Abstract
Study Design:
Systematic literature review with meta-analysis.
Objective:
Thoracolumbar (TL) fractures can be treated conservatively or surgically. Especially, the treatment strategy for incomplete and complete TL burst fractures (A3 and A4, AOSpine classification) in neurologically intact patients remains controversial. The aim of this work was to collate the clinical evidence on the respective treatment modalities.
Methods:
Searches were performed in PubMed and the Web of Science. Clinical and radiological outcome data were collected. For studies comparing operative with nonoperative treatment, the standardized mean differences (SMD) for disability and pain were calculated and methodological quality and risk of bias were assessed.
Results:
From 1929 initial matches, 12 were eligible. Four of these compared surgical with conservative treatment. A comparative analysis of radiological results was not possible due to a lack of uniform reporting. Differences in clinical outcomes at follow-up were small, both between studies and between treatment groups. The SMD was 0.00 (95% CI −0.072, 0.72) for disability and −0.05 (95% CI −0.91, 0.81) for pain. Methodological quality was high in most studies and no evidence of publication bias was revealed.
Conclusions:
We did not find differences in disability or pain outcomes between operative and nonoperative treatment of A3 and A4 TL fractures in neurologically intact patients. Notwithstanding, the available scores have been developed and validated for degenerative diseases; thus, their suitability in trauma may be questionable. Specific and uniform outcome parameters need to be defined and enforced for the evaluation of TL trauma.
Keywords: thoracolumbar burst fractures, A3 and A4 spinal fractures, AOSpine classification, neurologically intact patients, conservative therapy, surgical therapy, functional outcome, meta-analysis
Introduction
Burst fractures of the thoracolumbar spine account for approximately 45% of all major thoracolumbar injuries. At least half of the patients with thoracolumbar burst fractures maintain full neurological function.1 In spite of the high incidence of thoracolumbar burst fractures without neurological deficit and the extensive reporting on this topic in the literature, the optimal treatment strategies for this type of injury remain controversial.
Many reviews have compiled information to compare different treatment modalities. Since 2000, reviews and meta-analyses on surgical strategies have been published on fusion versus nonfusion,2 minimally invasive surgery versus open surgery,3,4 anterior versus posterior approach,5 early versus late treatment,6,7 or looked at a specific treatment types in itself, for example, pedicle screw fixation8 or surgical treatment in general.9 Fewer reviews have been published about conservative treatment options, for example, on the usefulness of orthoses.10,11
Likewise, the amount of reviews with the aim of directly comparing operative to non-operative treatment is scarce. Gnanenthiram et al12 published a meta-analysis in 2012, which identified 4 comparative primary studies published in 1998,13 2001,14 2003,15 and 2006.16 A Cochrane review, published in 200617 and updated in 2013,18 focused on randomized clinical trials (RCTs). In the update, 2 primary studies were deemed eligible,15,16 which were also included in the aforementioned meta-analysis. Another systematic review by Thomas et al19 in 2006 identified 21 studies of which only half were considered having a quality score of 50% or more. The 7 studies that achieved a quality score of greater than 50% dated from 1993 to 2004 and were presented in greater detail while the majority of the lower quality studies dated from the 1990s.
Ghobrial et al20 published a review on adverse events related to operative or nonoperative treatment in 2014. In contrast to our review, they excluded noncomparative studies and 63% of the operatively treated patients had a neurological deficit.
None of the aforementioned reviews comparing surgical with nonsurgical treatment narrowed the target population to AO A3 and A4 fractures21,22 in neurologically intact patients, although these are the most controversial fracture types with regard to treatment. In the AOSpine classification, the A3 type represents an incomplete burst fracture with involvement of the posterior wall but only one endplate, while the A4 fracture, a complete burst fracture, is characterized by an involvement of the posterior wall and both endplates.
General consensus exists that in less severe fractures (A0-A2) conservative treatment has the best risk/benefit ratio and that very severe fractures (B and C type) as well as patients with neurological compromise should be treated surgically. However, no such consensus exists in patients with incomplete (A3) and complete (A4) thoracolumbar burst fractures without neurological deficit.23,24
The most recent comprehensive systematic review with the aim of determining whether surgical or nonsurgical treatment achieves better results in these fracture types has been performed nearly 10 years ago.19
Therefore, the purpose of our review was to generate the best available evidence on the clinical outcomes achieved with current operative and nonoperative treatment modalities in A3 and A4 fractures in neurologically intact patients by performing a meta-analysis.
Materials and Methods
Search Strategy
A literature search was performed in PubMed and the Web of Science on April 7, 2015. Since the terminology used to describe thoracolumbar fractures is extremely varied, the search strings were deliberately kept general to avert the risk of missing eligible publications. The search strategy is depicted in Table 1.
Table 1.
Search Strategy.
| PubMed and Web of Science search; Filters: Publication date from 2000/01/01 to 2015/12/31; English | |
| #1 | lumbar OR thoracic OR thoracolumbar |
| #2 | burst fracture OR spinal fracture OR burst |
| #3 | spine |
| #4 | osteoporotic OR geriatric OR vertebroplasty OR kyphoplasty OR “vertebral body stenting” OR cervical OR unstable OR degenerative OR gunshot OR bisphosphonate OR alendronate OR osteoporosis OR lupus OR ankylosing spondylitis OR case report OR rat OR dog OR rabbit OR sheep OR pig OR experimental OR model |
| #5 | #1 AND #2 AND #3 |
| #6 | #5 NOT #4 |
Study Selection
In order to obtain results with a high reproducibility, the minimum population size per treatment group was set at 20 patients and only A3 and A4 fractures according to the present AOSpine classification, published by Vaccaro et al21 and Reinhold et al22 in 2013, were considered. Of note, the definition of A3 fractures according to Vaccaro et al21 and Reinhold et al22 is identical to the one of A3.1 fractures and the definition of A4 fractures according to Vaccaro et al21 and Reinhold et al22 is identical to A3.2 and A 3.3. fractures according to the previous AOSpine classification, published by Magerl et al25 in 1994, which got substituted with the present classification in 2013.
Titles and abstracts of the initial matches were independently screened by 2 reviewers to identify potentially eligible primary studies. In cases where the title or abstract did not allow determining eligibility, the full text was obtained in order to make a valid decision. In case of discrepancies, consensus was sought through discussion and in case of doubt, a third reviewer was consulted. Inclusion and exclusion criteria are presented in detail in Table 2. Additionally, the references of reviews and meta-analyses identified in this search were screened for further potentially eligible primary studies.
Table 2.
Inclusion and Exclusion Criteria.
| Inclusion criteria |
|---|
| A3 and A4 thoracolumbar fractures (T10-L3) (AO spine injury classification21,22) or, in the case of a mixed study population, with stratified analysis presenting results of patients with A3 and A4 fractures alone |
| Skeletally mature patients |
| Neurologically intact patients or, in the case of a mixed study population, with stratified analysis presenting results of neurologically intact patients alone |
| Intervention group size: ≥20 analyzed patients |
|
Any type of conservative treatment OR Any type of surgical treatment except
|
| Minimum mean follow-up time of 12 months |
| Publication date from 2000 onward |
| Exclusion criteria |
| Fractures other than A3 and A4 according to the AO spine injury classification21,22 |
|
Fractures caused by
|
Data Extraction
Information collected included inclusion and exclusion criteria of the respective study, demographic and injury characteristics, treatment details, outcomes concerning clinical, radiological and perioperative parameters, return to activity, adverse events, reoperations, follow-up (FU) time, and the proportion of patients lost to FU. This was completed via a standardized data extraction form.
Whenever comparative studies presented results of several groups and not all groups conformed to the minimum group size of 20 patients, only the group that contained a minimum of 20 patients was included in this analysis.
In case of missing information concerning parameters of interest, for example, outcome mean values at last FU or standard deviations, authors of the respective publications were contacted by email with the request to provide the missing information.
Data Synthesis
With regard to all measured indices of (a) disability and (b) pain, the pooled estimate of standardized mean difference (SMD) and 95% confidence intervals (CIs) were calculated by combining the SMD of each individual study that compared operative and nonoperative outcomes based on the mean, standard deviation, and sample size. SMD for disability was calculated based on the Roland Morris Disability Questionnaire (RMDQ)26 and the Low Back Outcome Score (LBOS),27 while pain was calculated based on pain visual analog scale (pain VAS) results. Missing values for standard deviation were imputed based on values from other studies in the analysis. Heterogeneity among studies was estimated by chi-square test and Cochran Q score (reported as I 2). An I 2 of 0% denotes no heterogeneity while an I 2 of 100% denotes maximum heterogeneity. The statistical significance level for heterogeneity was set at P < .05. In the presence of high heterogeneity, the random effects model was used. An SMD < 0 favored operative treatment when compared with nonoperative treatment. Publication bias was assessed by Egger’s regression and visual inspection of the funnel plots. The results of the meta-analyses were graphically presented as forest plots. The analysis was performed in the statistical software STATA version 13 (STATA Corp, College Station, TX, USA).
The mean values of clinical outcome parameters that were available for a minimum of 125 patients in both surgical and conservative treatment groups were depicted graphically to give an overview about results that also include the noncomparative studies.
Assessment of Methodological Quality
The quality of all studies was evaluated using a quality assessment tool previously used in similar publications.19 This tool is based on guidelines suggested by the Cochrane Collaboration Back Review Group28 and the University of British Columbia Department of Epidemiology “Evaluating Therapeutic Interventions” criteria. It contains 13 questions, which can be scored with “yes,” “no,” “unsure,” or “not applicable.” In prospective studies, 0 to 7 check marks denote a study of poor quality and 8 to 13 check marks indicate a study of good quality. In retrospective studies, 0 to 5 check marks denote a study of poor quality and 6 to 10 check marks indicate a study of good quality. A list of the respective items is given in Table 3.
Table 3.
Questions for Quality Rating According to Thomas et al (2006).19
| Is there a clear statement of purpose? |
| Was the study design randomized controlled trial (RCT) or prospective cohort? |
| Was the assessor blinded? |
| Is the population from which sample comes clearly described? |
| Is a burst fracture defined and the method of diagnosis stated? |
| Did authors account for every patient that was eligible but did not enter? (Question not applicable in retrospective studies) |
| Is the treatment clearly defined and replicable? |
| Were all patients accounted for (<25% lost to follow-up)? (Question not applicable in retrospective studies) |
| Were outcome measures relevant to the primary question? |
| Was statistical significance considered? |
| Were tests applied appropriately? |
| Was sample size calculated prior to study? (Question not applicable in retrospective studies) |
| Were the results/conclusions clinically significant? |
Risk of bias of studies directly comparing conservative to surgical treatment was evaluated with the Newcastle-Ottawa Quality Assessment Scale (NOS).29 This methodological rating scale was originally developed to rate the risk of bias in nonrandomized comparative studies. It rates the methodological quality of the 3 domains “selection,” “comparability,” and “outcome.” The maximum attainable ratings are 4 stars for selection, 2 stars for comparability, and 3 stars for outcome. Rather than defining absolute values denoting the methodological quality level, the authors advise to present the ratings as a visual comparison combined with the target outcomes of each study included in a review. This allows readers to make their own decision on the validity of respective outcomes.29
Ethical Aspects
No institutional review board approval is needed for systematic literature reviews and meta-analyses.
