Abstract
Study Design:
Meta-analysis and systematic review of literature.
Objective:
In the late 1990s, spinal surgeons experimented by using maxillofacial fixation plates as an alternative to sutures, anchors, and local spinous process autografts to provide a more rigid and lasting fixation for laminoplasty. This eventually led to the advent of laminoplasty mini-plates, which are currently used. The objective is to compare laminoplasty techniques with plate and without plate with regard to functional outcome results.
Methods:
Qualitative and quantitative analyses were performed to evaluate the currently available studies in an attempt to justify the use of a plate in laminoplasty.
Results:
The principal finding of this study was that there was no statistically significant difference in clinical outcome between the 2 different techniques of laminoplasty.
Conclusion:
There is not enough evidence in the literature to support one technique over the other, and hence, there is no evidence to support change in practice (using or not using the plate in laminoplasty). A randomized controlled trial will give a better comparison between the 2 groups.
Keywords: laminoplasty, myelopathy, meta-analysis
Introduction
Cervical spondylotic myelopathy (CSM) is a degenerative disease that has seen an evolution of its management over the past 70 years. The earliest decompression techniques were described in the 1940s using a posterior approach, and later, in the 1950s, the anterior approach was used via corpectomy. The posterior decompression technique was originally accomplished via multilevel laminectomy with subsequent incorporation of multilevel fusion techniques to reduce the potential for late instability and development of postoperative kyphosis.1
Tsuji first described the laminoplasty technique in 1982 as an alternative to laminectomy as the treatment for CSM.1 The technique was developed in an effort to eliminate the development of instability and kyphosis following laminectomy,2 while achieving minimal reduction in cervical range of movement (ROM).3 The concept revolves around canal expansion by opening the posterior elements in either a unilateral one-way hinge trap-door fashion (Hirabayashi technique) or midline spinous process splitting with bilateral hinges (French-door technique), but without completely removing the posterior arch. This in turn allows the posterior spinal musculature to heal to the residual posterior osseous elements, which lead to subsequent stability and potential ROM preservation.4 Studies have indicated that the laminoplasty results in about 30% to 50% loss of ROM of the cervical spine,5,6 which is much less than multilevel arthrodesis.
In the late 1990s, spinal surgeons experimented by using maxillofacial fixation plates as an alternative to sutures, anchors, and local spinous process autografts to provide a more rigid and lasting fixation.1,7 This eventually led to the advent of laminoplasty mini-plates, which are currently used.
However, there is very limited data with regard to the efficacy of these plates in comparison to nonplate techniques. Given the relatively high costs associated with the use of these plates,8 both qualitative and quantitative analyses were performed to evaluate the currently available literature in an attempt to justify its use.
Methods
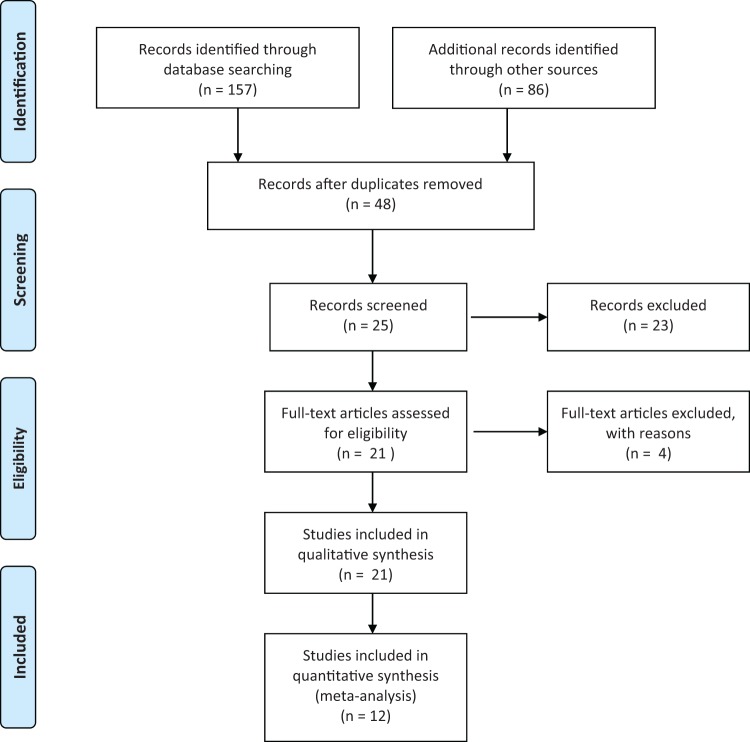
An experienced librarian conducted an extensive database search PubMed, Embase, Medline, CINAHL, and the Cochrane Library for literature published within the past decade. The keywords used were cervical laminoplasty, plate, plating, and mini-plate. The search was subsequently filtered for publications within the period of 2000 to 2013. The database search results—Medline (27 studies), PubMed (52), Embase (61), CINAHL (7), and the Cochrane Library (10)—were subsequently filtered for duplicates and inclusion criteria, which consisted of publications in English, noncadaveric studies, cohort of at least 10 patients, and a follow-up period of at least 18 months. The final results yielded a total of 21 studies, of which only 13 studies used a plate in their laminoplasty techniques (Figure 1).
Figure 1.
Article selection flow chart.
