Abstract
Although it has been shown that traffic-related air pollution adversely affects children’s lung function, few studies have examined the influence of traffic noise on this association, despite both sharing a common source.
Exposure estimates of noise (Ldn, dB), and freeway and non-freeway emission concentrations of oxides of nitrogen (NOx, ppb) were spatially assigned to children in Southern California who were tested for forced vital capacity (FVC, n=1345), forced expiratory volume in 1 second, (FEV1, n=1332), and asthma. The associations between traffic-related NOx and these outcomes, with and without adjustment for noise, were examined using mixed effects models.
Adjustment for noise strengthened the association between NOx and reduced lung function. A 14.5 mL (95 % Cl −40.0, 11.0 mL) decrease in FVC per interquartile range (13.6 ppb) in freeway NOx was strengthened to a 34.6 mL decrease after including a non-linear function of noise (95% CI −66.3, −2.78 mL).
Similarly, a 6.54 mL decrease in FEV1 (95% Cl −28.3, 15.3 mL) was strengthened to a 21.1 mL decrease (95% CI −47.6, 5.51) per interquartile range in freeway NOx.
Our results indicate that where possible, noise should be included in epidemiological studies of the association between traffic-related air pollution on lung function. Without taking noise into account, the detrimental effects of traffic-related pollution may be underestimated.
Keywords: Noise, air pollution, traffic, children’s respiratory health, lung function, negative confounding
1. Introduction
Numerous studies have examined the association between exposure to traffic-related air pollution and children’s respiratory health (e.g., Gauderman et al., 2007; McConnell et al., 2010; Rice et al., 2016; Urman et al., 2014). Long-term exposure to nitrogen oxides (NO, NO2, NOx), leads to a reduction in lung development in children (Gauderman et al., 2004; 2007). Fortunately, decreases in air pollution in Southern California over the past 17 years have led to significant reductions in these detrimental effects (Gauderman et al., 2015). Traffic is also a source of noise, but the joint effects of noise and air pollution on children’s respiratory health have not been studied in the U.S. despite high noise exposures. Noise levels in U.S. urban areas generally exceed the World Health Organization (WHO) community noise guideline (WHO, 1999) of 55 decibels (dB) for a day-evening noise average that includes a 10 dB evening and night penalty (“Ldn”). In downtown Los Angeles during the daytime (9am–5pm with no 10 dB penalty), the measured mean noise level at 26 locations was 66.4 dB, exceeding the WHO guideline by more than 10 dB (Lee et al., 2014). At the most extreme, an estimated 90% of New York City residents were exposed to noise levels greater than 70 dB (Neitzel et al., 2012).
In Europe, traffic noise ranks second, behind fine particles, as the environmental risk factor with the highest health impact (Hänninen et al., 2014). Studies of noise as an environmental stressor have shown associations with a variety of health outcomes including annoyance, sleep deprivation, cardiovascular disease prevalence, and premature mortality (Stansfeld, 2015). In children, noise has deleterious effects on behavioral (Tiesler et al., 2013), mental (Dreger et al., 2015), cardiovascular (Belojevic et al., 2008; Bilenko et al., 2013; Liu et al., 2014), and respiratory health (Ising et al., 2003, 2004; Niemann et al., 2006; Linares et al., 2006). In Madrid, noise (>80% of which is attributed to traffic sources) was found to be the variable most strongly associated with child hospitalization for respiratory causes in general, ahead of cold weather, and for pneumonia, ahead of pollen. These models included NOx, ozone and PM10 (Linares et al., 2006). In the Harz Mountain region of Northern Germany, a study of 400 children found that those with self-reported exposures to heavy lorry and motorcar traffic due to bedrooms facing traffic had high risk ratios for chronic bronchitis 10.8 (95% Cl 5.2, 22.4) (Ising et al., 2003). While air pollution and noise were not measured in that study, follow-up measurements of NO2 and noise outside of child bedroom windows (10pm – 6 am), along with salivary cortisol in a sub-study of 68 children (Ising et al., 2004) verified that noise levels above 54 dB and NO2 above ~21 ppb were associated with increased morning cortisol and increased doctor visits for bronchitis. Morning cortisol was a stronger predictor than NO2, indicating the stressful aspect of traffic noise may have been the driving mechanism of illness. In this study, we investigated the associations between traffic-related air pollution and noise on children’s respiratory health by taking advantage of a large, preexisting cohort of children in Southern California. While the association between air pollution and respiratory health has been studied extensively using this cohort, the role of noise has not. Our investigation of the dynamics between NOx, noise, and lung function begins with the a priori and scientifically substantiated hypothesis that there is an association between respiratory outcomes (Y) and air pollution (X) (Gauderman et al., 2004; 2007; 2015), and then consider the role of a third variable, noise (Z) on this relationship. We also hypothesized that while X has a direct effect on Y, Z plays an indirect role in that its inclusion in the regression allows for a more concise estimate of the association between X and Y. We specifically tested the associations (marginal and joint) between traffic NOx exposure, traffic noise, and children’s lung function measurements of forced expiratory volume in one second (FEV1, mL), forced vital capacity (FVC, mL), and asthma.