Results
Eligible Literature
The searches in PubMed and the Web of Science resulted in a total of 1929 matches (Figure 1).
Figure 1.

Study inclusion flow diagram.
After screening of titles and abstracts by two independent reviewers, 142 primary studies were considered potentially relevant. After full text assessment, 11 articles were deemed eligible.14,15,30–38 Additionally, 26 reviews and meta-analyses were screened for further potentially eligible references, which led to the identification of another primary study.39
Overall, 4 studies directly compared surgical with conservative treatment.14,15,33,35
One of them was an RCT.15 Six additional comparative studies had a different focus, and 3 studies compared different types of surgical treatment.34,37,38 Another 2 studies compared the outcome of patients with different degrees of injury severity,31,36 and 1 study, designed as an RCT, compared 2 types of conservative treatment.30
Finally, 2 case series were identified. One presented results of surgical treatment39 and the other analyzed results of patients treated nonoperatively.32
A total of 656 patients were included within these studies. No overlapping patient populations were identified. Overall, studies presented a high heterogeneity with regard to inclusion and exclusion criteria and the level of detail reported, particularly in the parameters used to evaluate treatment success. A summary of study characteristics for baseline data is given in Table 4 and for clinical outcome data in Table 5 and for radiological outcome data in Table 6.
Table 4.
Study Characteristics—Baseline.
| Author (Year) Study Design LoE | Inclusion and Exclusion Criteria | Treatment | Demographic Characteristics | Injury Characteristics (Grade, Level) |
|---|---|---|---|---|
| Wood (2003) RCT II | Inclusion criteria: Isolated burst fracture within the thoracolumbar region (T10 to L2) demonstrated on anteroposterior and lateral radiographs Computed tomography scan revealing a burst-type fracture with retropulsion of vertebral body bone posteriorly into the spinal canal No new neurological abnormality of the lower extremities or abnormality of bowel or bladder function Presentation less than 3 wk after the time of the injury An age between 18 and 66 years No medical illnesses that would preclude an operative intervention No ongoing cancer, infection, bleeding disorder, or skin disease An understanding of the English language. Concomitant stable compression fractures elsewhere in the spine were permitted if they did not require specific treatment. Exclusion criteria: Closed-head injury (a score of <14 points on the Glasgow coma scale on admission) Open vertebral fracture Neurological deficit related to the fracture Loss of structural Integrity within the posterior osteoligamentous complex (such as facet fracture, dislocation or flexion-distraction ligament disruption) Senile, osteopenic, or insufficiency fracture. A laminar fracture was neither an exclusionary criterion nor a contraindication for nonoperative treatment No absolute degree of kyphosis, canal encroachment by bone, or anterior loss of height was a criterion for exclusion | Operative: Short-segment (2- to 5-level) posterolateral spinal arthrodesis with pedicle screw-hook instrumentation and ICBG or Anterior 2-level fibular and rib-strut construct arthrodesis with local autogenous bone-grafting and instrumentation. | Operative: Mean age: 43.3 y Male: 16 (66.7%) Female: 8 (33.3%) | Operative: T11: 1 (4.2%) T12: 4 (16.7%) L1: 13 (54.2%) L2: 6 (25.0%) |
| Nonoperative: Body cast with manual kyphosis reduction through anterior force, worn for 8-12 wk, followed by thoracolumbosacral orthosis for 8 wk or Thoracolumbosacral orthosis with the spine in hyperextension to reduce the kyphosis and subsequent molded plaster cast that was then converted to an encompassing plastic jacket, worn for 24 h/d except for showering for 12-16 wk | Nonoperative: Mean age: 39.4 y Male: 16 (69.6%) Female: 7 (30.4%) | Nonoperative: T12: 4 (17.4%) L1: 15 (65.2%) L2: 4 (17.4%) | ||
| Landi (2014) Retrospective cohort III | Inclusion criteria: Magerl type A.3, involving only one level McCormack score 6 or less Spinal canal invasion 25% or less acc. to Hashimoto Disco-ligamentous integrity confirmed on MRI Neurologically intact (ASIA E) | Operative: Percutaneous short stabilization: One level above and one below | ND | A3.1:10 (40%) A3.2: 5 (20%) A3.3: 10 (40%) |
| Nonoperative: Rigid brace for 2 mo followed by semirigid brace for another 2 mo | ND | A3.1:12 (48%) A3.2: 7 (28%) A3.3: 6 (24%) | ||
| Post (2009) Retrospective cohort III | Inclusion criteria: Age 18-60 years at the time of injury A3 thoracolumbar (T7-L5) spinal fracture according to the Comprehensive Classification as diagnosed on radiographs and CT scans Without neurological deficit Treated at the University Medical Centre Groningen Exclusion criteria: Previous spinal disorders in the medical history Psychiatric illnesses Pathological fractures Insufficient command of the Dutch language. | Operative: Short fixation (for A3 fractures: called MSPI by other authors) involving 1 or two segments (depending on fx type, ie, with 2 damaged endplates: 2 segmental fixation; with 1 damaged endplate: 1-segmental fixation) | Operative: Mean age: 37.2 ± 11.8 y (18-56 y) Male: 26 (68%) Female: 12 (32%) | Operative: A3.1 15 (40%) A3.2 18 (47%) A3.3 5 (13%) Levels: T9-L5 Of these: T12/L1: 74% Multiple fractures: 5 patients* |
| Nonoperative: Bed rest (or rest on a Stryker frame) for 6 wk, followed by a reclination brace and mobilization. Weightbearing exercises after 3 months. Brace worn for 9 mo (24 h/d in first 6 months, only during the day in last 3 months). | Nonoperative: Mean age: 37.4 ± 12.2 y (19-58 y) Male: 15 (60%) Female: 10 (40%)” | Non-operative: A3.1 22 (88%) A3.2 3 (12%) A3.3 0 Levels: T7-L5 of these: T12/L1: 60% multiple fractures: 4 patients* | ||
| Difference in fx distribution (A3.2 and A3.3 vs A 3.1) ss: P < .01 | *Most severe registered, further fx not taken into account | |||
| Shen (2001) Prospective cohort III | Inclusion criteria: Neurologically intact with normal anal tone and no motor deficits, radiculopathy, or lower extremity spasms Single-level closed burst fracture involving T11, T12, L1, or L2 No dislocations, with pedicles and facet joints appearing intact, although the pedicles may have fractured from the vertebral body Nonosteopenic, nonpathologic adult 18 to 65 y of age No other major organ system or musculoskeletal injuries. Other radiographic parameters such as posterior column involvement, kyphosis angle, and degree of canal compromise were not used as inclusion or exclusion criteria. | Operative: Three-level fixation: Pedicle screws in the level above, in the fractured vertebrae, and in the level below the fractured vertebrae (3 levels, 6 screws). | Operative: Mean age: 42 y (20-64 y) Male: 18 (54.5%) Female: 15 (45.5%) | Operative: T11: 0 (0%) T12: 10 (30.5%) L1: 14 (42%) L2: 9 (27.5%) |
| Nonoperative: Bed rest with activity allowed (including ambulation) as tolerated by pain with hyperextension brace fitted in slight hyperextension with the patient standing. Brace worn 24 h/d (except when bathing) for 3 months (according to instructions, but no monitoring of compliance undertaken) | Nonoperative: Mean age: 44 y (19-64 y) Male: 23 (49%) Female: 24 (51%) | Nonoperative: T11: 1 (2%) T12: 11 (23%) L1: 23 (49%) L2: 12 (26%) | ||
| Wei (2010) RCT Ib | Inclusion criteria: Single-level closed burst fractures AO-ASIF type A3.1 and A3.2 involving T11–L2 No neurologic impairment Age 20-60 y Nonpathologic adult. Both pedicles intact without any cortical wall defect At least one of the endplate is intact or close to intact. Sagittal index (SI) > 15° or loss of anterior body height >50% Exclusion criteria: Other associated injuries, such as skull and brain injury, cervical whiplash injury, and fracture of the calcaneous, forearm, costal arches, and so on Poor bone mineral density (≤2.5 SD) Unfavorable body mass index (≥35 kg/m2) Multilevel involvement (>2 segments) | MSPI (mono-segmental pedicle instrumentation): Screws inserted into the vertebrae adjacent to the injured endplate (if the broken endplate was the superior and the adjacent vertebra was the upper, or if the broken endplate was the inferior and the adjacent vertebra was the lower). | MSPI Mean age: 39.3 ±14 y Male: 30 (71.5%) Female: 12 (28.5%) | MSPI: A3.1: 25 A3.2: 22 pts Levels: T11: 5 (10.7%) T12: 8 (17.0%) L1: 18 (38.30%) L2: 16 (34.0%) |
