Abstract
Self-rated health (SRH) is a multidimensional measure, predictive of morbidity and mortality. Comparative studies of determinants, however, are rare due to a lack of comparable cross-national data. This paper contributes towards filling in this gap, using data for persons aged 50 or higher in 11 European countries from the SHARE study (2004). The analysis aims at identifying key elements composing SRH using multinomial logistic regression models. In addition, the homogeneity of associations across populations is assessed. The findings indicate that education, depression, chronic conditions, mobility difficulties, somatic symptoms and levels of physical activity constitute important components of SRH; ADLs and obesity, on the other hand, are not significant and IADLs are important only in a few countries. All these associations point to the expected direction and are homogeneous across countries. However, demographic factors, age and gender, though significant in many countries have divergent associations. Effects of smoking also differentiate between southern and northern Europe.
Keywords: Self-rated health, SHARE, Cross-national comparison, Multinomial logistic regression, Determinants, Homogeneity across countries
Introduction
Self-rated or self-assessed health (SRH) is a multidimensional measure of health status, based on a respondent’s perception of how well he feels. A number of studies have revealed strong associations of the measure with various aspects of health, such as chronic conditions, functional disabilities and impairments, disease symptoms and behavioural risk factors (Idler and Kasl 1991; Verbrugge and Jette 1994; Baron-Epel and Kaplan 2001). On the other hand, it encompasses a strong subjective element and depends also on perceptions, attitudes and psychosocial factors (Simon et al. 2005).
In spite of its apparent subjectivity, SRH has proved a robust and reliable predictor of morbidity and mortality. Moreover, its predictive power of a person’s subsequent survival probability remains strong even when objective indicators of health have been taken into account (Appels et al. 1996; Idler and Benyamini 1997; Van Doorslaer and Gerdtham 2003). This leads researchers to suggest that such a question may identify not only the “at-risk” individuals but also illnesses and conditions which go undetected during routine evaluations (Eriksson et al. 2001; DeSalvo et al. 2005).
Reporting of SRH, however, may differ across subgroups of a population. It has been observed in several studies that the age gradient based on the question “how well do you feel” is underestimated among the older old, probably due to these persons having a milder view on what constitutes poor health (Ongaro and Salvini 1995; Bardage et al. 2005; Simon et al. 2005). The relationship with gender is inconsistent or negligible in some cases (Arber and Cooper 1999; Zimmer et al. 2000) while it seems that men report better health than women in other (Bardage et al. 2005; Gilmore et al. 2002). A strong positive association between socio-economic status (SES) and all health measures, including SRH, is a well established fact (Mackenbach et al. 1997; Zimmer et al. 2000; Lahelma et al. 2005). However, whether reporting is influenced by the socio-economic characteristics of the respondents is debatable. In Sweden, occupational class, income and education do not seem to affect the predictive power of SRH on mortality (Burström and Fredlund 2001; Van Doorslaer and Gerdtham 2003). By contrast, Dowd and Zajacova (2007) and Huisman et al. (2007) conclude that the measure is a better predictor among higher SES persons while Singh-Manoux et al. (2007) suggest the opposite (i.e., weaker associations with high income and occupational class).
Cross-national comparisons based on SRH are even more complex as health standards and reporting styles may vary across cultures; reporting may be influenced even by factors such as the wording of the question or the language (Angel and Guarnaccia 1989). Such comparisons are a tricky exercise and may result in biased conclusions if different populations use systematically different threshold levels for their evaluation despite having the same level of “true” health (Lindeboom and Van Doorslaer 2004; Jürges 2007). Even controlling for health status (chronic conditions, disabilities, symptoms), demographic characteristics (age and gender), socioeconomic factors (education, income, occupation, wealth) and health related behaviour (smoking, body mass index, physical activity), there are still differences in the self-assessment of health that cannot be accounted for by the observable characteristics of the respondents and should, at least partly, be attributable to differential reporting (Zimmer et al. 2000).
Studies comparing health status and differential reporting across populations based on SRH are fairly rare, due to the complexities of the measure and the lack of comparable cross-national data. In the few cases that such analyses have been undertaken the harmonization of the measures under study occurred only after the surveys had been carried out and could, thus, be questionable (Bardage et al. 2005; Zimmer et al. 2000). Exceptions are very few.
The present study contributes to the scarcely explored cross-national differentials in the reporting of SRH among older persons, using comparable information for 11 European countries from the Survey of Health, Ageing and Retirement in Europe (SHARE). The principal objective of the analysis is to identify the key elements composing SRH for each country among socio-demographic factors, health indicators and risky health behaviours and to discern whether associations are homogeneous across populations or differentiate.
Methods
Data
The data used in the analysis come from release 2 (July 2007) of the first wave of the Survey of Health, Ageing and Retirement in Europe. The survey is coordinated centrally at the Mannheim Research Institute for the Economics of Ageing and follows an established protocol of questionnaire design, data collection and electronic management system. It is modelled on the US Health and Retirement Survey (HSR) and the English Longitudinal Survey of Ageing (ELSA). The baseline was conducted in 2004 in 11 European countries, covering about 27 and a half thousand individuals (Börsch-Supan et al. 2005a, b). The information collected includes cross-national comparable micro data on health, socio-economic status and social and family networks of individuals aged 50 or over at the time of the survey. The countries included in the study are a balanced representation of the various regions of Europe, ranging from Scandinavia (Denmark and Sweden) through Central Europe (Austria, France, Germany, Switzerland, Belgium and The Netherlands) to the Mediterranean (Spain, Italy and Greece). The present analysis includes 27,215 individuals with non-missing information on socio-economic and health indicators; sample sizes by country are presented in Table 1.
Table 1.
Percentage distribution of the SHARE respondents by country and reported level of SRH
| Country | Very good | Good | Fair | Bad | Very Bad | Sample size |
|---|---|---|---|---|---|---|
| Switzerland | 32.5 | 47.7 | 16.3 | 2.9 | 0.6 | 941 |
| Denmark | 24.3 | 44.7 | 22.1 | 5.9 | 3.0 | 1,609 |
| Netherlands | 18.0 | 49.7 | 25.6 | 5.7 | 1.0 | 2,852 |
| Sweden | 27.2 | 35.5 | 26.7 | 8.3 | 2.3 | 2,989 |
| Belgium | 18.5 | 48.6 | 25.0 | 6.3 | 1.6 | 3,609 |
| Greece | 22.3 | 39.1 | 30.2 | 6.4 | 2.0 | 2,656 |
| Austria | 17.2 | 43.4 | 29.5 | 7.6 | 2.3 | 1,843 |
| France | 13.2 | 47.7 | 29.1 | 7.7 | 2.3 | 2,964 |
| Germany | 10.8 | 42.5 | 32.3 | 11.7 | 2.7 | 2,927 |
| Italy | 8.2 | 39.9 | 38.4 | 11.2 | 2.3 | 2,499 |
| Spain | 10.1 | 40.3 | 32.5 | 13.4 | 3.7 | 2,326 |
| Total | 13.0 | 43.0 | 31.6 | 10.0 | 2.4 | 27,215 |
Based on weighted data
Sampling strategies vary across countries, depended on the available means for constructing sampling frames. In Sweden and Denmark, stratified simple random sampling was used based on national population registers. In Germany, Italy, Spain, France and The Netherlands, multi-stage sampling was involved, using regional or local population registers. Finally, in Austria, Greece, Switzerland and Belgium single or multi-stage sampling using telephone directories as sampling frame was carried out (Klevmarken et al. 2005).
The average household response rate was 60.6%, ranging from 38.8% for Switzerland and 47.3% for Sweden to around 60–63% for Germany, Denmark, Greece and The Netherlands and to 79.2% for France (SHARE 2008). These rates are fairly similar or higher in some instances to the rates achieved in other European surveys carried out in the period 1994–2004, such as the European Community Household Panel, the European Labour Force Survey, the European Social Survey etc. (De Luca and Peracchi 2005). The average individual response rate—computed as the ratio of interviewed individuals over the number of eligible persons in the household (i.e. members aged 50 or higher as well as the spouse of the first respondent irrespectively of age)—was 85.0%; for the different countries the rates ranged from 73.7% (Spain) to 93.0% (Denmark).
