Abstract
A 2.5-month-old filly was presented with signs of esophageal obstruction. The filly was euthanized and postmortem examination revealed a vascular ring anomaly. The vascular ring anomaly was not caused by a persistent right aortic arch, which is the only vascular ring anomaly reported to occur in horses.
Abstract
Résumé — Malformation vasculaire annulaire inhabituelle chez un poulain. Une pouliche de 2 1/2 mois a été présentée avec des signes d’obstruction œsophagienne. Après euthanasie, l’examen a révélé une malformation vasculaire annulaire. L’anomalie vasculaire annulaire n’était pas due à la persistance de l’arc aortique droit, seule malformation vasculaire annulaire rapportée chez le cheval.
Traduit par Docteur André Blouin
A 2.5-month-old, quarter horse filly was admitted to the Veterinary Teaching Hospital with a 3-day history of bilateral frothy nasal discharge. On admission, the filly was slightly depressed and in good body condition, but she had an increased heart rate (110 beats/min), a rapid shallow respiratory rate (50 breaths/min), and an increased rectal temperature (39.0°C); she was 10% clinically dehydrated and had a capillary refill time of 3 s. Her packed cell volume was normal (0.49 L/L) and plasma total protein was increased (87 g/L; normal, 58 to 64 g/L). There were copious amounts of bilateral frothy nasal discharge containing saliva, milk, and oats. Ptylism, dysphasia, and continual retching were also present, and the cervical esophagus was visibly distended with a firm palpable mass. Bilateral harsh lung sounds were heard cranioventrally on inspiration and expiration. Analysis of arterial blood collected from the dorsal pedal artery revealed a mixed acidosis with hypercarbia and hypoxia (pH 7.28; pCO2 49.8 mmHg; pO2 65.3 mmHg; bicarbonate 22.3 mmol/L; base excess −4.2 mmol/L; lactate 4.7 mmol/L). The respiratory acidosis and hypoxia indicated a decreased respiratory function, likely caused by severe pulmonary lesions. Thus, a tentative diagnosis of secondary aspiration pneumonia was made. The metabolic acidosis was due to the high lactate caused by an increase in anaerobic metabolism from hypoxia and decreased perfusion of tissues due to dehydration.
Although the filly was sedated with xylazine (Rompun; Bayer, Toronto, Ontario), 0.5 mg/kg bodyweight (BW), IV, a nasogastric tube could be passed only 110 cm into the esophagus. Irrigation of the obstruction site with water and carboxymethyl cellulose, and additional sedation with xylazine 0.5 mg/kg BW, IV, and diazepam (Valium; Sabex, Boucherville, Quebec), 0.03 mg/kg, IV, failed to help. Endoscopic examination of the obstruction site showed a circumferential narrowing of the esophagus without any visible foreign body or abnormality of the mucosa.
To eliminate the possibility of esophageal spasm versus esophageal stricture, the filly was anesthetized with the intention that muscle relaxation would relax any esophageal spasm and allow a nasogastric tube to be passed easily into the stomach. The filly was already sedated with xylazine and diazepam, as stated above. A 14-gauge jugular catheter was placed and the filly was induced with ketamine (Vetalar; Bioniche, Belleville, Ontario), 2 mg/kg BW, IV. Anesthesia was maintained with halothane and oxygen. Unfortunately, passage of the endoscope and nasogastric tube yielded unsuccessful results. Even under general anesthetic, a circumferential stricture of the esophagus was still visualized with an endoscope.
Upon recovery from surgery, adventitial lung sounds consisting of crackles and wheezes were now audible during auscultation in both lung fields. Ceftiofur (Excenel; Pharmacia Animal Health, Orangeville, Ontario), 5 mg/kg BW, IV, and ketoprofen (Anafen; Merial Canada, Baie d’Urfé, Quebec), 2.2 mg/kg BW, IV, were given. A decision was made to allow the filly to rest overnight with no food and to reassess her condition in the morning. During the night, her condition continued to deteriorate and she became severely depressed. She occasionally tried to suckle the mare, resulting in regurgitation of milk from her nares, but spent most of the night in sternal recumbency. The following day, the filly showed no signs of clinical improvement. An endoscope was used to try and detect any improvement at the esophageal lesion. However, no change was observed.
Radiographs of the thorax showed patchy consolidation of a large area of the cranioventral part of the lung, consistent with aspiration pneumonia. In the dorsocranial portion of the thorax, superimposed over the ascending aorta and dorsocranial to the tracheal bifurcation, a partially air-filled structure, suspected to be dilated thoracic esophagus, was visible. The dilation extended dorsocaudally and then tapered drastically at the level of the base of the heart, indicating an esophageal stricture. The radiological evidence was classic in its appearance for a vascular ring anomaly (VRA). However, the location of the esophageal stricture was too far caudad to be caused by a persistent right aortic arch (PRAA).