| SSPI (short-segment pedicle instrumentation): Pedicle screws in one level above and one level below the injured vertebra. | SSPI Mean age: 42.0±13 y Male: 33 (76.8%) Female: 10 (23.2%) | SSPI: A3.1: 21 pts A3.2: 17 pts Levels: T11: 6 (12.5%) T12: 7 (14.5%) L1: 21 (44.0%) L2: 14 (29.0%) | ||
| In total: Mean age: 40.5 ±11.7 y (Range, 20-60 y) Male 63 (74%) Female 22 (26%) | In total: T11 + T12: 16 (19%) L1: 39 (46%) L2: 30 (35%) | |||
| Li (2012) Retrospective cohort III | Inclusion criteria: Thoracolumbar burst fracture examined through 3-dimensional CT to investigate pedicle and vertebral displacement. Intact pedicles Only in MSPI group: unilateral end-plate injury] Exclusion criteria: Oversized bone in the spinal canal Neurological deficit | MSPI (monosegmental pedicle instrumentation): Screws inserted into the vertebrae adjacent to the injured endplate (if the broken endplate was the superior and the adjacent vertebra was the upper, or if the broken endplate was the inferior and the adjacent vertebra was the lower). | MSPI: Mean age: 41.3 y (29-54 y) Male: 18 (60%) Female: 12 (40%) | MSPI: A3.1: 28 (93.5%) A3.2: 2 (6.5%) Levels: T11: 4 (13%) T12: 6 (20%) L1: 13 (43%) L2: 6 (20%) L3: 1 (3.3%) |
| SSPI (short-segment pedicle instrumentation) Pedicle screws in one level above and one level below the injured vertebra | SSPI: Mean age: 40.2 y (30-53 y) Male: 18 (60%) Female: 12 (40%) | SSPI: A3.1: 28 (93.5%) A3.2: 2 (6.5%) Levels: T11: 6 (20%) T12: 9 (30%) L1: 9 (30%) L2: 5 (16.7%) L3: 1 (3.3%) | ||
| Bailey (2014) RCT Ib | Inclusion criteria: Isolated AO-A3 burst fracture (vertebral body compression with retropulsion of the posterior vertebral body into the canal and excludes posterior element injury) between T10 and L3 Kyphotic deformity lower than 35° Neurologically intact 16 to 60 y of age Recruited within 3 days of injury Exclusion criteria: Patients who could not wear a brace (ie, pregnancy/body mass index >40 kg/m2) Mobilized with or without a brace before recruitment Suffered a pathologic or open fracture Alcohol or drug abusers Previous injury or surgery to the thoracolumbar region Unable to complete the outcome questionnaires | No orthosis (NO): Immediate mobilization as tolerated with restrictions to limit bending and rotating through the trunk. Return to normal activities encouraged after 8 weeks. | NO: Mean age: 39.8±15.3 y Male: 69.4% Female: 30.6% | NO: AO: A3 Levels: T11: 2 (4.1%) T12: 9 (18.4%) L1: 29 (59.2%) L2: 3 (6.1%) L3: 6 (12.2%) |
| Early mobilization with “off-the-shelf” adjustable thoracolumbosacral orthosis (TLSO): Strict bed rest until fitted with a TLSO and mobilization in the brace. The TLSO worn at all times except when lying flat in bed for a total of 10 wk with start of weaning from the brace at 8 weeks | TLSO: Mean age: 40.5±14.8 y Male: 70.2% Female: 29.8% | TLSO: AO: A3 Levels: T11: 2 (4.3%) T12: 9 (19.1%) L1: 21 (44.7%) L2: 12 (25.5%) L3: 3 (6.4%) | ||
| Proietti (2014) Retrospective cohort III | Inclusion criteria: Single-level A3 fracture between T11 and L5 Age 18-65 y No neurological involvement Exclusion criteria: Pathological or osteoporotic fracture Multilevel fracture Previous surgery at site of fracture | All patients (groups A + B): Short stabilization: One level above and one below | Total (groups A + B): Mean age: 51.2 y (20–65 y) Male: 38 (63.5%) Female: 22 (36.5%) | Total (groups A + B): Magerl classification A 3.1= 28 (47%) A 3.2= 8 (13%) A 3.3= 24 (40%) Levels: T11: 5 (8.3%) T12:17 (28.3%) L1: 17 (28.3%) L2: 8 (13.5%) L3: 9 (15%) L4: 3 (5%) L5: 1 (1.6%) |
| Group A, n = 39: SI value >10° ≤15° | ||||
| Group B, n = 21 SI > 15° | ||||
| Schmid (2011) Prospective cohort III | Inclusion criteria: Burst fractures (type A3 according to Magerl) of the thoracolumbar junction (T12-L2) No neurological deficits (Frankel/ASIA E) Age <60 y Exclusion criteria: Fractures above T12 or below L2 Fractures with intact posterior wall (A1 and A2 acc. to Magerl) Neurological deficits (Frankel/ASIA A–D) Pathological or osteoporotic fractures Incomplete radiological or clinical follow-up Nonresident patients | Short segmental posterior fixation with angular stable pedicle screw systems Plus posterolateral fusion Plus unilateral TLIF with monocortical strut grafts and cancellous bone (ICBG) Implant removal at a mean of 15.1 ± 3.7 months The analysis was performed separately for 2 patient groups, but only group B (“TLIF group”) was large enough to be eligible for this review, group A is not considered here | Mean age: 32.7±11.3 y Male: 16 (76%) Female: 5 (24%) | Magerl A3 T12: 7 (33.5%) L1: 11 (52.5%) L2: 3 (14.0%) |
| Jeong (2013) retrospective cohort III | Inclusion criteria: Thoracic and lumbar burst fractures A fractured posterior vertebral surface dislocated into the spinal canal No neurological deficit A minimum of 1-year follow-up Indirect decompression using the ligamentotaxis technique Short-segment implants (1 level above and 1 level below the fracture) Exclusion criteria: Complete tear of the PLL as seen on MRI Any neurolgical deficit. | Pedicle screws 1 level above and 1 level below the fracture level The analysis was performed separately for 2 patient groups, but only one group (“high grade fracture group”) was large enough to be eligible for this review, so the other group is not considered here | Mean age: 38.8 y (16-61 y) Male: 15 (65%) Female: 8 (35%) | McCormack ≥7 27 levels in 23 pts |
| Koller (2008) Retrospective case series IV | Inclusion criteria: Single-level thoracolumbar (T11–L2) or lumbar (L3–5) compression or burst fracture Absence of neurological injury (Frankel A-D) Age 18-60 y at injury Understanding of the author’s language ≤10 days between injury and index treatment Full set of injury lateral and anteroposterior radiographs; CTscans were not necessary for inclusion Exclusion criteria: Medical illness that precluded operative treatment Prior thoracic, lumbar, abdominal or genitourinary surgery Major organ system or musculoskeletal injuries Spinal disorders in the patient’s medical history requiring a specific medical treatment Chronic drug and alcohol abuse Concomitant serious head, thoracic, or abdominal injuries Proven evidence of osteoporosis Serious mental disorders leading to medical intervention Pregnancy End-stage medical diseases Lower extremity injuries affecting gait or limb length Failure to comply in wearing the brace Worker’s compensation claims Preexisting spinal deformity | Manual kyphosis reduction through anterior force, then 3 mo of brace (24 h/d) | Mean age: 49.1 ± 15.7 y Male: 15 (71.5%) Female: 6 (28.5%) | A3.1: 52.4% (n = 11) - A3.1.1: 9 - A3.1.2: 2 A3.2: 38.1% (n = 8) - A3.2.1: 7 - A3.2.2: 1 A3.3: 9.5% (n = 2) - A3.3.1: 1 - A3.3.3: 1 Levels: T12: 5 (23.8%) L1: 9 (42.9%) L2: 2 (9.5%) L3: 2 (9.5%) L4: 3 (14.3%) |
| Andress (2002) Retrospective case series IV | Inclusion criteria: Burst-compression fracture at the thoraco-lumbar spine (T11–L2) which involved the middle column but left the posterior column intact (type A 3 according to Magerl) No neurological deficit No pathologic fracture Exclusive dorsal stabilization with the AO internal fixator (Synthes Cooperation, Bochum, Germany) in combination with or without transpedicular bone grafting Single level injury Complete documentation of the case including a pre-operative spinal CT Conventional biplanar X-rays of the thoracolumbar spine pre- and postoperatively, at the time of implant removal and at follow-up Minimal time period between surgery and follow-up examination: 36 mo Implant removal 9-15 mo after surgery. Exclusion criteria: Neurological deficit Injuries at the dorsal column Rotation injuries | Internal fixator either with or without transpedicular spongiosa grafting with fixed-angle pedicle screw instrumentation and pedicle screws above and below the fractured vertebral body In cases where the kyphotic angle was large or where the fractured vertebral body was completely destroyed: transpedicular inter- and intracorporal autologous bone grafting after transpedicular discectomy Transpedicular spongiosa grafting: 29 pts (58%) No grafting: 21 pts (42%) | Mean age: 46.2 y (22-77 y) Male: 27 (54%) Female: 21 (46%) | Magerl A3: A3.1: 19 (38%) A3.2: 17 (34%) A3.3: 14 (28%) Levels: L1: 27 (54%) L2: 12 (24%) Th12: 11 (22%) |
Abbreviations: LoE, level of evidence; CT, computed tomography; RCT, randomized controlled trial; ICBG, iliac crest bone graft; SI, sagittal index; pts, patients.
Table 5.
Study Characteristics—Clinical Outcome.
