Abstract
Background
Brazil has the largest public health-system in the world, with 120 million people covered by its free primary care services. The Family Health Strategy (FHS) is the main primary care model, but there is no consensus on its impact on health outcomes. We systematically reviewed published evidence regarding the impact of the Brazilian FHS on selective primary care sensitive conditions (PCSC).
Methods
We searched Medline, Web of Science and Lilacs in May 2016 using key words in Portuguese and English, without language restriction. We included studies if intervention was the FHS; comparison was either different levels of FHS coverage or other primary health care service models; outcomes were the selected PCSC; and results were adjusted for relevant sanitary and socioeconomic variables, including the national conditional cash transfer program (Bolsa Familia). Due to differences in methods and outcomes reported, pooling of results was not possible.
Results
Of 1831 records found, 31 met our inclusion criteria. Of these, 25 were ecological studies. Twenty-one employed longitudinal quasi-experimental methods, 27 compared different levels the FHS coverage, whilst four compared the FHS versus other models of primary care. Fourteen studies found an association between higher FHS coverage and lower post-neonatal and child mortality. When the effect of Bolsa Familia was accounted for, the effect of the FHS on child mortality was greater. In 13 studies about hospitalizations due to PCSC, no clear pattern of association was found. In four studies, there was no effect on child and elderly vaccination or low-birth weight. No included studies addressed breast-feeding, dengue, HIV/AIDS and other neglected infectious diseases.
Conclusions
Among these ecological studies with limited quality evidence, increasing coverage by the FHS was consistently associated with improvements in child mortality. Scarce evidence on other health outcomes, hospitalization and synergies with cash transfer was found.
Introduction
Primary healthcare is essential for progress towards Universal Health Coverage [1], a key Sustainable Development Goal [2], which includes the provision of promotion, prevention, treatment, rehabilitation and palliative care to all citizens without significant financial burden [3]. Primary healthcare can contribute to Universal Health Coverage through expanding access to cost-effective, population-based healthcare and addressing the wider social determinants of health [4]. Further understanding of the impact of primary healthcare is essential to convincing policy-makers to invest in and expand it.
Brazil is an excellent setting for evaluating the impact of primary healthcare and Universal Health Coverage. Following health reform in the 80’s, Brazil has been expanding access to healthcare through the Unified Health System (SUS—Sistema Único de Saúde). Expansion of the SUS has been in line with the key principles outlined in the 1988 Brazilian Constitution of universalization, equity, and comprehensive care [5]–also core foundations of Universal Health Coverage [6]. The SUS can be considered the largest, universal, free-of-charge public health system in the world. Nearly 160 million people (76% of the Brazilian population) [7] depend exclusively on SUS services. Despite many limitations, the SUS is a major step towards Universal Health Coverage in Brazil [8].
At the heart of the SUS, is the Family Health Strategy (FHS) (Estratégia Saúde da Família in Portuguese), which is the main primary healthcare model in the country. It emphasizes health care in community health facilities and at home to a defined local population. Services are provided by family health teams composed of one physician, one nurse, one nurse aide, and from four to twelve full-time community health workers. Each team is responsible for up to 1000 families, or 3500–4500 people [9]. The FHS is progressively replacing the traditional primary healthcare units, which are based on physician-centered care, by either general practitioners or specialists.
The FHS has grown from previous healthcare models including the Community Health Agent Program (PACS, from Programa de Agentes Comunitários de Saúde in Portuguese) that was established by the Ministry of Health in 1994, which then became the Family Health Program in the late 1990s. In 2011, the Family Health Program was renamed FHS to place primary healthcare at the center of the SUS [10]. The population covered by the FHS has progressively increased from 7% in 1998 to 63% in 2015, corresponding to almost 120 million people [11, 12]. The FHS has expanded in a stepwise way across municipalities and across the country providing an opportunity for evaluation utilizing reasonable quality national databanks [13–16]. During expansion, priority catchment areas included preferentially the most vulnerable populations (poor neighborhoods, including slums) [12]. Concurrent with FHS expansion, conditional cash transfer programs were gradually implemented in the country as poverty-alleviating programs. In 2003, these programs were consolidated into the Bolsa Família Program, which includes specific health conditionality such as prenatal care, child development follow up and immunization [17]. The impact on health outcomes of these two large and interdependent national health programs is poorly understood.
There is evidence that primary healthcare in general can improve health outcomes–particularly child health, and infectious and cardiovascular diseases [18, 19]. However, although many studies of the impact of FHS on different outcomes have been published, results are inconsistent and have not been systematically reviewed previously. We undertook a systematic review to answer the following questions: (1) What is the impact of the Brazilian FHS expansion on primary health care health outcomes? (2) Is the FHS superior to other models of primary health care with regard to these outcomes? And (3) Does the Bolsa Familia Program enhance the effect of the FHS Program?
Material & methods
Literature search strategy
We searched three electronic databases [Medline (through PubMed), Web of Science and Lilacs] for records that included “Brazil” and “Family Health Strategy” (or multiple synonyms of these) and any relevant health outcomes in title or abstract, as key words, or as Medical Subject Heading (MeSH) term (see support information for PRISMA checklist and S1 Table with full search strategy). Relevant health outcomes included tuberculosis, child nutrition, infant mortality, low birth weight, infant diarrhea, breastfeeding, vaccination, AIDS/HIV, sexually transmitted diseases, dengue, neglected tropical diseases, prenatal care, and hospitalizations. Selected health outcomes were based on known primary healthcare sensitive-conditions [20]. Hospitalization due to conditions sensitive to primary care was defined according to the Brazilian Ministry of Health list [21], based on the 10th International Disease Classification. In Lilacs, the search strategy was conducted in Portuguese, MeSH terms in Portuguese (“Descritores em Saúde”– www.bireme.br) and their synonyms were used. The search was limited to the period from January 1994 (when the FHS started) until May 2016. No language restriction was used in the search. Lilacs includes theses from Brazilian Universities, and these were included.
