Abstract
Late-life depression is associated with disabled functioning and a poor quality of life (QOL). The aim of this cross-sectional study was to find out whether the attendance of a day care centre (DC) was associated with QOL in community-dwelling older adults suffering from a depressive disorder without dementia. The study enrolled 149 depressed older adults aged 70 or older, who consecutively underwent a comprehensive geriatric assessment from April to July 2008 at the Geriatric Medicine Unit of the Fondazione Ospedale Maggiore Policlinico in Milan, Italy. QOL was evaluated by means of the European Quality of Life Visual Analogue Scale (EuroQol VAS). DC attendance was quantified as number of days of attendance per week in the past month. Participants attending a DC at least once a week (n = 17) had a higher mean EuroQol VAS score than non-attendants (n = 132) (mean ± SD 58.8 ± 19 vs. 45.3 ± 22.5; P = 0.019). In multiple linear regression analysis a higher weekly attendance of DCs was related to a better quality of life according to the EuroQol VAS score (unstandardized coefficient 3.048, 95% CI 0.063–6.033, P = 0.045) after correction for age, sex, balance and gait abilities, comorbidity, pharmacotherapy, living alone, and severity of depression. Therefore, in older outpatients suffering from a depressive disorder without dementia the attendance of a DC was an independent correlate of the QOL. A randomized controlled longitudinal study will be necessary to determine whether attending a DC is really effective on the QOL in the management of late-life depression.
Keywords: Day care centres, Depression, Older outpatients, Quality of life, Social participation
Introduction
The recent Berlin declaration on the quality of life (QOL) for older adults underlined the need for studies investigating ‘what type of intervention is optimal at what time of the life span, and how such interventions can be implemented’ in order to improve QOL in real-life contexts (Fernandez-Ballesteros et al. 2009). Late-life depression represents a leading cause of a poor QOL and is associated with difficulty in physical and social functioning (Fauth et al. 2008; Unutzer 2007, Braam et al. 2004) as well as with increased morbidity and mortality from suicide and other causes (Unutzer 2007). Yet it often goes unrecognized or untreated in people living in the community (Ballabio et al. 2008; Klap et al. 2003).
A close relationship between social participation and depressive disorders has been recently emphasized. In community-dwelling older adults, a greater social activity was associated with a lower risk of depression and was also the main independent predictor of improvement of depressive symptoms in subjects with depression at baseline (Isaac et al. 2009).
As far as the correlation between social participation and QOL is concerned, there is evidence supporting the role of social factors in improving the QOL both in adults suffering from depressive disorders (Sung and Yeh 2007) and in older adults (de Belvis et al. 2008; Berg et al. 2006; Gabriel and Bowling 2004; Ho et al. 2003). However, it must be stressed that there are important differences in the determinants of QOL between adults and older people, with health and functional ability having a much greater importance among the latter (Bowling 2008; Walker 2005). Therefore, in order to improve the QOL in older adults suffering from depressive disorders, health and functional abilities should be promoted alongside social participation. Combined health and social programmes such as those provided by day care centres (DCs) for older people might be useful to this purpose.
DCs represent day care facilities which provide vulnerable older adults living in the community with assistance in the activities of daily living, social support, physical exercise and occupational therapy (Reilly et al. 2006). DCs address a wide range of needs including the prevention of physical and functional deterioration and the promotion of companionship and social stimulation. Actually, the majority of DC attendants are older people with cognitive impairment, as shown by a recent survey conducted in the North West of England, in which 72% of DC attendees had been diagnosed with dementia (Reilly et al. 2006). It is therefore not surprising that in assessing the effectiveness of DC services, the outcomes taken into account mainly refer to older adults with dementia and their caregivers: an improvement in the mood of the elders, a reduction or a delay in their admission to hospital and to long-term facilities, a lesser caregiver distress (Engedal 1989; Gitlin et al. 2006; Smits et al. 2007). An Italian study enrolling older subjects with dementia has recently demonstrated that a two-month period of DC assistance turned out to be effective in reducing behavioral and psychological symptoms of participants and in alleviating caregivers’ burden (Mossello et al. 2008).