| Author (Year) Study design LoE | Treatment | FU (SD and Range) n/N (% FU) | Clinical Outcomes at Follow-up Mean ± SD; Median (Range) [As Available] | Perioperative Outcomes and Return to Activity | Adverse Events (Complications/Reoperations) |
|---|---|---|---|---|---|
| Wood (2003) RCT II | Operative: Short-segment (2- to 5-level) posterolateral spinal arthrodesis with pedicle screw-hook instrumentation and ICBG or Anterior 2-level fibular and rib-strut construct arthrodesis with local autogenous bone-grafting and instrumentation. | Operative: 42.9 mo (SD: 14.8, range 24-72 mo) 24/26 (92%) | Operative: VAS (0-10): 3.3 (0-7.5) ODI: 20.75 (0-48) RMDQ: 8.16 (0-19) SF-36: Pain 59 Health Perception 69 Physical Function 63 Social Function 84 Role; Physical 51 Role; Emotional 80 Mental Health 81 Energy/Fatigue 84 | Operative: Time to return to regular work: 10 (42%) at 6 mo Plus 4 (17%) between 6 and 24 mo | Operative: 19 complications in 16 patients: Wound dehiscence (2) Instrumentation/bone failure (2) Wound infection (deep) (1) Pseudarthrosis (1) Neurapraxia (1) Ketoacidosis (1) Instrumentation break (2) Urinary tract infection (2) Seroma (1) Instrumentation removal (6) Impairments of neurological function (0) |
| Nonoperative: Body cast with manual kyphosis reduction through anterior force, worn for 8-12 wk, followed by thoracolumbosacral orthosis for 8 weeks or Thoracolumbosacral orthosis with the spine in hyperextension to reduce the kyphosis and subsequent molded plaster cast that was then converted to an encompassing plastic jacket, worn for 24 h/d except for showering for 1216 wk | Nonoperative: 45.8 mo (SD: 21.9, range 24-118 mo) 23/27 (85%) | Nonoperative: VAS (0-10): 1.9 (0-9) ODI: 10.7 (0-52) RMDQ: 3.9 (0-24) SF-36: Pain 72 Health Perception 72 Physical Function 86 Social Function 83 Role; Physical 85 Role; Emotional 79 Mental Health 75 Energy/Fatigue 56 | Nonoperative: Time to return to regular work: 17 (74%) at 6 mo Plus 2 (9%) at 24 mo | Nonoperative: 2 complications in 2 patients: Urinary tract infection (1) Skin blisters (1) | |
| Landi (2014) Retrospective cohort III | Operative: Percutaneous short stabilization: one level above and one below | Operative: 12 mo ND 25/25 (100%) | Operative: RMDQ: 1.4 (0-4) ODI: 14% (4-36%) VAS (0-10): 0 Patient satisfaction/quality of life (1-10): 9.4 | Operative: Blood loss: 10 cm3 OR time: 80 min Time for back to work: 29 days Time to normal activity: 31 days | ND |
| Nonoperative: Rigid brace for 2 mo followed by semirigid brace for another 2 mo | Nonoperative: 12 mo ND 25/25 (100%) | Nonoperative: RMDQ: 3.4 (0-7) ODI: 22% (5%-40%) VAS (0-10): 1.5 patient satisfaction/quality of life (1-10): 8 | Nonoperative: Time for back to work: 117 days Time to normal activity: 87.1 days | ND | |
| Post (2009) Retrospective cohort III | Short fixation (for A3 fractures: called MSPI by other authors) involving 1 or 2 segments (depending on fx type, ie, with 2 damaged endplates: 2 segmental fixation; with 1 damaged endplate: 1-segmental fixation) | Operative: 5. 7y (SD: 2.9, range 2.5-10.6 y) 38/46 (83%) | Operative: RMDQ: 3.3 ± 5.1; 0 (0-17) VAS Spine Score: 82.6 ± 21.9; 94.1 (17-100) | Operative: ND | No further surgery for late onset pain or late onset neurological deficit |
| Bed rest (or rest on a Stryker frame) for 6 weeks, followed by a reclination brace and mobilization. Weightbearing exercises after 3 mo. Brace worn for 9 months (24 h/d in first 6 mo, only during the day in last 3 mo). | Nonoperative: 4.8 y (SD: 2.9, range 2.1-10.4 y) 25/30 (83%) | Nonoperative: RMDQ: 3.1 ± 3.7; 1.0 (0-12) VAS Spine Score: 80.8 ± 19.4; 84.0 (31-100) | Nonoperative: ND | No further surgery for late onset pain or late onset neurological deficit | |
| Shen (2001) Prospective cohort III | Operative: Three-level fixation: Pedicle screws in the level above, in the fractured vertebrae, and in the level below the fractured vertebrae (3 levels, 6 screws). | Operative: 24 mo ND 33/33 (100%) | Operative: VAS (0-10): 1.8±1.3 LBOS: 61±11 Patient satisfaction (1-4) (1 = highest level of satisfaction): 10:18:3:2 | Operative: Blood loss: 350 mL (150-800 mL) Operation time: 142 min (110-180 min) Hospital stay: 10.4 days | Operative: Neurologic deficit, thromboembolism, or decubitus ulcers (0) Superficial infection (1) Broken screws: 3 screws in 2 pts Hardware removal (5): Of these: -prominence and aching pain (3) -hardware breakage (2) Donor site pain (3) |
| Nonoperative: Bed rest with activity allowed (including ambulation) as tolerated by pain with hyperextension brace fitted in slight hyperextension with the patient standing. Brace worn 24 h/d (except when bathing) for 3 months. (according to instructions, but no monitoring of compliance undertaken) | Nonoperative: 24 mo ND 47/50 (94%) | Nonoperative: VAS (0-10): 1.5 ± 1.3 LBOS: 65 ± 10 Patient satisfaction (1-4) (1 = highest level of satisfaction): 18:23:6:0 | Nonoperative: Hospital stay: 9.2 days | Nonoperative: Neurologic deficit, thromboembolism, or decubitus ulcers (0) Late surgery (0) | |
| Wei (2010) RCT Ib | MSPI (monosegmental pedicle instrumentation): Screws inserted into the vertebrae adjacent to the injured endplate (if the broken endplate was the superior and the adjacent vertebra was the upper, or if the broken endplate was the inferior and the adjacent vertebra was the lower). | MSPI: ND (only complete population) No. of pts: ND, assume 47/47 (100%) | MSPI: LBOS: 74.9 ± 8.7 ODI: 34.1 ± 9.7 | MSPI: Blood loss: 157 ± 49 mL (92-275 mL), OR time: 87 ± 24 min (61-123 min) | MSPI: Correction loss of 10°, including 1 screw loosening (3) Screw dislodgement requiring reoperation (1) |
| SSPI (short-segment pedicle instrumentation): Pedicle screws in one level above and one level below the injured vertebra. | SSPI: ND (only complete population) No. of pts: ND, Assume 38/38 (100%) | SSPI: LBOS: 60.2 ± 9.6 ODI: 37.6 ± 11.5 | SSPI: Blood loss: 460 ± 134 mL (240-810 mL). OR time: 138 ± 29 min (93-170 min). | SSPI: Correction loss of 10°, including 1 screw breakage* (2) Screw breakage after trauma not requiring reoperation* (1) *Possibly same patient, wording unclear | |
| Complete population: 27.8 mo (SD: 7.0, range 19-52 mo) ND, assume 95/95 (100%) | Neurological deteriorations after surgery (0) Urinary infection (4) Superficial infection (1) | ||||
| Li (2012) Retrospective cohort III | MSPI (monosegmental pedicle instrumentation): Screws inserted into the vertebrae adjacent to the injured endplate (if the broken endplate was the superior and the adjacent vertebra was the upper, or if the broken endplate was the inferior and the adjacent vertebra was the lower). | MSPI: 13.2 mo (range: 12-26 mo) NA (30/30, retrospective, only pts w/ FU) | MSPI: VAS: 1.4 ± 0.8 | MSPI: Blood loss: 180 ± 62 mL OR time: 90 ± 25 min | MSPI: Wound seroma (1) |
| SSPI (short-segment pedicle instrumentation): Pedicle screws in one level above and one level below the injured vertebra. | SSPI: 34.6 mo (range 12-64 mo) NA (30/30, retrospective, only pts w/ FU) | SSPI VAS: 1.1 ± 0.6 | SSPI: Blood loss: 203 ± 88 mL. OR time: 101 ± 28 min | SSPI: Screw removal due to breakage (1) Adjacent segment degeneration (1) | |
| Bailey (2014) RCT Ib | No orthosis (NO): Immediate mobilization as tolerated with restrictions to limit bending and rotating through the trunk. Return to normal activities encouraged after 8 wk. | NO: 24 mo: ND 36/49 (73%) 12 mo: 40/49 (82%) | NO at 24 mo: RMDQ: 4.44 ± 5.53(0-23) VAS: 2.03 ± 2.04 (0-7) NO at 12 mo: RMDQ: 5.33 ± 5.81 (0-17) VAS: 2.22 ± 1.89 (0-7) figures by personal communication | NO: Hospital stay (mean ± SD) 2.6 ± 2.7 days | NO: Surgical interventions (2) (A) Surgery before initial hospital discharge: - due to severe radicular pain not present when supine (1) - due to severe mechanical back pain necessitating surgical stabilization (1) |
| Early mobilization with “off-the-shelf” adjustable thoracolumbosacral orthosis (TLSO): Strict bed rest until fitted with a TLSO and mobilization in the brace. The TLSO worn at all times except when lying flat in bed for a total of 10 wk with start of weaning from the brace at 8 wk. | TLSO: 24 mo: ND 32/47 (68%) 12 mo: ND 41/47 (87%) | TLSO at 24 mo: RMDQ: 3.03 ± 4.8 (0-24) VAS: 1.58 ± 1.87 (0-8) TLSO at 12 mo: RMDQ: 3.2 ± 4.65 (0-14) VAS: 1.58 ± 1.87 (0-8) figures by personal communication | TLSO: Hospital stay (mean ± SD) 2.5 ± 2.9 days | TLSO: Surgical interventions (4) (A) Surgery before initial hospital discharge: - due to severe radicular pain not present when supine (1) - due to severe mechanical back pain necessitating surgical stabilization (2) (B) Surgery after initial hospital discharge: - osteotomy 8 months after fracture (1) | |
| Proietti (2014) Retrospective cohort III | All patients (group A* + group B**): Short stabilization: one level above and one below *Group A: SI > 10° ≤ 15° **Group B: SI > 15° | Total population (group A + group B) Minimum 12 mo (range12-48 mo) 60/63 (95%) | Group A: VAS: 1.8 (range 0.5-2.5) ODI: 12% (range 5%-17%) SF36 PCS: 83.2% (range 67.5%-95.4%) SF36 MCS: 79.9% (range 63.2%-83.5%) | Total population (group A + group B) Blood loss: 82 mL (50-96 mL) OR time: 67 min (50-96 min) Hospital stay: 4.9 days (3-7 days) | Total population (group A + group B) Superficial dehiscence at 6 wk: (1) Implant removal due to deep infection at 1 mo (1) Hardware failure at 5 years (1) |
| Group B: VAS: 4.25 (range 1.4-6.2) ODI: 38% (range 17%-45%) SF36 PCS: 73.5% (range 57.6%-85.3%) SF36 MCS: 68.8% (range 53.2%-75.6%) | |||||
| Schmid (2011) Prospective cohort III | Short segmental posterior fixation with angular stable pedicle screw systems Plus posterolateral fusion Plus unilateral TLIF with monocortical strut grafts and cancellous bone (ICBG) implant removal at a mean of 15.1 ± 3.7 mo Analysis performed separately for two patient groups, but only one (“TLIF group”) was large enough to be eligible for this review, so the other group is not mentioned here | 20.2 mo (SD: 6.1 mo) 21/21 (100%) | RMDQ: 4.4 ± 4.4 ODI: 14.4 ± 12.4 FFbH-R: 82.3 ± 19.3 VAS score: 73.0 ± 21.3 MPQ: 13.9 ± 18.4 | Mean surgery time: 176 ± 72 min Mean blood loss: 1000 ± 1280 mL Length of hospital stay: 11.8 ± 5.2 days Duration of work incapacity: 4.9 ± 5.1 mo | Posterior approach–related complaints No complaints (15) Mild complaints (5) Severe complaints (1) Anterior approach related complaints No complaints (21) Mild complaints (0) Severe complaints (0) Donor-site related complaints No complaints (15) Mild complaints (4) Severe complaints (2) |
| Jeong (2013) Retrospective cohort III | Pedicle screws 1 level above and 1 level below the fracture level | 27.6 mo (range 12-66 mo) NA (23/23, retrospective, only pts w/ FU) | VAS: 4.6 (3-6) ODI: 19.6 (6-27) | ND | Metal failure* (4) Posttraumatic kyphosis (5) Adjacent spine disease (6) *Pedicle screw pull-out or breakage |
| Koller (2008) Retrospective case series IV | Manual kyphosis reduction through anterior force, then 3 months of brace (24 h/d) | 112.8 mo (SD:47 mo) NA (21/21, retrospective, only pts w/ FU) | Mean ± SD RMDQ: 3.2 ± 5.0 LBOS: 49.5 ± 17.6 VAS Spine Score: 74 ± 15 SF-36 PCS: 47.1 ± 9.3 SF-36 MCS:49.4 ± 10.3 Median (25%-75% quartile) RMDQ: 1 (0-3) LBOS: 54 (41-62) VAS Spine Score: 75 (64-84) SF-36 PCS: 48.3 (43.9-54.1) SF-36 MCS: 53.3 (44.7-57) | ND | Pulmonary artery embolism during immobilization in cast (1) Symptomatic lumbar posttraumatic kyphotic deformity following burst fracture of L4 (1) |
| Andress (2002) Retrospective case series IV | Internal fixator either with or without transpedicular spongiosa grafting with fixed-angle pedicle screw instrumentation and pedicle screws above and below the fractured vertebral body In cases where the kyphotic angle was large or where the fractured vertebral body was completely destroyed: transpedicular inter- and intracorporal autologous bone grafting after transpedicular discectomy transpedicular spongiosa grafting: 29 pts (58%) not grafting: 21 pts (42%) | 68 mo (range 36-103 mo) NA (50/50, retrospective, only pts w/ FU) | Activity score (1-7): 4.92 points FFbH-R: 81.7 ± 14.4 points With bone graft or without: (mean ± SD) FFbH-R for pts w/ bone graft: 82.4±14.2 FFbH-R for pts w/o bone graft: 80.7±15.1 FFbH-R stratified according to fx type (mean ± SD) A 3.1: 81.1 ± 16.4 A 3.2: 80.6 ± 15.4 A 3.3: 84.3 ± 9.5 | ND | Harvest site pain in 2/29 (6.9%) |
Abbreviations: ND, not documented; w/, with; w/o, without; pt, patient; pts: patients, NA, not applicable; fx, fracture; SI, Sagittal Index; RMDQ, Roland Morris Disability Questionnaire25; VAS (0-10), visual analogue scale for pain; VAS spine score: VAS spine score42; LBOS, Low Back Outcome Score26; ODI, Oswestry Disability Index40; FFbH-R, Hannover Spine Score43; MPQ, McGill Pain Questionnaire44; SF-36 PCS: Short Form–36 Physical Health Summary Scale41; SF-36 MCS: Short Form–36 Mental Health Summary Scale.41
Table 6.
