Abstract
Isolated brain tumors contain cells that exhibit stem cell features and a tissue microenvironment bearing remarkable similarities to the normal neurogenic niche. This supports the idea that neural stem (NSCs) or progenitor cells, and their progeny are the likely tumor cell(s) of origin. This prompted the investigation of the relationship between NSCs/progenitors and the initiation of tumorigenesis. These studies led to the identification of common signaling machineries underlying NSC development and tumor formation, particularly those with known roles in proliferation and cell fate determination. This review will explore the molecular mechanisms that regulate NSC behavior in the neurogenic niche of the forebrain, and how deregulation of the developmental potential of NSCs might contribute to tumorigenesis.
Overview of the Neurogenic and Tumorigenic Niche
The neurogenic niche is a highly dynamic and complex microenvironment where new neurons or glial cells are generated from stem or progenitor cells. The primary role of the neurogenic niche is to promote a favorable environment for self-renewal and maintenance of neural stem/progenitor cell populations. Specifically, the niche provides signals that determine whether stem cells should remain quiescent, actively divide, or differentiate into specific precursor or postmitotic cell lineages capable of integrating into existing neuronal networks. There are a number of neurogenic niches in the developing and postnatal central nervous system, all of which possess distinct properties to produce region-specific progenies. This review will draw on the extensive studies conducted in the mouse ventricular/subventricular (V-SVZ) neurogenic niche of the mammalian cerebral cortex to examine the similarities and differences between the neurogenic and tumorigenic niche.
The mouse V-SVZ neurogenic niche is a highly heterogenous structure found along the striatal walls of the lateral ventricles with the ependymal cell lining along the cerebrospinal fluid (CSF)-filled ventricles and a rich vascular plexus on the opposite side defining its borders (Figure 1). It contains NSCs, or type B cells, that are distinguished based on their quiescent (qNSC) or actively dividing (aNSC) states. aNSCs may self-renew to maintain the qNSC or aNSC population within the V-SVZ, or they may divide to generate the lineage-restricted Type C transit-amplifying progenitors. Type C cells undergo several rounds of cell division to eventually give rise to either neuroblasts (Type A cells) or glial cells (oligodendrocytes or astrocytes) (Doetsch et al., 1999). Olig2+ Type C cells may differentiate into NG2 glia and myelinating oligodendrocytes that subsequently integrate into the corpus callosum, striatum, and fimbria fornix (Menn et al., 2006). On the other hand, Type A neuroblasts form into long chains, with the help of ensheathing astrocytes and the vasculature, to migrate towards the olfactory bulb. There, Type A cells will terminally differentiate into functional interneurons that will ultimately integrate into the existing circuitry (Lim and Alvarez-Buylla, 2016).
Figure 1.
Schematic Diagram of the Ventricular-Subventricular Zone (V-SVZ) Neurogenic Niche. Quiescent and activated neural stem cells (NSC) interact closely with other cell types within the V-SVZ such as the ependymal cells, endothelial cells, pericytes, postmitotic neurons, oligodendrocytes, and astrocytes. Additionally, since NSCs line the lateral ventricles, these cells are in contact with factors present in the cerebrospinal fluid (CSF). The result of these interactions contributes to the proliferative and differentiation capacities of NSCs, which is capable of self-renewal and the generation of lineage-specific transit amplifying cells that will either proliferate or differentiate into neurons or glial cell types.
The cytoarchitecture of the mouse V-SVZ and its location within the forebrain promote and maintain the self-renewing properties of NSCs and their progenies. It is therefore not surprising to find that the tumorigenic niche adopts these similar properties to promote the proliferation of tumorigenic or brain tumor stem cells (BTSC) and maintain their “stemness” (Singh et al., 2004). BTSCs possess properties that are highly characteristic of NSCs such as the ability to self-renew, divide, and differentiate into distinct cell lineages. Indeed, tumor invasiveness, recurrence, or overall poor survival of patients with glioblastoma multiforme (GBM) can be predicted based on the proximity of the tumors to the SVZ (Jafri et al., 2013; Lim et al., 2007), or whether tumors are in contact with the lateral ventricle (Mistry et al., 2016). Similar to the neurogenic niche, a characteristic signature of brain tumors are their highly vascular nature (Calabrese et al., 2007; Wesseling et al., 1993) and increased vascular density has long been considered a prognostic indicator of malignant tumor progression (Calabrese et al., 2007; Leon et al., 1996) (Figure 2). Indeed, factors released by blood vessels and other niche-associated cells are integral to the survival of both NSCs and BTSCs and in maintaining the structural organization of the niche. In the following sections, we will discuss examples of how the neurogenic and tumorigenic niche provides the trophic support necessary to maintain the proliferative properties of both NSCs and BTSCs.
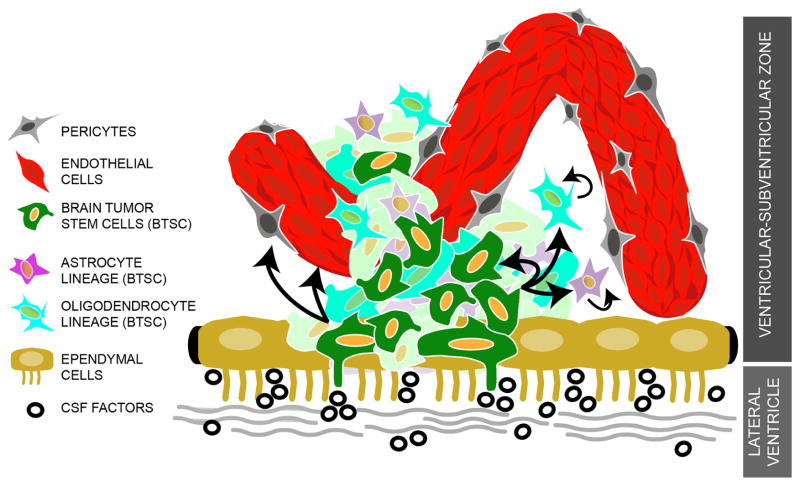
Figure 2.
