Abstract
Objective:
Percutaneous coronary intervention for coronary bifurcation lesion is very challenging, especially for true bifurcation lesions. Although the jailed semi-inflated balloon technique is one of the established methods for treatment of coronary bifurcation lesions, little is known regarding the configuration of the side branch orifice after stent implantation using this technique.
Methods:
We report a 73-year-old male patient with angina pectoris who was successfully treated with percutaneous coronary stent implantation for a true bifurcation lesion of the right coronary artery with an obtuse angle using the jailed semi-inflated balloon technique.
Results:
Three-dimensional optical frequency domain imaging clearly showed that there were no signs of plaque or carina shift into the side branch after stent implantation using this technique.
Conclusions:
This case report highlights that the jailed semi-inflated balloon technique is a safe and useful treatment for coronary true bifurcation lesions with an obtuse angle.
Keywords: Jailed balloon technique, true bifurcation lesion, percutaneous coronary intervention
Introduction
Percutaneous coronary intervention (PCI) for coronary bifurcation lesions remains one of the most important challenges for interventional cardiologists, even with recent drug-eluting stents. The provisional stenting technique is considered the standard method for most coronary bifurcation lesions.1–3 However, even when a protection guidewire is inserted into the side branch prior to main vessel stenting, there remains the risk of side branch occlusion after stent implantation, especially in true bifurcation lesions.4,5 To overcome difficulties associated with PCI for bifurcation lesions, the jailed balloon technique and the jailed semi-inflated balloon technique have been established.5–9 However, little is known regarding the configuration of bifurcation lesions after stent implantation using the jailed semi-inflated balloon technique, especially at the orifice of the side branch. We report a 73-year-old male patient with angina pectoris who was successfully treated with percutaneous coronary stent implantation for a true bifurcation lesion of the right coronary artery (RCA) with an obtuse angle using the jailed semi-inflated balloon technique. In this case report, three-dimensional optical frequency domain imaging (OFDI) findings suggest that the jailed semi-inflated balloon technique is a safe and useful treatment for coronary true bifurcation lesions with an obtuse angle.
Case report
A 73-year-old male patient with angina pectoris was referred to our hospital. He had no coronary risk factors except that his father had a history of coronary artery disease. Electrocardiography revealed complete right bundle branch block, but there were no clear findings of prior Q-wave myocardial infarction. Chest X-ray revealed no abnormal findings. He had a history of PCI in the middle segment of the RCA, and a drug-eluting stent (Nobori 3.5 × 24 mm; Terumo, Tokyo, Japan) was implanted in this lesion. To assess the degree of myocardial ischemia, stress myocardial perfusion scintigraphy was performed. It showed clear evidence of reversible myocardial ischemia in the posterior wall. He was admitted to our hospital to undergo coronary angiography and angioplasty.
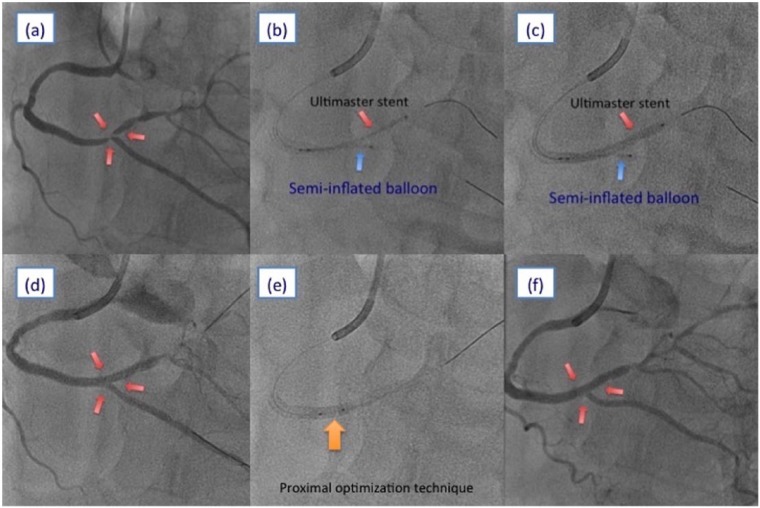
Coronary angiography revealed a true bifurcation lesion in the distal segment of the RCA between the posterior atrioventricular (PAV) artery and posterior descending artery (PDA) with an obtuse angle (Medina classification 1.1.1; Figure 1(a)). Because both PAV and PDA were large vessels, it was essential to preserve the blood flow of these vessels after stent implantation. Therefore, we decided to perform PCI using the jailed semi-inflated balloon technique for this true bifurcation lesion.
Figure 1.
