Abstract
Introduction
Participation in the decision-making process and health literacy may both affect health outcomes; data on how these factors are related among diverse groups are limited. This study examined the relationship between health literacy and decision-making preferences in a medically underserved population.
Methods
We analyzed a sample of 576 primary care patients. Multivariable logistic regression was used to examine the independent association of health literacy (measured by the Rapid Estimate of Adult Literacy in Medicine-Revised) and patients’ decision-making preferences (physician-directed or patient-involved), controlling for age, race/ethnicity, and gender. We tested whether having a regular doctor modified this association.
Results
Adequate health literacy (OR=1.7; p=0.009) was significantly associated with preferring patient-involved decision-making, controlling for age, race/ethnicity, and gender. Having a regular doctor did not modify this relationship. Males were significantly less likely to prefer patient-involved decision-making (OR=0.65; p=0.024).
Discussion
Findings suggest health literacy affects decision-making preferences in medically underserved patients. More research is needed on how factors, such as patient knowledge or confidence, may influence decision-making preferences, particularly for those with limited health literacy.
Keywords: shared decision making, health literacy, medically underserved patients
INTRODUCTION
In the United States, there has been a recent shift in decision-making models toward shared decision-making [1, 2]. With growing emphasis on patient-centered care, shared decision-making can better align medical decisions with the patient’s preferences for care [3–5]. Shared decision-making might be particularly important to improve outcomes among patients with limited health literacy, which is about 36% of U.S. adults [6]. Research shows that individuals with limited health literacy are more likely to be hospitalized and make medication errors and less likely to obtain preventive care and know how to manage their health problems [7–9].
However, research on the relationship between health literacy and decision-making preferences is limited [10–13]. Most prior studies have been framed around disease-specific contexts [10, 12–18], have largely examined white, highly educated, or female populations [11–13, 16–20], or have not specifically assessed decision-making preferences [17–20]. Examination of decision-making preferences among medically underserved groups is particularly warranted as research suggests that shared decision-making interventions may provide greater benefits for disadvantaged groups [21].
Our study examined the relationship between health literacy and decision-making preferences in a medically underserved population. We hypothesized that patients with limited health literacy would be more likely to prefer a physician-directed decision-making role than patients with adequate health literacy. We also explored whether having a regular doctor would modify this association.
METHODS
Setting
This study was conducted in the Primary Care Clinic in the Center for Outpatient Health (COH) at Barnes-Jewish Hospital, a large urban hospital. The COH primarily serves a medically underserved population drawn from St. Louis, Missouri and the surrounding region and is the primary training site for a large internal medicine residency program.
Data collection
Between July 2013 and April 2014, patients in the waiting rooms of the COH were approached by trained data collectors and asked to complete a self-administered written questionnaire and an assessment of health literacy that was verbally administered by a data collector. To be eligible for the study, participants had to be at least 18 years old, be a patient at the COH, and speak English. The primary reason for incomplete surveys was inadequate time between the start of the survey and when the clinic was ready to begin the patient evaluation. There were no significant differences in gender between individuals with complete surveys and those with incomplete surveys; a higher proportion of those not completing the survey were African Americans (75%) compared with those who completed the survey (63%; p=0.003). Survey respondents were similar to the underlying COH primary care clinic patient population with respect to gender, age, race, and location of residence. All participants completed a verbal consent process and signed a written consent form before completing the survey. This study was approved by the Human Research Protection Office at Washington University School of Medicine.
Measures
The outcome variable was patient decision-making preferences, measured by asking: “Which statement best describes how you would like decisions about medical treatments to be made?”. Response options were on a 5-point scale, adapted from the Control Preferences Scale [22]: I prefer to leave the decision to my doctor (1), I prefer that my doctor makes the decision, but seriously considers my opinion (2), I prefer that my doctor and I share responsibility for deciding (3), I prefer to make my own decision after seriously considering my doctor’s opinion (4), and I prefer to make my own decision regardless of my doctor’s opinion (5) [16]. For analysis, responses were categorized as physician-directed (1–2) or patient-involved (3–5) decision-making preference [13, 23], with the latter including any level of patient involvement from shared to patient-directed decision-making.
