Abstract
Objectives
Our two study objectives were: (1) to understand the relationship between the perception of a previous negative health care experience and race/ethnicity, and how socio-demographic, access-to-health-care, and self-reported health variables modified this relationship and (2) to assess how many behaviors participants reported changing as a result of experiencing a perceived negative health care experience, which behaviors they changed, and if there were differences in patterns of change across racial/ethnic groups.
Design
We conducted a cross-sectional survey of a convenience sample of 600 African American, Mexican-Hispanic, and white adults in socioeconomically diverse neighborhoods in Chicago, IL. We used multivariable logistic regression to analyze the relationship between a perceived negative health care experience in the last 5 years and race/ethnicity. We summed and then calculated the percentage of people who changed each of the 10 behaviors and evaluated whether or not there were differences in behavior change across racial/ethnic groups.
Principal Findings
More than 32% of participants reported a perceived negative health care experience in the past 5 years. Participants who had a bachelor’s degree or above (OR; 2.95,95%CI:1.01–8.63), avoided needed care due to cost (OR:1.84,95%CI:1.11–3.06), or who reported fair/poor health (OR:3.58,95%CI:1.66–7.80) had significantly increased odds of reporting a negative health care experience. Of these people, 88% reported “sometimes/always” changing at least one health seeking behavior. There were no racial/ethnic differences in reporting negative experiences or in patterns of behavior change.
Conclusions
Race/ethnicity was not related to reporting a perceived negative health care experience or reported patterns of behavior change in response to that experience. However those who avoided care due to cost, were more highly educated, or who indicated poorer health status reported having a negative experience more often. Our findings suggest that the perception of a previous negative experience may influence subsequent health care seeking behaviors.
Keywords: Negative Health Care Experience, Health Care Behaviors, Race/Ethnicity
1. Introduction
Negative health care experiences are an unfortunate reality in health care.(Avis, Bond et al. 1995; Lovgren, Engstrom et al. 1996; Phillips 1996; Coyle 1999; Rogers, Karlsen et al. 2000; Hsiung and Thomas 2001; Bankauskaite and Saarelma 2003; Suurmond, Uiters et al. 2011) These negative health care experiences likely lead to dissatisfaction with health care.(Eriksson and Svedlund 2007) Dissatisfaction is associated with lack of access,(Coyle 1999; Bankauskaite and Saarelma 2003; Martins 2008; Nickasch and Marnocha 2009; Lee, Moriarty et al. 2010) compassion,(Phillips 1996; Coyle 1999; Bankauskaite and Saarelma 2003; Martins 2008; Nickasch and Marnocha 2009; Lee, Moriarty et al. 2010; Suurmond, Uiters et al. 2011) quality amenities,(Bankauskaite and Saarelma 2003; Lee, Moriarty et al. 2010) and quality care.(Coyle 1999; Bankauskaite and Saarelma 2003; Martins 2008; Nickasch and Marnocha 2009; Lee, Moriarty et al. 2010; Suurmond, Uiters et al. 2011) Dissatisfaction with a health care encounter can lead to feelings of dehumanization,(Coyle 1999; Rogers, Karlsen et al. 2000) devaluation,(Lovgren, Engstrom et al. 1996; Coyle 1999) discrimination,(Eriksson and Svedlund 2007; Suurmond, Uiters et al. 2011) disempowerment,(Avis, Bond et al. 1995; Coyle 1999; Rogers, Karlsen et al. 2000) and distrust.(Eriksson and Svedlund 2007; Wen, Hudak et al. 2007; Martins 2008; Nickasch and Marnocha 2009; Suurmond, Uiters et al. 2011)
