Abstract
This study investigates life satisfaction in relation to impending death among the oldest-old using overall disease load, self-rated health, and personality as interacting covariates of level and change. We used data from a sample of 370 healthy individuals who completed the Life Satisfaction Index-Z at four measurement occasions during a 6-year period in the Swedish OCTO-Twin study of individuals aged 80 and older. Growth curve analyses showed a linear decrease in life satisfaction as individuals approached death. The decrease was not related to level or change in self-rated health and disease load. High disease load was, however, related to lower levels of life satisfaction, but, this association was moderated by locus of control, such that those with high disease load and high locus of control did not show lower life satisfaction. Poor self-rated health was also associated with lower life satisfaction, but, this association was moderated by neuroticism, such that those with poor-rated health and low neuroticism did not show lower live satisfaction. Personality factors such as locus of control and neuroticism can influence the association between health and life satisfaction. The findings suggest further investigations of the role of personality characteristics in late life satisfaction and whether interventions aimed to increase personal control can improve life satisfaction in old age.
The notion of lifelong stability of life satisfaction produced by a set-point equilibrium mechanism has been questioned in recent longitudinal studies of life satisfaction in the oldest-old. In a previous study we found a linear and largely homogenous decrease in life satisfaction across four measurement occasions during a 6-year period in individuals aged 80–98 (Berg et al. 2009). Our finding confirms the few longitudinal studies of life satisfaction changes in the oldest-old (Baird et al. 2010; Mroczek and Spiro 2005).
Subjective well-being includes an affective component of negative and positive affect, and a cognitive evaluation component of life satisfaction, often defined as “the way individuals cognitively evaluate their lives” (Diener 1984). Studies of the mechanisms of life satisfaction evaluations may be categorized into two diverging approaches top-down and bottom-up perspectives. Top-down theories such as adaptation or set-point theory assume that personal characteristics are most influential because well-being is found to be resistant to life events due to an innate mechanism of adjusting to changing life conditions and experiences (Headey and Wearing 1989). In contrast, the bottom-up perspective considers contextual sources as more influential assuming that well-being will fluctuate with changing life conditions. However, acknowledging empirical findings in support of both perspectives, attempts have been made to integrate the two perspectives and studies have been designed to test the hypothesis that personal characteristics may directly but also indirectly affect life satisfaction judgments (Brief et al. 1993; Schimmack et al. 2002). Personality traits and psychological resources are assumed to influence individual perceptions of contextual circumstances such as health.
Neuroticism and extraversion have repeatedly been found to relate to life satisfaction levels (Costa and McCrae 1980; DeNeve and Cooper 1998; Headey and Wearing 1989; Hilleras et al. 2001) and change (Mroczek and Spiro 2005), and also to health (Duberstein et al., 2003; Moor et al. 2006). Furthermore, defined by Rotter as a personality trait (Rotter 1966), locus of control has been found to be associated with both health (Sturmer et al. 2006) and life satisfaction (Hickson et al. 1988; Landau and Litwin 2001) and has also been found to moderate the health and well-being relationship (Landau and Litwin 2001) in old age. The perception of personal influence is assumed to become increasingly important in situations when individuals experience restrictions in their everyday life as a result of deteriorated health, compromised functional capacities and social changes. So far, little is known about the role of personality in the relationship between health and late life changes in life satisfaction.
The study of life satisfaction changes in samples of old individuals differs from the study of younger samples because of the mortality and pathology-related processes that accompany the age-graded changes (Baltes and Smith 1997; Berg 1996). Mroczek and Spiro used an aged-based model to investigate change in life satisfaction. They found a decline with advancing age, but also an accelerating effect of proximity to death as satisfaction with life showed a steeper decline 1 year before death (Mroczek and Spiro 2005). Accordingly, the use of time-in-study or chronological age as time metrics in late life changes in life satisfaction will also include effects of mortality-related processes given that individuals aged 80 and older border on or surpass the average life expectancy. In their studies of late life changes in life satisfaction, Gerstorf and colleagues applied a time-to-death time metric that mainly has been used in the investigation of psychological change in the end of life in terms of change in cognitive functions (Gerstorf et al. 2008a, b). Gerstorf et al. argue that a similar pattern of terminal decline, as seen in cognitive abilities (Bosworth and Siegler 2002; Bäckman and MacDonald 2006; Sliwinski et al. 2003, Wilson et al. 2003; Wilson et al. 2007), may be expected in subjective well-being given the age-graded stability in subjective well-being measures. Parallel findings have been presented for changes in self-perceptions of aging where satisfaction with aging showed a steeper mortality-related decline as compared to age-related decline (Kotter-Grühnet al. 2009). The psychological and biological mechanisms generating a cognitive terminal decline are thereby assumed to be present even in late life changes in well-being measures. Also, given that individuals differ markedly in health and psychosocial resources at these ages, chronological age may be an inadequate time structure in the study of changes in life satisfaction in advanced age. Distance to death seems to be an adequate and more informative time structure in the population of the oldest-old.
