Abstract
To systematically review experimental evidence about animal-assisted therapies (AAT) for children or adolescents with or at risk for mental health conditions, we reviewed all experimental AAT studies published between 2000–2015, and compared studies by animal type, intervention, and outcomes. Methods: Studies were included if used therapeutically for children and adolescents (≤21 years) with or at risk for a mental health problem; used random assignment or a waitlist comparison/control group; and included child-specific outcome data. Of 1,535 studies, 24 met inclusion criteria. Results: Of 24 studies identified, almost half were randomized controlled trials, with 9 of 11 published in the past two years. The largest group addresses equine therapies for autism. Conclusion: Findings are generally promising for positive effects associated with equine therapies for autism and canine therapies for childhood trauma. The AAT research base is slim; a more focused research agenda is outlined.
Keywords: Animal-assisted therapy, human-animal interactions, youth mental health, canine-assisted therapy, equine therapy
Under-recognition and under-treatment of children’s mental health needs are, unfortunately, well acknowledged in the scientific literature, dating back now to at least three decades (Knitzer and Olsen, 1982; Cooper et al., 2008; Institute of Medicine, 2006). Inattention to addressing children’s mental health needs by structuring and systematizing delivery of effective services is a problem long-recognized by state and federal authorities (McCarthy and Le, 2008; Substance Abuse and Mental Health Services Administration, 2005). In fact, this might be called the 20/20/2 problem: approximately 20% of children and adolescents will need mental health services in their lifetime (U.S. Department of Health and Human Services, 1999); of those, approximately 20% will actually receive such services (U.S. Public Health Service, 2000), and of those, only 2% receive evidence-based care (Bruns et al., in press).
While healthcare restructuring under the Patient Accountability and Affordability Act (2010) is likely to improve access to services for under-served populations, including children, it is not clear that (i) this is happening yet or that (ii) access to evidence-based services, as opposed to routine services, which are largely ineffective (Chorpita et al., 2013), will improve. One consequence of the long-standing problem of unmet need has been the proliferation of many different types of therapies, mostly unregulated, and mostly without empirical evidence for their effectiveness. In general, if a therapy can be paid for, someone will provide it.
One type of complementary and integrated therapy that is gaining popularity for children and adolescents with or at risk for mental health problems is animal-assisted therapy (AAT). We use the definitions of animal-assisted interventions and AAT as defined by the International Association of Human-Animal Interaction Organizations (IAHAIO, 2014). AAI is a “goal-oriented and structured intervention that intentionally includes or incorporates animals in health, education and human service…for the purpose of therapeutic gains in humans.” AAT is a subcategory that is a specific therapeutic intervention. In this paper, we focus on AAT, usually delivered by human service professionals with specialized expertise (Balluerka et al., 2014; Bass et al., 2009; Dietz et al., 2012; Kamioka et al., 2014). AATs are often a complement or adjunct to other therapies but sometimes are a stand-alone intervention. Animals are chosen because they are perceived as having a therapeutic benefit (Balluerka et al., 2014), enabling a safe and trusting relationship to be created between the child and the animal.
A thoughtful recent review of the psychological processes relevant to human-animal relations by Amiot and Bastian (2015) emphasized the interdependence and interactional nature of these relations. Several theories that explain the animal-human relationship were described, including biophilia, (emotional connection to other living things), and attachment (a bidirectional connectivity between humans and animals). The authors also describe the influence of religion, ideological beliefs, gender, work, and culture on the human-animal relationship. They point out that a range of therapies has arisen from these different theoretical and socio-cultural belief systems.
Studies of therapies on human-animal interaction have either targeted specific animals (e.g., horses or dogs) or specific populations (e.g., autism). To our knowledge, there have been no systematic reviews focused on AAT for children with or at risk for mental health conditions which examined the rigor of the evidence base by focusing on controlled studies, and which identified child-specific mental health outcomes, including social, behavioral, and emotional functioning. While general interest is expanding on the potential of AAI as a complementary or integrative therapy to other mental health services for different populations, there has not been a systematic review of the evidence base on AAT involving different species (canine, equine, mixed with children and adolescents (hereafter called children) who have mental health conditions or are at risk for developing such. Because the need for services among children far exceeds the availability and delivery of services, we undertook this review. The purpose of this review is to examine the state of rigorous studies on animal-assisted therapies for children with or at risk of developing mental health conditions, to synthesize findings across studies, and to identify areas for further research, thus promoting greater scientific attention to AAT.
Methods
We conducted a comprehensive database search of rigorous studies from 2000 to 2015 targeting the use of animal-assisted therapies (AAT) for children and adolescents who were at risk for mental health problems (e.g., anxiety due to a medical procedure), currently experiencing mental health problems, or who had a psychiatric diagnosis. An online search using both the PSYCinfo and Medline search systems was undertaken simultaneously, using the following terms: (Animal assist* OR animal OR horse OR equine OR hippo OR dog OR canine) AND (therapy OR intervention OR program) AND (child* OR youth OR juvenile* OR adol*) AND (emot* OR behav* OR mental* OR risk OR disorder); this search methodology replicates the recent O’Haire (2013) literature review. As shown above, search terms within each of the categories were linked with “or,” and larger categories were linked with “and” to capture studies that included at least one search term from all of the categories. Due to the variability of the two systems search limits (e.g., MEDLINE’s age limits spanned from 0–18, while PSYCINFO ranged from 0–17 years of age), the only search limit employed was publication year.
Inclusion and Exclusion Criteria
Interventions, or programs were included if they:
Were therapeutic interventions for children or adolescents 21 years or younger at risk for mental health symptoms (e.g., potential distress due to a dental procedure), currently experiencing symptoms or meeting criteria for a mental health condition.
Had been published (as journal articles or chapters) between 2000 and 2015,
Employed an experimental study design with a control or comparison group, including randomized trials, matched group designs, and designs in which the sample served as their own control,
Were part of the child or adolescent’s treatment,
Included data on outcomes, including health outcomes (e.g., motor control), mental health outcomes (e.g., depressive symptoms), and/or emotional-health (e.g., self-esteem, confidence).
