Abstract
Associations between disability and depression have been shown to be consistent across cultures among middle-aged adults. In later life the association between disability and depression is much more substantial and may be amenable to influences by health care facilities as well as economic and sociocultural factors. Fourteen community-based studies on depression in later life in 11 western European countries contribute to a total study sample of 22,570 respondents aged 65 years or older. Measures are harmonised for depressive symptoms (EURO-D scale) and disability. Using multilevel modelling to control for the stratified data structure we examined whether the association between disability and depressive symptoms is modified by national health care and mental health care availability, national economic circumstances, demographic characteristics and religious tradition. The association between depressive symptoms and disability is attenuated by health care expenditure and availability of mental health care and also by gross domestic product; it was more pronounced in countries with high levels of orthodox religious beliefs. Higher levels of depressive symptoms are found in countries with a larger gross domestic product (per capita) and higher health care expenses but are interpreted with care because of measurement differences between the centres. The findings from this contextual perspective indicate that general and mental health care should be geared to one another wherever possible.
Keywords: Depression, Disability, Cross-cultural, Contextual, Ecological
Introduction
In later life the most characteristic determinants of depression and depressive symptoms are disability due to poor physical functioning, widowhood, and cognitive decline (Berkman et al. 1986; Lenze et al. 2001). These risk factors largely differentiate depression in later life from early-onset depression (Cole and Dendukuri 2003). The strongest of these determinants is generally disability, which is influenced by depressive symptoms as well. The mutual association between these factors has been termed ‘synchrony of change’ (Ormel and Von Korff 2000; Ormel et al. 1993). Following this concept of a downward spiral of physical decline and depressive mood enhancing each other seems to lead to an open end. While biological research efforts are initiated to increase the understanding of the determinants of late-life depression in meticulous detail, any further factors need to be identified that also affect this spiral. This study examined the role of contextual social, economic and cultural factors as advocated by early theorists in social epidemiology such as Brown and Harris (1978). Gaining insight into the impact of the environment and society on this almost inevitable part of the ageing process is not only theoretically relevant but may also contribute to a framework for public health interventions.
The main contextual variables in this study were the availability of health care and mental health care. These health care characteristics are likely to affect the attention that both depressive symptoms and physical health problems receive form health care professionals. Cross-national findings based on national general practitioner characteristics (Wensing et al. 2004) and on the availability of gerontopsychiatric services (Bramesfeld 2003) indicate that there are considerable differences with respect to the quality and the extent of services provided in different western European countries. Some other national contextual variables from various domains are likely to influence the association between disability and depressive symptoms as well. Firstly, economic circumstances are known to affect depressive symptoms (Picket and Pearl 2001; Wilson et al. 1999). The more prosperous the contextual circumstances, the less depressed is the individual, also when controlling for the person’s own financial situation in the analyses (Meertens et al. 2003). Secondly, demographic characteristics of the population may affect the association between disability and depressive symptoms. In regions with a high population density society may be more complex for older persons, although the geographical distance to health care facilities may also be less than in countries with a low density. Similarly, the proportional increase in the ageing population may have the positive consequence that it leads to more experience in organising care for older adults. However, a shortage of services may also be a result because of a lack of political financial priority or to a want of professional staff in the care for older adults.
Finally, cultural factors such as value patterns attached to ageing are likely to influence the impact of disability on depressive symptoms. For example, lower expectations of level of functioning in later life may be found in cultures characterised by traditional value patterns, and high expectations in modern, individualistic value patterns, as can be characterised with the expression ‘successful ageing’. As has been discussed and implemented by Inglehart and Baker (2000), the more traditional value patterns are more likely to be observed in Roman Catholic countries and in countries with high levels of church attendance and high levels of orthodox Christian beliefs. More modern value patterns are expected to be present in Protestant countries, which are also more often secularised countries in western Europe (Halman and de Moor 1994). Apart from value patterns, a traditional religious climate is likely to facilitate the use of religion in terms of coping. A previous study on religious climate and depressive symptoms in western Europe found that depressive symptoms levels among older women were attenuated in countries characterised by regular church attendance (Braam et al. 2001).
The current study examined the impact of national contextual variables on the association between disability and depressive symptoms in later life. The data are used are from the EURODEP concerted action on depression and determinants of depression in later life (Copeland et al. 1999). EURODEP includes assessments from 14 study centres in 11 western European countries, covering a considerable cross-national variety of contextual factors. The main research question is whether national availability of health care and mental health care, economic circumstances, demographic characteristics, and religious traditions affect the association between depressive symptoms in older individuals and disability. Including other possibly relevant contextual factors, such as neighbourhood conditions and housing standard would lead to a study on local characteristics, for which most EURODEP centres were not equipped.
Methods and materials
Samples
The EURODEP Concerted Action is a consortium of 14 research groups from 11 European countries all engaged in population based research into the epidemiology of late-life depression (Copeland et al. 1999). In three of these countries there were two separate participating centres: Liverpool and London in the United Kingdom; Berlin and Munich in Germany; Amsterdam and the nation-wide sample of the Longitudinal Aging Study Amsterdam (LASA) in The Netherlands. Although there has been considerable collaboration between the centres in the design of the studies, especially with respect to the assessment of depression (Copeland et al. 1999), the collaboration is based on post-hoc possibilities of comparisons between the datasets, and harmonisation of measures has been applied where necessary (Prince et al. 1999a; Braam et al., submitted). Basic demographic characteristics of the 14 samples with data available for the present study are summarised in Table 1 (with references). The overall EURODEP dataset includes 22,570 subjects. More detailed information on sampling frame, interview procedures, and non- response has been presented by Copeland et al. (1999). The sampling frames are generally based either on municipality registers or on general practitioner registers. Except for Dublin, London (Gospel Oak district), Gothenburg and Iceland, where the complete registers were used, the samples were drawn randomly. These random samples were stratified for age and sex, which entails an even distribution of male and female respondents by over-sampling of male respondents. Although there were no exclusion criteria in most studies, subjects who were staying in hospitals and nursing homes are underrepresented. With respect to Liverpool, the first follow-up measurement, 2 years after baseline (Wilson et al. 1999) was used because this observation cycle included measures on physical functioning.