Unfortunately, due to her poor physical condition and the poor prognosis associated with aspiration pneumonia and repair of a VRA, the filly was euthanized with pentobarbital sodium (Euthanyl-forte; Biomeda, Cambridge, Ontario), 1.0 mL/5 kg BW, IV, and sent for postmortem examination.
On gross necropsy, the lungs were firm and dark red; on cut section, feed material was expressed from the airways. Histopathologic examination confirmed the presence of a suppurative bronchopneumonia. The esophagus was significantly dilated in the cranial thoracic region. Located 8 cm caudal to the base of the heart, the lumen of the esophagus was narrowed due to entrapment by an anomalous vascular structure. The vessel ran parallel to the right side of the aorta and then crossed over the esophagus, trapping the esophagus between the aorta and the trachea (Figure 1). The wall of the vessel was thin, suggesting it was a vein. However, a histopathologic examination was not performed. The anomalous vessel was transected during the necropsy and the pathologist was unable to determine its exact origin. Thus, the anomalous vessel could not be specifically identified. Postmortem findings confirmed the presence of a suspected VRA, which had resulted in esophageal constriction, megaesophagus, and a secondary aspiration pneumonia.
Figure 1.
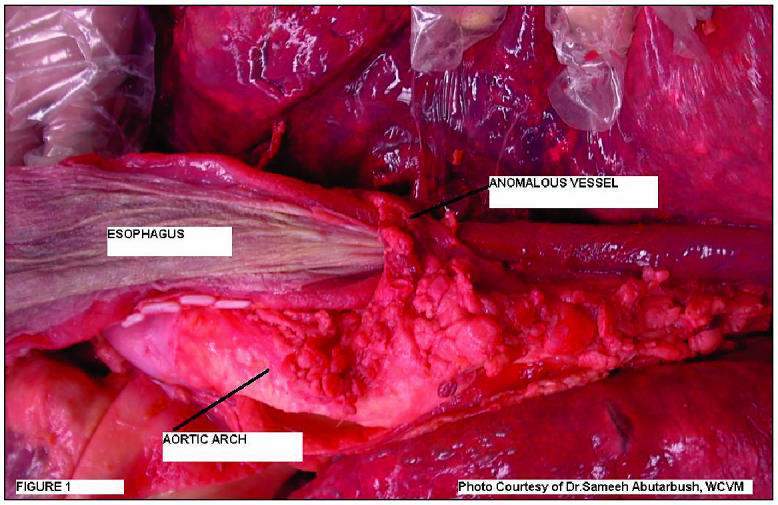
Photograph to show the vascular ring anomaly in a 2.5-month-old filly on postmortem examination.
Vascular ring anomalies in foals have been documented occasionally in the literature (1–4), but they are considered relatively rare. Vascular rings are formed during embryonic development. They result from the abnormal development of the great vessels from the aortic arches. The ring of vasculature that is created entraps the intrathoracic esophagus and trachea. The esophagus becomes compressed into the more resistant trachea by the vascular ring, causing esophageal constriction and dilation of the esophagus cranial to the constriction (5,6). Subsequently, the clinical signs of a VRA are associated with the effects of the esophageal constriction and most commonly include regurgitation, bilateral frothy nasal discharge, gagging, retching, ptylism, and dysphasia. Because these clinical signs are also seen with esophageal obstruction, a VRA must always be considered a differential diagnosis in a foal presenting with signs of an esophageal obstruction. Clinical signs of a VRA typically correlate with the transition to solid food at the time of weaning. The inability for the food to pass through the stenotic esophageal lesion leads to chronic regurgitation of feed, and often a secondary aspiration pneumonia (7,8).
The VRAs reported in the literature are as follows: persistent right aortic arch (PRAA), aberrant left or right subclavian artery, double aortic arch, right ductus arteriosus with left aortic arch, and aberrant intercostals arteries (8). However, the only VRA reported in the horse is due to persistence of the 4th dorsal right aortic arch (1–4), instead of the left. This results in the right aorta ascending to the right of the midline, arching over the origin of the right bronchus, and descending to the right or left of the vertebral column. The left ductus arteriosus, which later becomes the ligamentum arteriosum, forms a band between the pulmonary artery and the right aorta. Therefore, the ligamentum arteriosum, left pulmonary artery, and aorta form a vascular ring, that encircles the esophagus and trachea, causing esophageal constriction (2,5,8).
Although PRAA is the most commonly reported VRA in horses, it was not the cause of the VRA in this filly. Postmortem indicated that an anomalous vessel, not a PRRA, was the cause of the esophageal constriction. The pathologist described the vessel as being venous in structure. Unfortunately, as stated earlier, histopathologic examination of the vessel was not performed and the vessel was transected on postmortem, making it impossible for correct identification. Therefore, only hypotheses can be made as to the true nature of this vessel.