Measures
Self-rated health
The respondents at the survey were asked to assess their health status answering the following question: “Would you say your health is: very good, good, fair, bad, very bad”. This question is termed “the European version” of self-rated health. There is a US version as well, also with five possible answers, ranging from “excellent” to “poor”. However, the “European” version has been recommended for use among European populations (WHO 1996; Murray et al. 2002; Robine et al. 2003) while there are studies indicating that both versions represent parallel assessments of health (Jürges et al. 2007). Thus, there is ample justification for using the European version in the analysis.
The weighted distribution of the answers to this question, for all 11 countries, is heavily skewed towards the upper part of the scale, denoting at least fair health (Table 1). Proportions of respondents reporting very bad health are very small, ranging from 0.6% in Switzerland to 3.7% in Spain. Hence, for the purposes of the analysis these respondents were grouped together with those whose health was “bad” and are being referred to as having “poor” health, henceforth.
Socio-demographic variables
Age, measured in completed years, and gender are the demographic variables used in the models. Socio-economic status is represented in SHARE by several indicators: educational attainment, household income, household net wealth and current and last occupation. The latter was disregarded, as its relevance in a sample where retirees and homemakers constitute the majority is questionable (Grundy and Holt 2001). In the present study SES is represented by years in education, household income and household net wealth. Years in education are defined according to the highest qualification attained based on ISCED-97 coding (International Standard Classification of Education) (UNESCO 2006). The variables corresponding to finances are purchasing-power-parity adjusted using PPPs, i.e. rates of currency conversion that eliminate differences in price levels between countries, improving thus cross-country comparability. The adjustment was carried out by the SHARE team based on the OECD relevant figures (Paccagnella and Weber 2005). Household income includes the income of all household members in 2003. Household net wealth is a composite measure, calculated as the sum of a large number of items, including assets, mortgages, bank deposits, stock holdings, bonds, mutual funds, life insurance policies and individual retirement accounts. As for some of these items, in particular savings accounts, stock and shares, non-response was fairly high, 5–14% (Kalwij and van Soest 2005) the resulting variable is based both on reported and imputed values, estimated centrally by the SHARE team (Paccagnella and Weber 2005). Household income and household net wealth are introduced in the models in binary form; the respective variables denote whether a person’s income or net wealth is above the corresponding median for the total of the observations (Table 2).
Table 2.
Descriptive statistics for demographic and socio-economic variables used in the analysis by country
| Country | Mean age | 50–64 | 65–79 | 80 or more | Female | Mean years in education | Median household incomea | Income above medianb | Median household net wealtha | Wealth above medianb |
|---|---|---|---|---|---|---|---|---|---|---|
| Switzerland | 64.5 | 0.55 | 0.35 | 0.10 | 0.54 | 12.18 | 42,080 | 0.62 | 240,557 | 0.60 |
| Denmark | 64.5 | 0.58 | 0.31 | 0.11 | 0.53 | 12.80 | 36,171 | 0.58 | 164,230 | 0.48 |
| Netherlands | 64.3 | 0.57 | 0.32 | 0.11 | 0.53 | 11.00 | 36,758 | 0.60 | 150,648 | 0.47 |
| Sweden | 66.0 | 0.51 | 0.34 | 0.15 | 0.53 | 10.25 | 34,716 | 0.58 | 104,559 | 0.35 |
| Belgium | 65.8 | 0.49 | 0.38 | 0.12 | 0.54 | 10.28 | 27,438 | 0.48 | 241,284 | 0.63 |
| Greece | 65.5 | 0.50 | 0.40 | 0.10 | 0.54 | 8.41 | 15,487 | 0.25 | 128,275 | 0.38 |
| Austria | 65.1 | 0.53 | 0.37 | 0.10 | 0.56 | 11.40 | 29,181 | 0.50 | 127,405 | 0.41 |
| France | 65.8 | 0.51 | 0.35 | 0.14 | 0.55 | 8.50 | 28,995 | 0.49 | 219,701 | 0.57 |
| Germany | 65.3 | 0.50 | 0.38 | 0.11 | 0.55 | 13.36 | 29,895 | 0.51 | 126,334 | 0.42 |
| Italy | 65.8 | 0.50 | 0.38 | 0.12 | 0.55 | 7.18 | 23,367 | 0.39 | 159,856 | 0.48 |
| Spain | 66.3 | 0.47 | 0.39 | 0.14 | 0.54 | 5.65 | 16,333 | 0.29 | 170,130 | 0.49 |
| Total | 65.6 | 0.51 | 0.37 | 0.12 | 0.55 | 9.65 | 25,987 | 0.50 | 162,701 | 0.50 |
Based on weighted data
aFigures are in Euros and are purchasing-power-parity adjusted
bProportion of persons having income or wealth above the median of the whole sample
Health indicators
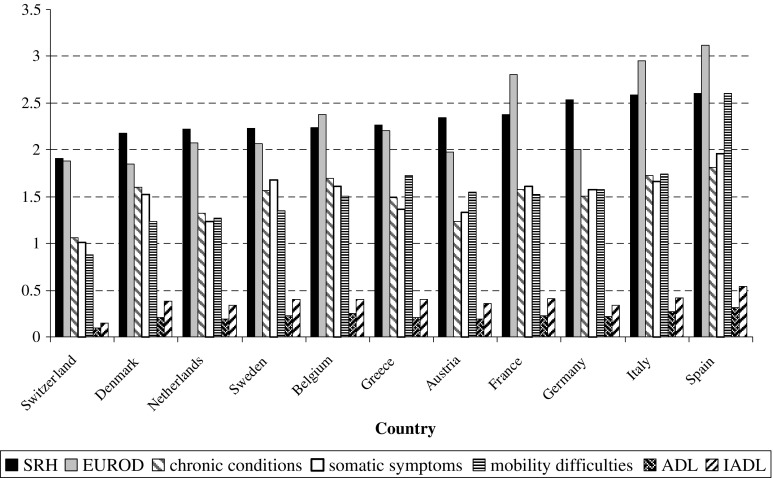
SHARE includes information on a number of health indicators. The respondents were asked whether they had a chronic disease diagnosed in their life-time out of a list of 14 specific conditions, whether they had experienced limitations in 6 activities of daily living or self-care activities (ADLs) (Katz et al. 1963, 1970; Katz 1983) and 7 instrumental activities of daily living or activities necessary for independent living in a community (IADLs) (Lawton and Brody 1969). They also reported whether they had difficulties performing any out of 10 activities related to stamina, strength, arm and fine motor function (mobility) (Fonda and Herzog 2004), and whether they had experienced, for at least a 6-month period, any of 11 somatic symptoms (Nicholas et al. 2003). Finally, their mental health status was assessed on the basis of 12 symptoms of depression (EURO-D) (Prince et al. 1999a). The variables used in the analysis represent the number of chronic conditions, of mobility difficulties, and of somatic and depressive symptoms the respondents reported. For the ADLs and the IADLs, where frequencies are small (see Fig. 1), a binary indicator was used which denotes the presence or absence of at least one such limitation. A list of the items (limitations, symptoms and conditions) comprising the aforementioned health measures is included in the Appendix.
Fig. 1.
Means (based on weighted data) for self-rated health (SRH) and objective health indicators by country
Behavioural risk factors
Risky health behaviours include, among others, smoking habits, being overweight or obese and physical inactivity. The relevant information derived from SHARE and used in the analysis deals with whether a respondent has been a smoker, his body mass index (based on the reported height and weight) and the frequency of doing some moderate or vigorous physical activities. Smoking in the models is represented by a three category variable distinguishing between individuals who are currently smoking, those who were smokers for at least a year but have stopped now and those who have never smoked in their lifetime. With respect to a person’s BMI a binary variable indicating obesity was employed (BMI ≥ 30). Finally, a variable denoting whether a person is hardly ever physically active (=0) or does on a regular basis some activities requiring at least moderate levels of physical effort (=1) such as gardening, cleaning the car etc., is used.
