Abstract
Background
Children with food allergies spend a large proportion of time in school but characteristics of allergic reactions in schools are not well studied. Some schools self-designate as peanut-free or have peanut-free areas, but the impact of policies on clinical outcomes has not been evaluated.
Objective
We sought to determine the effect of peanut-free policies on rates of epinephrine administration for allergic reactions in Massachusetts public schools.
Methods
In this retrospective study, we analyzed (1) rates of epinephrine administration in all Massachusetts public schools and (2) Massachusetts public school nurse survey reports of school peanut-free policies from 2006–2011 and whether schools self-designated as “peanut-free” based on policies. Rates of epinephrine administration were compared for schools with or without peanut restrictive policies.
Results
The percentage of schools with peanut restrictive policies did not change significantly in the study timeframe. There was variability in policies used by schools self-designated as peanut-free. No policy was associated with complete absence of allergic reactions. Both self-designated peanut-free schools and schools banning peanuts from being served in school or brought from home reported allergic reactions to nuts. Policies restricting peanuts from home, served in schools or having peanut-free classrooms did not affect epinephrine administration rates. Schools with peanut-free tables, compared to without, had lower rates of epinephrine administration (IR per 10,000 students 0.2 and 0.6, respectively, P=0.009).
Conclusions
These data provide a basis for evidence-based school policies for children with food allergies. Further studies are required before decisions can be made regarding peanut-free policies in schools.
Keywords: peanut allergy, food allergy, anaphylaxis, school, epinephrine
INTRODUCTION
Food allergy affects 4–8% of US children and its prevalence is increasing.(1, 2) Peanut allergy is the third leading food allergy in US children and rates are rising.(3) Peanut allergy is a frequent cause of fatal reactions and the most common cause of anaphylaxis in schools.(4, 5) Children spend a majority of their time in schools and 16–18% of children with food allergies experience reactions in school.(6, 7) Twenty-eight percent of children with peanut or tree nut allergy experiencing reactions in schools require epinephrine.(7) Peanut-free policies exist in some schools,(8) but it is unclear what policy, if any, is effective at preventing allergic reactions.
An unanswered question for families and school policymakers is the role of peanut-free tables, classrooms and/or schools. Banning peanuts from schools may reduce exposure to a potentially lethal allergen; however, bans are difficult to enforce and may cause a false sense of security.(8) Peanut-free guidelines have resulted in decreased peanut content of lunches,(9) but the impact on allergic reactions was not evaluated. Controversies over pros and cons of school peanut-free policies result from lack of evidence regarding effects of policies on clinical outcomes. The goal of this study was to investigate whether the clinical outcome of epinephrine administration in schools was affected by school peanut-free policies.
We surveyed Massachusetts public school nurses on their schools’ peanut-free policies and compared policies to mandatory reporting of epinephrine administration. We sought to (1) determine the frequency and types of school peanut-free policies and (2) evaluate the impact of peanut-free policies on rates of epinephrine administration for allergic reactions.
METHODS
Determination of Epinephrine Administration in Schools
After administering epinephrine, all Massachusetts school nurses must complete and submit a standardized data collection form (Figure E1)(10) to the Massachusetts Department of Public Health (MDPH). Reporting of epinephrine administration in all Massachusetts schools became mandatory in November 2003 under 105 CMR 210, the Regulations Governing the Administration of Prescription Medications in Public and Private Schools. Nurses completing forms were responsible for supplying allergy histories, including history of known allergy to specific foods, and trigger for reaction, if identifiable. Although nurses could enter “peanut” or “tree nut” (including specific tree nuts, e.g., walnut), in some cases only the word “nut” was supplied. Given difficulty among students, family and staff to correctly identify peanuts and tree nuts,(11, 12) high risk of cross-contamination among peanuts and tree nuts, (13) and generic use of the term “nut,” our analysis was based on “peanut or tree nut” exposure.
We reviewed epinephrine administration data from 2006–2011. Schools ranged from grade pre-kindergarten through special education beyond grade 12. Schools in the study were public schools in rural, suburban and urban settings throughout the state. For purposes of data analysis, grade 5 and below was defined as elementary school, grades 6–8 as middle school and grades 9 and above as high school. Some schools encompassed elementary as well as middle and/or high school grades, and thus were excluded from the analysis of strictly elementary or middle/high schools.
Assessment of School Policies
Through the MDPH, we had access to a database of email addresses for Massachusetts public school nurses. All 379 nurses in the database were surveyed by email to retrospectively report their schools’ peanut-free policies from 2006–2011 (Figure E2). Nurses were asked about the presence of specific policies and also whether their schools self-designated as “peanut free.” A school could be self-designated peanut-free regardless of other specific peanut-restrictive policies in place. Schools that allowed peanuts to be brought from home or served by school were also analyzed regarding policies for peanut-free tables and classrooms. The study was approved by the Institutional Review Board of Boston Children’s Hospital.
Statistical Analysis
Descriptive statistics were used to characterize the sample. Pearson chi-square test was used to compare the prevalence of specific peanut-free policies over time and between grade levels. To model rates of epinephrine administration by academic year and school policies, we used generalized estimating equations (Poisson family, log link), clustering on schools and defining exposure as the total number of students in the school. Wilcoxon rank sum test was used to compare school baseline demographic characteristics. A P value <0.05 was considered statistically significant.
RESULTS
School Epinephrine Administration
The number of students enrolled in Massachusetts public schools per academic year (AY) was publicly available: 968,661 students in 1,875 schools during AY 2006–2007; 962,806 students in 1,870 schools during AY 2007–2008; 958,910 students in 1,846 schools during AY 2008–2009; 975,053 students in 1,831 schools during AY 2009–2010 and 955,563 students in 1,824 schools during AY 2010–2011.
