attributes were included as measures of intra-individual factors. Depression was measured using the CES-D (Radloff 1977), which is a 20-item scale assessing the frequency of depressive symptoms occurring in the past week. Sample items included: “I had crying spells” and “I felt that people disliked me”. Responses ranged from 0 “never/nearly never” to 3 “always/nearly always”.
Feelings of mastery or global personal control were assessed using the 8-item Pearlin Mastery Scale (Pearlin and Schooler 1978). Sample items include: “You have little control over the things that happen to you”, and “There is really no way you can solve some of the problems you have”. Participants reported the extent to which they agreed with these statements, with responses ranging from 0 “not at all” to 3 “extremely”. Items were reverse coded such that a higher score indicated higher feelings of mastery (α = 0.759).
Finally, loneliness was assessed using a 5-item measure (Malmberg 1990). Four of these items were originally drawn from the UCLA Loneliness Scale (Russell 1982), and the fifth item, measuring global loneliness, was generated by Malmberg. Participants were asked the extent to which they agreed with the statements, ranging from 1 “not at all agree”, and 4 indicating “agree to a considerable extent” (α = 0.583).
Analyses
Analyses consisted of testing associations (Pearson correlations) and mediation effects (regression models), working left to right, to predict each part of the main pathway with the variables that preceded it. In the first step, correlations were used to determine the presence of significant associations between (1) adjacent variables in the main pathway, (2) risk factors and main pathway variables, and (3) psychosocial variables and main pathway variables. The results of these correlations are presented in Table 2, and were used primarily to dictate which variables were appropriate to include as independent variables in tests of mediation.
Table 2.
Results from Pearson correlation tests of model variables
| Risk factors | Path. | Impairments | Funct. limit. | Disability | Psychosocial | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GEN | AGE | MAR | EDU | DS | VIS | HEA | LF | PUL | BOS | GS | PL | DR | ADL | IM | DE | MY | LO | |
| GEN | 1.00 | |||||||||||||||||
| AGE | −0.02 | 1.00 | ||||||||||||||||
| MAR | −0.57* | −0.12 | 1.00 | |||||||||||||||
| EDU | −0.16 | −0.03 | 0.18 | 1.00 | ||||||||||||||
| DS | −0.04 | 0.11 | −0.04 | −0.04 | 1.00 | |||||||||||||
| VIS | −0.06 | −0.30* | 0.04 | 0.12 | 0.00 | 1.00 | ||||||||||||
| HEA | 0.10 | −0.32* | −0.02 | 0.11 | −0.12 | 0.16 | 1.00 | |||||||||||
| LF | −0.48* | −0.21* | 0.36* | 0.08 | −0.06 | 0.27* | 0.12 | 1.00 | ||||||||||
| PUL | 0.23* | 0.05 | 0.05 | 0.05 | 0.05 | −0.13 | −0.07 | −0.32* | 1.00 | |||||||||
| BOS | 0.08 | −0.01 | 0.01 | 0.07 | −0.13 | 0.15 | −0.12 | 0.10 | 0.07 | 1.00 | ||||||||
| GS | −0.47* | −0.19* | 0.35* | 0.11 | −0.12 | 0.16 | 0.10 | 0.33* | −0.02 | 0.04 | 1.00 | |||||||
| PL | 0.10 | 0.22* | −0.09 | −0.04 | 0.18* | −0.28* | −0.20* | −0.28* | 0.17* | −0.09 | −0.46* | 1.00 | ||||||
| DR | −0.03 | −0.13 | 0.07 | 0.01 | 0.00 | 0.10 | 0.14 | 0.07 | −0.13 | −0.03 | 0.14 | −0.32* | 1.00 | |||||
| ADL | −0.13 | −0.22* | 0.08 | 0.06 | −0.07 | 0.42* | 0.18* | 0.39* | −0.25* | 0.11 | 0.45* | −0.76* | 0.44* | 1.00 | ||||
| IM | 0.16* | 0.21* | −0.08 | −0.01 | 0.17* | −0.36* | −0.15 | −0.36* | 0.19* | −0.17* | −0.39* | 0.79* | −0.14 | −0.72* | 1.00 | |||
| DE | 0.10 | 0.00 | −0.12 | −0.04 | 0.15 | −0.18* | 0.02 | −0.19* | 0.13 | −0.06 | −0.03 | 0.26* | −0.13 | −0.33* | 0.34* | 1.00 | ||
| MY | −0.07 | −0.05 | 0.01 | −0.05 | −0.17* | 0.23* | −0.10 | 0.24* | −0.04 | 0.00 | 0.28* | −0.43* | −0.01 | 0.45* | −0.46* | −0.52* | 1.00 | |
| LO | 0.12 | 0.25* | −0.11 | −0.06 | −0.04 | −0.21* | −0.17* | −0.21* | 0.19* | −0.02 | −0.12 | 0.22* | −0.20* | −0.33* | 0.22* | 0.47* | −0.26* | 1.00 |
GEN = Gender; AGE = Age; MAR = Married; EDU = Education; DS = Disease Severity; VIS = Vision; HEA = Hearing; LF = Lung Function; PUL = Pulse; BOS = Blood Oxygen Saturation; GS = Grip Strength; PL = Physical Limitations; DR = Delayed Recall; ADL = ADL ability; IM = Immobility; DE = Depression; MY = Mastery; LO = Loneliness
* P < 0.05
Mediation models
Independent variables and mediator variables were selected based on the results of the initial correlations, and the dependent variables were impairments, functional limitations, and disability. In all mediation models, the risk factors that were significantly correlated with the independent, mediator, or dependent variables were controlled for by entering them first in the model. The classic Baron and Kenny (1986) approach was then used in testing mediation. To establish mediation, three criteria were necessary. There needed to be a significant direct effect between the independent and dependent variables (step A), a significant direct effect between the independent and mediator variables (step B), and a significant effect of the mediator on the dependent variable, after controlling for the independent variable (step C). An additional way to test mediation involved including a statistical measure of the strength of mediation. Sobel’s test was used to measure whether a critical ratio of the indirect effect of the independent variable on the dependent variable through the mediator was significantly different from zero (Sobel 1982). In Sobel’s test, a represents the unstandardized regression coefficient between the independent and mediator variables (sa = standard error of a) and b represents the unstandardized coefficient between the mediator and dependent variables (sb = the standard error of b). Sobel’s equation is: 
Finally, an equation provided by Mackinnon and Dwyer (1993) was used to determine the degree to which the mediator explained the direct effect between the independent variable (IV) on the dependent variable (DV).
 |
The first series of mediation models tested whether there were mediating relationships within the main pathway, for example, impairments would be tested as a mediator between disease and functional limitations, and functional limitations would be tested as mediators between impairments and disability. The other series of mediation models tested whether there were mediating relationships within the main pathway via the intra-individual factors. Psychosocial variables were tested to see if they mediated: (1) the relationship between disease and impairments, (2) the relationships between impairments and functional limitations, and (3) the relationships between functional limitations and disability.
Results
The descriptive statistics of variables included in the analyses are presented in Table 1. As discussed previously, the correlations will not be discussed in the text of the paper, but these results are presented in Table 2.
Table 1.
