Abstract
Forearm
Purpose fractures are one of the most commonly sustained injuries in children and are often treated non-operatively. The purpose of this study was to estimate the rate of inpatient surgical treatment of paediatric forearm fractures over time using a large, publicly available, national database.
Methods
The Healthcare Cost and Utilization Project (HCUP) Kids’ Inpatient Database (KID) was evaluated between 2000 and 2012. Forearm fractures and surgeries were identified using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9 CM) diagnosis and procedure codes. Univariable and multivariable logistic regression were used to determine variables associated with greater proportion of surgical treatment. All statistical analyses were performed using SAS statistical software v.9.4 (SAS Institute Inc., Cary, NC, USA). Statistical significance was set at p < 0.05.
Results
The database identified 30 936 forearm fracture admissions. Overall, 19 837 of these patients were treated surgically (64.12%). The percentage of patients treated with surgery increased from 59.3% in 2000 to 70.0% in 2012 (p < 0.001). Multivariable regression analysis found increased age (p < 0.001), more recent year (p < 0.001), male gender (p = 0.003) and admission to a children’s hospital (p < 0.001) were associated with an increased proportion of patients receiving surgical treatment. Medicaid payer status was associated with a lower proportion of surgical treatment (p < 0.001).
Conclusions
The rate of operative treatment for paediatric forearm fractures admitted to the hospital increased over time. Increased surgical rates were associated with older age, male gender, treatment at a children’s hospital and non-Medicaid insurance status.
Keywords: trauma, upper extremity, fixation, children
Introduction
Forearm fractures are one of the most common injuries in the paediatric population, estimated to occur at a rate of approximately 560 per 100 000 in the 5 to 14 years age group.1 Historically, a majority these injuries have been managed non-operatively due to the high remodelling potential in paediatric patients. This is in contrast to adult patients in whom these injuries are typically considered ‘fractures of necessity’ with regards to the need for operative intervention.
Recent literature has highlighted the increased rate of operative treatment for certain paediatric fractures.2,3 Paediatric forearm fractures, in particular, have seen an increased rate of surgical treatment despite the lack of comparative studies showing a clear benefit over non-operative treatment.4,5 In this study, we used The Healthcare Cost and Utilization Project (HCUP) Kids’ Inpatient Database (KID)6 to examine national trends in paediatric forearm fracture management in the United States. We hypothesised that there would be an increasing rate of surgical intervention in more recent years and that the rates of surgical intervention would increase with patient age and other demographic factors.
Patients and methods
Data collection
We used the HCUP-KID6 to examine trends in forearm fracture management in the United States between 2000 and 2012. The HCUP-KID is the largest publicly available all-payer paediatric inpatient database that is compiled based on two to three million hospital stays.6 The database is a result of the data collected in the 46 states that have partnered with the Agency for Healthcare Research and Quality and maintain state-wide data collection efforts. The database is a sample of all discharges of all hospitals in participating states. The large sample size generates data that is generalisable to the national inpatient paediatric population.
Paediatric forearm (radius and ulna shaft) fractures were identified using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9 CM) diagnosis codes. ICD-9 CM procedure codes were used to identify patients who received surgical treatment for the years between 2000 and 2012 (Table 1). Open fracture diagnosis codes and distal or proximal radius/ulna fractures were excluded. Demographic data collected included gender, age (stratified age from 0 to 4, 5 to 9, 10 to 14, 15 to 20 years) and insurance status (Medicaid, private, self-pay, other). Hospital-related data collected included hospital type (children’s or general hospital) and region (Northeast, Midwest, South, West).
Table 1.
ICD-9 diagnosis and procedure codes queried.
| ICD-9 Diagnosis Codes | Description | |
|---|---|---|
| 81320 | FX SHAFT FOREARM NOS-CLOSED | |
| 81321 | FX RADIUS SHAFT-CLOSED | |
| 81322 | FX ULNA SHAFT-CLOSED | |
| 81323 | FX SHAF RAD W ULNA-CLOSED | |
| 81380 | FX FOREARM NOS-CLOSED | |
| 81383 | FX RADIUS W ULNA NOS-CLOSED |
| ICD-9 Procedure Codes | Description | |
|---|---|---|
| 75.83 | INTERNAL FIXATION OF BONE WITHOUT FRACTURE REDUCTION, RADIUS AND ULNA | Surgery group |
| 79.12 | CLOSED REDUCTION OF FRACTURE WITH INTERNAL FIXATION, RADIUS AND ULNA | |
| 79.32 | OPEN REDUCTION OF FRACTURE WITH INTERNAL FIXATION, RADIUS AND ULNA | |
| 79.22 | OPEN REDUCTION OF FRACTURE WITHOUT INTERNAL FIXATION, RADIUS AND ULNA | |
| 79.02 | CLOSED REDUCTION OF FRACTURE WITHOUT INTERNAL FIXATION, RADIUS AND ULNA | No Surgery group |
Statistical Analysis
Univariable and multivariable logistic regression was used to determine variables associated with greater proportion of surgical treatment. All statistical analyses were performed using SAS statistical software v.9.4 (SAS Institute, Inc. Cary, NC, USA). Statistical significance was set at p < 0.05.
