Abstract
Objective:
UEscope is a new angulated videolaryngoscope (VL). This review aimed to describe the features of UEscope and provide clinical evidences regarding the efficacy and safety of this video device in adult tracheal intubation and its roles in airway management teaching.
Data Sources:
The Wan Fang Data, CNKI, PubMed, Embase, Cochrane Library, and Google Scholar were searched for relevant English and Chinese articles published up to January 15, 2017, using the following keywords: “HC video laryngoscope”, “UE videolaryngoscope”, “video laryngoscope”, and “videolaryngoscopy”.
Study Selection:
Human case reports, case series, observable studies, and randomized controlled clinical trials were included in our search. The results of these studies and their reference lists were cross-referenced to identify a common theme.
Results:
UEscope features the low-profile portable design, intermediate blade curvatures, all-angle adjustable monitor, effective anti-fog mechanisms, and built-in video recording function. During the past 5 years, there have been a number of clinical studies assessing the application and roles of UEscope in airway management and education. As compared with direct laryngoscope, UEscope improves laryngeal visualization, decreases intubation time (IT), and increases intubation success rate in adult patients with normal and difficult airways. These findings are somewhat different from the previous results regarding the other angulated VLs; they can provide an improved laryngeal view, but no conclusive benefits with regard to IT and intubation success rate. Furthermore, UEscope has extensively been used for intubation teaching and shown a number of advantages.
Conclusions:
UEscope can be used as a primary intubation tool and may provide more benefits than other VLs in patients with normal and difficult airways. However, more studies with large sample are still needed to address some open questions about clinical performance of this new VL.
Keywords: Airway Management, Direct Laryngoscope, Performance, Videolaryngoscope
INTRODUCTION
Since the introduction of Macintosh and Miller blades in the 1940s, direct laryngoscope (DL) has been the gold standard tool to facilitate tracheal intubation. Due to the need to obtain a line of sight by aligning oral, laryngeal, and pharyngeal axes, however, the intubation with a DL is a complex technical skill.[1] It is reported that the intubation success rate with a DL is only 50% in novices and a success rate of 90% cannot be expected until fifty intubations have been performed.[2] Thus, difficulty in intubation with a DL is a common problem in clinical practice, and complications associated with intubation using a DL are the main causes of perioperative morbidity and mortality.[3,4]
Advancements in science and technology have made a possibility to develop the alternative indirect devices that can acquire the laryngeal view through a mini camera placed at the blade tip, transmitting it to a video monitor independent of the line of sight. This has led to the development of videolaryngoscope (VL). Unlike DL, VL can enable the intubators to visualize the glottis indirectly, with a wide viewing angle and without the need for alignment of the airway axes. Thus, VL has been seen as a revolutionary step in intubation technology and resulted in the striking changes on airway management strategy.[5] As yet, there are a number of commercial VLs available, with the number constantly increasing and many existing devices being modified. The features of each particular VL may offer advantages or disadvantages, depending on the situations the clinicians have to manage.[6] The aim of this study was to describe the features of a new VL, UEscope, and provide clinical evidences regarding efficacy and safety of this device in adult tracheal intubation and its roles in modern airway management teaching according to the literatures published in the past 5 years.
UESCOPE'S FEATURES
UEscope was created by the Zhejiang UE Medical Corp., (Zhejiang, China; www.ueworld.com) and introduced into clinical practice in 2010. Before 2012, this device was named as HC VL. Since 2013, it was renamed as UEscope and has been available in the Asian, American, and European markets. UEscope is a VL with angulated blade or Miller blade available for use in patients from neonates to large adults and can provide high-quality, magnified airway images on a 2.5-inch portable color monitor [Figure 1]. The main design features are portable and ergonomic. The overall height and weight are <20 cm and <200 g, respectively. A streamlined slim handle makes it very easy to be manipulated by intubators. All-angle adjustable monitor may not only improve flexibility of device insertion, but also can make UEscope easily viewable for teaching, training, and educational purposes.[7,8] Moreover, its monitor is attached on the top of the handle, allowing the operator to focus on patient's face and monitor simultaneously.[6] Bayonet connection between the handle and monitor can effectively prevent their disconnection and image interruption. In addition, UEscope has functional design for saving intubation pictures and video images as a digital airway recorder.[9]
Figure 1.
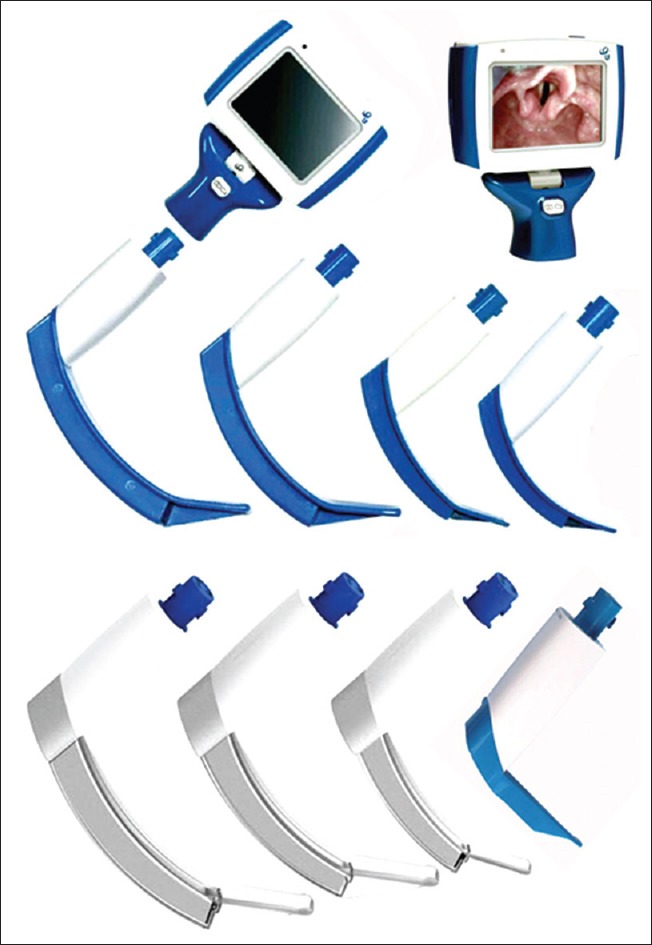
UEscopes. From left to right: Upper row, four reusable angulated blades (sizes 1–4); The bottom row, three disposable devices with angulated blades (sizes 2–4) and one reusable device with size 1 Miller blade. A separable 2.5-inch pocket LCD color monitor can be used for all models. The recommended angulated blade sizes are size 1 for infant and children aged 0–2 years, size 2 for children aged 2–6 years, size 3 for children aged >6 years and small adults, and size 4 for normal-obese adult patients. The recommended Miller blade sizes are size 0 for neonates and size 1 for infants and children aged <2 years.
