Abstract
Context
Eating disorders are severe conditions, but little is known about the prevalence or correlates of these disorders from population-based surveys of adolescents.
Objectives
To examine the prevalence and correlates of eating disorders in a large, reprefentative sample of US adolescents.
Design
Cross-sectional survey of adolescents with face-to-face interviews using a modified version of the Composite International Diagnostic Interview.
Setting
Combined household and school adolescent samples.
Participants
Nationally representative sample of 10 123 adolescents aged 13 to 18 years.
Main Outcome Measures
Prevalence and correlates of eating disorders and subthreshold conditions.
Results
Lifetime prevalence estimates of anorexia nervosa, bulimia nervosa, and binge-eating disorder were 0.3%, 0.9%, and 1.6%, respectively. Important differences were observed between eating disorder subtypes concerning sociodemographic correlates, psychiatric comorbidity, role impairment, and suicidality. Although the majority of adolescents with an eating disorder sought some form of treatment, only a minority received treatment specifically for their eating or weight problems. Analyses of 2 related subthreshold conditions suggest that these conditions are often clinically significant.
Conclusions
Eating disorders and subthreshold eating conditions are prevalent in the general adolescent population. Their impact is demonstrated by generally strong associations with other psychiatric disorders, role impairment, and suicidality. The unmet treatment needs in the adolescent population place these disorders as important public health concerns.
ALTHOUGH THE LIFETIME prevalence estimates of eating disorders from population-based studies of adults are relatively low (0.5%–1.0% for anorexia nervosa [AN] and 0.5%–3.0% for bulimia nervosa [BN]),1–8 their severity and dramatic impact have been repeatedly demonstrated through elevated rates of role impairment,1,2,9 medical complications,10 comorbidity,1,2,11 mortality,12–14 and suicide.12,13,15,16 Regarding children and adolescents, previous population-based studies of eating disorders have focused on youths who meet full DSM-IV criteria without presenting information on youths with eating problems that fall below current diagnostic thresholds. Eating disorder not otherwise specified (EDNOS), a broad category that covers clinically significant eating disorders that do not meet criteria for AN or BN, tends to be more frequently diagnosed in clinical settings than either of the DSM-IV eating disorder subtypes.17–19 In fact, adult population-based studies that have expanded measures to include EDNOS subtypes have found a greater prevalence of binge-eating disorder (BED) and related symptoms than that of AN and BN combined.1,2
Community studies that used dimensional measures in youths have also yielded far greater prevalences of disordered eating behaviors (ie, 14%–22%)20,21 than those found in studies that applied strict DSM-IV diagnostic criteria.22,23 Taken together, these findings indicate that the full spectrum of disordered eating is likely to be considerably higher than previously estimated, a possibility that may have major public health implications depending on their physical, mental, and social consequences. investigations of eating disorders in community samples of youths are relatively rare,22,23 and comprehensive descriptions of unspecified or subthreshold eating conditions have not been addressed in any prior representative adolescent samples to our knowledge.
This study examines eating disorders in the National Comorbidity Survey Replication Adolescent Supplement (NCS-A), a nationally representative sample of US adolescents aged 13 to 18 years. The objectives of this investigation are the following: (1) to present the lifetime and 12-month prevalences of AN, BN, BED, and subthreshold eating disorders; (2) to examine their sociodemographic and clinical correlates and patterns of comorbidity with other mental disorders; and (3) to describe the magnitude of role impairment, suicidal behavior, and service use associated with these disorders.
METHODS
SAMPLE
The NCS-A is a nationally representative face-to-face interview survey of 10 123 adolescents in the continental United States. The background, measures, design, and clinical validity of the NCS-A have been described in detail elsewhere.24–26 Briefly, the NCS-A sample was based on a nationally representative household sample (n = 879 adolescents) and a school sample (n=9244 adolescents), with a combined response rate of 82.9%. One parent or parental surrogate of each participating adolescent was asked to complete a self-administered questionnaire that contained questions about the adolescent’s mental health and service use; the self-administered questionnaire had a conditional response rate of 83.3%.
Sociodemographic variables assessed in the NCS-A include age, sex, race/ethnicity, parental education, parental or parental surrogate-reported marital status, household income, and urbanicity. Parental/surrogate marital status was grouped into married or cohabiting, previously married (including divorced, widowed, or separated), never married, and unknown. Household income was used to calculate the poverty income ratio, defined as the ratio of the income to the poverty line. The 2000 census definitions were used to code urbanicity by distinguishing large metropolitan areas from smaller metropolitan areas and rural areas.
ASSESSMENT OF DSM-IV DISORDERS
The DSM-IV disorders were assessed using a modification of the fully structured World Health Organization Composite International Diagnostic Interview (CIDI) administered to the adolescents by lay interviewers. In addition to the adolescent interviews, parent report from the self-administered questionnaire was incorporated to assess a selection of behavioral disorders, including attention-deficit/hyperactivity disorder, conduct disorder, and oppositional defiant disorder; attention-deficit/hyperactivity disorder was defined by parent report, while the other behavioral disorders were defined by endorsement of either the parent or adolescent. Definitions of all psychiatric disorders adhered to DSM-IV criteria except the definition of oppositional defiant disorder, which was modified to enhance clinical validity based on a clinical reappraisal subsample.27 Although service use has been included as an index of impairment in deriving DSM-IV diagnoses in other articles,28 this criterion was removed from the diagnostic algorithms for the purposes of these and other related analyses.29 Additionally, indices of disability assessed solely for 12-month disorders were not considered in defining lifetime disorder severity. Both lifetime and 12-month disorders were examined, as was the age at their onset. A more complete description of the diagnostic measures has been presented by Merikangas et al.24
The CIDI was designed to assess diagnostic criteria based on the DSM-IV criteria for AN, BN, and BED. In accordance with the diagnostic algorithms developed for the parallel adult US survey,2 both AN and BN followed the DSM-IV criteria and BED followed the proposed DSM-5 criteria.30 Because the CIDI did not directly assess loss of control associated with binge eating, items that tapped the cognition of loss of control were used to approximate this DSM-IV criterion. Diagnostic hierarchies were applied with AN taking precedence over BN, and BN superseding BED. More than 1 eating disorder subtype could be assigned only if there was clear evidence for a temporal distinction between the manifestations of the 2 subtypes.
Sufficient information was also available to define subthreshold AN (SAN) and subthreshold BED (SBED) among those youths who did not meet criteria for AN, BN, or BED. The definition of SAN included the following: (1) lowest body weight less than 90% of the adolescent’s ideal body weight; (2) intense fear of weight gain at the time of the lowest weight; and (3) no history of another threshold-level eating disorder. The definition of SBED included the following: (1) binge eating at least twice a week for several months; (2) perceived loss of control; and (3) no history of another threshold-level eating disorder or SAN. Combined, BED, SAN, and SBED capture a potentially large subset of the EDNOS category, but other symptom patterns of EDNOS could not be ascertained (eg, purging disorder, subthreshold BN).
IMPAIRMENT
Among subjects who met criteria for an eating disorder within the past 12 months, impairment was assessed using the Sheehan Disability Scale.31 The Sheehan Disability Scale captures the severity of role impairment in 4 domains: home, school or work, family, and social life. In each of these domains, the Sheehan Disability Scale measures impairment on a scale from 0 to 10 with anchors provided to the adolescent; non-0 scores indicate any impairment due to the disorder, while scores at or above 7 indicate severe or very severe impairment. In addition to this scale, these respondents were also asked to report the number of days on which they were “totally unable to go to school or work or carry out [their] normal activities because of problems with [their] eating or weight.”
SUICIDALITY
Adolescents were asked about lifetime suicide ideation, plans, and attempts. Because of the sensitivity of these questions, literate adolescents were not asked these questions directly in the face-to-face interview but rather read the questions and responded to them separately. Adolescents who could not read were instead asked these questions orally (n = 232). Adolescents were asked about suicide plans and attempts only if they endorsed suicide ideation.