Previous studies have found that some specific consequences of a negative health care experience include avoidance of or delays seeking further health care,(Eriksson and Svedlund 2007; Wen, Hudak et al. 2007; Peek, Sayad et al. 2008) distrust or suspicion of the health care system,(Eriksson and Svedlund 2007; Wen, Hudak et al. 2007; Martins 2008; Nickasch and Marnocha 2009; Suurmond, Uiters et al. 2011) and/or exclusive use of the emergency department for all health care needs.(Martins 2008) These specific behavior changes have been associated with lower satisfaction with care,(Weiss and Ramsey 1989; Benkert, Peters et al. 2006; Benkert, Hollie et al. 2009; van Walraven, Oake et al. 2010) lower adherence to treatment recommendations,(Altice, Mostashari et al. 2001; Bickell, Weidmann et al. 2009; van Walraven, Oake et al. 2010) worse self-reported health,(Lee and Lin 2009) reduced willingness to seek care,(O’Malley, Mandelblatt et al. 1997; Schout, de Jong et al. 2010) and lower quality relationships with care providers.(Altice, Mostashari et al. 2001; Benkert, Peters et al. 2006; Stefanacci and Guerin 2013)
Race and ethnicity may be one factor that influences whether patients report having a previous a negative health care experience and how they respond to it. Previous research has shown that racial and ethnic minority populations are more likely to report low quality care due to their race or ethnicity,(Johnson, Saha et al. 2004) and are less satisfied with provider interactions than white patients.(Barr 2004) Additionally, there is greater distrust of health care among racial/ethnic minority populations in the US,(Doescher, Saver et al. 2000; LaVeist, Nickerson et al. 2000; Boulware, Cooper et al. 2003; Schwei, Kadunc et al. 2014) These data suggest that the health care experiences of racial and ethnic minority patients are different from those of white patients.(Smedley, Stith et al. 2003)
Previous research has shown that negative health care experiences can impact an individual’s future health seeking behaviors and subsequent health status in certain circumstances. However, most of these previous studies have used qualitative methods,(Lovgren, Engstrom et al. 1996; Coyle 1999; Bankauskaite and Saarelma 2003; Eriksson and Svedlund 2007; Wen, Hudak et al. 2007; Martins 2008; Nickasch and Marnocha 2009; Lee, Moriarty et al. 2010; Suurmond, Uiters et al. 2011) have examined specific health care settings(Avis, Bond et al. 1995; Eriksson and Svedlund 2007) and populations,(Wen, Hudak et al. 2007; Martins 2008; Nickasch and Marnocha 2009; Suurmond, Uiters et al. 2011) or have been conducted outside of the United States.(Lovgren, Engstrom et al. 1996; Phillips 1996; Bankauskaite and Saarelma 2003; Eriksson and Svedlund 2007) We contribute to this existing literature by quantifying the frequency with which study participants perceived having a previous negative health care experiences and the changes they made as a result of having that negative health care experience in a diverse sample of adults.
We had two objectives in this study. First, we wanted to better understand the relationship between self-report of a previous negative health care experience and race/ethnicity and how socio-demographic variables, access-to-health-care variables or self-reported health might modify that relationship. Second, we wanted to assess how many behaviors participants reported changing as a result of having a negative health care experience and the pattern of those changes and how they might vary across racial/ethnic group. Given that there is greater distrust of health care among racial/ethnic minority populations in the US and that they more often report low quality health care due to race and dissatisfaction with provider encounters,(Doescher, Saver et al. 2000; LaVeist, Nickerson et al. 2000; Boulware, Cooper et al. 2003; Barr 2004; Johnson, Saha et al. 2004; Schwei, Kadunc et al. 2014) we hypothesized that racial and ethnic minorities would more often perceive and report previous negative health care experiences even after controlling for socio-demographic characteristics, access to health care and self-reported health status. We also hypothesized that all groups would report changing their behaviors based on these previous negative experiences, but that self-reported health-behavior changes would be greater among racial/ethnic minorities.
