Abstract
BACKGROUND
Anxiety disorders tend to precede onset of comorbid depression. Several researchers have suggested a causal role for anxiety in promoting depressive episodes, but few studies have identified specific mechanisms. The current study proposes an interpersonal model of comorbidity, where anxiety disorders disrupt interpersonal functioning, which in turn elevates risk for depression.
METHODS
At age 15 (T1), 815 adolescents oversampled for maternal depression completed diagnostic interviews, social chronic stress interviews, and self-report measures. At age 20 (T2), participants repeated all measures and reported on self-perceived interpersonal problems. At approximately age 23 (T3), a subset of participants (n= 475) completed a self-report depressive symptoms measure.
RESULTS
Consistent with other samples, anxiety disorders largely preceded depressive disorders. Low sociability and interpersonal oversensitivity mediated the association between T1 social anxiety disorder and later depression (including T2 depressive diagnosis and T3 depressive symptoms), controlling for baseline. Interpersonal oversensitivity and social chronic stress similarly mediated the association between generalized anxiety disorder before age 15 and later depression.
CONCLUSIONS
Interpersonal dysfunction may be one mechanism through which anxiety disorders promote later depression, contributing to high comorbidity rates.
Keywords: Social Phobia, Social Anxiety Disorder, Generalized Anxiety Disorder, Depressive Disorder, Interpersonal Relations, Comorbidity
Depression and anxiety disorders show pronounced comorbidity, with 50–60% of depressed individuals meeting lifetime criteria for an anxiety disorder [1]. Understanding how and why comorbidity emerges is critical to understanding etiology; however, research has rarely attempted to identify specific psychosocial risk factors that may contribute. The current study examines the little-explored role of interpersonal dysfunction.
Several researchers have suggested that anxiety disorders act as a causal risk factor for later depression [2–7]. This hypothesis is rooted in the widely-supported finding that anxiety typically temporally precedes depression [1; 5; 6; 8–12; for exception see 13]. Similarly, anxiety predicts increases in later depression in what may be a dose-response relationship [3; 14]. Causal models of comorbidity parsimoniously explain not only why anxiety and depression co-occur, but why anxiety usually comes first. Mathews et al. [15] recently supported the causality hypothesis, showing that among cases where anxiety preceded depression (i.e., most comorbid individuals), comorbidity was best explained using statistical models where anxiety directly predicted depression. In contrast, among the minority of cases where depression preceded anxiety, comorbidity was better explained by shared etiological factors, with no evidence for the reverse causality hypothesis that depression causes later anxiety.
Although this study provided support for the basic premise of the causal model, research specifying mechanisms explaining how anxiety impacts later depression risk remains limited [16; 17]. One promising category of possible mechanisms is interpersonal dysfunction. Depression has long been reciprocally linked to negative interpersonal behaviors, including poor social support, attachment disruptions, romantic distress, and chronic social stress [18–26]. A smaller but growing literature also links anxiety to a range of problematic interpersonal behaviors [27–36]. Interpersonal dysfunction may link anxiety disorders to later depression, as anxiety may provoke interpersonally destructive behaviors, and the resulting strain on relationships may trigger depressive episodes.
Although interpersonal mediators of comorbidity have rarely been explicitly tested, a few studies have tested similar hypotheses using various methodological approaches. Katz et al. [37] showed that social impairment at age 15 mediated the prospective association between social withdrawal at age 5 and depression at age 20. Grant et al. [38] found that avoidance of expressing emotion within relationships mediated the association between social anxiety and later depressive symptoms. In a daily diary study of generalized anxiety disorder (GAD), Starr and Davila [39] found that daily anxious mood fluctuations predicted higher subsequent depressed mood on days when self-reported interpersonal hassles and rejection were elevated. Whittal and Dobson [40] experimentally demonstrated that undergraduates with high need for social approval (associated with anxiety) responded to negative social feedback with greater depressive symptoms than controls. Finally, anxiety-depression comorbidity is associated with greater interpersonal impairment than non-comorbid anxiety or depression [27; 41–43], consistent with the basic idea that interpersonal dysfunction contributes to co-occurrence. However, no previous studies have directly tested interpersonal mediators of diagnostic comorbidity in a longitudinal database.
In the current study, we examined interpersonal mediators of the association between early anxiety disorders and later depression in a longitudinal sample following community youth at elevated depression risk from mid-adolescence into young adulthood. Adolescence is an appropriate age to address this question, as anxiety disorders typically have onsets by early adolescence [44], whereas depression rates grow steadily beginning in mid-adolescence [45]; thus, mechanisms bridging early anxiety with later depression may emerge during this developmental period. Further, better understanding the processes connecting early-onset anxiety to depression in young adulthood may help improve early detection of at-risk youth. Based on their prevalence in this age group and pre-existing evidence for associations with interpersonal distress, we selected two specific anxiety disorders to include in mediation models: social anxiety disorder (SAD) and GAD. Among anxiety disorders, SAD, being defined by social avoidance, has the widest support for linkages with interpersonal dysfunction [27; 32; 36; 46–50]. An emerging literature suggests that GAD also impairs interpersonal behaviors, with worry content often focusing on social relationships [31; 51–53].
Although we have discussed interpersonal dysfunction as if it were a monolithic construct, social relationships are complex and draw upon multiple competencies, and likewise disruptions in interpersonal functioning take a variety of forms. While numerous aspects of interpersonal dysfunction may bridge anxiety disorders and later depression, as a starting point, we examined three aspects of self-perceived interpersonal functioning with conceptual ties to anxiety: low sociability (difficulty socializing and interpersonal avoidance), interpersonal oversensitivity (over-heightened sensitivity, worry, and guilt over interpersonal failures and negative social responses), and unassertiveness (oversubmissive tendencies). As a preliminary step in the construction of mediation models, we conducted exploratory analyses examining associations between anxiety disorders and forms of interpersonal dysfunction. Low sociability and unassertiveness are both closely linked to SAD [36; 49; 50], and although it has not been explicitly researched within the context of anxiety disorders, interpersonal oversensitivity (reflecting excessive interpersonal worry and sensitivity to criticism and rejection) aligns with prior interpersonal conceptualizations of GAD [51]. As we anticipated that these three factors would be correlated, we adopted a multiple mediation approach.
As a consequence of gravitating individuals toward specific maladaptive interpersonal behaviors, anxiety disorders may lead to objectively higher levels of chronic stress within relationships. Social chronic stress (SCS) encompasses a broad range of factors impacting day-to-day functioning within salient interpersonal relationships, constituting a general index of interpersonal distress. SCS predicts depression [26] and in one study mediated the association between social withdrawal in early childhood and depression in young adulthood [37]. Thus, in addition to self-perceptions of specific interpersonal problems, we tested interview-assessed SCS as another potential comorbidity mediator.