UEscope has reusable and disposable device designs which are commercially available. A monitor can be used for all devices. The reusable device consists of an angulated blade with the handle and a monitor.[7] There are four-size reusable angulated blades (1–4) and two-size Miller blades (0 and 1) available. The reusable blades have a water-tight design and may be disinfected in hygienic traps. The edges of the blade are slanted to avoid damage to the upper airway.[10] The disposable device includes three main parts: the handle with camera stick, monitor, and transparent angulated plastic blade sheath. The camera is installed on the tip of the camera stick. The disposable plastic blade sheath can cover the camera stick completely, in such a way that no part of camera stick comes in direct contact with patient's mouth. Currently, UEscope has three-size disposable angulated blade sheaths (sizes 2–4). The reusable blade has an effective build-in anti-fog mechanism with multiple heating elements, and the disposable plastic blade sheath has a special anti-fog coating on its anterior transparent window.[1]
The angulated blade design of UEscope is significantly different from those of sharply angulated VLs, such as Glidescope (Verathon Medical, Bothell, WA, USA), McGrath (Aircraft Medical, Edinburgh, Scotland), and Storz D-Blade (KARL STORZ Endoscopy, Tuttlingen, Germany) devices. The upward angle of UEscope blade is about 40°, which is larger than that of Macintosh DL, but less than that of Glidescope, McGrath, and Storz D-Blade VLs [Figure 2]. Especially, Glidescope blade is curved upward with a 60° angle in the midline and the camera is located at a marked inflection point from which the distal portion of blade continues straightforward for another 58 mm.[6] Due to a 60° angle curvature of Glidescope blade, the field of view of camera located at the inflection point is not wide enough to cover the tangent of distal half of the blade, resulting in a blind area below the blade tip, which is 2 mm or 13 mm in the small- or medium-sized blades of original Glidescope VL, respectively.[11] The Storz D-Blade VL is more acutely angulated than Glidescope device, and the optical component is carried more distally than it is on Glidescope device.[12] The sharply angled blade is helpful to insert the device around the anatomic curve of the upper airway and to provide an improved laryngeal visualization by seeing “around the corner” in difficult airway situations.[13] In fact, Glidescope, McGrath, and Storz D-Blade VLs are specially designed for managing difficult airways. However, relatively cumbersome and long handles of Glidescope and Storz D-Blade VLs can lead to difficulty in the device insertion.[1,6] Furthermore, the difference in their projected video images may present a challenge for tube passage for some intubators when using Storz D-Blade VL, particularly for those who are more experienced with the more proximal lens location of Glidescope device.[12] Since the video lens of Storz D-Blade VL is very close to the tip of the blade, it is also more difficult to position the tracheal tube in front of the glottis.[14] When tracheal intubation is performed with sharply angulated VLs, thus, the ability to expose the larynx does not correlate with successful intubation, i.e., difficulty in passing the tube into the trachea through the glottis is a frequently troublesome problem.[15] That is, a good laryngeal view does not always ensure easy intubation. This may be one of the reasons why they are useful for difficult intubations but slow down easy intubations.[16]
Figure 2.
Blade shapes of various videolaryngoscopes. (a) Storz C-MAC videolaryngoscope (Macintosh type); (b) Storz D-Blade videolaryngoscope (angulated type); (c) Glidescope videolaryngoscope (angulated type); (d) McGrath series 5 videolaryngoscope (angulated type); (e) UEscope (angulated type); (f) Pentax-airway scope (guided-channel type).
In contrast, the location of UEscope's camera and the inflection point of the blade are between Glidescope and Storz D-Blade VLs. As the camera's field of vision covers the tangent of the distal half of blades, UEscope has no blind area below the blade tip and provides a panoramic view of the larynx, from above the epiglottis and posterior to the base of the tongue. These features of UEscope are designed for improvement of intubation performance and for use in normal and difficult airways.[1,7,8,9,10]
INTUBATION TECHNIQUE WITH UESCOPE
Just as other angulated VLs, UEscope is inserted along the midline of the mouth, and no sweep of the tongue is required.[1,7] Once the blade is in the mouth, it is gradually moved in the midline along the tongue into the vallecula. Unlike DL, the blade position of UEscope is obtained by rotating the device around the natural curvature of the upper airway and it does not involve direct lifting of the tongue to obtain the best laryngeal view. If a poor laryngeal view is obtained, the optimization maneuver involves rocking the handle toward the intubators. After the larynx is adequately exposed, the styletted tracheal tube is inserted into the mouth along with the right side of the blade. When the tip of the tracheal tube reaches the glottis, the stylet is withdrawn and the tracheal tube is advanced downward into the trachea.[8]
Technical tips and troubleshooting
Familiarity with the nuances of UEscope is critical prior to use in patients, and intubators should be trained on the utilization of this device. One common mistake is to place the blade tip too close to the glottis, especially for novice intubator. Both withdrawing the blade slightly and providing more of a “bird's eye” view allow more space for passage of tracheal tube and lessen the angle at which the tracheal tube must pass.[1]
As the tracheal tube has to be introduced “around the corner,” a rigid stylet is recommended to preshape the tracheal tube to match the blade's curvature. The manufacturer specifically supplies the bespoke stylets for adult patients with normal and difficult airways. In adult patients with a normal airway, Gao et al.[17] show that both 40° and 60° angles of styletted tracheal tube may ensure successful intubation with UEscope, but a 60° angle stylet results in a higher first-attempt intubation success (FAIS) and a shorter intubation time (IT).
To minimize the risk of airway trauma during laryngoscopy and intubation with UEscope, a four-step technique is recommended.[14] To facilitate insertion of the tube into the trachea, moreover, a slight rotation of the tracheal tube is required after removing the stylet in some cases.[8]
PERFORMANCE OF UESCOPE VERSUS DIRECT LARYNGOSCOPE
Normal airway
Orotracheal intubation
In a large randomized controlled trial (RCT) including 600 adult patients, Wang et al.[18] compared the performance of UEscope and Macintosh DL and revealed that UEscope provided a better laryngeal view, a higher FAIS, and the shorter times required for laryngeal visualization and intubation, but the two devices were comparable in terms of intubation complications. Similarly, two RCTs in patients with a normal airway showed that the laryngeal visualization was improved and the need of cricoid pressure during laryngoscopy and times required for laryngeal visualization and intubation were decreased with UEscope compared to Macintosh DL, but the incidence of airway traumatic complications was not different between the two devices.[19,20]
In 100 patients aged 32–68 years, Yang[21] found that the laryngeal view and intubation success rate were not significantly different between UEscope and Macintosh DL, but IT was significantly shorter, and severity of postoperative sore throat (POST) was decreased with UEscope. In a RCT including 72 adult patients, Sun et al.[22] demonstrated that an improved laryngeal view was obtained with UEscope, but IT and hemodynamic responses to intubation (HRTI) were not significantly different between UEscope and Macintosh DL.