Although cause of death may ostensibly provide the most relevant explanatory context for time-to-death-related changes in life satisfaction, the comorbidity and frailty that characterizes the oldest-old population obstruct the identification of a single death cause in old individuals and seriously restricts the validity of death certificates (Maudsley and Williams 1996; Myers and Farquhar 1998). In an attempt of identifying possible mechanisms in action for time-to-death-related changes in life satisfaction, Gerstorf et al. found initial level of comorbidity to predict level of life satisfaction, but not change in life satisfaction related to death (Gerstorf et al. 2008). In a recent study, Palgi et al. confirmed these results in their study of terminal change in subjective well-being; the inclusion of gender, marital status, place of residence, cognitive function and diagnoses did not reduce the terminal change effects (Palgi et al. 2010). Two limitations characterize these studies. First, the counterintuitive findings of a weak relationship between life satisfaction and objective health measures, also confirmed in our own previous studies (Berg et al. 2006; Berg et al. 2009), may reflect a neglect of the heterogeneity of health and personal resources in old age groups. Even if a large proportion of individuals aged 80 and older handle ill-health and frailty well, the lack of personal resources and the ability to cope in the presence of ill-health could affect life satisfaction negatively in specific subgroups. Second, the use of only time-invariant health predictors put obvious restrictions to the predictability of health on life satisfaction. A time-variant health predictor would probably explain a greater proportion of the variance of life satisfaction changes in late life. Finally, in a previous study we identified subjective health to strongly predict life satisfaction in the oldest-old (Berg et al. 2006). All in all, level and changes in overall load of disease and self-rated health are potential predictors of time-to-death-related changes in life satisfaction.
The aims of this study were to investigate if personality and personal control influence the association between subjective and objective measures of health and mortality-related level and change in life satisfaction in individuals aged 80 and older. Along the ideas from an integration of top-down and bottom-up perspectives we hypothesize that extraversion, emotional stability, and perceptions of inner locus of control may reduce the effect of poor self-rated health and high load of disease on life satisfaction.
Method
Sample
The study includes participants from the population based longitudinal study, “Origins of Variance in the Old-Old,” or OCTO-Twin Study (McClearn et al. 1997). The sample consisted of 351 pair of twins aged 80 and older living in Sweden. Only 453 individuals completed the Life Satisfaction Index-Z at the first measurement point. Individuals (n = 41) with a dementia diagnosis were excluded from the analyses because of reliability problems related to self-reports in this group. In addition, the time-to-death time metric required a further exclusion of 46 (6.6%) individuals that were still alive in December 2007, resulting in a sample of 370 participants at baseline with 43% of the individuals included in intact pair of twins. Across the three subsequent waves, the sample sizes were 227, 161, and 87, respectively. Attrition analysis of the selected sample and the excluded participants at wave 1 showed that the selected sample was older, t (700) = 3.17, p = .002, had fewer diagnoses, t (700) = −6.11, p < .001, but did not report better self-rated health, t (584) = −1.10, p = .278.
Procedure
Trained research nurses visited the participants in their homes for data collection every second year from 1991 to 1997. The testing sessions lasted 3–4 h including testing and rest breaks. Tests requiring concentration and vigilance were administered during the first hour. Participants were asked to complete and mail back the inventories after the testing session.
Measures
Outcome variable
Life satisfaction was measured with the Life Satisfaction Index-Z (LSI-Z; Wood et al. 1969) which is a 13-item version of the original 20-item Life Satisfaction Index-A (Neugarten et al. 1961) and consists of statements reflecting life satisfaction in old age such as: “As I grow older, things seem better than I thought they would be” and “When I think back over my life, I didn’t get most of the important things I wanted”. Participants rated each statement from “agree totally” = 1 to “do not agree at all” = 5. Negative items were reverse-coded. The sum of the scale ranges from 13 to 65, with higher scores indicating greater life satisfaction. A mean imputation was conducted for 70 individuals with 3 or less missing items on the LSI-Z at the first wave. Cronbach’s alpha at wave 1 was 0.78.
Independent variables
Socio-economic status (SES) refers to under, middle, and upper class.
Overall load of disease was indexed measured as total number of diagnoses for each participant. The number of diagnoses was determined by a physician collecting information from medical records dating back to 1985 and from the participants’ self-reported information of diagnoses (Nilsson et al. 2002). Number of diagnoses varied from 1 to 23 in this sample.
