Abstract
Background:
Rural to urban migration has become a salient feature of the country. However, there is a dearth of study highlighting impact of this movement on mental health of the migrant people.
Aims:
The main objective of the present study was to examine the relationship between specific components of social environment and psychological well-being of migrants in an urban center.
Settings and Design:
The National Capital Territory of Delhi was selected for intensive study and has an exploratory design supported by cross-sectional primary data.
Methodology:
A standardized questionnaire was used to obtain data about the socioeconomic characteristics of the respondents. For measuring the mental well-being, the World Health Organization Well-Being Index (WHO5) was used. The required information was procured through interview method from 1230 sampled respondents.
Statistical Analysis:
Influence of socioeconomic variables on mental well-being of the people was estimated through multivariate logistic regression methods. For different combinations of risk factors, five models were developed based on unstandardized likelihood coefficients.
Results:
Poor mental health was significantly higher among single/widow/divorced/separated (odds ratio [OR] =0.76, P < 0.01), unskilled (OR = 2.26, P < 0.01), daily wager (OR = 2.57, P < 0.01), and illiterate (OR = 2.55, P < 0.01). Longer year of immigration, younger age, and higher income level (P < 0.001) were positively related to mental health. Poor housing conditions (P < 0.001), adjustment problem (P < 0.001), and feeling insecure (P < 0.01) were independent predictors of poor mental health.
Conclusion:
Socioeconomic and environmental problem caused by the migrants and faced by the migrants is required in-depth study to formulate comprehensive policies.
Keywords: Delhi, host society, mental well-being, migrants
INTRODUCTION
Rapid urbanization has become a global phenomenon. The percentage of the population residing in urban areas is projected to gain 3.1 billion, passing from 3.3 billion in 2007 to 6.4 billion in 2050 worldwide. Virtually, all of the world's population growth will be absorbed by the urban areas of the less developed regions, whose population is projected to increase from 2.4 billion in 2007 to 5.3 billion in 2050.[1] The situation in India is not different from the rest of the world. A process of rapid urbanization has already been making strides in the form of the growth of big cities and urban agglomerations due to poverty induced rural-urban migration. In the word of Kingsley Davis, it is a process of “over-urbanization” where in urban misery and rural poverty exist side by side. The present movement toward urban living has become one of the most important global health issues of the 21st century.[2,3] More recently, there is ample evidence indicating toward increasing mental health problems in urban centers of developing countries.[4,5,6]
The idea that urban living is detrimental to mental health is a notion that has received a fair amount of attention, but most of the research has been conducted in developed countries. This has been referred to as the 90/10 gap, where 10% of the research and funding takes place in developing countries which experience 90% of the global burden. As far as the prevalence rate of mental health problem in India is concerned, the numerous epidemiological studies reported varying prevalence rates ranging from 9.5 to 370/1000 population in the country. According to another study, about 20% of the adult population in the community are affected with one or the other psychiatric disorder.[7] Furthermore, numerous studies show great variation in the prevalence rates of all mental disorders between rural and urban areas. According to the previous studies, the prevalence rate was 70.5/1000 for rural areas, 73/1000 for urban areas, and 73/1000 for both rural and urban areas.[8,9]
Considering these points, Delhi is selected for intensive study. Being a capital city of India, it has been experiencing unprecedented and unplanned urbanization from the last few decades. In addition, Delhi provides an ideal setting for intensive study as it represents typical characteristics of urbanization of developing countries in general and of India in particular. Therefore, it is imperative to develop better understanding of the process of urbanization and kinds of environmental influences that have major negative effects on mental well-being of the people through an intensive research. The main objectives of the study are to assess the mental well-being of the intra-country migrants residing in the National Capital Territory of Delhi and also to identify the underlying causes and risk factors for poor mental health. It was hypothesis that the social and cultural changes experienced by the immigrants in the host society are the potential risk factor for mental well-being.
METHODOLOGY
Following literature reviews on social determinants and mental health, a questionnaire was developed suited to the problems and requirement of the study area to collect primary data. Information regarding gender, age, education, occupation, marital status, family structure, year of immigration, housing conditions, accessibility to basic amenities and facilities, and social life were collected.