The primary predictor was patient health literacy, measured by the Rapid Estimate of Adult Literacy in Medicine-Revised (REALM-R), a validated word recognition measure where individuals are asked to read eight common medical words aloud [24]. Patients who pronounced 7–8 words correctly were categorized as having adequate health literacy, and those with 0–6 correct responses as limited health literacy. Additional covariates included age (measured continuously), whether they had a regular doctor or health professional (yes/no), race/ethnicity, and gender. Race/ethnicity was categorized as non-Hispanic White (reference group), non-Hispanic Black, and Other. Gender was categorized as male or female (reference group).
Analysis
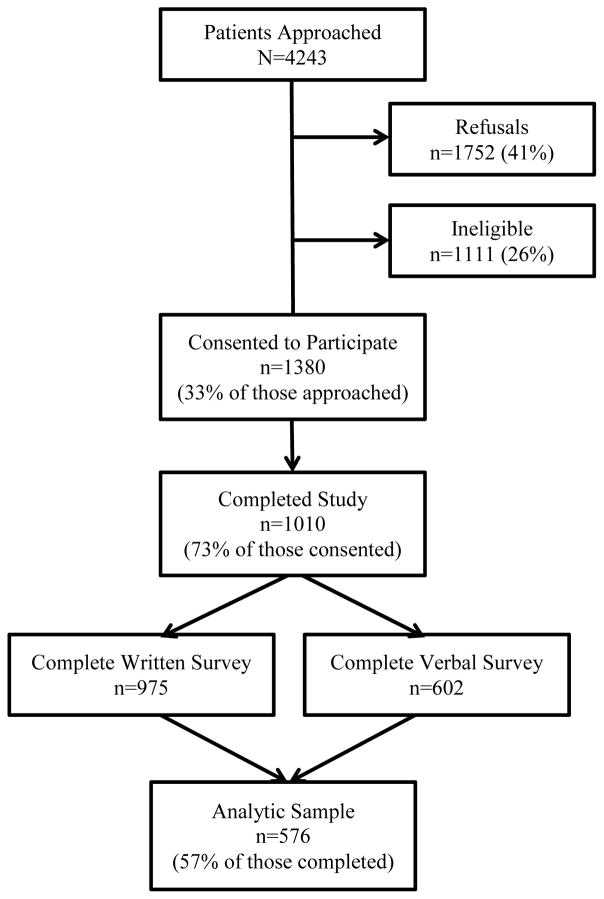
An analytic sample of 576 patients who had completed measures of health literacy and decision-making preferences was used for this analysis (Figure 1). Patients were categorized into patient-involved or physician-directed decision-making preferences, and bivariate analysis was used to examine patient characteristics that significantly differed between these two groups. Multivariable logistic regression analysis was used to examine the independent association of health literacy and decision-making preferences, controlling for sociodemographic characteristics. To investigate whether having a regular doctor moderated this relationship, we tested the interaction of health literacy and having a regular doctor on decision-making preferences in a multivariable model. All statistical analyses were conducted using SPSS for Windows, Version 20 (IBM Corp., Armonk, NY). Statistical significance was assessed as p<0.05.
Figure 1.
Recruitment flow diagram
RESULTS
Demographic characteristics are shown in Table 1. The mean age of patients was 51 years (range: 20–93); 66% were female, and 60% identified as non-Hispanic Black. The majority of patients (54%) had no more than a high school diploma/GED; 47% had a yearly household income less than $10,000. About half (45%) had limited health literacy; 58% preferred patient-involved decision-making. Most patients (67%) reported having a regular doctor.
Table 1.