The number of times epinephrine was administered each year for all causes was: 138 during AY 2006–2007; 117 during AY 2007–2008; 140 during AY 2008–2009; 176 during AY 2009–2010 and 168 during AY 2010–2011. The number of times epinephrine was administered each year for reactions to peanuts or tree nuts was: 21 during AY 2006–2007; 20 during AY 2007–2008; 26 during AY 2008–2009; 37 during AY 2009–2010 and 45 during AY 2010–2011. Epinephrine administered for reactions to peanuts or tree nuts is shown in Figure 1. On average, epinephrine administration increased by 23% per year for reactions to peanuts or tree nuts (P<0.001) during 2006–2011. This outpaced rates of epinephrine administration for all causes (P=0.04), which increased by 9% per year during this period. The effect of time on epinephrine use did not vary by school policies (all interaction effects P>0.40). There were no food allergy-related anaphylaxis deaths in Massachusetts public schools during this five-year period.
Figure 1. Epinephrine Administration for Peanut or Tree Nut Exposure by School Year.
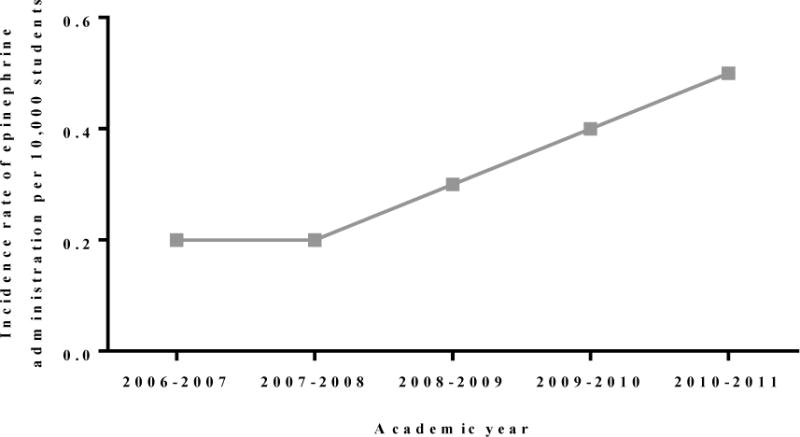
Incidence rate of epinephrine administration by school year for peanut or tree nut reactions. From 2006–2011, epinephrine administration increased each year on average by 23% for reactions to peanut or tree nut (P<0.001).
School Policy Survey Responses
Of the 379 nurses in the MDPH database, 209 (55.1%) responded. Responses represented 1,116,667 students from 2,223 public schools during AY 2006–2011. Some nurses were unable to provide information on all policies for all years, so those schools were excluded from analysis of a given policy. The number of schools was larger than the number of school nurses surveyed, as many nurses oversaw multiple schools. Table I displays baseline characteristics of schools responding to the survey in AY 2010–2011.
Table I.
Baseline Characteristics of Schools Responding to Policy Survey.
| Characteristic | Schools Responding to Survey (n=484) |
|---|---|
| No. students in school, median (IQR) | 428 (294,626) |
| Low income, median (IQR), % | 28 (11,69) |
| Special education, median (IQR), % | 16 (13,20) |
| Race, median (IQR), % | |
| African American | 3.4 (1.2,16.8) |
| Asian | 2.3 (1.1,5.9) |
| Hispanic | 7.1 (2.8,30.4) |
| White | 78.5 (28.4,90.7) |
| Native American | 0.1 (0,0.4) |
| Native Hawaiian, Pacific Islander | 0 (0,0.1) |
IQR, interquartile range
Characteristics of schools responding to survey during AY 2010–2011. Low-income indicates students eligible for free or reduced price lunch, receive Transitional Aid to Families benefits or eligible for food stamps. Special education indicates students with Individualized Education Program. IQR=interquartile range
Characterization of School Policies
We surveyed Massachusetts public school nurses on their schools’ policies (Table II). The percentage of schools self-designating as peanut-free ranged from 1.4–2.9% with no significant change during the study period. The percentage of schools with specific types of peanut restrictions also did not significantly change over the study period. Compared to elementary schools, middle/high schools were more likely to allow peanuts to be brought from home (85.5% [N=666/779] elementary schools and 97.9% [N=457/467] middle/high schools, odds ratio [OR]=7.08, 95% confidence interval [CI]=2.01–24.92, P=0.002), but less likely to have peanut-free tables (96.2% [N=1000/1040] elementary schools and 81.6% [N=565/692] middle/high schools, OR=0.15, 95% CI=0.07–0.33, P<0.001) and classrooms (74.5% [N=752/1010] elementary schools and 58.4% [N=398/681] middle/high schools, OR=0.48, 95% CI=0.32–0.73, P=0.001). Numerators and denominators are the cumulative number of schools with these designations over the five-year study.
Table II.
School Peanut-Free Policy by Academic Year.
