Abstract
Cadmium is a heavy metal that humans can be exposed to the in environment and occupation, and its relationship with cardiovascular diseases has been reported. in various reports. Epidemiological studies have also been associated with various inflammatory markers of cardiovascular diseases. In this study, we examined the relationship between monocyte count and monocyte to high density lipoprotein (HDL) ratio (MHR) and blood cadmium, which are one of the inflammatory markers of cardiovascular diseases. Data from a total of 733 male fire officers who received a health checkup at a hospital for one year in 2016 were analyzed. Populations were classified into 4 groups according to the quartile of blood cadmium and general characteristics were described. The relationship between monocyte count, MHR and cadmium in blood was statistically analyzed by linear regression analysis. In the univariate analysis and multivariate analysis, monocyte count was significantly higher in the second, third and fourth quartile groups than in the first quartile of cadmium, and the linear trend was significant. In univariate and multivariate analysis, MHR was significantly higher in the third and fourth quartile groups than in the first quartile group, and the linear trend was also significant. This study showed the significant relationship between blood cadmium and monocyte count and MHR among male fire officers. This was also statistically significant in the model adjusted for possible confounders and other cardiovascular risk factors and showed a linear trend.
Keywords: Cadmium, Cardiovascular Diseases, Cholesterol, HDL, Monocytes
Graphical Abstract
INTRODUCTION
Cadmium is a heavy metal that humans can be exposed to in the environment and occupation. It is a toxic metal that is not used for metabolism of in the human body. Environmental exposure to cadmium can occur exposed in the course of non-ferrous metal mining, phosphate fertilizer production, fossil fuel combustion, smelting, and electroplating, as well as negative water, air, soil, grain, vegetables, and smoking. When cadmium is absorbed into the body, it binds to plasma proteins and accumulates in the liver and kidneys. Cadmium stored in the liver slowly dissolves and is absorbed back into the kidney (1).
Cadmium is known to be associated with cardiovascular disease. Several epidemiological studies have shown the association of cadmium and cardiovascular disease; such as the prevalence of cardiovascular diseases (2), peripheral vascular diseases (3), and hypertension (4). It is known that cadmium causes inflammation of the body and activates reactive oxygen species (5), and the association of cadmium with inflammatory markers of cardiovascular diseases has been reported in epidemiological studies (6,7).
Monocyte count has been identified in several studies as a prognostic and predictive factor for cardiovascular disease (8,9,10). Monocyte to high density lipoprotein (HDL) ratio (MHR) has also been reported as a prognostic and predictive factor for various cardiovascular diseases (11,12,13,14,15,16). This index is known to act as a prognostic factor for cardiovascular disease independent of other prognostic factors including monocyte count (17).
Cadmium has been reported to be associated with monocyte elevation (18,19) and HDL reduction (20,21,22) in a number of studies. However, no study has reported the association of blood cadmium with monocyte count and MHR. We performed this study to determine the relationship between monocyte count, MHR and blood cadmium.
MATERIALS AND METHODS
Population
Seven hundred ninety-one fire officers visited the institute for routine health checkups in 2016. Blood sample including blood cadmium level and health survey were done for routine health checkup. Of the 791 fire officers, 733 subjects who were male and not missing any of the questionnaires in our interests (alcohol consumption, smoking, previous history of hypertension, hyperlipidemia, and diabetes), physical measurements, and the data of health examinations were included in our study, retrospectively.
Blood sample and health survey
Subjects fasted for at least 8 hours before blood sampling. Fasting blood glucose and lipid analyses were performed using ADVIA 2400 (Siemens, New York, NY, USA). Low density lipoprotein (LDL) was estimated by the Friedewald formula and direct test for LDL was performed when triglyceride exceeded 400 mg/dL. Total leukocyte count and differential leukocyte count were analyzed using Sysmex XE 2100 (Sysmex, Kobe, Japan). Monocyte count was calculated by multiplying white blood cell percentage by total white blood cell count. MHR was calculated by dividing monocyte count into HDL.
The questionnaires were filled out with informed consent and were checked by a doctor before the start of the health checkup. The questionnaires were self-filling questionnaires, and questionnaires on general characteristics were used to confirm smoking habits, alcohol drinking habits and previously diagnosed hypertension, diabetes, and hyperlipidemia. Weight and height were measured using an automated height and weight measuring device FA600 (Fanics, Busan, Korea) in an upright position and wearing light apparel without shoes. Body mass index (BMI) was calculated by dividing body weight by square of height.
Blood pressure was measured in a seated position using an automated sphygmomanometer TM2655 (Biospace, Seoul, Korea) and BP203RV (Colin, Tokyo, Japan) after at least 10 minutes of rest. Smoking habits were categorized as present smoking status. Participants who drank alcohol almost never to 2–3 times a months were classified as ‘low,’ and those who drank once or more than once a week were classified as ‘high.’ Participants with systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg or previously diagnosed with hypertension were classified as ‘hypertension.’ Participants with fasting blood glucose ≥ 126 mg/dL and previously diagnosed with diabetes were classified as ‘diabetes.’ Participants with LDL ≥ 160 mg/dL or total cholesterol ≥ 240 mg/dL or previously diagnosed with hyperlipidemia were classified as ‘hyperlipidemia,’ according to Adult Treatment Panel (ATP) III guideline (23).