A recent study performed on a small sample of old impoverished women showed that activities of adult day care centres played an important role in alleviating depression (Valadez et al. 2006). We can thus suppose that DC services might be effective in improving the QOL even in older people with a depressive disorder. To the authors’ knowledge no study has yet investigated either the effect of DC attendance on the QOL of community-dwelling older adults suffering from a depressive disorder or the possible correlation between DC attendance and QOL in this specific population.
The aim of this cross-sectional study was to find out whether the attendance of a DC was associated with QOL in community-dwelling older adults suffering from a depressive disorder without dementia.
Methods
Participants and setting
We considered 623 older adults living in the community who were consecutively evaluated from April to July 2008 at the outpatient Geriatric Medicine Unit of the Fondazione Cà Granda Ospedale Maggiore Policlinico, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) in Milan, Italy. From this group of patients, we selected those people aged at least 70 who were diagnosed with a depressive disorder according to the Diagnostic and Statistical Manual of Mental Disorders fourth edition text revision (DSM-IV-TR) criteria (American Psychiatric Association 2000). The exclusion criteria were evidence of a personality disorder, psychosis, dementia, and severe sensory impairment. Five of the 154 eligible patients were not willing to take part in our study. The study therefore enrolled a total of 149 participants. Written informed consent was obtained from all participants.
Design and measurement instruments
Cross-sectional study comparing subjects attending a DC (the “attendants” group) with those not attending a DC (the “non-attendants” group). We decided to quantify DC attendance on a weekly basis, in line with a recent study (Reilly et al. 2006), i.e., as the number of days of attendance per week in the past month, with once a week being the lowest possible attendance in our country. This seems to be a reasonable choice in our specific setting: the older persons in Milan generally attend DCs on specific days of the week which usually do not change over time.
The primary outcome measure was QOL as described by means of the European Quality of Life Visual Analogue Scale (EuroQol VAS) (The Euroqol Group 1990).
The correlation between QOL and DC attendance was investigated not only by taking into account acknowledged determinants of the QOL such as functional status, comorbidity and severity of depression (Walker 2005) but also the possible influence of the background characteristics of patients.
All subjects underwent a comprehensive geriatric evaluation: functional status was assessed by means of the scales for the Activities of Daily Living (ADL) (Katz et al. 1970) and the Instrumental Activities of Daily Living (IADL) (Lawton and Brody 1969), balance and gait abilities by means of the Performance-Oriented Mobility Assessment (POMA) (Tinetti 1986), cognitive status by means of the Mini Mental State Examination (MMSE) (Folstein et al. 1975), emotional status by means of the 30-item Geriatric Depression Scale (GDS) (Yesavage et al. 1983), morbidity by means of the Cumulative Illness Rating Scales (CIRS-m and CIRS-s) (Parmelee et al. 1995).
In the assessment of comorbidity, alongside the CIRS scores, we specifically considered a history of those diseases which have been shown to have an impact on the QOL such as lung disease, heart disease, eye disease and arthritis (Blane et al. 2008; Strandberg et al. 2008; Yu et al. 2008; Lane and Lip 2009, Good 2008; Westin et al. 2005; Lukkarinen 1998; Newman 2008; Centers for Disease Control and Prevention 2000).
Besides the attendance of a DC, the social characteristics taken into account were living alone and the number of relatives paying a visit to the older adult at least once a week in the past month.
Intervention
Regular DCs for vulnerable older adults provide them with a combined intervention program which involves a multidisciplinary team of health professionals: a doctor specialized in the care of the older adults, a trained nurse, nurse aides, a physiotherapist, an occupational therapist, a music therapist, a dietician. The intervention program is tailored to the clinical and functional needs of each single individual and is not exclusively designed for people with a specific psychogeriatric syndrome. People suffering from moderate to severe dementia as well as the older persons completely dependent in ADLs are not admitted to regular DCs. The patients themselves decide how often in a week they wish to attend the DC. Such multidisciplinary intervention serves a number of purposes: it helps the older adults with daily activities, it stimulates residual functional abilities, promotes functional improvement and social participation.