Study selection
Titles, abstracts and full texts were screened by two independent reviewers (MB and AT), with consensus in each stage. A third reviewer (DM) was consulted to resolve disagreements.
Records were included if: (i) the population was Brazilian; (ii) the intervention evaluated was the FHS; (iii) there was a comparator of any form including different levels of population coverage of FHS (over time or geographical) or other primary health care models; (iv) at least one of the health outcomes cited above was measured and reported as one of the following absolute rates: incidence, prevalence or mortality rates and hospitalization. Treatment outcomes and vaccination coverage were also included. Studies that reported only process indicators (such as number of pre-natal visits or directly-observed treatment for tuberculosis) were not included; (v) the final results were adjusted for at least one of the following group of relevant variables (potential confounders of health outcomes): socioeconomic (e.g. education or socioeconomic status), sanitary condition (e.g. water supply and sewage) or health system access (e.g. number of physicians, or number of hospital beds); and vi) the study design was either experimental or observational. Reviews, opinions, and case reports were not included.
Statistical analysis and data synthesis
Since there was overlap of study populations (same set of patients, in the same range of time and area) and heterogeneity in methods employed pooling of data was not attempted. Descriptive results for each study are reported in the supplemental material. We summarized the main results of each study by groups of outcomes. Whenever there was sufficient detail in the manuscript, we converted effect sizes into rate ratio outcomes in order to make outcome measures comparable. When infant mortality was divided into two age periods [neonatal (i.e. death of infant aged up to 27 days and post neonatal (i.e. death of infant aged 28 days to 1 year)], we presented stratified data.
Assessment of methodological quality
Two reviewers (MB and TH) assessed the quality of each included study using a published checklist for observational and longitudinal studies [22]. This checklist was chosen as all studies were observational in nature and a large proportion (21 of 31 studies) utilized longitudinal methods. Disagreements in scoring between reviewers were resolved by discussion. Since the majority of studies used an ecological design, with geographical areas as the unit of analysis, we excluded three questions related to consent of participants. The remaining 30 questions were scored with two points for “yes” (indicating a lower risk of bias), one point if the answer was “unclear” or zero if the answer was “no” (higher risk). The final scores were obtained by summing questions, studies grouped into “generally higher quality” or “generally lower quality” based on the distributions of the scores obtained in this review. Studies scoring under 37 (out of 60) were considered low-quality.
Results
Study selection and major methodological issues
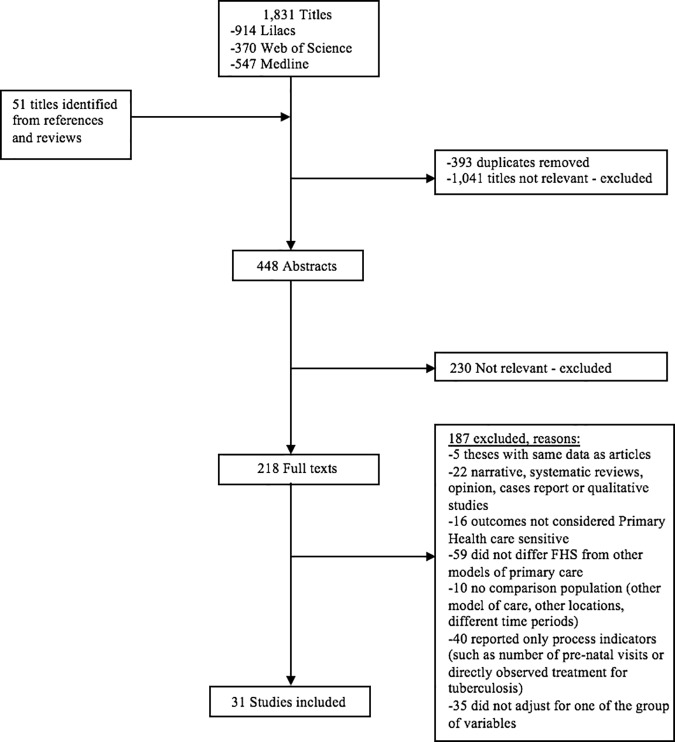
Of 1,831 publication titles found in the search, 218 studies were selected for full text review, from which 31 studies were selected that met our inclusion criteria (Fig 1).
Fig 1. Flow chart of study selection.
There was considerable variability concerning the units of analysis, the geographical regions included, methods of measurement of FHS coverage, and the outcome measured. Among the 31included studies [23–53], six used individual-level data [34, 47–49, 51, 52], with samples ranging from 961 to 7,534 subjects, whilst the remaining 25 studies were ecological analyses. Most (n = 19) ecological studies used municipalities as the unit of analysis, but three chose to analyze micro-regions (set of several neighbor municipalities) [25, 32, 44] or states [31, 37] (S2 Table). For these studies, potential ecological biases can be greater due to large differences in socio-economic characteristics between micro-regions, macro-regions, and states (e.g., the North and Northeast regions are poorer and less developed than the Southern and Southeast regions) [54].
The method of estimation of the proportion of the population covered by the FHS was different in the ecological studies. In six of them [27, 33, 37, 40, 46, 53], it was estimated by multiplying the number of family health teams by 3500 (estimated population covered by one team) while seven considered persons actually registered by the family health clinic [24, 30, 35, 38, 39, 41, 50]. The method was not specified in the 12 remaining ecological studies. No ecological study estimated the proportion of persons actually using the FHS clinics. Among the six individual-level studies, three studies [48, 49, 51] compared regular users of the service versus users of other models of primary health care.