SERVICE USE
Both the parent (or parental surrogate) and adolescent were asked whether the adolescent had ever been treated for emotional or behavioral problems. Reports of service use were classified into the following categories: (1) mental health specialty care: services provided by a psychiatrist in settings such as a mental health clinic, drug or alcohol clinic, emergency department, and admissions to hospitals and other facilities; (2) general medical care: services provided by a general health care practitioner, family physician, pediatrician, or any other physician; (3) human services: services involving a social worker, a counselor, a religious or spiritual advisor, or mental health crisis hotlines; (4) complementary and alternative medicine: participation in support groups, in self-help groups, or with any other healer; (5) juvenile justice: services provided by a probation or juvenile correction officer; and (6) school services: services rendered in the school environment, including attendance at a special school or special class for children with emotional and behavioral problems, treatment from a mental health nurse, school counseling, and school-administered medication. Adolescents who met criteria for AN, BN, or BED were also asked whether they had ever talked with a medical doctor or professional specifically about their eating or weight problems. With the exception of the eating disorder-specific question, the analysis of service use in this study is based on endorsement by either the parent or child; levels of agreement between the parent and adolescent reports on service use across the entire sample were acceptable (κ = 0.54). Further information on lifetime service use in the NCS-A has been reported elsewhere.29
STATISTICAL ANALYSES
All analyses were completed using the SUDAAN software system version 10 (RTI International, Research Triangle Park, North Carolina). The data were weighted to adjust for differential probabilities of selection of respondents within school and household samples, differential nonresponse, and residual differences between the sample and the US population on the cross-classification of sociodemographic variables.26 The Taylor series linearization method was implemented to adjust for the effects of weighting and clustering on all presented estimates and standard errors. Logistic regression models were used to obtain estimates of odds ratios, adjusting for age, sex, and race/ethnicity. Statistical significance was consistently evaluated using .05-level, 2-sided tests.
RESULTS
PREVALENCE AND SOCIODEMOGRAPHIC CORRELATES
Lifetime prevalence rates of AN, BN, BED, SAN, and SBED were 0.3%, 0.9%, 1.6%, 0.8%, and 2.5%, respectively (Table 1). The 12-month prevalence rates of AN, BN, BED, and SBED were 0.2%, 0.6%, 0.9%, and 1.1%, respectively, with 12-month to lifetime prevalence ratios of 57.9%, 72.0%, 56.0%, and 44.5%, respectively. Among adolescents with BN, 41.3% reported purging in their lifetime while the rest met criteria through nonpurging compensatory behaviors.
Table 1.
Sex-Specific Lifetime and 12-Month Prevalences and 12-Month to Lifetime Prevalence Ratios of Eating Disorder Subtypes Among 10 123 Adolescents
| Prevalence or Ratio | % (SE)
|
||||
|---|---|---|---|---|---|
| AN | BN | BED | SANa | SBED | |
| Lifetime prevalence | |||||
| Total | 0.3 (0.06) | 0.9 (0.16) | 1.6 (0.22) | 0.8 (0.09) | 2.5 (0.26) |
| Male | 0.3 (0.09) | 0.5 (0.19) | 0.8 (0.19) | 0.1 (0.04) | 2.6 (0.41) |
| Female | 0.3 (0.10) | 1.3 (0.22) | 2.3 (0.40) | 1.5 (0.20) | 2.3 (0.36) |
| 12-mo prevalence | |||||
| Total | 0.2 (0.05) | 0.6 (0.15) | 0.9 (0.16) | NA | 1.1 (0.12) |
| Male | 0.2 (0.08) | 0.3 (0.22) | 0.4 (0.09) | NA | 1.0 (0.17) |
| Female | 0.1 (0.06) | 0.9 (0.17) | 1.4 (0.33) | NA | 1.2 (0.22) |
| Ratio of 12-mo to lifetime prevalence | |||||
| Total | 57.9 (11.32) | 72.0 (8.50) | 56.0 (5.81) | NA | 44.5 (3.64) |
| Male | 69.9 (15.54) | 73.7 (19.89) | 43.3 (9.86) | NA | 38.0 (5.40) |
| Female | 46.7 (12.05) | 71.3 (8.04) | 60.9 (6.85) | NA | 52.4 (6.41) |
Abbreviations: AN, anorexia nervosa; BED, binge-eating disorder; BN, bulimia nervosa; NA, not applicable; SAN, subthreshold AN; SBED, subthreshold BED.
The 12-month prevalence of SAN was not assessed.
Regarding lifetime prevalence estimates, there were no sex differences in the prevalence of AN or SBED, while BN, BED, and SAN were more prevalent in girls (Table 2). Significant ethnic differences emerged for BN, with Hispanic adolescents reporting the highest prevalence; there was a trend toward ethnic minorities reporting more BED, while non-Hispanic white adolescents tended to report more AN. Measures of socioeconomic status, including parental education, household income, and parental/surrogate marital status, were not significantly associated with any eating disorder presentation.
Table 2.
Lifetime Prevalence by Sociodemographic Correlates Among 10 123 Adolescents
| Sociodemographic Correlate | % (SE)
|
||||
|---|---|---|---|---|---|
| AN | BN | BED | SAN | SBED | |
| Unweighted No. | 34 | 92 | 164 | 98 | 273 |
| Overall prevalence | 0.3 (0.06) | 0.9 (0.16) | 1.6 (0.22) | 0.8 (0.09) | 2.5 (0.26) |
| Age, y | |||||
| 13–14 | 0.3 (0.12) | 0.8 (0.25) | 1.4 (0.39) | 0.6 (0.15) | 2.4 (0.45) |
| 15–16 | 0.3 (0.12) | 0.9 (0.21) | 1.6 (0.28) | 0.9 (0.19) | 2.5 (0.33) |
| 17–18 | 0.2 (0.10) | 0.9 (0.21) | 1.9 (0.38) | 1.1 (0.18) | 2.5 (0.42) |
| Sex | |||||
| Male | 0.3 (0.09) | 0.5 (0.19)a | 0.8 (0.19)a | 0.1 (0.04)a | 2.6 (0.41) |
| Female | 0.3 (0.10) | 1.3 (0.22)a | 2.3 (0.40)a | 1.5 (0.20)a | 2.3 (0.36) |
| Race/ethnicity | |||||
| Hispanic | 0.2 (0.10) | 1.6 (0.83)a | 2.4 (0.87) | 1.0 (0.32) | 3.0 (0.43)a |
| Non-Hispanic black | 0.1 (0.09) | 1.0 (0.24)a | 1.5 (0.41) | 0.4 (0.16) | 3.5 (0.41)a |
| Other | 0.0 (0.03) | 1.3 (0.59)a | 1.4 (0.59) | 0.7 (0.28) | 3.5 (1.19)a |
| Non-Hispanic white | 0.4 (0.09) | 0.7 (0.16)a | 1.4 (0.28) | 0.9 (0.13) | 2.0 (0.32)a |
| Parental education | |||||
| <High school | 0.1 (0.07) | 1.1 (0.41) | 1.5 (0.34) | 0.6 (0.22) | 2.7 (0.49) |
| High school | 0.3 (0.15) | 0.9 (0.21) | 1.6 (0.30) | 0.7 (0.17) | 2.5 (0.35) |
| Some college | 0.3 (0.16) | 1.0 (0.36) | 2.0 (0.84) | 1.2 (0.28) | 2.9 (0.41) |
| College graduate | 0.3 (0.09) | 0.7 (0.18) | 1.4 (0.30) | 0.7 (0.15) | 2.1 (0.52) |
| Parental/surrogate marital status | |||||
| Married or cohabiting | 0.2 (0.07) | 0.8 (0.18) | 1.6 (0.33) | 0.8 (0.18) | 2.3 (0.43) |
| Previously married | 0.4 (0.24) | 1.6 (0.63) | 2.8 (1.34) | 0.8 (0.27) | 1.6 (0.48) |
| Never married | 0.0 (0.00) | 1.1 (0.76) | 0.7 (0.34) | 0.2 (0.14) | 2.5 (1.15) |
| Unknown | 0.3 (0.14) | 0.8 (0.15) | 1.3 (0.23) | 0.8 (0.16) | 2.8 (0.36) |
| Poverty index ratio | |||||
| <1.5 | 0.1 (0.04) | 1.2 (0.27) | 1.2 (0.47) | 0.8 (0.29) | 2.6 (0.40) |
| 1.5 to <3.0 | 0.2 (0.12) | 0.7 (0.23) | 1.6 (0.33) | 1.0 (0.20) | 1.9 (0.36) |
| 3.0 to <6.0 | 0.3 (0.14) | 0.9 (0.39) | 1.4 (0.23) | 1.0 (0.21) | 2.5 (0.38) |
| ≥6.0 | 0.4 (0.12) | 0.8 (0.23) | 1.9 (0.51) | 0.5 (0.14) | 2.7 (0.56) |
| Urbanicity | |||||
| Metropolitan | 0.3 (0.07) | 0.9 (0.26) | 1.5 (0.34) | 0.9 (0.17) | 2.7 (0.35) |
| Other urban | 0.2 (0.12) | 0.9 (0.24) | 1.8 (0.29) | 0.7 (0.12) | 2.2 (0.50) |
| Rural | 0.3 (0.23) | 0.8 (0.19) | 1.3 (0.24) | 0.9 (0.22) | 2.3 (0.55) |
Abbreviations: AN, anorexia nervosa; BED, binge-eating disorder; BN, bulimia nervosa; SAN, subthreshold AN; SBED, subthreshold BED.