Statistical analysis
In order to reject the null-hypothesis that the EuroQol VAS score was similar in the participants attending a DC at least once a week and in those not attending a DC, comparisons between the “attendants” and the “non-attendants” groups were made by using the Student t test for metric variables with a normal distribution, and the Pearson chi-squared test for nominal variables. A two-sided P value <0.05 was taken to indicate statistical significance. Multiple linear regression analysis was performed taking the EuroQol VAS score as the dependent variable and including weekly attendance of a DC among the covariates.
With regard to the sample size, since there are no data on the prevalence of DC attendance among community-dwelling depressed older adults without dementia, we based our statistical analysis on the 10% prevalence we found in our outpatient population (data not published). Thus a sample of 150 cases was considered to have an over-80% statistical power to detect a 33% relative difference in the EuroQol VAS score between “attendants” and “non-attendants” at a 5% significance level, assuming a mean EuroQol VAS score slightly lower than 50 out of 100 in participants not attending a DC.
Results
In our sample of 149 subjects (110 women and 39 men) the mean age was 82 (range 71–99). Sixty-three participant were living alone (42%). A major depressive disorder was diagnosed in 7 patients (5%) and the remaining 142 patients (95%) were diagnosed with minor depression or a dysthymic disorder according to the DSM IV criteria (American Psychiatric Association 2000). Apart from depression, participants were on average suffering from more than 4 chronic diseases according to CIRS-m scores.
On the basis of DC attendance (at least once a week vs. no attendance) 17 participants (11%) were included in the “attendants” group while 132 (89%) were included in the “non-attendants” group. The former group attended a total of 7 different DCs, all of which were regular day care centres providing full time services (i.e., from morning to late afternoon) for vulnerable older adults, including subjects with mild dementia. None of the subjects in the “non-attendants” group had ever attended a DC.
Table 1 shows the characteristics of the older participants belonging to the two groups. A higher mean EuroQol VAS score was found in the “attendants” group than in the “non-attendants” group (mean ± SD 58.8 ± 19 vs. 45.3 ± 22.5; P = 0.019). Moreover, in subjects attending DCs there was a higher prevalence of men and a lower consumption of drugs than in subjects not attending DCs. It is worth noting that the two groups were similar in terms of age, functional and emotional status, comorbidity and social conditions such as living alone and number of relatives paying a visit to the older participant at least once a week (Table 1).
Table 1.