In addition to differences in definitions of coverage, the classification of FHS coverage varied considerably including categorical ranges (e.g. <30%, 30–69%, >70%), as a continuous variable (i.e. percentage of the population covered), or simply availability or not of FHS in the municipality (S2 Table). Only four studies compared FHS with the traditional model of primary care [47–49, 51].
The outcome measurements and reported results were also highly variable (e.g. the proportion of reduction in mortality rate, number of deaths reduced per 1000 live births, and change in slope of association).
Of 21 studies that started after at least two years of the Bolsa Família Program implementation, only four [26, 30, 35, 50] examined the effect of this cash transfer program on health outcomes.
Quality of studies
All studies were observational in nature, with low overall quality of evidence. The lowest scoring study was 31, and the highest 45 (out of 60). Areas of potential bias that a high proportion of studies failed to address were justification of sample size (a risk of bias in conducting under-powered studies), reliability of outcomes and measurements used (a risk of measurement bias), issues of missing data and observations per time point, reporting of absolute effect sizes (most reported only relative effect sizes), quantitative assessment of any bias, and issues of generalizability (S1 Fig).
Of the 31 studies, we classified 10 into generally lower quality, and 21 as higher qualities. There was a general clustering of scores around 40–43 (S3–S5 Tables).
Impact on child mortality (n = 14, Table 1 & S3 Table) [23–36]
Table 1. Summary of results of included studies reporting neonatal (up to 27 days), post-neonatal (28 days- 1 year), infant (neonatal + post-neonatal) and child (up to 5 years) mortality (n = 14*).
| Outcome | N | Study Population | Effect in the Outcomes | Range of Effect Observed** | ||
|---|---|---|---|---|---|---|
| Improved | No effect | Worse | ||||
| Neonatal Mortality | 6 | – 5 studies: municipalities (range: 110–5,506 cities) | 423,24,27,28 | 225,26 | - | Ecological |
| – 2 studies: 11%-19% decrease in areas with ≥70% of FHS coverage | ||||||
| – 1 study: all Brazilian micro-regions (n = 558)† | – 1 study: 7.8%-13.8% decrease comparing areas with FHS vs. no FHS over a 3-year period | |||||
| – 1 study: decrease of 0.8/1,000 live births for each 10% increase of coverage. | ||||||
| Post-Neonatal Mortality | 8 | – 7 studies: municipalities (range: 110–5,506 cities) | 723−26,28–30 | 127 | - | Ecological |
| – 3 studies: 17%-66% decrease in areas with ≥70% of FHS coverage. | ||||||
| – 1 study: all Brazilian micro-regions (n = 558)† | – 3 studies: 0.8%-6% decrease for each 10% of increase of FHS coverage. | |||||
| – 1 study: 1.2%-9.8% decrease in areas with FHS vs. no FHS over a 3-year period. | ||||||
| Infant Mortality | 4 | – 1 study: all 26 Brazilian states | 331−33 | 134 | - | Ecological |
| – 2 studies: ~5% decrease for each 10% increase of FHS coverage. | ||||||
| – 1 study: 35 micro-regions from one state† | – 1 study: 3% decrease for each additional year after the municipality adopted the FHS. | |||||
| – 1 study: 4,488 municipalities | Individual level | |||||
| – No effect. | ||||||
| – 1 study: Individual level (2,144 children) | ||||||
| Child Mortality | 4 | – 4 studies: municipalities (range: 224–4,488 cities) | 424,33,35,36 | - | - | Ecological |
| – 2 studies: ~13% decrease in areas with ≥70% of FHS coverage | ||||||
| – 1 study: 5% decrease for each 10% increase in FHS | ||||||
| – 1 study: 3% decrease or each additional year in the FHS | ||||||
Notes
*5 studies reported both neonatal and post-neonatal mortality; 1 study reported neonatal, post-neonatal mortality and child mortality, 1 study reported both infant mortality and child mortality.
†Micro-regions: Set of several neighbor municipalities- (according with the Brazilian 2010 census the average population for micro-region is ~342,000)
** If no change–then results not summarized
Abbreviations: FHS: Family Health Strategy
Fourteen included studies examined the association between FHS coverage and mortality of children, of which five analyzed the effect on both neonatal (0–28 days) and post-neonatal (28 days to one year) mortality [23, 25–28], two only post-neonatal mortality [29, 30], one both infant mortality (0–1 year) and child (under 5) mortality [33], three just infant mortality [31, 32, 34], two just child mortality [35, 36], and one study reported neonatal, post-neonatal and child mortality [24]. All of these studies, apart from one [26], were scored of higher quality (S3 Table).
There was an association between higher FHS coverage and lower mortality in most studies (13 out of 14) across different age stratifications within child mortality. No studies reported increased mortality from FHS coverage. Of the six studies examining neonatal mortality, lower mortality was associated with increased FHS coverage in four. Of the eight studies examining the post-neonatal period, only one showed a non-significant finding, with the reductions in mortality rates ranging from 0.8% to 66%, depending on the level of coverage. Of four studies examining infant mortality, only one found a non-significant effect of FHS (Table 1).
Only one study employed individual-level data and reported no association between infant mortality and FHS coverage [34] (Table 1).
Three studies analyzed the period after the Bolsa Família Program implementation. All three [26, 30, 35] studies showed that FHS had an independent beneficial effect beyond improvements in health from the Bolsa Família Program. Two [26, 30] studies reported that the Bolsa Família Program effects were synergistic with the FHS (i.e. there were greater reductions in mortality from FHS coverage with higher Bolsa Família coverage). No studies that evaluated infant mortality compared the FHS with other models of primary care.