Statistical analysis
Descriptive statistics presented in the paper are based on weighted numbers. The weights adjust for non-response up to a point as they are calibrated, using the age and sex distribution of the population aged 50 and higher in each country (Klevmarken et al. 2005).
The importance of factors associated with SRH was assessed using multinomial logistic regression techniques. An advantage of the technique is that the estimated relative risk ratios (RRRs) compare separately persons having good, fair and poor health to those reporting very good SRH (reference category). Use of logistic regression was abandoned on the grounds that a binary variant of SRH would mean unnecessary loss of information. Use of ordinal regression, on the other hand, might have been suitable since SRH is a categorical variable of ordinal nature. However, that approach was not pursued as none of the available link functions (logit, probit, negative log–log and complementary log–log) were truly appropriate; even when such analysis was attempted the test of parallel lines failed. Hence, multinomial logistic regression was deemed the most appropriate technique to perform the present analysis (Chan 2005). The models were run for each country separately; the goodness of fit was evaluated on the basis of Pearson’s Chi-square and of the Deviance tests.
Subsequently, the homogeneity/non-homogeneity of the regression coefficients across countries for each predictor was tested using Dyer’s approach (Dyer 1986; Noale et al. 2005). More specifically, for each variable in the model, the coefficients were weighted by the inverse of their variance and were summed up, constructing thus a pooled estimate. Then, the hypothesis of homogeneity (i.e. that for each predictor, coefficients are equal across countries) was assessed at the 0.01 level, using a Chi-square test. The choice of the level was made on the grounds that as socio-economic factors are based both on observed and imputed values, greater flexibility should be allowed than would be granted based on the more stringent 0.05 level. All analyses were carried out using STATA 10.0.
Results
Descriptive findings
In Table 1 the weighted percentage distribution of the respondents by reported level of SRH is presented for all countries; unweighted sample sizes are also shown. The sequence of the countries in all tables is related to their mean SRH scores (see Fig. 1) starting on top with the lowest score (best health). The vast majority of the respondents report having very good, good or fair health; proportions reporting bad and very bad health are very small. The distribution of SRH differentiates quite substantially between countries. For instance, 32.5% of Swiss persons report having very good health compared to only 8.2% of the Italians. Comparing the figures it seems that the Swiss, the Danes and the Swedish have the best SRH while the Italians and the Spanish have the worst.
Table 2 shows means for selected socio-demographic variables used in the analysis, based on weighted data. Mean age of the respondents is lowest for The Netherlands (64.3 years) and highest for Spain (66.3 years); the mean for all persons is 65.6 years. The distribution of the respondents in broad age groups shows that 85–90% of them are below age 80. Proportions of females differ only very slightly between the 11 countries, ranging from 53% (Sweden, The Netherlands, Denmark) to 56% (Austria). According to years in education, the most educated Europeans over 50 seem to be the Germans with 13.4 years of schooling on average; they are followed closely by the Danes (12.8 years) and the Swiss (12.2 years). By contrast, respondents who reside in Southern Europe are characterized by lower educational attainment (5.7 years in Spain and 7.2 years in Italy).
A substantial divide between southern and the rest of Europe exists also with respect to financial resources. Italy and, in particular, Greece and Spain have median household incomes well below the median for the whole of the sample. In comparison, median income in Switzerland, The Netherlands, Denmark and Sweden is high. Medians for household net wealth, on the other hand, present a somewhat different picture to income, revealing differential tendencies across countries in the accumulation of resources over the life course. Sweden now has the lowest median while the highest is found in Belgium and Switzerland.
Comparing, across countries, means for the various health measures used in the analysis, it appears that ranking based on “subjective” (SRH) and “objective” indicators does not necessarily coincide (Fig. 1). It seems that the healthiest population in nearly all respects resides in Switzerland while the least healthy resides in Spain. The Netherlands, Germany, Austria and Denmark also seem to have healthier than average populations, if all indicators apart from SRH are considered.
Regarding smoking behaviour there does not seem to be a clear split between countries (Table 3). Proportions of smokers are highest in Denmark, The Netherlands and Greece (24–31%) while for non-smokers the highest percentages are found in Austria, Spain and France (59–63%). High proportions of ex-smokers reside in The Netherlands, Sweden and Denmark (33–37%). Obesity seems least prevalent in Northern European countries and Switzerland where also the highest levels of physical activity can be observed. Relatively high proportions of obese persons can be found in Greece, Austria and Spain while Italians seem to have the lowest levels of physical activity followed by Austrians and French.
Table 3.
Means for behavioural risk factors used in the analysis by country
| Country | Currently smoking | Ex-smoker | Never smoked | Obese | Low levels of activity |
|---|---|---|---|---|---|
| Switzerland | 0.20 | 0.24 | 0.56 | 0.13 | 0.13 |
| Denmark | 0.31 | 0.33 | 0.36 | 0.14 | 0.15 |
| Netherlands | 0.24 | 0.37 | 0.39 | 0.15 | 0.17 |
| Sweden | 0.17 | 0.37 | 0.46 | 0.14 | 0.15 |
| Belgium | 0.17 | 0.31 | 0.52 | 0.18 | 0.27 |
| Greece | 0.25 | 0.18 | 0.57 | 0.19 | 0.25 |
| Austria | 0.19 | 0.18 | 0.63 | 0.19 | 0.30 |
| France | 0.14 | 0.27 | 0.59 | 0.15 | 0.30 |
| Germany | 0.18 | 0.25 | 0.57 | 0.17 | 0.20 |
| Italy | 0.18 | 0.26 | 0.56 | 0.17 | 0.35 |
| Spain | 0.17 | 0.21 | 0.62 | 0.23 | 0.24 |
| Total | 0.18 | 0.26 | 0.56 | 0.17 | 0.26 |
Based on weighted data
Multinomial logistic regression models
In Table 4, Relative Risk Ratios (RRRs) are presented for socio-demographic variables and behavioural risk factors for the countries under study, derived using multinomial logistic regression. The results are shown separately for persons having good, fair and poor health in comparison to very good health (reference category). In the bottom of the table, Dyer’s chi-square test values (1986) are presented for each predictor separately, regarding whether coefficients are homogeneous across countries.
Table 4.