Characteristics of “attendants” compared with “non-attendants”
| Variables | Attendants n = 17 |
Non-attendants n = 132 |
P value |
|---|---|---|---|
| Mean (SD) or % (n) | Mean (SD) or % (n) | ||
| Physical variables | |||
| Age (years) | 82 (6.9) | 82.1 (5.7) | 0.931 |
| Sex: female | 53 (9) | 77 (101) | 0.037* |
| Functional status | |||
| ADL scorea | 4.5 (1.3) | 4.5 (1.4) | 0.969 |
| IADL scoreb | 4.4 (2.7) | 4.4 (2.6) | 0.925 |
| POMA scorec | 16.2 (6.8) | 14.9 (6.8) | 0.432 |
| MMSE scored | 25.7 (2.2) | 26.9 (2.5) | 0.072 |
| GDS scoree | 14.4 (4.4) | 16.2 (5.1) | 0.147 |
| Clinical assessment | |||
| CIRS-m scoref | 4 (1.7) | 4.7 (1.8) | 0.156 |
| CIRS-s scoreg | 1.7 (0.3) | 1.8 (0.3) | 0.170 |
| Major depression | 6 (1) | 5 (6) | 0.683 |
| Heart disease | 77 (13) | 86 (113) | 0.326 |
| Lung disease | 24 (4) | 31 (41) | 0.524 |
| Eye disease | 47 (8) | 57 (75) | 0.446 |
| Arthritis | 65 (11) | 82 (108) | 0.098 |
| Number of drugs taken | 4.5 (2) | 6.3 (3.3) | 0.027* |
| Hypnotics and anxiolytics | 12 (2) | 25 (33) | 0.226 |
| Antidepressants | 29 (5) | 39 (51) | 0.460 |
| Social variables | |||
| Living alone | 47 (8) | 42 (55) | 0.672 |
| Relationships with family kins (n)h | 1.8 (1.7) | 1.8 (1.3) | 0.995 |
| Quality of life assessment | |||
| EuroQol VAS scorei | 58.8 (19) | 45.3 (22.5) | 0.019* |
Values in italics represent % (n) not mean (SD)
DC day care centre
* P < 0.05
aActivities of Daily Living. Score range 0–6. Higher scores indicate better functional performance
bInstrumental Activities of Daily Living. Score range 0–5 for men and 0–8 for women. Higher scores indicate better functional performance
cPerformance-Oriented Mobility Assessment. Score range 0–28. Lower scores indicate worse balance and gait abilities as well as a greater risk of falling
dMini Mental State Examination. Score range 0–30. Higher scores indicate better cognitive function. Scores are corrected for age and education
eThirty Item—Geriatric Depression Scale. Score range 0–30. Higher scores indicate worse depressive status
fCumulative Illness Rating Scale Morbidity. Scores 0–13. Higher scores indicate higher morbidity
gCumulative Illness Rating Scale Severity. Scores 1–5. Higher scores indicate more severe multiple pathology
hNumber of relatives paying a visit to the participant at least once a week
iEuropean quality of life visual analogue scale. Score range 0–100. Higher scores indicate better quality of life
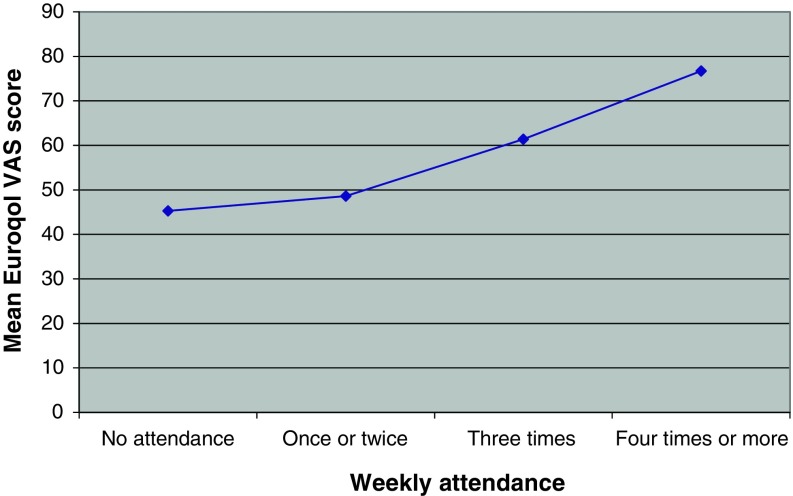
The median attendance of DCs was 3 days per week. As shown in Table 2, DCs were attended once or twice a week by seven participants, thrice a week by seven participants, and four or more times a week by three participants. Patients with a higher weekly attendance of DCs had a better QOL according to EuroQol VAS scores (Fig. 1) as well as lesser difficulties in gait and balance as assessed by means of the POMA scores (Table 2).
Table 2.
