Abstract
Purpose
To study the distribution of isolates and antimicrobial susceptibility of gram-negative bacteria among culture positive vitreous samples from patients with endophthalmitis.
Methods
The records from culture positive vitreous isolates (endophthalmitis cases) during a 24-year period (December 1990 to December 2014), at the Microbiology Department of Bascom Palmer Eye Institute were reviewed.
Results
In the current study, gram-negative bacteria were reported in 246/2134 (11.5%) vitreous isolates from endophthalmitis patients during 24-year period (December 1990 to December 2014) from a University Referral Center. The antimicrobial susceptibility to fluoroquinolones, aminoglycosides, carbapenems and ceftazidime remained stable among gram-negative bacteria during the study period.
Discussion/Conclusion
Antibiotic susceptibility pattern of gram-negative bacteria from vitreous isolates did not change significantly during the 24-year study period.
Keywords: antimicrobial susceptibility, endophthalmitis, gram-negative bacteria, gram-negative isolates
Introduction
Vitreous isolates obtained from patients with endophthalmitis are predominantly gram positive bacteria. Endophthalmitis caused by gram-negative bacteria is less common compared to gram-positive bacteria and generally has poor visual acuity outcomes. Gram-negative bacteria in the current study were classified in two groups: Enterics (Enterobacteriaceae) and Non-Enterics (Non-Enterobacteriaceae) on the basis of their biochemical profile and antibiotic resistance. Enterobacteriaceae group have pathogens which are becoming increasingly multidrug resistant and this is especially true of third generation cephalosporins due to the overproduction of beta-lactamases. However, Non-Enterobacteriaceae group are known to be inherently resistant to many third generation cephalosporins and fluoroquinolones. There are reports of increasing drug resistance among gram-negative bacteria to fluoroquinolones, aminoglycosides, piperacillin-tazobactam and ceftazidime.1,2 The purpose of the current study is to describe gram-negative bacteria among culture positive vitreous samples in order to report the distribution of isolates and antimicrobial susceptibilities.
Methods
The records from culture positive vitreous isolates (endophthalmitis cases) during a 24-year period (December 1990 to December 2014), at the Microbiology Department of Bascom Palmer Eye Institute were reviewed. The groups were divided into two time periods: Time Period I (December 1990 – December 1999) and Time Period II (January 2000 – December 2014). Gram-negative organisms in the current study were further grouped under two broad categories: Enterobacteriaceae group and Non-Enterobacteriaceae group. Distribution of gram-negative bacteria among culture positive vitreous samples were recorded and analyzed. Antimicrobial susceptibilities (measured by disk diffusion, Vitek 2, and Etest) were evaluated for four antibiotic groups: aminoglycosides, cephalosporins, carbapenems and fluoroquinolones.
The current study did not require Informed consent and institutional review board approval because samples were taken as part of routine medical care unrelated to this study and no patient identifying information was collected. For the same reasons, the Health Insurance Portability and Accountability Act compliance did not apply to this study.
Results
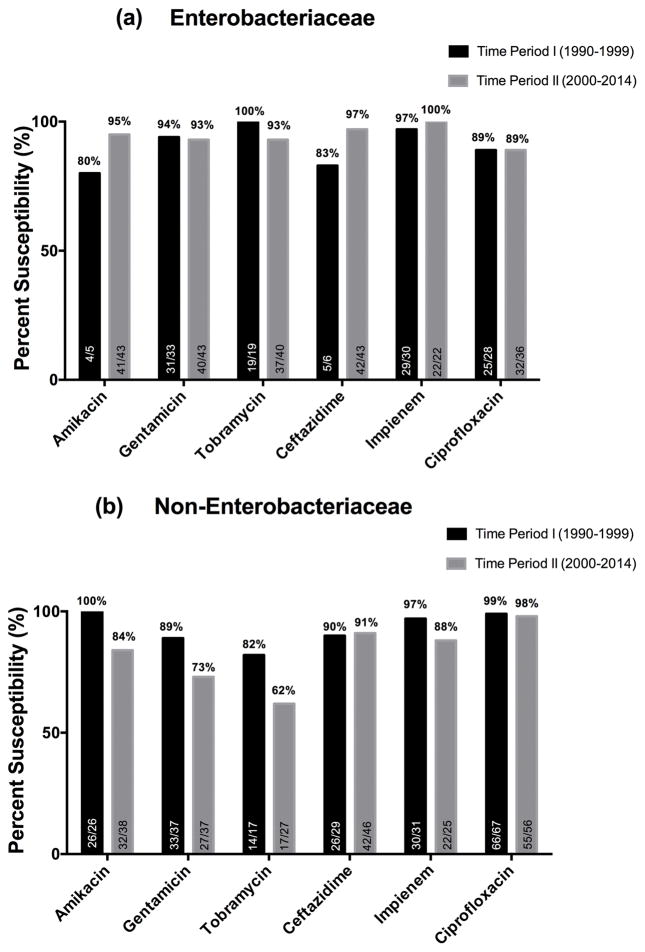