Descriptive Information for the sample
| N | % or mean (sd) | |
|---|---|---|
| Risk factors | ||
| Gender: % women | 149 | 69.8% |
| % Married (vs. unmarried, widowed, divorced) | 147 | 22.1% |
| Education in years of schooling | 148 | 6.79 (1.74) |
| Age | 149 | 89.49 (3.26) |
| Pathology | ||
| Disease severity (possible range: 0 “no diseases present”–3 “one or more very-life-threatening diseases present”) | 141 | 1.82 (1.03) |
| Impairments | ||
| Vision (possible range: 1 “Blind/Nearly Blind”–4 “No problems”) | 148 | 3.40 (0.78) |
| Hearing (possible range: 1 “Deaf/Nearly Deaf”–4 “No problems”) | 149 | 3.52 (0.63) |
| Lung Function (l/s) | 133 | 259.79 (115.01) |
| Pulse (per minute) | 146 | 70.51 (12.34) |
| Blood Oxygen Saturation (% of bound hemoglobin) | 146 | 95.14 (3.57) |
| Grip Strength (pounds per square inch) | 142 | 0.57 (0.20) |
| Functional Limitations | ||
| Physical Limitations (possible range:1 “no difficulty”–4 “unable to do”) | 149 | 1.84 (0.97) |
| Memory: Delayed recall (# correct out of 10) | 132 | 5.19 (2.57) |
| Disability | ||
| ADL (possible range: 0 “can’t do at all”–3 “can do without problems”) | 149 | 2.27 (0.90) |
| Immobility (possible range:1 “very good ability”–6 “unable to do at all”) | 145 | 2.54 (1.60) |
| Psychosocial factors | ||
| Depression (CES-D score: possible range: 0–60) | 133 | 9.37 (8.01) |
| Mastery (possible range: 0 Feel this way “not at all”–3 “extremely”) | 132 | 2.09 (0.64) |
| Loneliness (possible range: 1 Feel this way “not at all–4”extremely”) | 140 | 1.71 (0.54) |
Risk factors
Results from the correlations between risk factors (gender, age, marital status, and education), and main pathway variables indicated that education was not significantly related to any main pathway variables and was therefore excluded from all future models. Being female was related to lower lung function and grip strength, and higher scores on pulse and immobility. Being older was related to poorer vision, hearing, lung function, and grip strength, and to greater physical limitations, greater immobility, and higher feelings of loneliness. Participants who were married had higher lung function and grip strength, however, it should be noted that being married was also significantly negatively correlated (r = −0.57) with being female (most married participants were male).
Main pathway variables as mediators
The tests of whether functional impairments mediated the relationships between disease severity and functional limitations were not pursued because disease severity did not have any significant correlations with impairments. The correlation results did, however, support testing whether functional limitations mediated the relationships between impairments and disability (models 1–9). Model 1 tested whether the functional limitations variable of physical limitations (difficulty performing the series of functional tests like standing, walking, bending, etc.) mediated the relationship between the impairment variable of vision and the disability variable of ADL ability. Results from the regression models (Table 3) and the two follow-up tests (Sobel’s test and the percent of the direct effect explained by the mediator, Table 6) indicated that physical limitations was a significant mediator, explaining 31.8% of the direct effect between vision and ADL ability. Although a large amount of the original effect was mediated through physical limitations, the beta weight for the effect of vision on ADL ability was not reduced to zero (model 1.C), therefore this should be considered an example of partial mediation (as opposed to “full mediation”). Model 2 indicated that physical limitations significantly mediated the relationship between vision and immobility, explaining 31.8% of the direct effect, however, this, too, represents partial mediation. Model 3 was not pursued for mediation testing, because although correlations were significant between hearing and ADL ability and between hearing and physical limitations (Table 2), these relationships were not significant after controlling for age (see models 3.A and 3.B in Table 3). Models 4 and 5 indicated that physical limitations significantly mediated the relationship between lung function and ADL ability (explaining 36.4% of the direct effect), and between lung function and immobility (explaining 38.0% of the direct effect), however, both of these models should be interpreted as partial mediation, because lung function was still significant in models 4.C and 5.C. Models 6 did not demonstrate that physical limitations mediated the relationship between pulse and ADL ability because the direct effect between pulse and physical limitations (model 6.B) was not significant after controlling for age and gender. Likewise, model 7 did not demonstrate that physical limitations mediated the relationship between pulse and immobility because the direct effects between pulse and immobility (model 7.A) and between pulse and physical limitations (model 7.B) were not significant after controlling for age and gender. Models 8 and 9 demonstrated that physical limitations significantly and partially mediated grip strength and ADL ability (explaining 44.0% of the direct effect between grip strength and ADL ability), and significantly and fully mediated grip strength and immobility (explaining 52.1% of the direct effect between grip strength and immobility).
Table 3.
Main pathway mediation models: functional limitations as mediators
| Model (Dep. Variable) | Predictor variable | B | Std. error | Beta | P value | Model R 2 |
|---|---|---|---|---|---|---|
| 1.A (ADL ability) | Constant | 3.28 | 2.00 | 0.10 | 0.18 | |
| Age | −0.03 | 0.02 | −0.10 | 0.19 | ||
| Vision | 0.44 | 0.09 | 0.39* | 0.00 | ||
| 1.B (Physical limitations) | Constant | −0.97 | 2.26 | 0.67 | 0.10 | |
| Age | 0.04 | 0.02 | 0.15 | 0.08 | ||
| Vision | −0.29 | 0.10 | −0.24* | 0.00 | ||
| 1.C (ADL ability) | Constant | 2.66 | 1.38 | 0.06 | 0.61 | |
| Age | 0.00 | 0.01 | 0.00 | 0.97 | ||
| Vision | 0.25 | 0.06 | 0.22* | 0.00 | ||
| Physical limitations | −0.64 | 0.05 | −0.69* | 0.00 | ||
| 2.A (Immobility) | Constant | −1.11 | 3.81 | 0.77 | 0.16 | |
| Age | 0.06 | 0.04 | 0.12 | 0.16 | ||