Main characteristics of the 17 participants attending a day care centre according to weekly days of attendance
| Variables | Once or twice n = 7 |
Thrice n = 7 |
Four times or more n = 3 |
|---|---|---|---|
| Mean (SD) or % (n) | Mean (SD) or % (n) | Mean (SD) or % (n) | |
| Age (years) | 84.4 (8.3) | 78.4 (5.4) | 84.7 (3.5) |
| Sex: female | 43 (3) | 71 (5) | 33 (1) |
| ADL scorea | 3.7 (1.4) | 5.1 (1.1) | 4.7 (0.6) |
| POMA scoreb | 11.9 (6.5) | 18.7 (6) | 20.7 (4.2) |
| MMSE scorec | 25.2 (2.6) | 26.7 (1.8) | 24.7 (1.6) |
| GDS scored | 15.4 (5.5) | 13.7 (3.8) | 13.3 (3.2) |
| CIRS-m scoree | 3.3 (1.4) | 5 (1.6) | 3.3 (2.1) |
| CIRS-s scoref | 1.6 (0.2) | 1.8 (0.2) | 1.5 (0.4) |
| Number of drugs taken | 4.3 (1.7) | 5 (2.4) | 3.7 (2.1) |
| EuroQol VAS scoreg | 48.6 (13.5) | 61.4 (21.2) | 76.7 (11.5) |
Values in italics represent % (n) not mean (SD)
aActivities of Daily Living. Score range 0–6. Higher scores indicate better functional performance
bPerformance-Oriented Mobility Assessment. Score range 0–28. Lower scores indicate worse balance and gait abilities as well as a greater risk of falling
cMini Mental State Examination. Score range 0–30. Higher scores indicate better cognitive function. Scores are corrected for age and education
dThirty Item—Geriatric Depression Scale. Score range 0–30. Higher scores indicate worse depressive status
eCumulative Illness Rating Scale morbidity. Scores 0–13. Higher scores indicate higher morbidity
fCumulative Illness Rating Scale severity. Scores 1–5. Higher scores indicate more severe multiple pathology
gEuropean quality of life visual analogue scale. Score range 0–10. Higher scores indicate better quality of life
Fig. 1.
Weekly attendance of a day care centre and quality of life in older outpatients with depression
In multiple linear regression analysis (Table 3), a higher weekly attendance of DCs was found to be related to a better QOL according to the EuroQol VAS score (unstandardized coefficient 3.048, 95% CI 0.063–6.033, P = 0.045) after correction for age, sex, balance and gait abilities, comorbidity, pharmacotherapy, living alone, and severity of depression.
Table 3.
Correlates of the quality of life in multiple linear regression analysis
| Variables | Unstandardized coefficient (95% CI) | Standardized coefficient | t | P value |
|---|---|---|---|---|
| Age (years) | 3.28 E-02 (−0.553 to 0.618) | 0.008 | 0.111 | 0.912 |
| Sex | −3.420 (−10.982 to 4.143) | −0.067 | −0.894 | 0.373 |
| POMA score | 0.735 (0.202–1.267) | 0.221 | 2.726 | 0.007* |
| MMSE score | 0.229 (−1.069 to 1.527) | 0.025 | 0.349 | 0.728 |
| GDS score | −1.863 (−2.528 to −1.199) | −0.415 | −5.543 | <0.001* |
| CIRS-m score | 3.283 (−1.829 to 8.396) | 0.266 | 1.270 | 0.206 |
| CIRS-s score | −25.908 (−60.418 to 8.601) | −0.317 | −1.484 | 0.140 |
| Number of drugs taken | −0.514 (−1.668 to 0.640) | −0.074 | −0.880 | 0.380 |
| Living alone | 3.118 (−3.368 to 9.604) | 0.069 | 0.950 | 0.344 |
| Attendance of a DC (days per week) | 3.048 (0.063–6.033) | 0.140 | 2.019 | 0.045* |
Adjusted R 2 = 0.344
DC day care centre
* P < 0.05
Discussion
This cross-sectional study showed a correlation between a higher weekly attendance of DCs and a better QOL among community-dwelling older adults suffering from a depressive disorder without dementia. To our knowledge, this is the first study highlighting such kind of association, and it is interesting to note that the correlation was found to be independent of other well-acknowledged determinants of the QOL such as functional status, including balance and gait abilities, severity of depression and comorbidity (Walker 2005).
As far as QOL was concerned, measuring it in absolute terms seems to be quite a difficult task due to its multidimensional and complex nature (Walker 2005). We chose to use the EuroQol VAS because it is quick and easy to administer, and can provide a reliable measure of the subjective aspects of the QOL. Moreover, we have to underline that the comprehensive geriatric assessment we performed also considered objective determinants of the QOL, such as the clinical, functional and emotional status, mobility and cognitive function, which were included in the statistical analyses.
