Abstract
Müllerianosis is an embryonic Müllerian disease, resulting in the formation of the benign diseases adenomyosis, endometriosis, endosalpingiosis, and endocervicosis. Endocervicosis primarily affects the bladder, and rarely the cervix. Cervical endocervicosis, which is also a pseudoneoplastic glandular lesion, could be misinterpreted as a premalignant or even a malignant lesion. Because the treatment of these diseases is very different, early clinical diagnosis is important. Unfortunately, however, this lesion is difficult to diagnose preoperatively using clinical and radiological information, and pathological confirmation is needed. Herein, we report a rare case of cervical endocervicosis that was difficult to diagnosis preoperatively.
Keywords: Adenoma malignum, Differential diagnosis, Endocervicosis, Müllerianosis, Pseudoneoplastic glandular lesion
Introduction
Müllerianosis is an embryonic Müllerian disease in which organoid structures are misplaced during organogenesis, resulting in the formation of four benign diseases: adenomyosis, endometriosis, endosalpingiosis, and endocervicosis [1]. Endocervicosis is the rarest of the four Müllerian lesions, and it primarily affects the bladder. However, this pseudoneoplastic lesion has also been documented in other locations [2].
Endocervicosis involving the cervix is a rarely described entity. It is characterized by its histopathologic features and is therefore diagnosed by a pathologist, not a clinician. Such lesions could be misinterpreted as premalignant or even malignant lesions [3]. To the best of our knowledge, no case of cervical endocervicosis has been previously reported in Korea. Five cases have been reported worldwide, and we here report the sixth case of this case very rare non-neoplastic Müllerian lesion in the cervix.
Case report
A 47-year-old woman presented with a 3- to 4-month history of a vaginal mass, which protruded when abdominal pressure was increased. She had recently experienced increased vaginal spotting and discharge. There was no abdominal pain or urinary symptoms. She had a previous medical history of primary infertility with uterine didelphys. Blood tests revealed no specific findings, and her CA 125 level was within the normal range of 25.7 U/mL. In addition, results of Papanicolaou smears of both cervixes were negative for intraepithelial lesions or malignancies.
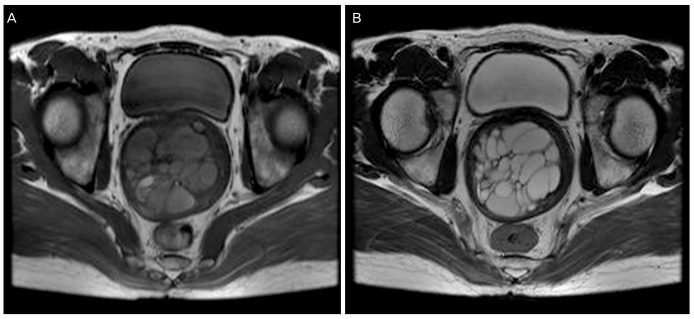
On the day of her presentation, a well-defined, multiseptated mass, 7.5×6.2 cm in size, was observed at the posterior wall of the cervix on transvaginal ultrasonography. Findings from the ultrasound raised the possibility of a cervical myoma. Magnetic resonance imaging (MRI) revealed a well-defined multilocular cystic mass, about 7.5 cm in size. The multicystic mass lesion with highsignal intensity was evident on both T1-weighted (T1W1) and T2-weighted (T2W1) imaging and did not invade the paracervical tissue (Fig. 1). Findings from MRI suggested that the differential diagnosis of the mass should include adenoma malignum and a pseudoneoplastic glandular lesion. The patient underwent removal of the cervical mass by transvaginal surgery. The results of a frozen biopsy indicated that the lesion was benign.
Fig. 1. (A) T1-weighted axial image of the pelvis showing a multiloculated cystic lesion not invading the cervical stroma with high-signal intensity. (B) T2-weighted axial image of the pelvis showing a multiloculated cystic lesion not invading the cervical stroma with high-signal intensity.