Table 1.
The EURODEP consortium studies, depression assessment, sociodemographics and mean EURO-D scores [BEL Antwerp, Belgium; BER Berlin, Germany; MUN Munich, Germany; AMS Amsterdam, Netherlands; NED LASA Longitudinal Aging Study (nationwide), Amsterdam [1], Netherlands; FIN Ähtäri, Finland; ICE Reykjavík, Iceland; SVE Gothenburg, Sweden; EIR Dublin, Ireland; LIV Liverpool, England; LON London, UK; ESP Zaragoza, Spain; FRA Personnes Agées QUID (Gironde and Dordogne districts, south west France); ITA Verona, Italy;Munic. municipality;Elect. electoral; GP general practitioner register; RR response rate; lay intensively trained lay interviewers; Medical physicians or psychiatrists; Psy. psychologists; Instrument instrument of depression assessment; Ref. sample described by; Educ. education higher levels]
| Type of register | RR (%) | Interviewer | Instrument | Reference | Age, mean (years; range) | Sex: F/M (%) | Educ. (%) | EURO-D mean score | Total | |
|---|---|---|---|---|---|---|---|---|---|---|
| BEL | Munic. | 67 | Lay | CES-D | Roelands et al. 1994 | 77 (65–99) | 47/58 | 23 | 1.9 | 1,130 |
| BER | Munic. | 27 | Medical | GMS | Helmchen et al. 1996 | 84 (70–103) | 49/30 | 27 | 2.5 | 488 |
| MUN | Elect. | 89 | Medical | GMS | Meller et al. 1993 | 88 (85–99) | 78/18 | 30 | 3.2 | 346 |
| AMS | GP | 85 | Nurse | GMS | van Ojen et al. 1995 | 74 (65–84) | 62/49 | 26 | 2.0 | 3,987 |
| NED | Munic. | 62 | Lay | CES-D | Berkman et al. 1995 | 75 (65–86) | 51/57 | 23 | 2.1 | 1,944 |
| FIN | Munic. | 84 | Medical | DSM-III | Pahkala et al. 1988 | 73 (65–95) | 61/49 | 7 | 1.6 | 1,035 |
| ICE | Nat. | 74 | Medical | GMS | Magnusson 1989 | 86 (83–89) | 60/28 | 22 | 2.0 | 772 |
| SVE | Munic. | 63 | Nurse | CPRS | Skoog et al. 1993 | 85 (85) | 70/23 | 25 | 2.2 | 449 |
| LIV | GP | 67 | Nurse | GMS | Wilson et al. 1999 | 79 (67–104) | 52/37 | 22 | 2.2 | 3,366 |
| LON | Elect., GP | 80 | Lay | SHORT-CARE | Livingston et al. 1990 | 75 (65–99) | 60/37 | 19 | 2.5 | 637 |
| EIR | GP | 85 | Nurse | GMS | Lawlor et al. 1994 | 74 (64–98) | 64/49 | 30 | 1.7 | 1,012 |
| ESP | Munic. | 95 | Lay | GMS | Lobo et al. 1995 | 77 (65–102) | 59/53 | 14 | 1.5 | 3,598 |
| FRA | Munic. | 68 | Psy. | CES-D | Dartigues et al. 1992 | 75 (65–101) | 58/58 | 19 | 2.2 | 3,604 |
| ITA | Munic. | 95 | Medical | GMS | Turrina et al. 1991 | 74 (65–100) | 62/53 | 23 | 1.8 | 202 |
| Total | – | – | – | – | – | 77 | 58/48 | 24 | 2.0 | 22,570 |
Measures on respondent level
Depressive symptoms
The depressive symptom measure in the current study is the EURO-D scale. This harmonised depressive symptom scale was developed to enhance analyses in the pooled EURODEP dataset because not all centres used the same depression assessment procedure (Table 1). Eight centres used the Geriatric Mental State (GMS) examination (Copeland et al. 1986), three other centres the CES-D (Radloff 1977), one the Comprehensive Psychopathological Rating Scale (CPRS; Åsberg et al. 1978), one the short version of the Comprehensive Assessment and Referral Evaluation (SHORT-CARE; Gurland et al. 1984), and one a Diagnostic and Statistical Manual of Mental Disorders (DSM) III interview with items identical to those used in the GMS. To obtain a pooled EURODEP dataset these five instruments were harmonised according to a procedure developed and validated by Prince et al. (1999a). This resulted in the EURO-D scale which comprises 12 items: depressive affect, pessimism, wishing death, guilt, sleep, interest, irritability, appetite, fatigue, concentration, enjoyment, and tearfulness (0=’not present’, 1=’present’; range 0–12). For each centre the EURO-D scale has been reported to be to be adequately internally consistent (Prince et al. 1999a). The value of Cronbach’s α was 0.72 in the current pooled sample, with centre-specific values ranging from 0.65 in Dublin to 0.83 in Finland. The sensitivity of the EURO-D for a diagnosis of depression was assessed in the GMS centres and ranged between 0.63 (Dublin) to 0.83 (Berlin; Prince et al. 1999a). The standard deviations differ between the centres, those using the GMS having larger standard deviations than those using the CES-D. Because this difference in variance is probably artefactual (Prince et al. 1999b), the EURO-D scale is applied in its version with standardised standard deviations. The mean EURO-D scores are presented in Table 1. Higher scores are found in Munich, London and Berlin and lower scores in Ireland, Finland and Spain. The harmonisation procedure cannot neutralise differences in original wording of the items between the instruments included, and differences between the countries are expected to remain with respect to the precise emotional content of translated items and the subsequent, to some degree, culturally biased responses. Therefore, as discussed by Prince and colleagues (1999a), there are disadvantages to using the EURO-D for comparison of EURO-D scale distribution between centres. Comparison of effect sizes for associations between risk-factors and EURO-D score between centres, however, is expected to be a valid application of the EURO-D scale.