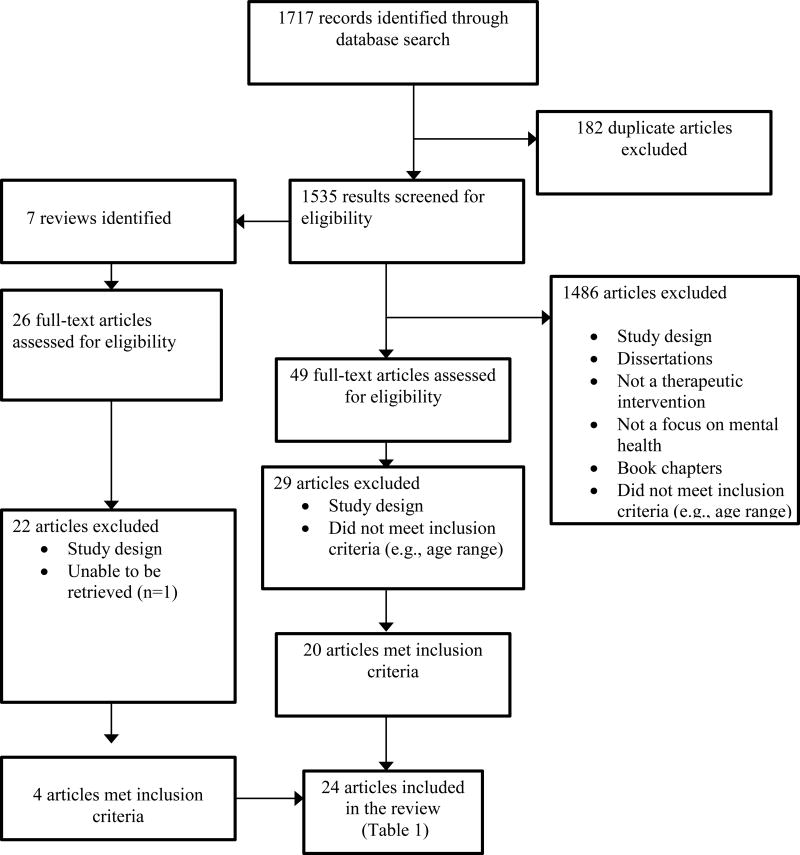
Studies were excluded if they did not have a specific focus on children’s mental health, did not have a comparison or control group, or if the intervention did not involve animals (e.g., simulated or virtual animals). See Figure 1 for the search history and results.
Figure 1.
PRISMA DIAGRAM
In order to be comprehensive, we also reviewed the bibliographies of systematic reviews identified through the computer search to identify studies that may have not been captured initially. Figure 1 presents the search history and results following the PRISMA paradigm.
Two of the authors reviewed each of the 49 original studies and 26 articles from reviews that met initial eligibility. These two authors assessed their eligibility using the inclusion criteria specified above. Discussion ensued until consensus was reached. Twenty-nine articles were excluded as original studies and 22 articles from the reviews were excluded. The remaining 24 articles met full inclusion criteria.
Data Extraction
Data were extracted and recorded for each study and included information on target population, animal utilized, study design, program description, and results. Any discrepancies were discussed among all of the authors until consensus was reached. Table 1 lists the 24 studies included in this review. To reduce variability, we grouped the studies into clusters depending on the different populations addressed by the intervention (emotional and behavioral issues, trauma and post traumatic stress disorder (PTSD), children with autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD)). Once the studies were clustered we re-reviewed the results to ensure consistent reporting.
Table 1.
Articles included in the review
| First Author | Journal | Population | Animal | Design | Program Description |
Results |
|---|---|---|---|---|---|---|
| Emotional / Behavioral Issues | ||||||
| 1. Bachi et al. (2012) | Clinical Child Psychology and Psychiatry | 29 adolescents, 14 to 18 yrs, in residential treatment. Emotional/behavioral issues. | Horse | Repeated measures, non-random assignment, matched comparison group. Follow-up data collected. | Equine Facilitated Psychotherapy (EFP). 14 to 26 weekly sessions in a horse stable. | Trend towards improvements in trust, self-control and self-image, but no significant differences between conditions. At follow-up, intervention group had fewer arrests and drug use. |
| 2. Beetz (2013) | Frontiers in Psychology | 46 children (mean age 8.5) with emotional/behavior issues (depression). | Dog | Pre/posttest with non-random assignment | School dog present for 1 day per week. Children encouraged to interact freely with her. | No significant improvements in depression in either condition. Intervention group showed significant improvements in attitudes about school and learning. |
| 3. Boshoff et al. (2015). | Journal of Psychology in Africa | Thirty-nine adolescents 14 to 18 years of age with behavior problems living in a care facility. | Horse | Solomon four-group design. | Eight sessions focusing on enhancing well-being and coping. Grooming and activities (e.g., leading horse through a path) | Significant improvements in subjective well-being, problem-focused coping, and emotion-focused coping within both groups; no significant differences between groups. No significant effect in either group with respect to dysfunctional coping. |
| 4. Conniff et al. (2005) | Anthrozoos | 23 adolescents, 13 to 17 yrs, with emotional/behavioral issues. | Multiple Animals | RCT | 8 week sessions, 1 hr per week. Interacting with animals of their choice | No significant differences between groups. |
| 5. O’Haire et al. (2015) | Anthrozoos | 128 children; 2:1 ratio of children without ASD and one child with ASD. The two children without ASD were randomly assigned to group with the child with ASD. | Guinea Pigs | RCT | Two conditions: experimental condition Vs WLC. Experimental condition consisted of two caged guinea pigs per classroom. Children were exposed to topics regarding the care of the animals, feeding, grooming, cage cleaning, health monitoring, etc.. | *Results are for children without ASD only; a separate publication (O’Haire et al 2014) reports results for children with ASD. Children in the guinea pig condition exhibited significant improvements in social skills (teacher report) and problem behaviors (teacher and parent report) in comparison to the control group. No significant changes in academic competence (teacher report) or social skills (parent support). |
| 6. Pendry et al. (2014) | Journal of Primary Prevention | 113 children, grades 5 to 8, with emotional/behavioral issues. | Horse | RCT, waitlist comparison | Equine Facilitated Learning (EFL), 11 sessions, individual and group. PATH certified instruction. | Significant improvements in social competence and behavior among the intervention group. |
| 7. Prothmann et al. (2006) | Anthrozoos | 100 children, 11–20 yrs. Emotional/behavioral issues. | Dog | Pre/posttest, non-random assignment | 5 weekly sessions. 30 minutes each. Non-directed, free play. No specific activities. | Significant improvements in mood and motivation among the intervention group. |
| 8. Trotter et al. (2008) | Journal of Creativity in Mental Health | 164 children, 3rd to 8th grades, at risk for emotional/behavioral issues. | Horse | Pre/posttest, non-random assignment | Equine Assisted Counseling (EAC), 12 weekly group sessions. | Significant improvements in both groups but greater gains in behavior among the intervention group. |
| Medical Procedures | ||||||
| 9. Barker et al. (2015) | Anthrozoos | Forty children between eight and 18 years of age who were hospitalized for medical reasons (appendicitis, abdominal pain). | Dog | RCT | Experimental condition-a 10 minute interaction with a dog, versus a jigsaw puzzle. The intervention consisted of unstructured interaction with the dog. | Children in the experimental group evidenced lower levels of anxiety in comparison to the comparison group at post; however, there were no significant differences from pre to post in either group. No significant reductions in pain across groups. |
| 10. Havener et al (2001). | Issues in Comprehensive Pediatric Nursing | 40 children, 7–11, high stress, undergoing a dental procedure. At risk for emotional/behavioral issues. | Dog | RCT | Dog as companion during dental procedure. | No significant differences in peripheral skin temperature. No significant differences in behavioral distress between groups. The presence of the dog was associated with reduced physiological arousal among children who reported distress initially.. |