| Gender | 0.47 | 0.27 | 0.14 | 0.08 | ||
| Vision | −0.63 | 0.17 | −0.31* | 0.00 | ||
| 2.B (Physical limitations) | Constant | −1.34 | 2.30 | 0.55 | 0.11 | |
| Age | 0.04 | 0.02 | 0.15 | 0.07 | ||
| Gender | 0.17 | 0.16 | 0.08 | 0.30 | ||
| Vision | −0.28 | 0.10 | −0.23* | 0.01 | ||
| 2.C (Immobility) | Constant | −0.32 | 2.48 | 0.90 | 0.65 | |
| Age | 0.01 | 0.03 | 0.02 | 0.74 | ||
| Gender | 0.34 | 0.17 | 0.10 | 0.06 | ||
| Vision | −0.23 | 0.11 | −0.11* | 0.04 | ||
| Physical limitations | 1.27 | 0.09 | 0.74* | 0.00 | ||
| 3.A (ADL ability) | Constant | 5.93 | 2.24 | 0.01 | 0.06 | |
| Age | −0.05 | 0.02 | −0.18* | 0.04 | ||
| Hearing | 0.18 | 0.12 | 0.13 | 0.14 | ||
| 3.B (Physical Limitations) | Constant | −1.79 | 2.41 | 0.46 | 0.07 | |
| Age | 0.05 | 0.03 | 0.17* | 0.05 | ||
| Hearing | −0.23 | 0.13 | −0.15 | 0.08 | ||
| 3.C (ADL ability) | Constant | 4.69 | 1.50 | 0.00 | 0.58 | |
| Age | −0.01 | 0.02 | −0.05 | 0.38 | ||
| Hearing | 0.02 | 0.08 | 0.02 | 0.78 | ||
| Physical limitations | −0.69 | 0.05 | −0.75* | 0.00 | ||
| 4.A (ADL ability) | Constant | 1.99 | 2.02 | 0.33 | 0.18 | |
| Age | −0.01 | 0.02 | −0.02 | 0.79 | ||
| Gender | 0.11 | 0.18 | 0.06 | 0.56 | ||
| Married | −0.02 | 0.19 | −0.01 | 0.91 | ||
| Lung function | 0.00 | 0.00 | 0.44* | 0.00 | ||
| 4.B (Physical limitations) | Constant | 1.48 | 2.32 | 0.53 | 0.10 | |
| Age | 0.01 | 0.02 | 0.04 | 0.63 | ||
| Gender | −0.15 | 0.21 | −0.08 | 0.49 | ||
| Married | −0.20 | 0.22 | −0.10 | 0.34 | ||
| Lung function | −0.00 | 0.00 | −0.29* | 0.00 | ||
| 4.C (ADL ability) | Constant | 2.79 | 1.59 | 0.08 | 0.50 | |
| Age | 0.00 | 0.02 | 0.00 | 0.96 | ||
| Gender | 0.03 | 0.14 | 0.02 | 0.85 | ||
| Married | −0.13 | 0.15 | −0.07 | 0.38 | ||
| Lung function | 0.00 | 0.00 | 0.27* | 0.00 | ||
| Physical limitations | −0.54 | 0.06 | −0.60* | 0.00 | ||
| 5.A (Immobility) | Constant | 4.72 | 3.77 | 0.21 | 0.13 | |
| Age | −0.01 | 0.04 | −0.03 | 0.77 | ||
| Gender | −0.11 | 0.34 | −0.04 | 0.74 | ||
| Married | −0.05 | 0.35 | −0.01 | 0.89 | ||
| Lung function | −0.00 | 0.00 | −0.38* | 0.00 | ||
| 5.B (Physical limitations) | Constant | 1.48 | 2.32 | 0.53 | 0.10 | |
| Age | 0.01 | 0.02 | 0.04 | 0.63 | ||
| Gender | −0.15 | 0.21 | −0.08 | 0.49 | ||
| Married | −0.20 | 0.22 | −0.10 | 0.36 | ||
| Lung function | −0.00 | 0.00 | −0.29* | 0.00 | ||
| 5.C (Immobility) | Constant | 2.60 | 2.55 | 0.31 | 0.61 | |
| Age | −0.02 | 0.03 | −0.05 | 0.40 | ||
| Gender | 0.10 | 0.23 | 0.03 | 0.68 | ||
| Married | 0.19 | 0.24 | 0.06 | 0.41 | ||
| Lung function | −0.00 | 0.00 | −0.18* | 0.01 | ||
| Physical limitations | 1.24 | 0.10 | 0.72* | 0.00 | ||
| 6.A (ADL ability) | Constant | 7.95 | 1.93 | 0.00 | 0.10 | |
| Age | −0.05 | 0.02 | −0.18* | 0.03 | ||
| Gender | −0.12 | 0.15 | −0.07 | 0.42 | ||
| Pulse | −0.02 | 0.01 | −0.23* | 0.01 | ||
| 6.B (Physical limitations) | Constant | −3.80 | 2.13 | 0.08 | 0.06 | |
| Age | 0.05 | 0.02 | 0.18* | 0.03 | ||
| Gender | 0.10 | 0.17 | 0.05 | 0.54 | ||
| Pulse | 0.01 | 0.01 | 0.15 | 0.08 | ||
| 6.C (ADL ability) | Constant | 5.44 | 1.35 | 0.00 | 0.57 | |
| Age | −0.01 | 0.01 | −0.05 | 0.36 | ||
| Gender | −0.06 | 0.11 | −0.03 | 0.60 | ||
| Pulse | −0.01 | 0.00 | −0.12* | 0.03 | ||
| Physical limitations | −0.66 | 0.05 | −0.71* | 0.00 | ||
| 7.A (Immobility) | Constant | −7.12 | 3.55 | 0.05 | 0.08 | |
| Age | 0.08 | 0.04 | 0.18* | 0.03 | ||
| Gender | 0.39 | 0.28 | 0.12 | 0.16 | ||
| Pulse | 0.02 | 0.01 | 0.16 | 0.06 | ||
| 7.B (Physical limitations) | Constant | −3.80 | 2.13 | 0.08 | 0.06 | |
| Age | 0.05 | 0.02 | 0.18* | 0.03 | ||
| Gender | 0.10 | 0.17 | 0.05 | 0.54 | ||
| Pulse | 0.01 | 0.01 | 0.15 | 0.08 | ||
| 7.C (Immobility) | Constant | −2.56 | 2.33 | 0.27 | 0.61 | |
| Age | 0.02 | 0.03 | 0.05 | 0.40 | ||
| Gender | 0.32 | 0.18 | 0.10 | 0.08 | ||
| Pulse | 0.00 | 0.01 | 0.03 | 0.55 | ||
| Physical limitations | 1.28 | 0.09 | 0.75* | 0.00 | ||
| 8.A (ADL ability) | Constant | 3.75 | 1.89 | 0.05 | 0.23 | |
| Age | −0.03 | 0.02 | −0.11 | 0.16 | ||
| Gender | 0.02 | 0.17 | 0.01 | 0.90 | ||
| Married | −0.12 | 0.18 | −0.06 | 0.49 | ||
| Grip Strength | 1.88 | 0.35 | 0.47* | 0.00 | ||
| 8.B (Physical limitations) | Constant | 1.49 | 2.09 | 0.47 | 0.23 | |
| Age | 0.02 | 0.02 | 0.07 | 0.35 | ||
| Gender | −0.17 | 0.19 | −0.09 | 0.36 | ||
| Married | 0.01 | 0.20 | 0.01 | 0.95 | ||
| Grip strength | −2.20 | 0.39 | −0.50* | 0.00 | ||
| 8.C (ADL ability) | Constant | 4.61 | 1.47 | 0.00 | 0.54 | |
| Age | −0.02 | 0.02 | −0.06 | 0.30 | ||
| Gender | −0.08 | 0.13 | −0.04 | 0.56 | ||
| Married | −0.11 | 0.14 | −0.06 | 0.41 | ||
| Grip strength | 0.62 | 0.30 | 0.15* | 0.04 | ||
| Physical limitations | −0.58 | 0.06 | −0.64* | 0.00 | ||
| 9.A (Immobility) | Constant | 0.46 | 3.68 | 0.90 | 0.16 | |
| Age | 0.04 | 0.04 | 0.08 | 0.35 | ||
| Gender | 0.20 | 0.33 | 0.06 | 0.56 | ||
| Married | 0.18 | 0.34 | 0.05 | 0.61 | ||
| Grip strength | −2.70 | 0.68 | −0.37* | 0.00 | ||
| 9.B (Physical limitations) | Constant | 1.49 | 2.09 | 0.48 | 0.23 | |
| Age | 0.02 | 0.02 | 0.07 | 0.35 | ||
| Gender | −0.17 | 0.19 | −0.09 | 0.36 | ||
| Married | 0.01 | 0.20 | 0.01 | 0.95 | ||
| Grip strength | −2.20 | 0.39 | −0.50* | 0.00 | ||
| 9.C (Immobility) | Constant | −1.75 | 2.54 | 0.49 | 0.61 | |
| Age | 0.01 | 0.03 | 0.03 | 0.63 | ||
| Gender | 0.45 | 0.23 | 0.14* | 0.05 | ||
| Married | 0.15 | 0.24 | 0.04 | 0.53 | ||
| Grip strength | 0.03 | 0.52 | 0.00 | 0.95 | ||
| Physical limitations | 1.31 | 0.11 | 0.76* | 0.00 |
Note: B is the unstandardized regression coefficient, Std. error is the standard error for this coefficient, and Beta is the standardized regression coefficient; * P value was <0.05; −0.00 represents a negative value that appears in the table as negative zero because only 2 decimal places were used. Models denoted by letter A indicate that this model tests the direct effect between the independent variable and the outcome variable; models denoted by letter B indicate that this model tests the direct effect between the independent variable and the mediator variable; models denoted by letter C indicate that this model tests the mediating effect between the independent variable and the outcome variable
Table 6.