Using a multivariate model taking into account all variables in this table, P< .05.
AGE AT ONSET
Age-at-onset curves for AN, BN, BED, and SBED are shown in the Figure. The median ages at onset of AN, BN, BED, and SBED were 12.3, 12.4, 12.6, and 12.6 years, respectively. Interquartile ranges for AN, BN, BED, and SBED were 11.2 to 13.0, 11.1 to 13.5, 11.2 to 13.5, and 10.0 to 14.3 years, respectively.
Figure.
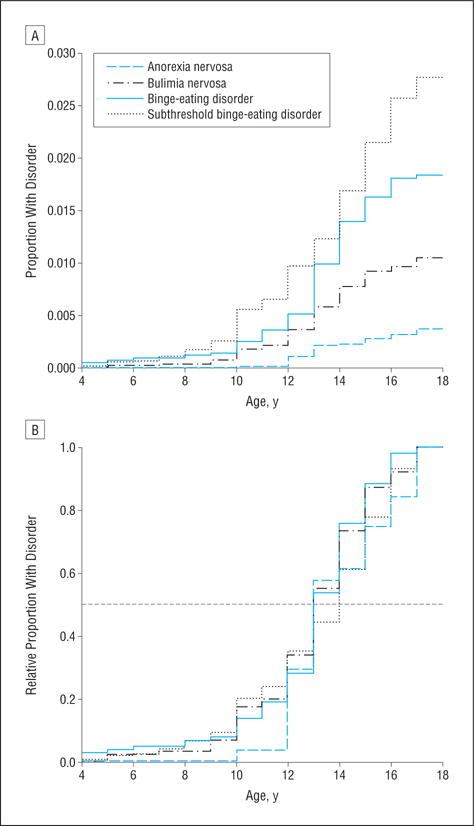
Age at onset of eating disorders, showing the proportion with disorders (A) and the relative proportion with disorders (B).
COMORBIDITY WITH OTHER MENTAL DISORDERS
The majority of respondents with an eating disorder met criteria for at least 1 other lifetime DSM-IV disorder assessed in this study across the lifetime, with 55.2%, 88.0%, 83.5%, 79.8%, and 70.1% of adolescents with AN, BN, BED, SAN, and SBED, respectively, endorsing 1 or more comorbid psychiatric disorders (Table 3). The adjusted odds ratios (95% confidence intervals) for comorbid disorders by eating disorder subtype were 1.5 (0.54.4) for AN, 8.6 (2.7–27.3) for BN, 5.9 (2.5–13.8) for BED, 4.3 (2.0–8.8) for SAN, and 2.7 (1.8–4.1) for SBED. Anorexia nervosa was not associated with any other mental disorder except oppositional defiant disorder. In contrast, BN and BED were significantly associated with nearly every disorder assessed. Both subthreshold presentations showed modest amounts of comorbidity across classes of DSM-IV disorders. In particular, BN and BED were strongly associated with mood and anxiety disorders and with multiple disorders, with 27.0% of adolescents with BN and 37.0% of adolescents with BED endorsing 3 or more classes of comorbid disorders.
Table 3.
Association Between Eating Disorder Subtypes and Other Lifetime Mental Disorders Among 10 123 Adolescents
|
DSM-IV Lifetime Mental Disorder |
No ED, % (SE) | AN
|
BN
|
BED
|
SAN
|
SBED
|
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| % (SE) | AOR (95% CI)a | % (SE) | AOR (95% CI)a | % (SE) | AOR (95% CI)a | % (SE) | AOR (95% CI)a | % (SE) | AOR (95% CI)a | ||
| Mood disorder | |||||||||||
| MDD | 10.0 (0.51) | 8.7 (4.10) | 0.7 (0.3–2.1) | 31.0 (6.01) | 3.2 (1.9–5.4)b | 35.4 (6.56) | 3.9 (2.2–7.0)b | 28.0 (7.87) | 2.3 (1.0–5.2)b | 20.7 (4.24) | 2.3 (1.3–4.0)b |
| Dysthymia | 1.7 (0.26) | 1.1 (0.86) | 0.6 (0.1–3.0) | 6.7 (2.60) | 3.6 (1.5–8.8)b | 5.8 (2.39) | 3.1 (1.3–7.5)b | 0.8 (0.56) | 0.3 (0.1–1.5) | 1.9 (0.89) | 1.2 (0.4–3.3) |
| Bipolar type I or II | 2.8 (0.23) | 2.1 (1.95) | 0.7 (0.1–4.9) | 18.5 (6.26) | 7.3 (3.1–17.2)b | 9.0 (2.69) | 3.0 (1.5–5.7)b | 8.1 (4.11) | 2.5 (0.7–8.2) | 2.6 (0.67) | 0.8 (0.5–1.5) |
| Any | 12.8 (0.56) | 10.9 (4.63) | 0.7 (0.3–2.0) | 49.9 (6.57) | 5.7 (3.2–9.9)b | 45.3 (6.40) | 4.6 (2.7–7.7)b | 33.0 (8.22) | 2.3 (1.0–5.1) | 23.3 (4.44) | 2.0 (1.2–3.4)b |
| Anxiety disorder | |||||||||||
| Agoraphobiac | 2.2 (0.19) | 3.5 (2.21) | 1.8 (0.5–6.8) | 7.5 (2.16) | 2.7 (1.4–5.0)b | 7.1 (2.52) | 2.6 (1.2–5.9)b | 7.3 (3.89) | 2.7 (0.9–8.7) | 3.9 (1.82) | 1.6 (0.6–4.3) |
| GAD | 0.9 (0.14) | 0.0 (0.00) | NAd | 4.4 (3.08) | 4.0 (0.8–18.9) | 2.0 (1.20) | 1.8 (0.5–5.8) | 1.9 (1.42) | 1.4 (0.3–6.9) | 1.8 (0.84) | 1.8 (0.6–5.5) |
| Social phobia | 5.0 (0.43) | 9.2 (4.88) | 1.8 (0.5–6.3) | 20.3 (6.23) | 3.9 (1.7–9.0)b | 26.3 (6.99) | 5.9 (2.8–12.4)b | 10.8 (4.84) | 1.7 (0.6–4.8) | 5.3 (2.20) | 1.0 (0.4–2.4) |
| Specific phobia | 14.2 (0.63) | 20.5 (8.71) | 1.5 (0.5–4.3) | 36.7 (6.75) | 3.1 (1.7–5.6)b | 32.1 (4.57) | 2.6 (1.6–4.1)b | 32.8 (6.67) | 2.6 (1.4–4.9)b | 22.6 (3.80) | 1.6 (1.0–2.6)b |
| Panic disorderc | 2.1 (0.19) | 0.9 (0.65) | 0.4 (0.1–1.8) | 11.1 (5.25) | 5.2 (1.9–14.7)b | 8.7 (2.74) | 4.0 (2.0–7.8)b | 5.0 (2.95) | 2.0 (0.5–7.1) | 5.2 (1.76) | 2.4 (1.1–5.4)b |
| PTSD | 3.4 (0.28) | 8.7 (5.08) | 2.0 (0.4–9.5) | 26.5 (6.53) | 7.6 (4.2–13.7)b | 13.2 (3.54) | 3.0 (1.4–6.3)b | 18.2 (5.91) | 3.4 (1.5–7.5)b | 8.5 (4.99) | 2.5 (0.7–9.3) |
| SAD | 6.5 (0.27) | 11.1 (5.11) | 1.8 (0.6–5.0) | 22.1 (6.20) | 3.5 (1.7–7.4)b | 16.8 (4.12) | 2.6 (1.4–4.8)b | 8.5 (3.70) | 1.1 (0.4–2.9) | 7.6 (2.13) | 1.1 (0.6–2.0) |
