Abstract
BACKGROUND
Numerous studies have supported an association between maternal depression and child psychiatric outcomes, but few have controlled for the confounding effects of both maternal and offspring comorbidity. Thus, it remains unclear whether the correspondence between maternal and offspring depressive and anxiety disorders is better explained by associations between shared features of maternal and offspring internalizing disorders or by specific effects exerted by unique aspects of individual disorders.
METHODS
Pairs of mothers and offspring overselected for maternal depression (N = 815) were assessed at offspring age 15 for anxiety and depressive disorders; 705 completed a follow-up at offspring age 20. For both mothers and offspring, structural equation modeling was used to distinguish transdiagnostic internalizing pathology—representing the overlap among all depressive and anxiety disorders—from diagnosis-specific forms of pathology. To discriminate between general versus specific pathways of intergenerational transmission of psychopathology, we examined (a) the general association between the maternal and offspring internalizing factors and (b) the correlations between maternal and offspring diagnosis-specific pathology for each disorder in an effort.
RESULTS
For mothers and offspring, a unidimensional latent variable model provided the best fit to the correlations among depressive and anxiety disorders. The maternal transdiagnostic internalizing factor strongly predicted the corresponding factor among offspring. In addition, the unique component of posttraumatic stress disorder among offspring was significantly related to the analogous unique component among mothers, but specific components of other maternal disorders, including depression, did not predict corresponding offspring pathology.
CONCLUSIONS
Results suggest that intergenerational transmission of internalizing disorders is largely non-specific.
Keywords: Intergenerational transmission, internalizing disorders, maternal depression, maternal anxiety disorders
Considerable evidence suggests that offspring of depressed mothers show higher depression rates than offspring of never-depressed women, and that this vulnerability also extends to other psychiatric disorders (Halligan et al., 2007, Hammen et al., 2008, Hammen et al., 1990, Klein et al., 2005, Lieb et al., 2002, Weissman et al., 2006, see review by Goodman et al., 2011). Similarly, although much research has exclusively focused on effects of depression, several studies indicate that other maternal disorders, including anxiety disorders, also confer risk for a broad range of psychiatric outcomes among offspring (Last et al., 1987, McClure et al., 2001, Turner et al., 1987, Weissman et al., 1984). However, the great majority of these studies have not accounted for comorbidity, potentially misrepresenting associations between parental disorders and youth outcomes and leaving it unclear whether familial vulnerability can be more accurately understood as transmission of a nonspecific liability to internalizing problems from parents to offspring.
The present study seeks to improve existing models of intergenerational transmission of internalizing disorders by accounting for comorbidity among individual disorders in both mothers and offspring, specifically by incorporating recent advances in the understanding of the latent structure of psychopathology. Recent research has supported a hierarchical-spectrum model of mental disorders (HSM; Krueger et al., 1998, Krueger and Markon, 2006), which assumes that internalizing disorders are manifestations of a transdiagnostic, continuously-distributed internalizing spectrum representing a common vulnerability trait for depressive and anxiety disorders. Several studies applying the HSM framework have suggested the existence of a general Internalizing factor (and a separate Externalizing factor) accounting for the shared variance of individual disorders, converging with numerous studies finding evidence for a shared substrate to anxiety and depressive disorders varyingly labeled neuroticism, general distress, and negative affect/affectivity (e.g., Brown and Barlow, 2002, Griffith et al., 2010, Watson et al., 1995). The HSM framework has been supported in adult (Eaton et al., 2012a, Krueger, 1999, Krueger and Markon, 2006, Vollebergh et al., 2001) and adolescent samples (Fergusson et al., 2006, Walton et al., 2011), and offers the ability to discriminate between the common (or transdiagnostic) and unique features of disorders. In turn, HSM-informed methods can differentiate between an external construct’s associations with these shared and specific elements. As such, applications of HSM have begun to yield insights into how key psychopathological processes map onto unique components of individual disorders versus shared pathology (Conway et al., in press, South et al., 2011).
The HSM method may prove useful in modeling the intergenerational transmission of internalizing disorders. First, it can address whether a transdiagnostic internalizing trait, representing vulnerability to all internalizing disorders, is transmitted from mothers to offspring. Second, it can pinpoint the degree to which diagnosis-specific pathology (represented by residual variances associated with each individual disorder) is also transmitted across generations. Thus, HSM can distinguish between general versus specific modes of intergenerational transmission.
To our knowledge, only two studies to date have used latent variable modeling techniques to disentangle the general and specific pathways of intergenerational transmission of psychopathology. Using data from the National Comorbidity Survey, Kendler et al. (1997) modeled internalizing and externalizing diagnoses as indicators of distinct latent factors among probands and their parents, and examined associations between parent and proband latent factors. Parental Internalizing and Externalizing factors each affected offspring standing on both Internalizing and Externalizing dimensions. Although this study did not directly model residual covariation, they tested specificity of transmission by controlling for presence of all other disorders when computing associations between particular parent and offspring diagnoses. For MDD, GAD, and alcohol use disorders, substantial intergenerational transmission effects remained, suggesting that some unique risk for these disorders is intergenerationally transmitted, independent of the transmission of general vulnerability. However, this study had two major limitations: first, parental psychopathology was assessed via offspring report, a clear potential source of bias (Milne et al., 2009). Second, only two internalizing disorders (GAD and MDD) were included, limiting the scope of the latent factor. Hicks et al. (2004) used the HSM framework to investigate heritability and familial transmission of a latent Externalizing trait in the Minnesota Twin Family Study. Results indicated that parent standing on the Externalizing factor was significantly related to offspring Externalizing levels. Unlike Kendler et al.’s (1997) findings, no significant residual correlations between parent and child diagnoses were detected after controlling for the general transmission effect, indicating an absence of disorder-specific transmission among externalizing disorders.