Patient characteristics
| Characteristic | n | % |
|---|---|---|
| Gender (n=565) | ||
| Female | 373 | 66.0 |
| Male | 192 | 34.0 |
| Race/Ethnicity (n=565) | ||
| Non-Hispanic White | 189 | 33.5 |
| Non-Hispanic Black | 339 | 60.0 |
| Other | 37 | 6.5 |
| Education Level (n=550) | ||
| Less than high school degree | 90 | 16.4 |
| High school diploma/GED | 207 | 37.6 |
| Some college/Associate degree | 168 | 30.5 |
| College degree or higher | 85 | 15.5 |
| Employment Status (n=551) | ||
| Employed | 96 | 17.4 |
| Unemployed | 113 | 20.5 |
| Retired | 57 | 10.3 |
| Disabled | 225 | 46.3 |
| Other | 30 | 5.4 |
| Household Income (n=515) | ||
| <$9,999 | 240 | 46.6 |
| $10,000-$29,999 | 186 | 36.1 |
| $30,000-$49,000 | 56 | 10.9 |
| $50,000+ | 33 | 6.4 |
| Marital Status (n=568) | ||
| Married/Living as married | 137 | 24.1 |
| Widowed | 40 | 7.0 |
| Divorced/Separated | 195 | 34.3 |
| Never married | 196 | 34.5 |
| Decision-Making Preference (n=576) | ||
| Leave decision to doctor | 109 | 18.9 |
| Doctor makes decision, but seriously considers patient’s opinion | 133 | 23.1 |
| Doctor and patient share responsibility | 218 | 37.8 |
| Make own decision after seriously considering doctor’s opinion | 97 | 16.8 |
| Make own decision regardless of doctor’s opinion | 19 | 3.3 |
| Health Literacy (n=576) | ||
| Limited | 262 | 45.5 |
| Adequate | 314 | 54.5 |
| Have Regular Doctor (n=550) | ||
| No | 184 | 33.5 |
| Yes | 366 | 66.5 |
| Perceived Health Status (n=561) | ||
| Good/Excellent | 216 | 38.5 |
| Fair | 255 | 45.6 |
| Poor | 90 | 16.0 |
| n | mean (SD) | |
| Age | 552 | 50.7 (11.676) |
In bivariate analysis (Table 2), health literacy was significantly associated with decision-making preferences (p<0.001), with patient-involved decision-making more preferred among those with adequate health literacy (65%) compared to those with limited health literacy (50%). Decision-making preferences were also significantly associated with gender, race/ethnicity, and education level (p<0.05).
Table 2.
Bivariate associations between decision-making preferences and patient characteristics
| Physician-Directed Decision-making | Patient-Involved Decision-making | t or χ2; p-value | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Health Literacy (n=576) | 13.81; p=<0.001 | ||||
| Limited | 132 | 50.4 | 130 | 49.6 | |
| Adequate | 110 | 35.0 | 204 | 65.0 | |
| Gender (n=565) | 7.45; p=0.006 | ||||
| Female | 140 | 37.5 | 233 | 62.5 | |
| Male | 95 | 49.5 | 97 | 50.5 | |
| Race/Ethnicity (n=565) | 6.52; p=0.038 | ||||
| Non-Hispanic White | 72 | 38.1 | 117 | 61.9 | |
| Non-Hispanic Black | 155 | 45.7 | 184 | 54.3 | |
| Other | 10 | 27.0 | 27 | 73.0 | |
| Education Level (n=550) | 18.52; p=<0.001 | ||||
| Less than high school degree | 52 | 57.8 | 38 | 42.2 | |
| High school diploma/GED | 96 | 46.4 | 111 | 53.6 | |
| Some college/Associate degree | 54 | 32.1 | 114 | 67.9 | |
| College degree or higher | 31 | 36.5 | 54 | 63.5 | |
| Employment Status (n=551) | 3.54; p=0.472 | ||||
| Employed | 42 | 43.8 | 54 | 56.3 | |
| Unemployed | 51 | 45.1 | 62 | 54.9 | |
| Retired | 23 | 40.4 | 34 | 59.6 | |
| Disabled | 107 | 42.0 | 148 | 58.0 | |
| Other | 8 | 26.7 | 22 | 73.3 | |
| Household Income (n=515) | 6.52; p=0.089 | ||||
| <$9,999 | 105 | 43.8 | 135 | 56.3 | |
| $10,000-$29,999 | 67 | 36.0 | 119 | 64.0 | |
| $30,000-$49,000 | 30 | 53.6 | 26 | 46.4 | |
| $50,000+ | 12 | 36.4 | 21 | 63.6 | |
| Marital Status (n=568) | 0.92; p=0.821 | ||||
| Married/Living as married | 59 | 43.1 | 78 | 56.9 | |
| Widowed | 16 | 40.0 | 24 | 60.0 | |
| Divorced/Separated | 77 | 39.5 | 118 | 60.5 | |
| Never married | 86 | 43.9 | 110 | 56.1 | |
| Have Regular Doctor (n=550) | 0.36; p=0.548 | ||||
| No | 73 | 39.7 | 111 | 60.3 | |
| Yes | 155 | 42.3 | 211 | 57.7 | |
| Perceived Health Status (n=561) | 2.47; p=0.292 | ||||
| Good-Excellent | 86 | 39.8 | 130 | 60.2 | |
| Fair | 115 | 45.1 | 140 | 54.9 | |
| Poor | 33 | 36.7 | 57 | 63.3 | |
| Age (Mean, SD) (n=552) | 50.68 | 12.19 | 50.75 | 11.32 | -0.07; p=0.942 |