2. Methods
2.1 Study Participants and Survey Development
We conducted a cross-sectional, computer administered survey among a convenience sample of adults shopping at selected supermarkets in 7 socioeconomically diverse neighborhoods in Chicago, IL. We sought to recruit African American, Mexican-Hispanic, and white community-based respondents with a range of socio-demographic characteristics. To meet this goal, we purposely recruited participants from grocery stores in 7 different Chicago neighborhoods based on the sociodemographic profile of those neighborhoods. These stores served neighborhoods that represented (1) upper middle class communities of mixed race, (2) predominantly Latino neighborhoods, and (3) several mixed income neighborhoods. Our goal was to recruit a sample that was diverse in their socioeconomic status and racial/ethnic identification.
Participants volunteered to complete one survey on the computer after passing the research table placed at the entrance of each supermarket; when we reached a sample of 200 participants from a particular racial/ethnic group, we no longer took volunteers from that group, allowing us to achieve a target study sample of 600 adults with equal proportions self-identifying as African American, Mexican-Hispanic and white. The original study was designed to examine the validity of a measure of trust in health care across three different racial/ethnic groups; hence, a sample of 200 from each racial/ethnic group was selected to achieve that goal. To be eligible, individuals were required to be fluent in English or Spanish, 18 years of age or older, and able to understand and provide consent. We administered the computer-administered survey in English or Spanish according to the preference of the respondent, and it took respondents between 20 and 30 minutes to complete. Respondents received $50 for participating. The Institutional Review Board of the Cook County Bureau of Health Services approved all study activities.
2.2 Measures
The questionnaire consisted of 235 items and evaluated numerous domains: socio-demographics, health care access and utilization, perception of having a previous negative health care experience, self-reported health and general attitudes and beliefs related to health care. All measures had been previously used with African American and Latino populations and had been validated for use in those populations.(Kaiser Permanente Division of Research 2005–2006; Matthews, Johnson et al. (2007) The entire survey was pilot-tested in 7 individuals in Spanish and English prior to use in the study. We used the following question to measure participants’ perception of having had a previous negative health care experience: “In the past five years, have you had a health care experience you considered to be bad or negative?” (yes or no). If participants responded yes, then they were asked “how often have you done the following (10) thing(s) because of that bad experience?”: decided not to follow your doctor’s advice; did not return for your next medical appointment; changed doctors or went for treatment elsewhere; stayed with the same doctor but trusted him or her less; stopped going to the doctor as often as you should; stopped treatment or going to the doctor entirely; did not go for treatment next time you were ill; changed hospitals or clinics; only go to the emergency room for treatment; and did not go for health care even though you thought you needed it. Possible responses for each question included “never”, “rarely”, “sometimes” or “always”. These 10 questions make up the Negative Health Care Experience Measure. (Matthews, Johnson et al. (2007)) There was one additional open ended question at the end of the Negative Health Care Experience Measure that asked individuals who had responded “rarely”, “sometimes” or “always” to the final item “please explain why you did not go for health care even though you thought you needed it?”
We included the following socio-demographic variables in logistic regression analyses: race/ethnicity, age (years), gender (male or female), marital status, employment status, income, and education level. Participants self-reported their race/ethnicity as African American, Mexican-Hispanic, or white; their marital status as married, previously married, or single (never married); their employment status as employed, unemployed, or homemaker/retired/student; their income as ≤ $15,999, $16,000-$34,999, $35,000-$74,999 or ≥ $75,000; and their education level as less than high school, high school/GED, trade school/associate’s degree, or bachelor’s degree and above.
We included three access-to-care variables in our analysis: insurance status, avoidance of care due to cost, and number of doctor visits in past 12 months. Participants reported their insurance status as private insurance, Medicare/Medicaid or no insurance. We asked participants the following question to see if they had previously avoided care due to cost: “Is there any time in the past two years, when you did not seek medical care because it was too expensive or health insurance did not cover it? Do not include dental care.” Possible responses included yes, no or not sure. We asked participants “Have you seen any doctor in the last 12 months? If yes, about how many times in the last 12 months have you seen a doctor (including your personal doctor)?” We ultimately classified responses into the following discrete categories: 0, 1–2, 3–5, or ≥ 6 visits in the last 12 months.