The present study approaches the generality versus specificity question with respect to internalizing disorders. Although ample evidence demonstrates that offspring of depressed and anxious mothers are vulnerable to a variety of disorders, no study has used the HSM framework to examine transgenerational effects of a broad range of internalizing disorders, directly assessed from mothers and offspring. The current study does so, modeling intergenerational transmission in a longitudinal, community sample of mothers and their adolescent offspring. Maternal psychopathology was assessed over the first 15 years of the youth’s lifetime (as evidence suggests that maternal depression during this developmental period exerts stronger effects; Hammen et al., 2008), and offspring psychopathology was assessed up to age 20 (allowing for greater representation of disorders that increase in prevalence during later adolescence; Lewinsohn et al., 1998, Merikangas et al., 2010; the staggered timing of the maternal and offspring diagnoses is justifable as the impact of maternal depression often persists after the depressive episode remits; Billings and Moos, 1985, Cox et al., 1987 ). Although HSM research has often examined Externalizing as well as Internalizing spectra (Krueger et al., 1998, South et al., 2011), the present study only tested depressive and anxiety disorders due to infrequent externalizing diagnoses among mothers. Although prior studies are limited, based on existing evidence we anticipated that the pathway between the maternal and offspring broad Internalizing factors would account for a substantial portion of the intergenerational transmission of internalizing disorders. We also tested pathways between the residual variance for individual maternal disorders and corresponding offspring disorders (e.g., maternal MDD predicting offspring MDD) but made no a priori hypotheses regarding these diagnosis-specific associations.
Previous research has exclusively utilized unidimensional models to examine intergenerational transmission of psychopathology (Hicks et al., 2004, Kendler et al., 1997), but recent research suggests that more complex models may better describe the latent structure of internalizing disorders (Krueger, 1999, Krueger and Markon, 2006, Simms et al., 2008, Simms et al., 2012, Watson, 2005). These include two-factor models, in which internalizing disorders bifurcate into Fear versus Distress factors (Krueger, 1999) or Anxiety versus Depression factors (i.e., the model implicitly endorsed by the Diagnostic and Statistical Manual, 4th-Edition [DSM-IV]; American Psychiatric Association, 1994), as well as hierarchical (including a superordinate Internalizing factor and additional lower-order factors) and bifactor (with all disorders loading onto both an Internalizing factor and a lower-order factor) models (Prenoveau et al., 2010, Simms et al., 2008, Simms et al., 2012). As a preliminary step, the current study tested alternative factor structures to determine which models are best suited to examine intergenerational transmission of internalizing disorders in this sample.
Method
Participants
Eight hundred fifteen Australian mother-offspring pairs participated as part of a large, longitudinal project. Participants were selected from a large birth cohort study conducted at the Mater Misericordiae Mother’s Hospital in Brisbane, Queensland (N= 7,775; Keeping et al., 1989), which tracked mothers and children born between 1981 and 1984. Mothers provided data, including self-reported depressive symptoms (assessed using the Delusions-Symptoms-States Inventory [DSSI]; Bedford and Foulds, 1978), during pregnancy, postpartum, and at child ages six months and five years. A subset of the initial sample was targeted for participation in a follow-up 15 years after birth, selected on the basis of maternal DSSI scores over the four data points, with mothers with elevated depression scores selectively oversampled (the DSSI was used only for sample selection purposes. Maternal depression as reported in the current analyses reflect clinical interview data). Nine hundred ninety-one families were identified for participation in the age 15 follow-up and 815 provided data. Mean maternal age was 40.4 years. Hammen and Brennan (2001) provide further detail on sample recruitment and characteristics. At offspring age 20, families were invited to participate in an additional follow-up, and 705 participated (363 offspring were female, 342 were male). Non-participating families could not be contacted (n= 58), declined to participate (n= 52), or were deceased (n= 2). Youth depression history did not predict attrition, but non-participating families reported lower income (t(783)=−2.11, p=.04) and offspring were more likely to be male (χ2(1)=8.63, p=.003). Mothers participating at age 20 were marginally more likely to have a depression history (χ2(1)=3.56, p=.06).
Procedure
Pregnant women were recruited into the MUSP study during their first prenatal visit and continued to provide questionnaire data until the child reached age 5. For further detail about MUSP procedures, see Keeping et al. (1989). At both age 15 and age 20 follow-ups, after providing consent/assent, mothers and offspring were individually interviewed in private locations by separate interviewers blind to maternal psychiatric history. Interviewers were advanced graduate students in clinical psychology, supervised by a licensed clinical psychologist, and were highly trained in administration of diagnostic interviews and required to meet high reliability standards. The institutional review boards of UCLA, Emory University, and University of Queensland approved this research.
Measures
Maternal psychiatric diagnoses were assessed using the Structured Clinical Interview for DSM-IV (SCID; Spitzer et al., 1995), a widely-used semi-structured interview designed to generate clinical diagnoses. For the current analyses, maternal diagnoses were assessed at offspring age 15 and reflect lifetime psychopathology until that point. Inter-rater (?) reliability was very good (kappas based on ratings of independent judges ranged between .87 for current and .84 for past depressive disorders, and between .82 and .85 for current and past anxiety disorders). Relevant to the current study, mothers were assessed for the following categorically-defined mood and anxiety disorders: MDD, dysthymia (DYS), social phobia (SOC), obsessive-compulsive disorder (OCD), GAD, specific phobia (SPEC), post-traumatic stress disorder (PTSD), panic disorder, and agoraphobia (panic disorder and agoraphobia were subsequently aggregated into a single disorder category [PAN]).
At age 15, youth were assessed using the Schedule for Affective Disorders and Schizophrenia—Child-Revised (Epidemiological Version) for the DSM-IV (K-SADS-E; Kaufman et al., 1997), a widely-used semi-structured interview designed for use with children and adolescents. Offspring were assessed for lifetime psychopathology up to that point. Following standard procedures, the K-SADS-E was administered to both mother and child, with final diagnostic decisions made by a clinical team using all available information. Interrater reliability based on independent ratings was good (kappas for current and past depressive disorder were .82 and .73 respectively, for anxiety disorders, κ= .79 for both current and past). At age 20, offspring disorders occurring between the ages of 15 and 20 were assessed using the SCID, with excellent interrater reliability (for current and past depressive disorders, kappas ranged from .83 to .89; for current/past anxiety disorders, kappas ranged from .89 to .94). At both data points, offspring were assessed for the same mood and anxiety disorder diagnoses as were mothers. For the current analyses, offspring current and past diagnoses assessed at ages 15 and 20 were aggregated to reflect categorical cumulative lifetime diagnoses through age 20.