The outcome measures considered in measuring the efficacy of each technique included changes in the Japanese Orthopaedic Association (JOA) scores, Hirabayashi recovery rate (measured as a percentage of change in JOA score from preprocedure to postprocedure), Nurick scores, and ROM. Age and gender were assessed in each study and adjusted for in the final outcomes. Due to the variable nature of reported outcomes among the included studies, a mixed analysis involving both qualitative and quantitative analyses was performed to thoroughly evaluate the available literature. The most consistent reported outcome measure was the JOA score and the Hirabayashi recovery rate, while reporting of changes in Nurick scores and ROM were extremely limited. Thus, the focus of the quantitative analysis was limited to only the Hirabayashi recovery rate as it also adjusted for the effect size of each individual study.
Statistical Analysis
Statistical heterogeneity was measured using the Q statistic, with the I 2 statistic used to describe the percentage of total variation across studies due to heterogeneity.9 An I 2 value of 0% represents no observed heterogeneity, while values approaching 100% indicate increasing heterogeneity. To account for heterogeneity between studies, DerSimonian and Laird random-effects models10 were used. Weighted effect sizes were estimated along with 95% confidence intervals for the Hirabayashi effect outcome, while an inspection of preoperative JOA scores was also considered.
Due to the small number of studies considered in the analysis, stratification to consider subgroups or meta-regression of the studies to explain heterogeneity was not considered to be suitable. The presence of publication bias was considered through the preparation of funnel plots, with the absence of bias identified from a symmetrical inverted funnel. However, due to the small number of studies, it was not appropriate to consider statistical methods to detect or correct for any biases that were identified.
All analyses were conducted using STATA/SE 12.1 (Stata-Corp, College Station, TX), with P values of less than .05 considered statistically significant.
Results
In total, 21 studies were identified through our literature search, excluding duplicates. Due to the discrepancies in the reported data including lack of reported and/or calculable standard deviations, standard errors, and application of inclusion and exclusion criteria (Table 1), only 12 of the included studies could be used in the meta-analysis. The studies are summarized in Table 2.
Table 1.
PICO Table Describing Inclusion and Exclusion Criteria.
| Study Component | Inclusion | Exclusion |
|---|---|---|
| Population |
|
|
| Intervention(s) |
|
|
| Outcomes |
|
|
| Publication |
|
|
| Study design |
|
|
Table 2.
Summary of Studies Included for Analysisa,b.
| Author | Year | Journal | Study Type | Evidence Level | Laminoplasty Patients | Percentage Male (%) | Mean Age | Follow-up Period (Months), Mean (SD) | Preoperative JOA Score, Mean (SD) | Postoperative JOA Score, Mean (SD) | Hirabayashi Recovery Rate (%), Mean (SE) | Preoperative Nurick Score, Mean (SD) | Postoperative Nurick Score, Mean (SD) | Preoperative ROM (°), Mean (SD) | Postoperative ROM (°), Mean (SD) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Plate Studies | |||||||||||||||
| Agrawal | 2004 | Neurol India | Retrospective review | 3 | 24 | 87 | 56.73 | 22 | N/A | N/A | N/A | 4.04 | 3.16 | N/A | N/A |
| Mizuno | 2006 | Spine J | Retrospective comparative | 3 | 10 | N/A | N/A | 24 | N/A | N/A | N/A | N/A | N/A | 32.1 ± 13.0 | 26.2 ± 11.0 |
| Orabi | 2008 | Neurosurg Rev | Prospective trial | 2 | 22 | 73 | 62.6 | 21.1 | 7.5 | 15.6 | 85.3 | N/A | N/A | N/A | N/A |
| Dimar | 2009 | Am J Orthop | Retrospective review | 3 | 104 | 61 | 59.2 | 50.2 ± 19 | N/A | N/A | N/A | 2.11 ± 0.85 | 0.63 ± 0.69 | N/A | N/A |
| Asgari | 2009 | Acta Neurochir | Prospective case series | 2 | 13 | 85 | 49 | 33 | 11 | 12 | 16.7 | N/A | N/A | N/A | N/A |
| Petraglia | 2010 | Neurosurgery | Retrospective review | 3 | 40 | 70 | 57 | 31.3 ± 15.1 | N/A | N/A | N/A | 2.08 | 0.93 | N/A | N/A |
| Jiang* | 2012 | Orthopedics | Retrospective comparison | 3 | 38 | 63 | 56 | 19 | 9.0 ± 0.7 | 13.3 ± 0.9 | 53.75 | N/A | N/A | 49.6 ± 6.9 | 40.1 ± 4.0 |
| Chen*+ | 2012 | Orthopedics | Retrospective review | 3 | 29 | 86 | 61.2 | 23.3 ± 7.2 | 9.48 ± 2.28 | 13.79 ± 1.78 | 57.48 (3.07) | N/A | N/A | 39.48 ± 8.74 | 36.07 ± 9.82 |