Disability
For disability, several versions of ‘activities of daily living’ scales were employed, as summarised in Table 2. To obtain comparable measures, total scores of each scale were trichotomised into ‘no’, ‘intermediate’ and ‘high’ levels of disability. Wherever possible the categories of ‘intermediate’ and ‘high’ levels of disability received equal proportions. As shown in Table 2, the distributions of levels of disability vary across the samples. It should be underlined that the comparability of disability scores between the centres with different items and especially with differing number of items is still limited. As is the case with the EURO-D scores, the only valid application of this harmonised disability scale is comparison of effects sizes of its association with outcome variables such as depressive symptoms. More details on this procedure as well as on alternative ways of harmonisation, such as comparison of centres with exactly the same items on activities of daily living are presented elsewhere (Braam et al., submitted).
Table 2.
Assessment of disability in the participating EURODEP centres; prevalences and means on the three-point harmonised scale (see Table 1 for explanation of acronyms)
| References | Prevalence on three-point harmonised scale (%) | Mean score on harmonised scale (0–2) | |||
|---|---|---|---|---|---|
| None | Some | Many | |||
| AMS | Katz et al. 1970 | 94 | 5 | 2 | 0.1±0.3 |
| BEL | Katz et al. 1970; McWhinnie 1981 | 62 | 18 | 20 | 0.6±0.8 |
| BER | Katz et al. 1970 | 78 | 12 | 10 | 0.3±0.7 |
| EIR | One item, observer question | 62 | 27 | 11 | 0.5±0.7 |
| ESP | Katz et al. 1970 (1 item added) | 90 | 6 | 4 | 0.1±0.4 |
| FIN | Pulska et al. 1997 | 30 | 37 | 33 | 1.0±0.7 |
| FRA | Katz et al. 1970 | 92 | 5 | 3 | 0.1±0.4 |
| ICE | Katz et al. 1970 | 72 | 20 | 8 | 0.4±0.6 |
| ITA | Belloc et al. 1971 | 81 | 5 | 14 | 0.3±0.7 |
| LIV | Katz et al. 1970; Prince et al. 1997 | 52 | 30 | 18 | 0.7±0.8 |
| LON | Katz et al. 1970; Prince et al. 1997 | 43 | 34 | 23 | 0.8±0.8 |
| MUN | Oswald and Fleischmann 1984 | 22 | 33 | 45 | 1.2±0.8 |
| NED | Kriegsman et al. 1997 | 49 | 21 | 30 | 0.8±0.9 |
| SVE | Östling and Skoog 2002 | 32 | 45 | 24 | 1.0±0.8 |
| Pooled | – | 72 | 16 | 12 | 0.4±0.7 |
Sociodemographic variables
Sociodemographic variables include gender, age, marital status and education. Marital status is dichotomised as ‘married’ vs. ‘non-married’ (never married, divorced or separated, or widowed). The distribution is shown in Table 1. In Munich, Iceland and Gothenburg, the samples were drawn primarily among octogenarians, which is accompanied by the lowest rates of the married category. As marital status is included only as a background variable, no further categorisation is used. Moreover, due to conservative cultural norms the percentage of divorced subjects is much lower in the countries with a predominantly Roman Catholic religious tradition (1% in Belgium, Spain, Italy and Belgium) than the other countries (2–9%). Therefore the use of all four categories of marital status would introduce an undesirable proxy variable for religious tradition, which is one of the contextual determinants under study.
Education was assessed in several ways in the different centres: years of education, degree of education, and classifications in ‘lower’, ‘intermediate’ and ‘higher’. To maintain maximal variability, the original assessment scores within each centre were divided by the maximum value that could be attained in the respective centre. The resulting score falls within a range between 0 (no education) and 1 (maximum of education). This education index is meant for use only as a control variable: the mean values between the centres vary and are not meant to be compared with each other or interpreted. The standard deviations vary between the centres (range 0.08–0.22), with 0.20 as the standard deviation for the total sample.
Assessment of contextual variables
General health care and mental health care
Two measures are selected as indices of the quality of the general health care system (Table 3). The first is the health expenditure per capita from the OECD 1990 dataset (OECD 1993). The second measure is the density of practising physicians. Because data for 1990 are far from complete, the figures from 1995 were used. An alternative would have been the density of general practitioners, but because the health care systems of the countries included in the present study differ in their organisation and the role of the general practitioner, the total number of physicians may provide a better index of the accessibility of medical physicians in general.
Table 3.