| School Policy | Academic Year | ||||
|---|---|---|---|---|---|
| 2006–2007 | 2007–2008 | 2008–2009 | 2009–2010 | 2010–2011 | |
| All schools | |||||
| Self-designated peanut-free school | 6/410 1.5% |
6/423 1.4% |
9/442 2.0% |
11/450 2.4% |
14/480 2.9% |
| No peanuts brought from home | 17/271 6.3% |
27/285 9.7% |
30/305 9.8% |
31/319 9.7% |
35/340 10.3% |
| No peanuts served by school | 149/263 56.7% |
163/278 58.6% |
172/299 57.5% |
185/313 59.1% |
189/334 56.6% |
| Peanut-free tables | 358/396 90.4% |
361/399 90.5% |
374/415 90.1% |
382/422 90.5% |
400/439 91.1% |
| Peanut-free classrooms | 258/386 66.8% |
263/390 67.4% |
272/406 67.0% |
276/413 66.8% |
282/430 65.6% |
| Elementary schools | |||||
| Self-designated peanut-free school | 4/211 1.9% |
5/217 2.3% |
7/226 3.1% |
7/229 3.1% |
9/248 3.6% |
| No peanuts brought from home | 16/141 11.3% |
22/150 14.7% |
24/160 15.0% |
25/170 14.7% |
26/158 16.5% |
| No peanuts served by school | 71/135 52.6% |
79/144 54.9% |
83/155 53.5% |
91/164 55.5% |
94/177 56.6% |
| Peanut-free tables | 193/201 96.0% |
193/201 96.0% |
200/208 96.2% |
201/209 96.2% |
213/221 96.4% |
| Peanut-free classrooms | 145/195 74.4% |
145/195 74.4% |
153/202 75.7% |
153/203 75.4% |
156/215 72.6% |
| Middle/high schools | |||||
| Self-designated peanut-free school | 2/141 1.4% |
1/142 0.7% |
1/144 0.7% |
2/140 1.4% |
3/480 2.0% |
| No peanuts brought from home | 0/88 0% |
2/90 2.2% |
2/93 2.2% |
2/95 2.1% |
4/101 4.0% |
| No peanuts served by school | 50/86 58.1% |
53/90 58.9% |
54/93 58.1% |
55/95 57.9% |
55/102 53.9% |
| Peanut-free tables | 114/139 82.0% |
114/138 82.6% |
114/140 81.4% |
110/136 80.9% |
113/139 81.3% |
| Peanut-free classrooms | 81/186 59.6% |
82/136 60.3% |
81/138 58.7% |
77/134 57.5% |
77/137 56.2% |
Number of schools with a given policy (numerator), total number of schools reporting policy (denominator) and percent of schools with policy are shown. Number of schools reporting policy (denominator) varies on the basis of schools supplying specific policy information for each year. Some schools encompassed elementary and middle/high school grade levels, so were excluded from analysis of strictly elementary or middle/high schools.
During the five-year study, 46 schools self-designated as peanut-free and 45 supplied complete policy information. These 45 schools with complete policy information were further analyzed (Figure 2). The definition of self-designated peanut-free school was variable. All self-designated peanut-free schools banned peanuts from being served. Seventy-one percent also banned peanuts from being brought from home. Twenty-four percent allowed peanuts to be brought from home but had peanut-free tables and classrooms. Four percent allowed peanuts to be brought from home and did not have peanut-free tables or classrooms.
Figure 2. Policies in Self-Designated Peanut-Free Schools.
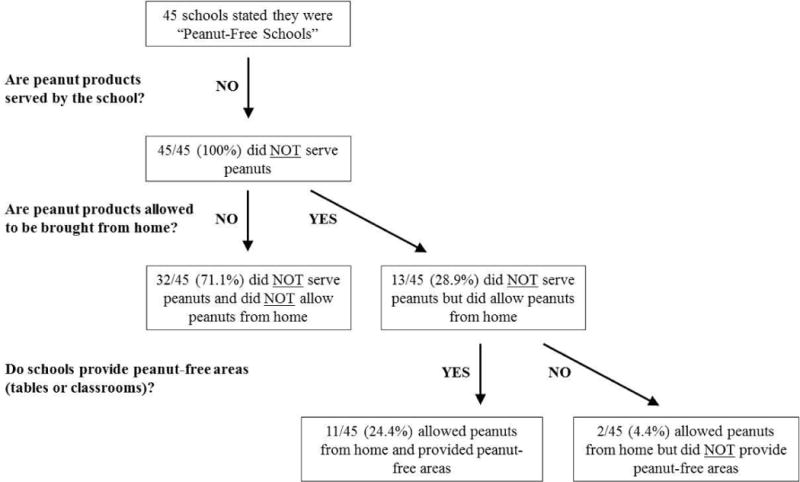
During the five-year study period, 46 schools identified as self-designated peanut-free and complete specific policy information was supplied for 45.
Impact of Policies on Epinephrine Administration
We had detailed school policy information for 18.1% (N=27/149) of students receiving epinephrine for peanut or tree nut exposure during the five-year study (Table III). Survey information was not available for where food exposure occurred, but rather where allergic symptoms developed. Because allergic reactions can occur minutes to hours after food ingestion(14), the location where symptoms developed may not be the same as where allergen exposure occurred.
Table III.
Clinical Information for Students Treated with Epinephrine for Peanut or Tree Nut Exposure.