2. Material and Methods
2.1 Study Population
Since its inception in the early 1990s, the Southern California Children’s Health Study (CHS) has enrolled over 11,000 children in a series of five cohorts. In this study, we focused on the most recent cohort enrolled in 2002–3 at ages 5–7 years and examined in 2011–12 when they were 14–17 years old. There was a total of 5,000 children, and those receiving lung function tests (approximately 1,400 children) resided and went to school in eight communities in the greater Los Angeles, California area: Anaheim, Glendora, Long Beach, Mira Loma, Riverside, Santa Barbara, San Dimas, and Upland (Figure 1). The CHS was designed to capture gradients of traffic emissions, with some communities (e.g. Anaheim) having many study subjects’ residential locations close to freeways to ensure that a portion of the cohort would have high freeway emission exposures as well as high noise exposures. Additional details of CHS community and subject selection have been previously reported (Peters et al., 1999; McConnell et al. 2006).
Figure 1.
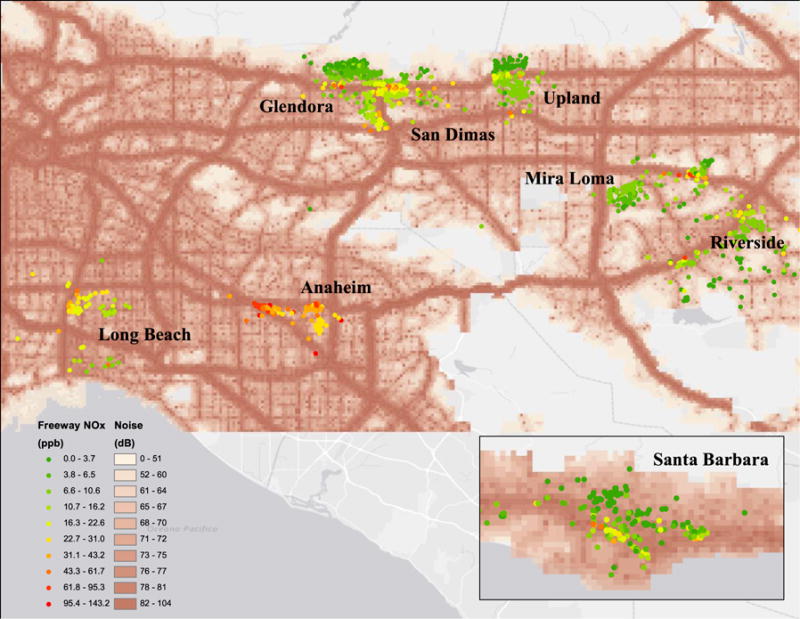
Map of study area with noise estimates (Ldn, dB) in the Southern California region and freeway NOx concentrations (ppb) at locations of subjects in the 8 CHS communities.
2.2 Health Outcomes
Pulmonary function tests were conducted on each child by trained respiratory staff. FEV1 and FVC were measured using pressure transducer-based spirometers (Screenstar Spirometers, Morgan Scientific, Haverhill, Massachusetts, USA). Asthma status was based on physician diagnoses, confirmed by a written questionnaire that also obtained information including age, sex, self-identified race and ethnic background, parental education, occurrences of acute respiratory illness, exercise, tobacco-smoke exposure (personal smoking or environmental), and house characteristics (air conditioning, age of house, presence of mildew, pets in the home). Ethnic background in the CHS specifically relates to Hispanic ancestry, identifying Caucasian subjects with Hispanic and non-Hispanic ethnicity.
2.3 Environmental Exposures
2.3.1 Air Pollution
We applied the CALINE4 line source dispersion model (Benson, 1992) to estimate annual average ambient concentration of NOx from local traffic at each subject’s residence for the calendar year preceding each child’s lung function test. The CALINE4 dispersion model uses residential locations, roadway geometry, vehicle traffic volume and emission rate by roadway link, and meteorological conditions as inputs. The estimated pollutant exposures included both freeway and non-freeway sources separately, and are regarded as indicators of incremental increases in air pollution over background ambient levels due to primary emissions from local vehicular traffic. CALINE4-estimated freeway NOx has been shown to explain much of the local-scale spatial variation in annual average ambient NO2 and NOx concentrations in Southern California (Franklin et al., 2012). A separate variable for distance from each study subject’s residential location to the nearest freeway was also examined.
2.3.2. Noise
The U.S. Federal Highway Administration (FHWA) developed the Traffic Noise Model (TNM) (FHWA, 2004) to estimate noise caused by vehicle traffic in order to aid in policy compliance for federal highway projects. The most recent validated version, TNM 2.5, (Shu et al., 2007) uses roads, hourly traffic volume, speed, pavement type, and type of vehicle (cars, heavy trucks, light trucks, buses and motorcycles). Specific data we used as inputs include average daily traffic volume obtained from Kalibrate (http://www.kalibrate.com/) and road segments information from HERE (https://company.here.com/). Output from TNM includes highway traffic noise in terms of an average day-night sound level (Ldn), which is an average noise decibel level over a day including a 10 dB penalty applied from 10:00 pm to 7:00 am.
HowLoud, Inc., a Los Angeles based company (http://howloud.com/), built the computational infrastructure to enable efficient implementation of TNM 2.5 to the thousand largest urban regions in the United States. They acquired TNM inputs for the U.S. over the years 2013–15, enabling uniform noise estimation on a national scale. For our study, HowLoud provided temporally averaged noise estimates for the Southern California region on a 100 m spatial grid, which we spatially matched to each CHS study subject’s residential location (see Figure 1).
2.4 Statistical Methods
Since study subjects were distributed within eight distinct communities over the Southern California region, mixed effects models were fit incorporating a random effect for community to allow for variations in regional (background) pollution by community. This approach was taken in previous studies involving the CHS data (McConnell et al. 2010, Jerrett et al. 2014). The associations between measured FVC and FEV1 and the traffic-related effects of interest, NOx and noise, were examined after adjustment for subject age, sex, height, weight, body mass index (BMI), race/ethnicity, housing characteristics (year built, presence of pets, water damage, mildew, pests), parental education level, exercise, and tobacco smoke. To examine noise as a potential effect modifier of the association between NOx and respiratory outcomes, we included interaction terms between NOx and noise.