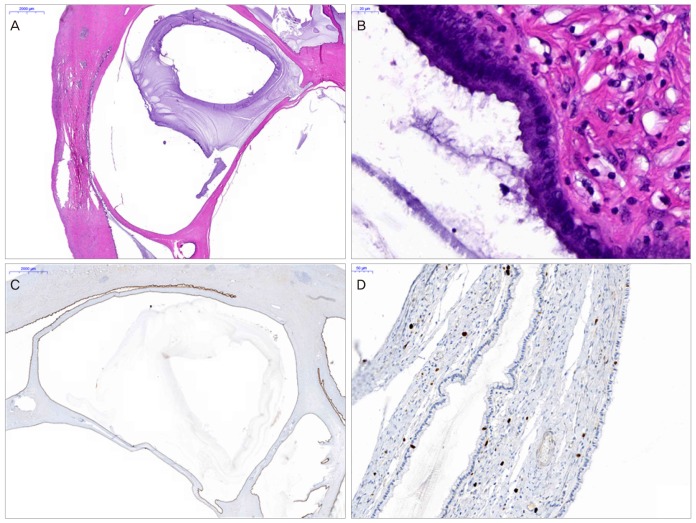
Grossly, the specimen was a multilocular cystic lesion filled with grayish mucinous fluid that occupied the posterior wall of the cervix and that measured about 8×7×6.5 cm, which is larger than previously reported cases; other cases did not exceed 3 cm in size. It connected the endocervix and extended through the anterior cervical wall. On histopathologic examination, variably sized mucous glands evocative of the endocervical gland were observed in the cervical mass. The glands were deeply seated in the cystic space. Additionally, cysts in the cervical mass were filled with mucin (Fig. 2A). The cystic wall was lined by a tall, single layer of mucinous columnar epithelium with basally oriented nuclei (Fig. 2B). The nuclei did not show nuclear pleomorphism or abnormal mitosis, which is commonly observed in malignant cells. Immunohistochemically, the cystic gland cells weakly expressed estrogen, progesterone receptor, and cytokeratin 7 (Fig. 2C). However, they were negative for carcinoembryonic antigen, MUC6, P53, and P16 and showed low cell proliferation, as evaluated by Ki 67 labeling (Fig. 2D). Pathologic and immunohistochemical results were similar to those in previous cases. The final pathologic diagnosis was endocervicosis of the uterine cervix. Twelve months after surgery, the patient is doing well and is asymptomatic and without complications.
Fig. 2. (A) The cervix shows several deep-seated cystic spaces. The cysts are filled with mucin (H&E, ×20). (B) The cystic wall is lined by single layer of mucinous columnar epithelium (H&E, ×800). (C) The lining cells of the cyst show diffuse cytokeratin 7 expression (immunohistochemistry for cytokeratin 7, ×20). (D) The cystic wall shows a low Ki 67 labeling index (immunohistochemistry for Ki 67, ×400).
Discussion
Endocervicosis is thought to originate from Müllerian lesions, and it shows endocervical type differentiation. According to its histogenesis, endocervicosis is the rarest of the Müllerian lesions and is thought to originate from the pelvic peritoneum or retroperitoneum [1]. Endocervicosis is one of the pseudoneoplastic glandular lesions and is characterized by an uneven arrangement of glands lined by a benign mucinous endocervical-type epithelium, often cystically dilated and occupying the cervical wall and extending to the paracervical tissue [2,4]. It has primarily been described in the urinary bladder [5] and rarely in the cervix [2], axillary lymph nodes [6], rectum [7], and mesosalpinx [8]. Interestingly, one report referred to its association with a mechanical etiology, like that seen in isthmocele, rather than that of Müllerianosis [2].
Clinical symptoms of cervical endocervicosis vary from asymptomatic, pelvic pain, and dysmenorrhea. It is a benign disease that does not require additional treatment after surgical resection [9]. However, in the initial diagnosis of pseudoneoplastic glandular lesions of the uterine cervix, benign diseases, like adenomyoma and endocervicosis, and premalignant or even malignant lesions, including adenoma malignum and carcinoma of the cervix, should also be considered [2,9,10]. The treatment for the above-mentioned diseases is very different. Unlike the treatment for benign diseases, that for premalignant or malignant diseases might require radical surgery and additional chemoradiation therapy. In addition, the preoperative diagnosis is important for determining the proper surgical treatment appropriate, which has a great influence on prognosis. However, accurate preoperative diagnostic tools for cervical endocervicosis are not established, and diagnosis is difficult because there are many similar pseudoneoplastic/neoplastic glandular lesions that require differential diagnosis.