In an unadjusted model, adequate health literacy was significantly associated with preferring patient-involved decision-making (OR=1.88; p<0.001; 95% CI=1.35–2.63). This association was also significant in an adjusted model controlling for age, gender, and race/ethnicity (OR=1.66; p=0.009; 95% CI=1.14–2.42). Gender was significantly associated with decision-making preferences in this model, with males less likely to prefer patient-involved decision-making (OR=0.65; p=0.024; 95% CI=0.45–0.94). When we added having a regular doctor to the multivariable model, this variable was not a significant predictor of decision-making preferences (p=0.958), and the interaction between having a regular doctor and health literacy on decision-making preferences was not significant (p=0.560).
DISCUSSION
To our knowledge, this study is novel in its examination of health literacy and decision-making preferences specifically among medically underserved patients. In our study, patients with adequate health literacy were almost two times more likely than those with limited health literacy to prefer patient-involved decision-making. This finding is consistent with previous work [10, 12] and highlights the impact of health literacy on the decision-making process. Patients with limited health literacy may have difficulty understanding medical information and lack the self-efficacy to be actively involved in their care [12, 18]. Due to the stigma of low health literacy, some patients may also experience feelings of shame, thereby not admitting their difficulties or seeking assistance when needed [25, 26]. Future research should examine the influence of factors such as patient knowledge, self-efficacy, and perceptions of stigma on decision-making preferences among those with limited health literacy.
Furthermore, patients with limited health literacy may be unaware of their options to participate in decision-making, instead assuming physicians know the best course of action. Particularly in cases where no clear solution exists, however, the engagement of patients and consideration of their values is important [27]. Physicians should clearly provide contextual information and available options, as improved communication can facilitate patients’ informed decision-making preferences. While some patients may ultimately prefer to leave decisions to their physicians, they may want to be engaged in the process [27]. This suggests that a broader definition of shared decision-making should be considered and that physicians should recognize patients’ expressed preferences regarding their decision-making role.
Additionally, gender was a significant predictor of decision-making preferences in our study, consistent with other research indicating that females prefer a patient-involved decision-making role [28–30]. We did not find other sociodemographic characteristics, such as race/ethnicity and age, to be associated with decision-making preferences, which differs from prior studies [15, 18, 28–32]. There may be other factors impacting decision-making preferences among this medically underserved population, further highlighting the importance of examining diverse patient populations.
Our hypothesis that having a regular doctor would modify the relationship between health literacy and decision-making preferences was not supported. Contrary to our findings, some prior research shows that having a well-established relationship with a health care provider may facilitate patient-involved decision-making for patients [33–35]. One explanation for our differing results is our variable of having a regular doctor did not take into account relational factors important for decision-making, such as trust and continuity. Due to the resident clinic structure of our setting, patients may be assigned a new regular provider every three years and do not necessarily see the same physician for every visit. More research is needed on how patient-provider relationships might affect decision-making preferences among patients with varying health literacy levels and who are seen in different health care contexts.