Summary of mediation effects
| Model# | Predictor | Mediator | Outcome | Sobel’s test | Percent of total effect explained by the mediator (%) |
|---|---|---|---|---|---|
| 1 | Vision | Physical limitations | ADL ability | 2.84* | 31.8 |
| 2 | Vision | Physical limitations | Immobility | −2.75* | 36.4 |
| 4 | Lung function | Physical limitations | ADL ability | 1.98* | 32.5 |
| 5 | Lung function | Physical limitations | Immobility | −2.95* | 38.0 |
| 8 | Grip strength | Physical limitations | ADL ability | 5.21* | 44.0 |
| 9 | Grip strength | Physical limitations | Immobility | −5.28* | 52.1 |
| 10 | Vision | Depression | Physical limitations | −1.77† | 17.2 |
| 11 | Vision | Mastery | Physical limitations | −2.26* | 28.6 |
| 15 | Lung function | Mastery | Physical limitations | −2.32* | 27.0 |
| 18 | Grip strength | Mastery | Physical limitations | −2.55* | 18.6 |
| 19 | Physical limitations | Depression | ADL ability | −2.18* | 10.2 |
| 20 | Physical limitations | Mastery | ADL ability | −3.92* | 19.6 |
| 21 | Physical limitations | Loneliness | ADL ability | 1.88† | 6.8 |
| 22 | Physical limitations | Depression | Immobility | 2.16* | 10.1 |
| 23 | Physical limitations | Mastery | Immobility | 3.87* | 20.1 |
| 25 | Delayed recall | Loneliness | ADL ability | 1.39 | 10.6 |
Note: Models 3, 6, 7, 12, 13, 14, 16, 17, and 24 had one or more portions of the mediation testing (A, B, or C) where key variables were non-significant, thus disqualifying the models from subsequent analyses of Sobel’s test or testing the % of the total effect explained by the mediator
* Statistical significance at a level of P < 0.05
†Indicates marginal significance at a level of P < 0.10
Psychosocial variables as mediators
It was originally planned to test psychosocial variables as mediators between (1) disease and impairment, (2) impairment and functional limitations, and (3) functional limitations and disability. The first of these tests was not run because there were no significant correlations between disease severity and impairments. It should be noted, however, that disease severity was significantly correlated with mastery (a psychosocial variable), and mastery was correlated with several impairment variables (vision, lung function, and grip strength). Therefore, while one of the main criterion for mediation (step A) was not met, we should consider the idea that indirect effects may still play a role in the relationships between disease severity, mastery, and the impairment variables of vision, lung function, and grip strength. Full mediation testing on the other two analyses (items 2 and 3 from above) were pursued, and are displayed in Tables 4 and 5. Follow-up tests (Sobel’s tests and the percent of the direct effect explained by the mediator) are presented for all mediation models in Table 6.
Table 4.
Psychosocial mediation between impairments and functional limitations
| Model (Dep. variable) | Predictor variable | B | Std. error | Beta | P value | Model R 2 |
|---|---|---|---|---|---|---|
| 10.A (Physical limitations) | (Constant) | −0.97 | 2.26 | 0.67 | 0.10 | |
| Age | 0.04 | 0.02 | 0.15 | 0.08 | ||
| Vision | −0.29 | 0.10 | −0.24* | 0.00 | ||
| 10.B (Depression) | (Constant) | 30.32 | 21.13 | 0.15 | 0.04 | |
| Age | −0.15 | 0.22 | −0.06 | 0.49 | ||
| Vision | −2.09 | 0.95 | −0.20* | 0.03 | ||
| 10.C (Physical limitations) | (Constant) | 0.74 | 2.22 | 0.74 | 0.13 | |
| Age | 0.02 | 0.02 | 0.07 | 0.44 | ||
| Vision | −0.25 | 0.10 | −0.22* | 0.01 | ||
| Depression | 0.02 | 0.01 | 0.23* | 0.01 | ||
| 11.A (Physical limitations) | (Constant) | −0.97 | 2.26 | 0.67 | 0.10 | |
| Age | 0.04 | 0.02 | 0.15 | 0.08 | ||
| Vision | −0.29 | 0.10 | −0.24* | 0.00 | ||
| 11.B (Mastery) | (Constant) | 0.93 | 1.71 | 0.59 | 0.05 | |
| Age | 0.01 | 0.02 | 0.03 | 0.77 | ||
| Vision | 0.20 | 0.08 | 0.24* | 0.01 | ||
| 11.C (Physical limitations) | (Constant) | 2.23 | 2.13 | 0.30 | 0.22 | |
| Age | 0.01 | 0.02 | 0.05 | 0.53 | ||
| Vision | −0.21 | 0.10 | −0.18* | 0.03 | ||
| Mastery | −0.52 | 0.11 | −0.38* | 0.00 | ||
| 12.A (Physical limitations) | (Constant) | −0.97 | 2.26 | 0.67 | 0.10 | |
| Age | 0.04 | 0.02 | 0.15 | 0.08 | ||
| Vision | −0.29 | 0.10 | −0.24* | 0.00 | ||
| 12.B (Loneliness) | (Constant) | −0.91 | 1.35 | 0.50 | 0.08 | |
| Age | 0.03 | 0.01 | 0.20* | 0.02 | ||
| Vision | −0.10 | 0.06 | −0.15 | 0.08 | ||
| 12.C (Physical limitations) | (Constant) | 0.66 | 2.22 | 0.77 | 0.13 | |
| Age | 0.02 | 0.02 | 0.07 | 0.41 | ||
| Vision | −0.32 | 0.10 | −0.27* | 0.00 | ||
| Loneliness | 0.25 | 0.14 | 0.15 | 0.08 | ||
| 13.A (Physical limitations) | (Constant) | −1.79 | 2.41 | 0.46 | 0.07 | |
| Age | 0.05 | 0.02 | 0.17* | 0.05 | ||
| Hearing | −0.23 | 0.13 | −0.15 | 0.08 | ||
| 13.B (Loneliness) | (Constant) | −1.13 | 1.38 | 0.42 | 0.07 | |
| Age | 0.04 | 0.01 | 0.21* | 0.01 | ||
| Hearing | −0.09 | 0.08 | −0.11 | 0.21 | ||