There were 2134 culture positive vitreous isolates with 1888/2134 (88.5%) gram-positive isolates and 246/2134 (11.5%) gram-negative isolates. Among 246 gram-negative isolates, there were 86 isolates from Enterobacteriaceae group and 160 isolates from Non-Enterobacteriaceae group. Distribution of gram-negative bacteria in the current study during Time Period I and Time Period II are shown in Table 1. Although there were some fluctuations in the distribution of organisms identified over time, the differences were small and were not statistically significant. Antimicrobial susceptibility among gram-negative organisms (Enterobacteriaceae group and Non-Enterobacteriaceae group) is shown in Figure 1a and 1b. Again there was no significant change in antimicrobial susceptibilities between the two time periods. Antimicrobial susceptibilities among Non-Enterobacteriaceae to gentamycin and tobramycin showed a slight decrease from time period I to Time period II but due to small sample size, this difference is not clinically significant.
Table 1.
Distribution of gram-negative bacteria (N=246) among culture positive vitreous samples during a period of 24 years (December 1990 to December 2014) at a University Referral Center.
| Gram-negative bacteria isolated | During 24 years (1990 – 2014) | Time Period I (1990–1999) | Time Period II (2000–2014) |
|---|---|---|---|
|
| |||
| Enterobacteriaceae group (N=86) | 86/246 | 40/125 | 46/121 |
| Non-Enterobacteriaceae group (N=160) | 160/246 | 85/125 | 75/121 |
|
| |||
| Enterobacteriaceae group | N=86 | N=40 | N=46 |
|
| |||
| Number of isolates n/N (%) | Number of isolates n/N (%) | Number of isolates n/N (%) | |
|
| |||
| • Proteus mirabilis | 13/86 (15%) | 12/40 (30%) | 1/46 (2%) |
|
| |||
| • Serratia marcescens | 24/86 (28%) | 8/40 (20%) | 16/46 (35%) |
|
| |||
| • Klebsiella pneumoniae | 12/86 (14%) | 7/40 (18%) | 5/46 (11%) |
|
| |||
| • Enterobacter species | 17/86 (20%) | 6/40 (15%) | 11/46 (24%) |
|
| |||
| • Eschericihia coli | 6/86 (7%) | 3/40 (8%) | 3/46 (7%) |
|
| |||
| • Achromobacter Xylosoxidans | 5/86 (6%) | 2/40 (5%) | 3/46 (7%) |
|
| |||
| • Klebsiella oxytoca | 2/86 (2%) | 2/40 (5%) | none |
|
| |||
| • Pantoea agglomerans | 2/86 (2%) | none | 2/46 (4%) |
|
| |||
| • Citrobacter freudii | 2/86 (2%) | none | 2/46 (4%) |
|
| |||
| • Escherichia hermannii | 1/86 (1%) | none | 1/46 (2%) |
|
| |||
| • Salmonella group B | 1/86 (1%) | none | 1/46 (2%) |
|
| |||
| • Ewingella americana | 1/86 (1%) | none | 1/46 (2%) |
|
| |||
| Non-Enterobacteriaceae group | N=160 | N=85 | N=75 |
|
| |||
| Number of isolates n/N (%) | Number of isolates n/N (%) | Number of isolates n/N (%) | |
|
| |||
| • Pseudomonas aeruginosa | 78/160 (49%) | 41/85 (48%) | 37/75 (49%) |
|
| |||
| • Haemophilus influenza | 30/160 (19%) | 15/85 (18%) | 15/75 (20%) |
|
| |||
| • Moraxella species | 16/160 (10%) | 8/85 (9%) | 8/75 (10%) |
|
| |||
| • Burkholderia species | 9/160 (6%) | 6/85 (7%) | 3/75 (4%) |
|
| |||
| • Ochrobactrum anthropi | 7/160 (4%) | 4/85 (5%) | 3/75 (4%) |
|
| |||
| • Bacteriodes species | 5/160 (3%) | 2/85 (2%) | 3/75 (4%) |
|
| |||
| • Neisseria mucosa | 6/160 (4%) | 5/85 (6%) | 1/75 (1%) |
|
| |||
| • Pseudomonas stutzeri | 3/160 (2%) | 2/85 (2%) | 1/75 (1%) |
|
| |||
| • Sphingomomas paucimobilis | 2/160 (1%) | 1/85 (1%) | 1/75 (1%) |
|
| |||
| • Capnocytophaga | 1/160 (<1%) | 1/85 (1%) | none |
|
| |||
| • Aggregatibacter actinomycetemcomitans | 1/160 (<1%) | none | 1/75 (1%) |
|
| |||
| • Branhamella catarrhalis | 1/160 (<1%) | none | 1/75 (1%) |
|
| |||
| • Rhizobium radiobacter | 1/160 (<1%) | none | 1/75 (1%) |
Time Period I – From December 1990 to December 1999 and Time Period II – January 2000 to December 2014
Figure 1.