Impact on hospitalization for primary care sensitive causes (n = 13, Table 2 & S4 Table) [34, 36–47]
Table 2. Summary of results of included studies reporting hospitalization due to primary care sensitive causes* (n = 13).
| Outcome | N | Study Population | Effect in the Outcomes | Range of Effect Observed** | ||
|---|---|---|---|---|---|---|
| Decrease | No effect | Increase | ||||
| Hospitalizations due to primary care sensitive causes (diseases not specified) | 6 | – 2 studies: municipalities (range 78–188 cities) | 337,40,44 | 241,47 | 145 | Ecological |
| – Decreased -3 studies: 4%-10% decrease in areas with FHS≥70% coverage | ||||||
| – 1 study: All states of Brazil (26 States) | – Increased—1 study: increase by 1.0/10,000 habitants for additional year in the FHS | |||||
| – 1 study: All Brazilian micro-region (n = 558)† | Individual level | |||||
| – No effect | ||||||
| – 1 study: 1,909 census tract in one municipality | ||||||
| – 1 study: Individual level (1,058 patients) | ||||||
| Hospitalizations due to chronic diseases | 4 | – All studies: municipalities (range: 137–5,507 cities) | 438,39,42,43 | - | - | Ecological |
| – Decreased | ||||||
| (e.g. diabetes, cardiovascular) | 2 studies: 13%-30% decrease in areas with high coverage of FHS | |||||
| 2 studies: 0.71–11% decrease for each 10% increase of FHS coverage, but only in women for selected outcomes (diabetes and myocardium infarction) | ||||||
| Hospitalizations due to diarrhea and lower respiratory infection | 3 | – 2 studies: municipalities (range: 12–224 cities) | 134 | 236,46 | - | Ecological |
| – No effect | ||||||
| – 1 study: Individual level (2,144 children) | Individual level | |||||
| – Decreased -1 study: 70% decrease when children were covered by FHS (due diarrhea) †† | ||||||
Notes
* Primary care sensitive causes included 20 groups of diagnosis available Alfradique et al21
†Micro-regions: Set of several neighbor municipalities (according with the Brazilian 2010 census the average population for micro-region is ~342,000)
** If no change–then results not summarized
†† Had no effect in the rates of hospitalization for respiratory infection.
Abbreviations: FHS: Family health strategy
There was variability in the selected conditions, categorization of exposure, target population, and outcomes measured in the 13 studies analyzing hospitalizations for primary care sensitive conditions. Four [41, 43, 46, 47] of these studies were considered of generally lower quality (S4 Table).
Of these studies, eight found a decrease in the hospitalization rates associated with increased FHS coverage, although in two [42, 43] the effect was seen only in women for diabetes and cardiovascular diseases. The reported effect sizes ranged from 0.71–11% for each 10% increase in FHS coverage. Only one [45] study showed increased hospitalizations from FHS expansion (Table 2). Of the four studies that showed no significant effects [36, 41, 46, 47], three [41, 46, 47] were considered of generally lower quality. All studies that showed decreased or increased in hospitalizations rate, apart from one [43], were scored as high quality.
Two [34, 47] studies had individual level design, one [34] of which associated a decrease in hospitalizations of children due to diarrhea with higher FHS coverage (Table 2).
Eleven studies analyzed the period after the Bolsa Família Program implementation, but none of these studies included the Bolsa Família as a co-variable in their regression models. Only one study [47] compared the FHS with other primary care models and no difference was observed (S4 Table).
Impact on other health outcomes (n = 7, Table 3 & S5 Table) [34, 48–53]
Table 3. Summary of results of included studies for all other health outcomes (n = 7*).
| Outcome | N | Study Population | Effect in the Outcomes | Range of Effect Observed** | ||
|---|---|---|---|---|---|---|
| Improved | No Effect | Worse | ||||
| Prenatal care | 2 | – 2 studies individual level: 961–2,144 population size | 148 | 134 | Individual Level | |
| – 1 study: 44% increase in vaccination coverage in pregnant women who attended prenatal care in FHS. 100% increase in maternal admission when prenatal care was in FHS. No effect on proportion with low birth weigh | ||||||
| Vaccination coverage | 2 | – 2 studies individual level: range 2,144–7,534 interviews | - | 234,49 | - | - |
| Infectious Diseases (Leprosy, Congenital Syphilis and Tuberculosis) | 3 | – 2 studies: municipality (range 897–1,358 cities) | 150 | 151 | 153 | Ecological Level |
| – 1 study: 12% increase in the detection rate of Leprosy when FHS>70% | ||||||
| – 1 study: Individual level:1,396 patients | – 1 study: 0.04/10,000 more cases of congenital syphilis for each 10% increase of FHS coverage | |||||
| Individual Level | ||||||
| – No Effect | ||||||
| Child Malnutrition | 1 | – 1 study: Individual level: 3,931 children | 152 | - | - | Individual Level |
| – 1 Study: Odds of child malnutrition were 48% lower in areas with FHS coverage of 50%. | ||||||
Notes
* One study reported both prenatal care (low weight birth outcome), and vaccination coverage
** If no change–then results not summarized
Abbreviations: FHS: Family health strategy.
Seven studies examined other health outcomes beyond child mortality and hospitalizations for primary health care sensitive conditions. All but two studies [34, 50] were considered of lower quality (S5 Table).
Two studies [34, 48] examined a range of pre-natal care outcomes. Only in one [48] study, which was of lower quality, and for only one outcome (tetanus vaccination) was the FHS coverage associated with better outcomes in prenatal care: a 44% increase in the vaccination coverage in pregnant women, when compared with another model of primary care. No effect was observed in the other two studies that reported vaccination coverage. A small increase of 0.04 per 1000 cases (CI 95% 0.003; 0.07) of congenital syphilis was observed for each 10% increase of FHS coverage [53]. There was an association between increased leprosy detection [50] and lower child malnutrition [52] with increasing FHS coverage. No effect in tuberculosis end of treatment outcomes was observed when FHS was compared with other models of primary care [51] (Table 3).