National, contextual characteristics of health care, economy, demography and religion
| Belgium | Finland | France | Germany | Iceland | Ireland | Italy | Netherlands | Spain | Sweden | UK | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| General health care | |||||||||||
| Health expenditure per capita, compared to US: 100 (%)a | 47.8 | 49.5 | 58.8 | 58.5 | 53.0 | 29.8 | 49.8 | 49.5 | 29.8 | 56.0 | 37.9 |
| Practising physicians, density/1000b | 3.5 | 2.8 | 3.2 | 3.1 | 3.0 | 2.1 | 3.9 | 2.9e | 2.5 | 2.8 | 1.8 |
| Mental health care c | |||||||||||
| Psychiatric beds per 10,000 | 25 | 11.6 | 12.1 | 7.6 | 4.2 | 11.5 | 1.7 | 18.7 | 4.4 | 6.7 | 5.8 |
| Psychiatrists per 100,000 | 18 | 16 | 20 | 7.3 | 25 | 5.2 | 9 | 9 | 3.6 | 20 | 11 |
| Mental health care: index of availability (sum of rankings) | 19 | 15 | 18 | 9 | 13 | 9 | 5 | 14 | 4 | 14 | 10 |
| Economy a | |||||||||||
| Unemployment rate (% of labour force) | 8.8 | 3.7 | 9.0 | 6.2 | 1.7 | 13.7 | 10.5 | 9.0 | 15.8 | 1.5 | 5.5 |
| Gross domestic product per capita (US$/year) | 18,009 | 18,026 | 18,162 | 20,359 | 20,031 | 12,917 | 17,430 | 17,706 | 12,971 | 18,660 | 16,228 |
| Demography a | |||||||||||
| Population density (per km2) | 306.3 | 14.7 | 102.9 | 223.5f | 2.5 | 50.0 | 188.3 | 440.7 | 78.9 | 20.8 | 223.9 |
| Population aged 65 years or older (%) | 14.8 | 13.5 | 14.0 | 15.3 | 10.7 | 11.3 | 15.3 | 12.8 | 13.7 | 17.8 | 15.7 |
| Religion d | |||||||||||
| Roman Catholic (%) | 68 | 0 | 58 | 45 | 1 | 93 | 83 | 29 | 85 | 1 | 10 |
| Protestant (%) | 1 | 89 | 1 | 43 | 94 | 2 | 1 | 17 | 0 | 77 | 45 |
| Weekly church attendance (%) | 27 | 4 | 10 | 18 | 2 | 81 | 38 | 27 | 30 | 4 | 14 |
| Orthodox beliefs, mean score (range 0–12) | 4.6 | 6.2 | 4.4 | 5.2 | 6.4 | 9.0 | 6.9 | 4.7 | 5.8 | 3.8 | 6.4 |
aSource: OECD 1990
bSource: OECD 1995
cSource: WHO Atlas Country Profiles 2001
dSources: European Value Survey 1990
eMean value between 1990 (2.5) and 2000 (3.2) because no value for 1995 was available
fComputed for 1991, when West Germany and East Germany were unified; 1990 data for East Germany are missing
For mental health care only information from the WHO in the year 2001 was suitable for deriving two measures available for all countries included in the study (World Health Organization 2001). The first is the number of psychiatric beds per 10,000 inhabitants, and the second is the number of psychiatrists per 100,000 inhabitants. These measures are proxies of quality and accessibility of mental health care only, and, as is shown in Table 3, the figures reflect fairly different types of organisation of mental health care. Therefore the ranked scores (with a range between 1 and 11) of both measures were added to one index of mental health care ranking (range 2–22). This index is also included in the analyses.
Economic characteristics
Two measures are included, based on the OECD 1990 data (OECD 1993, 2004), unemployment and gross domestic product. The latter figure was divided by the number of inhabitants of the country. The patterns of distribution of the economic characteristics are shown in Table 3, with Germany being most prosperous around 1990, and Spain the least.
Demographics
Two demographic characteristics of the countries are included, population density and the percentage of inhabitants aged 65 years or older (Table 3). Both series of figures are based on the OECD 1990 data (OECD 1993, 2004).
Religious tradition
Four different indicators on the national religious tradition were derived from the 1990 observation cycle of the European Value Survey (Halman and de Moor 1994). From the section ‘Churches, Religion and Moral Values’ the following estimates were selected: national percentages of (a) Roman Catholics, (b) Protestants, (c) weekly church attenders and (d) mean national score on the orthodoxy scale (Table 3). The orthodoxy scale assesses adherence to traditional Christian beliefs (life after death, soul, devil, hell, heaven, and sin; range 0–12; Middendorp 1979). As is shown in Table 3, Protestantism is prevalent in the north-west of Europe and Roman Catholicism in the south as well as in Ireland. Church attendance is generally higher in Roman Catholic than in Protestant regions. The national mean scores on orthodox beliefs, however, are high not only in Roman Catholic countries, as high scores are also found in two predominantly Protestant countries: the United Kingdom (Anglican) and Finland (Lutheran).
Statistical procedures
The data from the different centres were pooled into a single EURODEP sample. Associations between the estimates of physical health and depressive symptoms measured by the EURO-D score were examined using multilevel analysis (Bryk and Raudenbush 1992). Multilevel random regression modelling (MLRM) is ideally suited for conglomerate datasets of nested subsets for which each data point cannot be considered as equally independent. In fact, subjects from the same country are more similar to each other than subjects from different countries. While sampling characteristics, the assessment instruments used, and research design and context can differ between the centres included in the study, the target relation under study can be considered as fixed. MLRM corrects for these differential levels of independence and allows the control of known characteristics of the different subsets as well as the differential weighting of unknown dependencies within the data. Moreover, MLRM allows the analysis of associations between higher level characteristics and lower level characteristics, while controlling for covariates on either level.
In the present study the unit of measurement on the lower level was that of the individual respondent and that on the higher level that of the contributing centres. Characteristics on the lower level included EURO-D depression score, disability, and sociodemographics. Characteristics on the higher level were constituted by the contextual factors. MLRM also allows the assessment of interactions between variables on the country and individual level. This is of particular relevance for the present study, which focuses on how the relationship between disability and depressive symptoms on the individual level is modified by contextual factors at the country level. All analyses are adjusted for characteristics of the individual: gender, age, marital status, education and disability. Furthermore, interactions between gender and age with each other and with marital status and education are included as control variables as well. Two series of models are employed. First, in separate models the associations between each of the contextual variables and EURO-D scores are examined. Second, the research question is addressed by examining the interactions between each of the contextual variables and disability, again in separate models.