Schematic Diagram of the Tumorigenic Niche. Brain tumor stem cells (BTSC) interact closely with niche components that include factors released by the endothelial cells that make up the enhanced tumor vasculature, pericytes, and other tumor cell types. In cases where BTSCs are in close contact with the lateral ventricles, these cells may also be receptive to the same diffusible factors present in the CSF. The result of these interactions could have similar effects on the behavior of BTSCs, as it does on normal NSCs, such as the enhancement of BTSCs to self-renew and generate lineage-specific tumor cells (including the ability to generate endothelial cells) resulting in the aberrant expansion and invasiveness of a highly heterogeneous brain tumor.
The Crossroads of NSC and BTSC Proliferation
Sources of trophic factors that maintain NSCs in the V-SVZ not only include the NSCs or postmitotic cells, or the vascular network within the V-SVZ, but also include the cerebrospinal fluid (CSF). These molecules dictate the rate at which qNSCs stay quiescent, switch to an activated state, and the overall cell cycle dynamics of aNSCs. We refer the reader to recently published reviews that provide excellent information on the crucial factors involved in the development and maintenance of the neurogenic niche of the adult brain, including the V-SVZ (Bjornsson et al., 2015; Choe et al., 2016). In this review, we will summarize the roles of molecules that have been specifically implicated in the proliferation of NSCs and BTSCs.
Shh signaling is widely known for its mitogenic effect on proliferative cells throughout development (Sousa and Fishell, 2010), a role that is maintained in the postnatal V-SVZ (Choe et al., 2016). Shh ligands, originating from the CSF or nearby mature neurons, activate the Shh signaling pathway to induce proliferation of activated and quiescent Type B cells possibly by altering the of the cell cycle dynamics of qNSCs and aNSCs via Gli repressor activity (Ahn and Joyner, 2005; Balordi and Fishell, 2007; Daynac et al., 2016; Ihrie et al., 2011; Lehtinen et al., 2011; Machold et al., 2003; Petrova et al., 2013). Upregulation of Shh signaling pathway has been repeatedly observed in glioblastoma where it has also been found to potently synergize with key signaling pathways such as the phosphatidylinositol 3-kinase (PI3K) signaling to promote tumor growth (Bar et al., 2007; Becher et al., 2008; Chandra et al., 2015; Ehtesham et al., 2007; Gruber Filbin et al., 2013; Xu et al., 2008). In specific glioblastoma subtypes, Shh signaling affected BTSC proliferation and self-renewal, and could be suppressed upon treatment with Gli1-targeting siRNA or pharmacological inhibitors of Shh signaling (Bar et al., 2007; Ehtesham et al., 2007; Gruber Filbin et al., 2013; Xu et al., 2008).
Wnt ligands are found in the CSF and expressed by mature neurons or astrocytes within or near the SVZ. Activated Wnt signaling in Wnt-responsive Type B and Mash1+ Type C cells leads to increased proliferation and self-renewal (Adachi et al., 2007; Qu et al., 2010). The crucial roles of both canonical and non-canonical Wnt signaling in proliferation, particularly in stem and progenitor cells across various tissue types (Clevers et al., 2014), has established Wnt signaling as a critical force in tumor growth (Holland et al., 2013; Klaus and Birchmeier, 2008; Nusse, 2008; Polakis, 2012; Ring et al., 2014). In brain tumors, particularly in glioblastoma, aberrant Wnt activation is a hallmark of BTSC malignant transformation and high levels of Wnt activity correlate with dismal clinical outcomes (Sandberg et al., 2013; Schüle et al., 2012). Wnt signaling exerts this effect largely by maintaining the stem cell properties of BTSCs. Amplification of Wnt signaling in BTSCs is typically achieved via genetic mutations or alterations in upstream regulators, such as PLAGL2 or FoxM1, or through degulation of epigenetic states in BTSCs that render these cells highly responsive to Wnt signals (Gong and Huang, 2012; Rheinbay et al., 2013; Zhang et al., 2011; Zheng et al., 2010).
Targeting GPCR signaling has become an active area of research in the development of glioblastoma treatments (Cherry and Stella, 2014). Understanding the roles of factors that influence GPCR signaling in maintaining the neurogenic niche could prove helpful in this endeavor. With recent successes in the prospective identification and purification of qNSCs and aNSCs (Codega et al., 2014; Mich et al., 2014), GPCR signaling ligands, Sphingosine-1-Phosphate (S1P) and Prostaglandin D2, also found in the CSF, have been found to maintain the quiescent state of qNSCs (Codega et al., 2014). To date, very little is known about the role of Prostaglandin D2 in neurogenesis and in BTSCs. On the other hand, S1P, which is also secreted by endothelial cells, is known to promote neurogenesis during embryonic development (Mizugishi et al., 2005). In glioblastoma stem cells, S1P signaling is an emerging player as studies indicate important roles of activated S1P signaling in regulating the stemness and invasive qualities of BTSCs, albeit there are a number of conflicting findings. Linking its role in maintaining NSC quiescence in the V-SVZ, downregulation of S1P expression has been correlated with enhanced glioblastoma malignancy and shorter patient survival (Yoshida et al., 2010a, 2010b). However, another set of studies had opposite findings and showed that high S1P expression correlated with poor survival (Quint et al., 2014). Thus, whether S1P signaling promotes or inhibits BTSC proliferation is yet to be clarified (Van Brocklyn et al., 2005; Riccitelli et al., 2013).