Five studies [34, 48, 49, 51, 52] had an individual-level design; in two of them the FHS had a positive effect: on child malnutrition [52] and on tetanus vaccination [48] (Table 3).
Only one [50] study evaluated the Bolsa Família Program together with FHS, and reported a greater detection of leprosy cases when coverage by both the Bolsa Família Program and the FHS were higher (S5 Table).
Finally, none of the studies that met our inclusion criteria reported on breast-feeding, dengue, HIV/AIDS or other neglected infectious diseases.
Discussion
There is reasonable evidence that increased coverage of FHS is associated with lower infant (mainly post-neonatal) and child mortality. The association between FHS coverage and hospitalizations from primary care sensitive conditions was less clear, but many studies reported reductions in hospitalization rates. Although the FHS was also associated with improvements in other health outcomes such as child malnutrition, congenital syphilis, leprosy detection and prenatal anti-tetanic vaccination, the scarce number of publications and greater risk of bias in these studies precludes generalization.
Infant and child mortality were the most frequently studied outcomes, potentially explaining the generally more reliable evidence and consistent associations. FHS coverage was associated with larger reductions in post-neonatal mortality than in neonatal mortality, which may be expected given neonatal deaths are often related to birth complications or congenital conditions and less affected by improvement of primary care assistance [55, 56]. However, some studies did show some reduction in mortality in the neonatal period, which may be explained with better pre-natal care and timely referral to secondary care. The Bolsa Família Program and literacy of adults had a similar independent effect on infant mortality, sometimes stronger than the FHS effect [30, 31, 35]. The greater association between FHS coverage and improved health outcomes when Bolsa Familia was present is expected given the compulsory usage of healthcare services (for example childhood check-ups) to receive benefit payments.
The relationship between FHS coverage and hospitalizations for primary care sensitive conditions was less clear, although a majority of studies found hospitalization rates declined. Municipality selection, baseline conditions, number of existing hospital beds and healthcare workers, selected diagnoses and confounder adjustment may explain the differences between findings. Unfortunately, elucidating potential explanatory trends is beyond the ability of this review. Understanding the impact of the FHS on hospitalizations is important given hospitalizations are a major driver of health costs. The theory underpinning the relationship between primary health care and hospitalizations is complex and may partially explain the lack of clarity in the findings. Whilst primary care sensitive hospitalizations should fall with increased access to primary health care, this may not be the case if the services are weak (e.g. the technical capacity of staff is insufficient) or primary care sensitive conditions are in an advanced stage. In this case, hospitalizations may increase. On the other hand, the effect for chronic diseases such as hypertension or diabetes is likely to involve long time lags. Finally, hospitalization rates depend also on bed availability, not examined in the current study.
There has been significant improvement in socioeconomic and sanitary conditions in Brazil in the last three decades, which are likely to explain many improvements in health. To address this, we only included studies that adjusted for relevant socioeconomic, sanitary or health access conditions, which excluded 35 studies.
Regardless of the effect, only a minority of studies compared FHS with other models of primary care, so we cannot make conclusions on benefits from the FHS model or coverage compared to other models of primary care. The four studies that compared FHS versus other models [47–49, 51] showed no differences in the majority of outcomes. Even so, there is large variation in historical primary health care services across Brazil and between urban and rural areas. Many are fragmented, under philanthropic or private control, exist as part of hospital systems, or do not exist at all. Moreover, parts of both the FHS covered and non-covered population have access to private healthcare which constitute 24% of the Brazilian population [7]. This is likely to make the relationship between FHS coverage and health outcomes more complex and was insufficiently addressed in the studies. The lack of clarity in actual control or comparator services also clouds the ability to draw comparisons, and raises the question “what are we exactly comparing the FHS to?” The FHS is a highly standardized program with mandated components from the Federal level, so in some areas the FHS program is an expansion of services to an unserved population, whilst in other areas, it offers a change in the structure and strategy of primary health care services focusing on outreach, prevention, promotion, and person-centered care. More research is required on which dimensions of the FHS are driving the reported improvements in health.
Our review has a number of limitations. Firstly, our search may have missed important studies. We only searched three electronic databases, and non-peer reviewed articles and reports may have been missed. Secondly, we restricted our searches to a few outcomes, based on the assumption that those were the most primary care sensitive. Thirdly, our assessment of quality and bias was focused towards ecological, longitudinal studies, and only provides a weak understanding of the actual biases present. Inference on the quality of these studies beyond this review is limited. Our findings and analyses were based on weak, ecological studies with the potential for the ecological fallacy, with different methods to estimate the exposure to the FHS. However, many studies used municipalities, with small population sizes, potentially reducing this fallacy. Additionally, many studies employed panel or longitudinal regression, which can be considered of generally better evidence than cross-sectional studies, and can control for temporal changes beyond the FHS. Lastly, the expansion of the FHS was not completely random, with municipal governments opting to provide the FHS services and many clinics built preferentially in poorer neighborhoods [6, 18]. This may confound and bias many studies as unobserved factors determining the FHS uptake may also explain changes in health outcomes. As much of the ecological studies reviewed may suffer from these biases, we cannot consider the evidence conclusive, and studies with more robust methods must be conducted.
Despite these limitations, this is the first critical appraisal, to the authors’ knowledge, of the literature on the effect of the FHS on the health outcomes, and one of only a few systematic reviews examining a national primary care program in a low- or middle-income country. We employed a broad search strategy looking for studies published in different languages, used restriction criteria to ensure only studies of reasonably high quality were included, and considered conditions sensitive to primary care.