Noise was included both as a continuous variable and as a categorical variable defined by groups with cutoff values for the 5th, 25th, 50th, 75th, and 95th percentiles of its distribution. To examine noise as a possible confounder, we included noise linearly on the continuous scale, and accounted for a potential non-linear effect with inclusion of polynomial terms or cubic regression splines in a generalized additive model framework (Wood, 2006). Sensitivity analyses of the non-linear function of noise were conducted by varying the number of degrees of freedom of the cubic regression spline to ensure we were not overfitting the data.
NOx was modeled as a linear effect to provide an interpretable parameter estimate. Nevertheless, sensitivity analyses were conducted by modeling NOx with polynomials and regression splines to assess whether non-linear functions were more suitable.
For asthma, logistic mixed effects models were fit with the same covariate adjustments. Residual spatial correlation within each community was examined with mixed effects models with the addition of spatial covariance terms. In all models, higher order terms were included as orthogonal polynomials in order to avoid collinearity. Model sensitivity analyses were conducted through a leave-one-community-out cross-validation approach, leaving one entire community out of the dataset, refitting the models in each iteration, and examining changes in the effect estimates.
3. Results
The study population consisted of girls (52%) and boys (48%) of mean age 15.2 years with mean spirometric FEV1 (3673 mL) and FVC (4237 mL) measurements, and doctor diagnosed asthma (21%). Details of their physical characteristics, lung function, housing characteristics, and exposure levels of NOx and noise are shown in Table 1. Across communities the mean concentrations of non-freeway and freeway NOx were 4.8 (SD=2.7) ppb and 14.6 (SD=16.5) ppb, respectively. The community-specific distributions of freeway NOx and noise are shown in Figure 2. Of these communities, Anaheim had the highest average and most variable freeway NOx concentrations (47.7, SD =26.6 ppb). Glendora and Santa Barbara had the lowest average freeway NOx concentrations (7.8 and 8.4 ppb, respectively). The mean Ldn was 72 dB, far exceeding the WHO guideline, with the highest average noise levels observed in Anaheim (77.3 dB), and the lowest in Mira Loma (68.7 dB).
Table 1.
Characteristics of the study population
| Number of Subjects | % or mean (SD) | |
|---|---|---|
| Subjects | ||
| Boys | 671 | 48% |
| Girls | 726 | 52% |
| Age (years) | 1397 | 15.2 (0.6) |
| Height (cm) | 1397 | 166.1 (8.6) |
| Weight (lbs) | 1397 | 141.8 (35.0) |
| Race | ||
| Asian | 70 | 5% |
| African American | 30 | 2% |
| Caucasian | 594 | 43% |
| Mixed | 182 | 13% |
| Other | 338 | 24% |
| Unknown or missing | 183 | 13% |
| Ethnicity | ||
| Hispanic | 745 | 53% |
| Non-Hispanic | 585 | 42% |
| Unknown or missing | 67 | 5% |
| Forced Vital Capacity (mL) | 1345 | 4237 (851) |
| Forced Expiratory Volume (mL) | 1332 | 3673 (698) |
| Asthma | 1342 | 21% |
| Exposures | ||
| Distance to fwy (km) | 1397 | 1.4 (1.1) |
| Freeway NOx (ppb) | 1397 | 14.6 (16.5) |
| Non-freeway NOx (ppb) | 1397 | 4.8 (2.7) |
| Noise (dB) | 1397 | 72 (7.5) |
| Exposure to smoke | 1393 | 6% |
| Pets in home | 1317 | 58% |
| Housing Characteristics | ||
| Air conditioning use | 1333 | 72% |
| Home Built (year) | ||
| Before 1960 | 360 | 26% |
| 1960–1979 | 410 | 29% |
| 1980 or later | 296 | 21% |
| Unknown or missing | 331 | 24% |
| Communities | ||
| Anaheim | 136 | 10% |
| Glendora | 253 | 18% |
| Long Beach | 93 | 7% |
| Mira Loma | 190 | 14% |
| Riverside | 162 | 12% |
| Santa Barbara | 172 | 12% |
| San Dimas | 202 | 14% |
| Upland | 189 | 13% |
Figure 2.
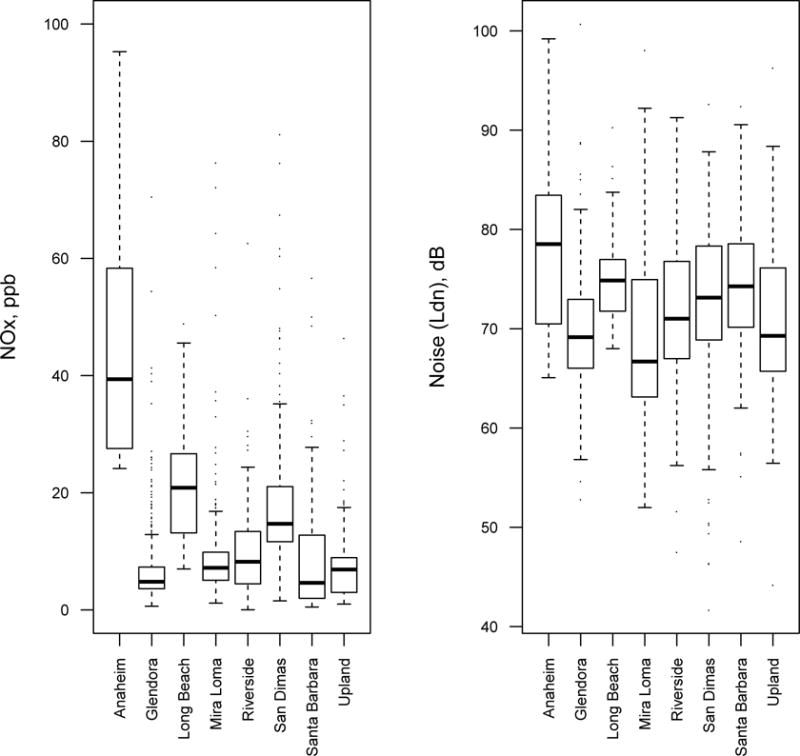
Distributions of freeway NOx (left) and noise (right) at subject homes in each of the 8 CHS communities.