Relative Risk Ratios based on multinomial logistic regression, full model, socio-demographic and behavioural risk factors
| Country | Level of SRH | Demographic characteristics | Socio-economic level | Behavioural risk factors | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age in years | Female | Years in education | Income > median | Wealth > median | Smoking (ref: smoker) | BMI (ref: BMI < 30) | Level of activity (ref: med-high) | |||
| Ex-smoker | Never smoked | Obese | Low | |||||||
| Ref: Very good SRH | ||||||||||
| Switzerland | Good | 1.017* | 0.691** | 0.943*** | 0.830 | 0.711* | 0.436*** | 0.676* | 2.549*** | 1.046 |
| Fair | 0.998 | 0.528** | 0.937** | 0.681 | 0.707 | 0.418** | 0.779 | 2.987*** | 1.884* | |
| Poor | 0.944** | 0.571 | 0.987 | 0.466 | 0.399 | 0.386 | 0.334* | 1.315 | 2.372 | |
| Denmark | Good | 0.995 | 0.678*** | 0.925*** | 0.801 | 0.966 | 0.861 | 0.650** | 1.261 | 1.587 |
| Fair | 0.986 | 0.478*** | 0.902*** | 0.597** | 0.841 | 0.666* | 0.636** | 1.713* | 2.401** | |
| Poor | 0.946*** | 0.393*** | 0.939 | 0.701 | 0.964 | 0.574 | 0.551* | 1.410 | 3.567*** | |
| Netherlands | Good | 0.999 | 0.877 | 0.942*** | 0.909 | 1.022 | 0.629*** | 0.762* | 1.552** | 1.665** |
| Fair | 1.000 | 0.526*** | 0.922*** | 0.872 | 0.799 | 0.543*** | 0.687* | 1.568* | 2.894*** | |
| Poor | 0.978* | 0.234*** | 0.941 | 0.686 | 0.499** | 0.461** | 0.547* | 1.310 | 5.798*** | |
| Sweden | Good | 1.010 | 0.781** | 0.899*** | 0.970 | 0.853 | 0.664*** | 0.680** | 0.911 | 1.542* |
| Fair | 1.002 | 0.673*** | 0.865*** | 0.907 | 0.813 | 0.665** | 0.661** | 1.043 | 2.014*** | |
| Poor | 0.955*** | 0.412*** | 0.891*** | 0.841 | 0.707 | 0.469*** | 0.354*** | 1.147 | 4.627*** | |
| Belgium | Good | 1.013** | 0.790** | 0.956*** | 0.948 | 0.968 | 0.939 | 1.039 | 1.432** | 1.033 |
| Fair | 1.006 | 0.488*** | 0.903*** | 0.803* | 0.863 | 1.035 | 1.058 | 1.228 | 1.725*** | |
| Poor | 0.970*** | 0.255*** | 0.902*** | 0.766 | 0.652** | 1.536 | 1.110 | 1.028 | 3.345*** | |
| Greece | Good | 1.027*** | 1.188 | 0.970** | 0.821 | 1.177 | 1.209 | 1.190 | 1.097 | 1.542*** |
| Fair | 1.040*** | 1.055 | 0.907*** | 0.946 | 1.010 | 1.446 | 1.157 | 1.174 | 1.888*** | |
| Poor | 1.017 | 0.625* | 0.862*** | 0.681 | 0.920 | 1.395 | 0.842 | 1.014 | 3.215*** | |
| Austria | Good | 1.020** | 0.882 | 0.967 | 0.940 | 1.210 | 0.653* | 0.934 | 1.393 | 1.399 |
| Fair | 1.039*** | 0.471*** | 0.909*** | 0.819 | 1.050 | 0.563* | 1.129 | 2.540*** | 2.108*** | |
| Poor | 1.021 | 0.320*** | 0.889** | 0.921 | 0.724 | 0.315*** | 0.757 | 2.304** | 6.246*** | |
| France | Good | 1.018** | 0.764* | 0.927*** | 0.816 | 0.948 | 0.789 | 1.180 | 1.103 | 1.496** |
| Fair | 1.027*** | 0.332*** | 0.890*** | 0.616*** | 0.720** | 0.696 | 1.432 | 1.055 | 1.808*** | |
| Poor | 0.999 | 0.150*** | 0.863*** | 0.669* | 0.883 | 0.723 | 1.208 | 1.130 | 3.480*** | |
| Germany | Good | 1.039*** | 1.237 | 0.913*** | 1.002 | 0.826 | 0.703* | 0.802 | 1.121 | 1.809** |
| Fair | 1.047*** | 0.756 | 0.857*** | 0.632*** | 0.781 | 0.592** | 0.745 | 1.363 | 2.034** | |
| Poor | 1.039*** | 0.395*** | 0.832*** | 0.467*** | 1.053 | 0.752 | 0.863 | 1.591 | 4.992*** | |
| Italy | Good | 1.012 | 1.364* | 0.946*** | 1.030 | 0.824 | 1.018 | 1.259 | 1.144 | 1.280 |
| Fair | 1.020* | 1.028 | 0.886*** | 0.914 | 0.698* | 1.141 | 1.671** | 1.349 | 2.242*** | |
| Poor | 1.015 | 0.507*** | 0.866*** | 0.688 | 0.772 | 0.709 | 1.286 | 1.352 | 4.438*** | |
| Spain | Good | 1.002 | 0.798 | 0.953** | 0.998 | 1.016 | 1.338 | 1.281 | 0.946 | 1.504* |
| Fair | 1.011 | 0.584** | 0.927*** | 1.026 | 0.935 | 1.749* | 1.818** | 1.171 | 1.868** | |
| Poor | 1.007 | 0.397*** | 0.935** | 0.974 | 0.735 | 1.488 | 1.538 | 1.049 | 3.429*** | |
| Chi-square test of homogeneity | Good | 20.313a | 23.357a | 19.501 | 4.602 | 12.711 | 40.707a | 27.093a | 6.616 | 5.127 |
| Fair | 35.256a | 108.328a | 14.129 | 18.881 | 7.528 | 31.666a | 23.526a | 3.957 | 0.684 | |
| Poor | 52.725a | 354.058a | 19.510 | 20.028 | 19.413 | 34.515a | 48.038a | 2.090 | 0.358 | |
a The hypothesis of the homogeneity of the country-specific coefficients is rejected (at the 0.01 level, 10 df)
* p < 0.1, ** p < 0.05, *** p < 0.01
In countries where SRH is better on average (Switzerland, Denmark, The Netherlands, Sweden and Belgium) associations with age are rather weak, with the exception of poor health; for the latter increasing age is related to lower chances of ill-health. A different pattern can be observed for all other countries, where increasing age is related to worse health; coefficients are not significant for Italy and Spain. The chi-square test also suggests that age has a non-homogeneous effect across countries. With respect to gender, RRRs indicate that women in nearly all countries report significantly better health than men. The difference is quite marked; in most instances, women have about 50–80% lower chances than men to report poor as opposed to very good SRH. Only in a few cases coefficients point to the opposite direction but they are non-significant. Again, according to the chi-square test, effects of gender on SRH are non-homogeneous.
Among SES indicators, years in education has the strongest association with SRH, significant at the 1% level in most instances. Income and wealth, on the other hand, are significant only for a few countries: Denmark, The Netherlands, Belgium, France and Germany. Coefficients in all cases, however, point to the same direction; having income or net wealth above the median reduces chances of reporting poor, fair or good as opposed to very good health. The effects of all SES predictors are homogeneous across countries and across levels of SRH.
Regarding behavioural risk factors, the association of smoking with SRH appears inconsistent. It seems that countries can be divided into two groups. Non-smokers in the Scandinavian countries, Switzerland, The Netherlands, Austria and Germany have significantly lower chances of reporting ill-health compared to smokers. In contrast, in Belgium, France and the countries of southern Europe associations point to the opposite direction though most are not significant. The chi-square test also indicates lack of homogeneity across populations. Coefficients for obesity and low levels of physical activity, on the other hand, are homogeneous. Both predictors are related to worse health though RRRs for obesity are significant only for Switzerland, The Netherlands and Austria. For levels of physical activity the ratios are very significant in most counties; the impact seems very pronounced for fair and particularly, for poor health.
Table 5 shows RRRs for the health indicators included in the analysis. EUROD (number of depressive symptoms), an important component of “true” health, is very significant, particularly with respect to fair and poor health; each additional symptom of depression increases the relative risk of reporting fair as opposed to very good health by 16% (Spain) to 42% (Austria) while it increases chances of reporting poor health by 33% (Spain) to 70% (Denmark). All indicators of physical health are also of great consequence. Overall, the number of chronic conditions seems to have a more considerable impact on SRH than the number of somatic symptoms and of mobility difficulties in most countries. By contrast, reporting at least one ADL limitation is not significantly related to SRH while reporting at least one IADL limitation is very significant in Sweden and, for poor health only, in Switzerland, Denmark, Belgium and Germany. Hence, though most health measures have a very strong association with SRH that is not the case for ADL and IADL difficulties. Nevertheless, associations with all health indicators are homogeneous across countries for all three levels of SRH. Homogeneity (Tables 4, 5) has been assessed at the 0.01 level; had the more stringent 0.05 level been used, results would have remained the same for all predictors apart from socio-economic factors (which are based both on observed and imputed values) where the test would have provided contrasting indications.
Table 5.