Results
Table 2 represents the demographic characteristics of patients who were diagnosed with closed diaphyseal forearm fractures. Table 3 represents the demographic characteristics of patients who were identified as having undergone surgical intervention. A total of 30 936 forearm fracture admissions were identified (Table 2) and 19 837 of these patients were treated surgically (64.12%; Table 3). The proportion of patients treated with surgery increased from 59.3% in 2000 to 70.0% in 2012 (p < 0.001) (Fig. 1; Table 4). Increasing rates of surgery were associated with increasing age, with the lowest rate of surgery occurring in those aged 0 to 4 years old (15.4%) and the highest rate in the 15 to 20 years age group (79.2%) (Table 4). Univariable analysis showed that patients admitted to a non-children’s hospital underwent surgery 64.3% of the time compared with 62.7% of those admitted to a children’s hospital. However, after multivariable analysis, we found that patients who were admitted to a children’s hospital were more likely to undergo surgery compared with those admitted to a non-children’s hospital (p < 0.001). Patients in more recent years were more likely to undergo surgical intervention as well, with the highest rate of surgery occurring in 2012 (70.0%). There were also regional differences in rates of surgery. Patients in the West were more likely to undergo surgery (67.8%) compared with the Northeast (59.9%) (p < 0.001).
Table 2.
Demographics of all paediatric forearm fractures, 2000 to 2012.
| 95% CI | 95% CI | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Value | Estimated number of patients | Standard error | Lower | Upper | Patients (%) | Standard error (%) | Lower (%) | Upper (%) |
| Gender | Male | 21 968 | 477 | 21 032 | 22 903 | 71.01 | 0.39 | 70.25 | 71.77 |
| Female | 8968 | 237 | 8503 | 9434 | 28.99 | 0.39 | 28.23 | 29.75 | |
| Age (yrs) | 0-4 | 2247 | 89 | 2072 | 2422 | 7.26 | 0.23 | 6.82 | 7.71 |
| 5-9 | 6557 | 200 | 6165 | 6950 | 21.20 | 0.41 | 20.40 | 21.99 | |
| 10-14 | 10 262 | 262 | 9748 | 10 775 | 33.17 | 0.45 | 32.30 | 34.04 | |
| 15-20 | 11 870 | 311 | 11 260 | 12 479 | 38.37 | 0.67 | 37.05 | 39.68 | |
| Hospital type | Children’s hospital | 3718 | 354 | 3024 | 4412 | 12.02 | 1.03 | 10.00 | 14.04 |
| General hospital | 27 217 | 566 | 26 108 | 28 327 | 87.98 | 1.03 | 85.96 | 90.00 | |
| Insurance status | Medicaid | 7549 | 235 | 7088 | 8010 | 24.40 | 0.52 | 23.38 | 25.43 |
| Private/Self-pay/other | 23 387 | 522 | 22 364 | 24 409 | 75.60 | 0.52 | 74.57 | 76.62 | |
| Year | 2000 | 7491 | 308 | 6888 | 8094 | 24.21 | 0.74 | 22.77 | 25.66 |
| 2003 | 6739 | 229 | 6290 | 7187 | 21.78 | 0.59 | 20.63 | 22.94 | |
| 2006 | 6365 | 233 | 5908 | 6821 | 20.57 | 0.55 | 19.50 | 21.65 | |
| 2009 | 5278 | 206 | 4875 | 5682 | 17.06 | 0.51 | 16.06 | 18.06 | |
| 2012 | 5063 | 196 | 4678 | 5448 | 16.37 | 0.69 | 15.01 | 17.72 | |
| Hospital region | Northeast | 5596 | 291 | 5026 | 6167 | 18.09 | 0.87 | 16.38 | 19.80 |
| Midwest | 6356 | 322 | 5725 | 6987 | 20.55 | 0.96 | 18.67 | 22.42 | |
| South | 11 561 | 436 | 10 706 | 12 416 | 37.37 | 1.15 | 35.11 | 39.63 | |
| West | 7423 | 379 | 6680 | 8165 | 23.99 | 1.08 | 21.88 | 26.11 | |
| Total | 30 936 | 667 | 29 628 | 32 244 | 71.01 | 0.39 | 70.25 | 71.77 | |
Table 3.