The current study examines several related hypotheses. First, we examined temporal sequencing of anxiety and depressive disorders within this dataset, expecting to replicate temporal antecedence of anxiety over depression as the modal pattern. Second, we conducted exploratory analyses examining how anxiety disorders and depression related to specific forms of interpersonal dysfunction. Finally, we predicted that interpersonal dysfunction would mediate sequential comorbidity between anxiety disorders and later depression. Initial analyses, evaluating diagnostic outcomes, tested mediation models across two time points, collected at ages 15 and 20. To improve causal inference by temporally spacing all variables, supplemental analyses used as outcomes self-reported depressive symptoms assessed at age 23 in a third, smaller follow-up.
Method
Participants
Youth were drawn from a birth cohort study following 7,775 children born at the Mater Misericordiae Mothers’ Hospital in Queensland, Australia, between 1981 and 1984. A subsample of 815 adolescents (403 female) was selected for follow-up at age 15. Participants were preferentially recruited on the basis of self-reported maternal depression, producing a sample with an overrepresentation of depressed mothers ranging in severity and chronicity. Participants were largely Caucasian (89%) and lower to lower-middle class (see [54]).
Youth were invited for an additional follow-up at age 20 (T2), and 705 participated (363 female, 92% Caucasian). T2 participants did not differ from those lost to attrition by depression/anxiety status or ethnicity, but were more likely to be female, p < .01 (details in [55]).
Participants were invited to participate in a third, smaller follow-up (T3) between ages 22 and 25, and 512 participated, of whom 475 provided complete relevant data (mean age= 23.75 years, 271 female). Participants lost to attrition did not differ by anxiety/depression history but were more likely to be male, p< .001.
Procedure
Pregnant women were recruited into the birth cohort study during their first antenatal visit (see [56]). When the child reached age 15, families selected for inclusion in the current study were telephoned and asked to participate in the T1 assessment. Interviewers conducted in-home interview sessions, including collection of consent/assent and interviews and questionnaire completion. When youths reached age 20, families were contacted and invited to participate in the T2 follow-up. Youth completed similar procedures as in T1. At T3, two to five years after the T2 follow-up (mean interval=3.32 years), participants completed a depression self-report measure in conjunction with DNA samples submission (unrelated to current analyses).
Measures
Diagnostic evaluations
The Schedule for Affective Disorders and Schizophrenia in School-Aged Children [57] was administered at T1 to establish current and lifetime psychiatric diagnoses. Following standard procedures, trained clinicians administered interviews separately to adolescents and their mothers and assigned diagnoses using all available data. Weighted kappas ranged from .76 to .82 for current disorders and .73 to .79 for past disorders. At T2, youth diagnoses between ages 15 and 20 were established using the Structured Clinical Interview for DSM-IV (SCID-IV [58]), administered by trained clinicians, to assess current and past psychopathology. Weighted kappas ranged from .83 to .94 for current and .89 for past disorders. Maternal depression was assessed at T1 using the SCID-IV (45% met criteria).
Self-reported depressive symptoms
The Beck Depression Inventory (BDI [59]) is a 21-item measure assessing depressive symptomatology, with widely supported reliability, validity, sensitivity, and specificity in community samples [60; 61].
Interpersonal problems
The Inventory for Interpersonal Problems (IIP [62]) has been widely adopted in psychological research. The original measure contains 127 items, including behaviors “hard for you to do” and that “you do too much.” The IIP shows good test-retest reliability and external validity [49; 63; 64]. Numerous shorter forms of the IIP have been developed [65]; here, we used the IIP-48 [66], which contains three bipolar (pathological at each extreme) subscales: interpersonal sensitivity, sociability, and assertiveness, with evidence for structural and external validity [66]. As we had a prioi interest in one particular pole of each subscale (high interpersonal sensitivity, low sociability, low assertiveness) and not in their opposite extremes (pathologically high sociability, etc.), we excluded items assessing low interpersonal sensitivity, high sociability, and high assertiveness, creating 8-item subscales assessing low sociability (LS; e.g., “hard to socialize,” “avoid others too much,” Cronbach’s alpha=.91), interpersonal oversensitivity (IO; “worry too much about disappointing others,” “too sensitive to criticism,” α=.88), and unassertiveness (UA; “hard to say ‘no’,” “hard to set limits,” α=.85). The IIP-48 was administered at T2.
Social Chronic Stress
A semi-structured interview for adolescents, adapted from the UCLA Life Stress Interview [67], was used to assess objective indicators of ongoing circumstances over the prior six months in four relationship categories: social group, close friends, romantic life, and family relationships. Ratings in each domain were averaged, creating a composite score of interpersonal functioning with higher scores reflecting greater chronic stress. For details, see [68]. Inter-rater reliability= .70.
Results
Temporal Sequencing of Anxiety and Depression
Among youth with a depressive (n=247, including major depression or dysthymia) or anxiety (n=295, including panic disorder, agoraphobia, obsessive-compulsive disorder [OCD], GAD, specific phobia, SAD, posttraumatic stress disorder [PTSD], and separation anxiety disorder) disorder by age 20, 135 met criteria for both. Of these, most (72%) reported anxiety disorder onset at least one year prior to depression onset, χ2(2, N=135)= 91.24, p< .001; 18% reported depressive onset first, and 10% reported same-year onset.
Interpersonal Problems as Correlates of Depression and Anxiety Disorders
As displayed in Table 1, all proposed interpersonal mediators were significantly correlated with each other. Table 2 presents associations between interpersonal variables and GAD, SAD, and depression diagnosis at T1 and T2, with gender and maternal depression status entered as covariates. Anxiety and depressive diagnoses were associated with broad interpersonal impairment. Of note, T1 GAD predicted higher interpersonal oversensitivity (IO), low sociability (LS), and unassertiveness (UA), and SAD predicted higher LS and IO. Interestingly, at T1 SCS showed no associations with anxiety disorders, but at T2 it was associated with all disorders. To ensure that associations between interpersonal problems and anxiety disorders were not explained by comorbid depression, associations were re-computed controlling for depression at corresponding time points. T1 GAD no longer predicted LS; otherwise, the significance pattern was unchanged (Table 2).
Table 1.
