Abstract
Pulmonary cryptococcosis is commonly found in immunocompromised patients. This microorganism rarely infects immunocompetent individuals, and when it does, it causes mild symptoms. The radiological findings of this disease may involve an intrapulmonary mass that mimics lung tumor. The objective of this study was to review the clinicopathological information, radiological findings, and treatment of patients who presented with intrapulmonary mass due to cryptococcosis. This study collected data from 7 patients who were treated at Songklanagarind Hospital, Songkhla, Thailand, between 2009 and 2014. Their clinical data, radiological findings, pathological results, and treatment protocols were reviewed. The patients were 2 women and 5 men, ranging in age from 37 to 79 years old. One case was an immunocompromised host. Four cases experienced the chest symptoms of dyspnea, hemoptysis, and chronic cough. The most common location of mass was the left lower lobe (71%). Four cases had a history of bird contact. Lung lobectomy was performed in 3 cases (42%), and all of the patients were treated with oral fluconazole. An intrapulmonary mass caused by this microorganism is mainly found in immunocompetent patients. Treatment with the antifungal drug fluconazole is very effective.
Keywords: Pulmonary cryptococcosis, lung mass, pathology, radiology, treatment
Introduction
Pulmonary cryptococcosis is a rare lung infection caused by Cryptococcus neoformans. This microorganism usually causes severe pneumonia in an immunocompromised patient, especially in patients with human immunodeficiency virus (HIV) infection, and can lead to death.1–3 However, immunocompetent hosts are rarely infected by this organism and usually experience silent symptoms. The signs and symptoms of this disease in immunocompetent patients are quite nonspecific. As a result, many cases are misdiagnosed as other diseases such as lung cancer. The diagnosis of this infection employs chest X-rays and computed tomographic (CT) scans to detect the lung lesion in combination with tissue biopsy and tissue culture to identify the specific type of microorganism. The chest X-ray findings in immunocompromised patients usually indicate diffuse lung infiltration. But in a normal host, the findings can be a lung mass that sometimes mimics lung cancer. So, the correct diagnosis of a lung mass is necessary for an appropriate treatment.
This study reports 7 cases of pulmonary cryptococcosis with radiological findings of lung mass. The objective of this study was to review the clinical data, radiological findings, lung histology results, and treatment of pulmonary cryptococcosis in patients who presented with lung mass.
Materials and Methods
Study patients
This study protocol was approved by the Ethics Committee of our institution. The subjects of this study were 7 patients who were treated at Songklanagarind Hospital, Hat Yai, Songkhla, Thailand, between 2009 and 2014.
Data collection
This study collected clinical data that consisted of age, sex, underlying disease, symptoms, and history of bird contact. Radiological data from chest X-rays and CT scans along with pathologic and treatment data were also collected. The patients with incomplete data were excluded from this study.
Results
Sex and age
The patients in this study were 5 men and 2 women. Their ages ranged from 39 to 79 years, and the mean age was 54.7 years.
Immune status and underlying disease
In all, 6 patients were immunocompetent hosts, and 1 of them had underlying diabetes mellitus. Only 1 patient was an immunocompromised host due to having underlying systemic lupus erythematosus. A history of bird contact was reported in 4 patients.
Symptoms and signs
Three cases did not have any chest-related symptoms, and their lung lesions were detected at an annual checkup via a chest X-ray. Two cases had mild chest symptoms—chronic cough and weight loss. The remaining 2 cases had severe chest symptoms—hemoptysis and dyspnea. In the cases that had chest symptoms, the time from symptom to diagnosis was 1 to 4 months. No cases had any neurological involvement.
Laboratory investigation
Blood serological tests for cryptococcal antigen were done in 3 cases, and the results showed positive in 1 case. A sputum culture was done in only 1 case, and the results showed positive for C neoformans. A tissue culture for fungal organisms was not done in any of the cases.
Radiological findings
The chest X-rays of all cases revealed lung masses that ranged from 1.2 to 12 cm in diameter. The most frequent location of the mass was the lower left lobe of the lung (71%). One case had a lesion in the upper left lobe, and one case in the lower right lobe.