| Any | 24.5 (0.56) | 23.9 (9.09) | 0.9 (0.3–2.6) | 66.2 (5.59) | 5.0 (3.1–8.1)b | 65.2 (5.77) | 5.0 (3.0–8.1)b | 59.4 (7.66) | 3.5 (1.8–6.8)b | 37.1 (5.10) | 1.7 (1.1–2.6)b |
| Substance abuse or dependence | |||||||||||
| Alcohol | 6.1 (0.45) | 9.1 (6.09) | 1.6 (0.3–7.7) | 14.3 (4.30) | 3.1 (1.3–7.2)b | 13.9 (2.90) | 2.4 (1.5–4)b | 10.8 (3.64) | 1.7 (0.8–3.9) | 12.8 (4.13) | 2.5 (1.1–5.7)b |
| Drug | 8.3 (0.68) | 13.0 (7.45) | 1.7 (0.4–6.3) | 19.3 (4.53) | 2.8 (1.5–4.9)b | 22.5 (6.89) | 3.2 (1.3–7.7)b | 15.1 (5.23) | 1.8 (0.7–4.6) | 19.2 (4.29) | 2.8 (1.6–4.9)b |
| Any use | 10.8 (0.71) | 13.0 (7.45) | 1.3 (0.3–4.9) | 20.1 (4.63) | 2.2 (1.3–4.0)b | 26.8 (6.82) | 3.1 (1.3–7.2)b | 20.2 (5.77) | 2.0 (0.9–4.6) | 22.6 (4.48) | 2.7 (1.6–4.6)b |
| Behavioral disorder | |||||||||||
| ADHDe | 8.6 (0.50) | 2.3 (1.73) | 0.2 (0.1–1.1) | 20.0 (10.46) | 3.6 (1.0–12.6)b | 12.6 (4.61) | 2.1 (0.9–4.6) | 8.0 (3.20) | 1.5 (0.6–3.7) | 19.1 (5.11) | 2.6 (1.4–4.9)b |
| ODDe | 6.9 (0.53) | 30.4 (13.59) | 5.1 (1.5–17.4)b | 24.4 (6.37) | 4.0 (1.8–8.8)b | 32.8 (14.83) | 6.2 (1.8–21.7)b | 24.7 (10.82) | 4.2 (1.3–13.7)b | 7.8 (2.69) | 1.0 (0.4–2.1) |
| CDe | 10.4 (0.97) | 5.7 (4.20) | 0.5 (0.1–2.5) | 29.0 (9.72) | 3.5 (1.1–11.0)b | 28.5 (14.89) | 3.6 (0.8–15.9) | 27.1 (10.79) | 3.2 (1.0–10.2)b | 18.8 (4.04) | 1.7 (1.0–3.1) |
| Anye | 20.1 (1.15) | 31.7 (13.34) | 1.7 (0.5–5.6) | 57.8 (9.84) | 5.9 (2.6–13.5)b | 42.6 (13.65) | 3.1 (1.0–9.4)b | 39.2 (9.99) | 2.9 (1.2–6.8)b | 41.4 (6.11) | 2.5 (1.4–4.2)b |
| Cross-class comorbidity | |||||||||||
| Any classe | 44.2 (1.22) | 55.2 (14.00) | 1.5 (0.5–4.4) | 88.0 (5.76) | 8.6 (2.7–27.3)b | 83.5 (6.00) | 5.9 (2.5–13.8)b | 79.8 (5.72) | 4.3 (2.0–9.0)b | 70.1 (4.02) | 2.7 (1.8–4.0)b |
| Exactly 1 classe | 28.4 (1.00) | 33.4 (12.05) | 1.3 (0.4–3.8) | 21.0 (6.28) | 0.6 (0.3–1.5) | 28.6 (11.45) | 1.0 (0.3–3.4) | 31.2 (8.53) | 1.1 (0.5–2.7) | 32.9 (6.91) | 1.2 (0.6–2.3) |
| Exactly 2 classese | 10.3 (0.89) | 15.9 (11.68) | 1.5 (0.3–9.5) | 40.1 (10.62) | 5.4 (2.0–14.5)b | 17.9 (5.26) | 1.8 (0.9–3.6) | 36.3 (10.15) | 4.4 (1.8–10.7)b | 28.5 (5.43) | 3.2 (1.8–5.4)b |
| 3 or 4 Classese | 5.5 (0.43) | 5.9 (4.23) | 0.9 (0.2–4.2) | 27.0 (8.09) | 5.3 (2.0–14.1)b | 37.0 (14.59) | 9.2 (2.8–31.0)b | 12.4 (5.77) | 1.6 (0.4–5.8) | 8.8 (3.14) | 1.4 (0.7–2.9) |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; AN, anorexia nervosa; AOR, adjusted odds ratio; BED, binge-eating disorder; BN, bulimia nervosa; CD, conduct disorder; CI, confidence interval; ED, eating disorder; GAD, generalized anxiety disorder; MDD, major depressive disorder; NA, not applicable; ODD, oppositional defiant disorder; PTSD, posttraumatic stress disorder; SAD, separation anxiety disorder; SAN, subthreshold AN; SBED, subthreshold BED.
Adjusted for age, sex, and race/ethnicity.
P < .05.
Agoraphobia is assessed without panic disorder, while panic disorder is assessed with or without agoraphobia.
No adolescents had both AN and GAD.
Disorders are assessed using both parent and child report (n = 6483).
IMPAIRMENT
Among adolescents with 12-month AN, BN, BED, and SBED, 97.1%, 78.0%, 62.6%, and 34.6%, respectively, reported impairment in the past 12 months; 24.2%, 10.7%, 8.7%, and 2.8%, respectively, reported severe impairment (Table 4). Eating disorders were most strongly associated with social impairment. Nearly all of those with AN (88.9%) reported social impairment, and 19.6% reported severe social impairment associated with their eating disorder. Adolescents with BN and BED also reported that their eating problems most impaired their social and family relationships. Although impairment in these domains was relatively high, youths with eating disorders rarely reported that their eating problems led to complete loss of role functioning for an entire day. Among adolescents with 12-month AN, BN, BED, and SBED, 11.6%, 14.4%, 9.8%, and 11.9%, respectively, reported at least 1 day in the past year when they were completely unable to carry out normal activities. The reported number of days out of role ranged from 0 to 90 days for AN, 0 to 10 days for BN, 0 to 30 days for BED, and 0 to 41 days for SBED.