Nasotracheal intubation
Two RCTs in adult patients undergoing elective maxillofacial surgery and requiring nasotracheal intubation showed that, compared with Macintosh DL, UEscope provided a better laryngeal view, a less need of adjuncts, a higher FAIS, a shorter IT, and a weaker HRTI.[23,24]
Double-lumen tube intubation
In a RCT including 70 patients aged 18–60 years who underwent elective thoracic surgery, Gong et al.[25] compared the placement of the double-lumen tube using UEscope and Macintosh DL and revealed that UEscope produced a better laryngeal view, but offered a longer IT. The time required for laryngeal visualization and HRTI were not significantly different between the two devices. Furthermore, they found that the cricoid pressure improved the success rate of the double-lumen tube placement with both devices. In 80 patients aged 19–65 years who underwent elective thoracic surgery, Yang et al.[26] used the Macintosh DL as control to evaluate the efficacy and safety of UEscope for double-lumen tube placement and showed that the laryngeal visualization and intubation manipulations were easier, IT was shorter, and HRTI was weaker with UEscope, but airway traumatic complications were comparable between the two devices. In sixty adult patients undergoing general thoracic surgery, Hu[27] demonstrated that the left double-lumen tube placement using UEscope compared with Macintosh DL was associated with a shorter IT, a higher success rate of passing the tube into the targeted bronchia, and a lower incidence of POST, but HRTI did not significantly differ between the two devices.
Difficult airway
Management of difficult airways is a challenge for anesthesiologists. Since the original aim of VL design is to solve a main issue of difficult airways, difficult intubation, it has rapidly become a first-line strategy for potential and/or encountered difficult intubations. In fact, most of the current algorithms for difficult airway management recommend VL as a rescue tool for difficult or failed intubation with a DL.[28,29,30] Hitherto, there have been many studies assessing the application and role of UEscope in difficult airway management.
In 40 patients with predicted difficult airways, Zeng et al.[31] compared the tracheal intubation using UEscope and Macintosh DL and showed that an improved laryngeal view was obtained with UEscope, but intubation success rate, number of intubation attempts (NIA), and IT were comparable with the two devices. Interestingly, in four patients with failed intubation with Macintosh DL due to a Cormack and Lehane class 4, all rescuing intubations with UEscope were success.
Patients with cervical spine injury often require the use of semirigid cervical collar or manual in-line stabilization (MILS) to prevent neck movements, which may cause the poor laryngeal visualization with a DL, leading to difficulty in intubation.[32,33,34] In a RCT including 120 patients aged 18–60 years with MILS, An et al.[7] applied Macintosh DL as control device to assess the clinical efficacy of UEscope for orotracheal intubation. They showed that UEscope provided an improved laryngeal view, a higher intubation success rate, an easier intubation procedure, and a weaker HRTI, but resulted in a longer time required for laryngeal visualization. In contrast, three other RCTs comparing their intubation performance in patients with MILS showed that the IT was decreased with UEscope.[35,36,37] Furthermore, similar results were also obtained in high-level cervical spine injury patients.[38] Thus, it is concluded that UEscope is a useful device for tracheal intubation in patients with cervical spine injury and MILS.[7,35,36,37,38]
Airway management of obese patients is challenging because the obese body habitus can make mask ventilation and tracheal intubation technically difficult.[32] In a RCT conducted on 80 obese patients aged 37–65 years with a body mass index >30 kg/m2, Wang and Zhang[39] compared the feasibility and safety of UEscope and Macintosh DL. They demonstrated that the FAIS was increased and incidences of airway traumatic complications and POST were decreased with UEscope, but HRTI did not significantly differ between the two devices.
In adult patients with predicted difficult airways who underwent cerebral aneurysm embolization, Liu et al.[40] used the Macintosh DL as control device to evaluate performance and safety of UEscope. They found that UEscope decreased IT, attenuated HRTI, and reduced the incidence of POST and hoarseness.
In a RCT including 56 patients with known difficult airways due to severe post-burn scar contracture of the face and neck, Li et al.[41] compared the clinical efficacy and safety of orotracheal intubation using UEscope and Macintosh DL. They showed that the laryngeal visualization was improved, intubation success rate was increased, and NIA and incidence of traumatic airway complications were decreased with UEscope. In five patients with failed intubation using a DL, moreover, successful intubation was achieved with UEscope. In 48 adult patients with difficult intubation using a DL, Wang and Xue[42] reported that UEscope improved the laryngeal visualization and achieved successful intubation in all patients.
Finally, Yang et al.[43] compared the performance and safety of UEscope and Macintosh DL for nasotracheal intubation in seventy patients undergoing maxillofacial surgery with predicted difficult airways. They showed that UEscope improved laryngeal visualization, increased intubation success rate, and decreased NIA, IT, and needs of adjuncts.
Emergency airway
Patients requiring tracheal intubations in emergency department, intensive care unit, and prehospital setting are typical emergency conditions associated with hemodynamic disorders and respiratory crisis. Moreover, these patients often have a high risk of difficult laryngoscopy and intubation, even for the clinicians with adequate airway management skills. If inexperienced clinicians are responsible for managing the airway under such challenging situations, the risk of difficult laryngoscopy and intubation can be further compounded.[32] Thus, there is an increased incidence of complications during emergency intubation compared with elective intubation in the operating room.[4] Given that the goal of emergency intubation is FAIS, the use of VL in emergency airway management has significantly grown and been shown to increase FAIS, especially for patients with difficult airway predictors and those with failed attempts with a DL.[44,45]
In a RCT including 265 patients aged 16–81 years and requiring intubation in emergency department, Wang et al.[46] compared the efficacy and safety of UEscope and Macintosh DL when intubation was performed by emergency attending physicians. They found that, in patients with a Cormack-Lehane class 3 or 4, UEscope was associated with significantly decreased times to laryngeal visualization and intubation, increased FAIS, and reduced incidences of traumatic airway complications and unintentional esophageal intubation. Furthermore, the results obtained by Pan et al.[47] in 40 patients with a Cormack-Lehane class 3 or 4 and undergoing emergency intubation are the same as the findings of Wang et al.’ study.[46]
By a RCT, Pan et al.[9] evaluated the efficacy of UEscope and DL for emergency intubation by unskilled residents and experienced attending physicians. They showed that, when emergency intubation was performed with a DL, unskilled residents compared to experienced attending physicians had the lower rates of successful laryngeal visualization and FAIS, an increased NIA, a prolonged IT, and an increased incidence of intubation complications. When emergency intubation was performed with UEscope, however, these differences were no longer significant between unskilled and experienced clinicians. Thus, they conclude that UEscope can improve the unskilled emergency physicians’ competence for intubation. Furthermore, several RCTs comparing the efficacy and safety of UEscope and DL for emergency intubation also demonstrated that UEscope provided a better laryngeal view, shorter times for laryngeal visualization and intubation, a higher intubation success rate, a better oxygenation, and a lower incidence of intubation complications.[48,49,50,51,52]
In 70 patients with cervical spine injury who required emergency intubation, Mao and Ling[53] compared UEscope and Macintosh DL and showed that UEscope improved laryngeal view, decreased IT, increased FAIS, and reduced traumatic airway complications. In a prehospital setting, two RCTs comparing the performance of UEscope and DL for emergency intubation demonstrate that laryngeal visualization is improved, times for laryngeal visualization and intubation are reduced, and FAIS and total intubation success rate are increased with UEscope.[54,55]
PERFORMANCE OF UESCOPE VERSUS OTHER VIDEOLARYNGOSCOPES
There are many VLs available and their efficacies maybe different among these devices due to various designs and shapes. To facilitate the suitable choice of these devices in airway management, comparing the performance of different devices in patients with various conditions is needed. In a RCT including 120 adult patients with MILS, An et al.[7] showed that the time required for laryngeal visualization was decreased and the ease of orotracheal intubation was improved with UEscope compared to Glidescope VL.