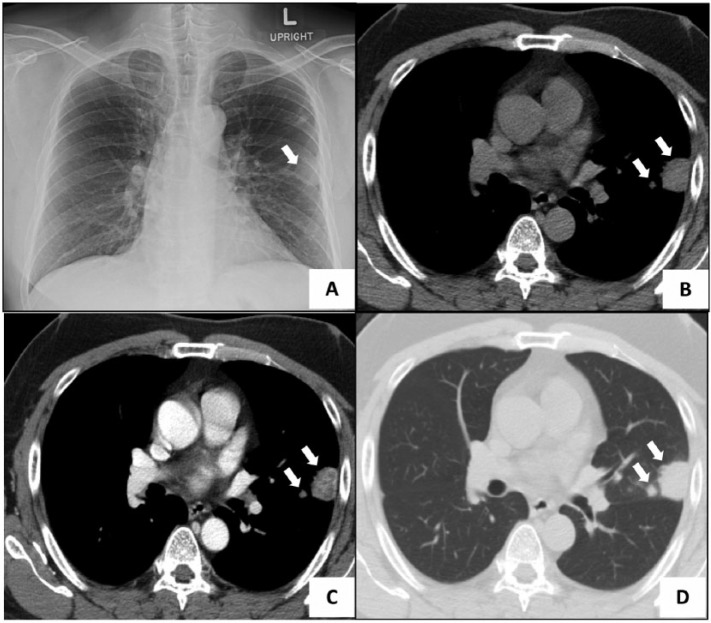
Figure 1 illustrates an example. Figure 1A shows a 3-cm mass with a well-defined border in the upper left lobe. Figure 1B and C shows enhanced and nonenhanced CT images of the mediastinal window of the middle lung that shows 2 nodules. The larger nodule was an irregularly bordered, homogeneous, 2.4-cm mass attached to the left lateral chest wall without the presence of destruction. The smaller 0.7-cm nodule lied medially. Figure 1D shows the lung window of the middle-lung CT image that revealed 2 nodules with irregular and well-defined borders in the lingular segment of the upper left lobe.
Figure 1.
(A) Chest X-ray revealing a nodule in the middle part of the upper left lung. (B) Mediastinal window nonenhanced CT image showing 2 masses attached to the chest wall (arrow). (C) Mediastinal window enhanced CT image showing heterogeneous enhancement in the nodules (arrow). (D) CT scan of lung window showing 2 masses at the lingular segment of upper left lobe (arrow). CT indicates computed tomography.
Histologic findings
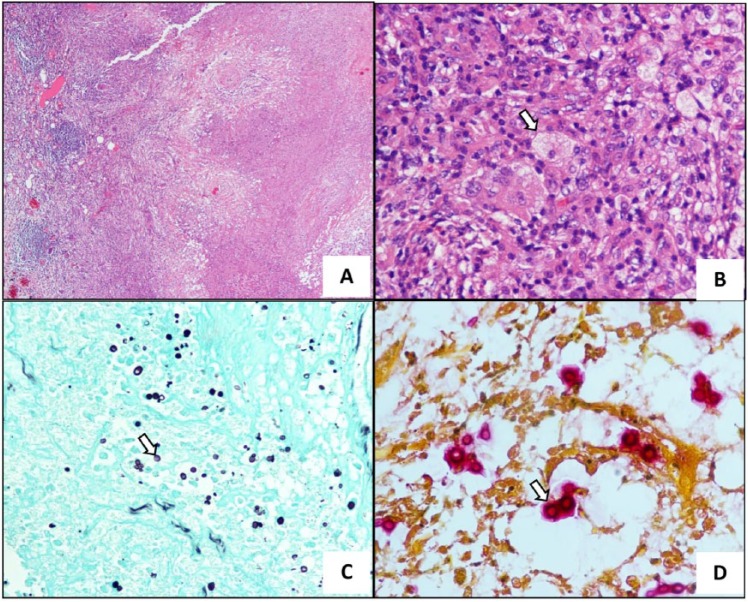
All cases had a tissue diagnosis via a transthoracic needle biopsy. Three cases underwent lung lobectomy. All of the specimens showed many intracellular microorganisms with a clear capsule on the hematoxylin and eosin slide. The Grocott methenamine silver (GMS) staining was performed in all cases, and the results showed positive staining in the cell walls of this microorganism. Mucin staining also showed positive staining in the capsule of this fungus (Figure 2).