Data Analytic Plan
All analyses used structural equation modeling. Observed internalizing diagnoses were treated as indicators of a latent Internalizing dimension for both mothers and offspring. Only diagnoses with frequencies above 5% of the sample were included as indicators to avoid model convergence problems and ensure acceptable reliability of diagnosis-specific variance terms. For mothers, diagnoses meeting that threshold were MDD, DYS, PAN, SOC, SPEC, and PTSD, with GAD (n= 26, 3%) and OCD (n= 8, 1%) excluded. For offspring, MDD, DYS, SOC, SPEC, PTSD, and GAD defined the corresponding Offspring Internalizing factor, with PAN (n=24, 3%) and OCD (n= 21, 3%) excluded. Model fit was evaluated on the basis of the likelihood ratio chi-square test, the comparative fit index (CFI; Bentler, 1990), the root-mean-square error of approximation (RMSEA; Browne and Cudeck, 1993), and the weighted root-mean-square residual (WRMR).
As a preliminary step, we compared several different factor structures for the Internalizing spectrum; comparative model fit was assessed using the Bayesian Information Criteria (BIC), CFI, and RMSEA. Next, we regressed the Offspring Internalizing factor(s) on the Maternal Internalizing factor(s) to examine intergenerational transmission of nonspecific internalizing pathology. Finally, we estimated the correlations between the residuals of maternal diagnoses and corresponding residuals of offspring diagnoses (no residual correlations were estimated for PAN and GAD because they were excluded from the offspring and maternal spectra respectively for low frequency). As an additional test, we compared model fit using BIC indices for models including versus excluding each residual pathway. We did not test cross-disorder associations to prevent an excessive number of tests.
Analyses were conducted in Mplus using the WLSMV estimator (Muthén & Muthén, 2007); ML estimation was used to generate BIC reports. Mplus employs full information maximum likelihood procedures for missing data (there were no missing data except for 110 families lost to attrition at age 20).
Results
Descriptive Statistics
Frequencies of maternal and offspring diagnoses, and tetrachoric correlations among them, are presented in Table 1. All maternal diagnoses were significantly correlated with multiple offspring diagnoses. Notably, maternal diagnoses did not always exhibit the highest correlations with corresponding offspring diagnoses. For instance, the correlation between maternal and offspring MDD was roughly one-third the magnitude of the correlation between maternal MDD and offspring PTSD.
Table 1.
Tetrachoric correlations between maternal and offspring internalizing diagnoses.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Maternal diagnoses | ||||||||||||
| 1. Major Depression | — | |||||||||||
| 2. Dysthymia | .30 | — | ||||||||||
| 3. Social Phobia | .36 | .40 | — | |||||||||
| 4. Specific Phobia | .17 | .36 | .30 | — | ||||||||
| 5. Post-Traumatic Stress Disorder | .34 | .39 | .32 | .31 | — | |||||||
| 6. Panic Disorder/Agoraphobia | .41 | .32 | .31 | .19 | .16 | — | ||||||
| Offspring Diagnoses | ||||||||||||
| 7. Major Depression | .08 | .14 | −.03 | .21 | .17 | .04 | — | |||||
| 8. Dysthymia | .20 | .25 | −.28 | .13 | −.04 | .15 | .45 | — | ||||
| 9. Social Phobia | .12 | .17 | −.13 | .02 | .12 | .01 | .28 | .24 | — | |||
| 10. Specific Phobia | .00 | −.06 | −.05 | .24 | −.04 | −.02 | .13 | .16 | .25 | — | ||
| 11. Post-Traumatic Stress Disorder | .27 | .18 | .13 | .25 | .39 | −.04 | .57 | .34 | .08 | .25 | — | |
| 12. Generalized Anxiety Disorder | .27 | .21 | .15 | .15 | .28 | −.09 | .56 | .37 | .45 | .32 | .36 | — |
|
| ||||||||||||
| N | 271 | 165 | 46 | 66 | 46 | 64 | 220 | 71 | 144 | 110 | 48 | 56 |
| % of sample | 33.2 | 20.2 | 5.6 | 8.1 | 5.6 | 7.8 | 31.2 | 10.1 | 20.4 | 15.6 | 6.8 | 7.9 |
Note. All correlations are tetrachoric correlations. Correlations greater than |.07| are significant at the .05 level; correlations greater than |.10| are significant at the .01 level. N = number of participants qualifying for a diagnosis.
Model Fit
To determine optimal latent structure of internalizing spectra within this dataset, we tested several competing models, including (a) a single factor representing internalizing distress (INT), (b) a two-factor model featuring correlated Distress (MDD, DYS, GAD, PTSD) and Fear (PAN, SPEC, SOC) based on Krueger’s (1999) conceptualization; (c) an oblique two-factor model reflecting the DSM-IV organization of Depression (MDD, DYS) and Anxiety (SOC, PAN, GAD, SPEC, PTSD); (d) a hierarchical model in which a superordinate Internalizing factor is marked by subordinate Fear and Distress factors; and (e) a bifactor model in which all disorders load on a general Internalizing factor as well as either the Fear or Distress unique factor (e.g., Simms et al., 2012).
Fit data are presented in Table 2. Models for mothers and offspring were run separately, but both yielded the same conclusions; for simplicity, we focus here on mothers. For both two-factor models (i.e., correlated Distress and Fear; correlated Depression and Anxiety), BIC favored the one-factor model; more importantly, the estimated factor correlation in both two-factor models exceeded 1.0, suggesting that the factors could not be reliably differentiated in this sample. The hierarchical model could not be estimated because it was underidentified. The bifactor model converged, but the factor loadings on the unique (Distress and Fear) factors were non-significant. Therefore, we concluded that the unique factors would not be useful in testing structural relations between mothers’ and offspring’s Internalizing factors. Remaining analyses utilize a one-factor model.
Table 2.