Demographics of surgically treated paediatric forearm fractures, 2000 to 2012.
| 95% CI | 95% CIC | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Value | Treated surgically (n) | Standard error | Lower | Upper | Patients (%) | Standard error (%) | Lower (%) | Upper (%) |
| Gender | Male | 14 580 | 335 | 13 923 | 15 237 | 73.5 | 0.46 | 72.60 | 74.40 |
| Female | 5258 | 160 | 4945 | 5570 | 26.5 | 0.46 | 25.60 | 27.40 | |
| Age (yrs) | 0-4 | 346 | 30 | 287.92 | 404.59 | 1.8 | 0.14 | 1.48 | 2.02 |
| 5-9 | 2862 | 121 | 2624 | 3100 | 14.4 | 0.44 | 13.56 | 15.29 | |
| 10-14 | 7223 | 202 | 6827 | 7620 | 36.4 | 0.55 | 35.34 | 37.48 | |
| 15-20 | 9405 | 238 | 8939 | 9871 | 47.4 | 0.78 | 45.89 | 48.94 | |
| Hospital type | Children’s hospital | 2330 | 253 | 1834 | 2825 | 11.7 | 1.15 | 9.50 | 13.99 |
| General hospital | 17 508 | 377 | 16 768 | 18 247 | 88.3 | 1.15 | 86.01 | 90.51 | |
| Insurance status | Medicaid | 4182 | 152 | 3884 | 4480 | 21.1 | 0.57 | 19.97 | 22.20 |
| Private/Self-pay/other | 15 655 | 369 | 14 931 | 16 379 | 78.9 | 0.57 | 77.80 | 80.03 | |
| Year | 2000 | 4440 | 203 | 4042 | 4839 | 22.4 | 0.78 | 20.86 | 23.91 |
| 2003 | 4188 | 160 | 3875 | 4502 | 21.1 | 0.66 | 19.82 | 22.41 | |
| 2006 | 4142 | 161 | 3827 | 4458 | 20.9 | 0.59 | 19.72 | 22.04 | |
| 2009 | 3524 | 144 | 3241 | 3808 | 17.8 | 0.56 | 16.67 | 18.86 | |
| 2012 | 3542 | 141 | 3266 | 3818 | 17.9 | 0.77 | 16.36 | 19.36 | |
| Hospital region | Northeast | 3351 | 202 | 2956 | 3746 | 16.9 | 0.94 | 15.06 | 18.73 |
| Midwest | 4024 | 203 | 3627 | 4421 | 20.3 | 0.95 | 18.42 | 22.14 | |
| South | 7427 | 290 | 6858 | 7995 | 37.4 | 1.20 | 35.08 | 39.79 | |
| West | 5036 | 265 | 4515 | 5556 | 25.4 | 1.16 | 23.11 | 27.66 | |
| Total | 19 837 | 454 | 18 947 | 20 727 | 35.9 | 0.50 | 63.14 | 65.11 | |
Fig. 1.
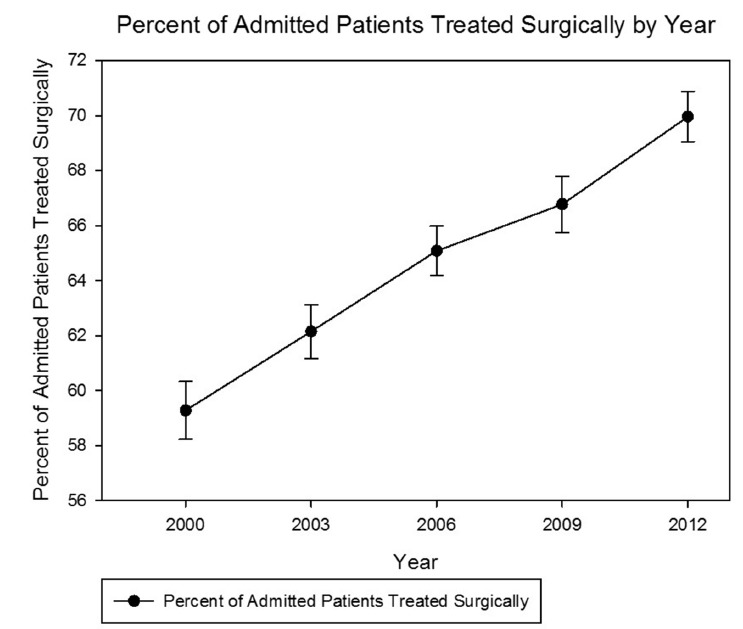
Percent of admitted patients treated surgically by year.
Table 4.