Cross-Sectional Bivariate Correlations among Interpersonal Variables, Assessed at Age 20
| 1. | 2. | 3. | 4. | |
|---|---|---|---|---|
| 1. Interpersonal Oversensitivity | -- | |||
| 2. Low Sociability | .67 | -- | ||
| 3. Unassertiveness | .58 | .60 | -- | |
| 4. Social Chronic Stress | .33 | .37 | .17 | -- |
| M (SD) | 14.90 (6.04) | 14.70 (6.40) | 16.26 (6.06) | 10.03 (2.58) |
Note. All correlations significant at p < .0001 level.
Table 2.
Standardized Coefficients for Associations between Interpersonal Functioning Variables and Anxiety Disorders and Depression
| %/M(SD) | IO | LS | UA | T1 Social CS | T2 SCS | |
|---|---|---|---|---|---|---|
| Model I | ||||||
| T1 Any Anxiety Disorder | 12.3% | .13** | .18*** | .06 | .07 | .16*** |
| T1 GAD | 1.6% | .17*** | .09* | .09* | .04 | .15*** |
| T1 SAD | 3.7% | .11** | .18*** | .03 | .06 | .10** |
| T1 Depressive Disorder | 13.5% | .13** | .16*** | .11** | .10* | .17*** |
| T1 BDI | 6.01 (6.76) | .29*** | .28*** | .22*** | .07* | .14*** |
| T2 Any Anxiety Disorder | 24.5% | .22*** | .19*** | .15*** | .07 | .18*** |
| T2 GAD | 6.5% | .32*** | .23*** | .16*** | .04 | .18*** |
| T2 SAD | 17.4% | .16*** | .18*** | .12** | .05 | .17*** |
| T2 Depressive Disorder | 26.5% | .35*** | .30*** | .22*** | .07 | .30*** |
| T2 BDI | 7.05 (8.40) | .61*** | .48*** | .34*** | .05 | .39*** |
| T3 BDI | 7.64 (8.52) | .46*** | .39*** | .27*** | −.05 | .26*** |
|
| ||||||
| Model II | ||||||
| T1 Any Anxiety Disorder | .10** | .16*** | .04 | .06 | .13*** | |
| T1 GAD | .16*** | .07 | .08* | .03 | .14*** | |
| T1 SAD | .09* | .16*** | .01 | .05 | .08* | |
| T2 Any Anxiety Disorder | .16*** | .14*** | .12*** | .05 | .13** | |
| T2 GAD | .26*** | .17*** | .12*** | .02 | .12** | |
| T2 SAD | .13*** | .16*** | .10*** | .05 | .14*** | |
p < .05,
p < .01,
p < .001.
Notes: Model I: Controlling for gender and maternal depression status. Model II: Controlling for gender, maternal depression status, and depression diagnosis at equivalent time point. BDI= Beck Depression Inventory, GAD= Generalized Anxiety Disorder, SAD= Social Anxiety Disorder, IO= interpersonal oversensitivity, LS= low sociability, UA= unassertiveness, SCS= social chronic stress. N= 815 at T1, N= 705 at T2, N= 475 at T3.
Interpersonal Problems as Mediators of Association between T1 Anxiety Disorders and T2 Depression
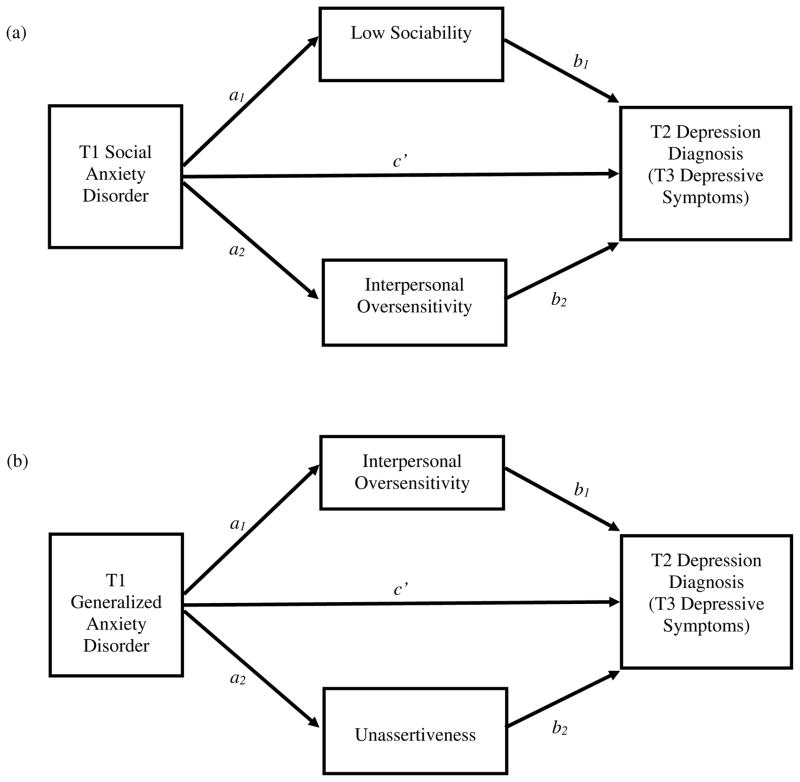
Multiple mediation models were tested using bootstrapping methods (5,000 resamples), using the SPSS PROCESS macro provided by Hayes [69]. This software conducts regression analyses to provide the magnitude and significance of the a (independent variable [IV] to mediator), b (mediator to dependent variable [DV]), c (IV to DV), and c′ (IV to DV, controlling for mediators) paths, and generates bias-corrected confidence intervals for indirect effects (ab). The PROCESS macro applies linear regression when outcomes are continuous (e.g., a paths predicting mediator variables from anxiety status) and logistic regression when outcomes are dichotomous (depression diagnosis). T1 depression, gender, and maternal depression status were entered as covariates in pathways predicting depression. Mediators were selected based on associations with disorders reported above (LS and IO for T1 SAD predicting T2 depression, and IO and UA for T1 GAD predicting T2 depression, illustrated in Figure 1), but including all three IIP-48 subscales in all models produced similar results.
Figure 1.
Models for mediation of associations between T1 anxiety diagnoses and later depression by interpersonal problems. See Tables 2 and 3 for path coefficients and estimates of indirect effects. T2 depression diagnosis and T3 depressive symptoms were separately evaluated as outcomes. T1 depression (or T1 depressive symptoms), maternal depression, and gender were entered as covariates in b and c paths. In models predicting T3 depressive symptoms, T3 age was also included as a covariate.
Table 3 displays mediation results. LS and IO both emerged as significant mediators of the association between SAD and later depression, as demonstrated by 95% CIs for indirect effects exclusive of zero. In addition, IO, but not UA, mediated the association between T1 GAD and T2 depression. In both models, c paths was significant but c′ paths was not, indicating full mediation.