Fit data for competing structural models of internalizing disorders for mothers and offspring
| Model | Model χ2 | Model df | p | AIC | BIC | CFI | RMSEA |
|---|---|---|---|---|---|---|---|
| Mothers | |||||||
| A. One-factor (Internalizing) | 5.94 | 8 | .65 | 3351.38 | 3407.84 | .99 | .001 |
| B. Two-factor oblique (Distress, Fear) a | 6.00 | 8 | .65 | 3353.47 | 3414.62 | .99 | .001 |
| C. Two-factor oblique (Depression, Anxiety) a | 4.72 | 8 | .79 | 3353.41 | 3414.57 | .99 | .001 |
| D. Hierarchical (Internalizing, Distress, Fear) b | -- | -- | -- | 3355.64 | 3421.50 | -- | -- |
| E. Bifactor (Internalizing, Distress, Fear) c, d | -- | -- | -- | 3360.53 | 3445.21 | -- | -- |
|
| |||||||
| Offspring | |||||||
| A. One-factor (Internalizing) | 18.49 | 8 | .02 | 3183.91 | 3238.63 | .95 | .043 |
| B. Two-factor oblique (Distress, Fear) | 17.86 | 8 | .02 | 3182.50 | 3241.78 | .96 | .042 |
| C. Two-factor oblique (Depression, Anxiety) | 19.83 | 8 | .01 | 3185.09 | 3244.36 | .95 | .05 |
| D. Hierarchical (Internalizing, Distress, Fear) e, f | -- | -- | -- | -- | -- | -- | -- |
| E. Bifactor (Internalizing, Distress, Fear) d, f | -- | -- | -- | -- | -- | -- | -- |
Notes. Model A = single Internalizing factor (MDD, DYS, PTSD, GAD, SOC, SPEC, PAN), Model B = oblique two-factor with Distress (MDD, DYS, PTSD, GAD) and Fear (SOC, SPEC, PAN), Model C = oblique two-factor model with Depression (MDD, DYS) and Anxiety (PTSD, GAD, SOC, SPEC, PAN), Model D = hierarchical model with superordinate Internalizing factor and subordinate Fear (SOC, SPEC, PAN) and Distress (MDD, DYS, PTSD, GAD) factors, Model E = bifactor model with all disorders loading on Internalizing factor as well as either Fear (SOC, SPEC, PAN) or Distress (MDD, DYS, PTSD, GAD). Because of low frequency in this sample, GAD was excluded from mother models and PAN from offspring models. AIC and BIC were estimated using ML estimator; CFI and RMSEA and χ2 were estimated using WLSMV. Model A was used in all subsequent analyses.
Factor correlation was greater than or equal to one.
Using ML estimator, the factor loadings of subfactors on Internalizing were = .99. Using WLSMV, model fit could not be computed, due to fact that all factor correlations were greater than or equal to one.
None of the factor loadings on the Fear and Distress unique factors were statistically significant.
Using WLSMV estimator, fit indices were not computed due to negative variances of unique factors.
Using WLSMV, model fit indices could not be computed. Factor loading of Fear subfactor on internalizing = .92.
Using ML, model fit indices could not be computed due to non-positive definite information matrix.
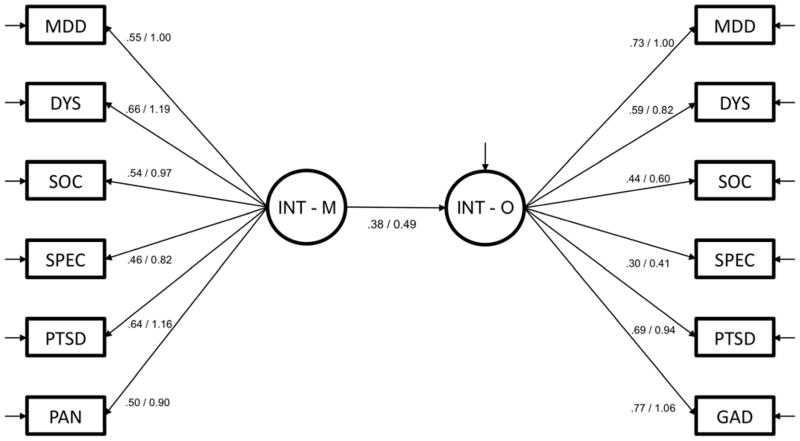
As indicated in Table 2, fit statistics for the factor model for mothers and offspring indicated that the unidimensional latent variable models provided an excellent fit to the data. All factor loadings on both factors were significant at an alpha level of .01, as displayed in Figure 1.
Figure 1.
A hierarchical-spectrum model of the intergenerational transmission of internalizing psychopathology.
Notes. Standardized/unstandardized coefficients. INT-M= Maternal Internalizing Factor (all observed variables loading on this latent factor reflect maternal diagnoses). INT-O= Offspring Internalizing Factor (all observed variables loading on this factor reflect offspring diagnoses). PAN= panic disorder or agoraphobia, MDD= major depressive disorder, SPEC= specific phobia, SOC= social phobia, DYS= dysthymia, PTSD= posttraumatic stress disorder, GAD= generalized anxiety disorder. For clarity of presentation, the correlations between residual variances—representing intergenerational transmission of diagnosis-specific pathology—are not depicted (see Table 3).
Intergenerational Transmission of Internalizing Disorders
The regression of the Offspring Internalizing factor on the Maternal Internalizing factor was significant with a moderate effect size (b =0.51, SE =0.12, p< .0001, β =.38), as illustrated in Figure 1. Gender moderation was tested using the DIFFTEST option in Mplus to examine whether constraining the path linking the maternal and offspring latent variables to equality across genders significantly reduced fit. The change in fit was not significant, χ2(1) = 2.58, p > .05, suggesting no differences in intergenerational associations by gender. Additionally, controlling for gender produced equivalent results.
To test residual correlations, we individually added pathways between residual terms for each disorder (an identical significance pattern was obtained when all residual correlations were entered simultaneously). As displayed in Table 3, none of the residual correlations among internalizing diagnoses were significant, with the exception of PTSD, which showed a significant residual association between mother and offspring disorder-specific components (β= .27, p< .05). As an additional test of disorder-specific associations, we examined whether model fit was improved by adding residual correlations. Compared to a model with no residual correlations (χ2(53)=82.11, p=.01, BIC= 6711.43, CFI= .94, RMSEA= .26), adding the PTSD correlation did not improve the BIC (6714.02) but did improve the CFI (.95) and RMSEA (.24), providing mixed evidence of model improvement (note that BIC penalizes increased model complexity). Residual pathways for other disorders did not improve fit. Taken together, findings offer tentative support for PTSD-specific effects, but not for other disorders. We used chi-square difference testing comparing nested models to evaluate the equivalence of residual correlations across gender, and found no significant gender differences in disorder-specific intergenerational transmission (ps >.05).
Table 3.
Associations between diagnosis-specific components of maternal and offspring internalizing disorders.
| Diagnosis | b | SE | β |
|---|---|---|---|
| Maternal Major Depression → Offspring Major Depression | −0.17 | 0.10 | −.14 |
| Maternal Dysthymia → Offspring Dysthymia | 0.12 | 0.08 | .13 |
| Maternal Social Phobia → Offspring Social Phobia | −0.21 | 0.12 | −.21 |
| Maternal Specific Phobia → Offspring Specific Phobia | 0.12 | 0.09 | .12 |
| Maternal Posttraumatic Stress Disorder → Offspring Posttraumatic Stress Disorder | 0.29 | 0.14 | .27* |
p < .05.