Subgroup analysis of admitted patients treated surgically.
| Variable | Value | Treated surgically (%) | Standard error | Lower | Upper | p value* |
|---|---|---|---|---|---|---|
| Gender | Male | 66.4 | 0.53 | 65.32 | 67.41 | 0.0036 |
| Female | 58.6 | 0.81 | 57.03 | 60.22 | ||
| Age (yrs) | 0-4 | 15.4 | 1.15 | 13.15 | 17.67 | < 0.0001 |
| 5-9 | 43.6 | 1.06 | 41.58 | 45.72 | ||
| 10-14 | 70.4 | 0.73 | 68.95 | 71.83 | ||
| 15-20 | 79.2 | 0.57 | 78.12 | 80.36 | ||
| Hospital type | Children’s hospital | 62.7 | 2.02 | 58.70 | 66.60 | < 0.0001† |
| General hospital | 64.3 | 0.50 | 63.34 | 65.31 | ||
| Insurance status | Medicaid | 55.4 | 0.91 | 53.62 | 57.18 | < 0.0001 |
| Private/Self-pay/other | 66.9 | 0.53 | 65.90 | 67.98 | ||
| Year | 2000 | 59.3 | 1.05 | 57.22 | 61.34 | < 0.0001 |
| 2003 | 62.2 | 0.98 | 60.22 | 64.08 | ||
| 2006 | 65.1 | 0.89 | 63.33 | 66.83 | ||
| 2009 | 66.8 | 1.02 | 64.77 | 68.77 | ||
| 2012 | 70.0 | 0.92 | 68.16 | 71.75 | ||
| Hospital region | Northeast | 59.9 | 1.31 | 57.32 | 62.44 | < 0.0001 |
| Midwest | 63.3 | 1.22 | 60.92 | 65.69 | ||
| South | 64.2 | 0.77 | 62.72 | 65.76 | ||
| West | 67.8 | 0.93 | 66.03 | 69.66 | ||
| Total | 64.1 | 0.50 | 63.14 | 65.11 |
multivariable logistic regression
after adjustment, children’s hospitals associated with higher rate of surgical treatment
Of patients who underwent surgery, 73.5% were male (Table 3). Additionally, 83.8% of patients were aged between 10 and 20 years. The majority of the surgeries occurred at a non-children’s hospital (88.3%). The majority of patients (78.9%) had non-Medicaid insurance (p < 0.001). Lastly, from a volume perspective, 37.4% of all surgeries occurred in the South, even though surgeries occurred at the highest rate in the West.
After adjusting for potential confounders (age, gender, year of admission, insurance payer, hospital type, geographic region), multivariable logistic regression analysis revealed that increased age (p < 0.001) (Fig. 2), male gender (p = 0.003), more recent year (p < 0.001) and admission to a children’s hospital (p < 0.001) were independently associated with an increased proportion of patients receiving surgical treatment. Medicaid payer status was associated with a lower proportion of surgical treatment (p < 0.001) and there was significant variability in surgical treatment between geographic regions (p < 0.0001).
Fig. 2.
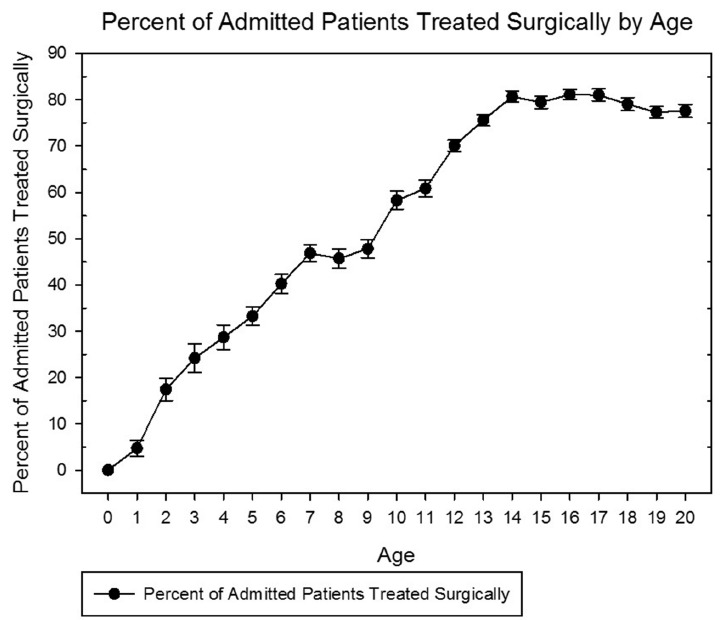
Percent of admitted patients treated surgically by age.