(a) Antimicrobial susceptibility pattern among Enterobacteriaceae. (b) Antimicrobial susceptibility pattern among Non-Enterobacteriaceae.
Discussion
The rate of endophthalmitis caused by gram-negative bacteria is reported to be 26–42% in developing countries while it is 5.9% –12% in developed countries. The Endophthalmitis Vitrectomy Study (EVS) in 1996 reported 19/323 (5.9%) gram-negative isolates.3 In the EVS, 2/19 gram-negative isolates were reported to be resistant to both ceftazidime and amikacin.3 In a recent publication by the Antibiotic Resistance Monitoring in Ocular Microorganisms (ARMOR) Surveillance Study in 2015, there was no increase in overall ocular resistance during the 5-year study period (January 2009 to December 2013).4 The current study results also showed no increase in antimicrobial resistance among gram-negative bacteria during the 24-year study period as compared to a prior 9 year (January 1982 to December 1990) study from same University Referral Center.5 Specifically the cephalosporins in the current study did not show any increase in resistance among Enterobacteriaceae and Non-Enterobacteriaceae groups. The collective experience from these studies shows that antibiotic susceptibility pattern of gram negative bacteria from vitreous isolates has not changed.
Summary Statement.
Review of 24 years records of gram-negative bacteria isolated from a University Referral Center showed no significant change in the distribution of isolates and antimicrobial susceptibilities.
Acknowledgments
Funding Support - We acknowledge support from the National Institute of Health (NIH) Center Core Grant P30EY014801 (Bethesda, Maryland), Research to Prevent Blindness Unrestricted Grant (New York, New York), and the Department of Defense (DOD Grant #W81XWH-09-1-0675) (Washington, DC).
Footnotes
This work was presented as a poster at ARVO 2015, at Denver, Colorado. (Posterboard #: 4074-A0251, Abstract number – 2167322, on May 06, 2015)
Conflict of Interest/Disclosures: None. None of the authors have any proprietary interest.
References
- 1.Jindal A, Pathengay A, Khera M, et al. Combined ceftazidime and amikacin resistance among Gram-negative isolates in acute-onset postoperative endophthalmitis: prevalence, antimicrobial susceptibilities, and visual acuity outcome. J Ophthalmic Inflamm Infect. 2013;3(1):62. doi: 10.1186/1869-5760-3-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Altan T, Acar N, Kapran Z, et al. Acute-onset endophthalmitis after cataract surgery: success of initial therapy, visual outcomes, and related factors. Retina. 2009;29(5):606–612. doi: 10.1097/IAE.0b013e3181953a31. [DOI] [PubMed] [Google Scholar]
- 3.Han DP, Wisniewski SR, Wilson LA, et al. Spectrum and susceptibilities of microbiologic isolates in the Endophthalmitis Vitrectomy Study. Am J Ophthalmol. 1996;122(1):1–17. doi: 10.1016/s0002-9394(14)71959-2. [DOI] [PubMed] [Google Scholar]
- 4.Asbell PA, Sanfilippo CM, Pillar CM, et al. Antibiotic Resistance Among Ocular Pathogens in the United States: Five-Year Results From the Antibiotic Resistance Monitoring in Ocular Microorganisms (ARMOR) Surveillance Study. JAMA Ophthalmol. 2015;133(12):1445–1454. doi: 10.1001/jamaophthalmol.2015.3888. [DOI] [PubMed] [Google Scholar]
- 5.Irvine WD, Flynn HW, Jr, Miller D, Pflugfelder SC. Endophthalmitis caused by gram-negative organisms. Arch Ophthalmol. 1992;110(10):1450–1454. doi: 10.1001/archopht.1992.01080220112031. [DOI] [PubMed] [Google Scholar]