| 11. Vagnoli et al. (2015) | Pain Management Nursing | 50 children between four and 11 years of age undergoing a blood draw. | Dog | RCT | Two conditions: dog or no dog during venipuncture. Dog was present in the room during the procedure. | Children in the experimental group evidenced significantly lower levels of distress and cortisol levels in comparison to the control group; no significant between group differences were found for pain ratings and parental anxiety. |
| Trauma & PTSD | ||||||
| 12. Balluerka et al. (2014) | Child & Youth Services Review | 46 adolescents, mean age 15, in residential treatment, trauma symptoms. | Multiple Animals | Pre/posttest design with non-random assignment to condition. | Animal-Assisted Therapy (AAT), 12 weeks. 2 days/week at a farm engaged in interactions with animals of their choice. | Significant differences in attachment, in favor of the intervention group (adolescents in the intervention group displayed a more secure attachment). |
| 13. Dietz et al. (2012) | Journal of Child Sexual Abuse | 153 children and adolescents, 7 to 17 yrs. Trauma symptoms. | Dog | Pre/posttest, non-random assignment. | 3 conditions. 12 weekly group sessions comparing Dogs with Stories, Dogs no stories, and No dogs. | Significant differences in anxiety, depression, anger, PTSD and dissociation, with greatest decreases in the Dogs With Stories condition. |
| 14. Hamama et al. (2011) | Child & Youth Services Review | 18 adolescents, 14–18 yrs, PTSD | Dog | Pre/posttest, non-random assignment | 12 weekly group sessions, 3 hrs per week; information, training, interaction. | Significant decrease in PTSD in intervention group. No difference between groups in depression symptoms or coping with stressful events. |
| Autism Spectrum Disorders (ASD) | ||||||
| 15. Bass et al. (2009) | Journal of Autism and Developmental Disorders | 34 children, 4 to 10 yrs, dx with ASD | Horse | RCT | Therapeutic Horseback Riding (THR), 12-week. | Significant improvements in social functioning, sensory seeking, and inattention-distractibility among intervention group. |
| 16. Fung & Leung (2014) | Journal of Contemporary Psychotherapy | 10 children between seven and 10 years of age with an ASD. | Dog | Initially stratified by age, diagnosis, and other variables and randomized to condition. | Two conditions: a baby doll and a live dog. The live dog condition was conducted over 20 weeks, during which the children played, groomed, fed and walked the dog. | Within group significant effects in social, non-social, and verbal social behaviors for the experimental group. No between group difference in social interaction, non-social behavior or verbal social behaviors. No significant within or between group change in nonsocial verbal behaviors. |
| 17. Gabriels et al. (2012) | Research in Autism Spectrum Disorders | 42 children and adolescents, 6 to 16, dx with ASD | Horse | Pre/posttest, waitlist comparison | Therapeutic Horseback Riding (THR), 10-week group sessions, PATH certified instruction. | Intervention group evidenced significant improvements in adaptive and motor skills in comparison to the control condition. |
| 18. Gabriels et al. (2015) | Journal of the American Academy of Child and Adolescent Psychiatry | One hundred twenty-seven children and adolescents between six and 16 years of age with ASD. | Horse | Initially stratified by nonverbal IQ score and randomly assigned to condition. | Two conditions: a 10-week therapeutic horseback riding program versus a barn activity control condition. | The experimental condition exhibited significant improvement in irritability, hyperactivity, social cognition, social communication, number of words and new words spoken in comparison to the control group. |
| 19. Garcia-Gomez et al. (2014) | Electronic Journal of Research in Educational Psychology | Sixteen children between the ages of seven and 16 diagnosed with an ASD. | Horse | Pre/posttest, non-random assignment | Three-month intervention, 2× week, for a total of 24 sessions lasting 45 minutes per session. | Significant within-group reduction in the experimental condition regarding aggressiveness and hyperactivity.Significant improvements in the experimental group in interpersonal relations and social inclusion in comparison to the control group. |
| 20. Jenkins et al. (2013) | Research in Autism Spectrum Disorders | 7 children and adolescents 6 to 14 yrs, dx ASD. | Horse | Multiple baseline, waitlist comparison. | Therapeutic Horseback Riding (THR), 9-weeks PATH certified instruction. | No significant differences in affect or behavior. |
| 21. Kern et al. (2011) | Alternative Therapies | Twenty-four children between three and 12 years of age with an ASD. | Horse | Within- participants, repeated-measures design. | Over the course of six months, participants rode 1 × week for 60 minutes. Intervention also included grooming and tacking. | Significant reduction in autism symptoms at three and six months of treatment. No significant differences in pre and post scores for parent-child interaction, with the exception of a slight improvement in the subscale negative regard at six months of riding, and of mood and tone, which improved significantly over three and six months of treatment. Statistically significant improvement in sensory seeking from baseline to three and six months of riding. Parents reported increase in quality of life. |
| 22. Lanning et al. (2014) | Journal of Autism and Developmental Disorders | 25 children, 5–14, dx with ASD | Horse | Repeated measures, nonrandom assignment | Equine Assisted Activities (EAA), 12 weekly sessions. | Intervention group displayed greater improvements in behavior. |
| 23. Martin & Farnum (2002) | Western Journal of Nursing Research | 10 children between three and 13 years of age diagnosed with a PDD | Dog | Within- participants, repeated-measures design. | Three conditions: 15 sessions with a ball, 15 sessions with a stuffed dog, 15 sessions with a live dog. | Children were significantly more likely to interact with the live dog (give treats, laugh more and for a longer duration, view the dog) in comparison to the other two conditions; and displayed enhanced verbal communication (e.g. talked less often about themselves than in the ball condition, talked to the talk more than the stuffed dog and ball, spent more time talking to the live dog and were less likely to talk about unrelated topics in comparison to the stuffed dog and ball). Youth were also more likely to say yes in response to a command and less likely to ignore questions in comparison to the stuffed dog condition. |