Relative risk ratios based on multinomial logistic regression, full model, objective health indicators
| Country | Level of SRH | EUROD | Chronic diseases | Somatic symptoms | Mobility difficulties | At least 1 ADL limitation | At least 1 IADL limitation |
|---|---|---|---|---|---|---|---|
| Ref: Very good SRH | |||||||
| Switzerland | Good | 1.132** | 1.486*** | 1.438*** | 1.257* | 1.674 | 1.182 |
| Fair | 1.322*** | 2.028*** | 1.961*** | 1.841*** | 5.611** | 1.012 | |
| Poor | 1.326** | 2.873*** | 2.060*** | 2.055*** | 2.803 | 6.393** | |
| Denmark | Good | 1.147*** | 1.378*** | 1.430*** | 1.813*** | 1.341 | 1.847 |
| Fair | 1.312*** | 1.917*** | 1.780*** | 2.538*** | 1.110 | 2.228* | |
| Poor | 1.702*** | 2.283*** | 1.958*** | 3.171*** | 1.358 | 3.086** | |
| Netherlands | Good | 1.067* | 1.822*** | 1.254*** | 1.590*** | 2.087 | 1.047 |
| Fair | 1.223*** | 2.911*** | 1.594*** | 2.053*** | 2.053 | 2.143 | |
| Poor | 1.365*** | 3.420*** | 1.679*** | 2.746*** | 2.746 | 1.706 | |
| Sweden | Good | 1.111*** | 1.631*** | 1.398*** | 1.446*** | 1.617 | 2.082** |
| Fair | 1.293*** | 1.930*** | 1.697*** | 1.765*** | 1.478 | 2.857*** | |
| Poor | 1.425*** | 2.483*** | 2.108*** | 2.150*** | 1.615 | 5.218*** | |
| Belgium | Good | 1.090*** | 1.528*** | 1.389*** | 1.230*** | 1.301 | 1.178 |
| Fair | 1.261*** | 2.111*** | 1.883*** | 1.529*** | 1.240 | 1.408 | |
| Poor | 1.475*** | 2.526*** | 2.026*** | 1.909*** | 1.735 | 2.444*** | |
| Greece | Good | 1.054 | 2.194*** | 1.469*** | 1.311*** | 1.347 | 0.641* |
| Fair | 1.227*** | 3.744*** | 1.756*** | 1.449*** | 1.378 | 0.789 | |
| Poor | 1.587*** | 4.843*** | 1.612*** | 1.905*** | 2.316 | 1.171 | |
| Austria | Good | 1.123** | 2.165*** | 1.164 | 1.607*** | 0.387* | 0.653* |
| Fair | 1.425*** | 3.146*** | 1.409*** | 2.112*** | 0.501 | 1.012 | |
| Poor | 1.666*** | 3.214*** | 1.587*** | 2.613*** | 1.164 | 1.163 | |
| France | Good | 1.112*** | 1.795*** | 1.210** | 1.402*** | 0.485* | 0.944 |
| Fair | 1.261*** | 2.495*** | 1.531*** | 1.859*** | 0.601 | 1.039 | |
| Poor | 1.556*** | 2.896*** | 1.652*** | 2.063*** | 0.890 | 1.950 | |
| Germany | Good | 0.995 | 2.132*** | 1.619*** | 1.405** | 1.046 | 1.034 |
| Fair | 1.237*** | 3.621*** | 1.908*** | 1.983*** | 1.468 | 1.391 | |
| Poor | 1.617*** | 3.751*** | 2.178*** | 2.313*** | 2.763 | 2.308* | |
| Italy | Good | 1.043 | 1.712*** | 1.238* | 1.360** | 1.643 | 0.515 |
| Fair | 1.160*** | 2.564*** | 1.512*** | 1.663*** | 3.016 | 0.889 | |
| Poor | 1.353*** | 3.543*** | 1.549*** | 1.938*** | 5.809* | 1.711 | |
| Spain | Good | 0.979 | 1.709*** | 1.387*** | 1.414*** | 2.867 | 0.607 |
| Fair | 1.156*** | 2.423*** | 1.785*** | 1.692*** | 2.256 | 0.794 | |
| Poor | 1.325*** | 2.542*** | 1.952*** | 2.038*** | 2.299 | 0.972 | |
| Chi-square test of homogeneitya | Good | 10.777 | 10.231 | 6.101 | 5.917 | 13.810 | 13.064 |
| Fair | 7.182 | 8.640 | 4.021 | 6.938 | 6.916 | 5.638 | |
| Poor | 8.744 | 3.295 | 4.099 | 2.950 | 1.741 | 3.055 | |
aIn this instance, coefficients of all variables are homogeneous across countries (the hypothesis of homogeneity is not rejected at the 0.01 level with 10 df)
* p < 0.1, ** p < 0.05, *** p < 0.01
Discussion
In this paper, multinomial regression models are used to explore associations of socio-demographic factors, health indicators and health related behaviour with SRH in 11 European populations, using data from the SHARE study (release 2). Key components among these factors are identified and assessed for homogeneity across countries. The study contributes to the scarcely explored area of cross-national differentials among older persons in the reporting of SRH. An advantage of this analysis is that information is comparable across countries due to the design of SHARE; in addition there is an extensive number of available covariates. It has been suggested, however, that testing a multitude of associations in epidemiological research may lead to false positive results (Ioannidis 2005; Boffetta et al. 2008). On the other hand, the cross-national comparative nature of the present study ensures that the analysis is replicated several times and hence, associations are re-evaluated; homogeneity of findings across countries assures reliability of the results.
Proportions of persons reporting very good, good, fair or poor SRH differ between countries. This is a common finding (Zimmer et al. 2000; Bardage et al. 2005) probably partly related to the multidimensional nature of SRH which is a measure affected by true health as well as perceptions and reporting style. Jürges (2007) using SHARE data (release 1) on 22,731 individuals and ten countries concludes that Danish and Swedish, who have among the best SRH scores, over-rate their health, Greeks report fairly accurately, while the rest and particularly the Germans, underrate it. He also suggests that even taking into account differences in the reporting style, variations in SRH are reduced but not eliminated. However, marked differentiation in SRH levels between countries may also be related, up to an extent, to substantial differences in response rates. For instance, in countries where response rates are low, such as Switzerland (39%) and Sweden (47%), persons having participated at the survey may be biased towards better health and perhaps higher SES, too.
The findings of the study indicate that associations of demographic factors with SRH vary across countries. In Germany, Austria, Greece and France increasing age is significantly related to worse health, in Italy and Spain there is no substantial association while for the remainder of the countries being older is related to lower chances of reporting poor health. Results of other studies also show divergent effects. Van Doorslaer and Gerdtham (2003) suggest that, among persons aged 20–84 in Sweden older individuals are more likely to report better health than younger ones due to a more stringent view on health status on the part of the latter. Similar results were found among Canadians aged 20–70 (Lindeboom and Van Doorslaer 2004). Ongaro and Salvini (1995) having controlled for “true” health status and other socio-demographic characteristics among Italians aged 65 or more, conclude that age has no influence on the perceptions of a person on his health condition. Similarly, Kivinen et al. (1998) found an absence of an age gradient among Finnish males aged 70–89. Bardage et al. (2005) conclude that among older adults increasing age was associated with worse health in The Netherlands and Spain but associations were weak in Finland and Sweden. Hence, the results of the present analysis, revealing a lack of homogeneity across countries, are in accordance with the findings of the aforementioned studies which also indicate divergent associations.
Regarding gender, it has been consistently found that although females experience lower mortality they have higher morbidity rates than men (Lahelma et al. 1999) and suffer more from depression (Prince et al. 1999b; Verropoulou and Tsimbos 2007) and disabilities (Hsu 2005). The present study shows that when health status has been taken into account women report significantly better health than men in nearly all countries. Associations, however, are inconsistent for Greece, Italy and Germany even thought coefficients are non-significant. Better SRH among women has also been noted by Arber and Cooper (1999), who label it “the new paradox” and by Lindeboom and Van Doorslaer (2004). However, it contrasts with the findings of Bardage et al. (2005) who find women reporting worse SRH than men in Sweden, The Netherlands and Spain. Thus, the heterogeneity across countries demonstrated by the present analysis is also reflected in the relevant literature.