| Jiang* | 2012 | J Clin Neurosci | Retrospective review | 3 | 26 | 65 | 62 | 22 | 9.1 ± 1.5 | 13.9 ± 1.6 | 60.7 (2.45) | N/A | N/A | 30.5 ± 8.2 | 27.5 ± 8.7 |
| Yang* | 2013 | Orthopedics | Retrospective review | 3 | 75 | 75 | 57.19 | 24 | 8.91 ± 1.23 | 13.55 ± 1.34 | 57.29 (1.78) | 2.40 ± 0.96 | 0.65 ± 0.71 | 29.88 ± 6.43 | 24.95 ± 6.24 |
| Fujimori | 2013 | Neurosurg Focus | Retrospective comparison | 3 | 60 | 67 | 63.1 | 20.9 ± 13.1 | 12.8 ± 3.1 | 14.5 ± 2.7 | 40.48 | 2 | 1 | 32.7 | 24.4 |
| Yang* | 2013 | J Spinal Disord Tech | Retrospective review | 3 | 42 | 86 | 61.4 | 23.2 ± 7.4 | 9.5 ± 1.8 | 13.9 ± 1.5 | 58.9 (2.75) | N/A | N/A | N/A | N/A |
| Hyun* | 2013 | Spine J | Prospective cohort | 2 | 18 | 67 | 56.4 | 68.1 | 10.1 ± 3.5 | 13.9 ± 2.0 | 55.0 (4.43) | N/A | N/A | 39.9 ± 11.2 | 24.5 ± 10.1 |
| No-Plate Studies | |||||||||||||||
| Iwasaki* | 2007 | Spine | Retrospective review | 3 | 66 | 77 | 57 | 122.4 | 9.2 | 13.7 | 55 (7.45) | N/A | N/A | N/A | N/A |
| Matsumoto* | 2008 | J Neurosurg | Retrospective review | 3 | 82 | 76 | 62.7 | 21.6 | 9.7 ± 3.1 | 13.7 ± 2.4 | 53.9 (3.30) | N/A | N/A | N/A | N/A |
| Yang | 2008 | Acta Orthop | Prospective series | 2 | 12 | 58 | 62 | 32 | 6.9 ± 3 | 13 ± 1.6 | 60.4 | N/A | N/A | N/A | N/A |
| Suzuki* | 2009 | Spine | Prospective cohort | 2 | 98 | 70 | 59.6 | 81.6 | 11.1 ± 3.96 | 14.3 ± 1.98 | 50.1 (3.8) | N/A | N/A | N/A | N/A |
| Kotani* | 2009 | Eur Spine J | Retrospective comparative | 3 | 84 | 76 | 62 | 32 | 9.1 ± 3.5 | 14.6 ± 1.6 | 69 (1.64) | N/A | N/A | N/A | N/A |
| Okada* | 2009 | Spine | Prospective RCT | 2 | 35 | 80 | 59.9 | 27.6 | N/A | 14.2 ± 1.6 | 52.8 (4.75) | N/A | N/A | N/A | N/A |
| Sivaraman | 2010 | J Spinal Disord Tech | Prospective comparison | 2 | 25 | 56 | 62.4 | 24 | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Liu* | 2011 | J Spinal Disord Tech | Retrospective comparative | 3 | 27 | 59 | 56 | 27.47 ± 11.06 | 8.59 ± 2.98 | 13.67 ± 2.7 | 59.54 (5.65) | N/A | N/A | 40.44 ± 10.25 | 36.15 ± 10.58 |
| Chen*+ | 2012 | Orthopedics | Retrospective review | 3 | 25 | 80 | 63.2 | 25.8 ± 8.5 | 9.24 ± 1.42 | 13.60 ± 0.87 | 56.10 (?) | N/A | N/A | 38.52 ± 9.99 | 29.52 ± 10.13 |
| Jiang+ | 2012 | Orthopedics | Retrospective comparison | 3 | 23 | 70 | 59 | 19 | 9.2 ± 1.0 | 13.1 ± 0.7 | 50 | N/A | N/A | 51.3 ± 8.1 | 41.4 ± 5.1 |
| Seng* | 2013 | Spine J | Retrospective analysis | 3 | 52 | 77 | 60.6 | 24 | 11 ± 3 | N/A | 53.1 (5.87) | N/A | N/A | N/A | N/A |
aAll studies were considered used for qualitative analysis, and only studies marked with asterisks were used for quantitative analysis.
bStudies marked with “*” and shaded gray = studies included in the meta-analysis. “+” = Same paper.
Systematic Review
The studies were stratified into levels of evidence based on the guidelines from the Journal of Bone & Joint Surgery (2003). There were 7 publications that were of level II evidence, and mostly consisted of prospective studies, while the remaining 14 were of level III evidence, which comprised predominantly retrospective studies.
Level II
Plate studies
Orabi et al11 described the use of a specific tailored plate as a modification to the double-door laminoplasty technique in a series of 22 patients with impressive results—an improvement of preoperative JOA score from a mean of 7.5 to 15.6, which is equivalent to a Hirabayashi recovery rate of 85.2%. Radiological assessments of outcome were equally impressive with 0% lordotic changes on cervical X-rays, no instrumentation failure, and no signs on instability subsequent computed tomography (CT) and magnetic resonance imaging (MRI) scans. The reported cervical spinal canal diameter improvement ranged from 40.7% to 100%. Although described as a prospective trial, the findings are unfortunately limited by the lack of a control group and small number.
Asgari et al12 performed a prospective comparison between 2 laminoplasty techniques—bilateral cutting with retro-positioning laminae with bilateral mini-plate fixation versus simple open-door technique with unilateral mini-plating. The differences between the 2 groups were minor, with only the open-door technique being slightly superior with regard to spinal canal diameter improvement and complication rates. Overall, while accounting for both cohorts, the mean JOA score improved from 11 to 12 postoperatively, which translates to a Hirabayashi recovery rate of 16.7%, which is vastly contrasting from that reported by Orabi et al.11 This was further supported by a similar mean improvement rate on the Nurick score of 12.3%.