Study Characteristics—Radiological Outcomes.
| Author (Year) Study Design LoE | Treatment | FU (SD and Range) n/N (% FU) | Radiological Outcomes at Follow-up Mean ± SD; Median (Range) [As Available] | Measurement Method to Determine Kyphosis |
|---|---|---|---|---|
| Wood (2003) RCT II | Operative: Short-segment (2- to 5-level) posterolateral spinal arthrodesis with pedicle screw-hook instrumentation and ICBG or Anterior 2-level fibular and rib-strut construct arthrodesis with local autogenous bone-grafting and instrumentation. | Operative: 42.9 mo (SD: 14.8, range 24-72 mo) 24/26 (92%) | Operative: Mean kyphosis angle at admission: 10.1° (–10° to 32°) Mean kyphosis angle at discharge: 5° (–10° to 25°) Mean kyphosis angle at last FU: 13° (–3° to 42°) | Kyphosis and loss of the anterior height of the vertebral body were calculated according to the method of Atlas et al.47 |
| Nonoperative: Body cast with manual kyphosis reduction through anterior force, worn for 8-12 wk, followed by thoracolumbosacral orthosis for 8 wks or Thoracolumbosacral orthosis with the spine in hyperextension to reduce the kyphosis and subsequent molded plaster cast that was then converted to an encompassing plastic jacket, worn for 24 h/d except for showering for 12-16 wk | Nonoperative: 45.8 mo (SD: 21.9, range 24-118 mo) 23/27 (85%) | Nonoperative Mean kyphosis angle at admission: 11.3° (–12° to 30°) Mean kyphosis angle at discharge: 8.8° (–5.5° to 22°) Mean kyphosis angle at last FU: 13.8° (–3° to 28°) | ||
| Landi (2014) Retrospective cohort III | Operative: Percutaneous short stabilization: one level above and one below | Operative: 12 mo ND 25/25 (100%) | Operative and Nonoperative: Radiological outcome determined 6 mo postoperatively: No figures given, Results “in normal range, (ie, 20°-60°) in both groups, “Minimal differences” in favor of operative group | “Sagittal kyphotic angle measurement was manually performed, directly on lateral plane X-ray images, using as reference the upper and lower edges of vertebral bodies L1–L5 and S1 upper edge.” |
| Nonoperative: Rigid brace for 2 months followed by semirigid brace for another 2 mo | Nonoperative: 12 mo ND 25/25 (100%) | |||
| Post (2009) Retrospective cohort III | Operative: Short fixation (for A3 fractures: called MSPI by other authors) involving 1 or 2 segments (depending on fx type, ie, with 2 damaged endplates: 2-segmental fixation; with 1 damaged endplate: 1-segmental fixation) | Operative: 5.7 y (SD: 2.9, range 2.5-10.6 y) 38/46 (83%) | Operative and Nonoperative: ND | NA |
| Nonoperative: Bed rest (or rest on a Stryker frame) for 6 wk, followed by a reclination brace and mobilization. Weight bearing exercises after 3 months. Brace worn for 9 mo (24 h/d in first 6 mo, only during the day in last 3 mo). | Nonoperative: 4.8 y (SD: 2.9, range 2.1-10.4 y) 25/30 (83%) | |||
| Shen (2001) Prospective cohort III | Operative: Three level fixation: pedicle screws in the level above, in the fractured vertebrae, and in the level below the fractured vertebrae (3 levels, 6 screws). | Operative: 24 mo ND 33/33 (100%) | Operative: Mean kyphosis angle at injury: 23° ± 6° (12°-33°) Mean kyphosis angle at 2 y: 12° ± 8° (21°-25°) Initial kyphosis correction: 17° ± 8° Mean initial retropulsion of midsagittal canal diameter: 32% Mean retropulsion of midsagittal canal diameter on 1 y CT: No information | Sagittal plane kyphosis was measured, as described by Knight et al,46 from the inferior endplate of the vertebral body above the fracture to the inferior endplate of the fractured body |
| Nonoperative: Bed rest with activity allowed (including ambulation) as tolerated by pain with hyperextension brace fitted in slight hyperextension with the patient standing. Brace worn 24 h/d (except when bathing) for 3 months. (According to instructions, but no monitoring of compliance undertaken) | Nonoperative: 24 mo ND 47/50 (94%) | Nonoperative: Mean kyphosis angle at injury: 21° ± 6° (11°-35°) Mean kyphosis angle at 2 y: 24° ± 7° (11°-36°) Initial kyphosis correction: None Mean initial retropulsion of midsagittal canal diameter: 34% Mean retropulsion of midsagittal canal diameter on 1 y CT: 15% | ||
| Wei (2010) RCT Ib | MSPI (monosegmental pedicle instrumentation): Screws inserted into the vertebrae adjacent to the injured endplate (if the broken endplate was the superior and the adjacent vertebra was the upper, or if the broken endplate was the inferior and the adjacent vertebra was the lower). | MSPI: ND (only complete population) No. of pts: ND, assume 47/47 (100%) | MSPI: Preop SI: 13.1° ± 5.4° Postop SI: 4.5° ± 2.7° SI at FU: 7.1° ± 4.2° Preop LSC: 6.8 ±1 LSC at FU: 2.9 ±1.1 | Sagittal index determined on plain radiographs according to Farcy et al52 |
| SSPI (short-segment pedicle instrumentation): Pedicle screws in one level above and one level below the injured vertebra. | SSPI: ND (only complete population) No. of pts: ND, assume 38/38 (100%) | SSPI: Preop SI: 11° ± 6.5° Postop SI: 2.3° ±1.6° SI at FU: 4.8° ±2.9° Preop LSC: 6.5 ± 0.7 LSC at FU: 2.7 ± 0.6 | ||
| Complete population: 27.8 mo (SD: 7.0, range 19-52 mo) ND, assume 95/95 (100%) | ||||
| Li (2012) Retrospective cohort III | MSPI (monosegmental pedicle instrumentation): Screws inserted into the vertebrae adjacent to the injured endplate (if the broken endplate was the superior and the adjacent vertebra was the upper, or if the broken endplate was the inferior and the adjacent vertebra was the lower). | MSPI: 13.2 mo (range 12-26 mo) NA (30/30, retrospective, only pts w/ FU) | MSPI: Kyphotic angles: Before surgery, 17.3° ± 9.3° 1 wk after surgery: 6.5° ± 6.5° Latest FU: 9.5° ± 6.4° | “The vertebral kyphotic angle was measured” |
| SSPI (short-segment pedicle instrumentation): Pedicle screws in one level above and one level below the injured vertebra. | SSPI: 34.6 mo (range 12-64 mo) NA (30/30, retrospective, only pts w/ FU) | SSPI: Kyphotic angles: Before surgery, 16.5° ± 9.1° 1 wk after surgery: 7.1° ± 6.9° Latest FU: 7.5° ± 5.2° | ||
| Bailey (2014) RCT Ib | No orthosis (NO): Immediate mobilization as tolerated with restrictions to limit bending and rotating through the trunk. Return to normal activities encouraged after 8 wk. | NO: 24 mo ND 36/49 (73%) 12 mo: 40/49 (82%) | NO group kyphosis angle: Admission: 14° ±6° Discharge: 20° ±8° 12 mo: 21° ± 9° 24 mo: 21° ± 9° | Kyphosis was measured based on the Cobb technique, as the angle succumbed between the perpendicular to the superior and inferior end plate of the vertebral body above and below the fractured level, respectively |
| Early mobilization with “off-the-shelf” adjustable thoracolumbosacral orthosis (TSLO): Strict bed rest until fitted with a TLSO and mobilization in the brace. The TLSO worn at all times except when lying flat in bed for a total of 10 wk with start of weaning from the brace at 8 wk. | TSLO: 24 mo ND 32/47 (68%) 12 mo: ND 41/47 (87%) | TLSO group kyphosis angle: Admission: 15° ± 8° Discharge: 18° ± 7° 12 mo: 22° ± 6° 24 mo: 22° ± 5° | ||
| Proietti (2014) retrospective cohort III | All patients (group A* + group B**): Short stabilization: one level above and one below *Group A: SI > 10° ≤ 15° **Group B: SI > 15° | Total population (group A + group B) Minimum 12 mo (range 12-48 mo) 60/63 (95%) | Group A: SI at 1 y: 9.3° (10°-15°) Correction loss 2.1° | Sagittal index: Sagittal index (SI) in accordance to Farcy’s criteria52 Definition: The measurement of segmental kyphosis at the level of a given mobile segment (1 vertebra and 1 disc) adjusted for the baseline sagittal contour at that level. The sagittal index is derived by subtracting the baseline values from the measured segmental kyphosis at the injured level. Farcy et al used the following baseline estimates for the intact sagittal curve: 5° in the thoracic spine, 0° in the thoracolumbar junction, and 10° in the lumbar spine. Segmental kyphosis at the fracture level was defined as a positive value. Subtracting the baseline values from the segmental kyphosis was used to derive the sagittal index. |
| Group B: SI at 1 y: 15.4° (13°-22°) Correction loss 3.7° | ||||
| Schmid (2011) prospective cohort III | Short segmental posterior fixation with angular stable pedicle screw systems Group A: plus posterolateral fusion Group B: plus unilateral TLIF with monocortical strut grafts and cancellous bone (ICBG) implant removal at a mean of 15.1±3.7months The analysis was performed separately for two patient groups, but only group B (“TLIF group”) was large enough to be eligible for this review, so the group A is not considered here | 20.2 mo (SD: 6.1) 21/21 (100%) | Initial monosegmental angle: −16.0° ± 10.0° Initial spinal canal narrowing: 34.3% ±16.4% Postoperative monosegmental angle: −0.8° ± 6.8° Monosegmental surgical correction: 15.1° ± 8.3° Postoperative spinal canal narrowing: 9.3% ± 9.3% Monosegmental angle at final FU: −5.6° ±7.6° Postoperative loss of correction 4.9° ±8.3° | Monosegmental angles were measured as endplate angles between both end plates adjacent to the fused segment in a lateral projection. The narrowing of the spinal canal was measured on axial CT scans and described in percentages with the width of the adjacent intact vertebra serving as a 100% reference |
| Jeong (2013) Retrospective cohort III | Pedicle screws 1 level above and 1 level below the fracture level | 27.6 mo (range 12-66 mo) NA (23/23, retrospective, only pts w/ FU) | Cobb angle: Preop 17.4° (7.7°-38.1°) Postop 4.9° (0.03°-18.9°) At last FU 9.3° (1.7°-29.6°) Anterior vertical compression ratio: Preop 37.5% (11.3%-60.7%) Postop 14.0% (6.3%-30.2%) At last FU 20.9% (4.5%-38.4%) | The Cobb’s angle and the anterior vertical compression ratio were calculated according to Jiang et al45 |