The Pearson correlations between freeway NOx, non-freeway NOx and noise were r = 0.53 and r = 0.33, respectively. There was also a moderate inverse correlation between distance to freeway and noise (r = −0.57), as well as between distance to freeway and freeway NOx (r = −0.52) (Table 2). The community-specific correlations between freeway NOx and noise indicated a consistent pattern in all communities (r = 0.53 to 0.65) except for in Long Beach, where the correlation was much lower (r = 0.13). The community specific correlations between freeway NOx and distance to freeway ranged from −0.51 in Upland to −0.84 in Long Beach. To avoid highly correlated variables, we did not include both freeway NOx and distance to freeway in our models.
Table 2.
Pearson correlation coefficients between key exposure variables
| Noise (dB) | Freeway NOx (ppb) | Non-Freeway NOx (ppb) | Distance to Freeway (km) | |
|---|---|---|---|---|
| Noise (dB) | 1.00 | 0.53 | 0.33 | −0.57 |
| Freeway NOx (ppb) | 1.00 | 0.38 | −0.52 | |
| Non-Freeway NOx (ppb) | 1.00 | −0.19 | ||
| Distance to Freeway (km) | 1.00 |
The mixed effects model that included adjustment for age, height, height squared, BMI, BMI squared, sex, race, freeway NOx and a random intercept for community showed a non-significant 14.5 mL decrease (95 % Cl −40.0, 11.0) in FVC associated with an IQR increase in freeway NOx (13.6 ppb) (Table 3). After adjusting for a linear, cubic polynomial, or categorical effect of noise, the FVC decrease associated with an IQR increase in freeway NOx was 27.7 mL (95 % CI −57.0, 1.5), 29.2 mL (95 % CI −59.9, 1.5), and 29.7 mL (95 % CI −60.8, 1.4), respectively. When noise was adjusted using a cubic regression spline, there was a statistically significant 34.6 mL decrease (95 % CI −66.3, −2.8) in FVC per IQR increase in freeway NOx. This last result represents a clinically important (−139%) change in the association between freeway NOx and FVC with the inclusion of noise in the baseline linear model that did not include any adjustment for noise (Figure 3). Varying the number of degrees of freedom of the regression spline between 5 and 10 yielded similar effect sizes that were all statistically significant (p ≤ 0.05). In Table 3 and Figure 3 we present the results of the model including a regression spline with 7 degrees of freedom. The shape of the fitted spline function followed a cubic functional form, in line with the cubic polynomial results (Figure 4).
Table 3.
Freeway NOx exposure effect estimates by model and outcome (in mL per IQR increase in NOx concentration, 13.6 ppb)*
| Model | Outcome | Effect Estimate (95% CI) |
|---|---|---|
| NOx | FVC | −14.5 (−40.0, 11.0) |
| NOx + noise linear | FVC | −27.7 (−56.7, 1.50)a |
| NOx + noise cubic | FVC | −29.2 (−59.9, 1.53)a |
| NOx + noise categories | FVC | −29.7 (−60.8, 1.39)a |
| NOx + noise splines | FVC | −34.6 (−66.3, −2.78)b |
| NOx | FEV1 | −6.54 (−28.3, 15.3) |
| NOx + noise linear | FEV1 | −17.1 (−41.7, 7.51) |
| NOx + noise cubic | FEV1 | −17.8 (−43.6, 7.98) |
| NOx + noise categories | FEV1 | −20.3 (−46.3, 5.80)a |
| NOx + noise splines | FEV1 | −21.1 (−47.6, 5.51)a |
p ≤ 0.1,
p ≤ 0.05
All models include covariate adjustment for age at time of lung function test, gender, race, ethnicity, height, BMI, and a random intercept for community.
Figure 3.