Discussion
This study revealed an increasing trend towards operative management of paediatric forearm fractures in patients who were admitted to the hospital. Increasing age, male gender, more recent year, admission to a children’s hospital and non-Medicaid insurance status were statistically significant factors in predicting operative intervention. We also found geographic variation in the rate of operative intervention for these injuries. Historically, closed paediatric forearm fractures have been treated non-operatively due to the high remodelling potential in paediatric patients. Tarmuzi et al reported on the successful closed management of 48 patients aged 4 to 12 years, with an 86% rate of excellent functional outcome.7 In this study, all fractures went on to union and 51.7% of radius and 73.9% of ulna fractures went on to perfect reduction (angulation less than 5°) in the anteroposterior plane by final follow-up. Perfect reduction was accomplished less often in the lateral plane (14.6% of radius and 54.3% of ulna fractures) with little effect on functional outcome.7 Zionts et al performed a prospective study of older paediatric patients with a mean age of 13.3 years (8 to 15) and observed outcomes of non-operative management after closed reduction.8 All 25 patients had full range of motion of their wrist and elbow with an average loss of 4° of forearm pronation and 6.8° of supination.8 Carey et al examined age differences among patients managed with closed reduction.9 The authors found that patients aged < 10 years with < 30° angulation at the time of reduction could expect minimal angulation and full range of motion at healing. In contrast, patients aged 11 to 15 years were expected to have residual angulation with 60% of patients experiencing residual loss of up to 30° of forearm rotation, albeit with no functional loss.9 Kay et al reported significantly worse outcomes in patients aged > 10 years treated with closed reduction only. In this study, all patients aged < 10 years had excellent results via non-operative management while nine of 14 patients aged between 10 and 16 years failed closed management, leading the authors to state that the success of closed management was over estimated in older patients.10 Even following successful non-operative management, re-fracture has been reported to occur at a rate of 4% to 8%.11 Our study supports the findings that operative treatment is used more frequently in older patients. In our sample, the majority of patients were managed non-operatively until the age of ten years, at which point surgery seemed to be the treatment of choice in greater than 50% of patients.
In addition to increased age, more recent year was associated with increased rates of surgical treatment. Other authors have reported an increase in childhood upper extremity fractures in recent years among developed nations, which may partly account for increasing rates of surgical treatment.12-15 Perhaps the trend towards increasing operative treatment for these injuries in developed nations like the United States is also related to recent advances in techniques and technology used to treat paediatric forearm fractures. There are several fixation methods available for the treatment of forearm fractures in skeletally immature patients. Compression plating, intramedullary nailing (IMN) with titanium elastic nails (TENS) or Kirchner wires (k-wires), and combined fixation methods with nailing and plating are all options, with intramedullary nailing being the most common technique.16 Flynn et al reviewed 149 operatively managed paediatric both bone forearm fractures over an 11-year period and found that 69.1% were managed with IMN compared with 29.5% with plating. The average age of patients treated surgically was 11.2 years and the study found a sevenfold increase in the rate of fixation over the course of the study,17 a trend similar to our findings. Other studies have also found a trend towards operative treatment for paediatric forearm fractures. Sinikumpu et al examined their experience at a children’s hospital that serves as a regional referral centre in Finland.12 The authors examined all paediatric forearm fractures that were evaluated at the hospital between 1997 and 2009 and found that the incidence of paediatric forearm fractures was increasing in general. Additionally, the rate of IMN for these injuries significantly increased during the study period. In another Finnish study, Helenius et al examined the rate of operative treatment of fractures in children.4 Between 1997 and 2006, the authors found a 28% overall increase in upper extremity fracture surgery. When examining forearm fractures specifically, the authors found a 62% increase in primary operative treatment.4
The reasons for the apparent increase in operative treatment for paediatric forearm fractures are unclear since there is limited comparative literature definitively showing the benefits of surgical over non-surgical treatment. Eismann et al reviewed the abstracts of research presented at the national meetings of the American Academy of Orthopaedic Surgeons (AAOS) and Pediatric Orthopaedic Society of North America (POSNA) between 1993 and 2012.5 The authors found that, overall, only 26% of studies examining the treatment of paediatric upper extremity fractures recommended operative treatment. Non-operative treatment was recommended in 47% of the sampled studies and a neutral recommendation was made in 27%. The lack of comparative effectiveness literature for the treatment of paediatric and adolescent forearm fractures likely contributes to the regional variation observed in this study, which is consistent with other authors’ findings among adult fracture patients.18-21 This lack of data is important because despite the potential for a more anatomic reduction, operative intervention for paediatric forearm fractures is not benign and can result in both minor and major complications. A study of 103 patients undergoing surgery via IMN reported a 14.6% complication rate including compartment syndrome, delayed union and poor functional outcome.16 Kang et al reported on 11 complications in a series of 90 patients treated with IMN. Reported complications included wound problems (7), superficial radial nerve palsy (2), malunion (1) and compartment syndrome (1).22
After multivariable logistic regression analysis, we found that patients with forearm fractures treated at children’s hospitals were more likely to undergo surgical treatment. While a lower overall percentage of patients at children’s hospitals were treated surgically (62.7%) compared with general hospitals (64.3%) (Table 3), after adjusting for patient demographics such as age, children’s hospitals were actually independently associated with an increased rate of surgical treatment (p < 0.0001). This finding may be explained by the younger mean age of patients (i.e. those who are less likely to undergo surgical treatment) seen at children’s hospitals. This increased rate of surgical treatment at children’s hospitals may be due to several factors, including whether a paediatric or non-paediatric orthopaedic surgeon treated the patient, the availability of paediatric specific implants, fracture complexity or the availability of paediatric specific ancillary services (i.e. paediatric nursing or anaesthesia). Fabricant et al also used the HCUP-KID to examine paediatric medial epicondyle fractures.23 The authors found that between 1997 and 2009, the proportion of hospital discharges from children’s hospitals increased for the treatment of medial epicondyle fractures compared with general hospitals. The authors postulated that their findings may indicate a move towards subspecialisation in the treatment for paediatric fractures.