Table 4.
Role Impairment at 12 Months by 12-Month Eating Disorder Subtype
| Impairment | % (SE)
|
|||
|---|---|---|---|---|
| AN | BN | BED | SBED | |
| Role impairment | ||||
| Household chore | 41.4 (23.36) | 65.3 (10.45) | 45.0 (12.76) | 23.5 (3.61) |
| School or work | 41.0 (23.20) | 63.3 (10.43) | 46.2 (11.25) | 20.6 (3.74) |
| Family life | 80.2 (14.12) | 59.9 (9.62) | 45.7 (11.09) | 21.3 (5.66) |
| Social life | 88.9 (9.66) | 72.1 (8.66) | 51.6 (11.55) | 20.9 (4.00) |
| Any | 97.1 (3.18) | 78.0 (9.58) | 62.6 (12.26) | 34.6 (5.63) |
| Severe role impairment | ||||
| Household chore | 0.0 (0.00) | 1.1 (1.04) | 4.8 (2.83) | 2.2 (1.95) |
| School or work | 0.0 (0.00) | 4.9 (2.88) | 1.9 (1.69) | 2.6 (1.99) |
| Family life | 5.1 (4.64) | 3.7 (2.50) | 3.7 (2.18) | 2.1 (1.94) |
| Social life | 19.6 (16.12) | 8.1 (4.00) | 5.7 (2.77) | 2.1 (1.94) |
| Any | 24.2 (16.02) | 10.7 (4.32) | 8.7 (3.55) | 2.8 (1.99) |
| Days out of role in past year | ||||
| % Reporting ≥1 d | 11.6 (11.92) | 14.4 (7.88) | 9.8 (4.99) | 11.9 (7.17) |
| Reported days, range, No. | 0–90 | 0–10 | 0–30 | 0–41 |
Abbreviations: AN, anorexia nervosa; BED, binge-eating disorder; BN, bulimia nervosa; SBED, subthreshold BED.
SUICIDALITY
Lifetime suicidality was associated with all subtypes of eating disorders (Table 5). Each eating disorder subtype was associated with significantly elevated levels of suicide ideation, while BN and SAN were further associated with suicide plans and BN and BED were associated with suicide attempts. Of note, adolescents with SAN reported levels of suicide ideation comparable to those of adolescents with AN and considerably more suicide plans and attempts. Suicidality was particularly associated with BN, as more than half of adolescents with BN reported suicide ideation and more than a third reported attempts.
Table 5.
Lifetime Suicidality by Eating Disorder Subtype Among 10 123 Adolescents
| Suicide Ideation and Behavior | % (SE)
|
|||||
|---|---|---|---|---|---|---|
| AN | BN | BED | SAN | SBED | No ED | |
| Suicide ideation | 31.4 (11.24)a | 53.0 (5.93)a | 34.4 (6.18)a | 30.0 (6.04)a | 18.3 (4.32)a | 11.2 (0.55) |
| Suicide plan | 2.3 (1.42) | 25.9 (6.46)a | 5.1 (1.91) | 14.2 (5.40)a | 5.1 (1.37) | 3.6 (0.37) |
| Suicide attempt | 8.2 (5.75) | 35.1 (6.56)a | 15.1 (7.17)a | 12.4 (4.83) | 5.3 (1.56) | 3.0 (0.24) |
Abbreviations: AN, anorexia nervosa; BED, binge-eating disorder; BN, bulimia nervosa; ED, eating disorder; SAN, subthreshold AN; SBED, subthreshold BED.
Significant differences between adolescents with the ED subtype and adolescents without the subtype (P < .05).
SERVICE USE
The majority of adolescents with an eating disorder received some sort of treatment for an emotional or behavioral problem. Among subjects with AN, BN, BED, SAN, and SBED, 77.6%, 88.2%, 72.6%, 70.5%, and 64.2%, respectively, received some form of treatment in their lifetime (Table 6). However, much smaller proportions had sought treatment specifically for their eating or weight problems (27.5%, 21.5%, 11.4%, and 3.4% for AN, BN, BED, and SBED, respectively). The majority of youths who had received services had sought treatment from a mental health specialty (68.8%, 60.9%, 60.4%, 54.3%, and 48.8% for AN, BN, BED, SAN, and SBED, respectively). A sizable minority of youths with AN had sought treatment from human services (40.0%) and school services (40.4%), while many of those with BN also sought treatment from the general medical sector (49.2%) and school services (45.4%). Adolescents with each of the eating dis-order subtypes were significantly more likely to seek any treatment and mental health specialty treatment than adolescents without these disorders.
Table 6.
Lifetime Service Use by Eating Disorder Subtype and Service Sector Among 6483 Adolescents
| Service Sector | % (SE)
|
|||||
|---|---|---|---|---|---|---|
| AN | BN | BED | SAN | SBED | No ED | |
| Mental health specialty | 68.8 (12.20)a | 60.9 (8.61)a | 60.4 (9.82)a | 54.3 (9.22)a | 48.8 (7.29)a | 28.6 (1.17) |
| General medicine | 26.9 (10.24) | 49.2 (8.80)a | 22.0 (8.72) | 17.4 (6.36) | 11.0 (3.33) | 11.5 (0.57) |
| Human service | 40.0 (14.56)a | 30.2 (7.95)a | 17.7 (7.78) | 29.2 (10.61)a | 7.7 (3.15) | 10.0 (0.63) |
| CAM | 24.2 (10.61)a | 13.8 (5.15) | 3.6 (1.92) | 7.7 (3.84) | 8.4 (2.69) | 7.5 (0.56) |
| Juvenile justice | 10.7 (8.26) | 1.5 (0.90) | 1.2 (0.74)a | 15.5 (10.71) | 5.2 (1.92) | 5.1 (0.72) |
| School service | 40.4 (13.99) | 45.4 (9.03)a | 19.5 (6.16) | 38.5 (11.12)a | 43.8 (8.64)a | 21.1 (0.80) |
| Any treatment | 77.6 (11.19)a | 88.2 (4.41)a | 72.6 (8.03)a | 70.5 (7.52)a | 64.2 (7.51)a | 44.4 (0.97) |
| Treatment specifically for eating or weight problems | 27.5 (11.56) | 21.5 (5.55) | 11.4 (2.97) | NA | 3.4 (1.21) | NA |
Abbreviations: AN, anorexia nervosa; BED, binge-eating disorder; BN, bulimia nervosa; CAM, complementary and alternative medicine; ED, eating disorder; NA, not applicable; SAN, subthreshold AN; SBED, subthreshold BED.
Significant differences between adolescents with the ED subtype and adolescents without the subtype (P < .05).
COMMENT
To our knowledge, this investigation provides the first report on the prevalence, correlates, impact, and service use patterns of both threshold and subthreshold eating disorders in a nationally representative sample of US adolescents. The observed prevalence estimates were generally similar to those of previous studies,1–8,22,23 and salient differences in sociodemographic and clinical correlates were observed between eating disorder subtypes. Subthreshold eating conditions that were frequent in this population were characterized by many of the same severity markers as cases meeting diagnostic criteria. While most adolescents with eating disorders received some form of treatment, only a minority of affected individuals received services specifically for eating or weight problems. These findings underscore the important public health implications for a wide spectrum of disordered eating among US youths as well as the necessity to improve treatment access for these conditions.