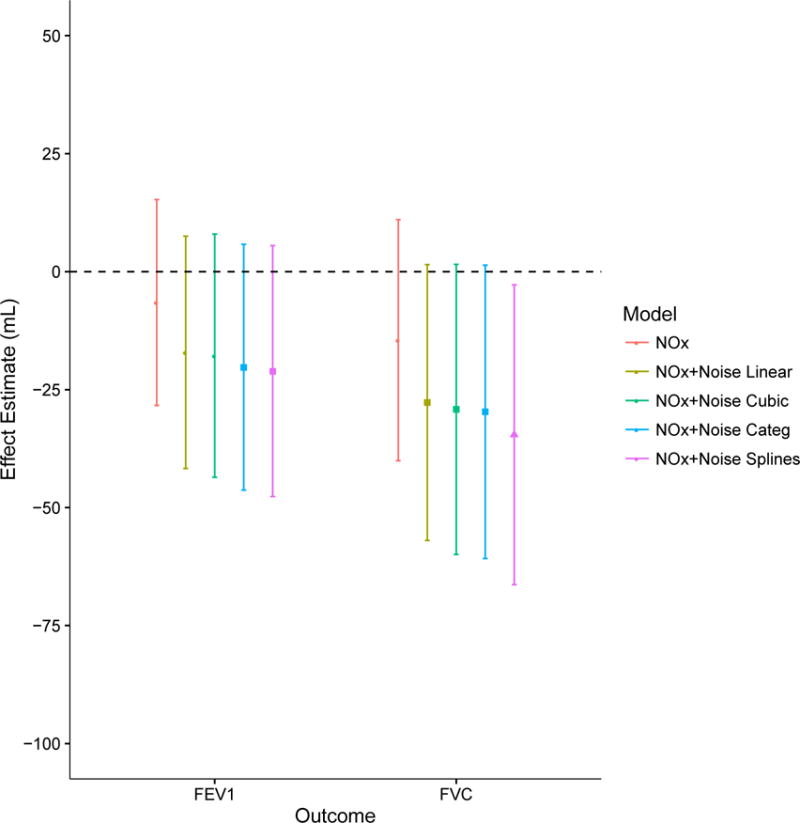
Effect estimates of the association between lung function and freeway NOx without adjustment for noise (orange), with linear adjustment for noise (yellow), with cubic polynomial adjustment for noise (green), with categorical adjustment for noise (blue), and with non-linear function of noise (purple). Circles, squares, and triangles represent freeway NOx effect estimates that are not statistically significant, statistically significant at p<0.10 and at p<0.05, respectively.
Figure 4.
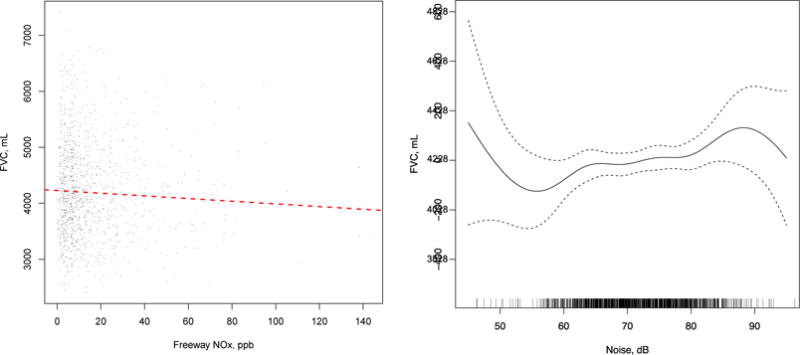
Mixed effects model examining the noise-adjusted association between FVC and freeway NOx. Left: adjusted linear association between freeway NOx and FVC (left). Right: cubic regression spline function of noise.
Similar results were found for FEV1 (Table 3). The effect estimate without adjustment for noise indicated a non-significant 6.54 mL decrease (95 % CI −28.3, 15.3) in FEV1 per IQR increase in freeway NOx. After adjusting for a linear, cubic polynomial, or categorical effect of noise, the FEV1 decrease associated with an IQR increase in freeway NOx was 17.1 mL (95 % CI −41.7, 7.51), 17.8 mL (95 % Cl −43.6, 7.98), and 20.3 mL (95 % Cl −46.3, 5.80), respectively. With the inclusion of noise with a cubic regression spline with 7 degrees of freedom, the decrease in FEV1 associated with an IQR increase in freeway NOx was 21.1 mL (95 % CI −47.6, 5.51). While this effect estimate is not statistically significant at p<0.05, we note that the inclusion of a non-linear effect of noise changes the freeway NOx effect estimate by −222%.
Cross validation was conducted for the spline models to examine whether any individual community was more influential on the model results than others. For both FVC and FEV1, with the removal of one community at a time, the coefficients for freeway NOx behaved similarly to the full model. None of the NOx coefficients changed more than 15% except when Anaheim was removed. Anaheim includes observations representing highest and most variable NOx concentrations and the highest noise values, and with its removal, the NOx effect estimate changed by 29% and 62% for FVC and FEV1, respectively.
When noise was examined alone with the same covariate adjustments, there was no evidence of a statistically significant association with lung function. Testing an interaction between freeway NOx and noise resulted in no significant associations, indicating that noise was not acting as an effect modifier. Tests for spatial random effects were not statistically significant, indicating no significant residual spatial correlation in any of the fitted models. Finally, none of the models for asthma showed significant results, so these results are not shown.
4. Discussion
By linking both traffic-related air pollution and noise exposure to a cohort of children in Southern California with a large database of measured health data, we were able to study the marginal and joint effects of freeway NOx and noise on children’s lung function. We consistently found that the inclusion of noise into our models amplified the strength of the negative association between freeway NOx and both FVC and FEV1. This observation led us to the conclusion that noise acts as a negative confounder on the association between traffic related air pollution and lung function. A negative confounding variable is defined as one that increases the estimated magnitude of the effect of another variable by its inclusion in a regression model (MacKinnon et al., 2000; Lynn, 2003). Essentially, the inclusion of Z (noise) may act to remove extraneous variation in X (air pollution), subsequently clarifying the association between X and Y (respiratory outcomes). Without the negative noise confounder there was under estimation of the main effect.