Blood cadmium analysis
To determine the cadmium concentration in the body, the blood cadmium concentration was measured. Whole blood was collected from each subject. The collected blood was stored in an ethylenediaminetetraacetic acid (EDTA) tube and stored at −20°C for freezing and used as an analytical sample. Analytical samples from each subject were first thawed at room temperature and then homogenized for about 40 minutes with a roller mix to prevent foaming, followed by sample pretreatment and standard water addition. Analysis of cadmium in blood was performed using a non-flame atomic absorption spectrophotometer Thermo iCE 3000 Series AA Spectrometer GFS9 (ThermoFisher Scientific, Cambridge, UK). Analytical wavelength was 228.8 nm, injection temperature was 20°C, drying temperature was 100°C, 150°C, painting temperature was 600°C, and atomization temperature was 1,000°C. Zeeman calibration was used for background correction and peak height was used for absorbance measurement. A standard cadmium solution (1,000 μg/mL) (Sigma-Aldrich, St. Louis, MO, USA) was used for the analysis. The standards were prepared by diluting the standard solution with 2% (w/w) nitric acid solution for 4 concentration levels (5 ppb, 2.5 ppb, 1.25 ppb, 0.625 ppb). Then 0.5 mL of Tritone X-100 and 0.3 g of NH4H2PO4 were dissolved in 0.2% nitric acid (HNO3) solution. As part of external quality assurance and control, the institute passed the Quality Assurance Program, operated by the Korea Occupational Safety and Health Agency. All blood samples for blood cadmium were above the detection limits.
Statistical analysis
The population was divided into 4 groups according to the quartile of the blood cadmium level. General characteristics and the distribution of blood cadmium level by each variable were described. Since blood cadmium level was not normally distributed, P value was calculated by Mann-Whitney test. P value < 0.050 was considered statistically significant. Then, univariate analysis was performed using a linear regression model with blood cadmium level categorized as quartiles as independent variables, monocyte count and MHR as dependent variables. For the multivariate analysis, we analyzed the correlations between monocyte count and MHR among the general characteristics of subjects. Variables with possible association with monocyte count and MHR were selected (P < 0.200). Age, smoking, alcohol drinking, and BMI were included in the model. In model 3, hypertension, diabetes, and hyperlipidemia, which are well known risk factors for cardiovascular disease, were additionally adjusted. In each model, we also calculated the P for trend by treating each blood cadmium quartiles as a continuous variable in addition to the coefficients of the cadmium in the blood. Residual analysis performed by least square method showed the presence of outliers, so robust linear regression analysis method was performed for multiple regression analysis. Statistical analysis was done using SPSS ver. 23 (SPSS Inc., Chicago, IL, USA) for univariate analysis and R version 3.3.2 (R Foundation, Vienna, Austria), package “MASS,” for multivariate robust linear regression analysis. For univariate and multivariate regression analysis, a P value < 0.050 was considered statistically significant for the estimated coefficients. Coefficients for independent variables and 95% confidence intervals (CIs) were reported.
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board (IRB) of Keimyung University Dongsan Medical Center (IRB No. 2017-02-023). Informed consent was waived by the IRB.
RESULTS
The total number of subjects was 733. There were 134 (18.3%) current smokers and 489 high alcohol drinkers (66.7%). The mean blood cadmium level was 0.750 ± 0.359 μg/L. The BMI was 24.5 ± 2.56 kg/m2. Mean HDL was 48.10 ± 11.42 mg/dL, White blood cell count was 6,240.80 ± 1,547.17 /μm3 and monocyte was 392.80 ± 140.00 /μm3. The MHR was 8.70 ± 4.16 mg/dL. Hypertension was observed in 184 patients (25.1%), diabetes in 22 patients (3.0%), and hyperlipidemia in 72 patients (9.8%) (Table 1).
Table 1. Baseline and demographical characteristics of the study population.
| Variables | No. (%) of subjects |
|---|---|
| No. (%) of total subjects | 733 (100.0) |
| Smoking | |
| Yes | 134 (18.3) |
| Ex- or no | 599 (81.7) |
| Age, yr | 42.30 ± 9.22 |
| Alcohol drinking* | |
| High | 489 (66.7) |
| Low | 244 (33.3) |
| Blood concentration of cadmium , µg/L | 0.750 ± 0.359 |
| Height, cm | 172.60 ± 5.33 |
| Weight, kg | 73.10 ± 8.94 |
| BMI, kg/m2 | 24.50 ± 2.56 |
| HDL, mg/dL | 48.10 ± 11.42 |
| WBC, 103/µL | 6,240.80 ± 1,547.16 |
| Monocyte, % | 6.40 ± 1.96 |
| Monocyte count, 103/µL | 392.80 ± 140.00 |
| MHR | 8.70 ± 4.16 |
| Hypertension† | |
| Yes | 184 (25.1) |
| No | 549 (74.9) |
| Diabetes‡ | |
| Yes | 22 (3.0) |
| No | 711 (97.0) |
| Hyperlipidemia§ | |
| Yes | 72 (9.8) |
| No | 661 (90.2) |
| Job category | |
| Fire extinguisher | 232 (31.7) |
| Fire field investigator | 16 (2.2) |
| Driver | 130 (17.7) |
| Rescue team | 80 (10.9) |
| Paramedic | 89 (12.1) |
| Administrative officer | 177 (24.1) |
Data are shown as mean ± standard deviation or number (%).
BMI = body mass index, HDL = high density lipoprotein, WBC = white blood cell, MHR = monocyte to high density lipoprotein ratio, LDL = low density lipoprotein.