Similar results were obtained when both offspring and maternal factors were limited to the same diagnoses (i.e., those meeting the 5% frequency threshold in both groups, with OCD, GAD, and PAN excluded), with comparable fit (χ2(34) = 55.70, p = .01, CFI = .93, RMSEA = .028) and correlation between latent INT factors (β = .40), and unchanged pattern of residual correlations.
Discussion
A large body of research persuasively links maternal depression with negative outcomes among offspring (Goodman and Gotlib, 1999, Goodman et al., 2011), but most studies do not account for the co-occurrence among internalizing disorders, leaving it unclear if maternal depression exerts a unique influence on offspring psychopathology, or examine if effects are related to its comorbidity with other internalizing diagnoses. Likewise, most previous studies examine individual offspring psychological disorders in isolation as outcomes, without controlling for their shared features. The current study applied latent variable modeling to clarify the extent to which intergenerational transmission occurs via disorder-specific versus transdiagnostic pathways.
As a preliminary step, we tested alternative structural models of internalizing disorders, and found that a unidimensional model (with a single latent factor representing shared variance across all internalizing disorders) provided the best fit to diagnostic correlations in the current sample. We then showed that transmission of internalizing disorders from mother to offspring is largely explained by the influence of this maternal Internalizing factor on the corresponding offspring factor. In contrast, with the exception of PTSD, mothers’ standing on diagnosis-specific forms of pathology (including MDD) was unrelated to offspring standing on these same constructs. This implies that, in large part, transmission of internalizing disorders is non-specific, with depression predicting risk for anxiety disorders and vice versa (fitting with other data; McLaughlin et al., 2012). Stated differently, mothers seem to pass down a general propensity to develop internalizing disorders, rather than risk for one particular disorder.
These findings carry several important implications. First, they suggest that bivariate associations between specific maternal and offspring diagnoses largely reflect the effects of a more general concordance of transdiagnostic pathology across generations, and should thus be interpreted with this in mind. Second, they suggest that mechanisms linking maternal and offspring anxiety and depression may operate predominantly via the overarching Internalizing trait. The current study was not designed to adjudicate between genetic and behavioral models of intergenerational transmission, and it is virtually certain that both factors contribute. That said, results may help inform future work on genetic and psychosocial models of transmission, as they suggest that that (a) genetic vulnerabilities (and other biological mechanisms, such as in utero conditions) may be more likely to predispose to standing on the broad Internalizing factor, rather than specific aspects of individual disorders (see Corley et al., 2008, Dick et al., 2008), and (b) psychosocial mechanisms of intergenerational transmission may be most influenced by shared internalizing features. Researchers point to a range of psychosocial mediators for the intergenerational transmission of depression, including parenting style, attachment, familial environment, interpersonal chronic stress, and disruptions in social competence (Burt et al., 2005, Elgar et al., 2004, Goodman and Gotlib, 1999, Hammen et al., 2004), and similarly, several factors (e.g., income and social resources) may jointly influence both maternal and offspring depression (Elgar et al., 2004). Current findings raise the possibility that these factors are most closely linked to common features of internalizing disorders, rather than unique components of depression.
In an important exception, PTSD showed evidence of disorder-specific transmission, although findings are tentative and require replication. Yehuda et al. (2001a) similarly found that parental PTSD specifically predicted offspring PTSD controlling for other anxiety disorders and depression in a sample of children of Holocaust survivors. Shared exposure to traumatic events (or shared contexts that promote likelihood of trauma exposure, such as poverty or chaotic environments) may explain the unique correspondence of diagnosis-specific aspects of PTSD between mother and child. Offspring of parents with PTSD also show greater exposure to traumas perpetrated by the PTSD-affected parent, such as neglect or emotional abuse (Yehuda et al., 2001b) and generally higher stress levels (Brand et al., 2011). Studies also suggest that offspring of mothers with PTSD show reduced salivary cortisol levels starting in infancy (Yehuda et al., 2005, Yehuda et al., 2007), and this in turn may elevate risk for PTSD in response to traumatic events (Delahanty et al., 2003, Raison and Miller, 2003). Interpreted in conjunction with the current results, PTSD may be one case where intergenerational transmission does not exclusively occur via transdiagnostic processes.
With the exception of PTSD, there was little evidence for specific transmission of individual disorders. On one hand, this could be interpreted as supporting the “lumper” position that the unique components of internalizing disorders are relatively unimportant, at least in terms of intergerational transmission of internalizing problems. Although more research is decidedly needed to determine whether diagnostic boundaries are fundamentally meaningful, we caution against blunt interpretations of current results given certain study limitations. First, we excluded disorders with low frequencies in this sample, and as mothers and offspring disorders exhibited different frequencies, different disorders were included on mother and child Internalizing factors. This contributed to dissimilarity between offspring and maternal latent Internalizing factors, which may have influenced intergenerational associations (although comparable results were produced when restricting both latent variables to diagnoses meeting the 5% threshold for both mothers and offspring). It is also possible that some of the excluded diagnoses (such as GAD) would show specific transmission. There may also be developmental differences in the structure of psychopathology, producing differences in latent and residual variables between mothers and offspring.
Further, our sample was overselected for maternal depression, and while this allowed for sufficient representation of clinically significant symptoms, results may differ in unselected samples. Also, cross-diagnostic associations (e.g., maternal depression predicting offspring social phobia) were not tested in the current study. Moreover, there has been limited research on the construct validity of the diagnosis-specific components of disorders in the HSM framework. Although researchers have speculated about what the disorder-specific components represent (e.g., anhedonia in MDD; Watson et al., 1995), further work is needed to evaluate whether these diagnosis-specific variances are related to external constructs in theoretically-plausible ways (Eaton et al., 2012b, Krueger and Markon, 2011, Simms et al., 2012). In addition, diagnosis-specific effects may be underestimated because of imperfect measurement reliability of individual diagnoses.
Finally, the lack of disorder-specific effects may be related to the age of the offspring in our sample. For example, some evidence suggests that the majority of the depressive effects of maternal depression manifests by age 15 (Hammen et al., 2008). First onsets of depression between age 15 and age 20 (when youth in the current study were assessed) may reflect transient episodes with other etiological roots; thus, examining transmission at an earlier age may reveal a stronger specific effect for depression.1 On the other hand, while most depressive effects of maternal depression emerge by mid-adolescence, depression-specific effects (as opposed to a general diathesis toward internalizing disorders) could potentially emerge later, as depression tends to have later onset than anxiety disorders (Kessler et al., 2005). If so, older samples may demonstrate depression-specific transmission.