Self-rated health consists of 4 items representing global health: “How do you perceive your health status?” (poor = 1, average = 2, good = 3), social comparison: “How do you perceive your health status as compared to other people at your age?” (worse = 1, about same = 2, better = 3), intraindividual comparison: “How do you perceive your current health status as compared with the status 2 years ago?” (worse = 1, about same = 2, better = 3), and to what degree health is perceived as a obstacle/hinder in everyday living: “Do you think your health status prevents you from doing things you want to do?” (yes = 1, to an extent = 2, not at all = 3). The total sum ranges from 4 to 12 points with higher scores indicating better perceived health. Cronbach’s alpha at wave 1 was 0.62.
Personality
Eysenck Personality Inventory (EPI) includes the personality traits neuroticism and extraversion and consists of 19 items. The neuroticism scale contains questions such as: “Are you sometimes happy, sometimes sad without any particular reason?” “Are you sometimes so restless that you can’t sit still?” or “Do you have nervous problems?” The extraversion scale contains questions such as: “Do you always have something to say when people talk to you?” “Do you like telling jokes to your friends?” or “Do you have a lively way?”. The items were dichotomous: “Yes” = 1 and “No” = 0. Negative items were reverse-coded. The total sum of scores for the Extraversion scale was 0–9 with higher scores indicating more extraversion. The Cronbach’s alpha was 0.64 at wave 1. For Neuroticism, the range was 0–10 with higher scores indicating more neuroticism. Cronbach’s alpha was 0.75 at wave 1.
Locus of control
The Locus of control-scale (Rotter 1966) consists of twelve questions concerning perceived internal and external locus of control. Participants rated locus of control on 5-point-scaled items such as: “When I make plans, I am almost certain that I can make them work” (internal locus of control) or “Sometimes I feel that I don’t have enough control over the direction my life is taking” (external locus of control). The total sum of the scale ranges from 12 to 60, with higher scores meaning higher degree of perceived internal control. Participants returned the inventory by mail. Cronbach’s alpha was .73 at wave 1.
Data analysis
Individual change trajectories in life satisfaction related to death were estimated using growth curves within the mixed modeling framework in the SPSS. Initially an unconditional model was estimated and then two models using either chronological age or time-to-death as time index. The time-to-death time metric was centered at time of death and the chronological age time metric of change was centered at mean age of 83.6 years. Age, gender, SES, years-to-death from baseline, self-rated health overall load of disease, extraversion, neuroticism, and locus of control were included as covariates. Three-level models were applied in order to hierarchically structure data in nested models and thereby accounting for three levels of variance; within-individual (Level 1), between-individuals (Level 2), and between-twin pairs (Level 3).
Fixed effects in the analyses reflect effects of the population mean trajectory, and the random effects reflect the covariance structure. Thus, fixed effects of time for life satisfaction represent the investigation of linear and polynomial changes of the population mean across the four measurement points, whereas the random effects reflect individuals’ deviation from the sample mean trajectory. In accordance to previous research both fixed linear and quadratic changes would need to be explored.
In a second step we explored the possible influence of a set of predictors. Finding that the time-to-death model had a better model fit as compared to the age-based model we included gender, SES, years-to-death at wave 1, self-rated health, and number of diagnoses as possible predictors of changes in life satisfaction in the time-to-death model. The variable Years-to-death at wave 1 was included to investigate possible effects of distance to death on baseline levels of life satisfaction. Two models were estimated: Model A1: Overall Load of Disease and Model B1: Self-rated Health, and were both represented by a Level-1 variable for within-person change and a Level-2 variable for between-persons differences. The within-person variables have occasion-specific values that reflect the deviance from the person-specific first occasion value, whereas the between-person variables have identical values across all waves that reflect the deviance at initial level from the initial sample mean (i.e., where 0 represents the sample mean). The initial sample mean for self-rated health was 9 and for number of diagnoses 10.
In a third step, Model A1: Overall Load of Disease and Model B1: Self-rated Health were expanded in order to investigate possible interactions between each health measure and neuroticism, extraversion, and locus of control on level and time-to-death-related changes in life satisfaction. The between-person variables were centered at the sample means: extraversion: 5.1 (SD = 2.1), neuroticism: 2.7 (SD = 2.4), and locus of control 37.1 (SD = 4.0).
Results
Table 1 presents descriptive characteristics of the sample across the 4 waves. Initially we estimated an unconditional model. The within-person, between-person, and between-twin pairs accounted for 35, 32, and 33% of the total variability, respectively. Then two unconditional growth models were estimated using different time metrics of changes in life satisfaction; chronological age; and time-to-death. In both the age-based model (−.32, SE = .07, p < .001) and in the time-to-death model (−.39, SE = .07, p < .001) there were significant linear declines in life satisfaction. No fixed or random quadratic slope effects were found significant. Finally, the model deviance values showed that the time-to-death model had a significantly better fit as compared to the chronological age-model with a difference in AIC of 870.519. Therefore, in the subsequent analyses a time-to-death time metric was used.