*Participants who drink alcohol almost never to 2–3 times a months were classified as ‘low,’ and those who drink once or more than once a week were classified as ‘high’; †Participants with systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg or previously diagnosed with hypertension were classified as ‘hypertension’; ‡Participants with fasting blood glucose ≥ 126 mg/dL and previously diagnosed with diabetes were classified as ‘diabetes’; §Participants with LDL ≥ 160 mg/dL or total cholesterol ≥ 240 mg/dL or previously diagnosed with hyperlipidemia were classified as ‘hyperlipidemia.’
The distribution of blood cadmium level by general characteristics of subjects was suggested in Table 2. Blood cadmium level was not normally distributed, so it is represented as quartiles. The first, second, and third quartile of blood cadmium was 0.49 μg/L, 0.70 μg/L, and 0.92 μg/L. Age, smoking status, hypertension, diabetes, HDL cholesterol, white blood cell count, monocyte count, and MHR were associated with blood cadmium level, while alcohol consumption, BMI, hyperlipidemia, and job category were not.
Table 2. The distribution of blood cadmium level by baseline and demographical characteristics of the study population.
| Variables | No. | Blood cadmium, µg/L | P value* |
|---|---|---|---|
| Total | 733 | 0.70 (0.49, 0.92) | |
| Age, yr | < 0.001 | ||
| ≥ 43 | 369 | 0.79 (0.61, 1.01) | |
| < 43 | 364 | 0.59 (0.39, 0.83) | |
| Smoking status | < 0.001 | ||
| Yes | 244 | 0.85 (0.85, 1.09) | |
| No or ex- | 489 | 0.66 (0.47, 0.87) | |
| Alcohol consumption† | 0.067 | ||
| High | 134 | 0.77 (0.50, 0.94) | |
| Low | 599 | 0.67 (0.48, 0.90) | |
| BMI, kg/m2 | 0.235 | ||
| ≥ 25 | 462 | 0.69 (0.48, 0.90) | |
| < 25 | 271 | 0.72 (0.50, 0.97) | |
| Hypertension‡ | < 0.001 | ||
| Yes | 184 | 0.76 (0.56, 1.00) | |
| No | 549 | 0.67 (0.47, 0.90) | |
| Diabetes§ | 0.016 | ||
| Yes | 22 | 1.10 (0.56, 1.28) | |
| No | 711 | 0.70 (0.49, 0.90) | |
| Hyperlipidemia¶ | 0.177 | ||
| Yes | 72 | 0.70 (0.49, 0.91) | |
| No | 661 | 0.91 (0.56, 1.02) | |
| HDL-cholesterol, mg/dL | 0.004 | ||
| High (≥ 46.1) | 370 | 0.66 (0.46, 0.89) | |
| Low (< 46.1) | 363 | 0.74 (0.53, 0.97) | |
| WBC, 103/µL | < 0.001 | ||
| High (≥ 6,000) | 368 | 0.71 (0.54, 0.96) | |
| Low (< 6,000) | 365 | 0.66 (0.45, 0.89) | |
| Monocyte, 103/µL | < 0.001 | ||
| High (≥ 382) | 368 | 0.76 (0.54, 0.99) | |
| Low (< 382) | 365 | 0.66 (0.45, 0.86) | |
| MHR | 0.004 | ||
| High (≥ 8.24) | 363 | 0.74 (0.53, 0.97) | |
| Low (< 8.24) | 370 | 0.66 (0.46, 0.89) | |
| Job category** | 0.809 | ||
| Fire fighter | 248 | 0.71 (0.50, 0.98) | |
| Non-fire fighter | 485 | 0.70 (0.49, 0.90) |
Values were presented as median (25 percentile, 75 percentile).
BMI = body mass index, HDL = high density lipoprotein, WBC = white blood cell.
* P value was calculated by Mann-Whitney test; †Participants who drink alcohol almost never to 2–3 times a months were classified as ‘low,’ and those who drink once or more than once a week were classified as ‘high’; ‡Participants with systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg or previously diagnosed with hypertension were classified as ‘hypertension’; §Participants with fasting blood glucose ≥ 126 mg/dL and previously diagnosed with diabetes were classified as ‘diabetes’; ¶Participants with LDL ≥ 160 mg/dL or total cholesterol ≥ 240 mg/dL or previously diagnosed with hyperlipidemia were classified as ‘hyperlipidemia’; **Fire extinguisher and fire field investigator are classified as ‘fire fighter.’ Driver, rescue team, paramedic, and officer were classified as ‘non-fire fighter.’
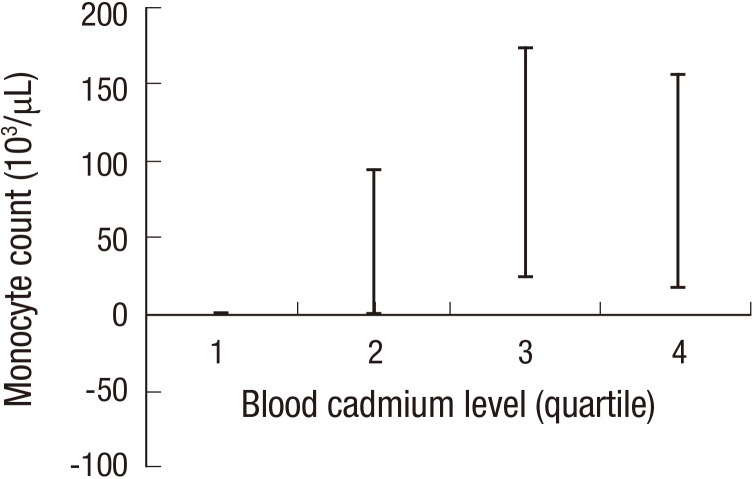
The subjects were classified into 4 groups according to the quartiles of blood cadmium level. Monocyte count and MHR were analyzed by univariate and multivariate models. Compared with the first quartile of cadmium, the second, third, and fourth quartile groups were significantly higher in monocyte count (P = 0.018, P < 0.001, P < 0.001), and trend was also significantly increased (P for trend < 0.001). This is also significant for models 2 (P = 0.043, P < 0.001, P = 0.001). In model 3, the monocyte counts of the third and fourth quartile groups were significantly increased compared to the first quartile (P = 0.001, P = 0.002; P for trend < 0.001) (Table 3) (Fig. 1).