These findings should be interpreted given study limitations. The outcome was measured by a single question, and general decision-making preferences were assessed rather decision-making preferences for a specific decision. Additionally, while health literacy was measured using a validated instrument, existing measures do not capture all domains of health literacy [36]. Secondly, convenience sampling was used to recruit patients, limiting the generalizability of results. As patients in this study were a difficult-to-reach, underserved population in a busy primary care clinic, the response and survey completion rates were low; as such, the survey participants may not be representative of the whole patient population. To generalize these findings, more work is needed with other medically underserved populations. Finally, this study assessed patients at a single point, but health literacy and decision-making preferences may change over time. Furthermore, individuals preferring a patient-involved role may engage in behaviors to improve their health literacy; examining the causal direction of this association is an area for future research.
Conclusion
This study addresses an important research gap in its examination of health literacy and decision-making preferences among medically underserved patients. Multiple factors may contribute to patients’ decision-making preferences, notably health literacy. Results suggest that interventions to promote shared decision-making may be particularly important for patients with limited health literacy. Since health literacy is a dynamic between the individual’s capabilities and the demands of a health care system [37, 38], interventions are likely needed both to assist patients with limited health literacy to participate in decision-making, as well as to support physicians in engaging with patients [13, 27]. Future research should examine other factors associated with decision-making preferences to identify additional points of intervention.
Acknowledgments
The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report. The following authors are employed by WUSM: Melody S. Goodman, Mary Politi, and Melvin Blanchard.
Financial support for the Survey of Center for Outpatient Health Patients and the project team was provided by the Barnes-Jewish Hospital Foundation, Siteman Cancer Center (Grant#: P30 CA91842), Washington University School of Medicine (WUSM), and WUSM Faculty Diversity Scholars Program.
The authors would like to thank the patients who participated in this study, data collection and data entry team, Center for Outpatient Health Primary Care Clinic staff, administrators, and residents for their contributions to our work, and Sarah Lyons for her valuable assistance in preparation for data analysis.
Footnotes
CONFLICTS OF INTEREST
JS, MG, MB, and KK declare no conflicts of interest. MP currently has an investigator initiated grant funded by Merck (2014–2015). The funding agency had no role in study design; collection, analysis and interpretation of data; writing of the report; or decision to submit the report for publication.
References
- 1.Kon AA. The shared decision-making continuum. Jama. 2010;304(8):903–4. doi: 10.1001/jama.2010.1208. [DOI] [PubMed] [Google Scholar]
- 2.McCaffery KJ, Smith SK, Wolf M. The challenge of shared decision making among patients with lower literacy: a framework for research and development. Medical decision making : an international journal of the Society for Medical Decision Making. 2010;30(1):35–44. doi: 10.1177/0272989X09342279. [DOI] [PubMed] [Google Scholar]
- 3.Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. The New England journal of medicine. 2012;366(9):780–1. doi: 10.1056/NEJMp1109283. [DOI] [PubMed] [Google Scholar]
- 4.Ferrer RL, Gill JM. Shared decision making, contextualized. Annals of family medicine. 2013;11(4):303–5. doi: 10.1370/afm.1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spatz ES, Spertus JA. Shared decision making: a path toward improved patient-centered outcomes. Circulation Cardiovascular quality and outcomes. 2012;5(6):e75–7. doi: 10.1161/CIRCOUTCOMES.112.969717. [DOI] [PubMed] [Google Scholar]
- 6.Kutner MA United States. Department of Education., National Center for Education Statistics. The health literacy of America’s adults : results from the 2003 National Assessment of Adult Literacy. Washington, DC: United States Department of Education ; National Center for Education Statistics; 2006. [Google Scholar]