| 13.C (Physical limitations) | (Constant) | −1.44 | 2.34 | 0.54 | 0.07 | |
| Age | 0.03 | 0.02 | 0.12 | 0.17 | ||
| Hearing | −0.11 | 0.13 | −0.07 | 0.41 | ||
| Loneliness | 0.30 | 0.14 | 0.18* | 0.04 | ||
| 14.A (Physical limitations) | (Constant) | 1.48 | 2.32 | 0.53 | 0.10 | |
| Age | 0.01 | 0.02 | 0.04 | 0.63 | ||
| Gender | −0.15 | 0.21 | −0.08 | 0.49 | ||
| Married | −0.20 | 0.22 | −0.10 | 0.36 | ||
| Lung function | −0.00 | 0.00 | −0.29* | 0.00 | ||
| 14.B (Depression) | (Constant) | 47.05 | 21.18 | 0.03 | 0.07 | |
| Age | −0.37 | 0.22 | −0.16 | 0.09 | ||
| Gender | −0.85 | 1.90 | −0.05 | 0.66 | ||
| Married | −2.32 | 1.94 | −0.13 | 0.23 | ||
| Lung function | −0.01 | 0.01 | −0.20 | 0.06 | ||
| 14.C (Physical limitations) | (Constant) | 1.55 | 2.24 | 0.49 | 0.09 | |
| Age | 0.00 | 0.02 | 0.02 | 0.84 | ||
| Gender | −0.04 | 0.20 | −0.03 | 0.83 | ||
| Married | −0.07 | 0.20 | −0.04 | 0.74 | ||
| Lung function | −0.00 | 0.00 | −0.23* | 0.03 | ||
| Depression | 0.02 | 0.01 | 0.15 | 0.12 | ||
| 15.A (Physical limitations) | (Constant) | 1.48 | 2.32 | 0.53 | 0.10 | |
| Age | 0.01 | 0.02 | 0.04 | 0.63 | ||
| Gender | −0.15 | 0.21 | −0.08 | 0.49 | ||
| Married | −0.20 | 0.22 | −0.10 | 0.36 | ||
| Lung function | −0.00 | 0.00 | −0.29* | 0.00 | ||
| 15.B (Mastery) | (Constant) | 0.02 | 1.71 | 0.99 | 0.07 | |
| Age | 0.02 | 0.02 | 0.10 | 0.29 | ||
| Gender | 0.04 | 0.16 | 0.03 | 0.79 | ||
| Married | 0.01 | 0.16 | 0.01 | 0.94 | ||
| Lung function | 0.00 | 0.00 | 0.27* | 0.01 | ||
| 15.C (Physical limitations) | (Constant) | 2.33 | 2.10 | 0.27 | 0.17 | |
| Age | 0.01 | 0.02 | 0.02 | 0.79 | ||
| Gender | −0.02 | 0.19 | −0.01 | 0.92 | ||
| Married | −0.09 | 0.19 | −0.05 | 0.66 | ||
| Lung function | −0.00 | 0.00 | −0.17 | 0.10 | ||
| Mastery | −0.42 | 0.11 | −0.33* | 0.00 | ||
| 16.A (Physical limitations) | (Constant) | 1.48 | 2.32 | 0.53 | 0.10 | |
| Age | 0.01 | 0.02 | 0.04 | 0.63 | ||
| Gender | −0.15 | 0.21 | −0.08 | 0.49 | ||
| Married | −0.20 | 0.22 | −0.10 | 0.36 | ||
| Lung function | −0.00 | 0.00 | −0.29* | 0.00 | ||
| 16.B (Loneliness) | (Constant) | 1.17 | 1.34 | 0.39 | 0.05 | |
| Age | 0.01 | 0.01 | 0.05 | 0.57 | ||
| Gender | −0.01 | 0.12 | −0.01 | 0.96 | ||
| Married | −0.07 | 0.12 | −0.06 | 0.59 | ||
| Lung function | −0.00 | 0.00 | −0.19 | 0.08 | ||
| 16.C (Physical limitations) | (Constant) | 1.96 | 2.21 | 0.38 | 0.09 | |
| Age | 0.00 | 0.02 | 0.01 | 0.87 | ||
| Gender | −0.07 | 0.20 | −0.04 | 0.73 | ||
| Married | −0.12 | 0.20 | −0.06 | 0.56 | ||
| Lung function | −0.00 | 0.00 | −0.29* | 0.01 | ||
| Loneliness | −0.01 | 0.15 | −0.01 | 0.92 | ||
| 17. A(Physical limitations) | (Constant) | −3.80 | 2.13 | 0.08 | 0.06 | |
| Age | 0.05 | 0.02 | 0.18* | 0.03 | ||
| Gender | 0.10 | 0.17 | 0.05 | 0.54 | ||
| Pulse | 0.01 | 0.01 | 0.15 | 0.08 | ||
| 17.B (Loneliness) | (Constant) | −2.18 | 1.22 | 0.08 | 0.09 | |
| Age | 0.04 | 0.01 | 0.22 | 0.01 | ||
| Gender | 0.08 | 0.10 | 0.07 | 0.39 | ||
| Pulse | 0.01 | 0.00 | 0.17* | 0.05 | ||
| 17.C (Physical limitations) | (Constant) | −2.34 | 2.10 | 0.27 | 0.06 | |
| Age | 0.03 | 0.02 | 0.13 | 0.15 | ||
| Gender | 0.11 | 0.17 | 0.06 | 0.50 | ||
| Pulse | 0.01 | 0.01 | 0.10 | 0.26 | ||
| Loneliness | 0.21 | 0.15 | 0.12 | 0.16 | ||
| 18.A (Physical limitations) | (Constant) | 1.49 | 2.09 | 0.48 | 0.23 | |
| Age | 0.02 | 0.02 | 0.07 | 0.35 | ||
| Gender | −0.17 | 0.19 | −0.09 | 0.36 | ||
| Married | 0.01 | 0.20 | 0.01 | 0.94 | ||
| Grip strength | −2.20 | 0.39 | −0.50* | 0.00 | ||
| 18.B (Mastery) | (Constant) | 1.18 | 1.64 | 0.47 | 0.08 | |
| Age | 0.01 | 0.02 | 0.03 | 0.77 | ||
| Gender | −0.02 | 0.15 | −0.01 | 0.92 | ||
| Married | −0.03 | 0.15 | −0.02 | 0.84 | ||
| Grip strength | 0.88 | 0.30 | 0.29* | 0.00 | ||
| 18.C (Physical limitations) | (Constant) | 2.40 | 1.96 | 0.22 | 0.28 | |
| Age | 0.01 | 0.02 | 0.05 | 0.53 | ||
| Gender | −0.07 | 0.18 | −0.04 | 0.68 | ||
| Married | 0.09 | 0.18 | 0.05 | 0.61 | ||
| Grip strength | −1.51 | 0.38 | −0.37* | 0.00 | ||
| Mastery | −0.43 | 0.11 | −0.32* | 0.00 |
Note: B is the unstandardized regression coefficient, Std. error is the standard error for this coefficient, and Beta is the standardized regression coefficient; * P-value was <0.05; −0.00 represents a negative value that appears in the table as negative zero because only 2 decimal places were used. Models denoted by letter A indicate that this model tests the direct effect between the independent variable and the outcome variable; models denoted by letter B indicate that this model tests the direct effect between the independent variable and the mediator variable; models denoted by letter C indicate that this model tests the mediating effect between the independent variable and the outcome variable. On several occasions, the R 2 values of model version C are less than those of version A, which is due the listwise deletion of cases missing data on the psychosocial mediator variables
Table 5.