All the four RCTs carried out in patients with normal airways demonstrate that the laryngeal views, IT, FAIS, and total intubation success rate are not significantly different between UEscope and Airtraq laryngoscope (Prodol, Vizcaya, Spain).[56,57,58,59,60,61] However, one of these trials finds that duration of heart rate increases after intubation with Glidescope VL and UEscope is longer than that with Airtraq laryngoscope, and the incidence of postoperative hoarseness and sore throat is significantly higher with Airtraq laryngoscope compared to Glidescope VL and UEscope.[59]
COMBINED USE OF UESCOPE AND OTHER DEVICES
With the evidence available in favor of VL, most anesthetists will rely on the VLs when confronted with a difficult intubation.[12] However, when patient is already anesthetized and the intubation with a VL fails, only a limited number of options remain and no uniformity of strategy to manage VL failure is recommended. The available evidence supports the usefulness of combined VL and other devices (including tube introducer, fiber optic bronchoscope [FOB], Bonfils intubation fiberscope, and Boedeker intubation forceps) in such difficult conditions.[60,61,62,63] There have also been some trials comparing the safety and efficacy of combined UEscope and other devices.
In a RCT including 90 adult patients with a normal airway, Zhao and An[64] assessed the clinical performance and safety of combined FOB and UEscope for orotracheal intubation. The patients were randomly assigned to receive the FOB, UEscope, and a combination of FOB with UEscope for intubations. The results showed no significant differences among the three techniques in the NIA, and between UEscope and combined techniques in the times required for laryngeal visualization and intubation. However, times required for laryngeal visualization and intubation were significantly longer when using a FOB technique than when using a combined technique. In elderly patients with Mallampati airway class 3 or 4, He et al.[65] used the UEscope as control to evaluate the clinical value of combined UEscope and FOB for orotracheal intubation and found that the times required for laryngeal visualization and intubation, NIA, HRTI, incidences of airway traumatic complications, and POST were decreased with a combined technique. In patients aged 20–60 years with a predicted difficult airway, He[66] showed that, compared to the FOB technique, combined FOB and UEscope decreased the times required for laryngeal visualization and intubation, NIA, and incidence of airway traumatic complications, but the two techniques were comparable with respect to HRTI. In patients with cervical spine immobilization who required nasotracheal intubation, combined UEscope and FOB provides a higher FAIS, a shorter IT, and a lower incidence of POST than the FOB technique.[67]
In adult patients with predicted difficult intubations, Shan et al.[68] assessed the clinical application of combined rigid bronchoscope and UEscope and showed that combined technique was superior to individual use of UEscope in terms of IT, NIA, and incidence of POST, but the two techniques were similar in terms of HRTI. In 80 adult patients with predicted difficult airways, moreover, Liu et al.[69] assessed the clinical performance of combined FOB and UEscope for double-lumen tube placement. They demonstrated that, compared to the FOB technique, combined technique provided an easier procedure, a higher FAIS, a weaker HRTI, and a lower incidence of POST.
UESCOPE AND TRACHEAL INTUBATION TEACHING
Teaching tracheal intubation with a DL involving the line-of-sight techniques is difficult because the teacher cannot share the airway images with student. In contrast, VL provides a shared view for teacher and student, i.e., the high-quality, magnified airway images on VL monitor allow teachers to explain the anatomy of the upper airway and procedures of laryngoscopy and intubation to students. Furthermore, when a student is endeavoring intubation, a teacher can see the video monitor and provide a feedback.[32]
Due to a portable design and an all-angle adjustable high-resolution video monitor with recording function, UEscope has extensively been used for tracheal intubation teaching and shown a number of advantages.[8,70,71,72,73] First, UEscope allows for skill training on simulator outside operating room, reducing the potential risk for patient injury when the student has only rudimentary skill.[8] Second, UEscope is a better educational tool than the “look over my shoulder” training method and allows the teacher to see in detail what the student is doing while performing intubation. Third, when the training is performed in the operating room, because the airway images can be seen by the teacher and student, and the procedure can be optimized in real time, it is more likely that the students can complete a tracheal intubation themselves without teacher taking over. This is especially useful for rapid sequence inductions and in patients at the risks of hypoxia and aspiration.[74] Fourth, during airway management training, the shared view on monitor can create a dynamic interaction, which facilitates teamwork and communication of the whole training team. This may stimulate enthusiasm of the students to learn intubation skill, improving the quality and outcomes of airway management training. Fifth, the ability to record the intubation as a “digital airway recorder” is useful for training as it allows the teacher to review with a student at leisure.[9]
The available evidence shows that the visual intubation teaching method with the UEscope is superior to traditional teaching method with a DL in terms of the training outcomes and satisfaction grades of students. Furthermore, acquisition of intubation skill with the UEscope by novice anesthesiologists is easier than attainment of intubation skill with a DL.[75] In addition, training novice anesthesiologists in intubation skill with a DL is more effective when using UEscope than when using Macintosh DL.[72]
Comments
Although VL is initially designed as difficult intubation device, nothing can guarantee intubation success. The current airway assessment is predicated on difficult intubation with a DL, but a predicated difficult intubation with a DL does not mean that intubation with a VL will be difficult and vice versa.[73] Thus, it is important to take all the essential steps to maximize FAIS, especially for patients with difficult airways and emergency conditions.[44,45] One key of such steps is choosing the best tool for the job. It is suggested that the optimal VL should be offered to all patients and not only in those considered most difficult. This will provide the best care in any condition, assuring an acquirement in the experience and competence with techniques and an improvement in the comprehension of their limitations and value.[74] Recently, the use of VL as a standard care to replace DL for all tracheal intubations has been appealed by airway experts.[75]
The available evidence shows that, compared with a DL, UEscope provides an improved laryngeal view, a decreased IT, and an increased intubation success rate in adult patients with normal and difficult airways. These findings are somewhat different from the results of previous publications regarding other angulated VLs, such as Glidescope device; they can improve laryngeal visualization in patients with normal and difficult airways, but there are no conclusive benefits with regard to IT and intubation success, especially for patients with normal airways.[5,6] Typically, they are useful for difficult intubations, but slow down easy intubations; they are associated with a higher intubation success rate and a faster IT only for unskilled intubators, but provide no benefit in either of these outcomes with skilled intubators.[5,76,77,78] Furthermore, a comparative study in patients with cervical spine immobilization shows that the time for laryngeal visualization is decreased and the ease of intubation is improved with UEscope when compared with Glidescope VL.[7] Accordingly, we reckon that UEscope may provide more benefits than other angulated VLs in patients with normal and difficult airways.