| Attention Deficit Hyperactivity Disorder | ||||||
| 24. Schuck et al. (2015) | Journal of Attention Disorders | Twenty-four children with ADHD (mean age 8.07). | Dog | RCT | Twelve-week CBT intervention with a canine-assisted intervention versus CBT without the canine-assisted intervention. Parents also participated in parent group therapy on a weekly basis. | Both groups evidenced improved social skills, positive behaviors, and reduced problem behaviors. Both groups also showed reductions in the severity of ADHD, although children in the CBT+ canine assisted intervention group showed greater decreases in symptoms. |
Results
Study Designs
Twelve studies (50%) compared the intervention to a comparison condition (Balluerka et al 2014; Bachi et al., 2012; Barker et al., 2015; Conniff et al., 2005; Dietz et al., 2012; Fung & Leung, 2014; Gabriels et al., 2015; Lanning et al., 2014; Martin & Farnum, 2002; Prothmann et al., 2006; Schuck et al., 2015; Trotter et al., 2008), including a substitute object such as a doll (Fung & Leung) or stuffed animal (Martin & Farnum, 2002); a substitute activity (e.g., a barn activity, Gabriels et al., 2015); or a therapeutic intervention without the animal component (e.g., CBT without the canine-assisted intervention, Schuck et al., 2015). The other half of the studies (n=12, 50%) compared the intervention to a control group (Bass et al., 2009; Beetz 2013; Boshoff et al., 2015; Gabriels et al., 2012; Garcia-Gomez et al., 2014; Hamama et al., 2011; Havener et al., 2001; Jenkins et al., 2013; Kern et al., 2011; O’Haire et al., 2015; Pendry et al., 2014; Vagnoli et al., 2015).
Over half (n=13, 54%) of the total number of studies did not randomly assign participants to conditions, but instead used a pretest/posttest design with non-random assignment to condition (Balluerka et al., 2014; Beetz et al., 2013; Dietz et al., 2012; Garcia-Gomez et al., 2014; Hamama et al. 2011; Prothmann et al., 2006; Trotter et al., 2008) or a waitlist comparison group (Gabriels et al., 2012); a multiple baseline design with a waitlist comparison group (Jenkins et al., 2013); a within-participants, repeated measures design (Kern et al., 2011; Martin & Farnum, 2002), a repeated measures design with a matched comparison group (Bachi et al., 2012), or a repeated measures design with nonrandom assignment to condition (Lanning et al., 2014).
The remaining 11 (46%) studies were randomized controlled trials (Barker et al., 2015; Bass et al., 2009; Boshoff et al., 2015; Conniff et al., 2005; Fung & Leung, 2014; Gabriels et al., 2015; Havener et al., 2001; O’Haire et al., 2015; Pendry et al., 2014; Schuck et al., 2015; Vagnoli et al., 2015); one of these studies utilized a Solomon Four-Group Design (Boshoff et al., 2015) and two stratified groups based upon sociodemographic variables (e.g., age, IQ, diagnosis) prior to randomization (Fung & Leung, 2014; Gabriels et al., 2015).
Target Population
The target group included youth between three and 20 years of age. Ten interventions (42%) were a combination of children and adolescents (Barker et al., 2015; Dietz et al., 2012; Gabriels et al., 2012, 2015; Garcia-Gomez et al., 2014; Jenkins et al., 2013; Lanning et al., 2014; Martin & Farnum, 2002; Trotter et al., 2008; Pendry et al., 2014), eight (33%) were interventions that included children only (Bass et al., 2009; Beetz, 2013; Fung & Leung, 2014; Havener et al., 2001; Kern et al., 2011; O’Haire et al., 2015; Schuck et al., 2015; Vagnoli et al., 2015), and six interventions (25%) included adolescents only (Balluerka et al 2014; Bachi et al., 2012; Boshoff et al., 2015; Conniff et al., 2005; Prothmann et al., 2006; Hamama et al., 2011).
Nine (38%) of the interventions were treatments for autism (Bass et al., 2009; Fung & leung, 2014; Gabriels et al., 2012, 2015; Garcia-Gomez et al., 2014; Jenkins et al., 2013; Kern et al., 2011; Lanning et al., 2014; Martin & Farnum, 2002), eight (n=7, 33%) of the interventions were treatments for youth at risk for or with identified emotional and/or behavioral problems (Bachi et al., 2012; Beetz 2013; Boshoff et al., 2015; Conniff et al., 2005; O’Haire et al., 2015; Pendry et al., 2014; Prothmann et al., 2006; Trotter et al., 2008), three (12%) addressed symptoms of trauma and PTSD (Balluerka et al., 2014; Dietz et al., 2012; Hamama et al., 2011), three (12%) were treatments for children at risk for an emotional or behavioral issue due to medical issues such as venipuncture or a dental procedure (Barker et al., 2015; Havener et al., 2001; Vagnoli et al., 2015), and one study by Schuck et al. (2015), was for children with attention-deficit hyperactivity disorder (ADHD).
Type of Animal
Eleven (46%) of the 24 studies examined equine therapies (Bachi et al., 2012; Bass et al., 2009; Boshoff et al., 2015; Gabriels et al., 2012, 2015;Garcia-Gomez et al., 2014; Jenkins et al., 2013; Kern et al., 2011; Lanning et al., 2014; Pendry et al., 2014; Trotter et al., 2008); 10 (42%) studied dog therapies (Barker et al., 2015; Beetz 2013; Dietz et al., 2012; Fung & Leung, 2014; Hamama et al., 2011; Havener et al., 2001; Martin & Farnum, 2002; Prothmann et al., 2006; Schuck et al., 2015; Vagnoli et al., 2015), and the remaining three studies (12%) tested interventions that included multiple animals, including horses, dogs, cats, rabbits, other farm animals, and guinea pigs (Balluerka et al., 2014; Conniff et al., 2005; O’Haire et al., 2015). Of the equine therapies, the therapeutic approaches varied, but most used a semi-structured curriculum called Equine Facilitated Psychotherapy, Equine Assisted Counseling, or Equine Facilitated Learning. All shared the same goal of regulating emotional or behavioral functioning. Of the studies using dogs, the primary therapeutic component was free, non-structured interaction (e.g., grooming, petting, playing). In the studies using multiple animals, the therapeutic elements were unstructured (e.g., playing with, grooming, and petting the animals).