Figure 2.
(A) Histologic slide showing chronic granulomatous inflammation with tissue necrosis (hematoxylin-eosin, original magnification ×40). (B) There were numerous intracellular round-shaped microorganisms in macrophages (arrow) (hematoxylin-eosin, original magnification ×100). (C) Grocott methenamine silver staining demonstrating many yeast-form fungal organisms in the lesion (arrow) (original magnification x100). (D) Mucin staining depicting red-pink color in the capsule of this fungal organism (arrow) (original magnification x400).
Management and follow-up
Three cases underwent lung lobectomy due to a large lung lesion and received oral antifungal medication (fluconazole: 200-400 mg/d) for 6 months. Four cases were treated with only oral antifungals (fluconazole: 400 mg/d) for 6 months. All of the cases experienced clinical improvement at the 6-month follow-up. The clinical data along with the X-ray findings and the treatment protocols are summarized in Table 1.
Table 1.
Clinical data, X-ray findings, and treatment protocols.
| Case | Sex | Age | Underlying disease | Chief complaint | Size of mass by X-ray, cm | Location | History of bird contact | Surgery | Medication |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | 54 | DM | Abnormal CXR | 3 | Upper left lobe | + | Lobectomy | Fluconazole (200) 1 × 2 (6 m) |
| 2 | Male | 79 | — | Progressive dyspnea | 3.4 | Lower left lobe | + | — | Fluconazole (200) 1 × 2 (6 m) |
| 3 | Female | 37 | — | Nonmassive hemoptysis | 12 | Lower left lobe | − | Lobectomy | Fluconazole (200) 2 × 1 (6 m) |
| 4 | Male | 61 | — | Abnormal CXR | 1.7 | Lower left lobe | − | Lobectomy | Fluconazole (200) 1 × 1 (6 m) |
| 5 | Female | 58 | — | Chronic cough with weight loss | 8 | Lower right lobe | + | — | Fluconazole (600) 1 × 2 (15 d) Fluconazole (200) 2 × 1 (6 m) |
| 6 | Male | 55 | SLE | Chronic cough | 3 | Lower left lobe | − | — | Fluconazole (200) 2 × 1 (6 m) |
| 7 | Male | 39 | — | Abnormal CXR | 2 | Lower left lobe | + | — | Fluconazole (200) 1 × 2 (6 m) |
Abbreviations: CXR, chest X-ray; DM, diabetes mellitus; SLE, systemic lupus erythematosus.
Literature review
Pathogen
The fungal organisms in the genus Cryptococcus are currently classified into 2 major pathogens. The first type is C neoformans species complex, including Cryptococcus neoformans var. grubii and Cryptococcus neoformans var. neoformans. The second type is Cryptococcus gattii.4 A definite diagnosis of the specific species uses tissue culture as the gold standard.