Proliferation of NSCs is also dependent on the vascular network within the neurogenic niche, which provides a broad number of growth factors and facilitates important cell-cell interactions that lead to NSC self-renewal. Perivascular signals induce stem and progenitor cell proliferation by releasing factors that activate mitogenic pathways such as nitric oxide signaling, purinergic signaling, vascular endothelial growth factor (VEGF), and Pigment Epithelium-Derived Factor (PEDF) signaling (Goldman and Chen, 2011). In GBM, tumor cells are highly dependent on the extensive vascular network and co-opt the same signaling mechanisms that govern vasculogenesis (Jhaveri et al., 2016). These signaling pathways are significantly augmented, leading to highly proliferative tumor cells. Furthermore, BTSCs also exert paracrine effects, such as the release of VEGF or stromal cell-derived factor 1 (SDF-1) to stimulate vasculogenesis within the tumorigenic niche by recruiting more endothelial cells into the tumor site or inducing increased proliferation (Jhaveri et al., 2016). As will be discussed below, BTSCs may also differentiate into functional endothelial cells that also contribute to the growth of the vascular network in tumors. Taken together, these data highlights how tumor growth and invasiveness are influenced by the relationship between tumorigenic cells and the vascular network within the niche.
The Crossroads between NSC Fate Specification and Tumorigenesis
The spatial organization of NSCs within the V-SVZ dictates the types of glial or neuronal cell lineages it will produce. For example, Type B cells located along the ventral V-SVZ produce transit amplifying Type C cells that generate Calbindin-positive interneurons and deep granule neurons in the olfactory bulb whereas Type B cells in the dorsal V-SVZ and subcallosal zones divide into Type C cells that produce Tyrosine Hydroxylase (TH)-positive and superficial granule neurons (Merkle et al., 2007; Ventura and Goldman, 2007). In recent years, evidence that specific glial lineages are also generated in a region-specific manner is emerging. For example, subcallosal V-SVZ region generates oligodendroglial cells that eventually migrate into the corpus callosum (Tong et al., 2015). Thus, the positioning of NSCs prime these cells to produce distinct lineages, indicating that the environmental cues are likely to be major determinants of cell fate. Not surprisingly, a number of factors that are known to regulate NSC fate specification also influence the cellular heterogeneity observed in specific glioblastoma subgroups likely due to the same environmental cues that may be enriched or absent within the tumorigenic niche. Adult V-SVZ NSCs or progenitors are the proposed source of gliomas with a number of studies showing that oligodendrocyte precursor cells (OPCs) as the cell of origin (Alcantara Llaguno et al., 2015; Alcantara Llaguno et al., 2009; Galvao et al., 2014; Liu et al., 2011). Thus, lineage-restricted control mechanisms of V-SVZ NSCs are now being examined for its role in tumorigenesis.
Both EGFR and PDGFRα signaling are critical in the proliferation and specification of adult progenitors towards the oligodendroglial lineage. Activation of EGFR signaling in a subpopulation of Type B and Type C cells results in increased proliferation and may exert this effect by interacting with Notch signaling (Aguirre et al., 2010; Doetsch et al., 2002). Numerous studies have shown that mutations in EGFR disrupt oligodendrogenesis in V-SVZ progenitors whereas its amplification accelerate the generation of oligodendrocytes (Gonzalez-Perez and Alvarez-Buylla, 2011). PDGFR signaling is also critical in the proliferation and specification of Type B cells by largely directing the differentiation of these cells towards the oligodendroglial lineage (Jackson et al., 2006). Local sources of PDGFR ligands are the vascular-associated cells, CSF, and postmitotic neurons (Betsholtz, 1995). Cells expressing EGFR ligands (EGF, fibroblast growth factor 2 (FGF2), or transforming growth factor alpha (TGFα)) within the V-SVZ is relatively low and instead the primary source of these ligands is likely the choroid plexus, which release these factors into the CSF (Bjornsson et al., 2015).
Amplification of both EGFR and PDGFR expression and signaling is a hallmark of major subtypes of gliomablastoma and leads to the expansion of tumorigenic cells and increased malignancy. For example, overexpression of PDGF in glial and neural progenitors that reside in the V-SVZ resulted in malignant gliomas (Dai et al., 2001; Jackson et al., 2006; Lindberg et al., 2009). Furthermore, increased expansion and malignancy correlated with the acquisition of oligodendroglial phenotypes. Investigating how the acquisition of gliogenic cell properties contributes to the progression and malignancy of gliomas could provide important pathways towards developing targeted therapies. Another possibility is that the molecular properties of neural stem and progenitor cells destined towards the glial lineage are more susceptible to oncogenic mutations, many of which can trigger enhanced proliferation, that lead to specific glioblastoma subtypes (Visvader, 2011), likely because glial progenitors such as OPCs persists and are abundant into adulthood (Geha et al., 2010). This is certainly the case for EGFR and PDGFR signaling, which is capable of driving both proliferation and specification of NSCs, and are amplified in various types of glioblastoma specifically in tumorigenic cells with stem cell properties (Cancer Genome Atlas Research Network, 2008; Phillips et al., 2013; Wu et al., 2014).