Finally, our data show that patients with non-Medicaid insurance were more likely to receive operative treatment compared to those who were insured by Medicaid. Other studies have found disparities in treatment and rate of complications associated with patients who have government-subsidised insurance. Dy et al examined revisit rates to the emergency department over a two-year period and found that non-White patients and patients with government-funded insurance were significantly more likely to return to the emergency department following closed reduction of paediatric fractures.24 Sabharwal et al examined paediatric patients who had presented to a tertiary care hospital for an orthopaedic complaint after having already visited another emergency department for the same complaint.25 A total of 94% of patients presented with a closed fracture and the authors found that 52% of children with private insurance received orthopaedic care within 24 hours compared with only 22% with government-subsidised health insurance.25 Skaggs et al examined access to orthopaedic care and its correlation with insurance status.26 Of the 230 paediatric orthopaedic surgery offices evaluated, 88 offered limited services to patients with Medicaid and 41 would not see a patient with Medicaid under any circumstance. There was also a correlation between willingness to see patients with Medicaid and the reimbursement rate in the region.26 Our study found increased rates of operative treatment in patients with non-Medicaid insurance. This may reflect differences in reimbursement rates between private and government subsidised insurance, surgeon bias when evaluating the risks of surgical versus non-surgical treatment or other unknown factors. With the data analysed, it is not possible to make absolute conclusions regarding treatment indications because data regarding fracture specific characteristics was not available.
Limitations
There are several limitations to this investigation. First, we must emphasise that the HCUP-KID only accounts for patients who were seen in the emergency department and/or sought hospital admission and is therefore subject to sampling bias. Patients who are admitted may have more severe injuries relative to those presenting directly to physician outpatient offices or treated in an ambulatory setting. This sample therefore, does not necessarily represent the majority of this overall patient population since many of these injuries can be treated in an outpatient setting. Further study is needed to examine whether our findings represent a true increased incidence in the surgical treatment of paediatric forearm fractures among the at-risk population as a whole.
Like any large nationally representative database, the HCUP-KID is at risk for coding misclassification. We were also unable to extract information on more specific fracture characteristics (displacement, angulation, etc.) or surgical treatment characteristics (plating vs intramedullary fixation, etc.), which limits our ability to fully understand how many of the annually admitted paediatric forearm fractures warranted surgical intervention based on accepted indications. We excluded ICD-9 CM codes that indicated open fractures since open fractures are one of the more widely accepted criteria for surgical treatment.27 We also chose to focus on diaphyseal forearm fractures and excluded distal and proximal radius/ulna fractures because treatment for these injuries is distinct from diaphyseal forearm fractures. This study also does not provide information on follow-up data such as functional outcome, fracture union or surgical complications to indicate the results of management decisions. Finally, our multivariable logistic regression model is limited by the variables recorded and available for analysis. Despite its weaknesses, the HCUP-KID database is widely accepted in the literature in the review of a number of other conditions28-40 and provides useful data when examining trends in paediatric fracture treatment. In conclusion, review of the HCUP-KID database showed that the rate of operative treatment of paediatric forearm fractures captured in this inpatient sample increased over time between 2000 and 2012. Increased surgical rates were associated with older age, male gender, treatment at a children’s hospital and non-Medicaid insurance status. While past literature has also shown increases in the rate of surgical treatment for paediatric forearm fractures, further study is necessary to elucidate whether the current findings reflect a similar trend in fractures treated in an outpatient or ambulatory care setting. If the overall rate of surgical treatment for paediatric forearm fractures is truly increasing, further study is also needed to examine the comparative effectiveness of surgical versus non-surgical treatment for these injuries.
Compliance with Ethical Standards
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical Statement
This article does not contain any studies with human participants or animals performed by any of the authors.
No funding was obtained in support of this work.