| Subject number | Age (years) | Gender | Known food allergies | Allergen causing reaction | Source of reaction | Symptoms | Location symptoms developed | Location epinephrine administered | Epinephrine administered by | School Policy | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Self-designated peanut-free school | Peanuts brought from home | Peanuts served by school | Peanut-free tables | Peanut-free classrooms | |||||||||||
| 1 | 8 | Male | Tree nuts | Tree nut | Ate cookie from home containing walnuts | Throat closing | Cafeteria | Nurse’s office | Nurse | Yes | Yes | No | Yes | Yes | |
| 2 | 14 | Female | Peanut | Peanut | Ate peanut butter cookie | Skin (generalized pruritus, flushing, urticaria and/or angioedema); respiratory (rhinorrhea, marked congestion, sensation of throat pruritus and/or tightness in chest or throat PLUS hoarseness, “barky” cough, difficulty swallowing, dyspnea, wheezing and/or cyanosis) | Hallway | Nurse’s office | Nurse | Yes | Yes | No | Yes | Yes | |
| 3 | 8 | Female | Peanut | Peanut | Another student had snack containing peanut butter | Skin (localized pruritus, flushing, urticaria and/or angioedema) | Classroom | Nurse’s office | Nurse | No | No | No | N/A | N/A | |
| 4 | 8 | ND | Nuts | Tree nut | Shared snack containing walnuts/tree nuts with another student | Throat pruritus, progressed to throat closing | Classroom | Nurse’s office | Nurse | No | Yes | No | Yes | Yes | |
| 5 | 11 | ND | None | Peanut | Ate peanuts | Diffuse pruritus, difficulty breathing, shaking and feeling cold | Classroom | Nurse’s office | Nurse | No | Yes | No | Yes | Yes | |
| 6 | 7 | Male | Peanut | Peanut | Ate half of peanut butter and jelly sandwich | Itchy throat and tongue, irregular heart rate | Nurse’s office | Nurse’s office | Nurse | No | Yes | No | Yes | Yes | |
| 7 | 9 | Male | Peanut | Peanut | ND | Respiratory (rhinorrhea, marked congestion, sensation of throat pruritus and/or tightness in chest or throat PLUS hoarseness, “barky” cough, difficulty swallowing, dyspnea, wheezing and/or cyanosis) | Classroom | Nurse’s office | Nurse | No | Yes | No | Yes | Yes | |
| 8 | 7 | Female | Peanut | Peanut | Ate peanut butter | Difficulty swallowing, lip and oropharyngeal angioedema | Cafeteria | Nurse’s office | Nurse | No | Yes | No | Yes | No | |
| 9 | 17 | Female | None | Tree nut | Ate trail mix containing almonds | GI (oral pruritus or “tingling” and/or mild lip swelling PLUS nausea PLUS repetitive vomiting); respiratory (rhinorrhea, marked congestion, sensation of throat pruritus and/or tightness in chest or throat PLUS hoarseness, “barky” cough, difficulty swallowing, dyspnea, wheezing and/or cyanosis) | Classroom | Nurse’s office | Nurse | No | Yes | No | Yes | No | |
| 10 | 15 | Female | Nuts, malt | Peanut | Ate granola bar containing peanut butter | Coughing, chest and throat tightness, difficulty swallowing, oral pruritus, lip swelling | Gym (lunch served in gym) | Nurse’s office | Nurse | No | Yes | No | Yes | No | |
| 11 | 13 | Male | Peanut, tree nuts, kiwi | Tree nut | Ate brownie with walnuts from cafeteria | Respiratory (rhinorrhea, marked congestion, sensation of throat pruritus and/or tightness in chest or throat) | Cafeteria | Nurse’s office | Nurse | No | Yes | No | No | No | |
| 12 | 13 | Female | Peanut | Peanut | Ate half an energy bar containing peanuts | GI (oral pruritus or “tingling” and/or mild lip-swelling PLUS nausea and/or emesis x1); tachycardia | Hallway | Nurse’s office | Nurse | No | Yes | No | No | No | |
| 13 | 8 | Male | Peanut | Peanut | Accidentally took bite of peanut butter and jelly sandwich and spit it out after realizing he ate peanut butter | Tongue and throat pruritus, erythematous rash on neck and face | Cafeteria | Nurse’s office | Nurse | No | Yes | Yes | Yes | Yes | |
| 14 | 6 | ND | Peanut | Peanut | Touched peanut butter in cooking class (family had not informed school of known peanut allergy) | Angioedema of tongue/throat, urticaria | Classroom | Nurse’s office | Nurse | No | Yes | Yes | Yes | Yes | |
| 15 | 5 | Male | Peanut | Peanut | Ate granola bar containing traces of peanuts (child’s mom sent the snack without realizing it contained peanuts) | Wheezing, shortness of breath, periorbital angioedema, rhinorrhea, anxiety | Classroom | Nurse’s office | ND | No | Yes | Yes | Yes | No | |
| 16 | 18 | Male | Fish, shellfish, peanut | Peanut | Ate energy bar containing peanuts | GI (oral pruritus or “tingling” and/or mild lip-swelling PLUS nausea and/or emesis x1) | Locker room | Unknown/other | Self | No | Yes | Yes | Yes | No | |
| 17 | 17 | Female | None | Tree nut | Ate almonds | GI (oral pruritus or “tingling” and/or mild lip-swelling); respiratory (rhinorrhea, marked congestion, sensation of throat pruritus and/or tightness in chest or throat PLUS hoarseness, “barky” cough, difficulty swallowing, dyspnea, wheezing and/or cyanosis) | Walking back from lunch | Nurse’s office | Nurse | No | Yes | Yes | Yes | No | |
| 18 | 12 | Female | Peanut | Peanut | Ate cookie containing peanut butter | Dry mouth | Classroom | ND | ND | No | Yes | Yes | Yes | No | |
| 19 | 13 | Female | Tree nuts | Nut | Ate coffee cake that may have contained nuts | Respiratory (rhinorrhea, marked congestion, sensation of throat pruritus and/or tightness in chest or throat) | Field trip | Field trip | Nurse | No | Yes | Yes | Yes | ND | |
| 20 | 15 | Female | Citrus fruit | Tree nut | Ate almonds the evening prior | Difficulty breathing, chest pressure | Nurse’s office | Nurse’s office | Nurse | No | Yes | Yes | No | No | |
| 21 | 15 | Female | Tree nuts | Nut | Ate nuts the evening prior | Difficulty breathing, throat tightness | Nurse’s office | ND | Nurse | No | Yes | Yes | No | No | |
| 22 | 16 | Female | Tree nuts | Tree nut | Ate chocolate bar containing tree nuts | Urticaria, throat closing | Nurse’s office | Nurse’s office | Nurse | No | Yes | Yes | No | No | |
| 23 | 15 | ND | Peanut, tree nuts | Nut | Nut exposure by possible inhalation | Throat pruritus, chest tightness, chest pressure | Cafeteria | Nurse’s office | Nurse | No | Yes | Yes | No | No | |
| 24 | 15 | Female | Tree nuts, celery | Nut | Ate candy bar containing nuts | Skin (generalized pruritus, flushing, urticaria and/or angioedema); respiratory (rhinorrhea, marked congestion, sensation of throat pruritus and/or tightness in chest or throat PLUS hoarseness, “barky” cough, difficulty swallowing, dyspnea, wheezing and/or cyanosis) | Commons | Nurse’s office | Nurse | No | Yes | Yes | No | No | |
| 25 | 9 | Female | Fish, shellfish, peanut | Peanut | Ate peanut butter in cafeteria | Skin (generalized pruritus, flushing, urticaria and/or angioedema); GI (oral pruritus or “tingling” and/or mild lip-swelling); respiratory (rhinorrhea, marked congestion, sensation of throat pruritus and/or tightness in chest or throat PLUS hoarseness, “barky” cough, difficulty swallowing, dyspnea, wheezing and/or cyanosis) | Classroom | Nurse’s office | Nurse | No | ND | ND | Yes | Yes | |
| 26 | 7 | Male | None | Peanut | Ate peanut butter sandwich | Skin (generalized pruritus, flushing, urticaria and/or angioedema); respiratory (rhinorrhea, marked congestion, sensation of throat pruritus and/or tightness in chest or throat) | Cafeteria | Nurse’s office | Nurse | No | ND | ND | Yes | Yes | |
| 27 | 10 | Male | Peanut | Peanut | Ate granola bar containing peanuts | Difficulty breathing, abdominal discomfort, skin flushing | Classroom | Nurse’s office | Nurse | No | ND | ND | Yes | Yes | |
One hundred and forty-nine students were treated with epinephrine for peanut or tree nut exposure during the five-year study period. Data for the 27 students for which school policy information was available are presented. In most cases, specific allergic reaction symptoms were documented. However, for subjects 2, 3, 7, 9, 11, 16, 17, 19 and 24–26, symptoms are reported in general categories, reflecting that year’s school reporting form documentation.