Understanding how the developmental potential of NSCs or progenitors within the neurogenic niche is restricted might shed light on the unique plasticity of BTSCs, which have been found to differentiate not only into neural or glial cell lineages, but also into cell types that form the vasculature. BTSCs have the capacity to differentiate into endothelial cells and vascular pericytes, which consequently promote angiogenesis within the tumor site (Cheng et al., 2013; Guichet et al., 2015; Ricci-Vitiani et al., 2010; Wang et al., 2010). The enhanced vasculature and differentiation potential of BTSCs are the likely culprits for the increased angiogenesis and invasiveness making these properties as the hallmark of GBM. This emphasizes the complexity of BTSCs within the tumorigenic niche and underscores the need to vigorously characterize and exploit the plasticity of NSCs/progenitors to gain a better understanding of how developmental potentials of NSCs or BTSCs may be altered in the presence of factors within the neurogenic or tumorigenic niche.
Therapeutic Implications and Conclusions
Brain tumors consist of highly heterogeneous cell populations that contribute to the growth and malignancy of the tumor. Our understanding of the developmental potential and cellular hierarchy of NSCs within the V-SVZ, and how it interacts with the environment has served as a useful framework when studying tumorigenesis and its heterogeneous nature. A number of studies in mice have exploited the properties of NSCs within the V-SVZ to induce tumors, and showed that the cells in this niche include NSCs and lineage-restricted progenitors that are more readily transformed than differentiated cells outside likely because these differentiated cells do not possess the molecular properties of NSCs or progenitors that make them receptive to factors exclusively present in the neurogenic niche (Alcantara Llaguno et al., 2015; Alcantara Llaguno et al., 2009; Glasgow et al., 2014; Holland et al., 2000; Kupp et al., 2016). Furthermore, both neural stem or progenitor cells and BTSCs are equipped with molecular properties that enable them to respond accordingly to the levels of signals within their environment, which is why these cells are specifically enriched in these regions. Supporting this, studies have shown that increased radiation dose in the SVZ correlates with improved survival in glioblastoma patients (Chen et al., 2013; Jafri et al., 2013; Lee et al., 2013). Thus, along with further molecular characterization of NSCs and its developmental potential, a better understanding of how the niche provides trophic support to NSCs and specific progenitor subtypes with temporal and spatial resolution can help elucidate the mechanisms that are also utilized by BTSCs in tumorigenic niches. Ultimately, vigorous exploration of these mechanisms could lead to the identification of efficient targets for therapeutic purpose that could lead to the treatment or cure of devastating brain tumors such as GBM.
References
- Adachi K, Mirzadeh Z, Sakaguchi M, Yamashita T, Nikolcheva T, Gotoh Y, Peltz G, Gong L, Kawase T, Alvarez-Buylla A, et al. β-Catenin Signaling Promotes Proliferation of Progenitor Cells in the Adult Mouse Subventricular Zone. Stem Cells. 2007;25:2827–2836. doi: 10.1634/stemcells.2007-0177. [DOI] [PubMed] [Google Scholar]
- Aguirre A, Rubio ME, Gallo V. Notch and EGFR pathway interaction regulates neural stem cell number and self-renewal. Nature. 2010;467:323–327. doi: 10.1038/nature09347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahn S, Joyner AL. In vivo analysis of quiescent adult neural stem cells responding to Sonic hedgehog. Nature. 2005;437:894–897. doi: 10.1038/nature03994. [DOI] [PubMed] [Google Scholar]
- Alcantara Llaguno SR, Wang Z, Sun D, Chen J, Xu J, Kim E, Hatanpaa KJ, Raisanen JM, Burns DK, Johnson JE, et al. Adult Lineage-Restricted CNS Progenitors Specify Distinct Glioblastoma Subtypes. Cancer Cell. 2015;28:429–440. doi: 10.1016/j.ccell.2015.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alcantara Llaguno S, Chen J, Kwon CH, Jackson EL, Li Y, Burns DK, Alvarez-Buylla A, Parada LF. Malignant astrocytomas originate from neural stem/progenitor cells in a somatic tumor suppressor mouse model. Cancer Cell. 2009;15:45–56. doi: 10.1016/j.ccr.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balordi F, Fishell G. Hedgehog signaling in the subventricular zone is required for both the maintenance of stem cells and the migration of newborn neurons. J Neurosci. 2007;27:5936–5947. doi: 10.1523/JNEUROSCI.1040-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bar EE, Chaudhry A, Lin A, Fan X, Schreck K, Matsui W, Piccirillo S, Vescovi AL, DiMeco F, Olivi A, et al. Cyclopamine-Mediated Hedgehog Pathway Inhibition Depletes Stem-Like Cancer Cells in Glioblastoma. Stem Cells. 2007;25:2524–2533. doi: 10.1634/stemcells.2007-0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becher OJ, Hambardzumyan D, Fomchenko EI, Momota H, Mainwaring L, Bleau AM, Katz AM, Edgar M, Kenney AM, Cordon-Cardo C, et al. Gli activity correlates with tumor grade in platelet-derived growth factor-induced gliomas. Cancer Res. 2008;68:2241–2249. doi: 10.1158/0008-5472.CAN-07-6350. [DOI] [PubMed] [Google Scholar]