Table 3.
Results of Mediation Models Examining Interpersonal Mediators of the Association between T1 Anxiety Disorders and Changes in Depressive Symptoms at T2
| Independent Variable | Mediators(s) | a path (IV to M) | b path (M to DV) | c path (total effect) | c′ path (direct effect) | ab (indirect effect) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| B | SE | B | SE | B | SE | B | SE | ab | SE | 95% CI | ||
| SAD | Full Model | .86* | .43 | .41 | .48 | .55 | .20 | [.18, .97] | ||||
| LS | 6.07*** | 1.34 | .04* | .02 | .24 | .15 | [.01, .60] | |||||
| IO | 3.35* | 1.27 | .09*** | .02 | .32 | .15 | [.08, .68] | |||||
|
| ||||||||||||
| GAD | Full Model | 2.06** | .70 | .84 | .32 | 1.00 | .31 | [.44, 1.68] | ||||
| IO | 8.33*** | 1.89 | .11*** | .02 | .92 | .31 | [.39, 1.60] | |||||
| UA | 4.34* | 1.92 | .02 | .02 | .08 | .11 | [−.06, .45] | |||||
p < .05,
p < .01,
p < .001. Bolded confidence intervals do not include zero, suggesting significant indirect effect.
Notes. Dependent variable= T2 depression diagnosis. T1 depression status, maternal depression, and gender entered as covariates in steps predicting DV. LS= low sociability, IO= interpersonal oversensitivity, social CS= social chronic stress.
Interpersonal Problems as Mediators of Association between T1 Anxiety Disorders and T3 Depressive Symptoms
Mediation models ideally include temporally lagged variables (IV preceding mediator, mediator preceding DV) to exclude reverse causality [70]. Although not possible in previous analyses because the IIP-48 was only administered at T2, we conducted supplemental analyses using self-reported depressive symptoms at T3 as the DV (N=475). Because youths varied in age at T3, we included T3 age as a covariate, along with maternal depression, gender, and T1 depressive symptoms. All analyses applied linear regression.
Table 4 displays results. For T1 SAD as a predictor of increased T3 depressive symptoms, IO was a significant mediator, but LS was not. However, when LS was examined in a single mediator model, it yielded a significant indirect effect, ab=2.68, SE=.97, 95% CI [1.11, 5.03]. When T1 GAD was included as the IV, IO produced a significant direct effect but UA did not, mirroring previous results.
Table 4.
Results of Mediation Models Examining Interpersonal Mediators of the Association between T1 Anxiety Disorders and Changes in Depressive Symptoms at T3
| Independent Variable | Mediators(s) | a path (IV to M) | b path (M to DV) | c path (total effect) | c′ path (direct effect) | ab (indirect effect) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| B | SE | B | SE | B | SE | B | SE | ab | SE | 95% CI | ||
| SAD | Full Model | 5.37** | 1.94 | 3.53 | 1.83 | 3.00 | 1.15 | [1.03, 5.64] | ||||
| LS | 5.77*** | 1.52 | .16* | .08 | 0.95 | .67 | [−.05, 2.74] | |||||
| IO | 4.32** | 1.51 | .48*** | .08 | 2.06 | .93 | [.60, 4.35] | |||||
|
| ||||||||||||
| GAD | Full Model | 5.64† | 2.91 | 1.27 | 2.81 | 5.35 | 1.72 | [2.50, 9.41] | ||||
| IO | 9.00*** | 2.23 | .59*** | .08 | 5.28 | 1.77 | [2.41, 9.48] | |||||
| UA | 2.11 | 2.16 | .03 | .07 | .07 | .29 | [−.28, 1.08] | |||||
|
| ||||||||||||
| SAD | SCS | .88 | .59 | .79*** | .15 | 5.37** | 1.94 | 4.85* | 1.89 | .70 | .48 | [−.06, 1.92] |
|
| ||||||||||||
| GAD | SCS | 2.78*** | .87 | .79*** | .16 | 5.64† | 2.91 | 4.03 | 2.85 | 2.19 | .98 | [.56, 4.47] |
p < .05,
p < .01,
p < .001,
p= .053. Bolded confidence intervals do not include zero, suggesting significant indirect effect.
Notes. Dependent variable= T3 depressive symptoms. T1 depressive symptoms, maternal depression, gender, and age at T3 entered as covariates in steps predicting DV. LS= low sociability, IO= interpersonal oversensitivity, SCS= social chronic stress.
SCS as Mediator of Association between Anxiety and Later Depression
We planned to test a model where T1 SCS mediated the association between T1 anxiety diagnosis and T2 depressive diagnosis (allowing mediators to precede DVs), but we did not conduct these analyses because GAD and SAD were not associated with T1 SCS (ps >.05). Note that models testing T2 SCS as a mediator of the association between T1 anxiety diagnosis and T2 depression met criteria for mediation for both disorders.
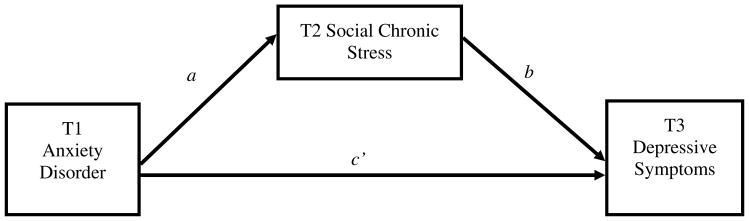
Next, we examined a fully temporally staggered model, with T2 SCS as a mediator of the association between T1 anxiety disorder and T3 depressive symptoms, with T1 depressive symptoms, gender, maternal depression, and age at T3 entered as covariates (see Figure 2). Results (Table 4) supported mediation for GAD, but not SAD.
Figure 2.
Model for mediation of association between T1 anxiety diagnosis and increases in depressive symptoms at T3 by T2 social chronic stress. T1 social anxiety disorder and T1 generalized anxiety disorder were tested as predictors in separate models. T1 depressive symptoms, maternal depression, gender, and age at T3 were entered as covariates in b and c paths. See Table 3 for estimates of path coefficients and indirect effects.
Discussion
The current study tested an interpersonal model of anxiety-depression comorbidity. First, we replicated the frequently reported temporal antecedence of anxiety over depressive disorders [7–11], as in most comorbid cases, anxiety onset preceded depression. This result is highly consistent with prior research (in fact, distribution of temporal patterns was remarkably similar to those reported elsewhere [11; 15; 71]), adding to mounting evidence of the temporal precedence of anxiety over depression. As this finding motivated the development of causal comorbidity models [3; 15], frequent replication is critical. The current dataset, as a large, longitudinal, high-risk, community-recruited, adolescent sample assessed using empirically-valid clinical interviews, is particularly well-suited to do so.