CV=cardiovascular
GI=gastrointestinal
ND=not documented
N/A=not applicable
We compared reporting of epinephrine administration for peanut or tree nut reactions to policies (Figure 3). Schools with peanut-free tables compared to without, had lower epinephrine administration rates (incidence rate [IR] per 10,000 students 0.2 and 0.6, respectively, P=0.009). Policies restricting peanuts brought from home, served in schools or having peanut-free classrooms had no effect on epinephrine administration rates. There was no difference in the impact of school policies on epinephrine administration for children with previously diagnosed versus new presentation of peanut or tree nut allergies. Stratified by grade level, middle/high schools with peanut-free classrooms compared to without had lower epinephrine administration rates (IR per 10,000 students 0.1 and 0.5, respectively, P=0.01). Grade level did not moderate the effect of other policies.
Figure 3. Epinephrine Administration for Peanut or Tree Nut Reactions by School Policy.
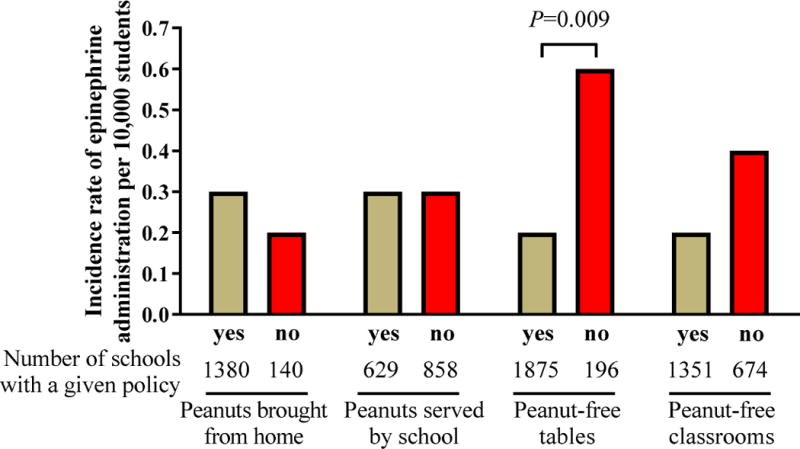
Incidence rate of epinephrine administration by policy pooled from 2006–2011. Number of schools with a given policy pooled from 2006–2011 are indicated.
School policies had no effect on rates of epinephrine administration for any cause, other food exposures or unknown triggers. Therefore, statistically significant differences in epinephrine administration in schools with policies regarding peanut-free tables and self-designation of peanut-free were specific to reactions to peanuts and tree nuts and not to other allergens.
Self-designated peanut-free compared to non-self-designated peanut-free schools had higher epinephrine administration rates (IR per 10,000 students 1.0 and 0.2, respectively, P =0.04). This finding was statistically significant, but because of the small number of self-designated peanut-free schools, there were only two students in two self-designated peanut-free schools treated with epinephrine (Table III): an 8-year-old boy with known tree nut allergy ate a walnut-containing cookie and developed symptoms in the cafeteria (subject 1) and a 14-year-old girl with known peanut allergy ate a peanut butter cookie and developed symptoms in the hallway (subject 2). It was not known where the peanut butter cookie was obtained but the walnut-containing cookie was brought from home. Both reactions occurred in schools that did not serve peanuts and had peanut-free tables and classrooms, but did allow peanuts to be brought from home. It was not known if the initial ingestions happened at peanut-free tables or in peanut-free classrooms.
There was no difference in epinephrine administration rates for schools both banning peanuts from being brought from home and not serving peanuts—what might be considered a “true” peanut-free school—compared to schools allowing peanuts from home and/or served by schools (IR per 10,000 students 0.3 and 0.3, respectively, P =0.88). There was one student in one school banning peanuts from being brought from home and served by school treated with epinephrine: an 8-year-old girl with known peanut allergy was exposed to another student with a snack containing peanut butter and developed symptoms in the classroom (subject 3). This school was not self-designated peanut-free. Of the 74 schools banning peanuts from being brought from home and served by schools, 43.2% (N=32) identified as self-designated peanut-free schools.
DISCUSSION
Our study is the first examining epinephrine administration rates for peanut and tree nut reactions in schools over time, and rates are increasing. While Banerjee et al. demonstrated peanut-free classrooms were associated with decreased lunch peanut content,(9) no studies have examined clinical outcomes of schools’ peanut-free policies. This is a crucial public policy question that must be addressed, especially as rates of food allergy and anaphylaxis to peanuts and tree nuts in schools rise. To attempt to improve the safety of children with food allergies in schools, the Centers for Disease Control and Prevention, in consultation with the U.S. Department of Education, developed voluntary guidelines for managing food allergies in schools.(15) Within this document, there are no formal recommendations for schools to implement school-wide nut-free policies.