There have been no reports of an anomalous venous structure leading to a VRA in any domestic species. However, one hypothesis, in concurrence with the vessel being a vein, is that the structure is an aberrant right azygous vein. In horses, during normal embryonic development, the azygous vein is formed from the right caudal cardinal vein and the right supracardinal vein. The vein runs dorsad to the right of the esophagus. At approximately the 7th intercostal space, it arches over the esophagus and trachea to empty directly into right atrium at the level of the 5th intercostal space (5). It could be postulated that the right azygous vein in this filly was aberrantly located and caused a severe esophageal constriction when it arched dorsally over the esophagus and trachea. This would mimic the effects seen with a PRAA. If the anomalous vessel was truly venous in origin, an anomaly in azygous vein development is a possibility, because the azygous vein is approximately the same diameter as that of the anomalous vessel and it is the only venous structure located in a similar vicinity to the anomaly in this case. With closer examination of the photograph (Figure 1), the vessel would appear to come from the right of midline and move dorsomedially over the esophagus. At this point, it is difficult to determine if the vessel is descending down midline or is actually an artery emerging from the aortic arch. If indeed it is a vein descending down midline, then the hypothesis of an aberrant right azygous vein is a plausible explanation.
The last hypothesis put forth to explain the VRA in this filly is an aberrant right subclavian artery. Normally, the artery branches off from the brachiocephalic trunk in a right lateral direction. In the case of aberrant placement, it arises directly from the aorta immediately distal to the left subclavian artery. It then must cross over the esophagus from left to right, constricting the esophagus dorsally (9). Although the hypothesis of an aberrant right subclavian artery would be in disagreement with the gross appearance of the vessel as a vein, there was no microscopic examination of the vessel to confirm that it was a vein. In further support of this hypothesis, in comparing the appearance of an aberrant right subclavian artery with the VRA in this case (Figure 1), they closely resemble each other. In Figure 1, the anomalous vessel could be arising from the left aortic arch, in which case its location is very similar to that of an aberrant right subclavian artery. Therefore, because a small artery, such as the subclavian artery in a filly, can be mistaken for a vein grossly, and the appearance of the VRA in this filly closely resembles an aberrant right subclavian artery, this hypothesis can be neither accepted nor disregarded.
A persistent right aortic arch is the only vascular ring anomaly reported in the literature to occur in horses. Remarkably, in this case, a PRAA was confirmed not to be the cause of the VRA. Unfortunately, due to inconclusive findings on postmortem, definitive identification of the vessel causing the ring anomaly could not be reached. Hypotheses can only be formed as to the potential causes for this VRA. Nevertheless, this case is still exciting because it has shown that a PRAA is not the only cause of a vascular ring anomaly in a horse. CVJ
Footnotes
Dr. Smith’s current address is Angell Animal Medical Centre, 350 South Huntington Avenue, Jamaica Plain, Massachusetts 02130, USA.
Dr. Smith will receive 50 free reprints of her article, courtesy of The Canadian Veterinary Journal.
References
- 1.Bartels JE, Vaughan JT. Persistent right aortic arch in the horse. J Am Vet Med Assoc. 1969;154:406–409. [PubMed] [Google Scholar]
- 2.Butt TD, MacDonald DG, Crawford WH, Dechant JE. Persistent right aortic arch in a yearling horse. Can Vet J. 1998;39:714–715. [PMC free article] [PubMed] [Google Scholar]
- 3.Mackey VS, Large SM, Breznock EM, Arnold JS. Surgical correction of a persistent right aortic arch in a foal. Vet Surg. 1986;15:325–328. [Google Scholar]
- 4.Petrick SW, Roos CJ, VanNiekerk J. Persistent right aortic arch in a horse. J S Afr Vet Assoc. 1978;49:355–358. [PubMed] [Google Scholar]
- 5.Noden DM, DeLahunta A. The Embryology of Domestic Animals: Developmental Mechanisms and Malformation. Baltimore: Williams and Wilkins, 1985:212–268.
- 6.VanGundy T. Vascular ring anomalies. Compend Contin Educ Pract Vet. 1989;11:36–48. [Google Scholar]
- 7.Blikslager AT, Jones SL. Disorders of the esophagus. In: Smith BP, ed. Large Animal Internal Medicine. St. Louis: CV Mosby, 2000:608–617.
- 8.Wagner PC, Rantanen NW, Grant BW. Differential diagnosis for dysphagia in a horse. Mod Vet Pract. 1979;60:1029–1033. [PubMed] [Google Scholar]
- 9.Watrous BJ. The esophagus. In: Thrall DE, ed. Textbook of Veterinary Diagnostic Radiology. Philadelphia: WB Saunders, 2002:341–343.