When comparing these findings of UEscope and other VLs obtained from different studies, however, there are several important considerations. First, the brand and blade design of VL have been shown to affect suitability for various clinical indications, the use of adjuncts, and volume of the oropharynx within which to maneuver. Moreover, slight design modification may significantly change the success rate and IT with VLs.[79,80] Thus, different designs may be attributable to more benefits with UEscope. Second, all the available trials comparing the performance of UEscope and DL are executed in Chinese patients. It is unclear whether these findings can be generalized into non-Chinese patients. Third, some of the clinical trials comparing UEscope with DL lack the definitions of competence for intubators. It is thus unclear whether different learning curves of studied devices would have been attributable to the study conclusions. Fourth, there are inconsistent conclusions as to whether or not UEscope is less likely to be stressful and traumatic than the DL, especially for patients with difficult airways. Fifth, there are many VLs available, but only few clinical trials have compared the clinical performance of UEscope with Glidescope VL and Airtraq laryngoscope. Thus, the lack of enough evidence gives overall recommendations as to the choice of these devices in various airway conditions. Sixth, some of the clinical trials comparing UEscope with DL have small clinical sample sizes and are not very powerful to provide clinical evidence.
CONCLUSIONS
As a new intubation tool, UEscope has several interesting features including the intermediate blade curvatures, the blades available for use from neonates to large adults, a compact overall size, a low weight, all-angle adjustable high-resolution monitor, effective anti-fog mechanisms, and built-in video recording function. These features make the use of UEscope very appealing. With a number of clinical studies published in the recent years, its roles in airway management and education have been well established. The available evidence supports that UEscope can be used as a primary intubation tool, particularly when the intubators have less experience of airway management and when preoperative airway screening suggests intubation difficult. However, some open questions remain: is UEscope the best care for all patients, including non-Chinese patients? Other than the limited mouth open, are there other causes of difficult intubation with UEscope? Can such difficulties be predicted preoperatively? Is intubation with UEscope less likely to be stressful and traumatic? To address these issues, more comparative studies with large samples are still needed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Yi Cui
REFERENCES
- 1.Xue FS, Liu QJ, Li HX, Liu YY. Videolaryngoscopy assisted intubation – New era for airway management. J Anesth Perioper Med. 2016;3:258–69. doi: 10.24015/JAPM.2016.0035. [Google Scholar]
- 2.Mulcaster JT, Mills J, Hung OR, MacQuarrie K, Law JA, Pytka S, et al. Laryngoscopic intubation: Learning and performance. Anesthesiology. 2003;98:23–7. doi: 10.1097/00000542-200301000-00007. doi: 0000542-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Caplan RA, Posner KL, Ward RJ, Cheney FW. Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology. 1990;72:828–33. doi: 10.1097/00000542-199005000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Cook TM, Woodall N, Frerk C. Fourth National Audit Project. Major complications of airway management in the UK: Results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: Anaesthesia. Br J Anaesth. 2011;106:617–31. doi: 10.1093/bja/aer058. doi: 10.1093/bja/aer058. [DOI] [PubMed] [Google Scholar]
- 5.Paolini JB, Donati F, Drolet P. Review article: Video-laryngoscopy: Another tool for difficult intubation or a new paradigm in airway management? Can J Anaesth. 2013;60:184–91. doi: 10.1007/s12630-012-9859-5. doi: 10.1007/s12630-012-9859-5. [DOI] [PubMed] [Google Scholar]
- 6.Niforopoulou P, Pantazopoulos I, Demestiha T, Koudouna E, Xanthos T. Video-laryngoscopes in the adult airway management: A topical review of the literature. Acta Anaesthesiol Scand. 2010;54:1050–61. doi: 10.1111/j.1399-6576.2010.02285.x. doi: 10.1111/j.1399-6576.2010.02285.x. [DOI] [PubMed] [Google Scholar]
- 7.An N, Chen M, Liu P, Yao SL, Yang D, Yang L. Comparison of tracheal intubations using HC visual laryngoscope, Glidescope video laryngoscope and Macintosh direct laryngoscope in patients with cervical spine immobilization. Acta Med Univ Sci Technol Huazhong. 2013;42:405–8. doi: 10.3870/j.issn.1672-0741.2013.04.007. [Google Scholar]
- 8.Fan XH, Wan J, Chen H, Ma Y, Hou J. The role of HC videolaryngoscope in anesthesiology practice by clinical students. J Mod Med Health. 2012;28:1093–4. [Google Scholar]
- 9.Pan LF, Yu L, Pei HH, Fan Y, Wang XB, Su LJ, et al. The usage of HC videolaryngoscope for emergency tracheal intubation by unskilled junior emergency resident doctors (in Chinese) Chin J Emerg Med. 2016;25:910–4. doi: 10.3760/cma.j.issn.1671-0282.2016.07.013. [Google Scholar]
- 10.Wan XX. Comparative analysis of application of domestic UE video laryngoscope and conventional laryngoscope in pediatric tracheal intubation (in Chinese) Mod J Interg Tradit Chin Wes Med. 2015;24:1232–4. doi: 10.3969/j.issn.1008-8849.2015.11.035. [Google Scholar]
- 11.Hirabayashi Y, Otsuka Y. Apparent blind spot with the GlideScope video laryngoscope. Br J Anaesth. 2009;103:461–2. doi: 10.1093/bja/aep220. doi: 10.1093/bja/aep220. [DOI] [PubMed] [Google Scholar]