One possibility for the observed negative confounding phenomenon is that noise may be acting to partly offset dispersion model error in nighttime freeway NOx emissions when wind speeds are low (<1.0 m/s) and CALINE4 cannot accurately predict the direction and extent of freeway emissions. During these times, the relatively high speed and low numbers of vehicles, particularly heavy duty vehicles, produces relatively large noise impacts compared to their NOx emissions, and these relatively high noise impacts may better simulate the long distance emissions impacts of nighttime traffic such as found by Hu et al. (2009) in Los Angeles during the near-calm conditions of night. They found freeway impacts on air quality routinely extend more than 2500 metres due to reduced mixing and low mixing layer heights at night and early morning. In our data, we also noted the modest inverse correlation between distance to freeway and noise, which may be in part due to differences in the effect of wind direction. Wind direction is taken into account in the air pollution estimates but not the noise estimates. While wind direction does have an effect on noise propagation, its effect is much less pronounced than it is for air emissions.
Air pollution has several demonstrated biological mechanisms of damage, including oxidative stress and chronic inflammation. The possible mechanisms for noise to affect lung function are not as clear, but in conjunction with air pollution, we hypothesize that noise may result in an increased susceptibility to the effects of air pollution due to an enhanced stress response acting along the hypothalamic-pituitary-adrenal (HPA) axis, which can aggravate existing inflammatory conditions (Recio et al., 2016) (Figure 5). In a study of German children aged 5 to 12 years, it was found that those exposed to elevated nighttime noise (54 – 70 dB) had significantly higher morning saliva cortisol concentrations, indicating activation of the HPA axis (Ising et al., 2004). Their study concluded that exposure to traffic noise activates the HPA axis, which then leads to nighttime immune system disruption with long-term increased susceptibility to aggravation of bronchitis. The possibility that noise acts by disrupting neuroendocrine states also means that it may also aggravate inflammatory-mediated susceptibility to respiratory diseases such as bronchitis, pneumonia, and cardio-pulmonary disease (Recio et al., 2016).
Figure 5.
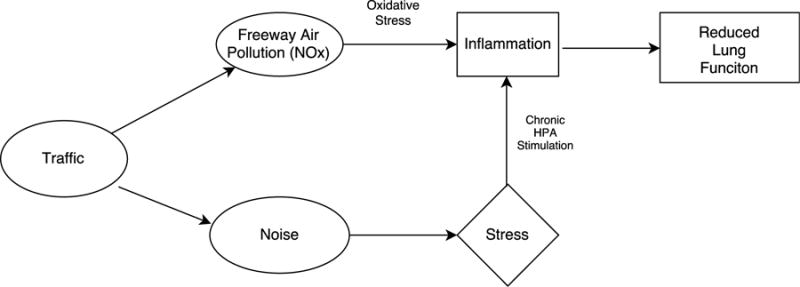
Hypothesized pathway of lung function health effects associated with traffic-related NOx and noise exposures.
It is important to emphasize that the negative confounding effect of noise did not appear to be linear, as we saw the stronger effects when noise was included as cubic, categorical, or non-linear regression spline in the mixed effects model. The most significant and consistent effect was uncovered with the regression spline models, which allowed for greater flexibility in the shape of the noise function. As shown in Figure 4, the shape of the non-linear noise association followed a cubic shape, with a few “bumps” in the mid-noise range regression splines. This form of the association indicates an interpretable phenomenon: that very low noise has less of an effect on lung function (evidenced by higher FVC), the effect is relatively flat in the mid-noise range, and high noise has a greater detrimental effect (evidenced by lower FVC). With a non-linear adjustment for noise, the resultant association between freeway NOx and lung function led us to suspect the times and locations of both low and high noise for a given NOx concentration might be compensating for relatively high uncertainty in the dispersion model estimates. A high noise (relative to NOx) situation might include the nighttime scenario described above. A low noise situation associated with under-prediction of freeway NOx may be occurring when hourly traffic volumes cannot distinguish between steady slow speeds and when congestion increases to the point of stop and go and/or creep conditions. In situations of irregular but low speeds, emissions per mile go up strongly (Zhang et al., 2011) while noise is relatively low under both speed conditions. It should also be noted that the associations with non-freeway NOx and lung function were never significant, either alone or including noise. The non-freeway NOx estimates (4.8 ppb) only averaged one-third of freeway NOx (14.6 ppb) so were not expected to produce a large incremental change compared to freeway NOx.
The observed correlation between freeway NOx and noise was modest (r = 0.53), and we note from Figure 2 that in most communities these two factors appear to co-vary. As a result we took measures to deal with the issue of collinearity by including orthogonal polynomials or splines in the regression models, resulting in minimal variance inflation factors. Nevertheless, collinearity can present issues in epidemiologic studies of multi-pollutants (Franklin and Schwartz, 2008) or multiple correlated environmental factors such as traffic-related noise and pollution. Collinearity, in combination with differential amounts of measurement error is harder to quantify and can further complicate the interpretation of effect estimates. For example, it is known that when covariates X (air pollution) and Z (noise) are highly correlated, the standard errors of the estimated coefficients will be inflated. It is similarly known that if X and Z are not correlated but possess relatively high measurement error, the effect of the measurement error would be to decrease the estimated effect sizes. However, when correlation and measurement error both exist at these levels of concern, the interpretation of the estimated coefficients of X and Z becomes more difficult. In our case we feel that the modest correlation between noise and air pollution has enabled us to conduct an examination of the joint role of noise and NOx on lung function, which may not be possible in studies where their pairwise correlation is high. Furthermore, it makes measurement error our chief concern. We suspect that the correlation was lower than in many other cities because Southern California traffic conditions of high congestion during rush hours produce situations of high emissions during stop and go traffic with simultaneous reductions in speed and therefore noise. Conversely, during off peak hours, the higher speeds produce stronger correlations between noise and emissions. While we included information regarding properties of the study subjects’ homes such as year built, and air conditioning use as proxies for noise insulation, it did not significantly modify our results. Not having more precise metrics of housing characteristics such as windowpane number and bedroom location could be a possible source of measurement error.