Type of Service Setting
Three quarters (n=18, 75%) of the interventions were delivered on an outpatient basis in settings such as horse stables (e.g., Bass et al., 2009; Gabriels et al., 2015; Lanning et al., 2014), a child advocacy center (Dietz et al., 2012), a classroom (Beetz 2013; O’Haire et al., 2015), and a medical or dental office (Havener et al., 2001; Vagnoli et al., 2015). Four (17%) were part of a residential treatment program (Balluerka et al., 2014; Bachi et al., 2012; Boshoff et al., 2015; Conniff et al., 2005), one (4%) was delivered within an inpatient psychiatric program (Prothmann et al., 2006), and one (4%) in a medical hospital (Barker et al., 2015).
Types of Outcomes
Outcomes that were assessed included symptoms (e.g., trauma, behaviors), regulatory processes (e.g., emotional regulation) and functioning (e.g., general functioning at home or school, or motor functioning). Among the 11 randomized trials, three studies found significant differences between groups, in favor of the intervention group, with respect to social competence, behavior (Pendry et al., 2014), social functioning (e.g., sensory seeking, inattention-distractibility) (Bass et al., 2009), irritability, hyperactivity, social cognition, and communication (Gabriels et al., 2015). A fourth study (Schuck et al., 2015) found that both groups had reductions in ADHD symptoms, although children in the experimental condition showed a greater decrease than the comparison group. There were no other differences between groups: both showed improvements in social skills and positive behaviors, and reductions in problem behaviors.
Four of the 11 randomized clinical studies found no difference between groups in behavior and emotional functioning (Conniff et al., 2005;Fung & Leung, 2014), coping, subjective ratings of well-being (Boshoff et al., 2015), or self-reported levels of pain or anxiety. One study found a significant difference between groups regarding anxiety levels at posttest but no within-group pre/post differences (Barker et al., 2015).
Three RCTs found mixed results with no significant differences overall, but significant differences for a subset of the most distressed children (Havener et al., 2001), and significantly lower levels of distress and cortisol levels among the experimental group in comparison to the control group, but no significant between group differences regarding pain ratings and parental anxiety (Vagnoli et al., 2015). The final study, by O’Haire et al. (2015), found children in the guinea pig condition exhibited significant improvements in social skills (teacher report) and problem behaviors (teacher and parent report) in comparison to the control group. No significant changes in academic competence (teacher report) or social skills (parent support) were found, however.
Collectively, the results of the 13 (46%) controlled non-randomized studies were mixed. Five studies showed changes in the intervention group in adaptive functioning and motor skills (Gabriels et al., 2012), in mood and motivation (Prothmann, et al., 2006), in PTSD symptoms (Hamama et al., 2011), in reduced aggressiveness and hyperactivity, and improved interpersonal relations and social inclusion (Garcia-Gomez et al., 2014), and improvement in attitudes towards learning (Beetz, 2013). In the latter study, however, there was no improvement in depression (Beetz, 2013).
Four of the 13 studies found both the intervention and comparison conditions led to improvement, but the intervention group showed greater changes in trauma symptoms, anxiety, depression, and attachment (Balluerka et al., 2014; Dietz et al., 2012; Lanning et al., 2014; Trotter et al., 2008).
Two studies (Kern et al., 2011; Martin & Farnum, 2002) found significant reductions in the quality and quantity of verbal communication after exposure to the intervention (Martin & Farnum, 2002) and improvements in autism symptoms and sensory seeking, although there was no change in the quality of the parent/child interaction (Kern et al., 2011).
And, two studies (Bachi et al., 2012; Jenkins et al., 2013) did not show any significant differences between groups. Outcomes that were assessed included affect, behavior (Jenkins et al., 2013), trust, self-control and life satisfaction (Bachi et al., 2012).
Outcomes × Targeted Condition
Emotional/Behavioral Problems
Eight studies targeted emotional or behavioral problems; of them, four were RCTs. Results of two of the four RCTs were non-significant in terms of behavior or emotional state (e.g. self-reported loneliness, anger or boredom (Conniff et al., 2005) and coping and subjective well-being (Boshoff et al., 2015). The third RCT, by Pendry et al. (2014), found significant differences in favor of the intervention group with respect to social competence and behavior, while the fourth, by O’Haire et al. (2015), found significant improvements in social skills based on teacher, but not parent report, and reductions in problem behaviors based upon both teacher and parent report, but no significant changes in academic competence based upon teacher report.
Among the four non-RCT controlled studies, one found significant improvements in alertness in the intervention group (Prothmann et al., 2006). Two studies found no differences between groups, although greater gains in the intervention group (Bachi et al 2012; Trotter et al., 2008). The fourth study found mixed results: neither the intervention nor the comparison group showed improvements in depression, although the intervention group demonstrated significant improvements in attitudes about school and learning (Beetz, 2013).
At Risk
Three studies, all RCTs, examined the impact of AAT upon children either experiencing a medical or dental procedure (Havener et al., 2001; Vagnoli et al., 2015), or who were hospitalized for a medical condition (Barker et al. (2015). Results of one of the three RCTs were non-significant in terms of behavioral distress, or physiological arousal, an indicator of stress (Havener et al., 2001), a second RCT found children in the experimental group evidenced significantly lower levels of distress and cortisol levels, but no significant between group differences were found for pain ratings and parental anxiety (Vagnoli et al., 2015), and the third RCT, by Barker et al. (2015), showed children in the experimental group had lower levels of anxiety at post; however, there were no significant differences in anxiety from pre to post in either group. Nor were there any significant reductions in pain across groups.
Autism Spectrum Disorder
Nine studies examined interventions for autism spectrum disorders (ASD) (Bass et al., 2009;Fung & Leung, 2014; Gabriels et al., 2012, 2015; Garcia-Gomez et al., 2014; Jenkins et al., 2013; Kern et al., 2011; Lanning et al., 2014; Martin & Farnum, 2002). Of them, three studies (Bass et al., 2009;Fung & Leung, 2014; Gabriels et al., 2015) were RCTs. Designs for the six remaining studies were pre/post, multiple baseline, and repeated measures designs with non-random assignment to either a comparison group (Lanning et al., 2014), a control group or a waitlist condition (Gabriels et al., 2012; Garcia-Gomez et al., 2014; Jenkins et al., 2013), or a within-participants design (Kern et al., 2011; Martin & Farnum, 2002).