Socio-economic status, here represented by years in education, household income and household net wealth, has a homogeneous effect across countries. Education in particular has a very significant impact in all instances, reducing chances of less than good SRH. Income and wealth, on the other hand are mostly non-significant though associations point to the expected direction. The SES gradient is a well established fact in the international literature (Mackenbach et al. 1997; Idler et al. 1999; Huisman et al. 2003; Kunst et al. 2005) while the importance of education as indicator among older persons has been demonstrated before (Grundy and Holt 2001; Van Ourti 2003; D’Uva et al. 2008). Strong associations between SES and SRH have been found in Asian populations (Zimmer et al. 2000) though other studies suggest that the impact of education weakens when health indicators are included in the analysis (Bardage et al. 2005; Lindeboom and Van Doorslaer 2004).
Health indicators also have a consistent effect across the populations under study. Chronic conditions have the strongest association, followed by mobility difficulties and then by somatic and depressive symptoms. Depression, rarely used in most similar analyses, has a strong and significant effect, especially pronounced among persons reporting poor health. The importance of depression as a predictor of SRH is also stressed by Kivinen et al. (1998). ADLs and, for certain countries IADLs as well, were not significantly associated with SRH in the present study. This is also in accordance with the results of Kivinen et al. (1998) who find that ADL limitations were the strongest predictor of depression, which was the strongest determinant of SRH. By contrast, Bardage et al. (2005) suggest that ADLs are a significant predictor; their models, however, did not include depression or other indicators of mobility difficulties as the present study does.
Regarding risky health behaviours, a low level of physical activity is a strong predictor of fair and poor SRH in all countries. Obesity also increases chances of ill-health but only in Switzerland, Austria, The Netherlands and Belgium associations are strong. Effects of low levels of physical activity and obesity are homogeneous across countries; however, this is not the case for smoking. In Scandinavian countries and most countries of central Europe non-smokers report significantly better health; the opposite is true for southern Europe and Belgium, though most associations are not significant. It has been suggested that European countries are at different stages of the so called “smoking epidemic” (Huisman et al. 2005; Mackenbach et al. 2008) and while smokers in northern Europe tend to have lower SES the opposite holds in countries of southern Europe.
To summarise, the findings of the present study indicate that associations of health measures, SES indicators and behavioural risk factors (with the exception of smoking) with SRH are homogeneous across countries. By contrast, age and gender have differential effects. Among the measures considered in the analysis the most significant predictors of SRH are health indicators (chronic conditions, depression, somatic symptoms and mobility difficulties), SES (educational attainment) and levels of physical activity.
Some limitations of the study should be considered. As the institutionalised population is excluded from the design of SHARE, prevalence of ill-health may have been underestimated, particularly among persons aged 80 or higher (who constitute 12% of the sample). According to Statistics Netherlands (2004) in 2003 the proportion of 80+ year olds living in old age and nursing homes in The Netherlands was 18% compared to 17.5% for France and 13% among the 75+ year olds in Belgium in 2000 (Van Oyen 2001). Within Europe there is also a north–south gradient with a smaller proportion of institutionalised population in southern European countries (Delbès et al. 2006). According to the 2001 Greek census, the proportion of persons over age 80 living in collective households was 3.2% (NSSG 2004). Hence, the extent of underestimation may be greater in northern Europe. Nevertheless, such underreporting would affect not only SRH but also the other health indicators and its overall impact is likely to be slight.
Another possible limitation is that all variables on health status are based on the respondents’ reporting. Hence, data on the number of chronic diseases, mobility difficulties and number of symptoms, which are taken here to reflect “true” health status, may not be entirely accurate. Finally, a methodological issue stems from the nature of the available data that are cross-sectional and do not allow inference of causality. The analysis, for instance, does not answer questions on whether low levels of physical activity are a cause or a consequence of poor health. Nevertheless, an important strength of the study is the comparability of data across countries due to the stringent standard procedures and protocols followed throughout questionnaire design and data collection.
The predictive value of SRH for mortality and morbidity is well documented and the higher risks for persons with poor self-rated health have been quantified (Appels et al. 1996; Idler and Benyamini 1997; Van Doorslaer and Gerdtham 2003; DeSalvo et al. 2005). SRH has the advantage that it is a simple measure, included in most surveys, while accurate morbidity data are hard to collect (Macintryre et al. 2005). Hence, unravelling the dimensions encompassed in this indicator in addition to exploring and validating associations across countries is of great value (Quesnel-Valée 2007). The present study has demonstrated the importance of health indicators, educational attainment and levels of activity as components of SRH among older persons and their homogeneous effects across northern, central and southern Europe. The divergent associations with age and gender found here reconfirm results of previous research and highlight the necessity of using such controls in similar analyses. Finally, a northern–southern divide regarding smoking has been demonstrated. Further progress would require availability of longitudinal data, to better assess causality and to link SRH to mortality of persons in the study.
Acknowledgments
The author is thankful to two anonymous referees for their constructive and helpful criticism. This paper uses data from release 2 of SHARE 2004. The SHARE data collection has been primarily funded by the European Commission through the 5th framework programme (project QLK6-CT-2001-00360 in the thematic programme Quality of Life). Additional funding came from the US National Institute on Ageing (U01 AG09740-13S2, P01 AG005842, P01 AG08291, P30 AG12815, Y1-AG-4553-01 and OGHA 04-064). Data collection in Austria (through the Austrian Science Foundation, FWF), Belgium (through the Belgian Science Policy Office) and Switzerland (through BBW/OFES/UFES) was nationally funded. The SHARE data collection in Israel was funded by the US National Institute on Aging (R21 AG025169), by the German–Israeli Foundation for Scientific Research and Development (G.I·F.), and by the National Insurance Institute of Israel. Further support by the European Commission through the 6th framework program (projects SHARE-I3, RII-CT-2006-062193, and COMPARE, CIT5-CT-2005-028857) is gratefully acknowledged. For details see Börsch-Supan et al. (2005a).
Appendix: Questions and items comprising various health indicators
Mobility difficulties
Because of a physical or health problem, do you have difficulty doing any of the activities on this card? Exclude any difficulties you expect to last less than three months.
Walking 100 m
Sitting for about 2 h
Getting up from a chair after sitting for long periods
Climbing several flights of stairs without resting
Climbing one flight of stairs without resting
Stooping, kneeling, or crouching
Reaching or extending your arms above shoulder level (either arm)
Pulling or pushing large objects like a living room chair
Lifting or carrying weights over 5 kilos, like a heavy bag of groceries
Picking up a small coin from a table
ADL (activities of daily living)
Here are a few more everyday activities. Please tell me if you have any difficulty with these because of a physical, mental, emotional or memory problem. Again exclude any difficulties you expect to last less than 3 months.
Dressing, including putting on shoes and socks
Walking across a room
Bathing or showering
Eating, including cutting up your food
Getting in or out of bed
Using the toilet, including getting up or down
IADL (instrumental activities of daily living)
Using a map to figure out how to get around in a strange place
Preparing a hot meal
Shopping for groceries
Making telephone calls
Taking medications
Doing work around the house or garden
Managing money, such as paying bills and keeping track of expenses
Chronic conditions
Has a doctor ever told you that you had any of the following conditions?
Heart attack including myocardial infarction or coronary thrombosis or any other heart problem including congestive heart failure
High blood pressure or hypertension
High blood cholesterol
A stroke or cerebral vascular disease
Diabetes or high blood sugar
Chronic lung disease such as chronic bronchitis or emphysema
Asthma
Arthritis, including osteoarthritis, or rheumatism
Osteoporosis
Cancer or malignant tumour, including leukaemia or lymphoma, excluding minor skin cancers
Stomach or duodenal ulcer, peptic ulcer
Parkinson disease
Cataracts
Hip fracture or femoral fracture
Other conditions, not yet mentioned
Somatic symptoms
For the past 6 months at least, have you been bothered by any of the following health conditions?