(a) Right coronary angiogram of the left anterior oblique cranial view. (b, c) Stent implantation using the jailed semi-inflated balloon technique. (d) Right coronary angiogram of the left anterior oblique cranial view after stent implantation. (e) Proximal optimization technique using a non-compliant balloon. (f) Final coronary angiogram.
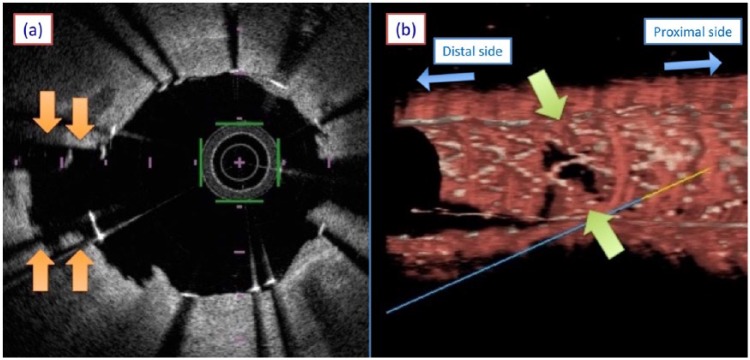
A 7-Fr Glidesheath Slender (Terumo) was inserted into the right radial artery. A 7-Fr JR4.0 guiding catheter with a side hole (Goodman, Aichi, Japan) was engaged into the RCA. A Runthrough NS Extra Floppy Guidewire (Terumo) was introduced into the PAV, and another was inserted into the PDA. The side branch balloon (Tazuna 2.0 × 20 mm; Terumo) in the PDA was initially inflated at low pressure (3 atm; Figure 1(b)). Subsequently, the main branch stent balloon (Ultimaster 2.75 × 33 mm; Terumo) in the PAV was inflated at nominal pressure, which jailed the side branch semi-inflated balloon (Figure 1(c)). Blood flow was preserved in both the PAV and the PDA after main vessel stenting (Figure 1(d)). Because three-dimensional OFDI (Terumo) clearly showed that the orifice of the PDA was patent (Figure 2(a) and (b)), we decided not to perform final kissing balloon inflation, and the protection guidewire was removed from the PDA. For optimization of stent apposition of the main branch, the proximal optimization technique was performed with a non-compliant balloon (Lifespear HP 3.25 × 12 mm; Japan Lifeline, Tokyo, Japan) (Figure 1(e)). A final coronary angiogram showed excellent results without any complications, including side branch narrowing or occlusion (Figure 1(f)).
Figure 2.
(a) Optical frequency domain imaging at the site of the side branch orifice after stent implantation. (b) Three-dimensional optical frequency domain imaging after stent implantation.
The post-procedure course was uneventful, and no major complications, including ischemic events, heart failure, or access-site complications, were observed. He was discharged the day after the procedure without any symptoms.
A follow-up coronary angiography was performed 8 months after the procedure. It showed excellent results and no findings of restenosis in both the main vessel and side branch.
Discussion
This case report, which includes three-dimensional OFDI findings, highlights the safety and efficacy of the jailed semi-inflated balloon technique for the treatment of coronary true bifurcation lesions with an obtuse angle. To the best of our knowledge, this is the first case report detailing a successful percutaneous coronary stent implantation observed by three-dimensional OFDI for a true bifurcation lesion using the jailed semi-inflated balloon technique.
PCI for coronary true bifurcation lesions remains challenging and is associated with the risk for side branch occlusion and a high rate of target lesion revascularization.10 Generally, the provisional stenting technique is recommended for most coronary bifurcation lesions.1–3 However, side branch occlusion or side branch narrowing after main vessel stenting sometimes occurs because of plaque shift, even when a protection guidewire is inserted into the side branch prior to stent implantation.4,5 Side branch occlusion may result in adverse outcomes, including procedure-related myocardial infarction and cardiac death.4 Therefore, efforts to reduce the risk for side branch occlusion are crucial.