For measuring mental well-being, the World Health Organization measure of mental well-being (WHO5) was used. The WHO5 is a short, psychometrically sound scale for measuring positive psychological well-being.[10] It consists of five items assessing positive mood, vitality, and general interest over the past 2 weeks. Although a general measure of mental well-being, the scale has actually proven to be a good screening instrument for the detection of depression in the general population.[11,12] The five items of the WHO5 are:
I have felt cheerful and in good spirits
I have felt calm and relaxed
I have felt active and vigorous
I woke up feeling fresh and rested
My daily life has been filled with things that interest me.
Respondents choose a response from “all of the time,” “most of the time,” “more than half of the time,” “less than half of the time,” “some of the time” to “at no time” which is closer to how they have been feeling over the previous 2 weeks. Answers are scored from 0 to 5 and summed to produce a score out of 25. Those scoring below 13 were classified as “cases” as a score below 13 indicates poor well-being and is an indication for testing for depression under International Classification of Diseases, Tenth Edition (Psychiatric Research Unit, WHO Collaborating Center for Mental Health 1998).
Data collection
The study is based on primary data which were obtained from a cross-sectional field survey conducted from August to November 2012 with the help of a questionnaire. For the collection of data, job-generating centers, i.e., service center (both private and public), construction companies, commercial centers, educational centers, food and allied, and health-care centers were taken into consideration. From each of the sectors, 10% of the sampled respondents were selected for interview. As the main objective of the study was to explore the mental well-being of migrants, the survey focused on questioning only migrant workers. For interview, only the adults (age 18 years or above) were consulted. The interview was based on questionnaires which lasted 25–45 min. In total, 1230 people were interviewed after getting their verbal consent.
Statistical techniques
Both descriptive and analytical techniques were applied for the analysis of data. Descriptive analysis showing the frequencies of selected variables is presented in the first instance. To investigate the influence of socioeconomic and housing-related variables on the mental well-being (with WHO5 cutoff point 13 or below) of the respondents, unadjusted odds ratio (OR) with 95% confidence interval was calculated. Unstandardized maximum likelihood coefficients and their significance levels after adjusting for different socioeconomic and demographic variables were calculated. When adjusting for different combinations of risk factors, the analysis was performed in five steps. Model 1 tests the relationship between years of immigration with mental well-being. Models 2 and 3 sequentially add age and income level to determine if the effects of years of immigration on mental well-being remain after their inclusion in the analyses. In model 4, the direct effect of housing conditions on mental well-being was estimated. In model 5, the effects of accessibility to amenities and facilities on mental well-being, and finally the effect of social life, were tested. Each variable was tested separately as a potential moderator using SPSS 16.0 (Chicago).
RESULTS
The household response rate was 90.8% comprising 1230 heads of the households. Characteristics of the study sample are shown in Table 1. The prevalence of poor mental well-being was higher to a statistically significant extent among single/widow/divorced/separated (OR = 0.76, P < 0.01), unskilled (OR = 2.26, P < 0.01), unemployed (OR = 2.16, P < 0.01), daily wager (OR = 2.57, P < 0.01), and illiterate (OR = 2.55, P < 0.01). Poor mental health was significantly higher among respondents those belong to low-income group (OR = 3.5 P < 0.01) and residing in the study area with <10 year (OR = 3.2, P < 0.01). Advancing age has also shown its negative impact on respondents’ mental well-being; age groups 58+ were more likely to experience poor mental health (OR = 1.89, P < 0.001), than the other age group. Statistically significant association with mental well-being was also found with household level risk factors, namely, poor housing condition (OR = 1.07, P < 0.001), lacking educational facilities (OR = 0.90, P < 0.01), and medical facilities (OR = 0.90, P < 0.01). A statistically significant association was found between lacking social support (OR = 1.24, P < 0.01), feeling insecure (OR = 1.44, P < 0.001), adjustment problem (OR = 0.74, P < 0.05), and respondents’ poor mental health.
Table 1.