Results also showed that, like depression, anxiety disorders are associated with broad interpersonal impairment, including specific maladaptive interpersonal styles as well as general social chronic stress, which in turn mediates sequential comorbidity between anxiety and later depression. Specifically, interpersonal oversensitivity and low sociability mediated the association between SAD and later depression, and IO and social chronic stress mediated the relationship between GAD and later depression. IO reflects hypervigilance over negative interpersonal experiences, such as perceived interpersonal failures or rejecting behavior by others. IO linked both GAD and SAD to depression, but may relate to each anxiety disorder for different reasons. The excessive worry that defines GAD frequently extends into the interpersonal sphere [53], likely often translating into extreme concern over social behaviors and other people’s opinions. Social phobics, for their part, may view the prospect of rejection and other negative interpersonal events as intensely aversive, and may become excessively concerned about avoiding these experiences. Once anxious individuals develop IO, it may serve as a common pathway to depression. Oversensitivity to negative interpersonal experiences such as rejection can become a self-fulfilling prophecy, where rejection-sensitive individuals enact relationship-eroding behaviors that ultimately provoke actual rejection [72; 73], in response to which oversensitive individuals may be especially prone to developing depression [74].
LS may be more specific as a mediator to SAD. The positive link between LS and SAD is not surprising [32; 36; 75], as avoidance of feared social stimuli, including general social situations, is a cardinal symptom of social anxiety disorder [76]. However, the notion that socialization difficulties help explain the link between social anxiety and later depression has never to our knowledge been tested, although one study [77] supported the role of behavioral avoidance (conceptually related to LS). Poor sociability likely impedes the development of close relationships, reduces available social support, limits engagement in enjoyable social experiences, and elevates loneliness and alienation, all of which may ultimately provoke depressive symptoms [27; 78; 79].
We did not test the reverse causal model, where depression leads to increased anxiety via interpersonal mechanisms, as testing both directions of effect would have required an excessive number of tests. Given the choice, temporal sequencing data (both in this sample and elsewhere) and prior conceptualizations in the literature (e.g., [3]) strongly supported treating anxiety as the independent variable rather than depression. Further, Mathews et al. [15] found no evidence supporting the hypothesis that depression causes anxiety, even in cases where depression preceded anxiety diagnosis. Further, we lacked anxiety data at T3. Nonetheless, the idea that depression exacerbates interpersonal functioning, in turn elevating risk for anxiety, is conceptually plausible and not mutually exclusive with the current study’s results, as there may be reciprocal, longitudinal associations between symptoms and disorders, perhaps bidirectionally linked by interpersonal disturbances. The current model may be oversimplified, and more research is likely needed to fully appreciate the intricacies of anxiety-depression comorbidity.
Our results support an interpersonal model of comorbidity, but interpersonal dysfunction undoubtedly does not exclusively explain anxiety-depression co-occurrence. Abundant research suggests that anxiety and depression share a common underlying substrate that contributes to comorbidity [80–83]. In addition, anxiety disorders and depression share an extensive range of biological and psychosocial etiological factors (e.g., genetic [84]) that presumably also promote comorbidity. Non-interpersonal causal mechanisms may link anxiety with later depression (e.g., cognitive factors [17]). Even within the realm of interpersonal mechanisms, the interpersonal variables examined here do not represent all potential mediators (see [38]). Far more work is needed to fully understand why anxiety and depression co-occur at such dramatic rates.
Our study boasts several strengths, including longitudinal design and use of bootstrapping and multiple mediation. However, several study limitations should also be noted. First, our primary interpersonal dysfunction scale assessed self-perceptions only, although this was supplemented by the chronic stress interview. Future research investigating interpersonal mediators of anxiety-depression co-occurrence should utilize alternative sources of information (peer-report, behavioral observations) when possible. Second, the IIP-48 was only administered at T2, and diagnoses were only collected at T1 and T2, so in some models, the mediator was assessed concurrently with the outcome. However, additional analyses examining self-reported depression at T3 as outcomes showed very consistent findings. Third, T1 interviewers did not discriminate between subtypes of SAD. Generalized social anxiety is more strongly linked both depression and interpersonal problems than situational social anxiety [48; 85]; thus, results may have been stronger if we were able to examine this subgroup in isolation. We also did not distinguish between common and specific elements of anxiety and depression. Shared symptoms (negative affectivity [80]) could more strongly predict interpersonal problems, perhaps partially explaining findings. Finally, although we have been referencing causality, mediation analyses and temporal antecedence offer only preliminary support for causation, not firm evidence. Although one cannot randomly assign participants to anxiety disorders, we encourage researchers to creatively examine analogous processes using experimental methods (e.g., randomly assignment into anxiety treatments or mood induction conditions) to draw stronger causal inferences about pathways from anxiety to depression.
Our results may have important implications for prevention and treatment. Causal models of comorbidity broadly imply that early intervention for anxiety disorders may be an effective and cost-effective method of reducing long-term risk for a variety of internalizing disorders. Although an intuitive conclusion, more research is needed to verify that treating anxiety early improves long-term depression prognosis. Results specifically support interpersonal problems as important targets for intervention for anxiety disorders. Future research should examine whether treatments that emphasize recognition and reduction of interpersonal oversensitivity, encourage socialization, and promote relationship harmony improve not only anxiety, but also subsequent depression risk. Overall, our findings stress the importance of maintaining an interpersonal perspective when exploring the origins, nature, and treatment of internalizing disorders.
Acknowledgments
This research was supported by NIMH R01MH052239 and NIMH T32MH082719. The authors thank the MUSP, M900, and M20 Research Teams, and participating families. We gratefully acknowledge the contributions of project coordinators Robyne LeBrocque, Cheri Dalton Comber and Sascha Hardwicke, and the cooperation of Professor Jake Najman of the University of Queensland (head of the MUSP program).