Current food allergy management consists of allergen avoidance and treating severe reactions with epinephrine.(16) Allergen avoidance in children poses unique challenges due to variable age-related communication and attention skills, poor impulse control, frequent tactile behaviors resulting in oral exposures and reliance on multiple caregivers for food allergy management and treatment.(8) These issues naturally raise the concern for families, school personnel, caregivers and the community in how to balance safety concerns with non-evidence-based policies that may be difficult to implement and could be perceived as overly restrictive.
A unique finding of our study was the diversity of school policies restricting peanuts. From 2006–2011, 56.6–59.1% of schools banned peanuts from being served, 90.5–91.1% had peanut-free tables, 65.6–67.4% had peanut-free classrooms and 6.3–10.3% banned peanuts from home. Importantly, there was considerable variability in how schools defined a self-designated peanut-free school, making the term misleading and open to misinterpretation. This poses significant risks for food-allergic children if people assume that the school environment contains no peanut when in fact peanut may be present. In a telephone survey of 80 schools and pre-schools in Maryland and Virginia during 1999–2000,(6) 26% had peanut-free tables, 24% restricted peanuts from schools or classrooms and 4% banned peanuts or tree nuts from being served by the school. In contrast, we found considerably more schools with peanut-free tables and classrooms and that banned peanuts from being served. This 2001 study was performed earlier in the peanut allergy epidemic, so policies may have changed significantly over the years.
Ours is the first study correlating specific peanut-restrictive policies with the outcome of epinephrine administration in school settings. Previous studies have described characteristics, triggers and emergency management of anaphylactic reactions in schools,(6, 10) but none has evaluated the impact of peanut-free policies on anaphylaxis. We examined the association between school policies and epinephrine administration and found that the presence of peanut-free tables was associated with decreased epinephrine administration rates. Although statistically significant, this finding was due to 7 reactions in 196 schools without peanut-free tables, compared to 19 reactions in 1,875 schools with peanut-free tables. The presence of peanut-free classrooms and banning peanuts from being brought from home or served by schools had no significant effect on epinephrine administration rates. One explanation for these findings is that policies regarding peanut-free classrooms or banning peanuts from being brought from home or served by schools are not effective at reducing exposure to peanuts and tree nuts. If peanuts are truly not allowed or present in these settings, one would expect a reduction in epinephrine administration rates. Therefore, it is likely that variability and/or difficulty in enforcing policies accounts for the lack of apparent impact. For example, schools may differ on who determines whether a food is “peanut-free” or “tree nut-free;” school personnel and students/families may have different interpretations of what constitutes a “peanut-free” or “tree nut-free” food; and students/families—with and without food allergies—may not always read labels carefully before sending food to school.
Self-designated peanut-free schools had higher epinephrine administration rates compared to schools not self-designated as peanut-free. This difference was due to reactions in two students in self-designated peanut-free schools that did not serve peanuts and had peanut-free classrooms and tables, but did allow peanuts brought from home. This highlights the fact that self-designated peanut-free schools allowing peanuts to be brought in are not “peanut-free.” It is noteworthy that the child with known tree nut allergy reacted to a walnut-containing cookie brought from his own home. Interestingly, there was no difference in rates of epinephrine administration in schools that banned peanuts from being brought from home and served by schools—what might be considered a “true” peanut-free school—compared to schools that allowed peanuts from home and/or served by schools. In fact, one student in a school that banned peanuts from being brought from home or served by the school reacted to a classmate’s peanut-containing snack. These reactions underscore the need for parents, school staff and children, as developmentally appropriate, to remain vigilant and carefully read food labels, even if they believe they are in a “peanut-free” setting.
From a practical perspective, it may be easier for school staff to enforce specific food allergen-free tables, affecting a limited number of students, rather than implementing classroom-wide or school-wide bans on specific food allergens. This is supported by our finding that peanut-free tables but not school-wide policies of banning peanuts from being served by or brought to school or labeling a school as peanut-free were associated with decreased rates of epinephrine administration.
Several limitations in our study must be acknowledged. We relied on school nurse reports of school policies, epinephrine administration and allergic triggers, which could introduce bias. However, school nurses, with their integral role in managing food-allergic children,(17–19) should provide an acceptable representation.(20) Reporting of epinephrine administration in Massachusetts schools is mandatory, and school nurses are experienced at accurately completing reporting questionnaires.(10) We used epinephrine administration as a proxy for anaphylaxis. However, allergic reactions can vary in severity and there may be heterogeneity in treatment.(16) We acknowledge that some symptoms may be misclassified as not being allergic reactions, and alternatively some symptoms may be incorrectly attributed to allergic reactions. Further, school nurses and students may not have been able to accurately identify the cause of an allergic reaction. The MDPH questionnaire provides information on where allergic symptoms developed, but not where allergen exposure occurred. Therefore, when analyzing the impact of peanut-free tables or classrooms on allergic reactions, if exposures did not occur at tables or in classrooms, the impacts of these policies could be overestimated or underestimated.
We received responses from 55.1% of nurses surveyed on policies, representing 24.0% of Massachusetts public schools. Schools supplying information may not be representative of all Massachusetts schools. Compared to schools not supplying policy information, either because nurse contact information was unavailable to distribute surveys or nurses did not return questionnaires, schools responding had similar numbers of enrolled students and proportions of low-income students and students in special education, but had a higher proportion of racial minorities (21.5% versus 18.1%, P<0.001). Our survey was limited to public school nurses, and prevalence of policies and rates and treatment of allergic reactions may differ between public and private schools.