Socioeconomic and demographic characteristics and its association with mental well-being of the study sample
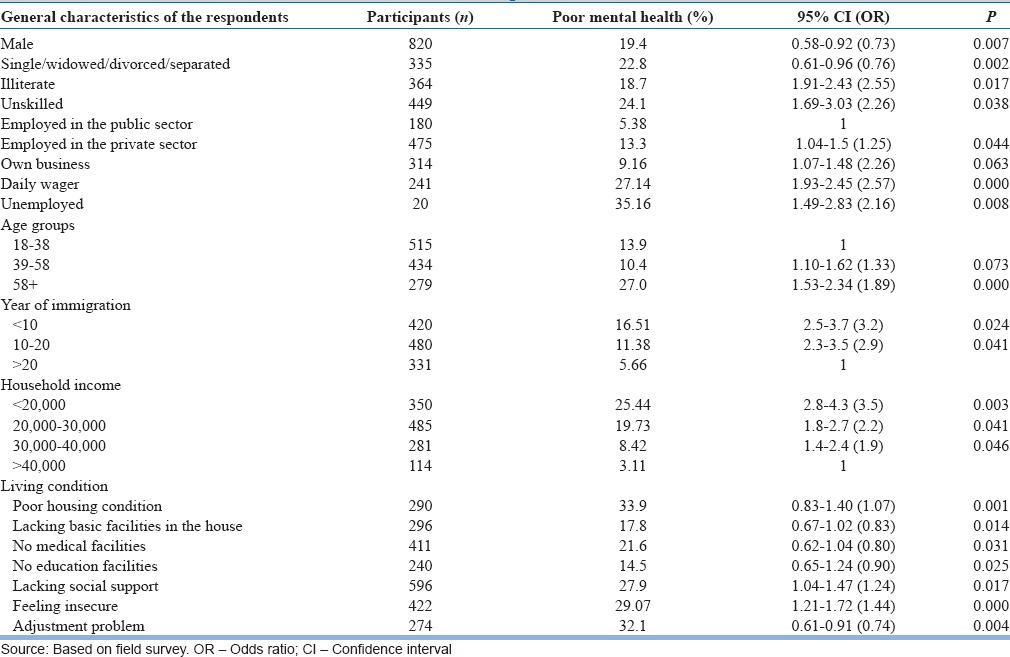
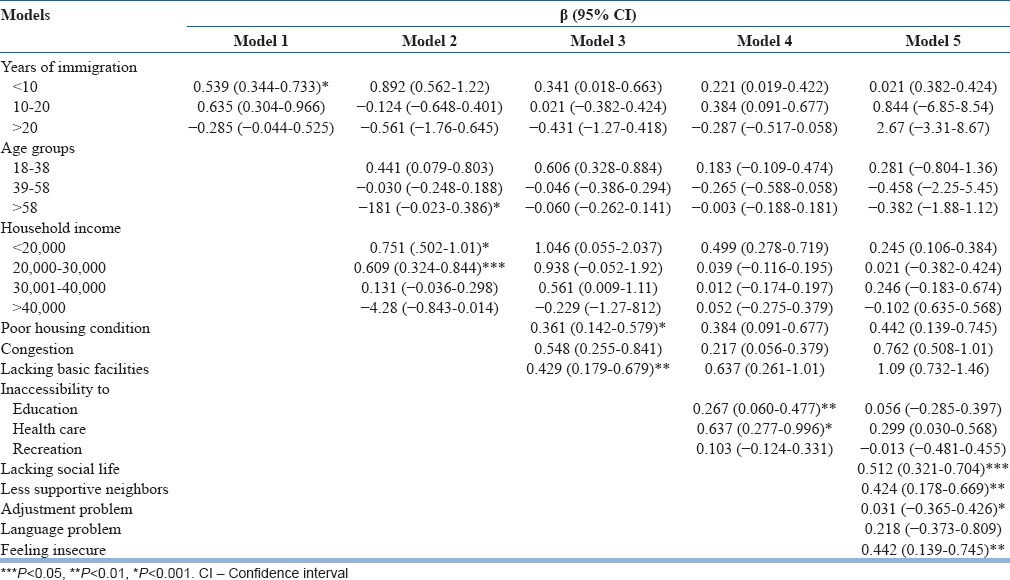
Table 2 shows the mental health status of the migrants when adjusting for various combinations of risk factors. Model 1 shows the impact of years of immigration on mental well-being when adjusting only for gender and age. Immigrants who have been living there for the past 15 years or more had a great prevalence of better mental well-being than who arrived recently (P = 0.01). When adjusting for education level and household income (model 2), the year of immigration moderated the relationship with poor mental well-being up to the level of statistical significance. A recent arrival in the city accompanied by low levels of education and income was associated with low level of mental well-being. Poor housing conditions (model 3) were more predictive of poor mental well-being among less educated and low-income group than the fortunate section of the society. In this model, the direct effect of housing statistically significantly related to poor mental well-being, but the association was weaker in better income group. Respondents who had inaccessibility to basic amenities and facilities were more likely to report poor mental health compared to those who had better accessibility but again to a lesser extent (model 4) when adjusting other socioeconomic confounders. Finally, the effect of social life on mental well-being (model 5) was tested. The highest rating of social support was associated with lower chances of poor mental well-being. No longer were education and income found significant predictor of mental health, after including variable of social life. Year of immigration remains a significant moderator of the relationship between social life and mental well-being.
Table 2.
Linear regression coefficient (β, 95% confidence interval) for mental well-being by contextual measure of socioeconomic and demographic factors
DISCUSSION
The present study sheds new light on the pathways linking significant relationship between the migratory status and psychological well-being of urban population. The study identified many afflictions that impacted on mental health. Uneducated or less educated and unemployed or underemployed urban migrants were facing hardships in acquiring basic necessities for survival, for instance, inaccessibility to health care, educational facilities, piped water connection, overcrowding, poor housing condition, ambient environmental pollution, and the burden of paying for house rent, electricity, water, and waste collection. Therefore, they were at much greater risk to experience poor mental health. On the contrary, educated households had better employment opportunities and feel better adjusted than others. They also had stronger aspirations to integrate into the host society. A similar association was also found in other studies conducted elsewhere.[13,14,15,16,17] Apart from the individual level factors, the process of urbanization, especially in developing countries, often occurs independently of a surge in industrialization, and thus is not associated with improved economic circumstances, often leads to poor socioeconomic conditions that leave people more vulnerable to poor mental health.[18,19]