Our analysis was based on a cross-sectional chronic study, with annual estimates of exposures being linked to health measurements collected at one point during the year. We must therefore assume that the exposures are representative of the time of diagnosis, and/or the diagnosis is representative of the year for which we have average exposures. Similarly, we assume the noise estimates, which were based on data from 2013–15, were representative of the time period during which health measurements and NOx were collected (2011–12). This is a reasonable assumption as average noise levels are not anticipated to have changed significantly in this short time span beyond incremental growth in traffic volumes proportional to population growth.
5. Conclusion
Overall, the findings in this study have important epidemiological and policy implications for studies of traffic related health effects. In terms of lung function outcomes, noise appears to act as a negative confounder. This result has two likely explanations. First, in joint models, noise may be offsetting error in nighttime dispersion model estimates of freeway NOx. Second, loud noise exposure may be activating of the HPA axis, resulting in exacerbation of preexisting or underlying respiratory disease. This in turn enhances the detrimental effect of near-roadway air pollution on lung function by making the lung more susceptible to the deleterious effects of the air pollutants. Thus, in order to gain a clearer understanding of the broad mechanistic pathway that air pollution plays on health, including noise as a covariate is a critical consideration when studying the association between traffic-related air pollution and respiratory outcomes.
Supplementary Material
Highlights.
The joint effects of traffic noise and air pollution exposure on health are examined
Noise enhances the detrimental impact of air pollution on children’s lung function
Noise is an important exposure to include in studies of traffic-related health outcomes
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Belojevic G, Jakovljevic B, Stojanov V, Paunovic K, Ilic J. Urban road-traffic noise and blood pressure and heart rate in preschool children. Environ Int. 2008;34(2):226–231. doi: 10.1016/j.envint.2007.08.003. [DOI] [PubMed] [Google Scholar]
- Benson PE. A review of the development and application of the CALINE3 and 4 models. Atmos Environ. 1992;26B:379–390. [Google Scholar]
- Bilenko N, van Rossem L, Brunekreef B, Beelen R, Eeftens M, Hoek G, et al. Traffic-related air pollution and noise and children’s blood pressure: Results from the PIAMA birth cohort study. Eur J of Prev Cardiol. 2013;22(1):4–12. doi: 10.1177/2047487313505821. [DOI] [PubMed] [Google Scholar]
- Dreger S, Meyer N, Fromme H, Bolte G. Environmental noise and incident mental health problems: A prospective cohort study among school children in Germany. Environ Res. 2015;143:49–54. doi: 10.1016/j.envres.2015.08.003. [DOI] [PubMed] [Google Scholar]
- Federal Highway Administration. TNM Version 2.5 Addendum to Validation of FHWA’s TNM® (TNM) Phase 1. Cambridge, MA: 2004. [Google Scholar]
- Franklin M, Schwartz J. The impact of secondary particles on the association between ambient ozone and mortality. Environ Health Perspec. 2008;116(4):453–458. doi: 10.1289/ehp.10777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin M, Vora H, Avol E, McConnell R, Lurmann F, Liu F, et al. Predictors of intra-community variation in air quality. J Expos Sci Environ Epidemiol. 2012;22(2):135–47. doi: 10.1038/jes.2011.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gauderman WJ, Avol E, Gilliland FD, Vora H, Thomas DC, Berhane K, et al. The effect of air pollution on lung development from 10 to 18 years of age. New Engl J Med. 2004;351(11):2239–2246. doi: 10.1056/NEJMoa040610. [DOI] [PubMed] [Google Scholar]
- Gauderman WJ, Vora H, McConnell R, Berhane K, Gilliland F, Thomas DC, et al. Effect of exposure to traffic on lung development from 10 to 18 years of age: a cohort study. Lancet. 2007;369(9561):571–577. doi: 10.1016/S0140-6736(07)60037-3. [DOI] [PubMed] [Google Scholar]
- Gauderman WJ, Urman R, Avol E, Berhane K, McConnell R, Rappaport E, et al. Association of Improved Air Quality with Lung Development in Children. New Engl J Med. 2015;372(10):905–913. doi: 10.1056/NEJMoa1414123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hänninen O, Knol AB, Jantunen M, Lim T-A, Conrad A, Rappolder M, et al. Environmental Burden of Disease in Europe: Assessing Nine Risk Factors in Six Countries. Environ Health Persp. 2014;122(5):439–446. doi: 10.1289/ehp.1206154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu S, Fruin S, Kozawa K, Mara S, Paulson SE, Winer AM. A wide area of air pollutant impact downwind of a freeway during pre-sunrise hours. Atmos Environ. 2009;43(16):2541–2549. doi: 10.1016/j.atmosenv.2009.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ising H, Lange-Asschenfeldt H, Lieber GF, Weinhold H, Eilts M. Respiratory and Dermatological Diseases in Children with Long-term Exposure to Road Traffic Immissions. Noise and Health. 2003;5(19):41–50. [PubMed] [Google Scholar]