Prevalence estimates for eating disorders have been difficult to compare across studies owing to differences in research methods as well as cultural and societal differences that affect base prevalence. The observed lifetime prevalence estimates of 0.3% for AN, 0.9% for BN, and 1.6% for BED were only slightly lower than those reported for US adults using parallel methods.2 However, the ages at onset of each of these disorders were markedly younger in the present sample, thereby underscoring the likelihood that retrospective assessments of adults may overestimate the age at onset of these conditions for a variety of possible reasons.32
The sex ratio for most eating spectrum disorders in this study was generally smaller than that in prior treatment-seeking samples and considerably smaller than the 9:1 ratio stated in the DSM-IV. The lack of a female preponderance of eating disorders could be attributable to either the methods of the present study or a true lack of a sex difference in eating disorders in adolescence. One indication that the difference may be genuine is provided by the large female to male ratio for SAN. Future analyses will explore possible explanations for sex differences in eating symptoms and disorders.
Prevalence estimates of eating spectrum disorders also varied by race, with Hispanic adolescents having the highest rates of BN. The greater prevalence of BN in Hispanic adolescents should be interpreted with caution as immigration status, country of birth, and length of residence in the United States may all have an effect on the risk of BN.33–35 Nonetheless, this larger prevalence highlights an important discrepancy between treatment-seeking samples and the full US adolescent population.36
Although the frequent crossover of eating disorder subtypes in longitudinal studies of adults37–39 suggests a lack of diagnostic specificity of eating disorder subtypes,40–42 differences in the correlates and clinical profiles between discrete subtypes in our study provide evidence for the validity of these distinctions. There was pervasive lifetime comorbidity among youths with BN, whereas AN was associated with only 1 other disorder (ie, oppositional defiant disorder). Likewise, suicidality was more common among adolescents with BN compared with those with AN, corroborating findings from previous community surveys43 and some clinical studies.12–14 By contrast, severe role impairment was more common among adolescents with AN relative to those with BN. The reasons for variation in clinical correlates remain to be explored but may include underlying differences in temperament and personality characteristics,44,45 genetic, physiological, and personal history variables,46,47 or other mechanisms that may differentiate AN, BN, and BED in general population samples.
The discrepancy between the lack of substantial comorbidity among adolescents in the current study48 and the high rates of comorbidity associated with AN among adults1,2 suggests that comorbid disorders may be a consequence of AN in youths. In fact, some prospective studies49,50 provide support for comorbid disorders emerging among youths with primary eating disorders in adolescence. Future analyses will compare the temporal order and progression of comorbid disorders in adults and youths in these parallel studies.
The high prevalence estimates of SAN (0.8%) and SBED (2.5%) provide evidence for a spectrum of eating disorders among youths in the general population.17–19 Subthreshold eating conditions were often characterized by many of the same severity markers as threshold cases. Most striking was the high endorsement of mental health service use for subthreshold conditions, with more than half of these adolescents having sought mental health specialty treatment. Patterns of comorbidity are also suggestive of the clinical significance of these subthreshold conditions in the population.20,21 Likewise, the significant association between suicide ideation and behavior with subthreshold conditions supports the importance of the spectrum concept of eating disorders.
The majority (72.6%–88.2%) of adolescents with eating disorders reported some contact with the service sector for emotional or behavioral problems, with the most frequently used sectors being mental health specialty care, school services, general medical services, and human services. However, only a minority (3.4%–27.5%) of individuals with eating disorders had actually talked to a professional specifically about their eating or weight problems. This could be attributable to denial of eating problems by adolescents, shame and/or stigma, or a lack of recognition of eating symptoms by professionals treating other targeted problems among these youths. The evidence that adolescents do indeed use services across sectors suggests possible avenues for prevention and early intervention strategies if recognition could be improved (eg, education of parents and youths to minimize stigma and of non-mental health care professionals to recognize signs of eating disorders). Moreover, the increased risk for certain forms of eating disorders among Hispanic and other minority adolescents warrants particular attention in education of youths, their families, and mental health care professionals.33,36
To our knowledge, this is the first population-based study in the United States to present the prevalence of eating disorders across the full adolescent age range. The large sample size is unparalleled, and the sampling design and weighting allow for generalizations to the general US adolescent population. Inclusion of subthreshold manifestations of eating disorders permitted assessment of a broader range of eating behaviors and their clinical significance. Further strengths are the use of face-to-face structured interviews of the adolescents as well as inclusion of reports from both the parent and adolescent in the assessment of service use and behavioral disorders.
However, the cross-sectional design of this study limits conclusions concerning temporal relationships among comorbid conditions and prevents confirmation of findings from adult samples concerning eating disorder crossovers or transitions from subthreshold to full-threshold conditions.37–39 In addition, the small number of adolescents with combinations of eating disorders (eg, only 6 adolescents met criteria for both AN and BN, and only 2 adolescents met criteria for both BN and BED) precluded our ability to investigate the correlates of combinations of threshold-level eating disorders.
Although 12-month prevalence is also reported, this article primarily focuses on lifetime prevalence and correlates of eating disorders. Such estimates are critical for a comprehensive life-course understanding of these disorders but may also be subject to unreliability of recall of past symptoms or disorders due to memory, bias, desirability of response, and other factors. Attempts to minimize such biases were built into the methods of the CIDI.28,51 In fact, growing evidence from prospective cohort studies suggests that retrospective recall yields underestimates as opposed to overestimates of the true prevalence of psychiatric disorders.52,53 Therefore, the estimates in this article may be a lower bound of the true prevalence of eating disorders.
Concerning other limitations, our diagnostic instrument had not been previously validated in adolescents, and studies using earlier versions of the CIDI found that the instrument tended to underdiagnose eating disorders in adults.54 However, the use of this same instrument in 2 large adult population-based investigations permitted direct comparisons across studies.1,2 An additional concern is that the structure of the survey may not capture all clinically significant cases that fall under a not-otherwise-specified (EDNOS) diagnosis, which corresponds to a majority of the identified cases of eating disorders. For example, the interview did not cover manifestations such as purging without binging, BN or BED with weekly binge eating (a criterion currently proposed for the DSM-5 for both BN and BED),30,55 or the age at onset and impairment of SAN.
Furthermore, analyses of associations may have been underpowered owing to the relatively small numbers of adolescents with eating disorders. In particular, as the unweighted number of adolescents with AN in this sample is only 34, the lack of findings for sociodemographic measures and comorbidity may be due to this methodologic issue rather than representing true null findings. Further, while the prevalence of subthreshold presentations was assessed, the CIDI was originally designed to assess only DSM-IV presentations; therefore, vital questions regarding the age at onset and impairment of SAN in particular were not asked. This is unfortunate in light of the research questions faced in the revision of the DSM, and the designers of future epidemiologic studies should consider the qualitative costs to research of enforcing skip logic along with the monetary costs.
Despite these limitations, this study provides key information concerning the epidemiology of eating disorders in the US adolescent population. The prevalence of these disorders is higher than previously expected in this age range, and the patterns of comorbidity, role impairment, and suicidality indicate that eating disorders represent a major public health concern. Finally, these findings support the nosological distinction between the major subtypes of eating disorders as well as the importance of inclusion of the full spectrum of eating behaviors in estimating the magnitude and correlates of eating disorders in the US population.
Acknowledgments
Funding/Support: This work was supported by the Intramural Research Program, National Institute of Mental Health. The NCS-A is supported by grants Z08-MH002808 and U01-MH60220 from the National Institute of Mental Health. Dr Crow is supported by Pfizer, GlaxoSmithKline, and Ortho-McNeil. Dr Le Grange is supported by grant R01 MH079979 from the National Institute of Mental Health and by the Baker Foundation (Australia).
Footnotes
Financial Disclosure: Dr Crow has received honoraria from Eli Lilly. Dr Le Grange receives royalties from Guilford Press.