Hyun et al13 looked at the long-term loss of flexion-extension ROM associated with laminoplasty over a 5-year period. They found that the overall ROM was worse in those with ossification of posterior longitudinal ligament (OPLL) in comparison to CSM (47.2% vs 72.7%). In addition, the laminar autofusion was associated with a greater reduction in ROM (55.6% decrease) in comparison to non-autofusion (13.4% decrease). The overall mean JOA of both cohorts showed an improvement from 10.1 to 13.9, which translates into a Hirabayashi recovery rate of 55%, which is much more consistent with other studies.
No-plate studies
Yang et al14 present a prospective series of 12 patients who underwent a modified unilateral open-door laminoplasty technique using suture anchor fixation with fairly good reported outcomes. The mean improvement in JOA score was 6.1 (from 6.9 to 13), with an average Hirabayashi recovery rate of 60.4%. The spinal canal diameter was improved by a mean of 49%, and mean ROM reduction was 24%. These outcomes are fairly consistent with reported literature.
Chen et al15 performed a prospective cohort study looking at the recovery process of patients with CSM who underwent a laminoplasty procedure. A total of 98 patients underwent a double-door laminoplasty procedure and were divided into 2 cohorts based on age (<70 and >70). The mean improvement in JOA score was 3.2 (11.1 to 14.3), which was equivalent of a Hirabayashi improvement rate of 50.1%. Interestingly, the improvement in JOA scores plateaued at 8.7 months, which is much earlier compared to the other 2 outcome measures—grasp strength and a 10-second grip and release test—which were much later at 21.7 and 25.6 months, respectively. Recovery was delayed in the more elderly group as expected. In addition, a subanalysis of the causes of myelopathy showed the least Hirabayashi recovery rate with OPLL, followed by spondylosis and disc herniation.
Okada et al16 performed a prospective randomized controlled trial comparing open-door laminoplasty and French-door laminoplasty techniques. The average Hirabayashi recovery rate for open-door laminoplasty was 52.8%, which was slightly better than French-door laminoplasty at 42% but was not statistically significant. Complication rates were noted to be higher in the open-door laminoplasty group, but Short Form-36 (SF-36) scores and postoperative axial pain were better improved by French-door laminoplasty.
Sivaraman et al17 performed a prospective nonrandomized study comparing skip laminectomy and laminoplasty, and the findings were significantly in favor of skip laminectomy. The main outcome measure was the percentage of ROM maintained postsurgery, whereby skip laminectomy was 84% while laminoplasty was 46%. This ROM reduction is much more significant if compared to that reported by Yang et al, but this may be attributable to difference in laminoplasty technique as double-door laminoplasty was used in this study. In addition, decompression by skip laminectomy was found to be better on MRI calculation of cervical spinal cord cross sectional area (122.9 mm2 vs 98.8 mm2) at 6 months and cervical pain scores on SF-12 (3.45 vs 2.95), both statistically significant.
Level III
Plate studies
Agrawal et al18 performed a retrospective study assessing the efficacy of laminoplasty with mini-plates as described by O’Brien in patients with severe CSM based on Nurick scores. The mean preoperative Nurick score was 4.04, which improved to 3.16 postoperatively. In the study, it was found that all patients with duration of symptoms less than 3 years and 50% of the patients with duration of symptoms between 3 and 6 years had improvement of 1 point Nurick score, while patients that suffered a duration of symptoms more than 6 years showed no change in Nurick score postoperatively. The Nurick score improvement of 0.88 was similar to those reported by Dimar et al19 (1.47-2.11 to 0.63) and Petraglia et al8 (1.15-2.08 to 0.93).
Jiang et al20 retrospectively reviewed 61 patients with CSM that underwent laminoplasty and compared the outcomes of plate versus suture laminoplasty. The mean improvement of JOA score in the plate group was slightly better than the suture group (4.3 vs 3.9), while the ROM reduction was slightly less in the suture compared to the plate group (8.9° vs 9.2°) but neither finding was statistically significant. The only statistically significant finding was the improvement in AP diameter that was better in plate group (5.1 mm vs 4.5 mm). However, Chen et al,15 who performed a similar review of 53 patients, found that the mean improvement of JOA score was slightly better in the plate group (4.36 vs 4.31), though the difference was not statistically significant. However, improvement in visual analog scales (VAS) scores (2.41 to 1.17 vs 2.56 to 2.44), axial symptoms, maintenance of cervical lordosis, and cervical ROM (39.48 to 36.07 vs 38.52 to 29.52) was statistically significant.
Yang et al21 retrospectively reviewed 141 CSM patients that underwent either plate-only laminoplasty or laminectomy and fusion to compare their outcomes. The authors found that there was no significant differences in the improvement of JOA scores (Hirabayashi recovery rate: 57.29 vs 58.87) and Nurick scores (2.40 to 0.65 vs 2.52 to 0.68), but the laminoplasty patients showed better improvement in Neck Disability Index (NDI) (34.11 to 14.67 vs 33.74 to 16.8) and VAS scores (2.85 to 1.11 vs 2.59 to 2.15). Complication rates in terms of C5 palsy and axial pain were also lower in the laminoplasty group. Maintenance of cervical canal cross-sectional area was similar for both groups at 24-month follow up, though the overall increase in area was better with the laminectomy group (52.68 mm2 vs 31.88 mm2). Overall, loss of ROM was also greater in the laminectomy group (63.03% vs 15.82%).