- Ising H, Lange-Asschenfeldt H, Moriske H-J, Born J, Eilts M. Low frequency noise and stress: bronchitis and cortisol in children exposed chronically to traffic noise and exhaust fumes. Noise Health. 2004;6(23):21–28. [PubMed] [Google Scholar]
- Jerrett M, McConnell R, Wolch J, Chang R, Lam C, Dunton G, et al. Traffic-related air pollution and obesity formation in children: a longitudinal, multilevel analysis. Environmental Health. 2014;13(1):49. doi: 10.1186/1476-069X-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EY, Jerrett M, Ross Z, Coogan PF, Seto EYW. Assessment of traffic-related noise in three cities in the United States. Environ Res. 2014;132:182–189. doi: 10.1016/j.envres.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linares C, Dias J, Tobias A, De Miguel JM, Otero A. Impact of urban air pollutants and noise levels over daily hospital admissions in children in Madrid: a time series analysis. Int Arch Occ Env Health. 2006;79(2):143–152. doi: 10.1007/s00420-005-0032-0. [DOI] [PubMed] [Google Scholar]
- Liu C, Fuertes E, Tiesler CMT, Birk M, Babisch W, Bauer CP, Koletzko S, von Berg A, Hoffmann B, Heinrich J. The associations between traffic-related air pollution and noise with blood pressure in children: Results from the GINIplus and LISAplus studies. Int J Hyg Envir Heal. 2014;217(4–5):499–505. doi: 10.1016/j.ijheh.2013.09.008. [DOI] [PubMed] [Google Scholar]
- Lynn HS. Suppression and Confounding in Action. Am Stat. 2003;57(1):58–61. [Google Scholar]
- MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the Mediation, Confounding and Suppression Effect. Prev Sci. 2000;1(4):173–181. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConnell R, Berhane K, Yao L, Jerrett M, Lurmann F, Gilliland F, et al. Traffic, Susceptibility, and Childhood Asthma. Environ Health Persp. 2006;114(5):766–772. doi: 10.1289/ehp.8594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConnell R, Islam T, Shankardass K, Jerrett M, Lurmann F, Gilliland F, et al. Childhood incident asthma and traffic-related air pollution at home and school. Environmental Health Perspectives. 2010;118(7):1021–1026. doi: 10.1289/ehp.0901232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neitzel RL, Gershon RRM, McAlexander TP, Magda LA, Pearson JM. Exposures to Transit and Other Sources of Noise Among New York City Residents. Environ Sci & Technol. 2012;46:500–508. doi: 10.1021/es2025406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niemann H, Bonnefoy X, Braubach M, Hecht K, Maschke C, Rodrigues C, Robbel N. Noise-induced annoyance and morbidity results from the panEuropean LARES study. Noise Health. 2006;8:63–79. doi: 10.4103/1463-1741.33537. [DOI] [PubMed] [Google Scholar]
- Peters JM, Avol E, Navidi W, London SJ, Gauderman WJ, Lurmann F, Linn WS, Margolis H, Rappaport E, Gong H. A study of twelve Southern California communities with differing levels and types of air pollution: Prevalence of respiratory morbidity. Am J Resp Crit Care Med. 1999;159(3):760–767. doi: 10.1164/ajrccm.159.3.9804143. [DOI] [PubMed] [Google Scholar]
- Recio A, Linares C, Banegas JR, Díaz J. Road traffic noise effects on cardiovascular, respiratory, and metabolic health: An integrative model of biological mechanisms. Environ Res. 2016;146:359–370. doi: 10.1016/j.envres.2015.12.036. [DOI] [PubMed] [Google Scholar]
- Rice MB, Rifas-Shiman SL, Litonjua AA, Oken E, Gillman MW, Kloog I, et al. Lifetime Exposure to Ambient Pollution and Lung Function in Children. Am J Resp Crit Care Med. 2016;193(8):881–888. doi: 10.1164/rccm.201506-1058OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shu N, Cohn LF, Harris RA, Kim TK, Li W. Comparative evaluation of the ground reflection algorithm in FHWA Traffic Noise Model (TNM 2.5) Appl Accoust. 2007;68(11–12):1459–1467. [Google Scholar]
- Stansfeld S. Noise Effects on Health in the Context of Air Pollution Exposure. Int J Environ Res Publ Health. 2015;12(10):12735–12760. doi: 10.3390/ijerph121012735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiesler CMT, Birk M, Thiering E, Kohlböck G, Koletzko S, Bauer CP, et al. Exposure to road traffic noise and children’s behavioural problems and sleep disturbance: Results from the GINIplus and LISAplus studies. Environ Res. 2013;123:1–8. doi: 10.1016/j.envres.2013.01.009. [DOI] [PubMed] [Google Scholar]
- Urman R, McConnell R, Islam T, Avol E, Lurmann F, Vora H, et al. Associations of children’s lung function with ambient air pollution: joint effects of regional and near-roadway pollutants. Thorax. 2014;69(6):540–7. doi: 10.1136/thoraxjnl-2012-203159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Guidelines for Community Noise. World Health Organization; Geneva, Switzerland: 1999. [Google Scholar]
- Wood SN. Generalized Additive Models: an Introduction with R. Chapman & Hall/CRC; 2006. [Google Scholar]
- Zeger SL, Thomas DC, Dominici F, Samet JM, Schwartz J, Dockery D, Cohen A. Exposure measurement error in time-series studies of air pollution: concepts and consequences. Environ Health Persp. 2000;108(5):419–26. doi: 10.1289/ehp.00108419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang K, Batterman S, Dion F. Vehicle emissions in congestion: Comparison of work zone, rush hour and free-flow conditions. Atmos Environ. 2011;(45):1929–1939. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