- 12.Aziz MF, Abrons RO, Cattano D, Bayman EO, Swanson DE, Hagberg CA, et al. First-attempt intubation success of video laryngoscopy in patients with anticipated difficult direct laryngoscopy: A multicenter randomized controlled trial comparing the C-MAC D-blade versus the GlideScope in a mixed provider and diverse patient population. Anesth Analg. 2016;122:740–50. doi: 10.1213/ANE.0000000000001084. doi: 10.1213/ANE.0000000000001084. [DOI] [PubMed] [Google Scholar]
- 13.Serocki G, Neumann T, Scharf E, Dörges V, Cavus E. Indirect videolaryngoscopy with C-MAC D-Blade and GlideScope: A randomized, controlled comparison in patients with suspected difficult airways. Minerva Anestesiol. 2013;79:121–9. [PubMed] [Google Scholar]
- 14.Holm-Knudsen R. The difficult pediatric airway – A review of new devices for indirect laryngoscopy in children younger than two years of age. Paediatr Anaesth. 2011;21:98–103. doi: 10.1111/j.1460-9592.2010.03487.x. doi: 10.1111/j.1460-9592.2010.03487.x. [DOI] [PubMed] [Google Scholar]
- 15.Levitan RM, Heitz JW, Sweeney M, Cooper RM. The complexities of tracheal intubation with direct laryngoscopy and alternative intubation devices. Ann Emerg Med. 2011;57:240–7. doi: 10.1016/j.annemergmed.2010.05.035. doi: 10.1016/j.annemergmed.2010.05.035. [DOI] [PubMed] [Google Scholar]
- 16.Xue FS, Liu GP, Sun C. Videolaryngoscope as a standard intubation device. Br J Anaesth. 2015;115:137–8. doi: 10.1093/bja/aev175. doi: 10.1093/bja/aev175. [DOI] [PubMed] [Google Scholar]
- 17.Gao ZY, Guo WW, He J, Luo Q, Tan J. The effects of angles of styletted tracheal tubes on intubation performance of HC videolaryngoscope (in Chinese) Sichuan Med J. 2016;37:98–100. doi: 10.16252/j.cnki.issn1004-0501-2016.01.028. [Google Scholar]
- 18.Wang YL, Qiu YQ, Huang M, Chen Y, He JL, Chen A. Application of HC videolaryngoscope in endotracheal intubation under general anesthesia (in Chinese) China Med Pharm. 2015;5:84–7. [Google Scholar]
- 19.Gong SK, Sun Z, Fan XC, Lv HM, Chu QJ, Zhang W. Comparison of HC video-laryngoscope versus Macintosh laryngoscope for tracheal intubation (in Chinese) Chin J Anesthesiol. 2013;33:76–8. doi: 10.3760/cma.j.issn.0254-1416.2013.01.020. [Google Scholar]
- 20.You ZB, Li M, Huang HH, Wang HQ. Comparative performance of HC video-laryngoscope and Macintosh laryngoscope for tracheal intubation (in Chinese) Chin J Rural Med Pharm. 2016;23:37–8. doi: 10.3969/j.issn.1006-5180.2016.08.021. [Google Scholar]
- 21.Yang Y. The clinical application of HC videolaryngoscope in tracheal intubation with general anesthesia (in Chinese) Guide China Med. 2015;13:65–6. [Google Scholar]
- 22.Sun Z, Gong SK, Han XP, Li PH. Clinical observation of HC videolaryngoscope and Macintosh laryngoscope for orotracheal intubation. J Pract Med. 2013;29:1161–3. doi: 10.3969/j.issn.1006-5725.2013. [Google Scholar]
- 23.Cai L, Zhou JP, Liu DY. Application of HC videolaryngoscope in nasotracheal intubation. Clin Educ Gener Pract. 2012;10:577–8. doi: 10.3969/j.issn.1672-3686.2012.05.037. [Google Scholar]
- 24.Luo SJ, Wang Q, Qiu QP, Chen Y, Peng SF. Application of HC videolaryngoscope for nasotracheal intubation in patients with maxillofacial fractures. Med Inform. 2015;28:20–2. [Google Scholar]
- 25.Gong SK, Sun Z, Li PL Zhang W. Comparison of double-lumen tube placement between HC videolaryngoscope and Macintosh laryngoscope (in Chinese) Chin J Exp Surg. 2013;30:1069–71. doi: 10.3760/cma.j.issn.1001-9030.2013.05.069. [Google Scholar]
- 26.Yang K, Ge KL, Yang R. Clinical study of HC videolaryngoscope for double-lumen tube placement (in Chinese) Zhejiang Med J. 2014;36:1647–9. [Google Scholar]
- 27.Hu FY. Clinical application of UE videolaryngoscope in the placement of left double-lumen tube (in Chinese) J Jiangsu Univ. 2014;24:522–4. doi: 10.13312/j.issn.1671-7783.y140140. [Google Scholar]
- 28.Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on management of the difficult airway. Anesthesiology. 2013;118:251–70. doi: 10.1097/ALN.0b013e31827773b2. doi: 10.1097/ALN.0b013e31827773b2. [DOI] [PubMed] [Google Scholar]
- 29.Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115:827–48. doi: 10.1093/bja/aev371. doi: 10.1093/bja/aev371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Japanese Society of Anesthesiologists. JSA airway management guideline 2014: To improve the safety of induction of anesthesia. J Anesth. 2014;28:482–93. doi: 10.1007/s00540-014-1844-4. doi: 10.1007/s00540-014-1844-4. [DOI] [PubMed] [Google Scholar]
- 31.Zeng Q, Li Q, Wang DQ, Tang SP. Comparative study of HC videolaryngoscope and disposable conventional laryngoscope for tracheal intubation (in Chinese) Clin J Med Off. 2014;42:860–2. doi: 10.3969/j.issn.1671-3826.2014.08.33. [Google Scholar]
- 32.Maldini B, Hodžovic I, Goranovic T, Mesaric J. Challenges in the use of video laryngoscopes. Acta Clin Croat. 2016;55(Suppl 1):41–50. doi: 10.20471/acc.2016.55.s1.05. [PubMed] [Google Scholar]
- 33.Ma LL, Yu XR, Zhu B, Huang YG, Shen JX, Zhang JG. Difficult airway for patients undergoing spine surgeries. Chin Med J. 2016;129:749–50. doi: 10.4103/0366-6999.178033. doi: 10.4103/0366-6999.178033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu M, Li XX, Guo XY, Wang J. Shikani optical stylet versus macintosh laryngoscope for intubation in patients undergoing surgery for cervical spondylosis: A randomized controlled trial. Chin Med J. 2017;130:297–302. doi: 10.4103/0366-6999.198926. doi: 10.4103/0366-6999.198926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cai XF, Chen LF. Comparative analysis of tracheal intubations using HC videolaryngoscope and conventional macintosh laryngoscope in patients with simulated cervical spine immobilization. Mod Diagn Treat. 2014;25:3484–5. [Google Scholar]