- Betsholtz C. Role of platelet-derived growth factors in mouse development. Int J Dev Biol. 1995;39:817–825. [PubMed] [Google Scholar]
- Bjornsson CS, Apostolopoulou M, Tian Y, Temple S. It Takes a Village: Constructing the Neurogenic Niche. Dev Cell. 2015;32:435–446. doi: 10.1016/j.devcel.2015.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Brocklyn JR, Jackson CA, Pearl DK, Kotur MS, Snyder PJ, Prior TW. Sphingosine kinase-1 expression correlates with poor survival of patients with glioblastoma multiforme: roles of sphingosine kinase isoforms in growth of glioblastoma cell lines. J Neuropathol Exp Neurol. 2005;64:695–705. doi: 10.1097/01.jnen.0000175329.59092.2c. [DOI] [PubMed] [Google Scholar]
- Calabrese C, Poppleton H, Kocak M, Hogg TL, Fuller C, Hamner B, Oh EY, Gaber MW, Finklestein D, Allen M, et al. A perivascular niche for brain tumor stem cells. Cancer Cell. 2007;11:69–82. doi: 10.1016/j.ccr.2006.11.020. [DOI] [PubMed] [Google Scholar]
- Cancer Genome Atlas Research Network. Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature. 2008;455:1061–1068. doi: 10.1038/nature07385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra V, Das T, Gulati P, Biswas NK, Rote S, Chatterjee U, Ghosh SN, Deb S, Saha SK, Chowdhury AK, et al. Hedgehog signaling pathway is active in GBM with GLI1 mRNA expression showing a single continuous distribution rather than discrete high/low clusters. PLoS One. 2015;10:e0116390. doi: 10.1371/journal.pone.0116390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L, Guerrero-Cazares H, Ye X, Ford E, McNutt T, Kleinberg L, Lim M, Chaichana K, Quinones-Hinojosa A, Redmond K. Increased Subventricular Zone Radiation Dose Correlates With Survival in Glioblastoma Patients After Gross Total Resection. Int J Radiat Oncol. 2013;86:616–622. doi: 10.1016/j.ijrobp.2013.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng L, Huang Z, Zhou W, Wu Q, Donnola S, Liu JK, Fang X, Sloan AE, Mao Y, Lathia JD, et al. Glioblastoma stem cells generate vascular pericytes to support vessel function and tumor growth. Cell. 2013;153:139–152. doi: 10.1016/j.cell.2013.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherry AE, Stella N. G protein-coupled receptors as oncogenic signals in glioma: Emerging therapeutic avenues. Neuroscience. 2014;278:222–236. doi: 10.1016/j.neuroscience.2014.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choe Y, Pleasure SJ, Mira H. Control of Adult Neurogenesis by Short-Range Morphogenic-Signaling Molecules. Cold Spring Harb Perspect Biol. 2016;8:a018887. doi: 10.1101/cshperspect.a018887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clevers H, Loh KM, Nusse R. An integral program for tissue renewal and regeneration: Wnt signaling and stem cell control. Science (80-) 2014:346. doi: 10.1126/science.1248012. [DOI] [PubMed] [Google Scholar]
- Codega P, Silva-Vargas V, Paul A, Maldonado-Soto AR, Deleo AM, Pastrana E, Doetsch F. Prospective identification and purification of quiescent adult neural stem cells from their in vivo niche. Neuron. 2014;82:545–559. doi: 10.1016/j.neuron.2014.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai C, Celestino JC, Okada Y, Louis DN, Fuller GN, Holland EC. PDGF autocrine stimulation dedifferentiates cultured astrocytes and induces oligodendrogliomas and oligoastrocytomas from neural progenitors and astrocytes in vivo. Genes Dev. 2001;15:1913–1925. doi: 10.1101/gad.903001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daynac M, Tirou L, Faure H, Mouthon MA, Gauthier LR, Hahn H, Boussin FD, Ruat M, Ahn S, Joyner AL, et al. Hedgehog Controls Quiescence and Activation of Neural Stem Cells in the Adult Ventricular-Subventricular Zone. Stem Cell Reports. 2016;7:735–748. doi: 10.1016/j.stemcr.2016.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doetsch F, Caillé I, Lim DA, García-Verdugo JM, Alvarez-Buylla A. Subventricular zone astrocytes are neural stem cells in the adult mammalian brain. Cell. 1999;97:703–716. doi: 10.1016/s0092-8674(00)80783-7. [DOI] [PubMed] [Google Scholar]
- Doetsch F, Petreanu L, Caille I, Garcia-Verdugo JM, Alvarez-Buylla A. EGF Converts Transit-Amplifying Neurogenic Precursors in the Adult Brain into Multipotent Stem Cells. Neuron. 2002;36:1021–1034. doi: 10.1016/s0896-6273(02)01133-9. [DOI] [PubMed] [Google Scholar]
- Ehtesham M, Sarangi A, Valadez JG, Chanthaphaychith S, Becher MW, Abel TW, Thompson RC, Cooper MK. Ligand-dependent activation of the hedgehog pathway in glioma progenitor cells. Oncogene. 2007;26:5752–5761. doi: 10.1038/sj.onc.1210359. [DOI] [PubMed] [Google Scholar]