For these reasons, although pseudoneoplastic glandular lesions of the cervix, like endocervicosis, require pathologic confirmation, preoperative clinical diagnosis is important, and imaging studies such as MRI may be helpful for determining the extent of the disease [11]. Endocervicosis usually does not invade deeply into the cervical stroma and does not contain solid-component enhancement on T2W1-MRI images. In contrast, a multicystic lesion that deeply invades the cervical stroma and contains solid-enhancement portions may indicate a malignant lesion, like carcinoma of the cervix, that usually shows high-signal intensity on T2W1 and post-contrast T1W1 images and low-signal intensity at the cervical stroma on T2 images [11,12]. In addition, morphologically and radiologically, endocervicosis can mimic adenoma malignum. Our case demonstrated a multicystic mass lesion with high-signal intensity on both T1W1 and T2W1 imaging that did not invade the paracervical tissue. These findings suggest that the differential diagnosis would include adenoma malignum and pseudoneoplastic glandular lesions, especially large Nabothian cysts. In the columnar epithelium of the Nabothian cyst, secretory mucus is secreted, which causes a chronic inflammation to form a retention cyst, which have many morphological similarities to endocervicosis. However, because the clinical symptoms alone are not distinguishable, imaging tests are also needed [13]. In short, it may be helpful to differentiate carcinoma of the cervix; there are no pathognomonic radiologic findings between adenoma malignum and endocervicosis [12]. A variety of diagnostic approaches, such as transvaginal power Doppler ultrasonography and transcervical sonography, can be considered, even though they have not yet found wide application. Despite the use of these contemporary diagnostic approaches, exploratory laparotomy and hysterectomy may still be required in case of unusually large and deep intracervical cysts, when malignancy cannot be excluded. In conclusion, if malignancy is not ruled out by considering the diagnostic dilemma, it is important to perform additional examinations carefully and to provide sufficient information to the patient. In other reports, differentiating endocervicosis from pseudoneoplastic glandular lesions and adenoma malignum was difficult with magnetic resonance images alone [14]. However, there are relatively few reports on the information that MRI can provide for diagnosing cervical lesions. Therefore, if malignancy cannot be ruled-out, although MRI is not the gold standard for diagnosis, it is valuable as a first tool for diagnosis.
MRI provides the detailed features described above and correlates them with pathologic findings, raising concern for adenoma malignum. In endocervicosis, the glands are mainly confined to the outer aspect of the cervix, whereas in adenoma malignum, the glands grow downward and originate from the mucosa. When endocervicosis involves the whole cervical wall, it may abut the normal endocervical gland, and it is the uniform cytologic features of the glands in endocervicosis that allow differentiation. Additionally, the glands in endocervicosis are cystic with irregular shapes and sizes and are filled with mucus [2,9]. Immunohistochemically, in contrast to those in adenoma malignum, the glands in endocervicosis express hormone receptors and cytokeratin 7, but they are negative for carcinoembryonic antigen and P53, and expression of Ki 67 is usually low [4,15]. The distinctive characteristics of cervical endocervicosis enable it to be discriminated from other benign glandular lesions of the cervix, such as large deep Nabothian cysts, papillary endocervicitis, diffuse laminar endocervical glandular hyperplasia, benign microglandular hyperplasia, and mesonephric remnants [2,9].