Pain in your back, knees, hips or any other joint
Heart trouble or angina, chest pain during exercise
Breathlessness, difficulty breathing
Persistent cough
Swollen legs
Sleeping problems
Falling down
Fear of falling down
Dizziness, faints or blackouts
Stomach or intestine problems, including constipation, air, diarrhoea
Incontinence or involuntary loss of urine
Other symptoms, not yet mentioned
Depressive symptoms comprising the EURO-D scale
Sadness—Depression
Pessimism
Suicidal tendency
Guilt
Trouble sleeping
Lack of Interest
Irritability
Loss of appetite
Fatigue
Lack of enjoyment
Tearfulness
Lack of concentration
References
- Angel R, Guarnaccia P. Mind, body and culture: somatization among hispanics. Soc Sci Med. 1989;28(12):1229–1238. doi: 10.1016/0277-9536(89)90341-9. [DOI] [PubMed] [Google Scholar]
- Appels A, Bosma H, Grabauskas V, Gostautas A, Sturmans F. Self-rated health and mortality in a Lithuanian and a Dutch population. Soc Sci Med. 1996;42(5):681–689. doi: 10.1016/0277-9536(95)00195-6. [DOI] [PubMed] [Google Scholar]
- Arber S, Cooper H. Gender differences in health in later life: the new paradox? Soc Sci Med. 1999;48:61–76. doi: 10.1016/S0277-9536(98)00289-5. [DOI] [PubMed] [Google Scholar]
- Bardage C, Pluijm SMF, Pedersen NL, Deeg DJH, Jylhä M, Noale M, Blumstein T, Otero A. Self-rated health among older adults: a cross-national comparison. Eur J Ageing. 2005;2:149–158. doi: 10.1007/s10433-005-0032-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron-Epel O, Kaplan G. General subjective health status or age-related subjective health status: does it make a difference? Soc Sci Med. 2001;53(10):1371–1481. doi: 10.1016/S0277-9536(00)00426-3. [DOI] [PubMed] [Google Scholar]
- Boffetta P, McLaughlin JK, La Vecchia C, Tarone RE, Lipworth L, Blot WJ. False-positive results in cancer epidemiology: a plea for epistemological modesty. J Natl Cancer Inst. 2008;100:988–995. doi: 10.1093/jnci/djn191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Börsch-Supan A, Brugiavini A, Jürges H, Mackenbach J, Siegrist J, Weber G (eds.) (2005a) Health, ageing and retirement in Europe, first results from the survey of health, ageing and retirement in Europe. Mannheim Research Institute for the Economics of Ageing (MEA), Mannheim
- Börsch-Supan A, Hank K, Jürges H. A new comprehensive and international view on ageing: introducing the “Survey of health, ageing and retirement in Europe”. Eur J Ageing. 2005;2(4):245–253. doi: 10.1007/s10433-005-0014-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burström B, Fredlund P. Self rated health: Is it as good a predictor of subsequent mortality among adults in lower as well as in higher Social classes. J Epidemiol Community Health. 2001;55(11):836–840. doi: 10.1136/jech.55.11.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan YH. Biostatistics 305. Multinomial logistic regression. Singapore Med J. 2005;46(6):259–269. [PubMed] [Google Scholar]
- D’Uva TB, O’Donnell O, van Doorslaer E. Differential health reporting by education level and its impact on the measurement of health inequalities among older Europeans. Int J Epidemiol. 2008;37:1375–1383. doi: 10.1093/ije/dyn146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Luca G, Peracchi F (2005) Survey Participation in the First Wave of SHARE. In: Börsch-Supan A, Jürges H (eds) The survey of health, ageing and retirement in Europe—methodology, Mannheim Research Institute for the Economics of Ageing (MEA), Mannheim, pp 88-101
- Delbès C, Gaymu J, Springer S (2006) Women grow old alone, but men grow old with a partner. A European overview. Population and Societies 419 INED, France
- DeSalvo KB, Bloser N, Reynolds K, He J, Munter P. Mortality prediction with a single general self-rated question: a meta analysis. J Gen Intern Med. 2005;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd JB, Zajacova A. Does the predictive power of self-rated health for subsequent mortality risk vary by socioeconomic status in the US? Int J Epidemiol. 2007;36:1214–1221. doi: 10.1093/ije/dym214. [DOI] [PubMed] [Google Scholar]
- Dyer AR. A method for combining results from several prospective epidemiological studies. Stat Med. 1986;5:303–317. doi: 10.1002/sim.4780050403. [DOI] [PubMed] [Google Scholar]
- Eriksson I, Undén AL, Elofsson S. Self-rated health. Comparisons between three different measures. Results from a population study. Int J Epidemiol. 2001;30:326–333. doi: 10.1093/ije/30.2.326. [DOI] [PubMed] [Google Scholar]
- Fonda S, Herzog A (2004) Documentation of physical functioning measured in the Health and Retirement Study and the Asset and Health Dynamics among the Oldest Old Study. HRS/AHEAD Documentation Report
- Gilmore A, McKee M, Rose R. Determinants of and inequalities in self-perceived health in Ukraine. Soc Sci Med. 2002;55:2177–2188. doi: 10.1016/S0277-9536(01)00361-6. [DOI] [PubMed] [Google Scholar]
- Grundy E, Holt G. The socioeconomic status of older adults: how should we measure it in studies of health inequalities? J Epidemiol Community Health. 2001;55(12):895–904. doi: 10.1136/jech.55.12.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu HC. Gender disparity of successful aging in Taiwan. Women Health. 2005;42:1–21. doi: 10.1300/J013v42n01_01. [DOI] [PubMed] [Google Scholar]
- Huisman M, Kunst AE, Mackenbach JP. Socio-economic inequalities in morbidity among the elderly: a European overview. Soc Sci Med. 2003;57:861–873. doi: 10.1016/S0277-9536(02)00454-9. [DOI] [PubMed] [Google Scholar]
- Huisman M, Kunst AE, Mackenbach JP. Inequalities in the prevalence of smoking in the European Union: comparing education and income. Prev Med. 2005;40:756–764. doi: 10.1016/j.ypmed.2004.09.022. [DOI] [PubMed] [Google Scholar]
- Huisman M, van Lenthe F, Mackenbach J. The predictive ability of self-assessed health for mortality in different educational groups. Int J Epidemiol. 2007;36:1207–1213. doi: 10.1093/ije/dym095. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- Idler EL, Kasl SV. Health perceptions and survival: do global evaluations of health status really predict mortality? J Gerontol. 1991;46(2):S55–S65. doi: 10.1093/geronj/46.2.s55. [DOI] [PubMed] [Google Scholar]
- Idler EL, Hudson SV, Leventhal H. The meanings of self-ratings of health: a qualitative and quantitative approach. Res Aging. 1999;21:458–476. doi: 10.1177/0164027599213006. [DOI] [Google Scholar]
- Ioannidis JPA. Why most published research findings are false. PLoS Med. 2005;2(8):696–701. doi: 10.1371/journal.pmed.0020124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jürges H. True health vs. response styles: exploring cross-country differences in self-reported health. Health Econ. 2007;16:163–178. doi: 10.1002/hec.1134. [DOI] [PubMed] [Google Scholar]
- Jürges H, Avendano M, Mackenbach J (2007) How comparable are different measures of self-rated health? Evidence from five European countries. Discussion Paper 137 Mannheim Research Institute for the Economics of Aging, Mannheim
- Kalwij A, van Soest (2005) Item non-response and alternative imputation procedures. in: Börsch-Supan A, Jürges H (eds) the Survey of Health, Ageing and Retirement in Europe—Methodology, Mannheim Research Institute for the Economics of Ageing (MEA), Mannheim, pp 128–150