We included one variable assessing self-reported health status in the analysis. We asked participants, “in general, would you say your health is: excellent, very good, good, fair or poor.” Self-reported ill health is a widely used general indicator of health status that is strongly related to mortality and other objective measures of health.(DeSalvo, Fisher et al. 2006; DeSalvo, Jones et al. 2009)
2.3 Data analysis
We initially compared survey responses using chi-square tests for categorical variables and one-way analysis of variance (ANOVA) for continuous variables. We next conducted multivariable logistic regression models to estimate the relationship between reporting a perceived previous negative health care experience and race/ethnicity. We chose to sequentially examine blocks of independent variables that have previously been shown to be associated with racial/ethnic differences in health care in order to (1) first examine the hypothesis that the perception of negative health care experiences varied by race/ethnicity while controlling for basic demographic variables, (2) to determine if potential racial/ethnic variability could be accounted for by additional differences in socio-demographic variables, and (3) to determine if racial/ethnic differences may be accounted for by variability in access-to-health-care or self-reported health. Model 1 included race, age, gender and marital status; Model 2 added several socioeconomic variables; and Model 3 added health care access, utilization, and self-reported health measures. Due to small numbers in the poor health category of self-reported health, we collapsed fair and poor health into one category. Participants with missing data were not included in the logistic regression models. In the first model, 53 participants were excluded due to missing data, in the second model an additional 49 participants were not included (102 total), and an additional 59 participants were not included in the third model (161 total).
Next, we examined how many behaviors, if any, participants reported changing in response to having a past negative health care experience and if there were differences across racial/ethnic group in the pattern of behavior change. In this analysis we only included participants who reported having a previous negative health care experience (n=187). Participants who did not answer all 10 questions (n=27) were dropped from these analyses. To facilitate the interpretation of the results, we dichotomized the 10 Negative Health Care Experience Measure questions into did-not-change behavior (“never” and “rarely”) and changed behavior (“sometimes” and “always”). We counted the number of behaviors changed by individual and summed the total. We also calculated the percentage of people who did and did not change each of the 10 behaviors in the Negative Health Care Experience Measure. To assess differences in self-reported behavior change across racial and ethnic groups, we used a chi-square test to compare the survey responses for each of the 10 items individually and the sum of the ten items. Statistical data analysis was performed using STATA 12.
Seventy six participants responded “rarely”, “sometimes” or “always” to the final item “did not go care even though you thought you needed it” and were asked the follow up question, “Please explain why you did not go for health care even though you thought you needed it?” We examined these responses to see if the participants in our study reported avoiding care for reasons that were consistent with what has previously been reported in the literature. To analyze the responses we categorized them into large overarching categories (ex: too expensive) and we reported the most common response categories.
3. Results
Of the 600 respondents, 35.6% self-identified as African American, 32.3% as Mexican-Hispanic and 33.0% as white. Socio-demographic, access-to-care and overall health status differences are reported by race/ethnicity in Table 1.
Table 1.