In summary, endocervicosis is a Müllerian disease and also pseudoneoplastic glandular lesion of the cervix. Since the treatment is very different between the two, it is important to distinguish between benign and premalignant/malignant disease. Herein, we reported a case of cervical endocervicosis, which is a rare cervical glandular lesion and also the rarest of the Müllerian diseases. This lesion is difficult to diagnose preoperatively with clinical and radiological findings only. MRI may be helpful in diagnosis, but ultimately, pathologic confirmation is needed.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Batt RE, Yeh J. Mullerianosis: four developmental (embryonic) mullerian diseases. Reprod Sci. 2013;20:1030–1037. doi: 10.1177/1933719112472736. [DOI] [PubMed] [Google Scholar]
- 2.Mobarki M, Karpathiou G, Forest F, Corsini T, Peoc’h M. Endocervicosis of the uterine cervix. Int J Gynecol Pathol. 2016;35:475–477. doi: 10.1097/PGP.0000000000000277. [DOI] [PubMed] [Google Scholar]
- 3.Cheah PL, Looi LM, Lee GE, Teoh KH, Mun KS, Nazarina AR. Unusual finding of endocervical-like mucinous epithelium in continuity with urothelium in endocervicosis of the urinary bladder. Diagn Pathol. 2011;6:56. doi: 10.1186/1746-1596-6-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCluggage WG, Price JH, Dobbs SP. Primary adenocarcinoma of the vagina arising in endocervicosis. Int J Gynecol Pathol. 2001;20:399–402. doi: 10.1097/00004347-200110000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Olivia Vella JE, Nair N, Ferryman SR, Athavale R, Latthe P, Hirschowitz L. Mullerianosis of the urinary bladder. Int J Surg Pathol. 2011;19:548–551. doi: 10.1177/1066896911409578. [DOI] [PubMed] [Google Scholar]
- 6.Mukonoweshuro P, McCluggage WG. Endocervicosis involving axillary lymph nodes: first case report. Int J Gynecol Pathol. 2014;33:620–623. doi: 10.1097/PGP.0000000000000089. [DOI] [PubMed] [Google Scholar]
- 7.Slotta JE, Schaefer TJ, Walter B, Bohle RM, Schilling MK, Plusczyk T. Endocervicosis of the rectum. Int J Colorectal Dis. 2011;26:683–684. doi: 10.1007/s00384-010-1044-0. [DOI] [PubMed] [Google Scholar]
- 8.Lim S, Kim JY, Park K, Kim BR, Ahn G. Mullerianosis of the mesosalpinx: a case report. Int J Gynecol Pathol. 2003;22:209–212. doi: 10.1097/00004347-200304000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Young RH, Clement PB. Endocervicosis involving the uterine cervix: a report of four cases of a benign process that may be confused with deeply invasive endocervical adenocarcinoma. Int J Gynecol Pathol. 2000;19:322–328. doi: 10.1097/00004347-200010000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Nucci MR. Pseudoneoplastic glandular lesions of the uterine cervix: a selective review. Int J Gynecol Pathol. 2014;33:330–338. doi: 10.1097/PGP.0000000000000139. [DOI] [PubMed] [Google Scholar]
- 11.Eskridge MR, Rovner ES, Payne KD, Workman RB, Curry NS. MRI of endocervicosis: an unusual cause of clustered periurethral cystic masses involving the bladder. AJR Am J Roentgenol. 2007;188:W147–W149. doi: 10.2214/AJR.05.1734. [DOI] [PubMed] [Google Scholar]
- 12.Castan Senar A, Pano B, Saco A, Nicolau C. Magnetic resonance imaging of adenoma malignum of the uterine cervix with pathologic correlation: a case report. Radiol Case Rep. 2016;11:323–327. doi: 10.1016/j.radcr.2016.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park SB, Lee JH, Lee YH, Song MJ, Choi HJ. Multilocular cystic lesions in the uterine cervix: broad spectrum of imaging features and pathologic correlation. AJR Am J Roentgenol. 2010;195:517–523. doi: 10.2214/AJR.09.3619. [DOI] [PubMed] [Google Scholar]
- 14.Kulkarni M, Hastak M, Chatterjee P. Adenoma malignum of the cervix: MR imaging appearance. Research. 2014;1:635. [Google Scholar]
- 15.Gong L, Zhang WD, Liu XY, Han XJ, Yao L, Zhu SJ, et al. Clonal status and clinicopathological observation of cervical minimal deviation adenocarcinoma. Diagn Pathol. 2010;5:25. doi: 10.1186/1746-1596-5-25. [DOI] [PMC free article] [PubMed] [Google Scholar]