The χ2 statistic generated by the MLRM routine in the Stata software (StataCorp, 2003 edition) was used to assess the significance of the prediction of the regression models and to assess the gain in fit of more complex over less complex models. Because the very large sample size may lead to an excess of statistical power (justifying an α value at the 0.01 level), but also because of the high number (13) of parallel analyses and the subsequent risk of significant interaction effects by chance, the level of significance and the risk of type I error (rejecting a true null hypothesis) was set at α=0.001. Findings with significance between 0.01 and 0.001 are shown and discussed, but are interpreted only with caution. When significant interaction terms are found, the direction of the interaction is examined by comparing mean EURO-D scores between relevant subgroups to obtain illustrations. The mean EURO-D scores (adjusted for sociodemographic covariates) are therefore computed for the subgroups of those without, with some, and with high disability, according to the levels of the contextual characteristics. For reasons of clarity the scores of the contextual characteristics in these illustrations are trichotomised.
The number of countries involved in the study is only 11. Therefore only one contextual characteristic at the country level was assessed in each model. Spearman’s correlation coefficient was computed between the contextual variables, to detect the possibility of mutual confounding and to facilitate interpretation of the results.
Results
Correlations between contextual variables
The strongest correlations (|r | ≥0.70) which may be of relevance for the interpretation of the results of the main analyses are summarised in the following. Especially unemployment was correlated highly significantly with many other contextual variables (P≤0.001 if not otherwise indicated): Roman Catholicism (r=0.89), Protestantism, (r=−0.91), and church attendance (r=0.88). Gross domestic product correlated strongly with health-expenditure (r=0.88). Number of psychiatrists correlated inversely with church-attendance (r=−0.77). As may be expected, Roman Catholicism was inversely associated with Protestantism (r=−0.91) and positively with church attendance (r=0.84). Similar but inverse correlations were found between Protestantism and church attendance (r=−0.78).
Associations between contextual variables and depressive symptoms
The basic model which was used for all analyses is shown in Table 4. This model includes all covariate background variables as well as disability. The interaction between gender and age did not reach statistical significance and reflected a statistical trend only. The term was kept in the model, however, to effect the maximal possible adjustment, as the inequalities between the samples with respect to age and sex distribution are considerable.
Table 4.
Association between depressive symptoms (EURO-D score) and contextual variables, basic multilevel model with unstandardised regression coefficients (B); Wald: χ2=2902 (9 d.f.)
| B | P | |
|---|---|---|
| Constant | 0.059 | 0.814 |
| Age | 0.021 | 0.001 |
| Female (vs. male) | 0.908 | 0.001 |
| Married (vs. nonmarried) | 0.926 | 0.001 |
| Education index (0–1) | -0.240 | 0.001 |
| Gender × age | -0.004 | 0.072 |
| Gender × married | -0.188 | 0.001 |
| Gender × education | -0.256 | 0.003 |
| Age × married | -0.009 | 0.001 |
| Disability |
0.430 |
0.001 |
As shown in Table 5, gross domestic product and health-care expenditure are associated with EURO-D score: higher levels of depressive symptoms are encountered in better economic circumstances and with higher expenses to health care.
Table 5.
Associations between contextual characteristics and depressive symptoms (EURO-D scores), adjusted for sociodemographics and disability in the first series of analyses, and for product terms between the contextual variables and disability from the second series of analyses. Results from multilevel analyses, unstandardised (B) and standardised regression coefficients (β)
| First series | Second series | |||||||
|---|---|---|---|---|---|---|---|---|
| β | P | χ2 increase | β and β product-term disability |
P and P product-term |
χ2 increase | |||
| Health care | ||||||||
| Health expenditure | 0.17 | <0.001* | 142 | 0.20 −0.21 |
<0.001* <0.001* |
153 | ||
| Physicians density | 0.00 | 0.964 | 0 | 0.02 −0.08 |
0.860 0.011 |
6 | ||
| Psychiatric beds / 10,000 | −0.05 | 0.406 | 3 | −0.04 −0.03 |
0.552 0.026 |
7 | ||
| Psychiatrists / 100,000 | −0.01 | 0.889 | 0 | −0.01 −0.01 |
0.926 0.531 |
0 | ||
| Mental health care, ranking | 0.00 | 0.973 | 16 | 0.01 −0.08 |
0.700 <0.001* |
27 | ||
| Economic | ||||||||
| Unemployment rate | −0.11 | 0.090 | 5 | 0.13 0.05 |
0.051 0.002 |
16 | ||
| Gross domestic product | 0.19 | <0.001* | 87 | 0.22 −0.31 |
<0.001* <0.001* |
90 | ||
| Demographics | ||||||||
| Population density | 0.11 | 0.194 | 1 | 0.13 −0.03 |
0.116 0.010 |
9 | ||
| Population aged 65+ | 0.13 | 0.039 | 7 | −0.14 −0.14 |
0.058 0.031 |
9 | ||
| Religious tradition | ||||||||
| Roman Catholic church member | −0.06 | 0.531 | 0 | −0.07 0.03 |
0.193 0.006 |
14 | ||
| Protestant church member | 0.01 | 0.893 | 0 | 0.02 0.02 |
0.821 0.088 |
1 | ||
| % regular church-attendance | −0.10 | 0.283 | 0 | −0.11 0.02 |
0.147 0.098 |
5 | ||
| Orthodox beliefs | −0.12 | 0.171 | 1 | 0.14 0.12 |
0.040 0.001* |
18 | ||
Effect modification of the association between disability and depressive symptoms by contextual variables