| Koller (2008) Retrospective case series IV | Manual kyphosis reduction through anterior force, then 3 months of brace (24 h/d) | 112.8 mo (SD: 47 mo) NA (21/21, retrospective, only pts w/ FU) | Regional kyphosis angle at FU: 4.7° ± 10.9° Segmental kyphosis angle at FU: 12.1° ± 6.3° | Regional kyphosis angle (RKA): Injury RKA was indicated as the Cobb angle on supine lateral and on standing full length radiographs Segmental kyphosis angle (SKA): angle between the inferior end plate of the vertebral body above the fracture and the inferior end plate of the fractured body |
| Andress (2002) Retrospective case series IV | Internal fixator either with or without transpedicular spongiosa grafting with fixed-angle pedicle screw instrumentation and pedicle screws above and below the fractured vertebral body In cases where the kyphotic angle was large or where the fractured vertebral body was completely destroyed: transpedicular inter- and intracorporal autologous bone grafting after transpedicular discectomy Transpedicular spongiosa grafting: 29 pts (58%) No grafting: 21 pts (42%) | 68 mo (range 36-103 mo) NA (50/50, retrospective, only pts w/ FU) | SI at FU stratified acc. to fx type (mean ± SD) A 3.1 0.82 ± 0.15 A 3.2 0.79 ± 0.12 A 3.3 0.81 ± 0.13 Sagittal plane kyphosis at FU stratified according to fx type (mean ± SD) A 3.1 −15.5 ± 6.5 A 3.2 −19.0 ± 7.1 A 3.3 −14.0 ± 6.6 | Using the ratio of the heights of the anterior and posterior vertebral wall (on lateral views of the injured vertebral body) we calculated the sagittal index (SI). Sagittal plane kyphosis (SPK): angle between the superior end plate of the vertebral body above the fracture and the inferior end plate of the fractured body |
Abbreviations; ND, not documented; w/, with, w/o; without, pt, patient; pts, patients; NA, not applicable; fx, fracture, FU, follow-up; SI: Sagittal Index, LSC: Load Sharing Classfication.53
The major reasons for exclusion after full text screening were (a) the use of a different classification to describe the fracture type, which did not allow to determine whether the fractures could have been classified as A3 or A4 acc. to AOSpine21,22; (b) populations consisting of a mix of fracture types in which A3 and A4 were indeed contained, however not analyzed separate from other fracture types; (c) populations including patients with a neurological deficit; and (d) group size below threshold.
Outcomes
A wide range of different clinical outcome parameters were presented in the eligible publications: Most frequently reported was the pain VAS (7 studies), followed by the Roland Morris Disability Questionnaire (RMDQ)26 and Oswestry Disability Index (ODI)40 (6 studies each) and Short Form–36 (SF-36)41 (4 studies). The VAS functional spine score,42 LBOS,27 and patient satisfaction were reported in 3 studies each; the Hannover Spine score (FFbH-R),43 was reported in 2 studies, whereas the McGill Pain Questionnaire (MPQ),44 and an unspecified Quality of Life (QoL) scale were reported in 1 study each.
Nearly all publications presented results in which both A3 and A4 fractures were contained without stratification.14,15,30,31,33–38 Only Andress et al39 presented results stratified for fracture type and Koller et al32 presented results and fracture type for each individual patient.32 Based on the lack of stratified results, we were unable to evaluate results of A3 and A4 fractures separately.
SMDs were calculated for all studies directly comparing operative with nonoperative treatment.14,15,33,36 All 4 of these studies reported on disability but only 3 reported on pain.14,15,33
Heterogeneity assessment of the studies combined to calculate the SMD for disability revealed an I 2 of 86.3% (P = .000), whereas for the studies combined to calculate the SMD for pain, the I 2 was 93.0% (P = .000). Based on the high heterogeneity, a random effects model was used to calculate the SMD. Estimation of the SMD for disability was based on RMDQ and LBOS scores, while for pain it was based on the pain VAS.
For disability, the overall SMD was 0 (95% CI −0. 72, 0.72) (Figure 2) and for pain it was −0.26 (95% CI −1.47, 0.95) (Figure 3). An SMD of less than 0 favors operative treatment whereas SMD values greater than 0 favor nonoperative treatment.
Figure 2.
Standardized mean difference for disability combined with Newcastle-Ottawa Scale for bias rating.
Figure 3.
Standardized mean difference for pain combined with Newcastle-Ottawa Scale for bias rating.
Egger’s regression did not reveal any evidence of publication bias with coefficients of −8.75 for studies pooled for disability SMD (P = .553) and −11.81 for studies pooled for pain (P = .591).
In addition to the meta-analysis performed with studies directly comparing operative with nonoperative treatment, clinical outcome parameters that were available for a minimum of 125 patients for each of the target treatment modalities were analyzed descriptively for all studies. This was done for RMDQ and pain VAS. Since some of these studies comprised more than 1 patient group, results are presented per treatment group rather than per study (Figures 4 and 5).
Figure 4.

Results and treatment group sizes of all studies reporting Roland Morris Disability Questionnaire (RMDQ) presented in the order of methodological quality. X and Ο represent the RMDQ mean values and the bars represent the standard deviation.
Figure 5.
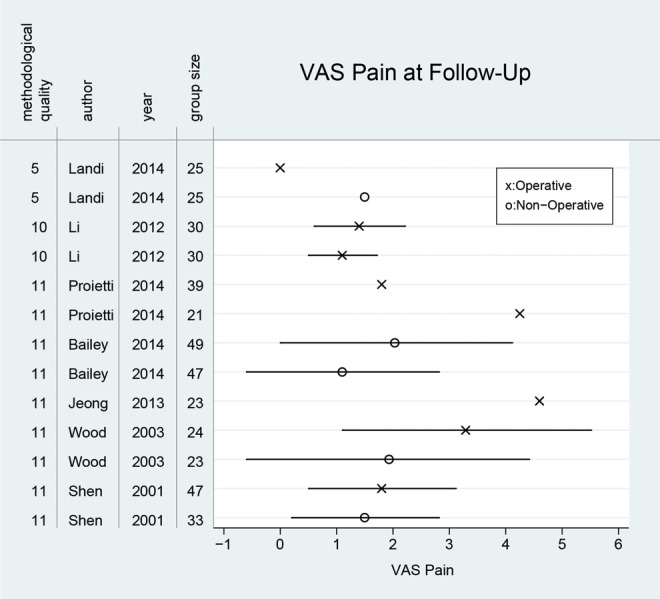
Results and treatment group sizes of all studies reporting pain visual analog scale (VAS) presented in the order of methodological quality. X and Ο represent the pain VAS mean values and the bars represent the standard deviation (as far as reported).
Generally, the differences in the respective outcome parameter results at FU were small, both between studies and between treatment groups. Nine of 13 treatment groups that presented pain VAS reported mean values between 1 and 2 at FU, with the most extreme values coming from operatively treated patients. The best pain VAS results were published by Landi et al33 for the surgical treatment group, where none of the patients reported any pain at FU. They had only included patients with a McCormack score of 6 or less and a maximum spinal canal invasion of 25%. The worst pain was reported by Jeong et al31 who surgically treated patients with a McCormack score of 7 or higher and reported a mean pain VAS of 4.6 at FU for this group. Similar pain values were reported for patients with a Sagittal Index (SI) >15°, treated surgically by Proietti et al.36 At FU, they reported a mean pain VAS of 4.3.
Likewise, 8 of 10 treatment groups with RMDQ results reported mean values between 3 and 4.4 at FU, also with the most extreme values coming from operatively treated patients. The best RMDQ results were reported by Landi et al,33 whose surgically treated patients reported a mean of 1.4 at FU while the worst RMDQ values were reported by Wood et al,15 whose surgically treated patients reported a mean of 8.2 at FU.
Only 3 studies provided information about the time after which their patients returned to normal work. Landi et al33 reported that patients treated operatively were back to work after 29 days while patients undergoing nonoperative treatment needed 117 days. Wood et al15 reported contrasting results: In the group treated operatively, 6 months after surgery 42% of patients were back to work while in the nonoperatively treated patients this proportion was 74%. After 2 years, 59% of the operatively treated patients were back to work whereas this was the case for 83% of the nonoperatively treated patients.15 Schmid et al37 treated patients operatively and reported a mean time for back to work of 4.9 months.
Complication outcomes are listed in Table 5 and were clearly in favor of nonoperative treatment since the majority of possible complications are related to surgery. The most important local adverse events reported in nonoperatively treated patients were the need for surgery due to persisting complaints. Interestingly, surgery after initial conservative treatment was only reported in patients from one study.30 In this study, which comprised 96 nonoperatively treated patients, 5 patients required surgery while still in hospital; 2 for severe radicular pain, and 3 for mechanical back pain. Another patient from this study required an osteotomy 8 months after her fracture. In operatively treated patients, instrumentation failure and donor site morbidity were the most significant adverse events. None of the included studies reported a neurological deterioration in any of their patients.
Most studies reported radiological outcomes with the target to describe the magnitude of kyphosis. However, a wide range of methods was used to measure it. Three studies provided no exact34 or an unclear33,37 description. Another 3 studies used the SI.36,38,39 The Cobb angle was presented in 3 studies.30–32 One of these studies additionally presented the anterior vertical compression ratio31 as described by Jiang et al.45 One study each14,15 used kyphosis measurement methods as described by Knight et al46 and Atlas et al,47 respectively. One study measured the segmental kyphosis angle (SKA),32 another study measured the sagittal plane kyphosis (SPK).39 The lack of uniform reporting made it impossible to pool the radiological results, which are listed in Table 6.