Sociodemographic Characteristics of Sample Across Three Racial Ethnic Groups
| Study Variables | Overall (n=600) | African American (n=208) | Mexican-Hispanic (n=194) | White (n=198) | P-Value‡ |
|---|---|---|---|---|---|
| Mean age (SD), y | 40 (14) | 42 (12) | 36 (14) | 43(16) | <0.001† |
| Female (%, #) | 59 (346) | 58 (117) | 64 (125) | 53 (104) | 0.066 |
| Marital Status (%) | <0.001† | ||||
| Married | 43 (253) | 25 (50) | 61 (117) | 44 (86) | |
| Previously Married | 17 (100) | 22 (44) | 8 (16) | 20 (40) | |
| Single (Never Married) | 40 (239) | 54 (109) | 31 (59) | 36 (71) | |
| Employment Status (%) | <0.001† | ||||
| Employed | 53 (315) | 46 (92) | 57 (109) | 58 (114) | |
| Unemployed | 28 (164) | 40 (81) | 18 (34) | 25 (49) | |
| Homemaker/Retired/Student | 19 (112) | 14 (28) | 26 (50) | 17 (34) | |
| Family Income (%) | <0.001† | ||||
| ≤$15,999 | 44 (244) | 60 (117) | 41 (72) | 30 (55) | |
| $16,000–$34,999 | 25 (140) | 25 (49) | 25 (44) | 26 (47) | |
| $35,000–$74,999 | 21 (114) | 12 (24) | 23 (40) | 27 (50) | |
| ≥$75,000 | 10 (55) | 3 (6) | 10 (18) | 17 (31) | |
| Education Level (%) | <0.001† | ||||
| Less than High School | 10 (58) | 9 (19) | 17 (32) | 4 (7) | |
| High School/GED | 53 (318) | 63 (130) | 49 (94) | 48 (94) | |
| Trade School/Associate’s Degree | 18 (107) | 18 (36) | 17 (32) | 20 (39) | |
| Bachelor’s Degree and Above | 19 (112) | 10 (20) | 18 (35) | 29 (57) | |
| Insurance Status (%) | <0.001† | ||||
| Private Insurance | 48 (269) | 39 (71) | 46 (88) | 57 (110) | |
| Medicare/Medicaid | 29 (166) | 43 (78) | 25 (47) | 21 (41) | |
| No Insurance | 23 (130) | 17 (31) | 29 (56) | 22 (43) | |
| Avoid Care due to Cost (%) | 0.436 | ||||
| No | 54 (318) | 52 (104) | 52 (100) | 58 (114) | |
| Yes | 38 (223) | 40 (79) | 38 (73) | 36 (71) | |
| Not Sure/Refused | 8 (45) | 9 (17) | 9 (18) | 5 (10) | |
| # Annual Doctor Visits (%) | 0.030* | ||||
| 0 | 22 (115) | 20 (32) | 27 (48) | 19 (35) | |
| 1–2 | 28 (151) | 21 (34) | 28 (50) | 35 (67) | |
| 3–5 | 32 (169) | 38 (61) | 56 (31) | 27 (52) | |
| ≥6 | 18 (95) | 21 (33) | 15 (27) | 19 (35) | |
| Self-Reported Health Status (%) | 0.022* | ||||
| Excellent | 15 (90) | 15 (30) | 13 (25) | 18 (35) | |
| Very Good | 27 (160) | 25 (50) | 24 (45) | 34 (65) | |
| Good | 34 (198) | 33 (66) | 36 (69) | 33 (63) | |
| Fair | 18 (108) | 21 (43) | 24 (45) | 10 (20) | |
| Poor | 5 (28) | 6 (12) | 4 (7) | 5 (9) | |
| Previous Negative Experience (%) | 32 (187) | 29 (56) | 33 (63) | 35 (68) | 0.355 |
Significant at P < 0.05,
Significant at P <0.001
p-values measure any difference in three racial/ethnic groups
Overall, 187 people or 32.3% (28.6% of African American, 33.1% of Mexican-Hispanic, and 35.2% of whites) reported a perceived negative health care experience in the past 5 years. There were no socio-demographic differences between people who perceived having a negative health care experience in the past 5 years and people who did not. However, people who perceived having had a negative health care experience in the last five years were more likely to have avoided care due to cost (51% vs. 31% p < 0.001) and were more likely to have ≥6 doctor visits in the past 12 months (24% vs. 15% p = 0.046) compared to those that did not have a previous negative experience. Furthermore, individuals who perceived having a negative experience in the past 5 years were more likely to self-report their current health status as poor compared to individuals who did not (8% vs. 3% p < 0.001).