Jiang et al22 retrospectively reviewed 26 patients with multilevel degenerative cervical spine disease that underwent plate-only open-door laminoplasty. The mean improvement in JOA score was 4.8 (9.1 to 13.9), which corresponds to a Hirabayashi recovery rate of 60.7%. There was also a reported average loss of cervical ROM by 3.2° (30.5° to 27.5°). These results were closely mirrored by those from Yang et al,23 who retrospectively reviewed 42 patients who underwent plate laminoplasty for degenerative cervical disease with a mean improvement of JOA score of 4.4 (9.5 to 13.9) and a Hirabayashi recovery rate of 58.9%.
Fujimori et al24 retrospectively reviewed a total of 60 patients who underwent plated laminoplasty to review the outcomes based on the cause of cervical spondylosis. The mean JOA scores were improved in both groups (12.8 to 14.5 vs 13.2 to 14.2). VAS scores seemed to be better improved in the CSM group (4.2 to 2.6 vs 3.6 to 3.1) but was not statistically significant. The authors also further found that cervical ROM was more significantly reduced in patients with OPLL compared to CSM (34.4° to 20.8° vs 32.7° to 24.4°).
Mizuno et al25 performed a retrospective review of patients with OPLL and compared the outcomes between those who underwent anterior corpectomy and expansive unilateral laminoplasty with mini-plate fixation. Surgery-related outcome was reported to be good in 80% and fair in the remaining 20%, although the exact measure was not discussed. Another outcome measure identified was the change in cervical spine ROM, which was reduced by a mean of 5.9° (32.1° to 26.2°), which translate to reduction of 18.1%, which is similar to that reported by Yang et al.
No-plate studies
Iwasaki et al26 retrospectively reviewed 66 patients who underwent classical laminoplasty for OPLL to evaluate the factors that predicted outcomes and also the limitations of laminoplasty. The mean improvement in JOA score at final follow-up was 4.5 (9.2 to 13.7), which was equivalent to a Hirabayashi recovery rate of 55%. Factors predicting a poorer outcome were found to be occupying ratio of greater than 60%, hill-shaped ossification, lower preoperative JOA score, postoperative change in cervical alignment, and older age at the time of surgery.
Matsumoto et al27 performed a retrospective analysis of 82 patients that underwent classical laminoplasty to identify risk factors for closure of lamina given its strong association with poorer patient satisfaction. Lamina closure occurred in 34% of the patients. No statistical difference was found between patients who had a closed or open lamina in mean JOA improvement scores (9.7 to 13.7 vs 10.6 to 13.3), Hirabayashi recovery rates (53.9 vs 44.3), neck pain scores, and patient satisfaction level at final follow-up. The only significant factor identified to pose a significant risk was the presence of preoperative cervical kyphosis.
Kotani et al6 performed a retrospective cohort study comparing 2 nonplate laminoplasty techniques—conventional open-door laminoplasty versus deep extensor muscle-preserving laminoplasty. The difference in JOA scores improvement (9.1 to 14.6 vs 8.6 to 13.8) and Hirabayashi recovery rates (69 vs 65) were not statistically significant. The use of a new tentative JOA scoring system showed statistically significant improved cervical spine function (84% vs 63%) and quality of life scores (61% vs 45%) in the muscle-preserving group. This was also found to be similar in average VAS scores at final follow-up, favoring the muscle-preserving group (4.9 vs 2.3). There were however no statistical differences in cervical ROM.
Liu et al28 compared anterior cervical discectomy and fusion (ACDF) with laminoplasty in a retrospective analysis of clinical outcomes, radiographic changes, and complications in 52 patients with multilevel CSM. ACDF was found to be a more time-consuming procedure (187.78 minutes vs 115.92 minutes) and caused more operative blood loss (361.11 mL vs 118.48 mL). Both groups had marked improvement in JOA scores with Hirabayashi recovery rates of 59.79 and 59.54, respectively. The laminoplasty group had a better preservation of cervical ROM compared to the ACDF group (11.39% vs 29.45% reduction in ROM). Complications were significantly higher in the ACDF group.
Seng et al29 also compared laminoplasty with ACDF to assess for potential advantages of either technique in treating CSM. A retrospective analysis of 116 patients (64 ACDF; 52 laminoplasty) found laminoplasty had better improvement of JOA scores in the short term (11 to 13.7 vs 11 to 12.4), Hirabayashi (37.7 vs 31.8), while ACDF had better NDI scores in the short term. As found earlier by Liu et al,28 blood loss was noted to be lower in the laminoplasty group. However, no statistical difference could be found at the final follow-up at 2 years in terms of JOA score improvements (11 to 13.5 vs 11 to 14.4), Hirabayashi recovery rate (51.9 vs 53.1), NDI, SF-36, AAOS-NSS, VAS, and cervical ROM.
Given the variability of reported outcomes, a meta-analysis was performed to obtain a more objective outcome with regard to the topic.