Table 1.
Descriptive characteristics of the sample at waves 1–4
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | |||||
|---|---|---|---|---|---|---|---|---|
| 1991 | 1993 | 1995 | 1997 | |||||
| (N = 370) | (N = 227) | (N = 161) | (N = 87) | |||||
| M | SD | M | SD | M | SD | M | SD | |
| Life Satisfaction Index-Z | 46.8 | 8.2 | 46.4 | 7.6 | 46.4 | 7.5 | 46.6 | 7.3 |
| Age | 83.3 | 2.8 | 84.6 | 2.2 | 86.6 | 2.1 | 88.3 | 1.9 |
| Sex | Men: 45% | Men: 47% | Men: 47% | Men: 44% | ||||
| SES | ||||||||
| Upper class (%) | 13.7 | 14.6 | 14.1 | 15.7 | ||||
| Middle class (%) | 38.6 | 41.9 | 43.7 | 47.1 | ||||
| Lower class (%) | 47.7 | 43.5 | 42.3 | 37.2 | ||||
| Number of diagnoses | 9.9 | 4.8 | 9.8 | 4.7 | 9.5 | 5.0 | 9.1 | 5.1 |
| Self-rated health | 9.0 | 1.8 | 8.9 | 1.7 | 8.7 | 1.8 | 8.4 | 1.9 |
| Age at death | 90.2 | 4.3 | ||||||
| Years-to-death at wave 1 | 7.0 | 3.8 | ||||||
| Extraversion | 5.1 | 2.1 | ||||||
| Neuroticism | 2.7 | 2.4 | ||||||
| Locus of control | 37.1 | 4.0 | ||||||
M Mean, SD Standard deviation
Table 2 presents the results from two estimated time-to-death models. Model A1 including gender, age, SES, years-to-death at wave 1, and overall load of disease as covariates and show that less overall load of disease was significantly related to higher levels of life satisfaction (.49, SE = .11, p < .001). Model B1 including gender, age, SES, years-to-death at wave 1 and self-rated health as predictors, higher self-rated health was significantly related to higher levels of life satisfaction (1.77, SE = .32, p < .001). Years-to-death at Wave 1 was not significantly related to level of life satisfaction, and an interaction with slope was therefore not tested. Age, gender, and SES were not significantly related to level of life satisfaction, and no interactions with the linear slope were significant. These parameters were therefore omitted in the following models.
Table 2.
Level and time-to-death-related change in LS: parameter estimates and standard errors for Model A1: age, years-to-death, gender, SES, and overall load of disease, and Model B1: age, years-to-death, gender, SES, and self-rated health
| Parameter | Model A1 | Model B1 | ||
|---|---|---|---|---|
| Overall load of disease | Self-rated health | |||
| Estimate | SE | Estimate | SE | |
| Fixed effects | ||||
| Intercept | 46.13*** | 1.15 | 46.18*** | 1.20 |
| Linear slope | −.45*** | .14 | −.53*** | .16 |
| Age | −.07 | .20 | .06 | .21 |
| Age*Slope | −.02 | .03 | −.01 | .03 |
| Years-to-death at wave 1 | .10 | .12 | .16 | .13 |
| Gender | .03 | 1.14 | −.18 | 1.15 |
| Gender*Slope | .20 | .15 | .26 | .15 |
| SES | −1.28 | .75 | −1.35 | .78 |
| SES*Slope | −.13 | .10 | −.12 | .11 |
| Overall load of disease-BP | −.49*** | .11 | ||
| Overall load of disease-BP*Slope | −.01 | .01 | ||
| Overall load of disease-WP | .02 | .17 | ||
| Overall load of disease-WP*Slope | .04 | .03 | ||
| Self-rated health-BP | 1.77*** | .32 | ||
| Self-rated health-BP*Slope | .05 | .04 | ||
| Self-rated health-WP | .40 | .30 | ||
| Self-rated health-WP*Slope | .00 | .05 | ||
| Person-level variance of intercept | 19.56 | 4.18 | 25.21 | 5.24 |
| Twin-level variance of intercept | 19.78 | 4.18 | 9.89 | 5.02 |
| Residual variance | 18.48 | 1.22 | 18.98 | 1.37 |
SE standard error, BP between-person, WP within-person
* p < .05