- Galvao RP, Kasina A, McNeill RS, Harbin JE, Foreman O, Verhaak RGW, Nishiyama A, Miller CR, Zong H. Transformation of quiescent adult oligodendrocyte precursor cells into malignant glioma through a multistep reactivation process. Proc Natl Acad Sci U S A. 2014;111:E4214–23. doi: 10.1073/pnas.1414389111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geha S, Pallud J, Junier MP, Devaux B, Leonard N, Chassoux F, Chneiweiss H, Daumas-Duport C, Varlet P. NG2 +/Olig2 + Cells are the Major Cycle-Related Cell Population of the Adult Human Normal Brain. Brain Pathol. 2010;20:399–411. doi: 10.1111/j.1750-3639.2009.00295.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow SM, Zhu W, Stolt CC, Huang TW, Chen F, LoTurco JJ, Neul JL, Wegner M, Mohila C, Deneen B. Mutual antagonism between Sox10 and NFIA regulates diversification of glial lineages and glioma subtypes. Nat Neurosci. 2014;17:1322–1329. doi: 10.1038/nn.3790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman SA, Chen Z. Perivascular instruction of cell genesis and fate in the adult brain. Nat Neurosci. 2011;14:1382–1389. doi: 10.1038/nn.2963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong A, Huang S. FoxM1 and Wnt/β-Catenin Signaling in Glioma Stem Cells. Cancer Res. 2012:72. doi: 10.1158/0008-5472.CAN-12-0953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Perez O, Alvarez-Buylla A. Oligodendrogenesis in the subventricular zone and the role of epidermal growth factor. Brain Res Rev. 2011;67:147–156. doi: 10.1016/j.brainresrev.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber Filbin M, Dabral SK, Pazyra-Murphy MF, Ramkissoon S, Kung AL, Pak E, Chung J, Theisen MA, Sun Y, Franchetti Y, et al. Coordinate activation of Shh and PI3K signaling in PTEN-deficient glioblastoma: new therapeutic opportunities. Nat Med. 2013;19:1518–1523. doi: 10.1038/nm.3328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guichet PO, Guelfi S, Teigell M, Hoppe L, Bakalara N, Bauchet L, Duffau H, Lamszus K, Rothhut B, Hugnot JP. Notch1 stimulation induces a vascularization switch with pericyte-like cell differentiation of glioblastoma stem cells. Stem Cells. 2015;33:21–34. doi: 10.1002/stem.1767. [DOI] [PubMed] [Google Scholar]
- Holland EC, Celestino J, Dai C, Schaefer L, Sawaya RE, Fuller GN. Combined activation of Ras and Akt in neural progenitors induces glioblastoma formation in mice. Nat Genet. 2000;25:55–57. doi: 10.1038/75596. [DOI] [PubMed] [Google Scholar]
- Holland JD, Klaus A, Garratt AN, Birchmeier W. Wnt signaling in stem and cancer stem cells. Curr Opin Cell Biol. 2013;25:254–264. doi: 10.1016/j.ceb.2013.01.004. [DOI] [PubMed] [Google Scholar]
- Ihrie RA, Shah JK, Harwell CC, Levine JH, Guinto CD, Lezameta M, Kriegstein AR, Alvarez-Buylla A. Persistent sonic hedgehog signaling in adult brain determines neural stem cell positional identity. Neuron. 2011;71:250–262. doi: 10.1016/j.neuron.2011.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson EL, Garcia-Verdugo JM, Gil-Perotin S, Roy M, Quinones-Hinojosa A, VandenBerg S, Alvarez-Buylla A. PDGFR alpha-positive B cells are neural stem cells in the adult SVZ that form glioma-like growths in response to increased PDGF signaling. Neuron. 2006;51:187–199. doi: 10.1016/j.neuron.2006.06.012. [DOI] [PubMed] [Google Scholar]
- Jafri NF, Clarke JL, Weinberg V, Barani IJ, Cha S. Relationship of glioblastoma multiforme to the subventricular zone is associated with survival. Neuro Oncol. 2013;15:91–96. doi: 10.1093/neuonc/nos268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jhaveri N, Chen TC, Hofman FM. Tumor vasculature and glioma stem cells: Contributions to glioma progression. Cancer Lett. 2016;380:545–551. doi: 10.1016/j.canlet.2014.12.028. [DOI] [PubMed] [Google Scholar]
- Klaus A, Birchmeier W. Wnt signalling and its impact on development and cancer. Nat Rev Cancer. 2008;8:387–398. doi: 10.1038/nrc2389. [DOI] [PubMed] [Google Scholar]
- Kupp R, Shtayer L, Tien A-C, Szeto E, Sanai N, Rowitch DH, Mehta S. Lineage-Restricted OLIG2-RTK Signaling Governs the Molecular Subtype of Glioma Stem-like Cells. 2016 doi: 10.1016/j.celrep.2016.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee P, Eppinga W, Lagerwaard F, Cloughesy T, Slotman B, Nghiemphu PL, Wang PC, Kupelian P, Agazaryan N, Demarco J, et al. Evaluation of High Ipsilateral Subventricular Zone Radiation Therapy Dose in Glioblastoma: A Pooled Analysis. Int J Radiat Oncol. 2013;86:609–615. doi: 10.1016/j.ijrobp.2013.01.009. [DOI] [PubMed] [Google Scholar]