Psychosocial mediation between functional limitations and disability
| Model (Dep. variable) | Predictor variable | B | Std. error | Beta | P value | Model R 2 |
|---|---|---|---|---|---|---|
| 19.A (ADL ability) | (Constant) | 4.88 | 1.32 | 0.00 | 0.58 | |
| Age | −0.01 | 0.01 | −0.05 | 0.32 | ||
| Physical limitations | −0.70 | 0.05 | −0.75* | 0.00 | ||
| 19. B (Depression) | (Constant) | 13.87 | 18.77 | 0.46 | 0.07 | |
| Age | −0.10 | 0.21 | −0.04 | 0.64 | ||
| Physical limitations | 2.47 | 0.78 | 0.27* | 0.00 | ||
| 19.C (ADL ability) | (Constant) | 4.39 | 1.30 | 0.00 | 0.53 | |
| Age | −0.01 | 0.01 | −0.04 | 0.53 | ||
| Physical limitations | −0.59 | 0.06 | −0.67* | 0.00 | ||
| Depression | −0.01 | 0.01 | −0.15* | 0.02 | ||
| 20.A (ADL ability) | (Constant) | 4.88 | 1.32 | 0.00 | 0.58 | |
| Age | −0.01 | 0.01 | −0.05 | 0.32 | ||
| Physical limitations | −0.70 | 0.05 | −0.75* | 0.00 | ||
| 20.B (Mastery) | (Constant) | 2.51 | 1.43 | 0.08 | 0.18 | |
| Age | 0.00 | 0.02 | 0.01 | 0.94 | ||
| Physical limitations | −0.31 | 0.06 | −0.43* | 0.00 | ||
| 20.C (ADL ability) | (Constant) | 3.96 | 1.31 | 0.00 | 0.54 | |
| Age | −0.01 | 0.01 | −0.05 | 0.43 | ||
| Physical limitations | −0.56 | 0.06 | −0.63* | 0.00 | ||
| Mastery | 0.22 | 0.08 | 0.18* | 0.01 | ||
| 21.A (ADL ability) | (Constant) | 4.88 | 1.32 | 0.00 | 0.58 | |
| Age | −0.01 | 0.01 | −0.05 | 0.32 | ||
| Physical limitations | −0.70 | 0.05 | −0.75* | 0.00 | ||
| 21.B (Loneliness) | (Constant) | −1.63 | 1.21 | 0.18 | 0.09 | |
| Age | 0.04 | 0.01 | 0.21* | 0.01 | ||
| Physical limitations | 0.11 | 0.05 | 0.18* | 0.03 | ||
| 21.C (ADL ability) | (Constant) | 4.03 | 1.32 | 0.00 | 0.57 | |
| Age | 0.00 | 0.02 | 0.00 | 0.95 | ||
| Physical limitations | −0.64 | 0.05 | −0.69* | 0.00 | ||
| Loneliness | −0.27 | 0.09 | −0.18* | 0.00 | ||
| 22.A (Immobility) | (Constant) | −2.50 | 2.27 | 0.27 | 0.64 | |
| Age | 0.02 | 0.03 | 0.05 | 0.36 | ||
| Gender | 0.35 | 0.18 | 0.10* | 0.05 | ||
| Physical limitations | 1.31 | 0.09 | 0.77* | 0.00 | ||
| 22.B (Depression) | (Constant) | 10.69 | 19.14 | 0.58 | 0.08 | |
| Age | −0.09 | 0.21 | −0.03 | 0.69 | ||
| Gender | 1.28 | 1.46 | 0.07 | 0.38 | ||
| Physical limitations | 2.42 | 0.78 | 0.26* | 0.00 | ||
| 22.C (Immobility) | (Constant) | −0.18 | 2.21 | 0.94 | 0.65 | |
| Age | −0.00 | 0.02 | −0.01 | 0.89 | ||
| Gender | 0.29 | 0.17 | 0.09 | 0.09 | ||
| Physical limitations | 1.28 | 0.09 | 0.75* | 0.00 | ||
| Depression | 0.02 | 0.01 | 0.13* | 0.02 | ||
| 23.A (Immobility) | (Constant) | −2.50 | 2.27 | 0.27 | 0.64 | |
| Age | 0.02 | 0.03 | 0.05 | 0.36 | ||
| Gender | 0.35 | 0.18 | 0.10* | 0.05 | ||
| Physical limitations | 1.31 | 0.09 | 0.77* | 0.00 | ||
| 23.B (Mastery) | (Constant) | 2.62 | 1.45 | 0.07 | 0.18 | |
| Age | 0.00 | 0.02 | 0.00 | 0.95 | ||
| Gender | −0.05 | 0.11 | −0.03 | 0.68 | ||
| Physical limitations | −0.31 | 0.06 | −0.43* | 0.00 | ||
| 23.C (Immobility) | (Constant) | 0.88 | 2.26 | 0.70 | 0.65 | |
| Age | −0.00 | 0.02 | −0.01 | 0.88 | ||
| Gender | 0.30 | 0.17 | 0.09 | 0.08 | ||
| Physical limitations | 1.23 | 0.10 | 0.72* | 0.00 | ||
| Mastery | −0.35 | 0.14 | −0.15* | 0.01 | ||
| 24. A (Immobility) | (Constant) | −2.50 | 2.27 | 0.27 | 0.64 | |
| Age | 0.02 | 0.03 | 0.05 | 0.36 | ||
| Gender | 0.35 | 0.18 | 0.10* | 0.05 | ||
| Physical limitations | 1.31 | 0.09 | 0.77* | 0.00 | ||
| 24.B (Loneliness) | (Constant) | −1.93 | 1.23 | 0.12 | 0.10 | |
| Age | 0.04 | 0.01 | 0.22* | 0.01 | ||
| Gender | 0.13 | 0.10 | 0.11 | 0.19 | ||
| Physical limitations | 0.10 | 0.05 | 0.17* | 0.05 | ||
| 24.C (Immobility) | (Constant) | −1.60 | 2.34 | 0.50 | 0.63 | |
| Age | 0.01 | 0.03 | 0.03 | 0.63 | ||
| Gender | 0.29 | 0.18 | 0.09 | 0.11 | ||
| Physical limitations | 1.33 | 0.10 | 0.77* | 0.00 | ||
| Loneliness | 0.08 | 0.16 | 0.03 | 0.63 | ||
| 25.A (ADL ability) | (Constant) | 4.35 | 1.82 | 0.02 | 0.20 | |
| Age | −0.03 | 0.02 | −0.12 | 0.14 | ||
| Delayed recall | 0.14 | 0.03 | 0.42* | 0.00 | ||
| 25.B (Loneliness) | (Constant) | −1.28 | 1.24 | 0.30 | 0.09 | |
| Age | 0.04 | 0.01 | 0.22* | 0.01 | ||
| Delayed recall | −0.03 | 0.02 | −0.17* | 0.05 | ||
| 25.C (ADL ability) | (Constant) | 3.26 | 1.83 | 0.08 | 0.20 | |
| Age | −0.01 | 0.02 | −0.05 | 0.58 | ||
| Delayed recall | 0.12 | 0.03 | 0.37* | 0.00 | ||
| Loneliness | −0.26 | 0.13 | −0.16* | 0.05 |
Note: B is the unstandardized regression coefficient, Std. error is the standard error for this coefficient, and Beta is the standardized regression coefficient; * P value was <0.05; −0.00 represents a negative value that appears in the table as negative zero because only 2 decimal places were used. Models denoted by letter A indicate that this model tests the direct effect between the independent variable and the outcome variable; models denoted by letter B indicate that this model tests the direct effect between the independent variable and the mediator variable; models denoted by letter C indicate that this model tests the mediating effect between the independent variable and the outcome variable. On several occasions, the R 2 values of model version C are less than those of version A, which is due the listwise deletion of cases missing data on the psychosocial mediator variables
Psychosocial mediators between impairments and limitations
Results from models 10–18 (Table 4) indicated that there were several significant psychosocial variables that mediated relationships between impairments and functional limitations. Model 10 demonstrated that depression met the criteria for partial mediation between vision and physical limitations, however, follow-up tests (Table 6) revealed Sobel’s test to be only marginally significant, with depression explaining 17.2% of the direct effect between vision and physical limitations. Model 11, however, indicated that the relationship between vision and physical limitations was significantly and partially mediated by mastery, with mastery explaining 28.6% of the direct effect between vision and physical limitations. Models 12, 13, and 14, did not find evidence that loneliness mediated the relationship between vision and physical limitations, that loneliness mediated the relationship between hearing and physical limitations, or that depression mediated the relationship between lung function and physical limitations. In each of these cases, the independent variable did not significantly predict the mediator variable (step B in the models). Model 15 indicated that mastery significantly mediated the relationship between lung function and physical limitations, explaining 27.0% of the direct effect. This model also suggests full mediation because in model 15.C, lung function became non-significant when the mediator, mastery, was added. Model 16 did not find that the relationship between lung function and physical limitations was mediated by loneliness because lung function did not significantly predict the mediator, loneliness, after controlling for age, gender, and being married (model 16.B). Model 17 did not find that the relationship between pulse and physical limitations was mediated by loneliness because pulse did not significantly predict physical limitations after controlling for age and gender (model 17.A). Finally, model 18 suggested that mastery partially, but significantly mediated the relationship between grip strength and physical limitations, explaining 18.6% of the direct effect.