Table 3. Association between blood cadmium level and monocyte count using linear regression model.
| Variables | Model 1* | Model 2† | Model 3‡ | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | 95% CI | P value | P for trend | Coefficient | 95% CI | P value | P for trend | Coefficient | 95% CI | P value | P for trend | |
| Blood cadmium | < 0.001 | < 0.001 | < 0.001 | |||||||||
| First quartile | Reference | Reference | Reference | |||||||||
| Second quartile | 34.33 | (5.94, 62.78) | 0.018 | 28.43 | (0.84, 43.35) | 0.043 | 26.81 | (−0.53, 41.60) | 0.054 | |||
| Third quartile | 53.97 | (25.57, 82.36) | < 0.001 | 51.31 | (22.51, 66.89) | < 0.001 | 52.84 | (24.19, 68.34) | < 0.001 | |||
| Fourth quartile | 53.55 | (25.15, 81.94) | < 0.001 | 49.37 | (19.34, 65.61) | 0.001 | 46.73 | (16.94, 62.84) | 0.002 | |||
| Smoking | - | - | - | - | 42.76 | (15.99, 57.23) | 0.002 | - | 55.68 | (14.80, 55.68) | 0.002 | - |
| Alcohol drinking | - | - | - | - | −11.34 | (−31.69, −0.33) | 0.276 | - | −1.14 | (−32.30, −1.14) | 0.243 | - |
| Age, yr | - | - | - | - | −0.69 | (−1.85, −0.06) | 0.244 | - | −0.47 | (−2.30, −0.47) | 0.069 | - |
| BMI, kg/m2 | - | - | - | - | 7.67 | (3.95, 9.68) | < 0.001 | - | 8.27 | (2.43, 8.27) | 0.001 | - |
| Hyperlipidemia | - | - | - | - | - | - | - | - | 54.86 | (5.73, 54.86) | 0.021 | - |
| Hypertension | - | - | - | - | - | - | - | - | 26.62 | (−8.89, 26.62) | 0.228 | - |
| Diabetes | - | - | - | - | - | - | - | - | 105.1 | (17.79, 105.10) | 0.009 | - |
BMI = body mass index, CI = confidence interval.
*Univariate regression analysis were done by least square method; †Multivariate regression analysis were done by robust regression method, adjusted by age, gender, smoking, alcohol drinking, and BMI; ‡Multivariate regression analysis were done by robust regression method, adjusted by age, gender, smoking, alcohol drinking, BMI, hypertension, diabetes, and hyperlipidemia.
Fig. 1.
Adjusted coefficient (95% CIs) for monocyte count (103/μL) associated with quartiles of blood cadmium level. The regression coefficient was adjusted by age, smoking, alcohol drinking, BMI, hypertension, diabetes, and hyperlipidemia.
CI = confidence interval.
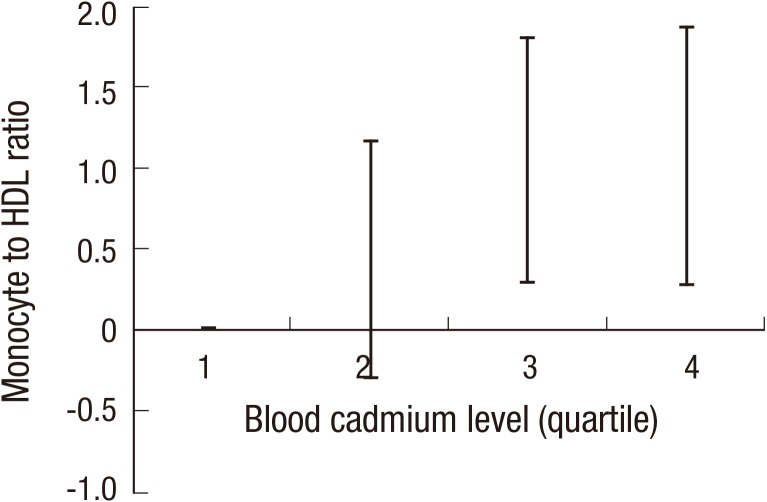
MHR was significantly higher in the third, fourth quartile groups than in the first quartile group (P = 0.013, P = 0.002) in model 1, and the trend was also significant (P for trend < 0.001). This is also significant for models 2 and 3, which are corrected for other confounders. In Model 2, the MHR of the third and fourth quartiles increased significantly compared to the first quartile (P = 0.011, P = 0.005; P for trend = 0.013), and the monocyte count of the third and fourth quartiles increased significantly in Model 3 compared to the first quartile (P = 0.007, P = 0.008; P for trend < 0.001) (Table 4) (Fig. 2).