References
- 1.Kaufman J, Charney D. Comorbidity of mood and anxiety disorders. Depression and Anxiety. 2000;12(s 1):69–76. doi: 10.1002/1520-6394(2000)12:1+<69::AID-DA9>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 2.Avenevoli S, Stolar M, Li J, et al. Comorbidity of depression in children and adolescents: models and evidence from a prospective high-risk family study. Biological Psychiatry. 2001;49(12):1071–1081. doi: 10.1016/s0006-3223(01)01142-8. [DOI] [PubMed] [Google Scholar]
- 3.Wittchen H-U, Beesdo K, Bittner A, Goodwin RD. Depressive episodes--Evidence for a causal role of primary anxiety disorders? European Psychiatry. 2003;18(8):384–393. doi: 10.1016/j.eurpsy.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Nelson CB, McGonagle KA, Liu J. Comorbidity of DSM-III-R major depressive disorder in the general population: Results from the US National Comorbidity Survey. British Journal of Psychiatry. 1996;168(Suppl 30):17–30. [PubMed] [Google Scholar]
- 5.Wittchen H-U, Kessler RC, Pfister H, Lieb M. Why do people with anxiety disorders become depressed? A prospective-longitudinal community study. Acta Psychiatrica Scandinavica. 2000;102:14–23. [PubMed] [Google Scholar]
- 6.Starr LR, Davila J. Temporal patterns of anxious and depressed mood in generalized anxiety disorder: A daily diary study. Behaviour Research and Therapy. 2012;50:131–141. doi: 10.1016/j.brat.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lewinsohn PM, Zinbarg R, Seeley JR, et al. Lifetime comorbidity among anxiety disorders and between anxiety disorders and other mental disorders in adolescents. Journal of Anxiety Disorders. 1997;11(4):377–394. doi: 10.1016/s0887-6185(97)00017-0. [DOI] [PubMed] [Google Scholar]
- 8.Orvaschel H, Lewinsohn PM, Seeley JR. Continuity of psychopathology in a community sample of adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34(11):1525–1535. doi: 10.1097/00004583-199511000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. Journal of Child Psychology and Psychiatry. 2005;46(11):1200–1210. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- 10.Kovacs M, Paulauskas SL, Gatsonis C, Richards C. Depressive disorders in childhood. III. Longitudinal study of comorbidity with and risk for conduct disorders. Journal of Affective Disorders. 1988;15:205–217. doi: 10.1016/0165-0327(88)90018-3. [DOI] [PubMed] [Google Scholar]
- 11.Essau CA. Comorbidity of anxiety disorders in adolescents. Depression and Anxiety. 2003;18(1):1–6. doi: 10.1002/da.10107. [DOI] [PubMed] [Google Scholar]
- 12.de Graaf R, Bijl RV, Spijker J, et al. Temporal sequencing of lifetime mood disorders in relation to comorbid anxiety and substance use disorders: Findings from the Netherlands Mental Health Survey and Incidence Study. Social Psychiatry and Psychiatric Epidemiology. 2003;38(1):1–11. doi: 10.1007/s00127-003-0597-4. [DOI] [PubMed] [Google Scholar]
- 13.Moffitt TE, Harrington H, Caspi A, et al. Depression and Generalized Anxiety Disorder: Cumulative and Sequential Comorbidity in a Birth Cohort Followed Prospectively to Age 32 Years. Arch Gen Psychiatry. 2007;64(6):651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- 14.Cole DA, Peeke LG, Martin JM, et al. A longitudinal look at the relation between depression and anxiety in children and adolescents. Journal of Consulting and Clinical Psychology. 1998;66(3):451–460. doi: 10.1037//0022-006x.66.3.451. [DOI] [PubMed] [Google Scholar]
- 15.Mathew AR, Pettit JW, Lewinsohn PM, et al. Co-morbidity between major depressive disorder and anxiety disorders: Shared etiology or direct causation? Psychological Medicine. 2011;41(10):2023–2034. doi: 10.1017/S0033291711000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cloninger CR, Martin RL, Guze SB, Clayton PJ. The empirical structure of psychiatric comorbidity and its theoretical significance. In: Maser JD, Cloninger CR, editors. Comorbidity of Mood and Anxiety Disorders. Washington, DC: American Psychiatric Press; 1990. [Google Scholar]
- 17.Starr LR, Davila J. Responding to anxiety with rumination and hopelessness: Mechanism of anxiety-depression symptom co-occurrence? Cognitive Therapy and Research. 2012;36(4):321–337. doi: 10.1007/s10608-011-9363-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98(2):310–357. [PubMed] [Google Scholar]
- 19.Whisman MA, Bruce ML. Marital dissatisfaction and incidence of major depressive episode in a community sample. Journal of Abnormal Psychology. 1999;108(4):674–678. doi: 10.1037//0021-843x.108.4.674. [DOI] [PubMed] [Google Scholar]
- 20.Hooley JM, Teasdale JD. Predictors of relapse in unipolar depressives: Expressed emotion, marital distress, and perceived criticism. Journal of Abnormal Psychology. 1989;98(3):229–235. doi: 10.1037//0021-843x.98.3.229. [DOI] [PubMed] [Google Scholar]
- 21.Abela JRZ, Hankin BL, Haigh EAP, et al. Interpersonal Vulnerability to Depression in High-Risk Children: The Role of Insecure Attachment and Reassurance Seeking. Journal of Clinical Child and Adolescent Psychology. 2005;34(1):182–192. doi: 10.1207/s15374424jccp3401_17. [DOI] [PubMed] [Google Scholar]
- 22.Kendler KS, Karkowski LM, Prescott CA. Causal Relationship Between Stressful Life Events and the Onset of Major Depression. American Journal of Psychiatry. 1999;156(6):837–841. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- 23.Joiner TE, Jr, Timmons KA. Depression in its interpersonal context. Handbook of Depression. 2009:322–339. [Google Scholar]
- 24.Davila J, Bradbury TN, Cohan CL, Tochluk S. Marital Functioning and Depressive Symptoms: Evidence for a Stress Generation Model. Journal of Personality and Social Psychology. 1997;73(4):849–861. doi: 10.1037//0022-3514.73.4.849. [DOI] [PubMed] [Google Scholar]
- 25.Katz J, Joiner TE, Jr, Kowalski RM. Behaving badly: Aversive behaviors in interpersonal relationships. Washington, DC: American Psychological Association; 2001. The aversive interpersonal context of depression: Emerging perspectives on depressotypic behavior; pp. 117–147. [Google Scholar]
- 26.Eberhart NK, Hammen CL. Interpersonal predictors of onset of depression during the transition to adulthood. Personal Relationships. 2006;13(2):195–206. [Google Scholar]
- 27.Starr LR, Davila J. Differentiating Interpersonal Correlates of Depressive Symptoms and Social Anxiety in Adolescence: Implications for Models of Comorbidity. Journal of Clinical Child & Adolescent Psychology. 2008;37(2):337–349. doi: 10.1080/15374410801955854. [DOI] [PubMed] [Google Scholar]