Signs and symptoms
Immunocompetent patients usually have mild chest symptoms such as low-grade fever and minimal cough. In this group of patients, the infection is usually detected by checkup chest X-rays.5,6 In contrast, immunocompromised patients experience more severe chest symptoms such as high-grade fever, severe chronic cough, dyspnea, and hemoptysis.6
Radiological findings
The radiological finding in immunocompetent patients is usually an intrapulmonary mass up to 3 cm in size. Occasionally, it presents with lung consolidation or a reticulonodular pattern.7 Other common findings are diffuse interstitial infiltration and multiple small pulmonary nodules.8 The most common location of infection in more than 50% of the cases is the lower lung lobes.9,10
Histologic findings
Cryptococcus neoformans is a fungus of about 5 to 10 µm in size. It is a budding yeast surrounded by a clear capsule. The capsular substance is a mucopolysaccharide that can be stained by mucin staining.1–3 The cell wall of this microorganism is stained by GMS staining which is used in the routine diagnosis of this infection. However, the gold standard for its diagnosis is a tissue culture. The histologic findings in a hematoxylin and eosin slide are granulomatous inflammation with many intracellular yeast-form microorganisms in macrophages.11
Treatment
The treatment protocol is based on the severity of the disease and the status of the patient. For nonsevere patients, fluconazole (400 mg/d) is the recommended oral antibiotic. Fluconazole is an antifungal agent that inhibits fungal cytochrome P450–dependent enzyme 14α-demethylase. This function inhibits the conversion of lanosterol to ergosterol which is an essential component of the fungal cell membrane and causes accumulation of lanosterol in the cell.12
In severe cases or in immunocompromised patients, the protocol of treatment has 3 phases. First is the induction phase which involves the use of intravenous drugs—amphotericin B (0.7-1 mg/kg) plus flucytosine (100 mg/kg)—for 2 weeks. The next one is the consolidation phase during which high-dose oral fluconazole (400 mg/d) for 8 weeks is employed. The last phase is the maintenance phase where the use of oral fluconazole (200 mg/d) for 6 to 12 months is continued.13,14
Discussion
Recently, the incidence of pulmonary cryptococcosis has been on the rise due to the high rates of HIV infection. The patients with HIV infection have a low immune function which makes them prone to infections by microorganisms such as bacteria and fungi. In a healthy person who inhales the spore of a fungus, the immune system will eliminate it through the histiocytes in the lung. However, some patients with an impaired function of pulmonary histiocytes, which can be caused by many factors (smoking, elderly, and chronic lung disease), have an increased risk of pulmonary infection, including fungal infections.2,3
Pulmonary cryptococcosis is an uncommon infection found worldwide. The incidence of pulmonary fungal infection caused by C neoformans is about 20%, secondary to an Aspergillus spp infection.10 This fungus is found in the soil and bird droppings.4,5 In southern Thailand, the incidence of a cryptococcal infection is quite high due to its favorable climate for fungal growth and many bird farms. The common species of birds associated with this fungus are Streptopelia chinensis and Pycnonotus jocosus. In this study, 4 out of the 7 cases reported a history of bird contact. So, living near a bird farm may increase the risk of a cryptococcal infection.
In immunocompetent patients, the clinical presentation is quite mild. The patient may have minimal respiratory symptoms with low-grade fever. In our study, about 40% of the cases did not have any specific symptom, but their disease was detected by means of a routine chest X-ray. Mild symptoms were experienced by 30% of the patients. Our findings were similar to those of a previous study which reported that symptoms are usually mild in immunocompetent patients.9
The radiological findings regarding pulmonary cryptococcosis among immunocompetent hosts are not specific. In most cases, an intrapulmonary mass without a specific cause is detected. A previous study reported the presence of nonspecific findings such as small-to-large mass, lung consolidation, and lung cavity in the chest X-rays.6 However, the radiological findings in immunocompromised hosts are quite different because these patients usually experience a more severe infection and disseminated disease. Therefore, the radiological findings in this group usually involve diffuse lung consolidation.7 Common locations of this infection are the lower lung lobes.8 This study also detected a lower-lobe infection in 85% of all the cases.
The laboratory diagnosis of pulmonary cryptococcosis is based on a lung biopsy and tissue culture. The histologic findings in a hematoxylin and eosin slide are quite specific to this disease, but it cannot identify the species because both C neoformans species complex and C gattii exhibit a similar morphology. However, pulmonary infection is rarely caused by C gattii, and only a few cases were reported.6
Before 1996, the traditional treatment for cryptococcal infection, including central nervous system and lung infection, was intravenous injections of amphotericin B with or without flucytosine. However, this regimen is associated with severe adverse drug reactions and a limited time for the use of intravenous injections. The current regimen of treatment involves oral fluconazole, which has the same efficiency but fewer side effects.11,12 Moreover, lung resection is recommended in severe cases associated with severe lung injury and massive hemorrhage.