At household level, the study demonstrates that the association became comparatively more significant after considering the individuals’ house condition, including enough space for each person, separate kitchen, proper lavatory system, open space, and proper ventilation. In Indian society, the house is considered as the most essential physical capital and perceived as a symbol of well-being; better the housing condition, the higher the social status. It is not a surprise that those having such facility feel better adjusted. The result of this study is in conformity with other studies which found a significant association between socioeconomic status and mental well-being.[20,21,22]
Exposure to different social environment, especially adjustment to the modern value-based urban society, and lacking social support in the host society were significant predictors of adverse mental well-being of the immigrants. In most of the cases, the migrants do not feel very welcome by the host society and perceived cultural differences such as language, traditions, food habit, and a way of life as the main reason hindering the development of social networks outside their own community. As a result, they feel insecure in the host society, tried to live in the clusters of their own community, preserved their regional identity, and continued to share the same traditions, norms, and culture, impending integration into the host society. To some extent, male migrants were observed to have wider networks compared to female. However, all of them attributed their perceived lack of integration to the attitudes of the host society and considered broader and stronger social networks as an important psychological support.[23,24,25,26,27,28]
The findings of this paper lend support to the hypothesis that the economic and sociocultural changes experienced by migrants are a potential risk factor for poor mental health. The process of urbanization has been recognized significant in the onset of poor mental health in the present study area. There are three different pathways, which could provide the explanation for these phenomena. First, changes in the economic system with high levels of unemployment and financial insecurity resulting in difficulties in maintaining reasonable quality of life. Second, the social and cultural change involving transformation from community life to one of individualistic societies lacking social support and negative response to migrants from the host community. Finally, city life itself and its built environment produce stress that impacts on mental health directly or indirectly and both ways. The adjustment process of migrants in a host society may be considered as a complex phenomenon which needs time and goes through various stages of development. There are numerous factors and elements that interact together to shape and act as facilitators or barriers to the adjustment process in different ways.