Table 2 presents the odds of reporting a perceived negative health care experience in the past 5 years across the three different logistic regression models. There was no significant relationship between race/ethnicity and report of a perceived, past negative health care experience (Model 1) and this did not change with adjustments (Models 2 and 3). There was an association between income and report of a negative health care experience in Model 2; The odds of reporting a perceived negative health care experience were lower in the family income category of greater than $75,000 compared to those who reported a family income of less than $16,000 (0.36; 95%CI: 0.16–0.81). In model 3, family income was no longer significantly associated with report of a previous negative experience. However, higher education, avoiding care due to cost, and reporting fair or poor health were associated with report of a perceived, past negative health care experience. The odds of reporting a previous negative health care experience were greater in the highest education group compared to those with less than a high school education (OR:2.95 95%CI:1.01–8.63); in the group reporting having avoided care due to cost compared to those who didn’t (OR:1.84, 95%CI:1.11–3.06); and those who reported fair/poor health status compared to those who reported excellent health (OR: 3.58, 95%CI 1.66–7.80).
Table 2.
Odds of a previous negative health care experience in 3 logistic regression models
| Model 1 n=547 OR (95% CI) |
Model 2 n=498 OR (95% CI) |
Model 3 n=439 OR (95% CI) |
|
|---|---|---|---|
| Race/Ethnicity | |||
| White | ref | ref | ref |
| African-American | 0.73 (0.46–1.14) | 0.67 (0.41–1.10) | 0.61 (0.34–1.10) |
| Mexican-Hispanic | 0.88 (0.57–1.38) | 0.93 (0.57–1.52) | 0.79 (0.47–1.34) |
| Age | 1.00 (0.98–1.01) | 1.00 (0.98–1.01) | 0.99 (0.97–1.01) |
| Female | 1.39 (0.96–2.02) | 1.49 (1.00–2.22) | 1.36 (0.87–2.16) |
| Marital Status | |||
| Married | ref | ref | ref |
| Previously Married | 0.89 (0.52–1.53) | 0.67 (0.37–1.21) | 0.69 (0.35–1.34) |
| Single (Never Married) | 0.85 (0.56–1.31) | 0.80 (0.50–1.26) | 0.71 (0.42–1.20) |
| Employment Status | |||
| Employed | ref | ref | |
| Unemployed | N/A | 1.52 (0.93–2.45) | 1.02 (0.58–1.82) |
| Homemaker/Retired/Student | N/A | 1.09 (0.63–1.88) | 1.29 (0.70–2.41) |
| Family Income | |||
| ≤$15,999 | ref | ref | |
| $16,000–$34,999 | N/A | 0.98 (0.59–1.60) | 1.80 (0.71–4.58) |
| $35,000–$74,999 | N/A | 0.57 (0.31–1.04) | 1.89 (0.81–4.39) |
| ≥$75,00 | N/A | 0.36 (0.16–0.81)* | 1.34 (0.59–3.07) |
| Education Level | |||
| Less than High School | ref | ref | |
| High School/GED | N/A | 1.39 (0.68–2.85) | 1.84 (0.71–4.74) |
| Trade School/Associate’s Degree | N/A | 2.05 (0.90–4.66) | 2.45 (0.86–7.01) |
| Bachelor’s Degree and Above | N/A | 2.14 (0.92–4.95) | 2.95 (1.01–8.63)* |
| Insurance Status | |||
| Private Insurance | ref | ||
| Medicare/Medicaid | N/A | N/A | 1.29 (0.71–2.33) |