In conclusion, pulmonary cryptococcosis is usually found in immunocompromised patients in tropical countries. The clinical and radiological findings make its diagnosis difficult. This infection can present with a lung mass that mimics lung cancer. Both tissue biopsy and culture are necessary for a definite diagnosis. The major option of treatment involves the use of oral antifungal drugs. The result of pulmonary cryptococcosis treatment in immunocompetent patients is excellent.
Footnotes
Peer review:Three peer reviewers contributed to the peer review report. Reviewers’ reports totaled 456 words, excluding any confidential comments to the academic editor.
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The funding of this research is supported by Faculty of Medicine, Prince of Songkla University.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: Study conception and design: KK and ZK. Acquisition of data: WT, WK and SP. Analysis and interpretation of data: KK and ZK. Drafting and revision of manuscript: KK.
References
- 1. Binford CH, Dooley JR. Disease caused by fungi and actinomycetes. In: Binford CH, Connor DH, eds. Pathology of Tropical and Extraordinary Diseases. Washington, DC: Armed Forces Institute of Pathology; 1976: 572–573. [Google Scholar]
- 2. McAdam AJ, Sharpe AH. General pathology of infectious disease. In: Kumar V, Abbas AK, Aster JC, eds. Robbins Basic Pathology. 9th ed. Philadelphia, PA: Elsevier Saunders; 2015: 313. [Google Scholar]
- 3. Husain AN. Lung pathology. In: Kumar V, Abbas AK, Aster JC, eds. Robbins Basic Pathology. 9th ed. Philadelphia, PA: Elsevier Saunders; 2015: 503–504. [Google Scholar]
- 4. Springer DJ, Chaturvedi V. Projecting global occurrence of Cryptococcus gattii. Emerg Infect Dis. 2010;16:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nunez M, Peacock JE, Chin R. Pulmonary cryptococcosis in the immunocompetent host. Therapy with oral fluconazole: a report of four cases and a review of the literature. Chest. 2000;118:527–534. [DOI] [PubMed] [Google Scholar]
- 6. Lam CL, Lam WK, Wong Y, et al. Pulmonary cryptococcosis: a case report and review of Asian-Pacific experience. Respirology. 2001;6:351–355. [DOI] [PubMed] [Google Scholar]
- 7. Shirley RM, Baddley JW. Cryptococcal lung disease. Curr Opin Pulm Med. 2009;15:254–260. [DOI] [PubMed] [Google Scholar]
- 8. Wu B, Liu H, Huang J, Zhang W, Zhang T. Pulmonary cryptococcosis in non-AIDS patients. Clin Invest Med. 2009;32:E70–E77. [DOI] [PubMed] [Google Scholar]
- 9. Ye F, Xie JX, Zeng QS, Chen G, Zhong S, Zhong N. Retrospective analysis of 76 immunocompetent patients with primary pulmonary cryptococcosis. Lung. 2012;190:339–346. [DOI] [PubMed] [Google Scholar]
- 10. Yu JQ, Tang KJ, Xu KJ, Xie CM, Light RW. Pulmonary cryptococcosis in non-AIDS patients. Braz J Infect Dis. 2012;16:531–539. [DOI] [PubMed] [Google Scholar]
- 11. Li S, Chen H, Shao C, Song Y, Bai C. Pulmonary cryptococcosis with tracheal wall invasion in an immunocompetent patient: a case report and literature review. Respiration. 2014;87:324–328. [DOI] [PubMed] [Google Scholar]
- 12. Cleary JD, Stover KR, Antifungal drugs. In: Smith KM, Riche DM, Henyan NN, eds. Clinical Drug Data. 11th ed. New York: McGraw-Hill; 2010: 92–93. [Google Scholar]
- 13. Meyohas MC, Meynard JL, Bollens D, et al. Treatment of non-meningeal cryptococcosis in patients with AIDS. J Infect. 1996;33:7–10. [DOI] [PubMed] [Google Scholar]
- 14. Dromer F, Mathoulin S, Dupont B, Brugiere O, Letenneur L. Comparison of the efficacy of amphotericin B and fluconazole in the treatment of cryptococcosis in human immunodeficiency virus-negative patients: retrospective analysis of 83 cases. Clin Infect Dis. 1996;22:154–160. [DOI] [PubMed] [Google Scholar]