Several additional limitations should also be considered. Our model included only maternal psychopathology, and several studies have suggested the importance of paternal or even grandparental effects (e.g., Brennan et al., 2002, Hammen et al., 2004, Pettit et al., 2008, Warner et al., 1999), although Tully et al. (2008) demonstrated that paternal depression has negligible impact on internalizing psychopathology. In addition, we could not evaluate transmission of the externalizing spectrum because these diagnoses were not well-represented among the mothers in our sample. Using similar methods, Hicks et al. (2004) found support for general transmission of externalizing disorders.
Finally, we used categorically-defined diagnoses as indicators of the latent Internalizing spectra, which excluded potentially important subthreshold symptoms. Dimensional indicators would be statistically preferable (Fergusson et al., 2006, Markon, 2010, Wright et al., in press), although note that numerous prominent studies examining the latent structure of psychopathology have also used categorical indicators (Cox et al., 2002, Eaton et al., 2012b, Krueger, 1999, Krueger et al., 1998, Krueger and Finger, 2001, Slade and Watson, 2006, Vollebergh et al., 2001) Our study is perhaps best interpreted as examining how internalizing disorders strictly as defined by the DSM-IV are transmitted from mothers to offspring. As mounting evidence suggests that few diagnostic constructs are truly taxonic (Haslam et al., 2012), it is possible that measuring the constructs using methods more in line with their natural psychometric properties (e.g., dimensional; Prisciandaro and Robert, 2009) would yield greater disorder-specific effects.
Although our data were most consistent with a single-factor model of internalizing pathology, different structural models may be more appropriate in other datasets. For example, our use of binary data may have limited our ability to fit more complex models. Future research should explore whether lower-order internalizing factors identified in prior studies (e.g., Fear versus Distress/Anxious Misery; Krueger, 1999, Prenoveau et al., 2010) are transmitted specifically from parents to offspring.
These limitations notwithstanding, the current study supplies new evidence that transdiagnostic processes may substantially account for intergenerational transmission of internalizing problems, challenging the assumption that maternal depression exerts a unique effect on offspring depression. This raises an interesting question: to the extent that children inherit (genetically or psychosocially) vulnerability to a general internalizing propensity rather than specific disorders, what factors then determine which specific internalizing disorders ultimately manifest, and where do these factors originate (if not from parental sources)? Researchers have begun to identify specific risk factors that predict anxiety versus depression, controlling for shared features (e.g., Craske et al., 2012), but more work is needed to better understand the unique etiologies of separate internalizing disorders. Ultimately, the current study suggests that, although a considerable volume of research has treated depression as a special class of disorder with unique effects, it may be better understood as a manifestation of a broader Internalizing trait, with causes and consequences that cut across diagnostic boundaries. As such, adopting a transdiagnostic perspective may facilitate exploration of key psychopathological processes.
Acknowledgments
This research was supported by NIMH R01MH052239 and NIMH T32MH082719. We are grateful to the MUSP, M900, and M20 Research Teams, and to the parents and youth in the Mater Cohort for their participation in this study. Particular thanks to project coordinators Robyne LeBrocque, Cheri Dalton Comber and Sascha Hardwicke. The cooperation of Professor Jake Najman of the University of Queensland and head of the MUSP program is gratefully acknowledged.
Footnotes
Declaration of Interest
None.
We also attempted to fit an analogous model using offspring lifetime diagnoses up to age 15, but the model showed inadequate fit due to low frequency of several diagnoses at that age.
Contributor Information
Lisa R. Starr, University of California, Los Angeles
Christopher C. Conway, University of California, Los Angeles
Constance Hammen, University of California, Los Angeles.
Patricia A. Brennan, Emory University
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Author; Washington, D.C: 1994. [Google Scholar]
- Bedford A, Foulds G. Delusions-Symptoms-States Inventory of Anxiety and Depression. NFER; Windsor, England: 1978. [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Billings AG, Moos R. Children of parents with unipolar depression: A controlled 1-year follow-up. Journal of Abnormal Child Psychology. 1985;14:149–166. doi: 10.1007/BF00917230. [DOI] [PubMed] [Google Scholar]
- Brand SR, Schechter JC, Hammen CL, Brocque RL, Brennan PA. Do adolescent offspring of women with PTSD experience higher levels of chronic and episodic stress? Journal of Traumatic Stress. 2011;24:399–404. doi: 10.1002/jts.20652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan PA, Hammen C, Katz AR, Le Brocque RM. Maternal depression, paternal psychopathology, and adolescent diagnostic outcomes. Journal of Consulting and Clinical Psychology. 2002;70:1075–1085. doi: 10.1037//0022-006x.70.5.1075. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. Classification of anxiety and mood disorders. In: Barlow DH, editor. Anxiety and its Disorders: The Nature and Treatment of Anxiety and Panic. Guilford; New York: 2002. pp. 292–327. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- Burt KB, Van Dulmen MHM, Carlivati J, Egeland B, Alan Sroufe L, Forman DR, Appleyard K, Carlson EA. Mediating links between maternal depression and offspring psychopathology: the importance of independent data. Journal of Child Psychology and Psychiatry. 2005;46:490–499. doi: 10.1111/j.1469-7610.2004.00367.x. [DOI] [PubMed] [Google Scholar]
- Conway CC, Hammen C, Brennan PA. Expanding Stress Generation Theory: Test of a Transdiagnostic Model. Journal of Abnormal Psychology. doi: 10.1037/a0027457. (in press) No Pagination Specified. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corley RP, Zeiger JS, Crowley T, Ehringer MA, Hewitt JK, Hopfer CJ, Lessem J, McQueen MB, Rhee SH, Smolen A, Stallings MC, Young SE, Krauter K. Association of candidate genes with antisocial drug dependence in adolescents. Drug and Alcohol Dependence. 2008;96:90–98. doi: 10.1016/j.drugalcdep.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox AD, Puckering C, Pound A, Mills M. The impact of maternal depression in young children. Journal of Child Psychology and Psychiatry. 1987;28:917–928. doi: 10.1111/j.1469-7610.1987.tb00679.x. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Clara IP, Enns MW. Posttraumatic stress disorder and the structure of common mental disorders. Depression and Anxiety. 2002;15:168–171. doi: 10.1002/da.10052. [DOI] [PubMed] [Google Scholar]