Furthermore, the outcomes examined have important implications for other low- or middle-income country’s considering expanding primary health care as part of universal health coverage.
Conclusion
The FHS expansion was consistently associated with reductions in post-neonatal and child mortality, and less-consistently with reductions in hospitalizations from primary care sensitive conditions. This evidence supports the vital role for primary healthcare in improving health outcomes, and as part of progress towards Universal Health Coverage and the Sustainable Development Goals.
Supporting information
(DOC)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We want to thank Dr. Ronir Raggio Luiz for his help in statistical interpretation and for his review of the first manuscript draft.
This work was funded by: Ministère des Relations Internationales de la Francophonie, (Quebec-Rio project Fund 238899), Fundação Carlos Chagas de Amparo à Pesquisa do Rio de Janeiro (FAPERJ, grant # E-26/110.637/2012). AT has a grant by Conselho Nacional de Desenvolvimento e Pesquisa (CNPq, grant # 303010/2015-0).
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was funded by: Ministère des Relations Internationales de la Francophonie, (Quebec-Rio project Fund 238899), Fundação Carlos Chagas de Amparo à Pesquisa do Rio de Janeiro (FAPERJ, grant # E-26/110.637/2012). AT has a grant by Conselho Nacional de Desenvolvimento e Pesquisa (CNPq, grant # 303010/2015-0). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Stigler FL, Macinko J, Pettigrew LM, Kumar R, van Weel C. No universal health coverage without primary health care. Lancet. 2016;387(10030):1811 Epub 2016/05/21. doi: 10.1016/s0140-6736(16)30315-4. . [DOI] [PubMed] [Google Scholar]
- 2.Tangcharoensathien V, Mills A, Palu T. Accelerating health equity: the key role of universal health coverage in the Sustainable Development Goals. BMC medicine. 2015;13:101 Epub 2015/05/01. doi: 10.1186/s12916-015-0342-3 ; PubMed Central PMCID: PMCPMC4415234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tracking universal health coverage: First global monitoring report. WHO. 2015. Available on: http://www.who.int/healthinfo/universal_health_coverage/report/2015/en/.
- 4.Pettigrew LM, De Maeseneer J, Anderson MI, Essuman A, Kidd MR, Haines A. Primary health care and the Sustainable Development Goals. Lancet. 2015;386(10009):2119–21. Epub 2015/12/08. doi: 10.1016/S0140-6736(15)00949-6 . [DOI] [PubMed] [Google Scholar]
- 5.Lei Nº 8.080, de 19 de Setemrbo de 1990. Preseidência da República do Brasil. Available on: http://www.planalto.gov.br/ccivil_03/leis/L8080.htm.
- 6.Paim J, Travassos C, Almeida C, Bahia L, Macinko J. The Brazilian health system: history, advances, and challenges. Lancet. 2011;377(9779):1778–97. Epub 2011/05/13. doi: 10.1016/S0140-6736(11)60054-8 . [DOI] [PubMed] [Google Scholar]
- 7.Agência Nacional de Saúde Suplementar. ANS. Sala da situação. Available on: http://www.ans.gov.br/perfil-do-setor/dados-e-indicadores-do-setor/sala-de-situacao. Acessed on June 2017.
- 8.Kleinert S, Horton R. Brazil: towards sustainability and equity in health. Lancet. 2011;377(9779):1721–2. Epub 2011/05/13. doi: 10.1016/S0140-6736(11)60433-9 . [DOI] [PubMed] [Google Scholar]
- 9.Política Nacional de Atenção Básica. Ministério da Saúde do Brasil. Available on: http://189.28.128.100/dab/docs/publicacoes/geral/pnab.pdf.
- 10.Fontenelle LF. Mudanças recentes na Política Nacional de Atenção Básica: uma análise crítica. 2012. 2012;7(22):5 Epub 2012-08-29. doi: 10.5712/rbmfc7(22)417 [Google Scholar]
- 11.Histórico da Cobertura. Ministério da Saúde do Brasil. Available on: http://dab.saude.gov.br/portaldab/historico_cobertura_sf.php.
- 12.Macinko J, Harris MJ. Brazil's family health strategy—delivering community-based primary care in a universal health system. The New England journal of medicine. 2015;372(23):2177–81. Epub 2015/06/04. doi: 10.1056/NEJMp1501140 . [DOI] [PubMed] [Google Scholar]
- 13.Rasella D, Aquino R, Barreto ML. Impact of the Family Health Program on the quality of vital information and reduction of child unattended deaths in Brazil: an ecological longitudinal study. BMC public health. 2010;10:380 Epub 2010/07/01. doi: 10.1186/1471-2458-10-380 ; PubMed Central PMCID: PMCPmc3091549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Szwarcwald CL. Strategies for improving the monitoring of vital events in Brazil. International journal of epidemiology. 2008;37(4):738–44. Epub 2008/07/26. doi: 10.1093/ije/dyn130 . [DOI] [PubMed] [Google Scholar]
- 15.Paes NA. Quality of death statistics by unknown causes in Brazilian states. Rev Saude Publica. 2007;41(3):436–45. Epub 2007/05/23. . [DOI] [PubMed] [Google Scholar]
- 16.Jorge MH, Laurenti R, Gotlieb SL. Quality analysis of Brazilian vital statistics: the experience of implementing the SIM and SINASC systems. Cien Saude Colet. 2007;12(3):643–54. Epub 2007/08/08. . [DOI] [PubMed] [Google Scholar]
- 17.Bolsa Família: Brazil’s social security cash transfer programme. International Social Security Association. 2013. Available on: https://www.issa.int/-/brazilian-social-security-programme-receives-prestigious-issa-award.