- Katz S. Assessing self maintenance: activities of daily living, mobility and instrumental activities of daily living. J Am Geriatr Soc. 1983;31(12):721–726. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardised measure of biological and psychological function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. 1970;10:20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- Kivinen P, Halonen P, Evonen M, Nissinen A. Self-rated health, physician-rated health and associated factors among elderly men: the Finnish cohorts of the seven countries study. Age Ageing. 1998;27(1):41–47. doi: 10.1093/ageing/27.1.41. [DOI] [PubMed] [Google Scholar]
- Klevmarken AN, Swensson B, Hesselins P (2005) The SHARE sampling procedures and calibrated design weights. In: Börsch-Supan A, Jürges H (eds) The survey of health, ageing and retirement in Europe—methodology, Mannheim Research Institute for the Economics of Ageing (MEA), Mannheim, pp 28–37
- Kunst AE, Bos V, Lahelma E, Bartley M, Lissau I, Regitor E, Mielck A, Cardano M, Daalstra J, Geurts J, Helmert U, Lennartsson C, Ramm J, Spadea T, Stronegger W, Mackenbach J. Trends in socioeconomic inequalities in mortality in self-assessed health in 10 European countries. Int J Epidemiol. 2005;34(2):295–305. doi: 10.1093/ije/dyh342. [DOI] [PubMed] [Google Scholar]
- Lahelma E, Martikainen P, Rahkonen O, Silventoinen K. Gender differences in illhealth in Finland: patterns, magnitude and change. Soc Sci Med. 1999;48:7–19. doi: 10.1016/S0277-9536(98)00285-8. [DOI] [PubMed] [Google Scholar]
- Lahelma E, Martikainen P, Rahkonen O, Roos E, Saastamoinen P. Occupational class inequalities across key domains of health: Results from the Helsinki study. Eur J Public Health. 2005;15(5):504–510. doi: 10.1093/eurpub/cki022. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. [PubMed] [Google Scholar]
- Lindeboom M, Van Doorslaer E. Cut-point shift and index shift in self-reported health. J Health Econ. 2004;23:1083–1099. doi: 10.1016/j.jhealeco.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Macintryre S, Der G, Norrie J. Are there socioeconomic differences in responses to a commonly used self report measure of chronic illness? Int J Epidemiol. 2005;34:1284–1290. doi: 10.1093/ije/dyi200. [DOI] [PubMed] [Google Scholar]
- Mackenbach JP, Kunst AE, Cavelaars A, Groenhof F, Geurts J. Socioeconomic inequalities in morbidity and mortality in western Europe. Lancet. 1997;349:1655–1659. doi: 10.1016/S0140-6736(96)07226-1. [DOI] [PubMed] [Google Scholar]
- Mackenbach JP, Stirbu I, Roskam AR, Schaap MM, Menvielle G, Leinsalu M, Kunst AE. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008;358:2468–2481. doi: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- Murray C, Salomon J, Mathers C, Lopez A (2002) Summary measures of population health: concepts, ethics, measurement and applications. WHO, Geneva
- National Statistical Service of Greece (2004) 2001 Census data. Available http://www.statistics.gr Accessed 29 January 2009
- Nicholas S, Huppert FA, McWilliams B, Melzer D (2003) Physical and cognitive function. In: Marmot M, Banks J, Blundell R, Lessof C, Nazroo J (eds) Health, wealth and lifestyles of the older population in England: the 2002 english longitudinal study of ageing, IFS, London, pp 249-271
- Noale M, Minicuci N, Bardage C, Gindin J, Nikula S, Pluijm S, Rodriguez-Laso A, Maggi S. Predictors of mortality: an international comparison of socio-demographic and health characteristics from six longitudinal studies on aging: the CLESA project. Exp Gerontol. 2005;40:89–99. doi: 10.1016/j.exger.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Ongaro F, Salvini S. Understanding self-perceived health in the elderly: an analysis of 1986 Italian data. Eur J Popul. 1995;11:123–141. doi: 10.1007/BF01264908. [DOI] [Google Scholar]
- Paccagnella O, Weber G (2005) Household income. In: Börsch-Supan A, Brugiavini A, Jürges H, Mackenbach J, Siegrist J, Weber G (eds.) Health, ageing and retirement in Europe, first results from the survey of health, ageing and retirement in Europe. Mannheim Research Institute for the Economics of Ageing (MEA), Mannheim, pp 296–301
- Prince MJ, Reischies F, Beekam ATF, Fuhrer R, Jonker C, Kivela SL, Lawlor BA, Lobo A, Magnusson H, Fichter M, Van Oyen H, Roelands M, Skoog I, Turrina C, Copeland JRM. Development of the EURO-D scale—a European Union initiative to compare symptoms of depression in 14 European centres. Br J Psychiatry. 1999;174:330–338. doi: 10.1192/bjp.174.4.330. [DOI] [PubMed] [Google Scholar]
- Prince MJ, Beekam ATF, Deeg DJH, Fuhrer R, Jonker C, Kivela SL, Lawlor BA, Lobo A, Magnusson H, Meller I, Van Oyen H, Reischies F, Roelands M, Skoog I, Turrina C, Copeland JRM. Depression symptoms in late life assessed using the EURO-D scale. Br J Psychiatry. 1999;174:339–345. doi: 10.1192/bjp.174.4.339. [DOI] [PubMed] [Google Scholar]
- Quesnel-Valée A. Self-rated health: caught in the crossfire of the quest for ‘true’ health? Int J Epidemiol. 2007;36:1161–1164. doi: 10.1093/ije/dym236. [DOI] [PubMed] [Google Scholar]
- Robine JM, Jagger C, Euro-REVES group Creating a coherent set of indicators to monitor health across Europe. Eur J Public Health. 2003;13(3 supplement):6–14. doi: 10.1093/eurpub/13.suppl_1.6. [DOI] [PubMed] [Google Scholar]
- SHARE documentation online (2008) Sample. Available http://www.share-project.org/ Accessed 23 December 2008
- Simon JG, De Boer JB, Joung IMA, Bosma H, Mackenbach JP. How is your health in general? A qualitative study on self-assessed health. Eur J Public Health. 2005;15(2):200–208. doi: 10.1093/eurpub/cki102. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Dugravot A, Shipley MJ, Ferrie JE, Martikainen P, Goldberg M, Zins M. The association between self-rated health and mortality in different socioeconomic groups in the GAZEL cohort study. Int J Epidemiol. 2007;36:1222–1228. doi: 10.1093/ije/dym170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Netherlands (CBS) (2004) Institutionalised population no longer decreasing. Available http://www.cbs.nl/ Accessed 15 January 2009
- United Nations Educational Scientific and Cultural Organization. (2006) International Standard Classification of Education, ISCED 1997. Re-edition, UIS/TD/06-01, UNESCO-UIS Available http://www.uis.unedco.org, Accessed 5 July 2008
- Van Doorslaer E, Gerdtham UG. Does inequality in self-assessed health predict inequality in survival by income? Evidence from Swedish data. Soc Sci Μed. 2003;57:1621–1629. doi: 10.1016/S0277-9536(02)00559-2. [DOI] [PubMed] [Google Scholar]
- Van Ourti T. Socio-economic inequality in ill-health amongst the elderly. Should one use current income or permanent income? J Health Econ. 2003;22:187–217. doi: 10.1016/S0167-6296(02)00125-X. [DOI] [PubMed] [Google Scholar]
- Van Oyen H (2001) The institutionalised population in health surveys. United Nations Statistics Division. ESA/STAT/AC.81/7-6. Available http://unstats.un.org/UNSD/disability/ Accessed 15 Jan 2009
- Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Verropoulou G, Tsimbos C. Socio-demographic and health-related factors affecting depression of the Greek population in later life: an analysis using SHARE data. Eur J Ageing. 2007;4(3):171–181. doi: 10.1007/s10433-007-0060-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (1996) Health interview surveys: towards international harmonization of methods and instruments. WHO Regional Publications European Series no. 58 WHO Regional Office for Europe, Copenhagen [PubMed]
- Zimmer Z, Natividad J, Lin HS, Chayovan N. A cross-national examination of the determinants of self-assessed health. J Health Soc Behav. 2000;41(4):465–481. doi: 10.2307/2676298. [DOI] [PubMed] [Google Scholar]