Five out of the nine studies favored the intervention, as they found significant improvements in social functioning, sensory seeking and distractability (Bass et al., 2009), behavior (Lanning et al., 2014), adaptive and motor skills (Gabriels et al., 2012), irritability, hyperactivity, social cognition and communication, and verbal communication (Gabriels et al., 2015), and verbal communication and interaction (Martin & Farnum, 2002).
Two studies were partially supportive of the intervention; the first found significant symptom reduction and improvement in sensory seeking over time, but no impact of the intervention upon parent-child interaction, with the exception of two subscales (negative regard, mood and tone), which improved over time. Further, parents reported an increase in their quality of life (Kern et al., 2011). The second study found those in the intervention group experienced significant reductions in aggressiveness and hyperactivity over time, and significant between group differences with respect interpersonal relations and social inclusion (Garcia-Gomez et al., 2014). Fung and Leung (2014) and Jenkins et al. (2013) found no significant improvements relative to the intervention.
Attention Deficit Hyperactivity Disorder (ADHD)
One study examined AAT for ADHD using an RCT design. Both the experimental and the control groups demonstrated improved social skills, positive behaviors, and reduced problem behaviors. Both groups also showed reductions in the severity of ADHD, although children in the experimental intervention group showed greater decreases in symptoms (Schuck et al., 2015).
Trauma and PTSD
Three studies (21.4%) examined AATs for trauma symptoms (Balleurka et al., 2014); Dietz et al., 2012) or PTSD (Hamama et al., 2011). All three favored in the intervention. All used a pre/post design with non-random assignment to condition. Of them, two found significant improvements in attachment (Balluerka et al., 2014), anxiety, depression, anger, PTSD, and dissociation (Dietz et al., 2012); the third found significant reductions in PTSD in the intervention group, although there was no difference in depression symptoms or coping between groups (Hamama et al., 2011).
Discussion
It has been noted many times that there is a huge gap between children’s need for services, based on the startling rise in prevalence of many mental health conditions (National Academies of Sciences, Engineering, and Medicine, 2015) and the proportion of those in need who have access to effective services. This is not new. This fact, however, lends greater urgency to the importance of developing a robust evidence base on complementary and integrative services that may narrow this gap.
A promising new line of research is focusing on animal-assisted therapies as an augmentation to traditional therapies for children. What this review uncovers is that the number of studies that meet inclusion criteria for rigorous designs is growing rapidly. Of the 24 studies we identified in the past 15 years, almost half used the gold standard of RCTs (46%, N=11) and of those eleven, nine were published in the past two years.
This review also showed that the age range, settings, and types of conditions that are being studied are broad and reflect an important population of children in need of mental health services: the studies covered both children and adolescents across the age spectrum, in both inpatient and outpatient settings, and with both diagnostically-specific (ADHD, autism), syndromal (trauma, emotional or behavioral problems), and at-risk conditions. This bodes well for further development of a useful knowledge base.
The types of animals that were most often used in these studies were fairly evenly split between horses and dogs, although multiple animals and other species (guinea pigs) were also being used therapeutically. This too is a positive trend suggestive of a broadening and deepening of the empirical foundation.
However, it is clear that establishment of AAT as an “evidence-based practice” that will meet criteria such as those developed by the American Academy of Child and Adolescent Psychiatry (AACAP, 2015), the American Academy of Pediatrics (AAP, 2015), The Substance Abuse and Mental Health Services Administration’s (SAMHSA) National Registry of Evidence-Based Programs and Practices (SAMHSA, 2015), or the Blueprints for Healthy Youth Development (University of Colorado at Boulder, 2015), awaits much more focused scientific attention. Of the 24 studies, 8 (33%) demonstrated positive effects associated with the active condition, 10 (42%) showed either mixed effects or an absence of a differential effect but a decrease in symptoms; and 6 (25%) demonstrated no effect. So the answer to the question is AAT effective for children with mental health conditions cannot be answered right now. The findings are promising, however, and suggestive of impact under certain conditions, with certain populations, and with clearly delineated procedures (manuals).
The mental health conditions with the strongest evidence presently are equine therapy for autism and canine therapy for trauma. Five of nine studies for autism showed positive effects favoring the intervention (Bass et al., 2009; Lanning et al., 2014; Gabriels et al., 2012; Gabriels et al., 2015; Martin & Farnum, 2002). Four of those used a horse and one study (Martin) a dog. Three out of three studies for trauma (Baluerka et al., 2014; Dietz et al., 2012; Hamama et al., 2011) showed positive effects, all using a dog. Of course, this is still a very small number of studies on which to base conclusions, but there is at least a signal that a targeted AAT for children’s autism and for trauma is likely to yield positive findings.
Strengthening the research base
To strengthen the knowledge base on AAT in children’s mental health, we suggest five avenues for examination. First, developing an empirical basis for a new type of modality such as AAT, however, requires more than controlled studies: as Kazdin and others have repeatedly pointed out, understanding the mechanisms of action that lead to a positive effect is critical (Kazdin 2007; Kazdin & Blasé, 2011). None of the studies thus far have attempted to address mechanisms of the therapeutic process. Second, comparative animal studies are needed to examine whether there are specific processes related to particular species that lead to change, or whether it is broadly the human-animal interaction. For instance, horses provide an opportunity for attachment and emotional bonding but also for muscle and motor activity. This is not true for dogs. So, perhaps for children with some disorders (i.e., autism), the ability to have direct motoric connectivity is uniquely advantageous.
Third, there is a need for studies to address outcomes that can be linked more directly to well-developed theories. The review by Amiot & Bastian (2015) identified psychological processes related to the interdependence of humans and animals, and described theories to structure the processes and outcomes. Few of the studies reviewed integrated theories with specifiable program elements or with precise measurement of outcomes. This is a limitation in the field, and one that will hinder further scientific advancement if not addressed. Fourth, there is considerable potential for studies to embed measures of psychophysiologic arousal (cortisol) and well-being (oxytocin) into these trials. Promising work by Beetz et al (2012) and Julius et al (2013) suggest that these arousal and regulatory processes may be important ways of understanding HAI. Finally, there is a clear need for specificity of interventions with manuals that outline explicit procedures and processes. We found few studies that specifically included a manual. In their absence, these interventions cannot be replicated.