Table 4. Association between blood cadmium level and MHR using linear regression model.
| Variables | Model 1* | Model 2† | Model 3‡ | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | 95% CI | P value | P for trend | Coefficient | 95% CI | P value | P for trend | Coefficient | 95% CI | P value | P for trend | |
| Blood cadmium | < 0.001 | < 0.001 | < 0.001 | |||||||||
| First quartile | Reference | Reference | Reference | |||||||||
| Second quartile | 0.46 | (−0.39, 1.31) | 0.288 | 0.47 | (−0.26, 0.87) | 0.205 | 0.42 | (−0.31, 0.82) | 0.253 | |||
| Third quartile | 1.07 | (0.22, 1.92) | 0.013 | 0.99 | (0.23, 1.41) | 0.011 | 1.05 | (0.29, 1.46) | 0.007 | |||
| Fourth quartile | 1.37 | (0.52, 2.21) | 0.002 | 1.14 | (0.35, 1.57) | 0.005 | 1.07 | (0.28, 1.50) | 0.008 | |||
| Smoking | - | - | - | - | 0.76 | (0.06, 1.15) | 0.036 | - | 0.76 | (0.05, 1.14) | 0.037 | - |
| Alcohol drinking | - | - | - | - | −0.79 | (−1.33, −0.50) | 0.004 | - | −0.82 | (−1.36, −0.53) | 0.003 | - |
| Age, yr | - | - | - | - | 0.02 | (−0.01, 0.03) | 0.315 | - | 0.00 | (−0.03, 0.02) | 0.772 | - |
| BMI, kg/m2 | - | - | - | - | 0.39 | (0.29, 0.44) | < 0.001 | - | 0.36 | (0.25, 0.41) | < 0.001 | - |
| Hyperlipidemia | - | - | - | - | - | - | - | - | 0.19 | (−0.66, 0.65) | 0.657 | - |
| Hypertension | - | - | - | - | - | - | - | - | 0.39 | (−0.22, 0.72) | 0.214 | - |
| Diabetes | - | - | - | - | - | - | - | - | 2.48 | (0.96, 3.30) | 0.001 | - |
MHR = monocyte to high density lipoprotein ratio, BMI = body mass index, CI = confidence interval.
*Univariate regression analysis were done by least square method; †Multivariate regression analysis were done by robust regression method, adjusted by age, gender, smoking, alcohol drinking, and BMI; ‡Multivariate regression analysis were done by robust regression method, adjusted by age, gender, smoking, alcohol drinking, BMI, hypertension, diabetes, and hyperlipidemia.
Fig. 2.
Adjusted coefficient (95% CIs) for MHR associated with quartiles of blood cadmium level. The regression coefficient was adjusted by age, smoking, alcohol drinking, BMI, hypertension, diabetes, and hyperlipidemia.
CI = confidence interval, MHR = monocyte to high density lipoprotein ratio, HDL = high density lipoprotein.
DISCUSSION
In this study, blood cadmium level and monocyte count, MHR were statistically significant and dose-dependent relationships were also found. To the best of our knowledge, this is the first epidemiological study of the relationship between cadmium and monocyte count and MHR, which are cardiovascular prognostic and predictive factors, in the human population.
Blood cadmium level was used as a biological index of cadmium in the body. It is known that blood cadmium level reflects both acute exposure and accumulated cadmium in the body, while urinary cadmium level mainly reflects body burden, especially in the kidneys. The initial half-life of blood cadmium is 2–3 months after acute exposure and is influenced by accumulated cadmium in the body after the cessation of exposure (24). In this study, cadmium was used as a biomarker of cadmium in the body, considering that many animal studies reports the significant effects of cadmium exposure on cholesterol or monocyte in several months, and blood cadmium level better reflects the short term exposure of cadmium. The mean of blood cadmium level among Korean adult population was reported to be 1.07 ± 0.01 μg/L (25). The blood cadmium levels of the participants in this study were lower than the average of Korean adults. This seems to be due to the age of the population in this study relatively low, which is between 23 and 60 years old, and the blood cadmium tends to rise in proportion to age (24).
Cadmium has a variety of effects on the immune system and can affect hematopoiesis. The differentiation and function of immune cells depend on the intracellular signal transduction pathway. Studies have shown that cadmium promotes monocyte differentiation under specific conditions in vitro (26). In one animal study, myeloid and monocytic cells were increased in bone marrow after intraperitoneal injection of cadmium into mice (27). Another animal study showed an increase in monocytes in rats exposed to cadmium solution for 8 weeks (19). The association of cadmium with monocyte elevation is also found in an epidemiologic study in which cadmium concentrations were higher in workers exposed to occupational exposure to cadmium than in unexposed ones (18). Also, cadmium has been has to cause a reduction in HDL in several animal studies (20,21,22). Although the mechanism by which cadmium causes HDL reduction is not known clearly, it has been reported that the reduction of HDL by cadmium decreases the lipoprotein secretion in the liver due to oxidative stress and disturbance of cell function (28).
Monocyte is a cell that plays a central role in atherosclerosis. Atherosclerosis activates the adhesion molecule of endothelium cells and binds to mononuclear cells. When monocytes are bound to the arterial endothelium, they enter the endothelial lining and enter the intima to form foam cells (29). CD11b+ monocyte is known to play an important role in atherogenesis in this process (30). In addition, circulating monocyte levels are known to affect lesional macrophage accumulation and plaque macrophage content (31). Clinically, monocyte count has been implicated in the development of cardiovascular disease in several epidemiological studies (8,9,10). HDL has also been associated with cardiovascular disease in several epidemiological studies (32,33). HDL suppresses hematopoietic stem cells and multipotent progenitor cell proliferation in the hematopoietic system (34). HDL inhibits monocyte CD11b, leading to mechanisms that act as monocyte activation, spreading, and inhibit activated monocytes (35). HDL also promotes vasorelaxation by increasing the expression of endothelial nitric oxide synthase (eNOS) (36).