Only about 11% of our sample of depressed older adults were attending a DC. This seems to be a low rate of attendance, yet if we compare it with the rate of attendance of DCs (both regular and specific DCs) in all community-dwelling subjects with dementia (28%) (Georges et al. 2008), we believe we have found results of a reasonable magnitude taking into account that: (i) dementia and depression have a similar prevalence in the community-dwelling older population (Ferri et al. 2005; Unutzer 2007), (ii) older people with dementia are the majority of DC attendees (Reilly et al. 2006).
Since the participants of our study attended regular DCs for vulnerable older adults, which were not designed for people with a specific psychogeriatric syndrome, our study can provide no information on particular models of day-care services associated with QOL in the elders with depression. However, the fact that none of the subjects belonging to the “non-attendants” group had ever attended a DC seems to suggest that older depressed people attending a regular DC do not often stop for instance because of reasons of dissatisfaction with the regular programme.
It must be noted that the cross-sectional nature of the study does not allow us to make any statement on the effectiveness of DC interventions on the QOL, since reverse causality might affect the interpretation of the results. In fact, we cannot exclude that subjects attending DCs may be a selected group who were “better off” from the very start, i.e., people who themselves decided to attend a DC to improve their social and physical functioning and people who were encouraged by their caregivers and/or GPs to attend a DC because likely to benefit from multidisciplinary interventions. In short, such subjects could have had a better QOL before starting the attendance of DCs.
Moreover, even in the hypothesis that a higher weekly attendance of DCs is actually able to improve the QOL in depressed older adults, it must be emphasized that in most developed countries, in Europe as well as in the US, the availability of DCs falls far short of what is necessary to serve the needs of the population suffering from debilitating illnesses (National Study of Adult Day Services 2002; Siebenaler et al. 2005; Tester 2001). For example, according to a recent European survey concerning health and social services for community-dwelling people with Alzheimer’s disease, day care services were available only for 42% of the patients suffering from dementia (Georges et al. 2008).
In conclusion, in older outpatients suffering from a depressive disorder without dementia the attendance of a DC was an independent correlate of the QOL. A longitudinal randomized controlled study will be necessary to determine whether attending a DC is really effective on the QOL even in an older population of this kind and to decide whether increasing the provision of DC services could actually be a valuable measure in the management of late-life depression.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders, text revision. 4. Washington: American Psychiatric Association Press; 2000. [Google Scholar]
- Ballabio C, Bergamaschini L, Mauri S, Baroni E, Ferretti M, Bilotta C, Vergani C. A comprehensive evaluation of elderly people discharged from an emergency department. Intern Emerg Med. 2008;3:245–249. doi: 10.1007/s11739-008-0151-1. [DOI] [PubMed] [Google Scholar]
- Berg A-I, Hassing L-B, McClearn G-E, Johansson B. What matters for life satisfaction in the oldest-old? Aging Mental Health. 2006;10:257–264. doi: 10.1080/13607860500409435. [DOI] [PubMed] [Google Scholar]
- Blane D, Netuveli G, Montgomery S-M. Quality of life, health and physiological status and change at older ages. Soc Sci Med. 2008;66:1579–1587. doi: 10.1016/j.socscimed.2007.12.021. [DOI] [PubMed] [Google Scholar]
- Bowling A. Enhancing later life: how older people perceive active ageing? Aging and Mental Health. 2008;12:293–301. doi: 10.1080/13607860802120979. [DOI] [PubMed] [Google Scholar]