Psychosocial mediators between limitations and disability
Models 19 and 20 (Table 5) indicated that the relationship between physical limitations and ADL ability was significantly and partially mediated by depression (explaining 10.2% of the direct effect), and mastery (explaining 19.6% of the direct effect). Although in model 21 the criteria was met for loneliness also mediating the relationhsip between physical limitations and ADL ability, Sobel’s test (Table 6) was only marginally significant, and loneliness explained only 6.8% of that direct effect. Models 22 and 23 also indicated that the relationship between physical limitations and immobility was significantly and partially mediated by depression (explaining 10.1% of this direct effect), and mastery (explaining 20.1% of the direct effect). Model 24 found that loneliness did not mediate the relationship between physical limitations and immobility because loneliness did not significantly predict immobility when physical limitations was also included as a predictor (model 24.C). Finally, model 25 indicated that the criteria was met for loneliness mediating the relationship between delayed recall and ADL ability, but Sobel’s test was not statistically significant. Loneliness did, however, explain 10.6% of the direct effect between delayed recall and ADL ability.
Discussion
In general, the results from mediation tests in the current study lend support for the hypothesized organization of constructs within the Disablement Process model. When observing the main pathway, for example, results showed that all impairments were predictive of at least one disability variable. When adding tests of mediation, however, it appears that much of these effects, specifically for vision, lung function, and grip strength, work indirectly via physical limitations, a finding which supports the placement of physical limitation variables in between impairments and disability in the model. In fact, physical limitations in basic body movements accounted for between 31 and 52% of the direct effects between the impairment variables of vision, lung function, and grip strength, and the disability variables ADL ability and immobility. The fact that physical limitation was a more important mediator in the model than cognitive ability (measured via delayed recall) is not surprising, as we would not expect problems in vision, pulmonary function, or muscular function to necessarily influence cognitive tasks like memory function.
Despite these findings that support the organization of the model’s main pathway, the predicted and predictive power of the pathology factor was not supported. In these analyses, a measure of “disease severity” was included as a proxy for pathology, yet disease severity had small, but significant associations with only three other variables in the model (physical limitations, immobility, and mastery), none of which were impairment variables. It is possible that these mostly null findings are caused by defining pathology in terms of how life-threatening a disease is. Diseases that are highly life threatening do not necessarily cause disablement, and diseases that are highly disabling may not necessarily be life threatening. Arthritis, for example, is listed by Gold’s (Gold et al. 2002) measure as “somewhat life threatening”, and heart disease is listed as “very life threatening”, but it is possible that a person with arthritis is more disabled by their disease than a person is with heart disease. Thus, it is possible that a scale like Gold’s or the widely used Charlson co-morbidity index (Charlson et al. 1987) measure how threatening a disease is to mortality, instead of how threatening it is to disability. Future studies should consider testing a pathology scale which assesses disability-risk, rather than mortality-risk.
In addition to these analyses supporting the general organization of the main pathway, evidence also emerged which substantiated the inclusion of psychosocial variables in the periphery of the model. Mastery, in particular, was found to be a consistent mediator between impairments and functional limitations accounting for between 18 and 29% of the direct effects, and between functional limitations and disability, accounting for approximately 20% of the direct effects. Depression mediated the relationship between vision and physical limitations, and between physical limitations and both disability variables, but explained a lower percentage of the direct effects (between 10 and 18%). Finally, loneliness met some but not all of the criteria to be considered a significant mediator between both physical and cognitive functional limitation variables and ADL ability, however, it only explained between 6 and 11% of the direct effects. These findings on psychosocial mediators support work by Femia et al. (1997), who found psychosocial variables in general, and mastery in particular, to play important mediating roles in the Disablement Process. A study by Caplan and Schooler (2003) also found that attributes related to mastery, namely self-confidence and fatalism, were related to disability outcomes.
Although the current analysis does not reveal why or how mastery acts a mediator, there is research which may explain such mechanisms. Mastery is a concept originally developed by Pearlin and Schooler (1978) as a kind of coping mechanism which protected people from stressors. In the face of disability, it is possible that feelings of mastery lead people to remain more physically active, whereas those with low mastery may become more physically passive once they realize their limitations. By causing increased activity, mastery may contribute to the maintenance of stronger muscle mass and overall physical health. Mastery also may cause individuals to feel more in control of their physical impairments, which leads them to be more proactive in their own care, and better at mobilizing resources which allow them to maintain function at the highest possible level. In addition, mastery may affect people’s performance on and self-report of their own physical abilities. People with higher mastery may have more confidence in their own ability, and therefore may try harder on the tests of physical limitations. They also may have more confidence in their ADL abilities and may foresee themselves as needing less help with these activities, even when some impairment does exist. Regardless of the underlying mechanisms, the fact that mastery has a significant influence on the process of disablement leads to important implications for sustaining independence in the oldest-old. Perhaps if older people can be made to feel more in control of their health and healthcare, they may be better able to cope with their losses in ability, and they may be able to improve their own functional performance and ability outcomes. On a final note, however, besides testing how psychosocial attributes such as mastery influence outcomes such as disability, we also should consider that disability may influence psychosocial attributes, and therefore, future studies should consider intra-individual variables both as predictors of disability, and as possible outcomes affected by disability.
Limitations and future directions
Several important limitations to the current study should be noted. These analyses were run on a sample of very old individuals, and the sample included people who were living independently and in institutions. Despite the effort to include individuals who were dependent on institutional care, the final sample must be viewed as one that potentially contains only the healthiest oldest-old. Those who were too physically or cognitively impaired to participate in the lengthy interview process were not included in the analyses. While this problem arises in nearly all studies of this age group, it is still important to consider that the current findings may not be generalizable to the entire oldest-old population.
A second caveat worth noting is that the model was tested using cross-sectional analyses. The fact that disablement is a process inherently implies that time must pass for disability to occur. People who develop an illness or disorder do not necessarily become concurrently disabled. While it is important to test the model cross-sectionally as a “first step”, it is also possible that different predictors and different mediators could emerge if time was introduced into the model. We suggest that future tests of the model utilize the longitudinal nature of NONA and other appropriate datasets, and that researchers compare results from the longitudinal and cross-sectional analyses to better understand how time effects relationships in the model.
A third point of importance is that the analyses tested a large number of associations, and thus included many tests of significance. With large numbers of significance tests, it is possible that some “statistically significant” effects discussed here have been found just by chance. Although theory, past research, and the Disablement Process model have guided variable selection and testing, results here should be interpreted as lending support for the Disablement Process model, not necessarily “confirming” it.
Finally, this study was not able to test the role of external factors in the Disablement Process, thus, like Femia et al. (2001), Lawrence and Jette (1996), and Peek et al. (2003), the current analyses represent only a partial test of the Disablement Process model. Future research should include reliable measures of extra-individual factors in order to test the full model. While the current study leant support that psychosocial variables such as mastery, depression, and loneliness may be explain some of the variance in relationships within the main pathway, there remains a lot of variance which still can be explained. It is likely that including other intra-individual factors, and perhaps more importantly, extra-individual factors, might reveal additional variables that are equally, if not more, important than mastery, depression, and loneliness in the Disablement Process. For example, type and quality of medical care, accessibility and use of personal care equipment, and the extent to which people’s physical environment accommodates their limitations or hinders them, would be particularly interesting to test as additional mediators. Research that includes extra-individual factors may be informative in explaining additional variance in basic research on disablement, and also be helpful in designing interventions aimed at preventing disability.
Conclusions
In conclusion, the current analyses provide further support for the theoretical and empirical relevance of the Disablement Process model. The inclusion of psychosocial factors, and mastery, in particular, revealed both the potential strengths of the relationships between psychological attributes and disablement, and it also provided information on areas of psychological functioning that might be amenable to interventions seeking to impede the Disablement Process. The current analysis also provides new evidence that this model is replicable in a sample of the oldest-old—a sample which has an elevated risk for developing disability.