Quality Assessment
The quality assessment scores ranged from 4 to 11 on the 13-point scale. Two studies were rated low quality33,37 with scores of 5 and 4, respectively, 1 study scored 9,32 4 studies scored 10,34,35,38,39 and 5 studies scored 11.14,15,30,31,36
Risk of bias in the studies comparing conservative to surgical treatment was evaluated with the NOS.29 The highest risk of bias was found in the domain “comparability” since none of the studies had matched the treatment groups or controlled for potential confounders in the analysis. The lowest risk of bias was seen in the domain “outcome” since FU was sufficiently long with an acceptable rate of drop-outs.
Discussion
In this systematic review and meta-analysis, we attempted to generate the best available evidence to support either operative or non-operative management of AO A3 and A4 thoracolumbar burst fractures in patients without neurological deficit.
Since we identified a number of primary studies that compared operative with nonoperative treatment, we were able to pool the respective results to generate SMDs for disability and pain. No difference between the operative and nonoperative management was revealed for any of these parameters. This finding is also supported by the results reported in the studies not comparing operative to non-operative treatment, even though no analytical statistics could be performed with these results.
Two RCTs that just missed inclusion in this review are worth mentioning: In 2015, Wood et al48 published long-term results of the same patient cohort that is included in this review and was not included here because the number of patients available for analysis had fallen below our group size limit. However, the long-term results confirmed the earlier findings, which were strongly in favor of nonoperative treatment, becoming even more pronounced in the 20-year follow-up. The other RCT that just missed inclusion was published by Siebenga et al16 in 2006 and was clearly in favor of operative treatment. Its group size was below our limit and some patients with fractures other than A3 or A4 had been included.
Generally, the differences in clinical outcomes of the included publications were small, both between studies and between treatment groups. In the vast majority of treatment groups, pain VAS results ranged from 1 to 2 on a 0 to 10 scale and RMDQ results ranged from 3 to 4.4.
In the context of chronic low back pain, the minimally important change (MIC) of RMDQ has been suggested to be defined as 5.49 For back pain VAS on a scale of 0 to 100, values of 15 (see Ostelo et al49) and 18 and 19 (see Hagg et al50) have been suggested. Assuming that the MIC is similar for trauma patients, hardly any of the treatment groups included in this review present clinically relevant differences.
Previous attempts to synthesize the available clinical evidence have produced similar results: The systematic literature review conducted by Thomas et al19 in 2006 included 21 studies with a total of 564 patients but a recognized overall low quality. The authors concluded that in spite of the wealth of published studies on thoracolumbar burst fractures, methodological limitations were pervasive such that at the time, the available evidence to justify the additional risks of surgery in neurologically intact patients with thoracolumbar junction burst fractures was minimal.
In 2012, a meta-analysis published by Gnanenthiram et al12 based their main analysis on 2 randomized trials that yielded contrasting results and comprised heterogeneous patient populations. They concluded that “operative management of thoracolumbar burst fractures without neurologic deficit may improve residual kyphosis, but does not appear to improve pain or function at an average of 4 years after injury and is associated with higher complication rates and costs.”12
Abudou et al18 performed a Cochrane review in 2013, which included the same 2 trials with a total of 79 participants on which Gnanethiram et al12 had published a meta-analysis in the year before. Abodou et al18 summarized that the contradictory evidence provided by 2 small and potentially biased randomized controlled trials was insufficient to conclude whether surgical or nonsurgical treatment yielded superior pain and functional outcomes for people with thoracolumbar burst fractures without neurological deficit. However, they acknowledged that surgery was associated with more early complications and the need for subsequent surgery, as well as with greater initial health care costs.
In the absence of any evidence that would clearly favor one of the treatment options with regard to clinical outcome, on one hand, considerations on complication incidence, cost of intervention and time until full recovery gain importance. On the other hand, surgical treatment may well be considered for patients with unsatisfactory clinical outcomes after conservative treatment and further studies are needed to identify subgroups of patients who would benefit from early surgery.
The occurrence of complications in the studies included in this review is clearly in favor of nonoperative treatment. The most important local adverse events reported in nonoperatively treated patients were the need for surgery due to persisting complaints, while in the operatively treated patients, this concerned instrumentation and donor site morbidity.
These findings are well in line with results reported by other researchers. In 2014, Ghobrial et al20 published a review specifically targeted at adverse events in the operative and nonoperative management of thoracolumbar burst fractures. They found significant differences in the incidence of infection (5.5% vs 0%, P = .0009) and instrumentation failure leading to revision surgery (4.4% vs 0%, P = .004). The incidence of all other types of complications as well as the overall complication rate was always higher in the operatively treated patients, but this never reached statistical significance.20
The time required to go back to work reported in the studies included in our review is inconclusive due to contradicting results of the individual studies.
The major limitation of this review is the heterogeneity of included studies, which was present in various aspects such as FU time, study population, treatment modalities, and outcome parameters. The FU times ranged from 1 year to 10 years. However, since the clinical results were fairly uniform independent of FU time, we believe this had only a minor influence. On the other hand, the heterogeneity concerning the study populations was striking and certainly limited the comparability of studies in general. Nonetheless, the effect on clinical outcomes was primarily visible in the studies that had the most extreme differences in in- and exclusion criteria. For instance, Landi et al33 only included patients with a McCormack score of ≤6 and reported a mean pain VAS of 0 at FU,33 while Jeong et al31 report a mean VAS of 4.6 at FU in patients with a McCormack sore of ≥7. This highlights how heterogeneous patient populations hamper the comparability among trials. The aforementioned differences in the included populations also show that the focus on AO A3/A4 fractures alone as an inclusion criterion may not be sufficient to define a uniform population for a systematic review. And yet, given that the 12 primary studies found eligible for this review were derived from 1929 initial matches in the literature databases, stricter inclusion criteria might have led to even less eligible studies.
A further important source of heterogeneity was the lack of uniformity amongst treatments. For instance, all studies analyzing non-operative treatment used different treatment modalities. The same applied to the studies analyzing operative treatment, but several studies used short segment stabilization or mono segmental stabilization techniques with pedicle screws.33–35,38
Another limitation of our review is the choice of target outcome parameters. We focused on the most common clinical outcome scores, but all of these were initially developed and validated for patients with chronic low back pain caused by degenerative diseases. Hence, these scores may not be suitable instruments to measure the success of spinal interventions after trauma. However, since no such instruments exist yet, we did not have an alternative.
Additionally, it was not possible to evaluate the radiological outcomes due to the lack of uniform reporting. However, several studies have demonstrated superior radiological results after operative treatment.14,16,33 Nonetheless, the clinical relevance of radiological outcome in itself is unclear - no studies are known to us that demonstrate an unequivocal association of radiological and clinical outcomes after A3 and A4 fractures. On the other hand, many physicians are familiar with reports of patients who initially underwent conservative treatment and later in life present with significant global alignment and/or severe adjacent level issues requiring far more substantial surgery than initial surgical treatment would have involved. Further long-term studies employing uniform radiological outcome measures in combination with appropriate clinical scores are needed to address this important topic.
Finally, for calculation of the disability SMD, we pooled the functional scores RMDQ and LBOS. Even though the very concept of SMD relies on pooling different scores that are aimed at measuring the same outcome for the purpose of synthesizing evidence from different studies, pooling of these 2 scores is precarious. Both scores measure pain and the ability to perform activities of daily living, but while RMDQ measures the pain aspect purely in terms of duration, LBOS measures pain in terms of intensity.
Conclusion
This systematic review and meta-analysis did not reveal any difference in disability or pain outcomes between operative and nonoperative treatment of A3 and A4 thoracolumbar fractures in neurologically intact patients.
Unfortunately, it is currently unclear if the scores used to evaluate disability are indeed suitable for the evaluation of thoracolumbar trauma, which essentially implies that we are not sure whether we measure the right things. A new project has been initiated by AOSpine to define a thoracolumbar trauma score, which will hopefully solve the issue.51
Although previous studies have shown a possible benefit of surgical treatment of A3 and A4 fractures with regard to radiographic outcomes, a structured analysis of radiological outcomes was not possible in this review due to the wide range of different measurement techniques employed.
Furthermore, this review demonstrated that so far, the majority of studies have not differentiated between incomplete (A3) and complete (A4) burst fractures, leaving potential outcome differences between the 2 entities undetected. The new AOSpine classification aims to overcome this drawback by emphasizing this difference with a clear distinction between these fracture types in the classification labels.
In the future, it will be important for the spine community to define and enforce the use of specific and uniform outcome parameters that should be applied in all studies evaluating thoracolumbar trauma.
Acknowledgments
The authors thank the AO Foundation TK System for funding this work and AOCID staff, in particular Anahí Hurtado-Chong and Alexander Joeris for critical review and helpful discussions.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Three authors (Elke Rometsch, Brigitte Sandra Gallo-Kopf, and Vasiliki Kalampoki) are employees of AO Foundation in the Department of Clinical Investigation and Documentation (AOCID). Concerning the work under consideration, Frank Kandziora has received travel support and honorary for board meetings by AO Spine. Financial activities outside the submitted work within the preceding 36 months are reported by Maarten Spruit for his activities as Chairman of AO TK Spine, by Frank Kandziora for his activities as a consultant for DePuy-Synthes, Siemens, and Silony, by Roger Härtl for his activities as a consultant for Brainlab, Lanx, Depuy-Synthes and AOSpine, and by Robert Alton McGuire for review of medical records for Rehab, Inc.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by the AO Foundation TK System.