*** p < .001
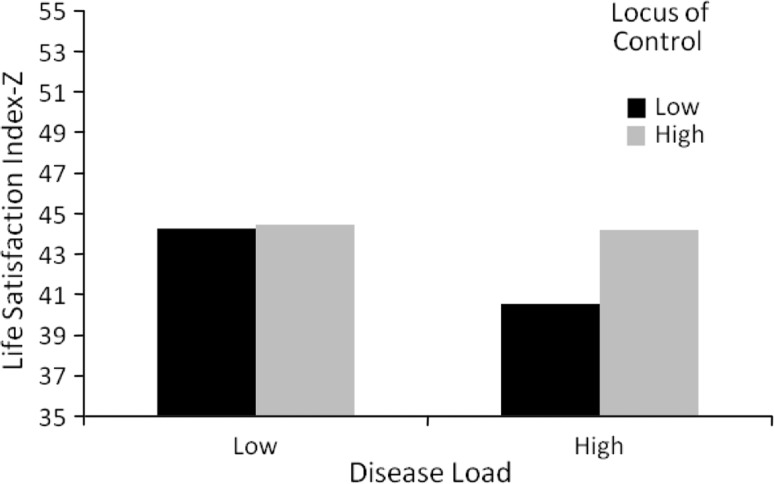
In Table 3, Model A2 investigates the relationship between overall load of disease and life satisfaction in terms of interactions with locus of control, neuroticism, and extraversion. The main effect of disease load was, as in previous models, significant (−.21, SE = .08, p < .05), where high disease load was related to lower life satisfaction. High scores on neuroticism (−.77, SE = .20, p < .001) and low scores on extroversion (.95, SE = .20, p < .001) were related to lower life satisfaction. The main effect of locus of control was significant (.24, SE = .09, p < .05) indicating the low scores on locus of control was related to low life satisfaction. There was a significant interaction between disease load and locus of control (.04, SE = .02, p < .05), where individuals with high disease load did not show lower life satisfaction in the presence of high locus of control (see Fig. 1). Interactions between overall load of disease and level of extraversion or neuroticism were not significant.
Table 3.
Level and time-to-death-related change in LS: parameter estimates and standard errors for Model A2: overall load of disease, neuroticism, extraversion, and locus of control and Model B2: self-rated health, neuroticism, extraversion, and locus of control
| Parameter | Model A2 | Model B2 | ||
|---|---|---|---|---|
| Overall load of disease | Self-rated health | |||
| Estimate | SE | Estimate | SE | |
| Fixed effects | ||||
| Intercept | 43.35*** | .61 | 43.72*** | .60 |
| Linear Slope | −.45*** | .08 | −.47** | .08 |
| Overall load of disease-BP | −.21* | .08 | ||
| Self-rated health-BP | .57** | .21 | ||
| Extraversion | .95*** | .20 | .93*** | .19 |
| Extraversion*Overall load of disease-BP | −.00 | .04 | ||
| Extraversion*Self-rated Health-BP | .01 | .10 | ||
| Neuroticism | −.77*** | .20 | −.70*** | .18 |
| Neuroticism*Overall load of disease-BP | .02 | .03 | ||
| Neuroticism*Self-rated Health-BP | .18* | .09 | ||
| Locus of control | .24* | .09 | .28** | .09 |
| Locus of control*Overall load of disease-BP | .04* | .02 | ||
| Locus of control*Self-rated Health | −.07 | .05 | ||
| Person-level intercept | 13.84 | 4.75 | 14.02 | 4.77 |
| Twin-level intercept | 7.77 | 4.80 | 6.65 | 4.68 |
| Residual Variance | 18.29 | 1.42 | 18.32 | 1.48 |
SE Standard Error, BP between-person
* p < .05
** p < .01
*** p < .001
Fig. 1.
The relationship between low and high disease load and life satisfaction in individuals with low and high inner locus of control
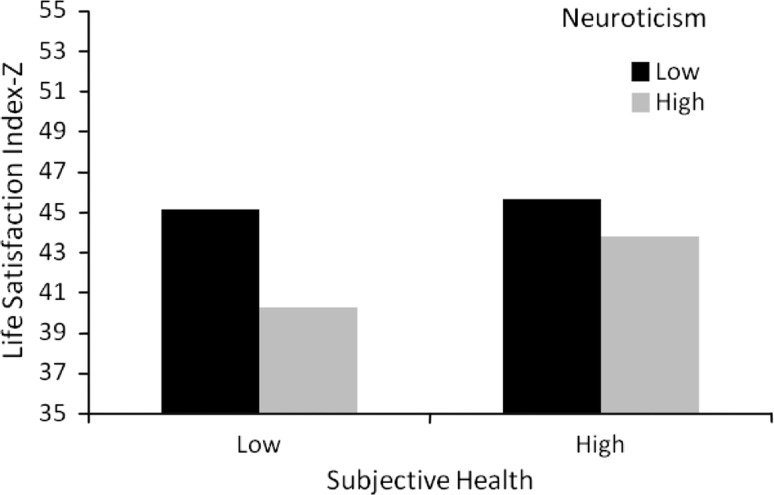
Model B2 presents the relationship between self-rated health and life satisfaction and the interactions of locus of control, neuroticism, and extraversion. Low scores on self-rated health (.57, SE = .21, p < .01), extraversion (.93, SE = .19, p < .001), and locus of control (.28, SE = .09, p < .01), in addition to high score on neuroticism (−.70, SE = .18, p < .001), were related to poorer life satisfaction. A significant interaction between self-rated health and neuroticism was found (.18, SE = .09, p < .05), such that individuals with low self-rated health did not show lower life satisfaction in the presence of low neuroticism (see Fig. 2). Non-significant interaction parameters were excluded from the models, and no random effects of the predictors were significant.