- 18.Macinko J, Starfield B, Shi L. The contribution of primary care systems to health outcomes within Organization for Economic Cooperation and Development (OECD) countries, 1970–1998. Health services research. 2003;38(3):831–65. Epub 2003/06/26. PubMed Central PMCID: PMCPMC1360919. doi: 10.1111/1475-6773.00149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. The Milbank quarterly. 2005;83(3):457–502. Epub 2005/10/06. doi: 10.1111/j.1468-0009.2005.00409.x ; PubMed Central PMCID: PMCPMC2690145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guia prático do Programa Saúde da Família. Ministério da Saúde. Secretaria das Políticas de Saúde, Departamento de Atenção Básica. 2001. Available on: http://bvsms.saude.gov.br/bvs/publicacoes/partes/guia_psf1.pdf.
- 21.Alfradique ME, Bonolo Pde F, Dourado I, Lima-Costa MF, Macinko J, Mendonca CS, et al. Ambulatory care sensitive hospitalizations: elaboration of Brazilian list as a tool for measuring health system performance (Project ICSAP—Brazil). Cad Saude Publica. 2009;25(6):1337–49. [DOI] [PubMed] [Google Scholar]
- 22.Tooth L, Ware R, Bain C, Purdie DM, Dobson A. Quality of reporting of observational longitudinal research. American journal of epidemiology. 2005;161(3):280–8. Epub 2005/01/27. doi: 10.1093/aje/kwi042 . [DOI] [PubMed] [Google Scholar]
- 23.Aquino R, de Oliveira NF, Barreto ML. Impact of the family health program on infant mortality in Brazilian municipalities. Am J Public Health. 2009;99(1):87–93. doi: 10.2105/AJPH.2007.127480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rasella D, Aquino R, Barreto ML. Reducing childhood mortality from diarrhea and lower respiratory tract infections in Brazil. Pediatrics. 2010;126(3):2009–3197. [DOI] [PubMed] [Google Scholar]
- 25.Macinko JMdSM F.; Guanais F. C.; da Silva Simoes C. C. Going to scale with community-based primary care: an analysis of the family health program and infant mortality in Brazil, 1999–2004. Social science & medicine (1982). 2007;65(10):2070–80. Epub 2007/08/11. doi: 10.1016/j.socscimed.2007.06.028 . [DOI] [PubMed] [Google Scholar]
- 26.Shei A. Brazil's conditional cash transfer program associated with declines in infant mortality rates. Health Aff. 2013;32(7):1274–81. [DOI] [PubMed] [Google Scholar]
- 27.Serra RAM. Uma avaliação empírica do impacto do programa saúde da família sobre a saúde infantil no estado de São Paulo In: Piola SFJ, Antonio Elias, editor. Prêmio em economia da saúde: 1ºprêmio nacional, 2004: coletânea premiada. Brasília: Instituto de Pesquisa Econômica Aplicada; 2005. p. 79–112. [Google Scholar]
- 28.Rocha FFN, Marislei; Duarte Peixoto, Sandro Garcia. Primary health care policies: investigation on morbidity. Applied Economics Letters. 2013;20(11):1046–51. doi: 10.1080/13504851.2013.774456 [Google Scholar]
- 29.Guanais FC, Macinko J. The health effects of decentralizing primary care in Brazil. Health Aff. 2009;28(4):1127–35. [DOI] [PubMed] [Google Scholar]
- 30.Guanais FC. The combined effects of the expansion of primary health care and conditional cash transfers on infant mortality in Brazil, 1998–2010. Am J Public Health. 2013;103(11):2000–6. doi: 10.2105/AJPH.2013.301452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Macinko J, Guanais FC, de Fatima M, de Souza M. Evaluation of the impact of the Family Health Program on infant mortality in Brazil, 1990–2002. J Epidemiol Community Health. 2006;60(1):13–9. doi: 10.1136/jech.2005.038323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zanini RR, Moraes AB, Giugliani ER, Riboldi J. Infant mortality trends in the State of Rio Grande do Sul, Brazil, 1994–2004: a multilevel analysis of individual and community risk factors. Cad Saude Publica. 2009;25(5):1035–45. [DOI] [PubMed] [Google Scholar]
- 33.Rocha R, Soares RR. Evaluating the impact of community-based health interventions: evidence from Brazil's Family Health Program. Health Econ. 2010;19:126–58. doi: 10.1002/hec.1607 [DOI] [PubMed] [Google Scholar]
- 34.Roncalli AGL, Costa de Kenio. Impacto do Programa Saúde da Família sobre indicadores de saúde da criança em municípios de grande porte da região Nordeste do Brasil. Ciênc saúde coletiva. 2006;11(3):713–24. [Google Scholar]
- 35.Rasella D, Aquino R, Santos CA, Paes-Sousa R, Barreto ML. Effect of a conditional cash transfer programme on childhood mortality: a nationwide analysis of Brazilian municipalities. Lancet. 2013;382(9886):57–64. doi: 10.1016/S0140-6736(13)60715-1 [DOI] [PubMed] [Google Scholar]
- 36.Rasella D . Impact of the Water for All Program (PAT) on childhood morbidity and mortality from diarrhea in the Bahia State, Brazil. Cad Saude Publica. 2013;29(1):40–50. [DOI] [PubMed] [Google Scholar]
- 37.Dourado I, Oliveira VB, Aquino R, Bonolo P, Lima-Costa MF, Medina MG, et al. Trends in primary health care-sensitive conditions in Brazil: the role of the Family Health Program (Project ICSAP-Brazil). Med Care. 2011;49(6):577–84. doi: 10.1097/MLR.0b013e31820fc39f [DOI] [PubMed] [Google Scholar]