Conclusion
Animal assisted therapies for children with or at risk for developing mental disorders are a complementary and integrative therapeutic approach with limited, but growing scientific support. A handful of studies suggest that for certain types of problem areas – autism and trauma – a structured therapeutic intervention using either horses or dogs may lead to improved functioning. Five areas for further research include attention to mechanisms of change, comparative animal studies, theories to explicate processes and outcomes, inclusion of psychophysiological measures, and replication. Despite the limitations in the evidence base, given the high levels of unmet need among children with mental health and developmental disabilities and the extreme shortage of available and effective treatments for children, expansion of the research base on AAT is both promising and has high public health salience.
Acknowledgments
Funded by The National Institute of Mental Health, 5P30MH090322-04
References
- American Academy of Child and Adolescent Psychiatry. Practice Parameters. 2015 Retrieved from http://www.jaacap.com/content/pracparam on October 14, 2015.
- American Academy of Pediatrics. Evidence-based Child and Adolescent Psychosocial Interventions. 2015 Retrieved from: https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Mental-Health/Pages/default.aspx on October 14, 2015.
- Amiot CE, Bastian B. Toward a psychology of human-animal relations. Psychology Bulletin. 2015;141(1):6–47. doi: 10.1037/a0038147. [DOI] [PubMed] [Google Scholar]
- Anestis MD, Anestis JC, Zawilinski LL, Hopkins TA, Lilienfeld SO. Equine-related treatments for mental disorders lack empirical support: a systematic review of empirical investigations. Journal of Clinical Psychology. 2014;70(12):1115–32. doi: 10.1002/jclp.22113. [DOI] [PubMed] [Google Scholar]
- Bachi K, Terkel J, Teichman M. Equine-facilitated psychotherapy for at-risk adolescents: The influence on self-image, self-control, and trust. Clinical Child Psychology and Psychiatry. 2012;2:298–312. doi: 10.1177/1359104511404177. [DOI] [PubMed] [Google Scholar]
- Balluerka N, Muela A, Amiano N, Caldentey MA. Influence of animal-assisted therapy (AAT) on the attachment representations of youth in residential care. Children and Youth Services Review. 2014;42:103–109. [Google Scholar]
- Barker SB, Knisely JS, Schubert CM, Green JD, Ameringer S. The Effect of an Animal-Assisted Intervention on Anxiety and Pain in Hospitalized Children. Anthrozoos: A Multidisciplinary Journal of The Interactions of People & Animals. 2015;28(1):101–112. [Google Scholar]
- Bass MM, Duchowny CA, Llabre MM. The effect of therapeutic horseback riding on social functioning in children with autism. Journal of Autism and Developmental Disorders. 2009;39(9):1261–1267. doi: 10.1007/s10803-009-0734-3. [DOI] [PubMed] [Google Scholar]
- Beetz A, Uvnäs-Moberg K, Julius H, Kotrschal K. Psychosocial and Psychophysiological Effects of Human-Animal Interactions: The Possible Role of Oxytocin. Frontiers in Psychology. 2012;3:234. doi: 10.3389/fpsyg.2012.00234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beetz A. Socio-emotional correlates of a schooldog-teacher-team in the classroom. Frontiers in Psychology. 2013;4:886. doi: 10.3389/fpsyg.2013.00886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boshoff C, Grobler H, Nienaber A. The evaluation of an equine-assisted therapy programme with a group of boys in a youth care facility. Journal of Psychology in Africa. 2015;25(1):86–90. [Google Scholar]
- Bruns EJ, Kerns SE, Pullmann MD, Hensley S, Lutterman T, Hoagwood KE. Research, Data, and Evidence-Based Treatment Use in State Behavioral Health Systems 2001–2012. Psychiatric Services. doi: 10.1176/appi.ps.201500014. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorpita BF, Weisz JR, Daleiden EL, Schoenwald SK, Palinkas LA, Miranda J, Higa-McMillan CK, Nakamura BJ, Austin AA, Borntrager C, Ward AM, Wells KC, Gibbons RD, the Research Network on Youth Mental Health Long term outcomes for the Child STEPs randomized effectiveness trial: A comparison of modular and standard treatment designs with usual care. Journal of Consulting and Clinical Psychology. 2013;81:999–1009. doi: 10.1037/a0034200. [DOI] [PubMed] [Google Scholar]
- Conniff KM, Scarlett JM, Goodman S, Appel LD. Effects of a pet visitation program on the behavior and emotional state of adjudicated female adolescents. Anthrozoos: A Multidisciplinary Journal of The Interactions of People & Animals. 2005;18(4)(17):379–395. [Google Scholar]
- Cooper JL, Aratani Y, Knitzer J, Douglas-Hall A, Masi R, Banghart P, Dababnah S. Unclaimed Children Revisited: The Status of State Children's Mental Health Service Systems. National Center for Children in Poverty, Mailman School of Public Health; Columbia University: 2008. [Google Scholar]
- Dietz TJ, Davis D, Pennings J. Evaluating animal-assisted therapy in group treatment for child sexual abuse. Journal of Child Sex Abuse. 2012;21(6):665–83. doi: 10.1080/10538712.2012.726700. [DOI] [PubMed] [Google Scholar]
- Fung S, Leung AS. Pilot Study Investigating the Role of Therapy Dogs in Facilitating Social Interaction among Children with Autism. Journal of Contemporary Psychotherapy. 2014;44(4):253–262. [Google Scholar]
- Gabriels RL, Agnew JA, Holt KD, Shoffner A, Zhaoxing P, Ruzzano S. Pilot study measuring the effects of therapeutic horseback riding on school-age children and adolescents with autism spectrum disorders. Research in Autism Spectrum Disorders. 2012;6(2):578–588. [Google Scholar]
- Gabriels RL, Pan Z, Dechant B, Agnew JA, Brim N, Mesibov G. Randomized Controlled Trial of Therapeutic Horseback Riding in Children and Adolescents With Autism Spectrum Disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54(7):541–9. doi: 10.1016/j.jaac.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Gomez A, Risco LM, Rubio JC, Guerrero E, Garcia-Pena IM. Effects of a Program of Adapted Therapeutic Horse-riding in a Group of Augitsm Spectdrium Disorder Children. Electronic Journal of Research in Educational Psychology. 2014;12(1):107–128. [Google Scholar]
- Hamama L, Hamama-Raz Y, Dagan K, Greenfeld H, Rubinstein C, Ben-Ezra M. A preliminary study of group intervention along with basic canine training among traumatized teenagers: A 3-month longitudinal study. Children and Youth Services Review. 2011;33(10):1975–80. [Google Scholar]
- Havener L, Gentes L, Thaler B, Megel ME, Baun MM, Driscoll FA, Beiraghi S, Agrawl N. The effects of a companion animal on distress in children undergoing dental procedures. Comprehensive Pediatric Nursing. 2001;24(2):137–152. doi: 10.1080/01460860118472. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Improving the Quality of Health Care for Mental and Substance-Use Conditions. Quality Chasm Series. Washington DC: National Academies Press; 2006. Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders. [Google Scholar]
- International Association of Human-Animal Interaction Organizations. White Paper 2014: The IAHAIO Definitions for Animal Assisted Intervention and Guidelines For Wellness of Animals Involved. 2014 Retrieved from: http://www.iahaio.org/new/fileuploads/4163IAHAIO%20WHITE%20PAPER-%20FINAL%20-%20NOV%2024-2014.pdf on October 14, 2015.