Fig. 2.
The relationship between poor and good self-rated health and life satisfaction in individuals with low and high scores on neuroticism
Discussion
We investigated possible interaction effects between health measures and extraversion, neuroticism, and locus of control in time-to-death-related changes in life satisfaction at four measurement points across 6 years in a sample of cognitively intact individuals aged 80 and over.
Individuals in the study became less satisfied with life over measurement occasions and as they approached death, but neither level nor changes in overall load of disease nor self-rated health accounted for the change. However, both overall load of disease and self-rated health were associated with level of life satisfaction. Interestingly we found higher levels of life satisfaction in individuals with higher overall disease load and higher internal locus of control, whereas in individuals with poorer self-rated health, higher scores on neuroticism were related to lower levels of life satisfaction.
Change in life satisfaction was not related to initial level or change in medically based or self-rated health measures. The oldest-old population consists of a heterogeneous group of individuals who greatly vary in health and functioning and, in contrast to younger populations, psychological change would expectedly be related to mortality-related and pathology-related underlying processes (Baltes and Smith 1997). However, in this study the time-to-death-related decline in life satisfaction was not accounted for by level or change in overall load of disease and self-rated health. The investigation of possible powerful predictors of change related to distance from death must be dealt with in future research.
However, personality was found to interact on cross-sectional relationships between health and life satisfaction, a finding that also supports the integration of top-down and bottom-up perspectives on life satisfaction judgments. First, the experience of internal control in states of ill-health to level of life satisfaction supports previous findings of psychological resources as significant filters of the experience of objective health conditions. Interestingly, as illustrated in Fig. 1, the perception of being in control of one’s life was important only for individuals with high disease load. Individuals with high disease load and inner locus of control were just as satisfied as more healthy individuals. The subgroup of individuals with poor health who also lack the experience of control is at particular risk of dissatisfaction. These individuals will require more support from health care and could probably benefit from psychological treatment.
Individuals with an emotionally instable personality and poor self-rated health accentuated the dissatisfaction with life (see Fig. 2). Although neuroticism and self-rated health are interrelated (10% of the variation related in the present sample), numerous findings of self-rated health as a central predictor of mortality (Idler and Benyamini 1997) suggest that there is a need of identifying protective factors in these high risk groups for lower life satisfaction.
Limitations of this study associated with attrition is less related to losing individuals across the study period, given that death thaws the main reason for attrition which is representative for the oldest-old population. However, the procedure of leaving the LSI-Z, EPI, and Locus of Control scales with the participants to complete and return by mail probably resulted in a select sample of individuals aged 80 and over. Thus, as the attrition analysis suggests, the conclusions drawn from the study are above all valid for a healthier segment of the oldest-old. A potential selection bias due to twinship, (i.e., twins differ from non-twins), has previously been investigated in the current sample (Simmons et al. 1997). Singletons and twins did not differ with regard to education, socio-economic status, marital status, housing, health status, or biobehavioral functions such as cognitive function or well-being. Furthermore, variance related to twinship was controlled for in all analyses by the use of three levels analysis; within-person, within-pair and between-person.
Strengths of the present longitudinal study of inter-individual differences in intra-individual time-to-death-related changes in life satisfaction across multiple measurement occasions concerns in particular the identification of specific subgroups at risk for dissatisfaction with life. As previously mentioned, the results are applicable to a healthier group of individuals aged 80+, but nonetheless, the comorbidity rates are high also in the present sample. The identification of specific personality characteristics that may interact with health and put mental health at risk is vital. Furthermore, the application of time-to-death as a time metric in the study of changes in life satisfaction, including both time-invariant and time-varying predictors of medically based health and self-rated health, have provided knowledge to a largely unexplored field in life satisfaction research of the oldest-old.
In sum, this study provides evidence that personality characteristics in late life act as a possible agent in the multifaceted relationship between health and life satisfaction. The investigation of cross-sectional interactions between health and personality on life satisfaction offers a better understanding of interrelating processes of life satisfaction in late life. The existence of the top-down processes in the evaluations of health and life in general should be further recognized in health care and more efforts must be directed at the instigation of psychological interventions also among the oldest-old.