References
- 1. Limb D, Shaw DL, Dickson RA. Neurological injury in thoracolumbar burst fractures. J Bone Joint Surg Br. 1995;77:774–777. [PubMed] [Google Scholar]
- 2. Tian NF, Wu YS, Zhang XL, Wu XL, Chi YL, Mao FM. Fusion versus nonfusion for surgically treated thoracolumbar burst fractures: a meta-analysis. PloS One. 2013;8:e63995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barbagallo GM, Yoder E, Dettori JR, Albanese V. Percutaneous minimally invasive versus open spine surgery in the treatment of fractures of the thoracolumbar junction: a comparative effectiveness review. Evid Based Spine Care J. 2012;3:43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Boerger TO, Limb D, Dickson RA. Does ‘canal clearance’ affect neurological outcome after thoracolumbar burst fractures? J Bone Joint Surg Br. 2000;82:629–635. [DOI] [PubMed] [Google Scholar]
- 5. Xu GJ, Li ZJ, Ma JX, Zhang T, Fu X, Ma XL. Anterior versus posterior approach for treatment of thoracolumbar burst fractures: a meta-analysis. Eur Spine J. 2013;22:2176–2183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dimar JR, Carreon LY, Riina J, Schwartz DG, Harris MB. Early versus late stabilization of the spine in the polytrauma patient. Spine (Phila Pa 1976). 2010;35(21 suppl):S187–S192. [DOI] [PubMed] [Google Scholar]
- 7. Xing D, Chen Y, Ma JX, et al. A methodological systematic review of early versus late stabilization of thoracolumbar spine fractures. Eur Spine J. 2013;22:2157–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cheng LM, Wang JJ, Zeng ZL, et al. Pedicle screw fixation for traumatic fractures of the thoracic and lumbar spine. Cochrane Database Syst Rev. 2013;5:CD009073. [DOI] [PubMed] [Google Scholar]
- 9. Verlaan JJ, Diekerhof CH, Buskens E, et al. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine. 2004;29:803–814. [DOI] [PubMed] [Google Scholar]
- 10. Alcala-Cerra G, Paternina-Caicedo AJ, Diaz-Becerra C, Moscote-Salazar LR, Fernandes-Joaquim A. Orthosis for thoracolumbar burst fractures without neurologic deficit: a systematic review of prospective randomized controlled trials. J Craniovertebr Junction Spine. 2014;5:25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Giele BM, Wiertsema SH, Beelen A, et al. No evidence for the effectiveness of bracing in patients with thoracolumbar fractures. Acta Orthop. 2009;80:226–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gnanenthiran SR, Adie S, Harris IA. Nonoperative versus operative treatment for thoracolumbar burst fractures without neurologic deficit: a meta-analysis. Clin Orthop Relat Res. 2012;470:567–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hitchon PW, Torner JC, Haddad SF, Follett KA. Management options in thoracolumbar burst fractures. Surg Neurol. 1998;49:619–626. [DOI] [PubMed] [Google Scholar]
- 14. Shen WJ, Liu TJ, Shen YS. Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine (Phila Pa 1976). 2001;26:1038–1045. [DOI] [PubMed] [Google Scholar]
- 15. Wood K, Buttermann G, Mehbod A, et al. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am. 2003;85-A:773-781. [DOI] [PubMed] [Google Scholar]
- 16. Siebenga J, Leferink VJ, Segers MJ, et al. Treatment of traumatic thoracolumbar spine fractures: a multicenter prospective randomized study of operative versus nonsurgical treatment. Spine (Phila Pa 1976). 2006;31:2881–2890. [DOI] [PubMed] [Google Scholar]
- 17. Yi L, Jingping B, Gele J, Baoleri X, Taixiang W. Operative versus non-operative treatment for thoracolumbar burst fractures without neurological deficit. Cochrane Database Syst Rev. 2006;(4):CD005079. [DOI] [PubMed] [Google Scholar]
- 18. Abudou M, Chen X, Kong X, Wu T. Surgical versus non-surgical treatment for thoracolumbar burst fractures without neurological deficit. Cochrane Database Syst Rev. 2013;6:CD005079. [DOI] [PubMed] [Google Scholar]
- 19. Thomas KC, Bailey CS, Dvorak MF, Kwon B, Fisher C. Comparison of operative and nonoperative treatment for thoracolumbar burst fractures in patients without neurological deficit: a systematic review. J Neurosurg Spine. 2006;4:351–358. [DOI] [PubMed] [Google Scholar]
- 20. Ghobrial GM, Maulucci CM, Maltenfort M, et al. Operative and nonoperative adverse events in the management of traumatic fractures of the thoracolumbar spine: a systematic review. Neurosurg Focus. 2014;37:E8. [DOI] [PubMed] [Google Scholar]
- 21. Vaccaro AR, Oner C, Kepler CK, et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976). 2013;38:2028–2037. [DOI] [PubMed] [Google Scholar]
- 22. Reinhold M, Audige L, Schnake KJ, Bellabarba C, Dai LY, Oner FC. AO spine injury classification system: a revision proposal for the thoracic and lumbar spine. Eur Spine J. 2013;22:2184–2201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Verheyden AP, Holzl A, Ekkerlein H, et al. Recommendations for the treatment of thoracolumbar and lumbar spine injuries [in German]. Unfallchirurg. 2011;114:9–16. [DOI] [PubMed] [Google Scholar]
- 24. Vaccaro A, Kandziora F, Fehlings M, Shanmughanathan R. AO surgery reference—thoracic and lumbar trauma. AO Foundation. https://www2.aofoundation.org/wps/portal/surgery?showPage=diagnosis&bone=Spine&segment=TraumaThoracolumbar. Accessed January 14, 2016/
- 25. Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184–201. [DOI] [PubMed] [Google Scholar]
- 26. Roland M, Morris R. A study of the natural history of low-back pain. Part II: development of guidelines for trials of treatment in primary care. Spine (Phila Pa 1976). 1983;8:145–150. [DOI] [PubMed] [Google Scholar]
- 27. Greenough CG, Fraser RD. Assessment of outcome in patients with low-back pain. Spine (Phila Pa 1976). 1992;17:36–41. [DOI] [PubMed] [Google Scholar]
- 28. van Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Spinal radiographic findings and nonspecific low back pain. A systematic review of observational studies. Spine (Phila Pa 1976). 1997;22:427–434. [DOI] [PubMed] [Google Scholar]
- 29. Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomised studies in metaanalyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed January 1, 2016.
- 30. Bailey CS, Urquhart JC, Dvorak MF, et al. Orthosis versus no orthosis for the treatment of thoracolumbar burst fractures without neurologic injury: a multicenter prospective randomized equivalence trial. Spine J. 2014;14:2557–2564. [DOI] [PubMed] [Google Scholar]
- 31. Jeong WJ, Kim JW, Seo DK, et al. Efficiency of ligamentotaxis using PLL for thoracic and lumbar burst fractures in the load-sharing classification. Orthopedics. 2013;36:e567–e574. [DOI] [PubMed] [Google Scholar]
- 32. Koller H, Acosta F, Hempfing A, et al. Long-term investigation of nonsurgical treatment for thoracolumbar and lumbar burst fractures: an outcome analysis in sight of spinopelvic balance. Eur Spine J. 2008;17:1073–1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Landi A, Marotta N, Mancarella C, Meluzio MC, Pietrantonio A, Delfini R. Percutaneous short fixation vs conservative treatment: comparative analysis of clinical and radiological outcome for A.3 burst fractures of thoraco-lumbar junction and lumbar spine. Eur Spine J. 2014;23(suppl 6):671–676. [DOI] [PubMed] [Google Scholar]
- 34. Li X, Ma Y, Dong J, Zhou XG, Li J. Retrospective analysis of treatment of thoracolumbar burst fracture using mono-segment pedicle instrumentation compared with short-segment pedicle instrumentation. Eur Spine J. 2012;21:2034–2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Post RB, van der Sluis CK, Leferink VJ, Ten Duis HJ. Long-term functional outcome after type A3 spinal fractures: operative versus non-operative treatment. Acta Orthop Belg. 2009;75:389–395. [PubMed] [Google Scholar]
- 36. Proietti L, Scaramuzzo L, Schiro GR, Sessa S, D’Aurizio G, Tamburrelli FC. Posterior percutaneous reduction and fixation of thoraco-lumbar burst fractures. Orthop Traumatol Surg Res. 2014;100:455–460. [DOI] [PubMed] [Google Scholar]
- 37. Schmid R, Krappinger D, Blauth M, Kathrein A. Mid-term results of PLIF/TLIF in trauma. Eur Spine J. 2011;20:395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wei FX, Liu SY, Liang CX, et al. Transpedicular fixation in management of thoracolumbar burst fractures: monosegmental fixation versus short-segment instrumentation. Spine (Phila Pa 1976). 2010;35:E714–E720. [DOI] [PubMed] [Google Scholar]
- 39. Andress HJ, Braun H, Helmberger T, Schurmann M, Hertlein H, Hartl WH. Long-term results after posterior fixation of thoraco-lumbar burst fractures. Injury. 2002;33:357–365. [DOI] [PubMed] [Google Scholar]
- 40. Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 41. Ware JE, Jr, Snow KK, Kosinski M, Gandek MS. SF-36 Health Survey—Manual & Interpretation Guide. Lincoln, RI: QualityMetric; 2000. [Google Scholar]
- 42. Knop C, Oeser M, Bastian L, Lange U, Zdichavsky M, Blauth M. Development and validation of the Visual Analogue Scale (VAS) Spine Score [in German]. Unfallchirurg. 2001;104:488–497. [DOI] [PubMed] [Google Scholar]
- 43. Kohlmann T, Raspe H. Hannover Functional Questionnaire in ambulatory diagnosis of functional disability caused by backache [in German]. Rehabilitation (Stuttg). 1996;35:I–VIII. [PubMed] [Google Scholar]
- 44. Melzack R. The McGill Pain Questionnaire In: Melzack R, ed. Pain Measurement and Assessment. New York, NY: Raven Press; 1983:41–47. [Google Scholar]
- 45. Jiang SD, Wu QZ, Lan SH, Dai LY. Reliability of the measurement of thoracolumbar burst fracture kyphosis with Cobb angle, Gardner angle, and sagittal index. Arch Orthop Trauma Surg. 2012;132:221–225. [DOI] [PubMed] [Google Scholar]
- 46. Knight RQ, Stornelli DP, Chan DP, Devanny JR, Jackson KV. Comparison of operative versus nonoperative treatment of lumbar burst fractures. Clin Orthop Relat Res. 1993(293):112–121. [PubMed] [Google Scholar]
- 47. Atlas SW, Regenbogen V, Rogers LF, Kim KS. The radiographic characterization of burst fractures of the spine. AJR Am J Roentgenol. 1986;147:575–582. [DOI] [PubMed] [Google Scholar]
- 48. Wood KB, Buttermann GR, Phukan R, et al. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit: a prospective randomized study with follow-up at sixteen to twenty-two years. J Bone Joint Surg Am. 2015;97:3–9. [DOI] [PubMed] [Google Scholar]
- 49. Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. (Spine Phila Pa 1976). 2008;33:90–94. [DOI] [PubMed] [Google Scholar]
- 50. Hagg O, Fritzell P, Nordwall A. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12:12–20. [DOI] [PubMed] [Google Scholar]
- 51. Oner FC, Sadiqi S, Lehr AM, et al. Towards the development of an outcome instrument for spinal trauma: an international survey of spinal surgeons. Spine (Phila Pa 1976). 2015;40:E91–E96. [DOI] [PubMed] [Google Scholar]
- 52. Farcy JP, Weidenbaum M, Glassman SD. Sagittal index in management of thoracolumbar burst fractures. Spine (Phila Pa 1976). 1990;15:958–965. [DOI] [PubMed] [Google Scholar]
- 53. McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994;19:1741–1744. [DOI] [PubMed] [Google Scholar]