MHR is a novel inflammatory marker identified by Kanbay et al. (14) as an independent predictor of cardiovascular disease prediction in patients with chronic kidney disease. The association of MHR with the presence of slow coronary flow and the systemic inflammation marker high sensitivity C-reactive protein (CRP) was reported (12). There was also a relationship between elevation of the Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) score, which is associated with coronary artery anatomy (11), thrombus burden after percutaneous coronary intervention (PCI) (13), and cryoballoon-based catheter ablation in patients with arterial fibrillation. Moreover, the relation between stent restenosis (15) and other cardiovascular outcomes were reported (16). Several studies have consistently demonstrated that MHR is a reliable factor for inflammation and anti-oxidation and is associated with prognosis and disease progression in several cardiovascular diseases. However, there is a lack of research on the significance of MHR as a cardiovascular disease predictor and risk factor in the general population not yet having cardiovascular disease.
Cadmium has been associated with various cardiovascular diseases (2), peripheral vascular disease (3), and cerebrovascular disease (37). It has also been reported that cardiovascular risk factors such as hypertension (4), diabetes (38), and dyslipidemia (39) are also associated with cadmium exposure. Moreover, the inflammatory markers associated with cardiovascular diseases, such as soluble CRP, fibrinogen (6) and urokinase plasminogen activator receptor (7), have been reported to be associated with MHR. As is known, among the subjects of this study, blood cadmium level was associated with hypertension, diabetes and HDL cholesterol level. However, there is no study that investigated the relationship between cadmium and monocyte count and MHR. This study showed that cadmium could have a subclinical effect on the human body even at low concentrations by confirming a dose-dependent association with the monocyte count and MHR, which are the cardiovascular risk and prognostic indicators.
The limitations of this study include that a cross-sectional study cannot clearly identify cause-effect relationships. Also, there is a limit to the fact that we have carried out the study on a special group of Korean fire officers. However, although workers in the firefighting department may be exposed to a variety of chemicals, our data did not show a significant relationship between cadmium exposure, monocyte elevation and working as a firefighter (fire extinguisher and field investigator) (P > 0.200). Although exposure to the fire site may increase the blood level of cadmium for a short period of time, data on recent fire field exposure could not be obtained. However, this study is a study of association parameters rather than population level parameters. It is difficult to say that race and occupation used in this study have effect measure modification in the relationship between cadmium and monocyte. Another limitation is that, the metabolism and health effect of cadmium have been reported to be different in male and female populations (40), therefore, analysis should be done with stratification of sex. However, our study population consisted of 43 female and 733 male subjects without missing value. Therefore, the analysis was done for only the male population in consideration of model instability in regression analysis. In further research, the analysis should include a sufficient number of female subjects.
Monocyte count and MHR are known to be prognostic and predictors of cardiovascular disease, but MHR has not been sufficiently studied in relation to the change of its index in the general population without cardiovascular disease and the clinical state and the onset of cardiovascular disease. In order to confirm a clinical meaning, additional research on the meaning of the monocyte count and MHR in the general population will be needed.
The strong point of this study is that the effect of cadmium exposure can be shown to have a very low threshold. This will be the reference material for evaluating the effects of exposure to low-concentration cadmium at a later time and setting thresholds for biological exposure index and exposure.
This study showed the relationship between blood cadmium level and monocyte count and MHR. This was also statistically significant in the model adjusted for disturbance and other cardiovascular risk factors and showed a linear trend.
Footnotes
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conceptualization: Baek K, Chung IS. Data curation: Baek K, Chung IS. Formal analysis: Baek K, Chung IS. Investigation: Baek K. Writing - original draft: Baek K, Chung IS. Writing - review & editing: Baek K, Chung IS.
References
- 1.Faroon O, Ashizawa A, Wright S, Tucker P, Jenkins K, Ingerman L, Rudisill C. Toxicological Profile for Cadmium. Atlanta, GA: Agency for Toxic Substances and Disease Registry; 2012. [PubMed] [Google Scholar]