Acknowledgments
This study was supported by National Institutes of Health; NIA (AG 08861) and Swedish Council for Working Life and Social Research; FAS 2002-0659, FAS 2007-0554, FAS 2006-1506.
References
- Bäckman L, MacDonald S. Death and cognition: synthesis and outlook. Eur Psychol. 2006;11:224–235. doi: 10.1027/1016-9040.11.3.224. [DOI] [Google Scholar]
- Baird BM, Lucas RE, Donnellan M. Life satisfaction across the lifespan: findings from two nationally representative panel studies. Soc Indic Res. 2010 doi: 10.1007/s11205-010-9584-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baltes PB, Smith J. A systemic-wholistic view of psychological functioning in very old age: introduction to a collection of articles from the Berlin Aging Study. Psychol Aging. 1997;12:395–409. doi: 10.1037/0882-7974.12.3.395. [DOI] [PubMed] [Google Scholar]
- Berg S. Aging, behavior, and terminal decline. In: Birren JE, Schaie KW, editors. Handbook of the psychology of aging. 4. San Diego, CA: Academic Press; 1996. pp. 323–337. [Google Scholar]
- Berg AI, Hassing LB, Johansson B, McClearn G. What matters for life satisfaction in the oldest-old? Aging Ment health. 2006;10(3):257–264. doi: 10.1080/13607860500409435. [DOI] [PubMed] [Google Scholar]
- Berg AI, Hoffman L, Hassing LB, Johansson B. What matters, and what matters most, for change in life satisfaction in the oldest-old? A study over 6 years among individuals 80+ Aging Ment Health. 2009;13:191–201. doi: 10.1080/13607860802342227. [DOI] [PubMed] [Google Scholar]
- Bosworth HB, Siegler IC. Terminal change in cognitive function: an updated review of longitudinal studies. Exp Aging Res. 2002;28:299–315. doi: 10.1080/03610730290080344. [DOI] [PubMed] [Google Scholar]
- Brief AP, Butcher AH, George JM, Link KE. Integrating bottom-up and top-down theories of subjective well-being: the case of health. J Pers Soc Psychol. 1993;64:646–653. doi: 10.1037/0022-3514.64.4.646. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr, McCrae RR. Influence of extraversion and neuroticism on subjective well-being: happy and unhappy people. J Pers Soc Psychol. 1980;38:668–678. doi: 10.1037/0022-3514.38.4.668. [DOI] [PubMed] [Google Scholar]
- DeNeve KM, Cooper H. The happy personality: a meta-analysis of 137 personality traits and subjective well-being. Psychol Bull. 1998;124:197–229. doi: 10.1037/0033-2909.124.2.197. [DOI] [PubMed] [Google Scholar]
- Diener E. Subjective well-being. Psychol Bull. 1984;95:542–575. doi: 10.1037/0033-2909.95.3.542. [DOI] [PubMed] [Google Scholar]
- Duberstein PR, Sorensen S, Lyness JM, King DA, Conwell Y, Seidlitz L, et al. Personality is associated with perceived health and functional status in older primary care patients. Psychol Aging. 2003;18:25–37. doi: 10.1037/0882-7974.18.1.25. [DOI] [PubMed] [Google Scholar]
- Gerstorf D, Ram N, Rocke C, Lindenberger U, Smith J. Decline in life satisfaction in old age: longitudinal evidence for links to distance-to-death. Psychol Aging. 2008;23:154–168. doi: 10.1037/0882-7974.23.1.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstorf D, Ram N, Estabrook R, Schupp J, Wagner GG, Lindenberger U. Life satisfaction shows terminal decline in old age: longitudinal evidence from the german socio-economic panel study (SOEP) Dev Psych. 2008;23:154. doi: 10.1037/0012-1649.44.4.1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Headey B, Wearing A. Personality, life events, and subjective well-being: toward a dynamic equilibrium model. US: Am Psychol Assoc; 1989. [Google Scholar]
- Hickson J, Housley WF, Boyle C. The relationship of locus of control, age, and sex to life satisfaction and death anxiety in older persons. Int J Aging Hum Dev. 1988;26:191–199. doi: 10.2190/E5CK-THBM-QVQG-C3DN. [DOI] [PubMed] [Google Scholar]
- Hilleras PK, Jorm AF, Herlitz A, Winblad B. Life satisfaction among the very old: a survey on a cognitively intact sample aged 90 years or above. Int J Aging Hum Dev. 2001;52:71–90. doi: 10.2190/B8NC-D9MQ-KJE8-UUG9. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- Kotter-Grühn D, Kleinspehn-Ammerlahn A, Gerstorf D, Smith J. Self-perceptions of aging predict mortality and change with approaching death: 16-year longitudinal results from the Berlin Aging Study. Psychol Aging. 2009;24:654–667. doi: 10.1037/a0016510. [DOI] [PubMed] [Google Scholar]