- Lehtinen MK, Zappaterra MW, Chen X, Yang YJ, Hill AD, Lun M, Maynard T, Gonzalez D, Kim S, Ye P, et al. The Cerebrospinal Fluid Provides a Proliferative Niche for Neural Progenitor Cells. Neuron. 2011;69:893–905. doi: 10.1016/j.neuron.2011.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon SP, Folkerth RD, Black PM. Microvessel density is a prognostic indicator for patients with astroglial brain tumors. Cancer. 1996;77:362–372. doi: 10.1002/(SICI)1097-0142(19960115)77:2<362::AID-CNCR20>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- Lim DA, Alvarez-Buylla A. The Adult Ventricular-Subventricular Zone (V-SVZ) and Olfactory Bulb (OB) Neurogenesis. Cold Spring Harb Perspect Biol. 2016:8. doi: 10.1101/cshperspect.a018820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim DA, Cha S, Mayo MC, Chen MH, Keles E, VandenBerg S, Berger MS. Relationship of glioblastoma multiforme to neural stem cell regions predicts invasive and multifocal tumor phenotype. Neuro Oncol. 2007;9:424–429. doi: 10.1215/15228517-2007-023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindberg N, Kastemar M, Olofsson T, Smits A, Uhrbom L. Oligodendrocyte progenitor cells can act as cell of origin for experimental glioma. Oncogene. 2009;28:2266–2275. doi: 10.1038/onc.2009.76. [DOI] [PubMed] [Google Scholar]
- Liu C, Sage JC, Miller MR, Verhaak RGW, Hippenmeyer S, Vogel H, Foreman O, Bronson RT, Nishiyama A, Luo L, et al. Mosaic analysis with double markers reveals tumor cell of origin in glioma. Cell. 2011;146:209–221. doi: 10.1016/j.cell.2011.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machold R, Hayashi S, Rutlin M, Muzumdar MD, Nery S, Corbin JG, Gritli-Linde A, Dellovade T, Porter JA, Rubin LL, et al. Sonic hedgehog is required for progenitor cell maintenance in telencephalic stem cell niches. Neuron. 2003;39:937–950. doi: 10.1016/s0896-6273(03)00561-0. [DOI] [PubMed] [Google Scholar]
- Menn B, Garcia-Verdugo JM, Yaschine C, Gonzalez-Perez O, Rowitch D, Alvarez-Buylla A. Origin of Oligodendrocytes in the Subventricular Zone of the Adult Brain. J Neurosci. 2006:26. doi: 10.1523/JNEUROSCI.1299-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merkle FT, Mirzadeh Z, Alvarez-Buylla A. Mosaic organization of neural stem cells in the adult brain. Science. 2007;317:381–384. doi: 10.1126/science.1144914. [DOI] [PubMed] [Google Scholar]
- Mich JK, Signer RA, Nakada D, Pineda A, Burgess RJ, Vue TY, Johnson JE, Morrison SJ, Ahn S, Joyner A, et al. Prospective identification of functionally distinct stem cells and neurosphere-initiating cells in adult mouse forebrain. Elife. 2014;3:e02669. doi: 10.7554/eLife.02669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mistry AM, Hale AT, Chambless LB, Weaver KD, Thompson RC, Ihrie RA. Influence of glioblastoma contact with the lateral ventricle on survival: a meta-analysis. J Neurooncol. 2016 doi: 10.1007/s11060-016-2278-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizugishi K, Yamashita T, Olivera A, Miller GF, Spiegel S, Proia RL. Essential role for sphingosine kinases in neural and vascular development. Mol Cell Biol. 2005;25:11113–11121. doi: 10.1128/MCB.25.24.11113-11121.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nusse R. Wnt signaling and stem cell control. Cell Res. 2008;18:523–527. doi: 10.1038/cr.2008.47. [DOI] [PubMed] [Google Scholar]
- Petrova R, Garcia ADR, Joyner AL. Titration of GLI3 repressor activity by Sonic hedgehog signaling is critical for maintaining multiple adult neural stem cell and astrocyte functions. J Neurosci. 2013;33:17490–17505. doi: 10.1523/JNEUROSCI.2042-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips JJ, Aranda D, Ellison DW, Judkins AR, Croul SE, Brat DJ, Ligon KL, Horbinski C, Venneti S, Zadeh G, et al. PDGFRA amplification is common in pediatric and adult high-grade astrocytomas and identifies a poor prognostic group in IDH1 mutant glioblastoma. Brain Pathol. 2013;23:565–573. doi: 10.1111/bpa.12043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polakis P. Wnt signaling in cancer. Cold Spring Harb Perspect Biol. 2012:4. doi: 10.1101/cshperspect.a008052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu Q, Sun G, Li W, Yang S, Ye P, Zhao C, Yu RT, Gage FH, Evans RM, Shi Y. Orphan nuclear receptor TLX activates Wnt/β-catenin signalling to stimulate neural stem cell proliferation and self-renewal. Nat Cell Biol. 2010;12:31–40. doi: 10.1038/ncb2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quint K, Stiel N, Neureiter D, Schlicker HU, Nimsky C, Ocker M, Strik H, Kolodziej MA. The role of sphingosine kinase isoforms and receptors S1P1, S1P2, S1P3, and S1P5 in primary, secondary, and recurrent glioblastomas. Tumor Biol. 2014;35:8979–8989. doi: 10.1007/s13277-014-2172-x. [DOI] [PubMed] [Google Scholar]
- Rheinbay E, Suvà ML, Gillespie SM, Wakimoto H, Patel AP, Shahid M, Oksuz O, Rabkin SD, Martuza RL, Rivera MN, et al. An Aberrant Transcription Factor Network Essential for Wnt Signaling and Stem Cell Maintenance in Glioblastoma. Cell Rep. 2013;3:1567–1579. doi: 10.1016/j.celrep.2013.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricci-Vitiani L, Pallini R, Biffoni M, Todaro M, Invernici G, Cenci T, Maira G, Parati EA, Stassi G, Larocca LM, et al. Tumour vascularization via endothelial differentiation of glioblastoma stem-like cells. Nature. 2010;468:824–828. doi: 10.1038/nature09557. [DOI] [PubMed] [Google Scholar]