It is now well understood that unprecedented urbanization in the developing world is associated with poor social conditions and consequent high level of stress. However, there remains a gap in the literature regarding specific stressors associated with urbanization and its impact on mental health. This paper can be considered a contribution toward understanding the complexity of the mental health impact of urbanization (i.e., fuelled by rural to urban migration) in India in general and of developing world in particular. Our findings could be considered pioneering as it emphasizes understanding the context in which mental health problems occur and identified that in urban centers, the risk for poor mental health is structured by economic and social institutions. The study reiterates the importance of contextual factors on individual and societal level and suggests more in-depth focus on specific areas of environmental stressor to understand the mechanisms involved in the development of mental ill-health. In addition, a longitudinal study needs to be conducted to parse out the influences of socioeconomic institutions on the mental health of migrants and to determine the causal effects of specific stressors.
The main weakness of the study is the cross-sectional design, which makes it impossible to claims of causality. The present work could have been biased by the fact that we had to rely on a self-reported mental health status of the sampled respondents. Factors related to behavior and health history of the family were not directly taken into consideration that might be mediated the association between migratory status and the mental health.
CONCLUSION
The present study concludes that the unprecedented urbanization mainly caused by rural to urban migration is associated with poor mental health in the general population. Those who are involved in both treatment and prevention of disease, it is of great importance to consider this possible pathway in designing the treatment facilities and in planning the distribution of health-care facilities. The study could be utilized for integrated rural-urban planning by focusing on regional, subregion, and local economic and social characteristics to reduce the level of migration. At the local level, it may be used exclusively to identify the best possible locations for better distribution of basic facilities and promoting community activities to make the migrants feel at home.
Financial support and sponsorship
University Grants Commission.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.United Nations. World Urbanization Prospects: The 2003 Revision. United Nations. 2004. [Last accessed on 2013 Jan 13]. Available from: http://www.un.org/esa/population/publications/wup2003/2003Highlights.pdf .
- 2.Murray CJ, Lopez A. The Global Burden of Disease. Boston: Harvard School of Public Health; 1996. [Google Scholar]
- 3.WHO. The World Health Report 2002. Geneva: WHO; 2002a. [Google Scholar]
- 4.Harpham T. Urbanization and mental health in developing countries: A research role for social scientists, public health professionals and social psychiatrists. Soc Sci Med. 1994;39:233–45. doi: 10.1016/0277-9536(94)90332-8. [DOI] [PubMed] [Google Scholar]
- 5.Ludermir AB, Harpham T. Urbanization and mental health in Brazil: Social and economic dimensions. Health Place. 1998;4:223–32. doi: 10.1016/s1353-8292(98)00017-3. [DOI] [PubMed] [Google Scholar]
- 6.Harpham T, Molyneux C. Urban health in developing countries: A review. Progress in Development Studies. 2001;1:113–37. [Google Scholar]
- 7.Math SB, Srinivasaraju R. Indian psychiatric epidemiological studies: Learning from the past. Indian J Psychiatry. 2010;52(Suppl 1):S95–103. doi: 10.4103/0019-5545.69220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reddy MV, Chandrashekar CR. Prevalence of mental and behavioral disorders in India: A meta-analysis. Indian J Psychiatry. 1998;40:149–57. [PMC free article] [PubMed] [Google Scholar]