- Landau R, Litwin H. Subjective well-being among the old-old: the role of health, personality and social support. Int J Aging Hum Dev. 2001;52:265–280. doi: 10.2190/RUMT-YCDX-X5HP-P2VH. [DOI] [PubMed] [Google Scholar]
- Maudsley G, Williams EM. ‘Inaccuracy’ in death certification—where are we now? J Public Health Med. 1996;18:59–66. doi: 10.1093/oxfordjournals.pubmed.a024463. [DOI] [PubMed] [Google Scholar]
- McClearn GE, Johansson B, Berg S, Pedersen NL, Ahern F, Petrill SA, et al. Substantial genetic influence on cognitive abilities in twins 80 or more years old. Science. 1997;276:1560–1563. doi: 10.1126/science.276.5318.1560. [DOI] [PubMed] [Google Scholar]
- Moor C, Zimprich D, Schmitt M, Kliegel M. Personality, aging self-perceptions, and subjective health: a mediation model. Int J Aging Hum Dev. 2006;63:241–257. doi: 10.2190/AKRY-UM4K-PB1V-PBHF. [DOI] [PubMed] [Google Scholar]
- Mroczek DK, Spiro A., III Change in life satisfaction during adulthood: findings from the veterans affairs normative aging study. J Pers Soc Psychol. 2005;88:189–202. doi: 10.1037/0022-3514.88.1.189. [DOI] [PubMed] [Google Scholar]
- Myers KA, Farquhar DR. Improving the accuracy of death certification. Can Med Assoc J. 1998;158:1317–1323. [PMC free article] [PubMed] [Google Scholar]
- Neugarten BL, Havighurst RJ, Tobin SS. The measurement of life satisfaction. J Gerontol. 1961;16:134–143. doi: 10.1093/geronj/16.2.134. [DOI] [PubMed] [Google Scholar]
- Nilsson SE, Johansson B, Berg S, Karlsson D, McClearn GE. A comparison of diagnosis capture from medical records, self-reports, and drug registrations: a study in individuals 80 years and older. Aging Clin Exp Res. 2002;14:178–184. doi: 10.1007/BF03324433. [DOI] [PubMed] [Google Scholar]
- Palgi Y, Shrira A, Ben-Ezra M, Spalter T, Shmotkin D, Kavé G. Delineating terminal change in subjective well-being and subjective health. J Gerontol B Psychol Sci Soc Sci. 2010;65B(1):61–64. doi: 10.1093/geronb/gbp095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotter JB. Generalized expectancies for internal versus external control of reinforcement. Psychol Monogr. 1966;80:1–28. [PubMed] [Google Scholar]
- Schimmack U, Diener E, Oishi S. Life-satisfaction is a momentary judgment and a stable personality characteristic: the use of chronically accessible and stable sources. J Pers. 2002;70:345–384. doi: 10.1111/1467-6494.05008. [DOI] [PubMed] [Google Scholar]
- Simmons SF, Johansson B, Zarit SH, Ljungquist B, Plomin R, McClearn GE. Selection bias in samples of older twins? A comparison between octogenarian twins and singletons in Sweden. J Aging Health. 1997;9:553–567. doi: 10.1177/089826439700900407. [DOI] [PubMed] [Google Scholar]
- Sliwinski MJ, Hofer SM, Hall C, Buschke H, Lipton RB. Modeling memory decline in older adults: the importance of preclinical dementia, attrition, and chronological age. Psychol Aging. 2003;18:658–671. doi: 10.1037/0882-7974.18.4.658. [DOI] [PubMed] [Google Scholar]
- Sturmer T, Hasselbach P, Amelang M. Personality, lifestyle, and risk of cardiovascular disease and cancer: follow-up of population based cohort. BMJ. 2006;332:1359. doi: 10.1136/bmj.38833.479560.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson RS, Beckett LA, Bienias JL, Evans DA, Bennett DA. Terminal decline in cognitive function. Neurology. 2003;60:1782–1787. doi: 10.1212/01.wnl.0000068019.60901.c1. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Beck TL, Bienias JL, Bennett DA. Terminal cognitive decline: accelerated loss of cognition in the last years of life. Psychosom Med. 2007;69:131–137. doi: 10.1097/PSY.0b013e31803130ae. [DOI] [PubMed] [Google Scholar]
- Wood V, Wylie ML, Sheafor B. An analysis of a short self-report measure of life satisfaction: correlation with rater judgments. J Gerontol. 1969;24:465–469. doi: 10.1093/geronj/24.4.465. [DOI] [PubMed] [Google Scholar]