- 36.Zhu L, Zhao ZB, Ding MY. Comparative performance of HC videolaryngoscope and traditional Macintosh laryngoscope for endotracheal intubation under general anesthesia. Mod Diagn Treat. 2014;25:5297–8. [Google Scholar]
- 37.Xiang J. Comparative performance of HC videolaryngoscope and Macintosh laryngoscope for intubation under general anesthesia in patients with simulated cervical spine immobilization (in Chinese) Med J Chin PAP. 2014;25:1193–4. doi: 10.3969/j.issn.1004-3594.2014.12.002. [Google Scholar]
- 38.He ZY, Li CM. Selection of tracheal intubation methods with general anesthesia in patients with high-level cervical spine and spinal injury (in Chinese) Qingdao Med J. 2015;47:139–41. doi: 10.3969/j.issn.1006-5571.2015.02.022. [Google Scholar]
- 39.Wang H, Zhang MF. The observation of tracheal intubation with UE videolaryngoscope in obese patients (in Chinese) Zhejiang Med J. 2013;35:1282–3. [Google Scholar]
- 40.Liu XC, Du D, Wu WY, Zhang YX. Application of UE videolaryngoscopy in patients with an abnormal airway anatomy and undergoing cerebral aneurysm embolization (in Chinese) Chin J Clin Anat. 2015;33:479–81. doi: 10.13418/j.issn.1001-165x.2015.04.024. [Google Scholar]
- 41.Li Z, Meng JS, Hu Y. Application of HC videolaryngoscope for endotracheal intubation in patients with difficult airways by burn scar. Pract J Med Pharm. 2013;30:397–8. doi: 10.3969/j.issn.1671-4008.2013.05.006. [Google Scholar]
- 42.Wang TQ, Xue J. Comparative analysis on applications of two laryngoscopes in 48 patients with difficult intubation (in Chinese) Chin Foreign Med Treat. 2013;32:43–5. [Google Scholar]
- 43.Yang XD, Liu RC, Gao L, Li ZZ, Wang XD. Application of HC videolaryngoscope for nasotracheal intubation in patients with predicted difficult airway and undergoing oral maxillofacial surgery. J Pract Stomatol. 2015;31:833–6. doi: 10.3969/j.issn.1001-3733.2015.06.021. [Google Scholar]
- 44.De Jong A, Molinari N, Conseil M, Coisel Y, Pouzeratte Y, Belafia F, et al. Video laryngoscopy versus direct laryngoscopy for orotracheal intubation in the Intensive Care Unit: A systematic review and meta-analysis. Intensive Care Med. 2014;40:629–39. doi: 10.1007/s00134-014-3236-5. doi: 10.1007/s00134-014-3236-5. [DOI] [PubMed] [Google Scholar]
- 45.Ahmadi K, Ebrahimi M, Hashemian AM, Sarshar S, Rahimi-Movaghar V. GlideScope video laryngoscope for difficult intubation in emergency patients: A quasi-randomized controlled trial. Acta Med Iran. 2015;53:738–42. [PubMed] [Google Scholar]
- 46.Wang WL, Wang L, Wang ZH, Li XF, Wang SL. Comparative performance of HC videolaryngoscope and direct laryngoscope for tracheal intubation (in Chinese) Shandong Med J. 2015;55:39–40. doi: 10.3969/j.issn.1002-266X.2015.11.014. [Google Scholar]
- 47.Pan LF, Fang H, Yu L, Dang XY, Shi XY. Application of HC videolaryngoscope in emergency intubation in patients with difficult airways (in Chinese) Shaanxi Med J. 2015;44:1378–80. doi: 10.3969/j.issn.1000-7377.2015.10.047. [Google Scholar]
- 48.Dang XY, Yin MJ, Pan LF, Chen EX, Qin Y. Application of HC videolaryngoscope for urgent intubation in emergency department (in Chinese) Shaanxi Med J. 2013;42:1376–7. doi: 10.3969/j.issn.1000-7377.2013.10.050. [Google Scholar]
- 49.Chen JM, Wang P, Hu XP. Comparative efficacy of HC videolaryngoscope and direct laryngoscope for emergency intubation (in Chinese) Zhejiang J Trauma Surg. 2015;20:1182–4. doi: 10.3969/j.issn.1009-7147.2015.06.056. [Google Scholar]
- 50.Cheng JY, Xu W, Zhan SF. Application of HC videolaryngoscope in emergency intubation (in Chinese) Med Innov China. 2014;11:47–50. doi: 10.3969/j.issn.1674-4985.2014.29.017. [Google Scholar]
- 51.Song ZP, Qu LC, Liu ZY. Application of HC videolaryngoscope in the in-hospital emergency intubation (in Chinese) Jiangxi Med J. 2014;49:907–9. doi: 10.3969/j.issn.1006-2238.2014.09.056. [Google Scholar]
- 52.Li YF, Xiao AF. Application of HC videolaryngoscope in emergency intubation (in Chinese) Heilongjiang Med J. 2014;38:1223–4. doi: 10.3969/j.issn.1004-5775.2014.10.054. [Google Scholar]
- 53.Mao ZH, Ling GQ. Comparison of emergency tracheal intubations using visual laryngoscope and macintosh direct laryngoscope; in patients with cervical spine injury (in Chinese) Chin J Prim Med Pharm. 2017;24:454–5. doi: 10.3760/cma.j.issn.1008-6706.2017.03.034. [Google Scholar]
- 54.Zhai HY. Usability of HC videolaryngoscope in the prehospital emergency intubation (in Chinese) Chin J Trauma Disabil Med. 2014;22:113. doi: 10.13214/j.cnki.cjotadm.2014.14.082. [Google Scholar]
- 55.Qian Y, Xiao ZH, Gu W. Comparative performance of HC videolaryngoscope and macintosh laryngoscope for the prehospital intubation (in Chinese) Mod Med J China. 2014;16:52–3. doi: 10.3969/j.issn.1672-9463.2014.10.016. [Google Scholar]
- 56.Wang WH, Chen L, Hu CH. Comparative performance of Airtraq® laryngoscope, UE videolaryngoscope and macintosh laryngoscope for tracheal intubation in patients undergoing cervical surgery (in Chinese) Shandong Med J. 2016;56:56–7. doi: 10.3969/j.issn.1002-266X.2016.02.023. [Google Scholar]
- 57.Wang WH, Ma L, Li SY. Comparison of hemodynamic responses to intubation with Airtraq® videolaryngoscope, UE videolaryngoscope and Macintosh laryngoscope in elderly patients without difficult intubation (in Chinese) China Mod Med. 2016;23:93–6. [Google Scholar]
- 58.Zhang CX. Clinical performance of two videolaryngoscopes versus direct laryngoscope for endotracheal intubation: A comparative study (in Chinese) Anhui Med J. 2013;34:900–3. doi: 10.3969/j.issn.1000-0399.2013.07.014. [Google Scholar]