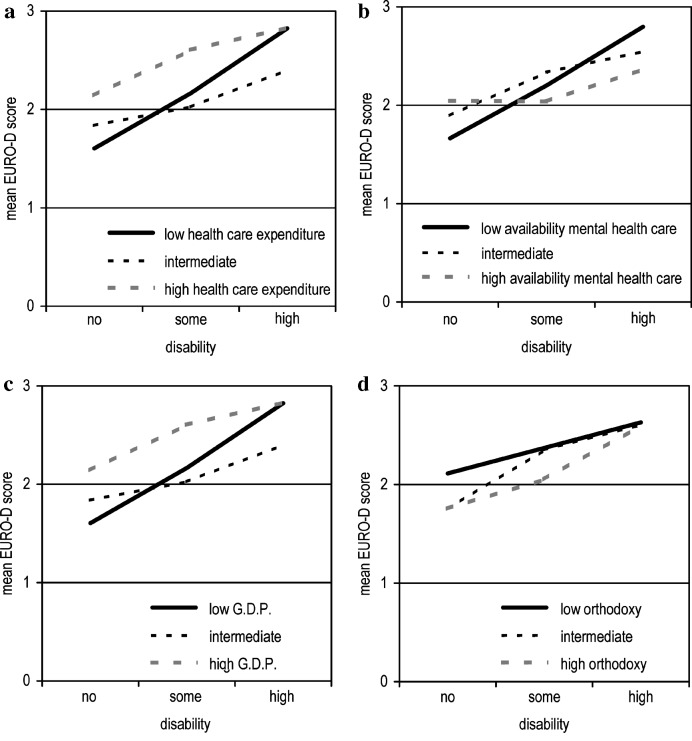
Several contextual variables modified the association between disability and depressive symptoms, but only four reached the required 0.001 level of significance. The interaction with health expenditure provided the best improvement in the multilevel model (Table 5). Subsequent comparing of mean EURO-D scores for subgroups, adjusted for covariates, serving to illustrate the findings (Fig. 1a) makes clear that the association between disability and depressive symptoms is less pronounced in countries with higher health care expenses. The figure also shows that levels of depressive symptoms are generally higher in the countries with higher health care expenses. The second highly significant interaction is with mental health care rating. A similar pattern is found as described for health care expenses, but levels of depressive symptoms among those with disability are notably lower in countries with higher rankings of mental health care availability (Fig. 1b). The third interaction, with gross domestic product (Fig. 1c), exactly follows the pattern as described for health care expenses. The fourth interaction is found for levels of orthodox beliefs. In countries with high levels of orthodox beliefs, the association between disability and depressive symptoms is more pronounced than in countries with low levels of orthodox beliefs (Fig. 1d).
Fig. 1.
Levels of depressive symptoms and degrees of disability, for tertiles of the following four contextual varables in 11 western European countries: a national health care expenditure, b availability of mental health care (psychiatric beds and psychiatrists) , c gross domestic product (G.D.P.) and d national levels of orthodox religious beliefs
The product tem between unemployment rate and disability almost reached the 0.001 level of significance. The association mirrors the effect of gross national product. The significance of the product tem between percentage of Roman Catholics and disability was below 0.01 as well. This type of effect modification parallels that shown by level of orthodox beliefs. Finally, there is a small interaction effect by population density and disability. In countries with high levels of population density the association between disability and depressive symptoms is somewhat less pronounced. A similar small interaction effect is found for physician density.
Discussion
The current study examined the modifying effect of a range of contextual factors on the association between disability and depressive symptoms in a large set of samples among older European citizens. After multivariate adjustment higher levels of depressive symptoms were found in countries with a larger gross domestic product (per capita) and higher health care expenses. Regarding the main research question on the association between depressive symptoms and disability it was demonstrated that this association was attenuated by health care expenditure, availability of mental health care and gross domestic product. The findings provided support for the hypothesis that the association between physical health and depression is less pronounced with better health care facilities available, as well as in a more prosperous environment. In contrast with the hypothesis on religious tradition, the association between depressive symptoms and disability was more pronounced in countries with high levels of orthodox religious beliefs. Furthermore, there was an indication that the association between depressive symptoms and disability was less pronounced in countries with a high level of population density.
The high depressive symptom scores in prosperous western European countries are also paralleled by higher prevalences of depression, as was demonstrated in a EURODEP publication on cases of depression (Copeland et al. 1999). The more prosperous countries in question are Germany, Iceland and Sweden. These are also the centres that had the oldest samples: primarily octogenarians. This may be especially relevant for the two German centres, Germany being the most prosperous country at the time of measurement. One factor that should be taken into account is that adjustment for age, gender and marital status may not have ruled out the effect of belonging to the oldest cohort. More information on physical as well as cognitive decline would have been desirable to include in the analyses.
A second consideration pertains to Germany in particular. Although the current study did not focus on post-traumatic stress reactions, it may be of relevance that the subjects of the oldest cohort in Germany, the generation born around 1910, experienced the second world war with great violence when they were in their thirties. Many German respondents are very likely to have lost relatives due to combat or bombings. The personal suffering may not have been revealed to or shared with others throughout life because of a different cultural climate with respect to expression of emotions in the post-war years compared to the current period. This aspect of silence on personal trauma may be even more pronounced in Germany than in countries that participated in the Allied forces, due to a sense of political correctness. This can be indirectly inferred from the number of publications based on a Medline search which provided only one publication on post-traumatic reactions among older Germans (Maercker and Herrle 2003).