Given difficulty among children, adults and health care professionals to correctly identify peanuts and tree nuts,(11, 12) and high risk of cross-contamination, we analyzed epinephrine administered for combined peanut and tree nut reactions rather than only peanuts. However, our survey focused on peanut-free rather than peanut and tree nut-free policies and we compared these policies to epinephrine administration for peanuts and tree nuts. This could result in potential misrepresentation of the effects of peanut-free policies, because peanut-free policies may not address the presence of tree nuts. Schools with peanut-free policies may have a higher prevalence of peanut and tree nut-allergic students or a lower threshold for suspecting and treating allergic reactions, which could impact results.
When considering the implications of our findings and proposing school policies for management of students with food allergies, we must recognize that school-wide peanut-free policies affect all students and families, not just those with food allergies. Potential positive impacts are improving the safety of children with food allergies and increasing school and community awareness of food allergy and management. However, there may be unanticipated negative consequences of certain policies. For example, children at peanut-free tables may feel isolated from peers and could become targets of bullies. This is not insignificant, as children with food allergies report decreased quality of life,(21, 22) increased stress and anxiety,(23–25) and are frequent victims of bullying, often in schools and by classmates.(23) Policy-makers need to consider these issues and make thoughtful decisions such as, for example, allowing friends with “safe” lunches to be seated at peanut-free tables(1) or allowing students to “opt out” of sitting at peanut-free tables if psychosocial consequences outweigh potential medical safety benefits. Policies may also negatively impact students without food allergies. Students without allergies may be prevented from bringing lunches containing peanuts or tree nuts, causing frustration for students and families. Peanuts and tree nuts can be healthy and important nutrition sources for nonallergic children and may be key components of certain diets such as vegetarians.(26)
Our findings provide the first report of the prevalence and range of school peanut-free policies and the potential impact on allergic reactions. The lack of uniformity in school peanut-free policies is concerning and suggests the need for standardizing these policies, or, perhaps better, eliminating the label of self-designated peanut-free school and instead using descriptive terminology for specific restriction policies. This study is a first step that can lead to evidence-based school policies that could significantly improve safety for children with food allergies in schools. Implementing school policies focused specifically on peanut-free tables may decrease rates of allergic reactions and epinephrine administration for peanut or tree nut exposure. However, since a small number of students had allergic reactions in schools without peanut-free tables in our study, it is possible that larger studies may not show that peanut-free tables are effective at decreasing reactions. The success of policies will likely depend largely on the extent to which policies are appropriately and consistently enforced. Regardless of policies in place, it is important to remain vigilant that food allergens may still make their way into schools despite such policies, and to always have ready access to epinephrine for timely treatment. Our hope is that our findings will lead to evidence-based strategies and policies for preventing food allergic reactions and anaphylaxis in schools.
CONCLUSIONS
Anaphylaxis in schools is a significant public health problem. Schools with peanut-free tables compared to those without, had lower epinephrine administration rates for peanut or tree nut reactions. Our data provide the first report of school peanut-free policies and the impact of these policies on epinephrine administration. Determining the influence of peanut-free policies on allergic reactions may inform school policies for food allergy management.
Supplementary Material
Figure E1. School Report of Epinephrine Administration. Survey completed by Massachusetts school nurses following every administration of epinephrine.
Figure E2. School Policy Survey. Survey completed by Massachusetts public school nurses regarding their schools’ peanut-free policies.
CLINICAL IMPLICATIONS.
Schools with peanut-free tables, compared to without, had lower epinephrine administration rates. Other peanut restrictive policies did not affect epinephrine administration rates. These findings may inform school policies.
CAPSULE SUMMARY.
In this retrospective study of epinephrine administration in Massachusetts public schools, schools with peanut-free tables, compared to without, had lower epinephrine administration rates. Other peanut restrictive policies did not affect epinephrine administration rates.
Acknowledgments
Funding: This research is supported by NIH grants R01 AI 073964, U01 AI 110397 and K24 AI 106822 (PI, Dr. Phipatanakul), an NIH Pediatric Research Loan Repayment Program grant L40 AI 113590 (PI, Dr. Bartnikas) and NIH grant K23 AI 104780 (PI, Dr. Sheehan). Funding was provided by The Allergy and Asthma Awareness Initiative, Inc. This work was conducted with support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR001102) and financial contributions from Harvard University and its affiliated academic health care centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, or the National Institutes of Health.