Meta-Analysis
The trials included a total of 634 patients, with 190 from the plate group and 444 from the no-plate group. The number of participants ranged from 29 to 75 for the plate group and from 27 to 98 for the no-plate group. Length of follow-up ranged from 20.9 to 122.4 months across both groups. The mean or median age of participants ranged from 56 to 63.1 years, with the participants being predominantly male, ranging from 56% to 86% across studies. The majority of the included studies were retrospective studies (9), which were at most level III evidence. In addition, the lack of direct comparison between laminoplasty techniques allows for only relative comparison between outcome measures between the 2 groups, as statistical significance with P values was not calculable. Studies are presented in chronological order in Table 1 and in Figures 2 to 4.
Figure 2.
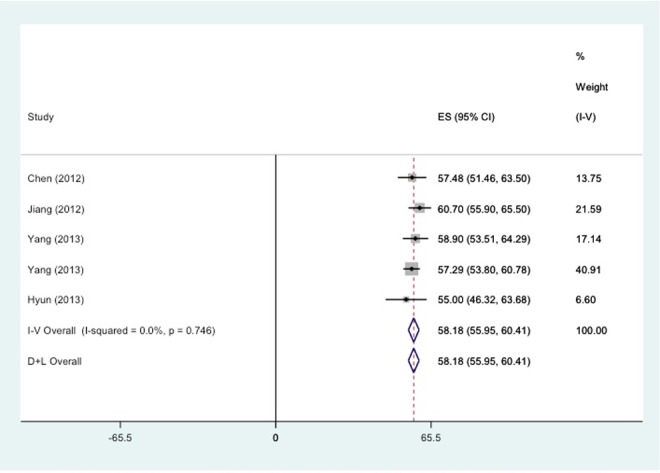
Forest plot comparing the Hirabayashi ES (%) at the end of follow-up for plate studies. ES, effect size; 1-V, inverse variance; D+L, DerSimonian and Laird method, weights are estimated from random effects analysis and contribute to D+L overall estimate.
Figure 3.
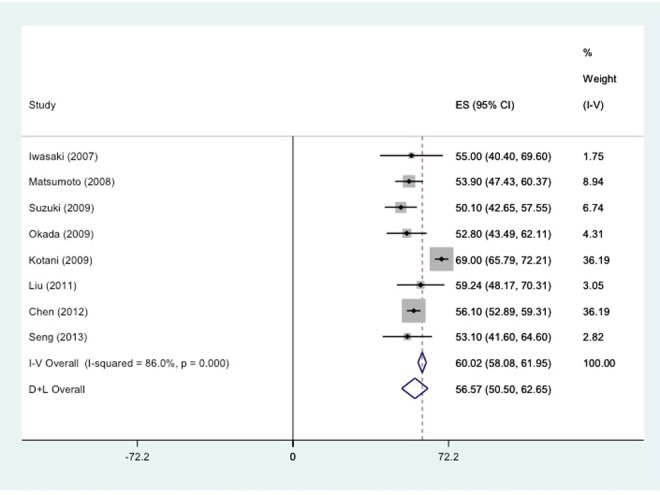
Forest plot comparing the Hirabayashi ES at the end of follow-up for no-plate studies. ES, effect size; 1-V, inverse variance; D+L, DerSimonian and Laird method, weights are estimated from random effects analysis and contribute to D+L overall estimate.
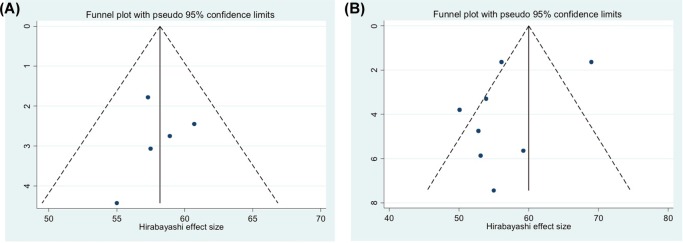
Figure 4.
(A) Funnel plot of Hirabayashi ES at the end of follow-up for plate studies. (b) Funnel plot of Hirabayashi ES at the end of follow-up for no-plate studies.
The pooled effect size for the plate group studies was 58.18% (95% confidence interval [CI] = 55.95% to 60.41%) compared to the pooled effect size for the no-plate group of 60.02% (95% CI = 58.08% to 61.95%). While there was no evidence of heterogeneity across the plate group, evidence of a high level of heterogeneity was observed in the no-plate group, with an I 2 value of 86.0% (P < .001). Thus, the DerSimonian and Laird (D+L) random-effects pooled effect size of 56.57% (95% CI = 50.50% to 62.65%) indicates an effect size that is slightly less that the plate group pooled effect size estimate, with wider 95% confidence intervals for the no-plate group reflecting the conservative assessment via the D+L random-effects method.
Given the Hirabayashi recovery rate takes into account preoperative JOA scores, an assessment of differences in preoperative scores was conducted for the 5 plate studies and the 7 no-plate studies. There was only evidence of a mild level of heterogeneity in the plate group (I 2 = 34.8%, P = .189) with mean JOA preoperative score of 9.19 (95% CI = 8.87 to 9.52). Of the 8 no-plate studies, the Iwasaki26 and Okada16 studies could not be assessed due to lack of either preoperative JOA mean or standard deviation values. For the 6 remaining studies, the mean JOA preoperative score was 9.77 (95% CI = 9.47 to 10.07), although this estimate was based on the random-effects D+L method due to a high level of heterogeneity in the preoperative JOA scores (I 2 = 83.7%, P < .001).