- 59.Fang Y, Huang J, Zou ZY. The effects of endotracheal intubation with three videolaryngoscopes (GlideScope, Airtraq and UE) on hemodynamics and postoperative airway complications (in Chinese) J Kunming Med Univ. 2014;35:135–8. doi: 10.3969/j.issn.1003-4706.2014.10.037. [Google Scholar]
- 60.Ohchi F, Komasawa N, Imagawa K, Minami T. Combination of videolaryngoscope and tracheal tube introducer for difficult infant airway management. J Clin Anesth. 2016;33:498–9. doi: 10.1016/j.jclinane.2015.09.006. doi: 10.1016/j.jclinane.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 61.Gupta A, Kapoor D, Awana M, Lehl G. Fiberscope assisted videolaryngoscope intubation in the surgical treatment of TMJ ankylosis. J Maxillofac Oral Surg. 2015;14:484–6. doi: 10.1007/s12663-014-0619-7. doi: 10.1007/s12663-014-0619-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Strøm C, Barnung S, Kristensen MS, Bøttger M, Tvede MF, Rasmussen LS. Tracheal intubation in patients with anticipated difficult airway using Boedeker intubation forceps and McGrath videolaryngoscope. Acta Anaesthesiol Scand. 2015;59:1154–60. doi: 10.1111/aas.12543. doi: 10.1111/aas.12543. [DOI] [PubMed] [Google Scholar]
- 63.Van Zundert AA, Pieters BM. Combined technique using videolaryngoscopy and Bonfils for a difficult airway intubation. Br J Anaesth. 2012;108:327–8. doi: 10.1093/bja/aer471. doi: 10.1093/bja/aer471. [DOI] [PubMed] [Google Scholar]
- 64.Zhao GS, An J. The observation on clinical performance of combined fiberoptic bronchoscope and HC videolaryngoscope for tracheal intubation in general anesthetized patients (in Chinese) China J Endosc. 2014;20:772–4. [Google Scholar]
- 65.He W, Li JQ, Yuan QH, Xie DW, Wei FS, Dai GM, et al. Clinical study of HC videolaryngoscope combined fiberoptic bronchoscope for intubation with general anesthesia in elderly patients (in Chinese) China Med Equip. 2016;13:63–6. doi: 10.3969/J.ISSN.1672-8270.2016.08.019. [Google Scholar]
- 66.He ZY. Performance assessment of combined fiberoptic bronchoscope and UEscope for intubation in patients with predicted difficult airways (in Chinese) China Pract Med. 2015;10:113–4. doi: 10.14163/j.cnki.11-5547/r.2015.08.074. [Google Scholar]
- 67.Hao RZ, Zhou RH, Ao Q. Clinical application of combined rigid bronchoscope and UEscope in patients with difficult intubation (in Chinese) Chin J Clin. 2013;7:11846–7. doi: 10.3877/cma.j.issn.1674-0785.2013.24.183. [Google Scholar]
- 68.Shan HM, Yu L, Wu HF. Application of HC video laryngoscope combined with fiberoptic bronchoscopy in tracheal intubation in patients with cervical spine immobilization (in Chinese) China J Endosc. 2017;23:233–6. doi: 10.3969/j.issn.1007-1989.2017.03.012. [Google Scholar]
- 69.Liu JJ, Wei ZH, Lv HY. Application of videolaryngoscope combined with fiberoptic bronchoscope for double-lumen tube placement in patients with predicted difficult airways (in Chinese) China Mod Doct. 2016;54:100–3. [Google Scholar]
- 70.Wu HJ. Application and outcomes of videolaryngoscope in tracheal intubation training (in Chinese) China Foreign Med Res. 2013;11:24. [Google Scholar]
- 71.Fan JB, Chen L. Experience of using videolaryngoscope in practice teaching of clinical anesthesia. Basic Med Educ. 2015;17:58–9. doi: 10.13754/j.issn2095-1450.2015.01.20. [Google Scholar]
- 72.Long RH, Chen WD, Zhang DF, Shao JL. Comparison of visual and traditional teaching methods for endotracheal intubation teaching of medical students (in Chinese) J Kunming Med Univ. 2015;36:150–2. doi: 10.3969/j.issn.1003-4706.2015.12.039. [Google Scholar]
- 73.Liu YT, Zhao HY, Zhang B. Use and outcomes of the Shikani optical stylet, HC videolaryngoscope and direct laryngoscope in the endotracheal intubation teaching (in Chinese) Xinjiang Med J. 2015;45:274–6. [Google Scholar]
- 74.Asai T. Videolaryngoscopes: Do they have role during rapid-sequence induction of anaesthesia? Br J Anaesth. 2016;116:317–9. doi: 10.1093/bja/aev544. doi: 10.1093/bja/aev544. [DOI] [PubMed] [Google Scholar]
- 75.Aziz MF, Brambrink AM, Healy DW, Willett AW, Shanks A, Tremper T, et al. Success of intubation rescue techniques after failed direct laryngoscopy in adults: A retrospective comparative analysis from the multicenter perioperative outcomes group. Anesthesiology. 2016;125:656–66. doi: 10.1097/ALN.0000000000001267. doi: 10.1097/ALN.0000000000001267. [DOI] [PubMed] [Google Scholar]
- 76.Agrò FE, Doyle DJ, Vennari M. Use of GlideScope® in adults: An overview. Minerva Anestesiol. 2015;81:342–51. [PubMed] [Google Scholar]
- 77.Zaouter C, Calderon J, Hemmerling TM. Videolaryngoscopy as a new standard of care. Br J Anaesth. 2015;114:181–3. doi: 10.1093/bja/aeu266. doi: 10.1093/bja/aeu266. [DOI] [PubMed] [Google Scholar]
- 78.Griesdale DE, Liu D, McKinney J, Choi PT. Glidescope® video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: A systematic review and meta-analysis. Can J Anaesth. 2012;59:41–52. doi: 10.1007/s12630-011-9620-5. doi: 10.1007/s12630-011-9620-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kleine-Brueggeney M, Greif R, Schoettker P, Savoldelli GL, Nabecker S, Theiler LG. Evaluation of six videolaryngoscopes in 720 patients with a simulated difficult airway: A multicentre randomized controlled trial. Br J Anaesth. 2016;116:670–9. doi: 10.1093/bja/aew058. doi: 10.1093/bja/aew058. [DOI] [PubMed] [Google Scholar]
- 80.Yumul R, Elvir-Lazo OL, White PF, Sloninsky A, Kaplan M, Kariger R, et al. Comparison of three video laryngoscopy devices to direct laryngoscopy for intubating obese patients: A randomized controlled trial. J Clin Anesth. 2016;31:71–7. doi: 10.1016/j.jclinane.2015.12.042. doi: 10.1016/j.jclinane.2015.12.042. [DOI] [PubMed] [Google Scholar]