Abbreviations
- AY
academic year
- CV
cardiovascular
- GI
gastrointestinal
- IR
incidence rate
- MDPH
Massachusetts Department of Public Health
- ND
not documented
- N/A
not applicable
- OR
odds ratio
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sicherer SH, Mahr T. American Academy of Pediatrics Section on A, Immunology. Management of food allergy in the school setting. Pediatrics. 2010;126(6):1232–9. doi: 10.1542/peds.2010-2575. [DOI] [PubMed] [Google Scholar]
- 2.Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011;128(1):e9–17. doi: 10.1542/peds.2011-0204. [DOI] [PubMed] [Google Scholar]
- 3.Sicherer SH, Sampson HA. Food allergy. J Allergy Clin Immunol. 2010;125(2 Suppl 2):S116–25. doi: 10.1016/j.jaci.2009.08.028. [DOI] [PubMed] [Google Scholar]
- 4.Longo G, Berti I, Burks AW, Krauss B, Barbi E. IgE-mediated food allergy in children. Lancet. 2013;382(9905):1656–64. doi: 10.1016/S0140-6736(13)60309-8. [DOI] [PubMed] [Google Scholar]
- 5.Shah SS, Parker CL, O’Brian Smith E, Davis CM. Disparity in the Availability of Injectable Epinephrine in a Large, Diverse US School District. J Allergy Clin Immunol Pract. 2014;2(3):288–93 e1. doi: 10.1016/j.jaip.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 6.Nowak-Wegrzyn A, Conover-Walker MK, Wood RA. Food-allergic reactions in schools and preschools. Arch Pediatr Adolesc Med. 2001;155(7):790–5. doi: 10.1001/archpedi.155.7.790. [DOI] [PubMed] [Google Scholar]
- 7.Sicherer SH, Furlong TJ, DeSimone J, Sampson HA. The US Peanut and Tree Nut Allergy Registry: characteristics of reactions in schools and day care. J Pediatr. 2001;138(4):560–5. doi: 10.1067/mpd.2001.111821. [DOI] [PubMed] [Google Scholar]
- 8.Young MC, Munoz-Furlong A, Sicherer SH. Management of food allergies in schools: a perspective for allergists. J Allergy Clin Immunol. 2009;124(2):175–82. 82 e1–4. doi: 10.1016/j.jaci.2009.04.004. quiz 83–4. [DOI] [PubMed] [Google Scholar]
- 9.Banerjee DK, Kagan RS, Turnbull E, Joseph L, St Pierre Y, Dufresne C, et al. Peanut-free guidelines reduce school lunch peanut contents. Arch Dis Child. 2007;92(11):980–2. doi: 10.1136/adc.2006.113118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McIntyre CL, Sheetz AH, Carroll CR, Young MC. Administration of epinephrine for life-threatening allergic reactions in school settings. Pediatrics. 2005;116(5):1134–40. doi: 10.1542/peds.2004-1475. [DOI] [PubMed] [Google Scholar]
- 11.Kao L, Bhangoo PS, Roy L, Bird JA. Identification of peanuts and tree nuts: are allergists smarter than their patients? Ann Allergy Asthma Immunol. 2013;111(4):282–5. doi: 10.1016/j.anai.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 12.Hostetler TL, Hostetler SG, Phillips G, Martin BL. The ability of adults and children to visually identify peanuts and tree nuts. Ann Allergy Asthma Immunol. 2012;108(1):25–9. doi: 10.1016/j.anai.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 13.Furlong TJ, DeSimone J, Sicherer SH. Peanut and tree nut allergic reactions in restaurants and other food establishments. J Allergy Clin Immunol. 2001;108(5):867–70. doi: 10.1067/mai.2001.119157. [DOI] [PubMed] [Google Scholar]
- 14.Sampson HA, Aceves S, Bock SA, James J, Jones S, Lang D, et al. Food allergy: a practice parameter update-2014. J Allergy Clin Immunol. 2014;134(5):1016–25 e43. doi: 10.1016/j.jaci.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Voluntary guidelines for managing food allergies in schools and early care and education programs. Washington, DC: US Department of Health and Human Services; 2013. [Google Scholar]
- 16.Lieberman P, Nicklas RA, Randolph C, Oppenheimer J, Bernstein D, Bernstein J, et al. Anaphylaxis-a practice parameter update 2015. Ann Allergy Asthma Immunol. 2015;115(5):341–84. doi: 10.1016/j.anai.2015.07.019. [DOI] [PubMed] [Google Scholar]
- 17.Robinson JM, Ficca M. Managing the student with severe food allergies. J Sch Nurs. 2012;28(3):187–94. doi: 10.1177/1059840511429686. [DOI] [PubMed] [Google Scholar]
- 18.Zadikoff EH, Whyte SA, Desantiago-Cardenas L, Harvey-Gintoft B, Gupta RS. The development and implementation of the Chicago public schools emergency EpiPen(R) policy. The Journal of school health. 2014;84(5):342–7. doi: 10.1111/josh.12147. [DOI] [PubMed] [Google Scholar]
- 19.Carlisle SK, Vargas PA, Noone S, Steele P, Sicherer SH, Burks AW, et al. Food allergy education for school nurses: a needs assessment survey by the consortium of food allergy research. J Sch Nurs. 2010;26(5):360–7. doi: 10.1177/1059840510369482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knorr RS, Condon SK, Dwyer FM, Hoffman DF. Tracking pediatric asthma: the Massachusetts experience using school health records. Environ Health Perspect. 2004;112(14):1424–7. doi: 10.1289/ehp.7146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Avery NJ, King RM, Knight S, Hourihane JO. Assessment of quality of life in children with peanut allergy. Pediatr Allergy Immunol. 2003;14(5):378–82. doi: 10.1034/j.1399-3038.2003.00072.x. [DOI] [PubMed] [Google Scholar]
- 22.Primeau MN, Kagan R, Joseph L, Lim H, Dufresne C, Duffy C, et al. The psychological burden of peanut allergy as perceived by adults with peanut allergy and the parents of peanut-allergic children. Clin Exp Allergy. 2000;30(8):1135–43. doi: 10.1046/j.1365-2222.2000.00889.x. [DOI] [PubMed] [Google Scholar]
- 23.Shemesh E, Annunziato RA, Ambrose MA, Ravid NL, Mullarkey C, Rubes M, et al. Child and parental reports of bullying in a consecutive sample of children with food allergy. Pediatrics. 2013;131(1):e10–7. doi: 10.1542/peds.2012-1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bacal LR. The impact of food allergies on quality of life. Pediatr Ann. 2013;42(7):141–5. doi: 10.3928/00904481-20130619-12. [DOI] [PubMed] [Google Scholar]
- 25.Lieberman JA, Weiss C, Furlong TJ, Sicherer M, Sicherer SH. Bullying among pediatric patients with food allergy. Ann Allergy Asthma Immunol. 2010;105(4):282–6. doi: 10.1016/j.anai.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 26.O’Neil CE, Keast DR, Nicklas TA, Fulgoni VL., 3rd Out-of-hand nut consumption is associated with improved nutrient intake and health risk markers in US children and adults: National Health and Nutrition Examination Survey 1999–2004. Nutrition research. 2012;32(3):185–94. doi: 10.1016/j.nutres.2012.01.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure E1. School Report of Epinephrine Administration. Survey completed by Massachusetts school nurses following every administration of epinephrine.
Figure E2. School Policy Survey. Survey completed by Massachusetts public school nurses regarding their schools’ peanut-free policies.