Disclaimer: The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or US government.
Contributor Information
Ms Sonja A. Swanson, Genetic Epidemiology Research Branch, Intramural Research Program, National Institute of Mental Health, Bethesda, Maryland.
Dr Scott J. Crow, Department of Psychiatry, University of Minnesota, Minneapolis.
Dr Daniel Le Grange, Department of Psychiatry and Behavioral Neuroscience, University of Chicago, Chicago, Illinois.
Dr Joel Swendsen, National Center for Scientific Research, Bordeaux, France.
Dr Kathleen R. Merikangas, Genetic Epidemiology Research Branch, Intramural Research Program, National Institute of Mental Health, Bethesda, Maryland.
References
- 1.Preti A, Girolamo G, Vilagut G, Alonso J, Graaf R, Bruffaerts R, Demyttenaere K, Pinto-Meza A, Haro JM, Morosini P, ESEMeD-WMH Investigators The epidemiology of eating disorders in six European countries: results of the ESEMeD-WMH project. J Psychiatr Res. 2009;43(14):11, 25–1132. doi: 10.1016/j.jpsychires.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garfinkel PE, Lin E, Goering P, Spegg C, Goldbloom D, Kennedy S, Kaplan AS, Woodside DB. Should amenorrhoea be necessary for the diagnosis of anorexia nervosa? evidence from a Canadian community sample. Br J Psychiatry. 1996;168(4):500–506. doi: 10.1192/bjp.168.4.500. [DOI] [PubMed] [Google Scholar]
- 4.Walters EE, Kendler KS. Anorexia nervosa and anorexic-like syndromes in a population-based female twin sample. Am J Psychiatry. 1995;152(1):64–71. doi: 10.1176/ajp.152.1.64. [DOI] [PubMed] [Google Scholar]
- 5.Bijl RV, Ravelli A, van Zessen G. Prevalence of psychiatric disorder in the general population: results of the Netherlands Mental Health Survey and Incidence Study (NEMESIS) Soc Psychiatry Psychiatr Epidemiol. 1998;33(12):587–595. doi: 10.1007/s001270050098. [DOI] [PubMed] [Google Scholar]
- 6.Bushnell JA, Wells JE, Hornblow AR, Oakley-Browne MA, Joyce P. Prevalence of three bulimia syndromes in the general population. Psychol Med. 1990;20(3):671–680. doi: 10.1017/s0033291700017190. [DOI] [PubMed] [Google Scholar]
- 7.Kendler KS, MacLean C, Neale M, Kessler R, Heath A, Eaves L. The genetic epidemiology of bulimia nervosa. Am J Psychiatry. 1991;148(12):1627–1637. doi: 10.1176/ajp.148.12.1627. [DOI] [PubMed] [Google Scholar]
- 8.Garfinkel PE, Lin E, Goering P, Spegg C, Goldbloom DS, Kennedy S, Kaplan AS, Woodside DB. Bulimia nervosa in a Canadian community sample: prevalence and comparison of subgroups. Am J Psychiatry. 1995;152(7):1, 052–1, 058. doi: 10.1176/ajp.152.7.1052. [DOI] [PubMed] [Google Scholar]
- 9.Wells JE, Browne MA, Scott KM, McGee MA, Baxter J, Kokaua J, New Zealand Mental Health Survey Research Team Prevalence, interference with life and severity of 12 month DSM-IV disorders in Te Rau Hinengaro: the New Zealand Mental Health Survey. Aust N Z J Psychiatry. 2006;40(10):845–854. doi: 10.1080/j.1440-1614.2006.01903.x. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. 2006;19(4):438–443. doi: 10.1097/01.yco.0000228768.79097.3e. [DOI] [PubMed] [Google Scholar]
- 11.Steinhausen HC, Weber S. The outcome of bulimia nervosa: findings from one-quarter century of research. Am J Psychiatry. 2009;166(12):1331–1341. doi: 10.1176/appi.ajp.2009.09040582. [DOI] [PubMed] [Google Scholar]
- 12.Crow SJ, Peterson CB, Swanson SA, Raymond NC, Specker S, Eckert ED, Mitchell JE. Increased mortality in bulimia nervosa and other eating disorders. Am J Psychiatry. 2009;166(12):1342–1346. doi: 10.1176/appi.ajp.2009.09020247. [DOI] [PubMed] [Google Scholar]
- 13.Papadopoulos FC, Ekbom A, Brandt L, Ekselius L. Excess mortality, causes of death and prognostic factors in anorexia nervosa. Br J Psychiatry. 2009;194(1):10–17. doi: 10.1192/bjp.bp.108.054742. [DOI] [PubMed] [Google Scholar]
- 14.Sullivan PF. Mortality in anorexia nervosa. Am J Psychiatry. 1995;152(7):1, 073–1074. doi: 10.1176/ajp.152.7.1073. [DOI] [PubMed] [Google Scholar]
- 15.Bulik CM, Thornton L, Pinheiro AP, Plotnicov K, Klump KL, Brandt H, Crawford S, Fichter MM, Halmi KA, Johnson C, Kaplan AS, Mitchell J, Nutzinger D, Strober M, Treasure J, Woodside DB, Berrettini WH, Kaye WH. Suicide attempts in anorexia nervosa. Psychosom Med. 2008;70(3):378–383. doi: 10.1097/PSY.0b013e3181646765. [DOI] [PubMed] [Google Scholar]
- 16.Harris EC, Barraclough BM. Suicide as an outcome for medical disorders. Medicine (Baltimore) 1994;73(6):281–296. doi: 10.1097/00005792-199411000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Eddy KT, Celio Doyle A, Hoste RR, Herzog DB, le Grange D. Eating disorder not otherwise specified in adolescents. J Am Acad Child Adolesc Psychiatry. 2008;47(2):156–164. doi: 10.1097/chi.0b013e31815cd9cf. [DOI] [PubMed] [Google Scholar]
- 18.Fairburn CG, Bohn K. Eating disorder NOS (EDNOS): an example of the troublesome “not otherwise specified” (NOS) category in DSM-IV. Behav Res Ther. 2005;43(6):691–701. doi: 10.1016/j.brat.2004.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Turner H, Bryant-Waugh R. Eating disorder not otherwise specified (EDNOS): profiles of clients presenting at a community eating disorder service. Eur Eat Disord Rev. 2004;12(1):18–26. doi: 10.1002/erv.552. [DOI] [Google Scholar]
- 20.Jones JM, Bennett S, Olmsted MP, Lawson ML, Rodin G. Disordered eating attitudes and behaviours in teenaged girls: a school-based study. CMAJ. 2001;165(5):547–552. [PMC free article] [PubMed] [Google Scholar]
- 21.Hölling H, Schlack R. Eating disorders in children and adolescents: first results of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS) [in German] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2007;50(5–6):794–799. doi: 10.1007/s00103-007-0242-6. [DOI] [PubMed] [Google Scholar]
- 22.Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics. 2010;125(1):75–81. doi: 10.1542/peds.2008-2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roberts RE, Roberts CR, Xing Y. Rates of DSM-IV psychiatric disorders among adolescents in a large metropolitan area. J Psychiatr Res. 2007;41(11):959–967. doi: 10.1016/j.jpsychires.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Merikangas K, Avenevoli S, Costello J, Koretz D, Kessler RC. National Comorbidity Survey Replication Adolescent Supplement (NCS-A), I: background and measures. J Am Acad Child Adolesc Psychiatry. 2009;48(4):367–369. doi: 10.1097/CHI.0b013e31819996f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kessler RC, Avenevoli S, Costello EJ, Green JG, Gruber MJ, Heeringa S, Merikangas KR, Pennell BE, Sampson NA, Zaslavsky AM. National Comorbidity Survey Replication Adolescent Supplement (NCS-A), II: overview and design. JAm Acad Child Adolesc Psychiatry. 2009;48(4):380–385. doi: 10.1097/CHI.0b013e3181999705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kessler RC, Avenevoli S, Costello EJ, Green JG, Gruber MJ, Heeringa S, Merikangas KR, Pennell BE, Sampson NA, Zaslavsky AM. Design and field procedures in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A) Int J Methods Psychiatr Res. 2009;18(2):69–83. doi: 10.1002/mpr.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler RC, Avenevoli S, Green J, Gruber MJ, Guyer M, He Y, Jin R, Kaufman J, Sampson NA, Zaslavsky AM. National Comorbidity Survey Replication Adolescent Supplement (NCS-A), III: concordance of DSM-IV/CIDI diagnoses with clinical reassessments. J Am Acad Child Adolesc Psychiatry. 2009;48(4):386–399. doi: 10.1097/CHI.0b013e31819a1cbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Merikangas KR, He JP, Burstein M, Swendsen J, Avenevoli S, Case B, Georgiades K, Heaton L, Swanson S, Olfson M. Service utilization for lifetime mental disorders in US adolescents: results of the National Comorbidity Survey-Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2011;50(1):32–45. doi: 10.1016/j.jaac.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American Psychiatric Association. DSM-5 development. http://www.dsm5.org. Accessed February 24, 2010.