- Craske MG, Wolitzky-Taylor KB, Mineka S, Zinbarg R, WAters AM, Vrshek-Schalihorn S, Epstein A, Naliboff B, Ornitz E. Elevated responding to safe conditions as a specific risk factor for anxiety versus depressive disorders: Evidence from a longitudinal investigation. Journal of Abnormal Psychology. 2012;121:315–324. doi: 10.1037/a0025738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delahanty DL, Raimonde AJ, Spoonster E, Cullado M. Injury severity, prior trauma history, urinary cortisol levels, and acute PTSD in motor vehicle accident victims. Journal of Anxiety Disorders. 2003;17:149–64. doi: 10.1016/s0887-6185(02)00185-8. [DOI] [PubMed] [Google Scholar]
- Dick DM, Aliev F, Wang JC, Grucza RA, Schuckit M, Kuperman S, Kramer J, Hinrichs A, Bertelsen S, Budde JP. Using dimensional models of externalizing psychopathology to aid in gene identification. Archives of General Psychiatry. 2008;65:310. doi: 10.1001/archpsyc.65.3.310. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Whittle L, Lim C, Wechsler H. Youth risk behavior surveillance - United States, 2011. MMWR. Surveillance Summaries. 2012a;61:1–162. [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Markon KE, Keyes KM, Skodol AE, Wall M, Hasin DS, Grant BF. The Structure and Predictive Validity of the Internalizing Disorders. The Journal of Abnormal Psychology. 2012b doi: 10.1037/a0029598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elgar FJ, McGrath PJ, Waschbusch DA, Stewart SH, Curtis LJ. Mutual influences on maternal depression and child adjustment problems. Clinical Psychology Review. 2004;24:441–459. doi: 10.1016/j.cpr.2004.02.002. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Boden JM. Structure of internalising symptoms in early adulthood. The British Journal of Psychiatry. 2006;189:540–546. doi: 10.1192/bjp.bp.106.022384. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clinical child and family psychology review. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Griffith JW, Zinbarg RE, Craske MG, Mineka S, Rose RD, Waters AM, Sutton JM. Neuroticism as a common dimension in the internalizing disorders. Psychological Medicine. 2010;40:1125. doi: 10.1017/S0033291709991449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halligan SL, Murray L, Martins C, Cooper PJ. Maternal depression and psychiatric outcomes in adolescent offspring: a 13-year longitudinal study. Journal of Affective Disorders. 2007;97:145–54. doi: 10.1016/j.jad.2006.06.010. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan P, Keenan-Miller D. Patterns of Adolescent Depression to Age 20: The Role of Maternal Depression and Youth Interpersonal Dysfunction. Journal of Abnormal Child Psychology. 2008;36:1189–1198. doi: 10.1007/s10802-008-9241-9. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA. Depressed adolescents of depressed and nondepressed mothers: Tests of an Interpersonal Impairment Hypothesis. Journal of Consulting and Clinical Psychology. 2001;69:284–294. doi: 10.1037//0022-006x.69.2.284. [DOI] [PubMed] [Google Scholar]
- Hammen C, Burge D, Burney E, Adrian C. Longitudinal study of diagnoses in children of women with unipolar and bipolar affective disorder. Archives of General Psychiatry. 1990;47:1112–1117. doi: 10.1001/archpsyc.1990.01810240032006. [DOI] [PubMed] [Google Scholar]
- Hammen C, Shih JH, Brennan PA. Intergenerational Transmission of Depression: Test of an Interpersonal Stress Model in a Community Sample. Journal of Consulting and Clinical Psychology. 2004;72:511–522. doi: 10.1037/0022-006X.72.3.511. [DOI] [PubMed] [Google Scholar]
- Haslam N, Holland E, Kuppens P. Categories versus dimensions in personality and psychopathology: a quantitative review of taxometric research. Psychological Medicine. 2012;42:903–920. doi: 10.1017/S0033291711001966. [DOI] [PubMed] [Google Scholar]
- Hicks BM, Krueger RF, Iacono WG, McGue M, Patrick CJ. Family transmission and heritability of externalizing disorders: A twin-family study. Archives of General Psychiatry. 2004;61:922–928. doi: 10.1001/archpsyc.61.9.922. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keeping JD, Najman JM, Morrison J, Western JS, Anderson MJ, Williams GM. A prospective longitudinal study of social, psychological, and obstetrical factors in pregnancy: Response rates and demographic characteristics of the 8,556 respondents. British Journal of Obstetrics and Gynaecology. 1989;96:289–297. doi: 10.1111/j.1471-0528.1989.tb02388.x. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Davis CG, Kessler RC. The familial aggregation of common psychiatric and substance use disorders in the National Comorbidity Survey: a family history study. British Journal of Psychiatry. 1997;170:541–548. doi: 10.1192/bjp.170.6.541. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Walters EE. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Klein DN, Lewinsohn PM, Rohde P, Seeley JR, Olino TM. Psychopathology in the adolescent and young adult offspring of a community sample of mothers and fathers with major depression. Psychological Medicine. 2005;35:353–65. doi: 10.1017/s0033291704003587. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): A longitudinal-epidemiological study. Journal of Abnormal Psychology. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Finger MS. Using item response theory to understand comorbidity among anxiety and unipolar mood disorders. Psychological Assessment. 2001;13:140–151. [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting Comorbidity: A Model-Based Approach to Understanding and Classifying Psychopathology. Annual Review of Clinical Psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. A dimensional-spectrum model of psychopathology: Progress and opportunities. Archives of General Psychiatry. 2011;68:10–11. doi: 10.1001/archgenpsychiatry.2010.188. [DOI] [PubMed] [Google Scholar]
- Last CG, Hersen M, Kazdin AE, Francis G, Grubb HJ. Psychiatric illness in the mothers of anxious children. American Journal of Psychiatry. 1987;144:1580–1583. doi: 10.1176/ajp.144.12.1580. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seely JR. Major depressive disorder in older adolescents: Prevalence, risk factors, and clinical implications. Clinical Psychology Review. 1998;18:765–794. doi: 10.1016/s0272-7358(98)00010-5. [DOI] [PubMed] [Google Scholar]