- 7.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Annals of internal medicine. 2011;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 8.Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient education and counseling. 2003;51(3):267–75. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 9.Miller DP, Jr, Brownlee CD, McCoy TP, Pignone MP. The effect of health literacy on knowledge and receipt of colorectal cancer screening: a survey study. BMC family practice. 2007;8:16. doi: 10.1186/1471-2296-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeWalt DA, Boone RS, Pignone MP. Literacy and its relationship with self-efficacy, trust, and participation in medical decision making. American journal of health behavior. 2007;31(Suppl 1):S27–35. doi: 10.5555/ajhb.2007.31.supp.S27. [DOI] [PubMed] [Google Scholar]
- 11.Goggins KM, Wallston KA, Nwosu S, Schildcrout JS, Castel L, Kripalani S, et al. Health literacy, numeracy, and other characteristics associated with hospitalized patients’ preferences for involvement in decision making. Journal of health communication. 2014;19(Suppl 2):29–43. doi: 10.1080/10810730.2014.938841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mancuso CA, Rincon M. Asthma patients’ assessments of health care and medical decision making: the role of health literacy. The Journal of asthma : official journal of the Association for the Care of Asthma. 2006;43(1):41–4. doi: 10.1080/02770900500447052. [DOI] [PubMed] [Google Scholar]
- 13.Naik AD, Street RL, Jr, Castillo D, Abraham NS. Health literacy and decision making styles for complex antithrombotic therapy among older multimorbid adults. Patient education and counseling. 2011;85(3):499–504. doi: 10.1016/j.pec.2010.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aboumatar HJ, Carson KA, Beach MC, Roter DL, Cooper LA. The impact of health literacy on desire for participation in healthcare, medical visit communication, and patient reported outcomes among patients with hypertension. Journal of general internal medicine. 2013;28(11):1469–76. doi: 10.1007/s11606-013-2466-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kumar R, Korthuis PT, Saha S, Chander G, Sharp V, Cohn J, et al. Decision-making role preferences among patients with HIV: associations with patient and provider characteristics and communication behaviors. Journal of general internal medicine. 2010;25(6):517–23. doi: 10.1007/s11606-010-1275-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lillie SE, Brewer NT, O’Neill SC, Morrill EF, Dees EC, Carey LA, et al. Retention and use of breast cancer recurrence risk information from genomic tests: the role of health literacy. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2007;16(2):249–55. doi: 10.1158/1055-9965.EPI-06-0525. [DOI] [PubMed] [Google Scholar]
- 17.Peek ME, Odoms-Young A, Quinn MT, Gorawara-Bhat R, Wilson SC, Chin MH. Race and shared decision-making: perspectives of African-Americans with diabetes. Social science & medicine. 2010;71(1):1–9. doi: 10.1016/j.socscimed.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peek ME, Wilson SC, Gorawara-Bhat R, Odoms-Young A, Quinn MT, Chin MH. Barriers and facilitators to shared decision-making among African-Americans with diabetes. Journal of general internal medicine. 2009;24(10):1135–9. doi: 10.1007/s11606-009-1047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barton JL, Trupin L, Tonner C, Imboden J, Katz P, Schillinger D, et al. English language proficiency, health literacy, and trust in physician are associated with shared decision making in rheumatoid arthritis. The Journal of rheumatology. 2014;41(7):1290–7. doi: 10.3899/jrheum.131350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Katz SJ, Lantz PM, Janz NK, Fagerlin A, Schwartz K, Liu L, et al. Patient involvement in surgery treatment decisions for breast cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2005;23(24):5526–33. doi: 10.1200/JCO.2005.06.217. [DOI] [PubMed] [Google Scholar]
- 21.Durand MA, Carpenter L, Dolan H, Bravo P, Mann M, Bunn F, et al. Do interventions designed to support shared decision-making reduce health inequalities? A systematic review and meta-analysis. PloS one. 2014;9(4):e94670. doi: 10.1371/journal.pone.0094670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Degner LF, Sloan JA, Venkatesh P. The Control Preferences Scale. The Canadian journal of nursing research = Revue canadienne de recherche en sciences infirmieres. 1997;29(3):21–43. [PubMed] [Google Scholar]