- 9.Ganguli HC. Epidemiological findings on prevalence of mental disorders in India. Indian J Psychiatry. 2000;42:14–20. [PMC free article] [PubMed] [Google Scholar]
- 10.Bech P. Measuring the dimensions of psychological general well-being by the WHO-5. Qual Life Newsl. 2004;32:15–6. [Google Scholar]
- 11.Henkel V, Mergl R, Kohnen R, Maier W, Möller HJ, Hegerl U. Identifying depression in primary care: A comparison of different methods in a prospective cohort study. BMJ. 2003;326:200–1. doi: 10.1136/bmj.326.7382.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Löwe B, Spitzer RL, Gräfe K, Kroenke K, Quenter A, Zipfel S, et al. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. J Affect Disord. 2004;78:131–40. doi: 10.1016/s0165-0327(02)00237-9. [DOI] [PubMed] [Google Scholar]
- 13.Bahar E, Henderson AS, Mackinnon AJ. An epidemiological study of mental health and socioeconomic conditions in Sumatera, Indonesia. Acta Psychiatr Scand. 1992;85:257–63. doi: 10.1111/j.1600-0447.1992.tb01466.x. [DOI] [PubMed] [Google Scholar]
- 14.Desjarlais R, Eisenberg L, Good B, Kleinman A. World Mental Health: Problems and Priorities in Low Income Countries. New York: Oxford University Press; 1995. [Google Scholar]
- 15.Patel V, Araya R, de Lima M, Ludermir A, Todd C. Women, poverty and common mental disorders in four restructuring societies. Soc Sci Med. 1999;49:1461–71. doi: 10.1016/s0277-9536(99)00208-7. [DOI] [PubMed] [Google Scholar]
- 16.Patel V, Abas M, Broadhead J, Todd C, Reeler A. Depression in developing countries: Lessons from Zimbabwe. BMJ. 2001;322:482–4. doi: 10.1136/bmj.322.7284.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health Organ. 2003;81:609–15. [PMC free article] [PubMed] [Google Scholar]
- 18.Mumford DB, Minhas FA, Akhtar I, Akhter S, Mubbashar MH. Stress and psychiatric disorder in urban Rawalpindi. Community survey. Br J Psychiatry. 2000;177:557–62. doi: 10.1192/bjp.177.6.557. [DOI] [PubMed] [Google Scholar]
- 19.Parkar SR, Fernandes J, Weiss MG. Contextualizing mental health: Gendered experiences in a Mumbai slum. Anthropol Med. 2003;10:291–308. doi: 10.1080/1364847032000133825. [DOI] [PubMed] [Google Scholar]
- 20.Fiscella K, Franks P. Individual income, income inequality, health, and mortality: What are the relationships? Health Serv Res. 2000;35(1 Pt 2):307–18. [PMC free article] [PubMed] [Google Scholar]
- 21.Kahn RS, Wise PH, Kennedy BP, Kawachi I. State income inequality, household income, and maternal mental and physical health: Cross sectional national survey. BMJ. 2000;321:1311–5. doi: 10.1136/bmj.321.7272.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weich S, Lewis G, Jenkins SP. Income inequality and the prevalence of common mental disorders in Britain. Br J Psychiatry. 2001;178:222–7. doi: 10.1192/bjp.178.3.222. [DOI] [PubMed] [Google Scholar]
- 23.Farooq M, Ahmad M, Cheema MA. Elderly migrants adjustment problems in the urban areas. J Agric Soc Sci. 2005;3:283–4. [Google Scholar]
- 24.Cohen S. Psychosocial models of the role of social support in the etiology of physical disease. In: Salovey P, Rothman AJ, editors. Social Psychology of Health. New York: Psychology Press; 2003. pp. 227–44. [DOI] [PubMed] [Google Scholar]
- 25.Uchino BN. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29:377–87. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 26.Hogan BE, Linden W, Najarian B. Social support interventions: Do they work? Clin Psychol Rev. 2002;22:383–442. doi: 10.1016/s0272-7358(01)00102-7. [DOI] [PubMed] [Google Scholar]
- 27.House JS, Landis KR, Umberson D. Social relationships and health. In: Salovey P, Rothman AJ, editors. Social Psychology of Health. New York: Psychology Press; 2003. pp. 218–26. [Google Scholar]
- 28.Seeman T. How do others get under our skin?: Social relationships and health. In: Ryff CD, Singer BH, editors. Emotion, Social Relationships, and Health. New York: Oxford University Press; 2001. pp. 189–210. [Google Scholar]