- 2.Tellez-Plaza M, Guallar E, Howard BV, Umans JG, Francesconi KA, Goessler W, Silbergeld EK, Devereux RB, Navas-Acien A. Cadmium exposure and incident cardiovascular disease. Epidemiology. 2013;24:421–429. doi: 10.1097/EDE.0b013e31828b0631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tellez-Plaza M, Guallar E, Fabsitz RR, Howard BV, Umans JG, Francesconi KA, Goessler W, Devereux RB, Navas-Acien A. Cadmium exposure and incident peripheral arterial disease. Circ Cardiovasc Qual Outcomes. 2013;6:626–633. doi: 10.1161/CIRCOUTCOMES.112.000134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gallagher CM, Meliker JR. Blood and urine cadmium, blood pressure, and hypertension: a systematic review and meta-analysis. Environ Health Perspect. 2010;118:1676–1684. doi: 10.1289/ehp.1002077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Messner B, Bernhard D. Cadmium and cardiovascular diseases: cell biology, pathophysiology, and epidemiological relevance. Biometals. 2010;23:811–822. doi: 10.1007/s10534-010-9314-4. [DOI] [PubMed] [Google Scholar]
- 6.Lin YS, Rathod D, Ho WC, Caffrey JJ. Cadmium exposure is associated with elevated blood C-reactive protein and fibrinogen in the U. S. population: the third national health and nutrition examination survey (NHANES III, 1988–1994) Ann Epidemiol. 2009;19:592–596. doi: 10.1016/j.annepidem.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Fagerberg B, Borné Y, Barregard L, Sallsten G, Forsgard N, Hedblad B, Persson M, Engström G. Cadmium exposure is associated with soluble urokinase plasminogen activator receptor, a circulating marker of inflammation and future cardiovascular disease. Environ Res. 2017;152:185–191. doi: 10.1016/j.envres.2016.10.019. [DOI] [PubMed] [Google Scholar]
- 8.Pinto EM, Huppert FA, Morgan K. Mrc Cfas, Brayne C. Neutrophil counts, monocyte counts and cardiovascular disease in the elderly. Exp Gerontol. 2004;39:615–619. doi: 10.1016/j.exger.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 9.Kannel WB, Anderson K, Wilson PW. White blood cell count and cardiovascular disease. Insights from the Framingham Study. JAMA. 1992;267:1253–1256. [PubMed] [Google Scholar]
- 10.Lee CD, Folsom AR, Nieto FJ, Chambless LE, Shahar E, Wolfe DA. White blood cell count and incidence of coronary heart disease and ischemic stroke and mortality from cardiovascular disease in African-American and White men and women: atherosclerosis risk in communities study. Am J Epidemiol. 2001;154:758–764. doi: 10.1093/aje/154.8.758. [DOI] [PubMed] [Google Scholar]
- 11.Kundi H, Kiziltunc E, Cetin M, Cicekcioglu H, Cetin ZG, Cicek G, Ornek E. Association of monocyte/HDL-C ratio with SYNTAX scores in patients with stable coronary artery disease. Herz. 2016;41:523–529. doi: 10.1007/s00059-015-4393-1. [DOI] [PubMed] [Google Scholar]
- 12.Canpolat U, Çetin EH, Cetin S, Aydin S, Akboga MK, Yayla C, Turak O, Aras D, Aydogdu S. Association of monocyte-to-HDL cholesterol ratio with slow coronary flow is linked to systemic inflammation. Clin Appl Thromb Hemost. 2016;22:476–482. doi: 10.1177/1076029615594002. [DOI] [PubMed] [Google Scholar]
- 13.Arısoy A, Altunkaş F, Karaman K, Karayakalı M, Çelik A, Ceyhan K, Zorlu Ç. Association of the monocyte to HDL cholesterol ratio with thrombus burden in patients with ST-segment elevation myocardial infarction. Clin Appl Thromb Hemost. 2016 doi: 10.1177/1076029616663850. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 14.Kanbay M, Solak Y, Unal HU, Kurt YG, Gok M, Cetinkaya H, Karaman M, Oguz Y, Eyileten T, Vural A, et al. Monocyte count/HDL cholesterol ratio and cardiovascular events in patients with chronic kidney disease. Int Urol Nephrol. 2014;46:1619–1625. doi: 10.1007/s11255-014-0730-1. [DOI] [PubMed] [Google Scholar]
- 15.Ucar FM. A potential marker of bare metal stent restenosis: monocyte count - to- HDL cholesterol ratio. BMC Cardiovasc Disord. 2016;16:186. doi: 10.1186/s12872-016-0367-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Çiçek G, Kundi H, Bozbay M, Yayla C, Uyarel H. The relationship between admission monocyte HDL-C ratio with short-term and long-term mortality among STEMI patients treated with successful primary PCI. Coron Artery Dis. 2016;27:176–184. doi: 10.1097/MCA.0000000000000343. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Y, Li S, Guo YL, Wu NQ, Zhu CG, Gao Y, Xu RX, Dong Q, Liu G, Sun J, et al. Is monocyte to HDL ratio superior to monocyte count in predicting the cardiovascular outcomes: evidence from a large cohort of Chinese patients undergoing coronary angiography. Ann Med. 2016;48:305–312. doi: 10.3109/07853890.2016.1168935. [DOI] [PubMed] [Google Scholar]
- 18.Karakaya A, Yücesoy B, Sardas OS. An immunological study on workers occupationally exposed to cadmium. Hum Exp Toxicol. 1994;13:73–75. doi: 10.1177/096032719401300202. [DOI] [PubMed] [Google Scholar]
- 19.Kacar Kocak M, Yazihan N, Akcil E, Bay M, Aslan O. The effect of chronic cadmium toxicity on blood pressure and plasma viscosity. Pathophysiol Haemost Thromb. 2010;37:82–87. doi: 10.1159/000323702. [DOI] [PubMed] [Google Scholar]