Visual inspection of the funnel plot for the no-plate studies indicated that there may be some evidence of publication bias, with a lack of results in the higher Hirabayashi score range with high standard error that may reflect smaller studies. However, given the small number of studies considered, it is also possible that the Kotani et al6 study with a high Hirabayashi effect size and low standard error may be an outlier, and is the main cause of the high level of heterogeneity in the no-plate study.
Considering a sensitivity analysis where the Kotani et al6 study is removed from the no-plate group analysis, there is no evidence of heterogeneity across the plate group (I 2 = 0.0%, P = .796), with the fixed effects size being 54.92% (95% CI = 52.50% to 57.34%).
Discussion
The principal finding of this study was that there were no statistically significant differences in clinical outcomes between the plate and nonplate laminoplasty techniques. Nonetheless, there was some evidence to suggest that the postoperative ROM of the cervical spine was slightly better with nonplate laminoplasty techniques but remain statistically not significant.
The current evidence base is presented with a number of limitations: the majority of included studies were retrospective in nature with relatively small sample sizes and were at most level III evidence. In addition, the lack of direct comparison between plate and nonplate laminoplasty techniques only allowed for relative comparison of outcome measures between the 2 groups.
The study groups were also plagued with very high heterogeneity due to the variability in reported outcomes measures—both clinical (JOA, Nurick, Hirabayashi recovery rate, and ROM) and radiological (X-ray, CT, and MRI)—leading to difficulty comparing outcomes. In addition, the complication and reoperation rates were not clearly documented in some of the studies, further accentuating the difficulty for comparison.
The heterogeneity further extends into the variability of surgical techniques described in both the plate and nonplate laminoplasty subgroups and the postoperative rehabilitation, which may affect the outcome measures reported. Furthermore, the introduction of rigid fixation with plate techniques have led to a paradigm shift in postoperative rehabilitation protocols that favor earlier ROM rather than traditional hard-collar bracing, whose effects on outcome measures were not clearly explored in the analyzed studies.
Based on the limitations of currently available evidence, this study is unable to obtain any strong conclusions to support the routine use of plates in laminoplasty, especially given its costs. Petraglia et al in their study quoted an estimated cost of a single laminoplasty plate alone in their institute in New York to be between $663 and $1967 depending on systems used, excluding the costs of allografts and screws required.8 As laminoplasty is often performed multilevel, the aforementioned costs would be expected to at least double if not triple per case for the plate alone. Sutures or stainless wires instead would unlikely accrue such instrumentation costs.
An alternative analysis of cost can be inferred based on reimbursements made by private health funds. In Australia, an independent organization—Private Healthcare Australia—has compiled a list of standardized minimum benefits based on prosthesis used for various procedures for all surgical specialties.30 According to their data, reimbursements are as follows: laminoplasty plates (US$760 per plate), screws (US$200 per screw), cerclage wire (US$12 per wire), anchors (US$310 per anchor), spacers (US$235 per spacer). Although these costs seem fairly similar to those quoted by Petraglia et al in their article, it may not be an accurate reflection of the cost in other parts of the world due to the high variability in the global spine market.
The current level of evidence surrounding this topic is unfortunately insufficient to properly answer the study question and certainly not adequate to suggest changing practice. A properly powered prospective randomized controlled study is required to further investigate and thoroughly evaluate the study question.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Emery SE. Cervical spondylotic myelopathy: diagnosis and treatment. J Am Acad Orthop Surg. 2001;9:376–388. [DOI] [PubMed] [Google Scholar]
- 2. Hirabayashi K, Satomi K. Operative procedure and results of expansive open-door laminoplasty. Spine (Phila Pa 1976). 1988;13:870–876. [DOI] [PubMed] [Google Scholar]
- 3. Lehman RA, Jr, Taylor BA, Rhee JM, Riew KD. Cervical laminoplasty. J Am Acad Orthop Surg. 2008;16:47–56. [DOI] [PubMed] [Google Scholar]
- 4. Kimura I, Shingu H, Nasu Y. Long-term follow-up of cervical spondylotic myelopathy treated by canal-expansive laminoplasty. J Bone Joint Surg Br. 1995;77:956–961. [PubMed] [Google Scholar]
- 5. Ratliff JK, Cooper PR. Cervical laminoplasty: a critical review. J Neurosurg. 2003;98(3 suppl):230–238. [DOI] [PubMed] [Google Scholar]