- Braam A-W, Delespaul P, Beekman A-T-F, Deeg D-J-H, Peres K, Dewey M, et al. National context of healthcare, economy and religion, and the association between disability and depressive symptoms in older Europeans: results from the EURODEP concerted action. Eur J Aging. 2004;1:26–36. doi: 10.1007/s10433-004-0013-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Health-related quality of life among adults with arthritis. Behavioural risk factor surveillance system, 11 States, 1996–1998. Morb Mortal Wkly Rep. 2000;49:366–369. [PubMed] [Google Scholar]
- de Belvis A-G, Avolio M, Sicuro L, Rosano A, Latini E, Damiani G, et al. Social relationships and HRQOL: a cross-sectional survey among older Italian adults. BMC Public Health. 2008;8:348. doi: 10.1186/1471-2458-8-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engedal K. Day care for demented patients in general nursing homes: effect on admissions to institutions and mental capacity. Scand J Prim Health Care. 1989;7:161–166. doi: 10.3109/02813438909087234. [DOI] [PubMed] [Google Scholar]
- Fauth E-B, Zarit S-H, Malmberg B. Mediating relationships within the disablement process model: a cross-sectional study of the oldest-old. Eur J Aging. 2008;5:161–179. doi: 10.1007/s10433-008-0092-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez-Ballesteros R, Frensch P-A, Hofer S-M, Park D-C, Pinquart M, Silbereisen R-K, et al. Berlin declaration on the quality of life for older adults: closing the gap between scientific knowledge and intervention. Eur J Aging. 2009;6:49–50. doi: 10.1007/s10433-009-0107-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferri C-P, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, Hall K, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366:2112–2117. doi: 10.1016/S0140-6736(05)67889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein M-F, Folstein S-E, McHugh P-R. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gabriel Z, Bowling A. Quality of life from the perspectives of older people. Ageing Soc. 2004;24:675–692. doi: 10.1017/S0144686X03001582. [DOI] [Google Scholar]
- Georges J, Jansen S, Jackson J, Meyrieux A, Sadowska A, Selmes M. Alzheimer’s disease in real life—the dementia carer’s survey. Int J Geriatr Psychiatry. 2008;23:546–551. doi: 10.1002/gps.1984. [DOI] [PubMed] [Google Scholar]
- Gitlin L-N, Reever K, Dennis M-P, Mathieu E, Hauck W. Enhancing quality of life of families who use adult day services: short- and long-term effects of the adult day services program. Gerontologist. 2006;46:630–639. doi: 10.1093/geront/46.5.630. [DOI] [PubMed] [Google Scholar]
- Good GA. Life satisfaction and quality of life of older New Zealanders with and without impaired vision: a descriptive, comparative study. Eur J Aging. 2008;5:223–231. doi: 10.1007/s10433-008-0087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho H-K, Matsubayashi K, Wada T, Kimura M, Yano S, Otsuka K, et al. What determines the life satisfaction of the elderly? Comparative study of residential care home and community in Japan. Geriatr Gerontol Int. 2003;3:79–85. doi: 10.1046/j.1444-1586.2003.00067.x. [DOI] [Google Scholar]
- Isaac V, Stewart R, Artero S, Ancelin M-L, Ritchie K. Social activity and improvement in depressive symptoms in older people: a prospective community cohort study. Am J Geriatr Psychiatry. 2009;17:688–696. doi: 10.1097/JGP.0b013e3181a88441. [DOI] [PubMed] [Google Scholar]
- Katz S, Downs T-D, Cash H-R, Grotz R-C. Progress in development in the index of ADL. Gerontologist. 1970;10:20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- Klap R, Unroe K-T, Unutzer J. Caring for mental illness in the United States: a focus on older adults. Am J Geriatr Psychiatry. 2003;11:517–524. [PubMed] [Google Scholar]
- Lane D-A, Lip G-Y-H. Quality of life in older people with atrial fibrillation. Journal of Interventional Cardiac Electrophysiology. 2009;25:37–42. doi: 10.1007/s10840-008-9318-y. [DOI] [PubMed] [Google Scholar]