The strongest modifying effect on the association between disability and depressive symptoms was by health care expenditure. There was a very high correlation between health care expenditure and gross domestic product, suggesting that the degree of prosperity forms part of the explanation. Nevertheless, the modifying effect by gross domestic product on the association between disability and depressive symptoms was weaker than that for health care expenditure. The modifying effect by health care expenditure therefore does not seem to depend on the degree of prosperity entirely. The modifying effect by mental health care availability did not seem to depend on gross domestic product, with which there was no significant correlation.
The modifying effect of national level of orthodox beliefs on the association between disability and depressive symptoms was only partly dependent on economic circumstances. The correlation between orthodox beliefs and gross national product was not significant but still reached the level of a statistical trend (r=−0.50). Furthermore, it should be noted that Ireland, which was the country with (by far) the highest level of orthodox beliefs, disability was assessed with a one-item interview question only, which may have decreased the reliability of measurement. This measurement problem may have led to a spuriously high association between disability and depressive symptoms. Other countries where the stronger association between disability and depressive symptoms was observed along with orthodoxy are Finland and Iceland. Both countries are Lutheran and characterised by low levels of church attendance. If this cultural pattern would mean that religiosity is mainly an important but personal aspect of life, some of the advantages of religious participation, such as social support and communication of positive cognitions such as hope, may be less available.
Some limitations of the current study should be addressed. A main concern is the varying response rate across the participating studies. Generally, the oldest and the more disabled among the elderly are under-represented in community-based studies. This may lead to less pronounced findings and possibly the risk of overlooking cross-national differences. A second limitation is that the measurement of disability and also the depression instruments showed considerable variation across the centres. Although the harmonisation procedures followed are straightforward and easy to reproduce, some categorisations may include a bias. Furthermore, the assessment of mental health care was restricted to number of psychiatric beds and number of psychiatrists. The number of beds may be less relevant than the duration for which a bed is generally used, and the categories of patients for which it is available. For example, in Belgium residential care for the mentally retarded falls within the field of psychiatry from an organisational point of view. Furthermore, assessment of ambulant mental health care was not available for the range of European countries involved in the current study, whereas the field of ambulant care is generally the first place where assistance and treatment is organised for common mental health problems such as late life depression.
A point of caution with studies using characteristics on aggregated groups such as national figures is the ‘ecological fallacy’, i.e. treating the characteristics of an overall group as though they applied to each member of that group. An example of possible misinterpretation in the current study pertains to economic circumstances. That the gross national product is high in certain countries does not necessarily mean that the older population is prosperous. There is even a risk that the older population lives in marked contrast with the rest of the population, which is then not recognised in the analytical strategy followed. The present method avoided this shortcoming as far as possible by applying the multilevel approach. This allowed controlling for effects of individual background variables as well as systematic inspection of cross-relationships between the higher and lower levels of measurement. Nevertheless, income data on the individual level were not available, and the only variable that remained as a type of proxy for the economic standard attained was level of education. Furthermore, a measure for individual use of health care was not available.
The main finding of the current contribution is that public health expenditure, as a derivative of the degree of economic prosperity, and the availability of psychiatric services are related to with a weaker association between disability and depressive symptoms. Of course, this is what one might expect of health care services. Effectiveness of care may be a factor here, although many other, unobserved environmental variables may play a role. Nevertheless, that these ecological associations could be demonstrated supports the suggestion that health care policies directly influence the association between functional and mental well-being in older persons. Many processes, such as primary health care organisation, financial resources for older persons and their caregivers, availability and acceptation of care for mental disorders, as well as a sense of optimism in a more prosperous environment may be explanatory factors. In another, European cross-cultural study in the field of research of primary health care, several characteristics of primary care organisation were studied in more detail (Wensing et al. 2004). Considerable differences were observed between countries, such as density of general practitioners and the gate-keeper role of the general practitioner towards specialised care. However, the degree of satisfaction among primary care patients was not associated with primary health care organisation.
The results show that it worked out well to make international comparisons by specifically focusing on interactions that reflect variations in individual processes, such as the disablement process with its emotional consequences. The results warrant further explorations into the course of depressive symptoms and other outcomes of effectiveness of care as well as other environmental characteristics, also on the local level, such as ambulatory mental health care and housing standard. The biological and psychological factors need to be identified that can curb the downward spiral of disability and depression. Furthermore, the current findings warrant the recommendation to health care decision makers that general and mental health care should be geared to one another wherever possible.
Acknowledgements
The EURODEP collaboration was supported by the European Commission BIOMED 1 initiative. The current study was supported by a grant from the Universitair Stimuleringsfonds of the Vrije Universiteit Amsterdam.