- Jenkins SR, DiGennaro Reed FD. An experimental analysis of the effects of therapeutic horseback riding on the behavior of children with autism. Research in Autism Spectrum Disorders. 2013;7:721–740. [Google Scholar]
- Julius H, Beetz A, Kotrschal K, Turner DC, Uvnäs-Moberg K. Attachment to Pets: An Integrative View of Human-Animal Relationships with Implications for Therapeutic Practice. Hogrefe Publishing; Cambridge, MA: 2013. [Google Scholar]
- Kamioka H, Okada S, Tsutani K, Park H, Okuizumi H, Handa S, Oshio T, Park SJ, Kitayuguchi J, Abe T, Honda T, Mutoh Y. Effectiveness of animal-assisted therapy: A systematic review of randomized controlled trials. Complementary Therapies in Medicine. 2014;22(2):371–90. doi: 10.1016/j.ctim.2013.12.016. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Blasé SL. Rebooting Psychotherapy Research and Practice to Reduce the Burden of Mental Illness. Perspectives on Psychological Science. 2011;6(1):21–37. doi: 10.1177/1745691610393527. [DOI] [PubMed] [Google Scholar]
- Kern JK, Fletcher CL, Garver CR, Mehta JA, Grannemann BD, Knox KR, Richardson TA, Trivedi MH. Prospective trial of equine-assisted activities in autism spectrum disorder. Alternative Therapies in Health and Medicine. 2011;17(3):14–20. [PubMed] [Google Scholar]
- Knitzer J, Olson L. Unclaimed Children: The Failure of Public Responsibility to Children and Adolescents in Need of Mental Health Services. The Children’s Defense Fund; Washington, D.C.: 1982. [Google Scholar]
- Lanning BA, Baier ME, Ivey-Hatz J, Krenek N, Tubbs JD. Effects of Equine assisted activities on Autism Spectrum Disorder. Journal of Autism andDevelopmental Disorders. 2014;44(8):1897–1907. doi: 10.1007/s10803-014-2062-5. [DOI] [PubMed] [Google Scholar]
- Martin F, Farnum J. Animal-assisted therapy for children with pervasive developmental disorders. Western Journal of Nursing Research. 2002;24(6):657–670. doi: 10.1177/019394502320555403. [DOI] [PubMed] [Google Scholar]
- McCarthy J, Le LT. Financing Behavioral Health Services and Supports for Children, Youth and Families in the Child Welfare System. Washington, DC: Georgetown University Center for Child and Human Development, National Technical Assistance Center for Children’s Mental Health; 2008. [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. Mental disorders and disabilities among low-income children. Washington, DC: The National Academies Press; 2015. [PubMed] [Google Scholar]
- O’Haire ME. Animal-assisted intervention for autism spectrum disorder: A systematic literature review. Journal of Autism and Developmental Disorders. 2013;43(7):1606–1622. doi: 10.1007/s10803-012-1707-5. [DOI] [PubMed] [Google Scholar]
- O'Haire ME, McKenzie SJ, McCune S, Slaughter V. The Journal of Alternative and Complementary Medicine. 2014;20(3):162–168. doi: 10.1089/acm.2013.0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Haire ME, McKenzie SJ, Beck AM, Slaughter V. Animals may act as social buffers: Skin conductance arousal in children with autism spectrum disorder in a social context. Developmental Psychobiology. 2015;57(5):584–95. doi: 10.1002/dev.21310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patient Accountability and Affordability Act. 2010 Retrieved from http://www.gpo.gov/fdsys/pkg/PLAW-111publ148/pdf/PLAW-111publ148.pdf on June 1, 2015.
- Pendry P, Carr AM, Smith AN, Roeter SM. Improving adolescent social competence and behavior: a randomized trial of an 11-week equine facilitated learning prevention program. Journal of Primary Prevention. 2014;35(4):281–93. doi: 10.1007/s10935-014-0350-7. [DOI] [PubMed] [Google Scholar]
- Prothmann A, Biernet M, Ettrich C. Dogs in child psychotherapy: Effects on state of mind. Anthrozoos. 2006;19(3):265–277. [Google Scholar]
- Schuck SE, Emmerson NA, Fine AH, Lakes KD. Canine-assisted therapy for children with ADHD: Preliminary findings from The Positive Assertive Cooperative Kids Study. Journal of Attention Disorders. 2015;19(2):125–137. doi: 10.1177/1087054713502080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Transforming Mental Health Care in America. The Federal Action Agenda: First Steps. Rockville, MD: United States Department of Health and Human Services; 2005. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) National Registry of Evidence-Based Programs and Practices (NREPP) 2015 Retrieved from http://nrepp.samhsa.gov/Index.aspx on October 14, 2015.
- Trotter K, Chandler C, Goodwin-Bond D, Casey J. A comparative study of the efficacy of group equine assisted counseling with at-risk children and adolescents. Journal of Creativity in Mental Health. 2008;3(3):254–284. [Google Scholar]
- University of Colorado at Boulder. Blueprints for Healthy Youth Development. 2015 Retrieved on October 14, 2015 from http://blueprintsprograms.com.
- U.S. Department of Health and Human Services. Mental Health: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; 1999. [Google Scholar]
- U.S. Public Health Service. Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda. Washington DC: Department of Health and Human Services; 2000. [Google Scholar]
- Vagnoli L, Caprilli S, Vernucci C, Zagni S, Mugnai F, Messeri A. Can presence of a dog reduce pain and distress in children during venipuncture? Pain Management Nursing. 2015;16(2):89–95. doi: 10.1016/j.pmn.2014.04.004. [DOI] [PubMed] [Google Scholar]