- Lawton M-P, Brody E-M. Assessment of older people; self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- Lukkarinen H. Quality of life in coronary artery disease. Nurs Res. 1998;47:337–343. doi: 10.1097/00006199-199811000-00007. [DOI] [PubMed] [Google Scholar]
- Mossello E, Caleri V, Razzi E, Di Bari M, Cantini C, Tonon E, et al. Day care for older dementia patients: favorable effects on behavioural and psychological symptoms and caregiver stress. Int J Geriatr Psychiatry. 2008;23:1066–1072. doi: 10.1002/gps.2034. [DOI] [PubMed] [Google Scholar]
- National Study of Adult Day Services, 2001–2002 (2002) Partners in caregiving: the adult day services program. Wake Forest University School of Medicine, Winston-Salem. http://www.rwjf.org/pr/product.jsp?id=20735. Accessed on 7 Aug 2009
- Newman B-Y. Nursing home optometry: improving the quality of life. Optometry. 2008;79:360–361. doi: 10.1016/j.optm.2008.05.001. [DOI] [PubMed] [Google Scholar]
- Parmelee P-A, Thuras P-D, Katz I-R, Lawton M-P. Validation of the cumulative illness rating scale in a geriatric residential population. J Am Geriatr Soc. 1995;43:130–137. doi: 10.1111/j.1532-5415.1995.tb06377.x. [DOI] [PubMed] [Google Scholar]
- Reilly S, Venables D, Hughes J, Challis D, Abendstern M. Standards of care in day hospitals and day centres: a comparison of services for older people with dementia. Int J Geriatr Psychiatry. 2006;21:460–468. doi: 10.1002/gps.1495. [DOI] [PubMed] [Google Scholar]
- Siebenaler K, O’Keeffe J, O’Keeffe C, Brown D, Koetse B (2005) Regulatory review of adult day services: final report. U.S. Department of Heath and Human Services. http://aspe.hhs.gov/daltcp/reports/adultday.htm#note7. Accessed on 7 Aug 2009
- Smits C-H-M, de Lange J, Droes R-M, Meiland F, Vernooij-Dassen M, Pot A-M. Effects of combined intervention programmes for people with dementia living at home and their caregivers: a systematic review. Int J Geriatr Psychiatry. 2007;22:1181–1193. doi: 10.1002/gps.1805. [DOI] [PubMed] [Google Scholar]
- Strandberg A-I, Strandberg T-E, Pitkala K, Salomaa V-V, Tilvis R-S, Miettinen T-A. The effect of smoking in midlife on health-related quality of life in old age: a 26-year prospective study. Arch Intern Med. 2008;168:1968–1974. doi: 10.1001/archinte.168.18.1968. [DOI] [PubMed] [Google Scholar]
- Sung S-C, Yeh M-Y. Factors related to quality of life in depressive outpatients in Taiwan. Psychiatry Clin Neurosci. 2007;61:610–615. doi: 10.1111/j.1440-1819.2007.01726.x. [DOI] [PubMed] [Google Scholar]
- Tester S. Day services for older people. In: Clark C-L, editor. Adult day services and social inclusion: better days. London: Jessica Kingsley Publishers; 2001. pp. 19–45. [Google Scholar]
- The Euroqol Group EuroQol: a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- Tinetti M-E. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34:119–126. doi: 10.1111/j.1532-5415.1986.tb05480.x. [DOI] [PubMed] [Google Scholar]
- Unutzer J. Late-life depression. NEJM. 2007;357:2269–2276. doi: 10.1056/NEJMcp073754. [DOI] [PubMed] [Google Scholar]
- Valadez A-A, Lumadue C, Gutierrez B, de Vries-Kell S. Las comadres and adult day care centers: the perceived impact of socialization on mental wellness. J Aging Stud. 2006;20:39–53. doi: 10.1016/j.jaging.2005.02.003. [DOI] [Google Scholar]
- Walker A. A European perspective on quality of life in old age. Eur J Aging. 2005;2:2–12. doi: 10.1007/s10433-005-0500-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westin L, Nilstun T, Carlsson R, Erhardt L. Patients with ischemic heart disease: quality of life predicts long-term mortality. Scand Cardiovasc J. 2005;39:50–54. doi: 10.1080/14017430410003903. [DOI] [PubMed] [Google Scholar]
- Yesavage J-A, Brink T-L, Rose T-L, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1983;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- Yu D-S, Lee D-T, Kwong A-N, Thompson D-R, Woo J. Living with chronic heart failure: a review of qualitative studies of older people. J Adv Nurs. 2008;61:474–483. doi: 10.1111/j.1365-2648.2007.04553.x. [DOI] [PubMed] [Google Scholar]