- 20.Samarghandian S, Azimi-Nezhad M, Shabestari MM, Azad FJ, Farkhondeh T, Bafandeh F. Effect of chronic exposure to cadmium on serum lipid, lipoprotein and oxidative stress indices in male rats. Interdiscip Toxicol. 2015;8:151–154. doi: 10.1515/intox-2015-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rogalska J, Brzóska MM, Roszczenko A, Moniuszko-Jakoniuk J. Enhanced zinc consumption prevents cadmium-induced alterations in lipid metabolism in male rats. Chem Biol Interact. 2009;177:142–152. doi: 10.1016/j.cbi.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 22.Olisekodiaka MJ, Igbeneghu CA, Onuegbu AJ, Oduru R, Lawal AO. Lipid, lipoproteins, total antioxidant status and organ changes in rats administered high doses of cadmium chloride. Med Princ Pract. 2012;21:156–159. doi: 10.1159/000333385. [DOI] [PubMed] [Google Scholar]
- 23.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S1–S45. doi: 10.1161/01.cir.0000437738.63853.7a. [DOI] [PubMed] [Google Scholar]
- 24.Järup L, Berglund M, Elinder CG, Nordberg G, Vahter M. Health effects of cadmium exposure--a review of the literature and a risk estimate. Scand J Work Environ Health. 1998;24(Suppl 1):1–51. [PubMed] [Google Scholar]
- 25.Shin JY, Kim JM, Kim Y. The association of heavy metals in blood, fish consumption frequency, and risk of cardiovascular diseases among Korean adults: the Korean National Health and Nutrition Examination Survey (2008–2010) Korean J Nutr. 2012;45:347–361. [Google Scholar]
- 26.Ober-Blöbaum JL, Engelhardt G, Hebel S, Rink L, Haase H. Cadmium ions promote monocytic differentiation of human leukemia HL-60 cells treated with 1α, 25-dihydroxyvitamin D3. Biol Chem. 2010;391:1295–1303. doi: 10.1515/BC.2010.135. [DOI] [PubMed] [Google Scholar]
- 27.Burchiel SW, Hadley WM, Cameron CL, Fincher RH, Lim TW, Stewart CC. Flow cytometry Coulter volume analysis of lead- and cadmium-induced cellular alterations in bone marrow obtained from young adult and aged Balb/c mice. Toxicol Lett. 1986;34:89–94. doi: 10.1016/0378-4274(86)90149-9. [DOI] [PubMed] [Google Scholar]
- 28.Murugavel P, Pari L. Diallyl tetrasulfide protects cadmium-induced alterations in lipids and plasma lipoproteins in rats. Nutr Res. 2007;27:356–361. doi: 10.1016/j.nutres.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 29.Gerrity RG. The role of the monocyte in atherogenesis: I. Transition of blood-borne monocytes into foam cells in fatty lesions. Am J Pathol. 1981;103:181–190. [PMC free article] [PubMed] [Google Scholar]
- 30.Stoneman V, Braganza D, Figg N, Mercer J, Lang R, Goddard M, Bennett M. Monocyte/macrophage suppression in CD11b diphtheria toxin receptor transgenic mice differentially affects atherogenesis and established plaques. Circ Res. 2007;100:884–893. doi: 10.1161/01.RES.0000260802.75766.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Combadière C, Potteaux S, Rodero M, Simon T, Pezard A, Esposito B, Merval R, Proudfoot A, Tedgui A, Mallat Z. Combined inhibition of CCL2, CX3CR1, and CCR5 abrogates Ly6C(hi) and Ly6C(lo) monocytosis and almost abolishes atherosclerosis in hypercholesterolemic mice. Circulation. 2008;117:1649–1657. doi: 10.1161/CIRCULATIONAHA.107.745091. [DOI] [PubMed] [Google Scholar]
- 32.Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am J Med. 1977;62:707–714. doi: 10.1016/0002-9343(77)90874-9. [DOI] [PubMed] [Google Scholar]
- 33.Després JP, Lemieux I, Dagenais GR, Cantin B, Lamarche B. HDL-cholesterol as a marker of coronary heart disease risk: the Québec cardiovascular study. Atherosclerosis. 2000;153:263–272. doi: 10.1016/s0021-9150(00)00603-1. [DOI] [PubMed] [Google Scholar]
- 34.Westerterp M, Gourion-Arsiquaud S, Murphy AJ, Shih A, Cremers S, Levine RL, Tall AR, Yvan-Charvet L. Regulation of hematopoietic stem and progenitor cell mobilization by cholesterol efflux pathways. Cell Stem Cell. 2012;11:195–206. doi: 10.1016/j.stem.2012.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ansell BJ, Navab M, Hama S, Kamranpour N, Fonarow G, Hough G, Rahmani S, Mottahedeh R, Dave R, Reddy ST, et al. Inflammatory/antiinflammatory properties of high-density lipoprotein distinguish patients from control subjects better than high-density lipoprotein cholesterol levels and are favorably affected by simvastatin treatment. Circulation. 2003;108:2751–2756. doi: 10.1161/01.CIR.0000103624.14436.4B. [DOI] [PubMed] [Google Scholar]
- 36.Kuvin JT, Rämet ME, Patel AR, Pandian NG, Mendelsohn ME, Karas RH. A novel mechanism for the beneficial vascular effects of high-density lipoprotein cholesterol: enhanced vasorelaxation and increased endothelial nitric oxide synthase expression. Am Heart J. 2002;144:165–172. doi: 10.1067/mhj.2002.123145. [DOI] [PubMed] [Google Scholar]
- 37.Peters JL, Perlstein TS, Perry MJ, McNeely E, Weuve J. Cadmium exposure in association with history of stroke and heart failure. Environ Res. 2010;110:199–206. doi: 10.1016/j.envres.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Edwards JR, Prozialeck WC. Cadmium, diabetes and chronic kidney disease. Toxicol Appl Pharmacol. 2009;238:289–293. doi: 10.1016/j.taap.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhou Z, Lu YH, Pi HF, Gao P, Li M, Zhang L, Pei LP, Mei X, Liu L, Zhao Q, et al. Cadmium exposure is associated with the prevalence of dyslipidemia. Cell Physiol Biochem. 2016;40:633–643. doi: 10.1159/000452576. [DOI] [PubMed] [Google Scholar]
- 40.Nishijo M, Satarug S, Honda R, Tsuritani I, Aoshima K. The gender differences in health effects of environmental cadmium exposure and potential mechanisms. Mol Cell Biochem. 2004;255:87–92. doi: 10.1023/b:mcbi.0000007264.37170.39. [DOI] [PubMed] [Google Scholar]