The jailed semi-inflated balloon technique is an established method for treating coronary bifurcation lesions. It provides a high rate of procedural success and preserved side branch blood flow after main vessel stenting mainly because of the prevention of carina or plaque shift.7 However, there are little data regarding the configuration of bifurcation lesions after main vessel stenting using this technique. The OFDI can provide clearer and higher resolution images compared with intravascular ultrasound.11,12 Accordingly, we sought to evaluate the configuration of a true bifurcation lesion after stent implantation using the jailed semi-inflation balloon technique by three-dimensional OFDI. In this case, three-dimensional OFDI clearly showed that the orifice of the side branch was patent after main vessel stenting, and there were no signs of plaque or carina shift into the side branch (Figure 2(a) and (b)). The most important advantage of this method is that reinsertion of the guidewire into the jailed side branch via stent struts and final kissing balloon inflation are not essential after main vessel stenting. In this case, we decided not to perform final kissing balloon inflation after stenting according to OFDI findings of the orifice of the PDA. Only the proximal optimization technique was performed after main vessel stenting and removal of the protection guidewire from the side branch. To perform final kissing balloon inflation, it is necessary to reinsert a guidewire into the jailed side branch via stent struts. Because reinsertion of the guidewire after stenting is sometimes challenging and is also associated with the risk for side branch injury, the jailed semi-inflated balloon technique without final kissing balloon inflation is simpler and better than conventional provisional stenting techniques, especially in true bifurcation lesions.
There are some limitations with this technique. First, the proximal marker of the side branch balloon should be located more proximal to the stent edge to prevent entrapment.9 Therefore, we sometimes need a long balloon with double markers. Second, if the side branch is originating from the main branch at an acute angle, the responses of the plaque and carina after stent implantation may be different from what is reported here. Further studies on this technique using larger populations are needed to clarify this point.
In conclusion, our case report, which included three-dimensional OFDI findings, highlights that the jailed semi-inflated balloon technique is a safe and useful treatment for coronary true bifurcation lesions with an obtuse angle.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Information on hospital approval: our hospital does not require ethical approval for reporting individual cases.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
References
- 1. Hildick-Smith D, de Belder AJ, Cooter N, et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation 2010; 121: 1235–1243. [DOI] [PubMed] [Google Scholar]
- 2. Katritsis DG, Siontis GC, Ioannidis JP. Double versus single stenting for coronary bifurcation lesions: a meta-analysis. Circ Cardiovasc Interv 2009; 2: 409–415. [DOI] [PubMed] [Google Scholar]
- 3. Brunel P, Lefevre T, Darremont O, et al. Provisional T-stenting and kissing balloon in the treatment of coronary bifurcation lesions: results of the French multicenter “TULIPE” study. Catheter Cardiovasc Interv 2006; 68: 67–73. [DOI] [PubMed] [Google Scholar]
- 4. Hahn JY, Chun WJ, Kim JH, et al. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II Registry (COronary BIfurcation Stenting). J Am Coll Cardiol 2013; 62: 1654–1659. [DOI] [PubMed] [Google Scholar]
- 5. Burzotta F, Trani C. Jailed balloon protection and rescue balloon jailing techniques set the field for safer bifurcation provisional stenting. Int J Cardiol 2015; 201: 376–377. [DOI] [PubMed] [Google Scholar]
- 6. Burzotta F, Trani C, Sianos G. Jailed balloon protection: a new technique to avoid acute side-branch occlusion during provisional stenting of bifurcated lesions. Bench test report and first clinical experience. EuroIntervention 2010; 5: 809–813. [DOI] [PubMed] [Google Scholar]
- 7. Cayli M, Seker T, Gur M, et al. A novel-modified provisional bifurcation stenting technique: jailed semi-inflated balloon technique. J Interv Cardiol 2015; 28: 420–429. [DOI] [PubMed] [Google Scholar]
- 8. Depta JP, Patel Y, Patel JS, et al. Long-term clinical outcomes with the use of a modified provisional jailed-balloon stenting technique for the treatment of nonleft main coronary bifurcation lesions. Catheter Cardiovasc Interv 2013; 82: E637–E646. [DOI] [PubMed] [Google Scholar]
- 9. Singh J, Patel Y, Depta JP, et al. A modified provisional stenting approach to coronary bifurcation lesions: clinical application of the “jailed-balloon technique.” J Interv Cardiol 2012; 25: 289–296. [DOI] [PubMed] [Google Scholar]
- 10. Tiroch K, Mehilli J, Byrne RA, et al. Impact of coronary anatomy and stenting technique on long-term outcome after drug-eluting stent implantation for unprotected left main coronary artery disease. JACC Cardiovasc Interv 2014; 7: 29–36. [DOI] [PubMed] [Google Scholar]
- 11. Kobayashi Y, Kitahara H, Tanaka S, et al. Quantitative precision of optical frequency domain imaging: direct comparison with frequency domain optical coherence tomography and intravascular ultrasound. Cardiovasc Interv Ther 2016; 31: 79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Okamura T, Onuma Y, Garcia-Garcia HM, et al. First-in-man evaluation of intravascular optical frequency domain imaging (OFDI) of Terumo: a comparison with intravascular ultrasound and quantitative coronary angiography. EuroIntervention 2011; 6: 1037–1045. [DOI] [PubMed] [Google Scholar]