References
- Åsberg M, Perris C, Schalling D, Sedvall G. CPRS: development and applications of a psychiatric rating scale. Acta Psychiatr Scand Suppl. 1978;271:1–69. doi: 10.1111/j.1600-0447.1978.tb02357.x. [DOI] [PubMed] [Google Scholar]
- Beekman J Affect Disord. 1995;36:65. doi: 10.1016/0165-0327(95)00061-5. [DOI] [PubMed] [Google Scholar]
- Belloc Am J Epidemiol. 1971;93:328. doi: 10.1093/oxfordjournals.aje.a121265. [DOI] [PubMed] [Google Scholar]
- Berkman Am J Epidemiol. 1986;124:372. doi: 10.1093/oxfordjournals.aje.a114408. [DOI] [PubMed] [Google Scholar]
- Braam Psychol Med. 2001;31:803. doi: 10.1017/S0033291701003956. [DOI] [PubMed] [Google Scholar]
- Bramesfeld Int J Geriatr Psychiatry. 2003;18:392. doi: 10.1002/gps.841. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris TO (1978) Social origins of depression; a study of psychiatric disorder in women. Tavistock, London
- Bryk Hierarchical linear. 1992;models:applications. [Google Scholar]
- Cole Am J Psychiatry. 2003;160:1147. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- Copeland Psychol Med. 1986;16:89. doi: 10.1017/s0033291700057779. [DOI] [PubMed] [Google Scholar]
- Copeland Br J Psychiatry. 1999;174:312. doi: 10.1192/bjp.174.4.312. [DOI] [PubMed] [Google Scholar]
- Dartigues Am J Epidemiol. 1992;135:981. doi: 10.1093/oxfordjournals.aje.a116410. [DOI] [PubMed] [Google Scholar]
- Gurland J Gerontol. 1984;39:166. doi: 10.1093/geronj/39.2.166. [DOI] [PubMed] [Google Scholar]
- Halman L, Moor R de (1994) Value patterns and modernity. In: Ester P, Halman L, de Moor R (eds) The individualizing society; value change in Europe and North America. Tilburg University Press, Tilburg, pp 155–162
- Helmchen Nervenartz. 1996;67:739. doi: 10.1007/s001150050048. [DOI] [PubMed] [Google Scholar]
- Inglehart Am Soc Rev. 2000;65:19. [Google Scholar]
- Katz Gerontologist. 1970;10:20. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- Kriegsman J Epidemiol Community Health. 1997;51:676. doi: 10.1136/jech.51.6.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawlor Ir J Psychol Med. 1994;11:157. [Google Scholar]
- Lenze A J Geriatr Psychiatry. 2001;9:113. doi: 10.1176/appi.ajgp.9.2.113. [DOI] [PubMed] [Google Scholar]
- Livingston Psychol Med. 1990;20:137. doi: 10.1017/s0033291700013313. [DOI] [PubMed] [Google Scholar]
- Lobo Arch Gen Psychiatry. 1995;52:497. doi: 10.1001/archpsyc.1995.03950180083011. [DOI] [PubMed] [Google Scholar]
- Maercker J Traum Stress. 2003;16:579. doi: 10.1023/B:JOTS.0000004083.41502.2d. [DOI] [PubMed] [Google Scholar]
- Magnusson H. Mental health of octogenarians in Iceland. An epidemiological study. Acta Psychiatr Scand. 1989;79([Suppl 349):4–104. [PubMed] [Google Scholar]
- McWhinnie Rev Epidemiol Sante Publique. 1981;29:413. [PubMed] [Google Scholar]
- Meertens Soc Health Illn. 2003;25:208. doi: 10.1111/1467-9566.00332. [DOI] [PubMed] [Google Scholar]
- Meller Eur Arch Psychiatry Clin Neurosci. 1993;242:286. doi: 10.1007/BF02190388. [DOI] [PubMed] [Google Scholar]
- Middendorp CP (1979) Ontzuiling, politisering en restauratie in Nederland. De jaren 60 en 70 [The break down of traditional and socio-political barriers, politicising, and restoration in the Netherlands. The sixties and seventies]. Boom, Amsterdam
- OECD (1993) OECD health systems; facts and trends 1960–1991. OECD, Paris
- OECD (2004) OECD health data 2004. OECD, Paris [http://www.oecd.org/home]
- Ojen J Affect Disord. 1995;33:159. doi: 10.1016/0165-0327(94)00064-G. [DOI] [PubMed] [Google Scholar]
- Ormel Arch Gen Psychiatry. 2000;57:381. doi: 10.1001/archpsyc.57.4.381. [DOI] [PubMed] [Google Scholar]
- Ormel Am J Public Health. 1993;83:385. doi: 10.2105/ajph.83.3.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Östling S, Skoog I. Psychotic symptoms and paranoid ideation in a non-demented population-based sample of the very old. Arch Gen Psychiatry. 2002;59:53–59. doi: 10.1001/archpsyc.59.1.53. [DOI] [PubMed] [Google Scholar]
- Oswald Arch Gerontol Geriatr. 1985;4:299. doi: 10.1016/0167-4943(85)90037-8. [DOI] [PubMed] [Google Scholar]
- Pahkala Soc Psychiatry Psychiatr Epidemiol. 1988;30:99. doi: 10.1007/BF00802037. [DOI] [PubMed] [Google Scholar]
- Picket J Epidemiol Community Health. 2001;55:111. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince Psychol Med. 1997;27:311. doi: 10.1017/S0033291796004473. [DOI] [PubMed] [Google Scholar]
- Prince Br J Psychiatry. 1999;174:330. doi: 10.1192/bjp.174.4.330. [DOI] [PubMed] [Google Scholar]
- Prince Br J Psychiatry. 1999;174:339. doi: 10.1192/bjp.174.4.339. [DOI] [PubMed] [Google Scholar]
- Pulska Int J Geriatr Psychiatry. 1997;12:942. doi: 10.1002/(SICI)1099-1166(199709)12:9<942::AID-GPS668>3.3.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- Radloff Appl Psychol Meas. 1977;1:385. [Google Scholar]
- Roelands Neuroepidemiology. 1994;13:155. doi: 10.1159/000110374. [DOI] [PubMed] [Google Scholar]
- Skoog Int Psychogeriatr. 1993;5:33. doi: 10.1017/S1041610293001371. [DOI] [PubMed] [Google Scholar]
- Turrina Int J Geriatr Psychiatry. 1991;6:647. [Google Scholar]
- Wensing Health Policy. 2004;68:353. doi: 10.1016/j.healthpol.2003.10.010. [DOI] [PubMed] [Google Scholar]
- Wilson Br J Psychiatry. 1999;175:549. doi: 10.1192/bjp.175.6.549. [DOI] [PubMed] [Google Scholar]
- World Health Organisation (2001) WHO atlas, country profiles on mental health. World Health Organisation, Geneva