- 23.Chewning B, Bylund CL, Shah B, Arora NK, Gueguen JA, Makoul G. Patient preferences for shared decisions: a systematic review. Patient education and counseling. 2012;86(1):9–18. doi: 10.1016/j.pec.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bass PF, 3rd, Wilson JF, Griffith CH. A shortened instrument for literacy screening. Journal of general internal medicine. 2003;18(12):1036–8. doi: 10.1111/j.1525-1497.2003.10651.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Easton P, Entwistle VA, Williams B. How the stigma of low literacy can impair patient-professional spoken interactions and affect health: insights from a qualitative investigation. BMC health services research. 2013;13:319. doi: 10.1186/1472-6963-13-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parikh NS, Parker RM, Nurss JR, Baker DW, Williams MV. Shame and health literacy: the unspoken connection. Patient education and counseling. 1996;27(1):33–9. doi: 10.1016/0738-3991(95)00787-3. [DOI] [PubMed] [Google Scholar]
- 27.Politi MC, Dizon DS, Frosch DL, Kuzemchak MD, Stiggelbout AM. Importance of clarifying patients’ desired role in shared decision making to match their level of engagement with their preferences. Bmj. 2013;347:f7066. doi: 10.1136/bmj.f7066. [DOI] [PubMed] [Google Scholar]
- 28.Arora NK, McHorney CA. Patient preferences for medical decision making: who really wants to participate? Medical care. 2000;38(3):335–41. doi: 10.1097/00005650-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 29.Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. Journal of general internal medicine. 2005;20(6):531–5. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Say R, Murtagh M, Thomson R. Patients’ preference for involvement in medical decision making: a narrative review. Patient education and counseling. 2006;60(2):102–14. doi: 10.1016/j.pec.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 31.Chung GS, Lawrence RE, Curlin FA, Arora V, Meltzer DO. Predictors of hospitalised patients’ preferences for physician-directed medical decision-making. Journal of medical ethics. 2012;38(2):77–82. doi: 10.1136/jme.2010.040618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Murray E, Pollack L, White M, Lo B. Clinical decision-making: Patients’ preferences and experiences. Patient education and counseling. 2007;65(2):189–96. doi: 10.1016/j.pec.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 33.Shay LA, Lafata JE. Understanding patient perceptions of shared decision making. Patient education and counseling. 2014;96(3):295–301. doi: 10.1016/j.pec.2014.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davey HM, Barratt AL, Davey E, Butow PN, Redman S, Houssami N, et al. Medical tests: women’s reported and preferred decision-making roles and preferences for information on benefits, side-effects and false results. Health expectations : an international journal of public participation in health care and health policy. 2002;5(4):330–40. doi: 10.1046/j.1369-6513.2002.00194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smith SK, Dixon A, Trevena L, Nutbeam D, McCaffery KJ. Exploring patient involvement in healthcare decision making across different education and functional health literacy groups. Social science & medicine. 2009;69(12):1805–12. doi: 10.1016/j.socscimed.2009.09.056. [DOI] [PubMed] [Google Scholar]
- 36.Mancuso JM. Assessment and measurement of health literacy: an integrative review of the literature. Nursing & health sciences. 2009;11(1):77–89. doi: 10.1111/j.1442-2018.2008.00408.x. [DOI] [PubMed] [Google Scholar]
- 37.Nielsen-Bohlman L, Panzer AM, Kindig DA, editors. Health Literacy: A Prescription to End Confusion. Washington (DC): National Academies Press; 2004. [PubMed] [Google Scholar]
- 38.Kaphingst KA, Weaver NL, Wray RJ, Brown ML, Buskirk T, Kreuter MW. Effects of patient health literacy, patient engagement and a system-level health literacy attribute on patient-reported outcomes: a representative statewide survey. BMC health services research. 2014;14:475. doi: 10.1186/1472-6963-14-475. [DOI] [PMC free article] [PubMed] [Google Scholar]