- 6. Kotani Y, Abumi K, Ito M, et al. Minimum 2-year outcome of cervical laminoplasty with deep extensor muscle-preserving approach: impact on cervical spine function and quality of life. Eur Spine J. 2009;18:663–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. O’Brien MF, Peterson D, Casey AT, Crockard HA. A novel technique for laminoplasty augmentation of spinal canal area using titanium miniplate stabilization. A computerized morphometric analysis. Spine (Phila Pa 1976). 1996;21:474–483. [DOI] [PubMed] [Google Scholar]
- 8. Petraglia AL, Srinivasan V, Coriddi M, Whitbeck MG, Maxwell JT, Silberstein HJ. Cervical laminoplasty as a management option for patients with cervical spondylotic myelopathy: a series of 40 patients. Neurosurgery. 2010;67:272–277. [DOI] [PubMed] [Google Scholar]
- 9. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. [DOI] [PubMed] [Google Scholar]
- 11. Orabi M, Chibbaro S, Makiese O, Cornelius JF, George B. Double-door laminoplasty in managing multilevel myelopathy: technique description and literature review. Neurosurg Rev. 2008;31:101–110. [DOI] [PubMed] [Google Scholar]
- 12. Asgari S, Bassiouni H, Massoud N, Schlamann M, Stolke D, Sandalcioglu IE. Decompressive laminoplasty in multisegmental cervical spondylotic myelopathy: bilateral cutting versus open-door technique. Acta Neurochir (Wien). 2009;151:739–749. [DOI] [PubMed] [Google Scholar]
- 13. Hyun SJ, Riew KD, Rhim SC. Range of motion loss after cervical laminoplasty: a prospective study with minimum 5-year follow-up data. Spine J. 2013;13:384–390. [DOI] [PubMed] [Google Scholar]
- 14. Yang SC, Niu CC, Chen WJ, Wu CH, Yu SW. Open-door laminoplasty for multilevel cervical spondylotic myelopathy: good outcome in 12 patients using suture anchor fixation. Acta Orthop. 2008;79:62–66. [DOI] [PubMed] [Google Scholar]
- 15. Chen G, Luo Z, Nalajala B, Liu T, Yang H. Expansive open-door laminoplasty with titanium miniplate versus sutures. Orthopedics. 2012;35:e543–e548. [DOI] [PubMed] [Google Scholar]
- 16. Okada M, Minamide A, Endo T, et al. A prospective randomized study of clinical outcomes in patients with cervical compressive myelopathy treated with open-door or French-door laminoplasty. Spine (Phila Pa 1976). 2009;34:1119–1126. [DOI] [PubMed] [Google Scholar]
- 17. Sivaraman A, Bhadra AK, Altaf F, et al. Skip laminectomy and laminoplasty for cervical spondylotic myelopathy: a prospective study of clinical and radiologic outcomes. J Spinal Disord Tech. 2010;23:96–100. [DOI] [PubMed] [Google Scholar]
- 18. Agrawal D, Sharma BS, Gupta A, Mehta VS. Efficacy and results of expansive laminoplasty in patients with severe cervical myelopathy due to cervical canal stenosis. Neurol India. 2004;52:54–58. [PubMed] [Google Scholar]
- 19. Dimar JR, 2nd, Bratcher KR, Brock DC, Glassman SD, Campbell MJ, Carreon LY. Instrumented open-door laminoplasty as treatment for cervical myelopathy in 104 patients. Am J Orthop (Belle Mead NJ), 2009;38:E123–E128. [PubMed] [Google Scholar]
- 20. Jiang L, Chen W, Chen Q, Xu K, Wu Q, Li F. Clinical application of a new plate fixation system in open-door laminoplasty. Orthopedics. 2012;35:e225–e231. [DOI] [PubMed] [Google Scholar]
- 21. Yang L, Gu Y, Shi J, et al. Modified plate-only open-door laminoplasty versus laminectomy and fusion for the treatment of cervical stenotic myelopathy. Orthopedics. 2013;36:e79–e87. [DOI] [PubMed] [Google Scholar]
- 22. Jiang JL, Li XL, Zhou XG, Lin H, Dong J. Plate-only open-door laminoplasty with fusion for treatment of multilevel degenerative cervical disease. J Clin Neurosci. 2012;19:804–809. [DOI] [PubMed] [Google Scholar]
- 23. Yang HL, Chen GD, Zhang HT, Wang L, Luo ZP. Open-door laminoplasty with plate fixation at alternating levels for treatment of multilevel degenerative cervical disease. J Spinal Disord Tech. 2013;26:E13–E18. [DOI] [PubMed] [Google Scholar]
- 24. Fujimori T, Le H, Ziewacz JE, Chou D, Mummaneni PV. Is there a difference in range of motion, neck pain, and outcomes in patients with ossification of posterior longitudinal ligament versus those with cervical spondylosis, treated with plated laminoplasty? Neurosurg Focus. 2013;35:E9. [DOI] [PubMed] [Google Scholar]
- 25. Mizuno J, Nakagawa H. Ossified posterior longitudinal ligament: management strategies and outcomes. Spine J. 2006;6(6 suppl):282S–288S. [DOI] [PubMed] [Google Scholar]
- 26. Iwasaki M, Okuda S, Miyauchi A, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: part 1: clinical results and limitations of laminoplasty. Spine (Phila Pa 1976). 2007;32:647–653. [DOI] [PubMed] [Google Scholar]
- 27. Matsumoto M, Watanabe K, Tsuji T, et al. Risk factors for closure of lamina after open-door laminoplasty. J Neurosurg Spine. 2008;9:530–537. [DOI] [PubMed] [Google Scholar]
- 28. Liu T, Yang HL, Xu YZ, Qi RF, Guan HQ. ACDF with the PCB cage-plate system versus laminoplasty for multilevel cervical spondylotic myelopathy. J Spinal Disord Tech. 2011;24:213–220. [DOI] [PubMed] [Google Scholar]
- 29. Seng C, Tow BP, Siddiqui MA, et al. Surgically treated cervical myelopathy: a functional outcome comparison study between multilevel anterior cervical decompression fusion with instrumentation and posterior laminoplasty. Spine J. 2013;13:723–731. [DOI] [PubMed] [Google Scholar]
- 30. Private Healthcare Australia. Part A—Prostheses list. http://www.privatehealthcareaustralia.org.au/prostheses/august%202016/Part%20A%20-%20Prostheses%20List.pdf. Accessed April 11, 2017.