- Riccitelli E, Giussani P, Di Vito C, Condomitti G, Tringali C, Caroli M, Galli R, Viani P, Riboni L. Extracellular sphingosine-1-phosphate: a novel actor in human glioblastoma stem cell survival. PLoS One. 2013;8:e68229. doi: 10.1371/journal.pone.0068229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ring A, Kim YM, Kahn M. Wnt/catenin signaling in adult stem cell physiology and disease. Stem Cell Rev. 2014;10:512–525. doi: 10.1007/s12015-014-9515-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandberg CJ, Altschuler G, Jeong J, Strømme KK, Stangeland B, Murrell W, Grasmo-Wendler UH, Myklebost O, Helseth E, Vik-Mo EO, et al. Comparison of glioma stem cells to neural stem cells from the adult human brain identifies dysregulated Wnt- signaling and a fingerprint associated with clinical outcome. Exp Cell Res. 2013;319:2230–2243. doi: 10.1016/j.yexcr.2013.06.004. [DOI] [PubMed] [Google Scholar]
- Schüle R, Dictus C, Campos B, Wan F, Felsberg J, Ahmadi R, Centner FS, Grabe N, Reifenberger G, Bermejo JL, et al. Potential canonical wnt pathway activation in high-grade astrocytomas. Scientific World Journal. 2012;2012:697313. doi: 10.1100/2012/697313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh SK, Hawkins C, Clarke ID, Squire JA, Bayani J, Hide T, Henkelman RM, Cusimano MD, Dirks PB. Identification of human brain tumour initiating cells. Nature. 2004;432:396–401. doi: 10.1038/nature03128. [DOI] [PubMed] [Google Scholar]
- Sousa VH, Fishell G. Sonic hedgehog functions through dynamic changes in temporal competence in the developing forebrain. Curr Opin Genet Dev. 2010;20:391–399. doi: 10.1016/j.gde.2010.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong CK, Fuentealba LC, Shah JK, Lindquist RA, Ihrie RA, Guinto CD, Rodas-Rodriguez JL, Alvarez-Buylla A. A Dorsal SHH-Dependent Domain in the V-SVZ Produces Large Numbers of Oligodendroglial Lineage Cells in the Postnatal Brain. Stem Cell Reports. 2015;5:461–470. doi: 10.1016/j.stemcr.2015.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura RE, Goldman JE. Dorsal radial glia generate olfactory bulb interneurons in the postnatal murine brain. J Neurosci. 2007;27:4297–4302. doi: 10.1523/JNEUROSCI.0399-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visvader JE. Cells of origin in cancer. Nature. 2011;469:314–322. doi: 10.1038/nature09781. [DOI] [PubMed] [Google Scholar]
- Wang R, Chadalavada K, Wilshire J, Kowalik U, Hovinga KE, Geber A, Fligelman B, Leversha M, Brennan C, Tabar V. Glioblastoma stem-like cells give rise to tumour endothelium. Nature. 2010;468:829–833. doi: 10.1038/nature09624. [DOI] [PubMed] [Google Scholar]
- Wesseling P, Vandersteenhoven JJ, Downey BT, Ruiter DJ, Burger PC. Cellular components of microvascular proliferation in human glial and metastatic brain neoplasms. A light microscopic and immunohistochemical study of formalin-fixed, routinely processed material. Acta Neuropathol. 1993;85:508–514. doi: 10.1007/BF00230490. [DOI] [PubMed] [Google Scholar]
- Wu G, Diaz AK, Paugh BS, Rankin SL, Ju B, Li Y, Zhu X, Qu C, Chen X, Zhang J, et al. The genomic landscape of diffuse intrinsic pontine glioma and pediatric non-brainstem high-grade glioma. Nat Genet. 2014;46:444–450. doi: 10.1038/ng.2938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Q, Yuan X, Liu G, Black KL, Yu JS. Hedgehog Signaling Regulates Brain Tumor-Initiating Cell Proliferation and Portends Shorter Survival for Patients with PTEN-Coexpressing Glioblastomas. Stem Cells. 2008;26:3018–3026. doi: 10.1634/stemcells.2008-0459. [DOI] [PubMed] [Google Scholar]
- Yoshida Y, Nakada M, Sugimoto N, Harada T, Hayashi Y, Kita D, Uchiyama N, Hayashi Y, Yachie A, Takuwa Y, et al. Sphingosine-1-phosphate receptor type 1 regulates glioma cell proliferation and correlates with patient survival. Int J Cancer. 2010a;126:2341–2352. doi: 10.1002/ijc.24933. [DOI] [PubMed] [Google Scholar]
- Yoshida Y, Nakada M, Harada T, Tanaka S, Furuta T, Hayashi Y, Kita D, Uchiyama N, Hayashi Y, Hamada J. The expression level of sphingosine-1-phosphate receptor type 1 is related to MIB-1 labeling index and predicts survival of glioblastoma patients. J Neurooncol. 2010b;98:41–47. doi: 10.1007/s11060-009-0064-5. [DOI] [PubMed] [Google Scholar]
- Zhang N, Wei P, Gong A, Chiu WT, Lee HT, Colman H, Huang H, Xue J, Liu M, Wang Y, et al. FoxM1 Promotes β-Catenin Nuclear Localization and Controls Wnt Target-Gene Expression and Glioma Tumorigenesis. Cancer Cell. 2011;20:427–442. doi: 10.1016/j.ccr.2011.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H, Ying H, Wiedemeyer R, Yan H, Quayle SN, Ivanova EV, Paik JH, Zhang H, Xiao Y, Perry SR, et al. PLAGL2 Regulates Wnt Signaling to Impede Differentiation in Neural Stem Cells and Gliomas. Cancer Cell. 2010;17:497–509. doi: 10.1016/j.ccr.2010.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]