- 38.Macinko J, Dourado I, Aquino R, Bonolo Pde F, Lima-Costa MF, Medina MG, et al. Major expansion of primary care in Brazil linked to decline in unnecessary hospitalization. Health Aff. 2010;29(12):2149–60. [DOI] [PubMed] [Google Scholar]
- 39.Rasella D, Harhay MO, Pamponet ML, Aquino R, Barreto ML. Impact of primary health care on mortality from heart and cerebrovascular diseases in Brazil: a nationwide analysis of longitudinal data. Bmj. 2014;3(349). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carvalho SC, Mota E, Dourado I, Aquino R, Teles C, Medina MG. Hospitalizations of children due to primary health care sensitive conditions in Pernambuco State, Northeast Brazil. Cad Saude Publica. 2015;31(4):744–54. Epub 2015/05/07. . [DOI] [PubMed] [Google Scholar]
- 41.Pazo RG, Frauches Dde O, Molina Mdel C, Cade NV. Hierarchical modeling of determinants associated with hospitalizations for ambulatory care sensitive conditions in Espirito Santo State, Brazil. Cad Saude Publica. 2014;30(9):1891–902. [DOI] [PubMed] [Google Scholar]
- 42.Guanais F, Macinko J. Primary care and avoidable hospitalizations: evidence from Brazil. J Ambul Care Manage. 2009;32(2):115–22. doi: 10.1097/JAC.0b013e31819942e51 [DOI] [PubMed] [Google Scholar]
- 43.Luz Cde C, Junger WL, Cavalini LT. Analysis of prehospital care for stroke and acute myocardial infarction in the elderly population of Minas Gerais, Brazil. Rev Assoc Med Bras. 2010;56(4):452–6. [DOI] [PubMed] [Google Scholar]
- 44.Macinko J, de Oliveira VB, Turci MA, Guanais FC, Bonolo PF, Lima-Costa MF. The influence of primary care and hospital supply on ambulatory care-sensitive hospitalizations among adults in Brazil, 1999–2007. Am J Public Health. 2011;101(10):1963–70. doi: 10.2105/AJPH.2010.198887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mendonca CS, Harzheim E, Duncan BB, Nunes LN, Leyh W. Trends in hospitalizations for primary care sensitive conditions following the implementation of Family Health Teams in Belo Horizonte, Brazil. Health Policy Plan. 2012;27(4):348–55. doi: 10.1093/heapol/czr043 [DOI] [PubMed] [Google Scholar]
- 46.Monahan LJ, Calip GS, Novo PM, Sherstinsky M, Casiano M, Mota E, et al. Impact of the Family Health Program on gastroenteritis in children in Bahia, Northeast Brazil: an analysis of primary care-sensitive conditions. J Epidemiol Glob Health. 2013;3(3):175–85. doi: 10.1016/j.jegh.2013.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Silva JAd. A study of primary health care through the indicator: Hospitalization for Ambulatory Care Sensitive Conditions (CSAA).: State University of Rio de Janeiro; 2011. [Google Scholar]
- 48.Mendoza-Sassi RA, Cesar JA, Teixeira TP, Ravache C, Araujo GD, Silva TC. Differences in prenatal care between health services under the Family Health Strategy and traditional primary care clinics in Rio Grande, Rio Grande do Sul State, Brazil. Cad Saude Publica. 2011;27(4):787–96. [DOI] [PubMed] [Google Scholar]
- 49.Lima-Costa MF, Turci MA, Macinko J. A comparison of the Family Health Strategy to other sources of healthcare: utilization and quality of health services in Belo Horizonte, Minas Gerais State, Brazil. Cad Saude Publica. 2013;29(7):1370–80. [DOI] [PubMed] [Google Scholar]
- 50.Nery JS, Pereira SM, Rasella D, Penna ML, Aquino R, Rodrigues LC, et al. Effect of the Brazilian conditional cash transfer and primary health care programs on the new case detection rate of leprosy. PLoS Negl Trop Dis. 2014;8(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.de Albuquerque Mde F, Ximenes RA, Lucena-Silva N, de Souza WV, Dantas AT, Dantas OM, et al. Factors associated with treatment failure, dropout, and death in a cohort of tuberculosis patients in Recife, Pernambuco State, Brazil. Cad Saude Publica. 2007;23(7):1573–82. Epub 2007/06/19. . [DOI] [PubMed] [Google Scholar]
- 52.Benicio MH, Martins AP, Venancio SI, Barros AJ. Estimates of the prevalence of child malnutrition in Brazilian municipalities in 2006. Rev Saude Publica. 2013;47(3):560–70. [DOI] [PubMed] [Google Scholar]
- 53.Araujo CL, Shimizu HE, Sousa AI, Hamann EM. Incidence of congenital syphilis in Brazil and its relationship with the Family Health Strategy. Rev Saude Publica. 2012;46(3):479–86. [DOI] [PubMed] [Google Scholar]
- 54.Censo demográfico Brasileiro. IBGE. 2010. Available: http://biblioteca.ibge.gov.br/visualizacao/periodicos/93cd_2010_caracteristicas_populacao_domicilios.pdf.
- 55.Martines J, Paul VK, Bhutta ZA, Koblinsky M, Soucat A, Walker N, et al. Neonatal survival: a call for action. Lancet. 2005;365(9465):1189–97. Epub 2005/03/30. doi: 10.1016/s0140-6736(05)71882-1 . [DOI] [PubMed] [Google Scholar]
- 56.Victora CG, Bryce J, Fontaine O, Monasch R. Reducing deaths from diarrhoea through oral rehydration therapy. Bulletin of the World Health Organization. 2000;78(10):1246–55. Epub 2000/12/02. ; PubMed Central PMCID: PMCPMC2560623. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.