- 28.Overbeek G, Vollebergh W, de Graaf R, et al. Longitudinal associations of marital quality and marital dissolution with the incidence of DSM-III-R disorders. Journal of Family Psychology. 2006;20(2):284–291. doi: 10.1037/0893-3200.20.2.284. [DOI] [PubMed] [Google Scholar]
- 29.Zaider TI, Heimberg RG, Iida M. Anxiety disorders and intimate relationships: A study of daily processes in couples. Journal of Abnormal Psychology. 2010;119(1):163–173. doi: 10.1037/a0018473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McLeod JD. Anxiety disorders and marital quality. Journal of Abnormal Psychology. 1994;103(4):767–776. doi: 10.1037//0021-843x.103.4.767. [DOI] [PubMed] [Google Scholar]
- 31.Whisman MA, Sheldon CT, Goering P. Psychiatric disorders and dissatisfaction with social relationships: Does type of relationship matter? Journal of Abnormal Psychology. 2000;109(4):803–808. doi: 10.1037//0021-843x.109.4.803. [DOI] [PubMed] [Google Scholar]
- 32.Darcy K, Davila J, Beck JG. Is social anxiety associated with both interpersonal avoidance and interpersonal dependence? Cognitive Therapy and Research. 2005;29(2):171–186. [Google Scholar]
- 33.Eng W, Heimberg R. Interpersonal correlates of generalized anxiety disorder: Self versus other perception. Journal of Anxiety Disorders. 2006;20(3):380–387. doi: 10.1016/j.janxdis.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 34.Beck JG. Interpersonal Processes in the Anxiety Disorders: Implications for Understanding Psychopathology and Treatment. Washington, DC: American Psychological Association; 2010. [Google Scholar]
- 35.Heerey EA, Kring AM. Interpersonal Consequences of Social Anxiety. Journal of Abnormal Psychology. 2007;116(1):125–134. doi: 10.1037/0021-843X.116.1.125. [DOI] [PubMed] [Google Scholar]
- 36.Alden LE, Taylor CT. Interpersonal processes in social phobia. Clinical Psychology Review. 2004;24(7):857–882. doi: 10.1016/j.cpr.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 37.Katz SJ, Conway CC, Hammen CL, et al. Childhood social withdrawal, interpersonal impairment, and young adult depression: A mediational model. Journal of Abnormal Child Psychology. 2011;39(8):1227–1238. doi: 10.1007/s10802-011-9537-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grant DM, Beck JG, Farrow SM, Davila J. Do interpersonal features of social anxiety influence the development of depressive symptoms? Cognition and Emotion. 2007;21:646–663. [Google Scholar]
- 39.Starr LR, Davila J. Cognitive and Interpersonal Moderators of Daily Co-occurrence of Anxious and Depressed Moods in Generalized Anxiety Disorder. Cognitive Therapy and Research. doi: 10.1007/s10608-011-9434-3. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Whittal M, Dobson KS. An investigation of the temporal relationship between anxiety and depression as a consequence of cognitive vulnerability to interpersonal evaluation. Canadian Journal of Behavioural Science. 1991;23(4):391–398. [Google Scholar]
- 41.Lewinsohn PM, Rohde P, Seeley JR. Adolescent psychopathology: III. The clinical consequences of comorbidity. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34(4):510–519. doi: 10.1097/00004583-199504000-00018. [DOI] [PubMed] [Google Scholar]
- 42.Daley SE, Hammen C, Burge D, Davila J. Predictors of the generation of episodic stress: A longitudinal study of late adolescent women. Journal of Abnormal Psychology. 1997;106(2):251–259. doi: 10.1037//0021-843x.106.2.251. [DOI] [PubMed] [Google Scholar]
- 43.Pettit JW, Paukert AL, Joiner TE., Jr Refining moderators of mood contagion: Men’s differential responses to depressed and depressed-anxious presentations. Behavior Therapy. 2005;36(3):255–263. [Google Scholar]
- 44.Kessler RC, Berglund P, Demler O, et al. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 45.Lewinsohn PM, Hops H, Roberts RE, Seeley JR. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III--R disorders in high school students. Journal of Abnormal Psychology. 1993;102(1):133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- 46.Davila J, Beck JG. Is social anxiety associated with impairment in close relationships? A preliminary investigation. Behavior Therapy. 2002;33(3):427–446. [Google Scholar]
- 47.Wenzel A, Graff-Dolezal J, Macho M, Brendle JR. Communication and social skills in socially anxious and nonanxious individuals in the context of romantic relationships. Behaviour Research and Therapy. 2005;43(4):505–519. doi: 10.1016/j.brat.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 48.Kachin KE, Newman MG, Pincus AL. An interpersonal problem approach to the division of social phobia subtypes. Behavior Therapy. 2001;32(3):479–501. [Google Scholar]
- 49.Alden LE, Phillips N. An interpersonal analysis of social anxiety and depression. Cognitive Therapy and Research. 1990;14(5):499–512. [Google Scholar]
- 50.Stangier U, Esser F, Leber S, et al. Interpersonal problems in social phobia versus unipolar depression. Depression and Anxiety. 2006;23(7):418–421. doi: 10.1002/da.20190. [DOI] [PubMed] [Google Scholar]
- 51.Newman MG, Erickson TM. Generalized Anxiety Disorder. In: Beck JG, editor. Interpersonal Processes in the Anxiety Disorders: Implications for Understanding Psychopathology and Treatment. Washington, DC: American Psychological Association; 2010. pp. 235–259. [Google Scholar]
- 52.Salzer S, Pincus AL, Hoyer, et al. Interpersonal Subtypes Within Generalized Anxiety Disorder. Journal of Personality Assessment. 2008;90(3):292–299. doi: 10.1080/00223890701885076. [DOI] [PubMed] [Google Scholar]
- 53.Roemer L, Molina S, Borkovec TD. An investigation of worry content among generally anxious individuals. Journal of Nervous and Mental Disease. 1997;185(5):314–319. doi: 10.1097/00005053-199705000-00005. [DOI] [PubMed] [Google Scholar]
- 54.Hammen C, Brennan PA. Depressed adolescents of depressed and nondepressed mothers: Tests of an Interpersonal Impairment Hypothesis. Journal of Consulting and Clinical Psychology. 2001;69(2):284–294. doi: 10.1037//0022-006x.69.2.284. [DOI] [PubMed] [Google Scholar]