- Lieb R, Isensee B, Hofler M, Pfister H, Wittchen HU. Parental major depression and the risk of depression and other mental disorders in offspring: a prospective-longitudinal community study. Archives of General Psychiatry. 2002;59:365–74. doi: 10.1001/archpsyc.59.4.365. [DOI] [PubMed] [Google Scholar]
- Markon KE. Modeling psychopathology structure: A symptom-level analysis of Axis I and II disorders. Psychological Medicine. 2010;40:273–288. doi: 10.1017/S0033291709990183. [DOI] [PubMed] [Google Scholar]
- McClure EB, Brennan PA, Hammen C, Le Brocque RM. Parental anxiety disorders, child anxiety disorders, and the perceived parent-child relationship in an Australian high-risk sample. Journal of Abnormal Child Psychology. 2001;29:1–10. doi: 10.1023/a:1005260311313. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J-p, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) Journal of the Academy of Child & Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milne BJ, Caspi A, Crump R, Poulton R, Rutter M, Sears MR, Moffitt TE. The validity of the family history screen for assessing family history of mental disorders. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics. 2009;150B:41–49. doi: 10.1002/ajmg.b.30764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettit JW, Olino TM, Roberts RE, Seeley JR, Lewinsohn PM. Intergenerational Transmission of Internalizing Problems: Effects of Parental and Grandparental Major Depressive Disorder on Child Behavior. Journal of Clinical Child & Adolescent Psychology. 2008;37:640–650. doi: 10.1080/15374410802148129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prenoveau JM, Zinbarg RE, Craske MG, Mineka S, Griffith JW, Epstein AM. Testing a hierarchical model of anxiety and depression in adolescents: A tri-level model. Journal of Anxiety Disorders. 2010;24:334–344. doi: 10.1016/j.janxdis.2010.01.006. [DOI] [PubMed] [Google Scholar]
- Prisciandaro JJ, Robert JE. A comparison of the predictive abilities of dimensional and categorical models of unipolar depression in the National Comorbidity Survey. Psychological Medicine. 2009;39:1087–1096. doi: 10.1017/S0033291708004522. [DOI] [PubMed] [Google Scholar]
- Raison CL, Miller AH. When not enough is too much: the role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. American Journal of Psychiatry. 2003;160:1554–65. doi: 10.1176/appi.ajp.160.9.1554. [DOI] [PubMed] [Google Scholar]
- Simms LJ, Grös DF, Watson D, O’Hara MW. Parsing the general and specific components of depression and anxiety with bifactor modeling. Depression and Anxiety. 2008;25:E34–E46. doi: 10.1002/da.20432. [DOI] [PubMed] [Google Scholar]
- Simms LJ, Prisciandaro JJ, Krueger RF, Goldberg DP. The structure of depression, anxiety and somatic symptoms in primary care. Psychological Medicine. 2012;42:15–28. doi: 10.1017/S0033291711000985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological Medicine. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- South SC, Krueger RF, Iacono WG. Understanding general and specific connections between psychopathology and marital distress: A model based approach. Journal of Abnormal Psychology. 2011;120:935. doi: 10.1037/a0025417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First M. Structured Clinical Interview for DSM-IV (SCID-IV) American Psychiatric Association; Washington, D.C: 1995. [Google Scholar]
- Tully EC, Iacono WG, McGue M. An adoption study of parental depression as an environmental liability for adolescent depression and childhood disruptive disorders. The American journal of psychiatry. 2008;165:1148. doi: 10.1176/appi.ajp.2008.07091438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner SM, Beidel DC, Costello A. Psychopathology in the offspring of anxiety disorders patients. Journal of Consulting and Clinical Psychology. 1987;55:229–235. doi: 10.1037//0022-006x.55.2.229. [DOI] [PubMed] [Google Scholar]
- Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: the NEMESIS study. Archives of General Psychiatry. 2001;58:597. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- Walton KE, Ormel J, Krueger RF. The dimensional nature of externalizing behaviors in adolescence: Evidence from a direct comparison of categorical, dimensional, and hybrid models. Journal of Abnormal Child Psychology. 2011;39:553–561. doi: 10.1007/s10802-010-9478-y. [DOI] [PubMed] [Google Scholar]
- Warner V, Weissman MM, Mufson L, Wickramaratne PJ. Grandparents, Parents, and Grandchildren at High Risk for Depression: A Three-Generation Study. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:289–296. doi: 10.1097/00004583-199903000-00016. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Weber K, Assenheimer JS, Strauss ME, McCormick RA. Testing a tripartite model: II. Exploring the symptom structure of anxiety and depression in student, adult, and patient samples. Journal of Abnormal Psychology. 1995;104:15–25. doi: 10.1037//0021-843x.104.1.15. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Leckman JF, Merikangas KR, Gammon GD, Prusoff BA. Depression and anxiety disorders in parents and children: Results from the Yale family study. Archives of General Psychiatry. 1984;41:845–852. doi: 10.1001/archpsyc.1984.01790200027004. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. American Journal of Psychiatry. 2006;163:1001–8. doi: 10.1176/ajp.2006.163.6.1001. [DOI] [PubMed] [Google Scholar]
- Wright AGC, Krueger RF, Hobbs MJ, Markon KE, Eaton NR, Slade T. The Structure of Psychopathology: Toward an Expanded Quantitative Empirical Model. Journal of Abnormal Psychology. doi: 10.1037/a0030133. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehuda R, Engel SM, Brand SR, Seckl J, Marcus SM, Berkowitz GS. Transgenerational Effects of Posttraumatic Stress Disorder in Babies of Mothers Exposed to the World Trade Center Attacks during Pregnancy. Journal of Clinical Endocrinology and Metabolism. 2005;90:4115–4118. doi: 10.1210/jc.2005-0550. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Halligan SL, Bierer LM. Relationship of parental trauma exposure and PTSD to PTSD, depressive and anxiety disorders in offspring. Journal of Psychiatric Research. 2001a;35:261–270. doi: 10.1016/s0022-3956(01)00032-2. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Halligan SL, Grossman R. Childhood trauma and risk for PTSD: Relationship to intergenerational effects of trauma, parental PTSD, and cortisol excretion. Development and Psychopathology. 2001b;13:733–753. doi: 10.1017/s0954579401003170. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Teicher MH, Seckl JR, Grossman RA, Morris A, Bierer LM. Parental posttraumatic stress disorder as a vulnerability factor for low cortisol trait in offspring of holocaust survivors. Archives of General Psychiatry. 2007;64:1040–1048. doi: 10.1001/archpsyc.64.9.1040. [DOI] [PubMed] [Google Scholar]