References
- 1.Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg [Am] 2001;26-A:908–915. [DOI] [PubMed] [Google Scholar]
- 2.Heyworth BE, Galano GJ, Vitale MA, Vitale MG. Management of closed femoral shaft fractures in children, ages 6 to 10: national practice patterns and emerging trends. J Pediatr Orthop 2004;24:455–459. [PubMed] [Google Scholar]
- 3.Naranje SM, Stewart MG, Kelly DM, et al. Changes in the treatment of pediatric femoral fractures: 15-year trends from United States Kids’ Inpatient Database (KID) 1997 to 2012. J Pediatr Orthop 2016;36:e81–e85 [DOI] [PubMed] [Google Scholar]
- 4.Helenius I, Lamberg TS, Kääriäinen S, Impinen A, Pakarinen MP. Operative treatment of fractures in children is increasing. A population-based study from Finland. J Bone Joint Surg [Am] 2009;91-A:2612–2616. [DOI] [PubMed] [Google Scholar]
- 5.Eismann EA, Little KJ, Kunkel ST, Cornwall R. Clinical research fails to support more aggressive management of pediatric upper extremity fractures. J Bone Joint Surg [Am] 2013;95:1345–1350. [DOI] [PubMed] [Google Scholar]
- 6.No authors listed Healthcare Cost and Utilization Project (HCUP) | Agency for Healthcare Research & Quality. https://www.ahrq.gov/research/data/hcup/index.html (date last accessed 7April2017). [PubMed]
- 7.Tarmuzi NA, Abdullah S, Osman Z, Das S. Paediatric forearm fractures: functional outcome of conservative treatment. Bratisl lekárske List 2009;110: 563–568. [PubMed] [Google Scholar]
- 8.Zionts LE, Zalavras CG, Gerhardt MB. Closed treatment of displaced diaphyseal both-bone forearm fractures in older children and adolescents. J Pediatr Orthop 2005;25:507–512. [DOI] [PubMed] [Google Scholar]
- 9.Carey PJ, Alburger PD, Betz RR, Clancy M, Steel HH. Both-bone forearm fractures in children. Orthopedics 1992;15:1015–1019. [DOI] [PubMed] [Google Scholar]
- 10.Kay S, Smith C, Oppenheim WL. Both-bone midshaft forearm fractures in children. J Pediatr Orthop 1986;6:306–310. [DOI] [PubMed] [Google Scholar]
- 11.Bould M, Bannister GC. Refractures of the radius and ulna in children. Injury 1999;30:583–586. [DOI] [PubMed] [Google Scholar]
- 12.Sinikumpu JJ, Pokka T, Serlo W. The changing pattern of pediatric both-bone forearm shaft fractures among 86,000 children from 1997 to 2009. Eur J Pediatr Surg 2013;23:289–296. [DOI] [PubMed] [Google Scholar]
- 13.Sinikumpu JJ, Lautamo A, Pokka T, Serlo W. The increasing incidence of paediatric diaphyseal both-bone forearm fractures and their internal fixation during the last decade. Injury 2012;43:362–366. [DOI] [PubMed] [Google Scholar]
- 14.Khosla S, Melton LJ III, Dekutoski MB, et al. Incidence of childhood distal forearm fractures over 30 years: a population-based study. JAMA 2003;290:1479–1485. [DOI] [PubMed] [Google Scholar]
- 15.de Putter CE, van Beeck EF, Looman CWN, et al. Trends in wrist fractures in children and adolescents, 1997-2009. J Hand Surg Am 2011;36:1810–1815. e2. [DOI] [PubMed] [Google Scholar]
- 16.Kelly BA, Shore BJ, Bae DS, Hedequist DJ, Glotzbecker MP. Pediatric forearm fractures with in situ intramedullary implants. J Child Orthop 2016;10:321–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flynn JM, Jones KJ, Garner MR, Goebel J. Eleven years experience in the operative management of pediatric forearm fractures. J Pediatr Orthop 2010;30: 313–319. [DOI] [PubMed] [Google Scholar]
- 18.Fanuele J, Koval KJ, Lurie J, et al. Distal radial fracture treatment: what you get may depend on your age and address. J Bone Joint Surg [Am] 2009;91-A:1313–1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chung KC, Shauver MJ, Yin H, et al. Variations in the use of internal fixation for distal radial fracture in the United States medicare population. J Bone Joint Surg [Am] 2011;93-A: 2154–2162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bariteau JT, Hsu RY, Mor V, et al. Operative versus nonoperative treatment of geriatric ankle fractures: a Medicare Part A claims database analysis. Foot Ankle Int 2015;36:648–655. [DOI] [PubMed] [Google Scholar]