- 31.Leon AC, Olfson M, Portera L, Farber L, Sheehan DV. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. IntJ Psychiatry Med. 1997;27(2):93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD. [DOI] [PubMed] [Google Scholar]
- 32.Favaro A, Caregaro L, Tenconi E, Bosello R, Santonastaso P. Time trends in age at onset of anorexia nervosa and bulimia nervosa. J Clin Psychiatry. 2009;70(12):1715–1721. doi: 10.4088/JCP.09m05176blu. [DOI] [PubMed] [Google Scholar]
- 33.Cachelin FM, Striegel-Moore RH. Help seeking and barriers to treatment in a community sample of Mexican American and European American women with eating disorders. Int J Eat Disord. 2006;39(2):154–161. doi: 10.1002/eat.20213. [DOI] [PubMed] [Google Scholar]
- 34.Alegria M, Woo M, Cao Z, Torres M, Meng XL, Striegel-Moore R. Prevalence and correlates of eating disorders in Latinos in the United States. Int J Eat Disord. 2007;40(suppl):S15–S21. doi: 10.1002/eat.20406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chamorro R, Flores-Ortiz Y. Acculturation and disordered eating patterns among Mexican American women. Int J Eat Disord. 2000;28(1):125–129. doi: 10.1002/(sici)1098-108x(200007)28:1<125::aid-eat16>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 36.le Grange D, Crosby RD, Rathouz PJ, Leventhal BL. A randomized controlled comparison of family-based treatment and supportive psychotherapy for adolescent bulimia nervosa. Arch Gen Psychiatry. 2007;64(9):1049–1056. doi: 10.1001/archpsyc.64.9.1049. [DOI] [PubMed] [Google Scholar]
- 37.Eddy KT, Dorer DJ, Franko DL, Tahilani K, Thompson-Brenner H, Herzog DB. Diagnostic crossover in anorexia nervosa and bulimia nervosa: implications for DSM-V. Am J Psychiatry. 2008;165(2):245–250. doi: 10.1176/appi.ajp.2007.07060951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eddy KT, Swanson SA, Crosby RD, Franko DL, Engel S, Herzog DB. How should DSM-V classify eating disorder not otherwise specified (EDNOS) presentations in women with lifetime anorexia or bulimia nervosa? Psychol Med. 2010;40(10):1735–1744. doi: 10.1017/S0033291709992200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Agras WS, Crow S, Mitchell JE, Halmi KA, Bryson S. A 4-year prospective study of eating disorder NOS compared with full eating disorder syndromes. Int J Eat Disord. 2009;42(6):565–570. doi: 10.1002/eat.20708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fairburn CG, Cooper Z, Doll HA, O’Connor ME, Bohn K, Hawker DM, Wales JA, Palmer RL. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am J Psychiatry. 2009;166(3):311–319. doi: 10.1176/appi.ajp.2008.08040608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behav Res Ther. 2003;41(5):509–528. doi: 10.1016/s0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- 42.Wade TD, Bergin JL, Martin NG, Gillespie NA, Fairburn CG. A transdiagnostic approach to understanding eating disorders. J Nerv Ment Dis. 2006;194(7):510–517. doi: 10.1097/01.nmd.0000225067.42191.b0. [DOI] [PubMed] [Google Scholar]
- 43.Newman DL, Moffitt TE, Caspi A, Magdol L, Silva PA, Stanton WR. Psychiatric disorder in a birth cohort of young adults: prevalence, comorbidity, clinical significance, and new case incidence from ages 11 to 21. J Consult Clin Psychol. 1996;64(3):552–562. [PubMed] [Google Scholar]
- 44.Díaz-Marsá M, Carrasco JL, Sáiz J. A study of temperament and personality in anorexia and bulimia nervosa. J Pers Disord. 2000;14(4):352–359. doi: 10.1521/pedi.2000.14.4.352. [DOI] [PubMed] [Google Scholar]
- 45.Harrison A, O’Brien N, Lopez C, Treasure J. Sensitivity to reward and punishment in eating disorders. Psychiatry Res. 2010;177(1–2):1–11. doi: 10.1016/j.psychres.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 46.Fairburn CG, Harrison PJ. Eating disorders. Lancet. 2003;361(9355):407–416. doi: 10.1016/S0140-6736(03)12378-1. [DOI] [PubMed] [Google Scholar]
- 47.Scherag S, Hebebrand J, Hinney A. Eating disorders: the current status of molecular genetic research. Eur Child Adolesc Psychiatry. 2010;19(3):211–226. doi: 10.1007/s00787-009-0085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lock J, Le Grange D, Agras WS, Moye A, Bryson SW, Jo B. Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Arch Gen Psychiatry. 2010;67(10):1025–1032. doi: 10.1001/archgenpsychiatry.2010.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wentz E, Gillberg IC, Anckarsäter H, Gillberg C, Råstam M. Adolescent-onset anorexia nervosa: 18-year outcome. Br J Psychiatry. 2009;194(2):168–174. doi: 10.1192/bjp.bp.107.048686. [DOI] [PubMed] [Google Scholar]
- 50.Patton GC, Coffey C, Carlin JB, Sanci L, Sawyer S. Prognosis of adolescent partial syndromes of eating disorder. Br J Psychiatry. 2008;192(4):294–299. doi: 10.1192/bjp.bp.106.031112. [DOI] [PubMed] [Google Scholar]
- 51.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 52.Angst J, Gamma A, Neuenschwander M, Ajdacic-Gross V, Eich D, Rössler W, Merikangas KR. Prevalence of mental disorders in the Zurich Cohort Study: a twenty year prospective study. Epidemiol Psichiatr Soc. 2005;14(2):68–76. doi: 10.1017/s1121189x00006278. [DOI] [PubMed] [Google Scholar]
- 53.Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R. How common are common mental disorders? evidence that lifetime prevalence rates are doubled by prospective vs retrospective ascertainment. Psychol Med. 2010;40(6):899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Thornton C, Russell J, Hudson J. Does the Composite International Diagnostic Interview underdiagnose the eating disorders? Int J Eat Disord. 1998;23(3):341–345. doi: 10.1002/(sici)1098-108x(199804)23:3<341::aid-eat11>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 55.Walsh BT, Sysko R. Broad Categories for the Diagnosis of Eating Disorders (BCD-ED): an alternative system for classification. Int J Eat Disord. 2009;42(8):754–764. doi: 10.1002/eat.20722. [DOI] [PMC free article] [PubMed] [Google Scholar]