Acknowledgments
This research was funded in part by grants from the Swedish Council for Working Life and Social Research, by the National Institute of Mental Health, Interdisciplinary Training in Gerontology, 5 T32 MH18904-17, and by the National Institute on Aging, Interdisciplinary Training in Gerontology, 5 T32 AG00048-27.
References
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bauco C. Functional status and well-being of centenarians. Arch Gerontol Geriat. 1996;Suppl 5:363–366. doi: 10.1016/0167-4943(96)86962-7. [DOI] [PubMed] [Google Scholar]
- Beckett LA, Brock DB, Lemke JH, Mendes de Leon CF, Guralnik JM, Fillenbaum GG, Branch LG, Wetle TT, Evans DA. Analysis of change in self-reported physical function among older persons in four population studies. Am J Epidemiol. 1996;143:766–778. doi: 10.1093/oxfordjournals.aje.a008814. [DOI] [PubMed] [Google Scholar]
- Camacho TC, Strawbridge WJ, Cohen RD, Kaplan GA. Functional ability in the oldest-old: cumulative impact of risk factors from the preceding two decades. J Aging Health. 1993;5:439–454. doi: 10.1177/089826439300500402. [DOI] [Google Scholar]
- Caplan LJ, Schooler C. The roles of fatalism, self-confidence, and intellectual resources in the disablement process in older adults. Psychol Aging. 2003;18(3):551–561. doi: 10.1037/0882-7974.18.3.551. [DOI] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Cook NR, Evans DA, Scherr PA, Speizer FE, Vedal S, Branch LG, Huntley JC, Hennekens CH, Taylor JO. Peak expiratory flow rate in an elderly population. Am J Epidemiol. 1989;130:66–78. doi: 10.1093/oxfordjournals.aje.a115324. [DOI] [PubMed] [Google Scholar]
- Clarke P, George LK. The role of the built environment in the disablement process. Am J Public Health. 2005;95(11):11–17. doi: 10.2105/AJPH.2004.054494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Femia EE, Zarit SH, Johansson B. Predicting change in activities of daily living: a longitudinal study of the oldest-old in Sweden. J Gerontol Ser B Psychol Sci Soc Sci. 1997;52(6):1079–5014. doi: 10.1093/geronb/52b.6.p294. [DOI] [PubMed] [Google Scholar]
- Femia EE, Zarit SH, Johansson B. The disablement process in very late life: a study of the oldest-old in Sweden. J Gerontol Ser B Psychol Sci Soc Sci. 2001;56:12–23. doi: 10.1093/geronb/56.1.p12. [DOI] [PubMed] [Google Scholar]
- Gold C, Malmberg B, McClearn GE, Pederson NL, Berg S. Gender and health: a study of older unlike-sex twins. J Gerontol Soc Sci. 2002;57B(3):S168–S176. doi: 10.1093/geronb/57.3.s168. [DOI] [PubMed] [Google Scholar]
- House JS, Landis KR, Umberson D. Social direct effects and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Johansson B (1988/1989) The MIR-memory in reality test. Psykologiforlaget AB, Stockholm
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness and the aged. The index of ADL: a standardized measure of biological and psychosocial function. J Am Med Assoc. 1963;185:914–923. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Kempen GIJM, van Heuvelen MJG, van Sonderen E, van den Brink RHS, Kooijman AC, Ormel J. The direct effect of functional limitations to disability and the moderating effects of psychological attributes in community dwelling older persons. Soc Sci Med. 1999;48:1161–1172. doi: 10.1016/S0277-9536(98)00427-4. [DOI] [PubMed] [Google Scholar]
- Kobasa SCO, Maddi SR, Puccetti MC, Zola MA. Effectiveness of hardiness, exercise and social support as resources against illness. In: Steptoe A, Wardle J, editors. Psychosocial processes and health: a reader. New York: Cambridge University Press; 1994. pp. 247–260. [Google Scholar]
- Kunkel SR, Appelbaum RA. Estimating the prevalence of long-term disability for an aging society. J Gerontol Soc Sci. 1992;47:S253–S260. doi: 10.1093/geronj/47.5.s253. [DOI] [PubMed] [Google Scholar]
- Lauretani F, Russo CR, Bandinelli S, Bartali B, Cavazzini C, Di Iorio A, Corsi AM, Rantanen T, Guralnik JM, Ferrucci L. Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J Appl Physiol. 2003;95:1851–1860. doi: 10.1152/japplphysiol.00246.2003. [DOI] [PubMed] [Google Scholar]
- Lawrence RH, Jette AM. Disentangling the disablement process. J Gerontol Soc Sci. 1996;51B:S173–S182. doi: 10.1093/geronb/51b.4.s173. [DOI] [PubMed] [Google Scholar]
- Lawton MP. The functional assessment of older people. J Am Geriatr Soc. 1971;19:465–481. doi: 10.1111/j.1532-5415.1971.tb01206.x. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev. 1993;17:144–158. doi: 10.1177/0193841X9301700202. [DOI] [Google Scholar]
- Malmberg B (1990) Access to resources in different age-cohorts. Implications for activity level, loneliness and life satisfaction. Unpublished dissertation. Linköping University, Linköping, Sweden
- Mendes de Leon C, Glass T, Beckett L, Seeman T, Evans D, Berkman L. Social networks and disability transitions across eight intervals of yearly data in the New Haven EPESE. J Gerontol. 1999;54:S162–S172. doi: 10.1093/geronb/54b.3.s162. [DOI] [PubMed] [Google Scholar]
- Pearlin L, Schooler C. The structure of coping. J Health Soc Behav. 1978;19:2–21. doi: 10.2307/2136319. [DOI] [PubMed] [Google Scholar]
- Peek MK, Ottenbacher KJ, Markides KS, Ostir GV. Examining the disablement process among older Mexican American adults. Soc Sci Med. 2003;57(3):413–425. doi: 10.1016/S0277-9536(02)00367-2. [DOI] [PubMed] [Google Scholar]
- Palatini P. Heart rate as an independent risk factor for cardiovascular disease: current evidence and basic mechanisms. Drugs. 2007;67 (Suppl 2):3–13. doi: 10.2165/00003495-200767002-00002. [DOI] [PubMed] [Google Scholar]
- Potter VA. Pulse oximetry in general practice: how would a pulse oximeter influence patient management? Euro J Gen Prac. 2007;13(4):216–220. doi: 10.1080/13814780701574762. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Rogers RG, Rogers A, Belanger A. Disability-free life among the elderly in the United States. J Aging Health. 1992;4:19–42. doi: 10.1177/089826439200400102. [DOI] [Google Scholar]
- Russell D. The measurement of loneliness. In: Peplau LA, Perlman D, editors. Loneliness: a sourcebook of current theory, research and therapy. New York: Wiley; 1982. [Google Scholar]
- Smits CHM, Deeg DJH, Jonker C. Cognitive and emotional predictors of disablement in older adults. J Aging Health. 1997;9:204–221. doi: 10.1177/089826439700900204. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological methodology. San Francisco: Jossey-Bass; 1982. pp. 290–312. [Google Scholar]
- Stuck A, Walthert J, Nikolaus T, Büla C, Hohmann C, Beck J. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999;48:445–469. doi: 10.1016/S0277-9536(98)00370-0. [DOI] [PubMed] [Google Scholar]
- Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Wilcox V, Kasl S, Berkman L. Social support and physical disability in older people after hospitalization: a prospective study. Health Psychol. 1994;13:170–179. doi: 10.1037/0278-6133.13.2.170. [DOI] [PubMed] [Google Scholar]