- 21.Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg [Am] 2009;91-A:1868–1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kang SN, Mangwani J, Ramachandran M, Paterson JMH, Barry M. Elastic intramedullary nailing of paediatric fractures of the forearm: a decade of experience in a teaching hospital in the United Kingdom. J Bone Joint Surg [Br] 2011;93-B:262–265. [DOI] [PubMed] [Google Scholar]
- 23.Fabricant PD, Seeley MA, Anari JB, et al. Medial epicondyle fractures in children and adolescents: shifting care from general hospitals to children’s hospitals? J Pediatr 2015;167:1116–1120. [DOI] [PubMed] [Google Scholar]
- 24.Dy CJ, Lyman S, Do HT, et al. Socioeconomic factors are associated with frequency of repeat emergency department visits for pediatric closed fractures. J Pediatr Orthop 2014;34:548–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sabharwal S, Zhao C, McClemens E, Kaufmann A. Pediatric orthopaedic patients presenting to a university emergency department after visiting another emergency department: demographics and health insurance status. J Pediatr Orthop 2007;27:690–694. [DOI] [PubMed] [Google Scholar]
- 26.Skaggs DL, Lehmann CL, Rice C, et al. Access to orthopaedic care for children with Medicaid versus private insurance: results of a national survey. J Pediatr Orthop 2006;26:400–404. [DOI] [PubMed] [Google Scholar]
- 27.Franklin CC, Robinson J, Noonan K, Flynn JM. Evidence-based medicine: management of pediatric forearm fractures. J Pediatr Orthop 2012;32:S131–S134. [DOI] [PubMed] [Google Scholar]
- 28.Lin Y, Pan IW, Mayer RR, Lam S. Complications after craniosynostosis surgery: comparison of the 2012 Kids’ Inpatient Database and Pediatric NSQIP Database. Neurosurg Focus 2015;39:E11. [DOI] [PubMed] [Google Scholar]
- 29.Heslin KC, Elixhauser A. Mental and Substance Use Disorders Among Hospitalized Teenagers, 2012: Statistical Brief #202. http://www.ncbi.nlm.nih.gov/pubmed/27253007 (date last accessed 7April2017). [PubMed]
- 30.To A, Puckett Y. Risk factors for inpatient hospital admission in pediatric burn patients. Cureus 2016;8:e602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Puckett Y, Ta A. Socioeconomic factors impact inpatient mortality in pediatric lymphoma patients. Cureus 2016;8:e624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Christian EA, Jin DL, Attenello F, et al. Trends in hospitalization of preterm infants with intraventricular hemorrhage and hydrocephalus in the United States, 2000-2010. J Neurosurg Pediatr 2016;17:260–269. [DOI] [PubMed] [Google Scholar]
- 33.Vigneswaran HT, Grabel ZJ, Eberson CP, Palumbo MA, Daniels AH. Surgical treatment of adolescent idiopathic scoliosis in the United States from 1997 to 2012: an analysis of 20,346 patients. J Neurosurg Pediatr 2015;16:322–328. [DOI] [PubMed] [Google Scholar]
- 34.Qureshi H, Ference E, Novis S, et al. Trends in the management of pediatric peritonsillar abscess infections in the U.S., 2000-2009. Int J Pediatr Otorhinolaryngol 2015;79:527–531. [DOI] [PubMed] [Google Scholar]
- 35.Witt WP, Weiss AJ, Elixhauser A. Overview of Hospital Stays for Children in the United States, 2012: Statistical Brief #187. http://www.ncbi.nlm.nih.gov/pubmed/25695124 (date last accessed 6April2017). [PubMed]
- 36.Novis SJ, Pritchett CV, Thorne MC, Sun GH. Pediatric deep space neck infections in U.S. children, 2000-2009. Int J Pediatr Otorhinolaryngol 2014;78:832–836. [DOI] [PubMed] [Google Scholar]
- 37.Hasegawa K, Tsugawa Y, Brown DFM, Camargo CA Jr.. Childhood asthma hospitalizations in the United States, 2000-2009. J Pediatr 2013;163: 1127–33. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gipson DS, Messer KL, Tran CL, et al. Inpatient health care utilization in the United States among children, adolescents, and young adults with nephrotic syndrome. Am J Kidney Dis 2013;61:910–917. [DOI] [PubMed] [Google Scholar]
- 39.Tzong KYS, Han S, Roh A, Ing C. Epidemiology of pediatric surgical admissions in US children: data from the HCUP kids inpatient database. J Neurosurg Anesthesiol 2012;24:391–395. [DOI] [PubMed] [Google Scholar]
- 40.Wier LM, Encinosa W. Obesity in Children: Hospitalizations from 2000 to 2009: Statistical Brief #138. http://www.ncbi.nlm.nih.gov/pubmed/22953352 (date last accessed 6April2017). [PubMed]