- 55.Hammen C, Brennan PA, Keenan-Miller D, et al. Chronic and acute stress, gender, and serotonin transporter gene–environment interactions predicting depression symptoms in youth. Journal of Child Psychology and Psychiatry. 2010;51(2):180–187. doi: 10.1111/j.1469-7610.2009.02177.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Keeping JD, Najman JM, Morrison J, et al. A prospective longitudinal study of social, psychological, and obstetrical factors in pregnancy: Response rates and demographic characteristics of the 8,556 respondents. British Journal of Obstetrics and Gynaecology. 1989;96:289–297. doi: 10.1111/j.1471-0528.1989.tb02388.x. [DOI] [PubMed] [Google Scholar]
- 57.Orvaschel H. Schedule for Affective Disorders and Schizophrenia for School-Age Children: Epidemiologic Version-5. Fort Lauderdale, FL: Nova Southeastern University, Center for Psychological Studies; 1995. [Google Scholar]
- 58.Spitzer RL, Williams JBW, Gibbon M, First M. Structured Clinical Interview for DSM-IV (SCID-IV) Washington, D.C: American Psychiatric Association; 1995. [Google Scholar]
- 59.Beck AT, Steer RA, Brown GK. Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation; 1996. pp. 1–82. [Google Scholar]
- 60.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- 61.Lasa L, Ayuso-Mateos JL, Vazquez-Barquero JL, et al. The use of the Beck Depression Inventory to screen for depression in the general population: a preliminary analysis. Journal of Affective Disorders. 2000;57(1–3):261–265. doi: 10.1016/s0165-0327(99)00088-9. [DOI] [PubMed] [Google Scholar]
- 62.Horowitz LM. On the cognitive structure of interpersonal problems treated in psychotherapy. Journal of Consulting and Clinical Psychology. 1979;47:5–15. doi: 10.1037//0022-006x.47.1.5. [DOI] [PubMed] [Google Scholar]
- 63.Woodward LE, Murrell SA, Bettler RF. Stability, reliability, and norms for the inventory of interpersonal problems. Psychotherapy Research. 2005;15(3):272–286. doi: 10.1080/10503300512331334977. [DOI] [PubMed] [Google Scholar]
- 64.Horowitz LM, Rosenberg SE, Baer BA, Ureno G. Inventory of interpersonal problems: Psychometric properties and clinical applications. Journal of Consulting and Clinical Psychology. 1988;56(6):885–892. doi: 10.1037//0022-006x.56.6.885. [DOI] [PubMed] [Google Scholar]
- 65.Hughes J, Barkham M. Scoping the inventory of interpersonal problems, its derivatives and short forms: 1988–2004. Clinical Psychology & Psychotherapy. 2005;12(6):475–496. [Google Scholar]
- 66.Gude T, Moum T, Kaldestad E, Friis S. Inventory of Interpersonal Problems: A Three-Dimensional Balanced and Scalable 48-Item Version. Journal of Personality Assessment. 2000;74(2):296–310. doi: 10.1207/S15327752JPA7402_9. [DOI] [PubMed] [Google Scholar]
- 67.Hammen C. Depression runs in families: The social context of risk and resilience in children of depressed mothers. New York: Springer; 1991. [Google Scholar]
- 68.Hammen C, Brennan P, Keenan-Miller D. Patterns of Adolescent Depression to Age 20: The Role of Maternal Depression and Youth Interpersonal Dysfunction. Journal of Abnormal Child Psychology. 2008;36(8):1189–1198. doi: 10.1007/s10802-008-9241-9. [DOI] [PubMed] [Google Scholar]
- 69.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: Guilford; in press. [Google Scholar]
- 70.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation Analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Roza SJ, Hofstra MB, van der Ende J, Verhulst FC. Stable Prediction of Mood and Anxiety Disorders Based on Behavioral and Emotional Problems in Childhood: A 14-Year Follow-Up During Childhood, Adolescence, and Young Adulthood. American Journal of Psychiatry. 2003;160(12):2116–2121. doi: 10.1176/appi.ajp.160.12.2116. [DOI] [PubMed] [Google Scholar]
- 72.Downey G, Freitas AL, Michaelis B, Khouri H. The self-fulfilling prophecy in close relationships: Rejection sensitivity and rejection by romantic partners. Journal of Personality and Social Psychology. 1998;75(2):545–560. doi: 10.1037//0022-3514.75.2.545. [DOI] [PubMed] [Google Scholar]
- 73.Downey G, Feldman SI. Implications of rejection sensitivity for intimate relationships. Journal of Personality and Social Psychology. 1996;70(6):1327–1343. doi: 10.1037//0022-3514.70.6.1327. [DOI] [PubMed] [Google Scholar]
- 74.Ayduk O, Downey G, Kim M. Rejection sensitivity and depressive symptoms in women. Personality and Social Psychology Bulletin. 2001;27(7):868–877. [Google Scholar]
- 75.La Greca AM, Lopez N. Social anxiety among adolescents: Linkages with peer relations and friendships. Journal of Abnormal Child Psychology. 1998;26(2):83–94. doi: 10.1023/a:1022684520514. [DOI] [PubMed] [Google Scholar]
- 76.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, D.C: Author; 1994. [Google Scholar]
- 77.Moitra E, Herbert JD, Forman EM. Behavioral avoidance mediates the relationship between anxiety and depressive symptoms among social anxiety disorder patients. Journal of Anxiety Disorders. 2008;22(7):1205–1213. doi: 10.1016/j.janxdis.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 78.Stice E, Rohde P, Gau J, Ochner C. Relation of depression to perceived social support: Results from a randomized adolescent depression prevention trial. Behaviour Research and Therapy. 2011;49(5):361–366. doi: 10.1016/j.brat.2011.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Joiner TE, Jr, Lewinsohn PM, Seeley JR. The core of loneliness: Lack of pleasurable engagement -more so than painful disconnection-predicts social impairment, depression onset, recovery from depressive disorders among adolescents. Journal of Personality Assessment. 2002;79(3):472–491. doi: 10.1207/S15327752JPA7903_05. [DOI] [PubMed] [Google Scholar]
- 80.Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- 81.Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56(10):921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 82.Watson D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114(4):522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- 83.Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- 84.Middeldorp CM, Cath DC, Van Dyck R, Boomsma DI. The co-morbidity of anxiety and depression in the perspective of genetic epidemiology. A review of twin and family studies. Psychological Medicine. 2005;35(05):611–624. doi: 10.1017/s003329170400412x. [DOI] [PubMed] [Google Scholar]
- 85.Kessler RC, Stein MB, Berglund P. Social Phobia Subtypes in the National Comorbidity Survey. American Journal of Psychiatry. 1998;155(5):613–619. doi: 10.1176/ajp.155.5.613. [DOI] [PubMed] [Google Scholar]