| No Insurance | N/A | N/A | 0.90 (0.46–1.75) |
| # Annual Doctor Visits | |||
| 0 | ref | ||
| 1–2 | N/A | N/A | 1.53 (0.79–2.96) |
| 3–5 | N/A | N/A | 1.29 (0.68–2.43) |
| ≥ 6 | N/A | N/A | 1.93 (0.92–4.06) |
| Avoided Care Due to Cost | |||
| No | ref | ||
| Yes | N/A | N/A | 1.84 (1.11–3.06)* |
| Not Sure/Refused | N/A | N/A | 0.80 (0.32–1.99) |
| Self-Reported Health Status (%) | |||
| Excellent | ref | ||
| Very Good | N/A | N/A | 1.09 (0.52–2.27) |
| Good | N/A | N/A | 1.92 (0.95–3.90) |
| Fair or Poor | N/A | N/A | 3.58 (1.66–7.80)* |
Significant at p<0.05
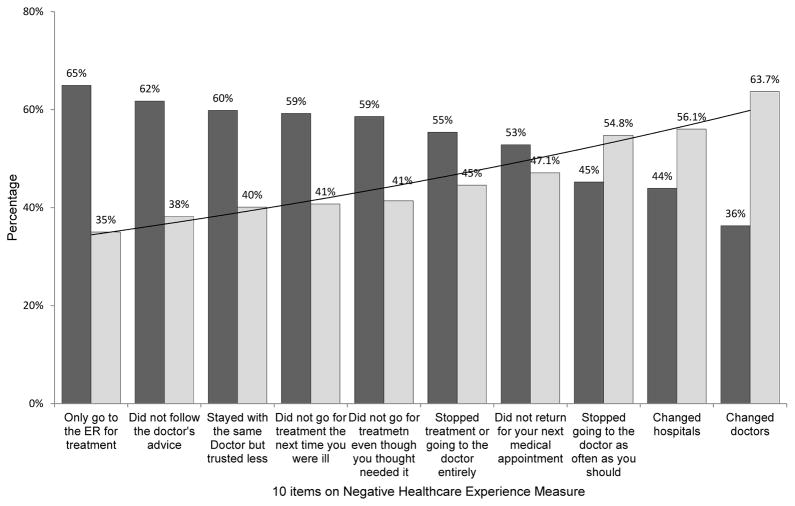
On average, individuals reported changing 4.6 behaviors as a result of a negative health care experience, and 88% of individuals reported changing at least one behavior. The four most commonly changed behaviors (Figure 1) were “changed doctors or went for treatment elsewhere” (63.8%), “changed hospitals or clinics” (56.9%), “stopped going to the doctor as often as you should” (53.4%), and “did not return for your next medical appointment” (46.9%). We found no differences in the frequency of report of changes in each of the ten specific behaviors in the Negative Health Care Experience Measure across racial/ethnic groups.
Figure 1.
The Percentage of Participants who Self-Reported Changing the Individual Behaviors on the 10-Item Negative Health Care Experience Measure (n=160)
 Never or Rarely Changed Behaviors
Never or Rarely Changed Behaviors
 Sometimes or Always Changed Behaviors
Sometimes or Always Changed Behaviors
59% of respondents answered “rarely”, “sometimes” or “always” to the final item and they identified various reasons for not seeking health care even though they thought they needed it. The most common reasons identified were too expensive or no insurance, difficulty scheduling an appointment, lack of compassion from health care workers, and a general feeling that they do not receive quality care from their health care system.
4. Discussion
Overall, one third of individuals in our sample reported having perceived at least one negative health care experience in the last five years, and those who did were more educated, had poorer access-to-care and had poorer health status than those that did not. There were no differences by race/ethnicity in frequency of perception of negative health care experiences or in frequency of report of changes in each of the ten specific behaviors in the Negative Health Care Experience Measure. About 9-in-10 individuals reporting a negative health care experience changed at least one behavior as a result of the perceived negative encounter and on average, individuals reported changing 4.6 of the 10 behaviors.
We were surprised that we did not find differences in report of perceived previous negative health care experience across racial and ethnic groups given that previous studies have shown that there is greater dissatisfaction with care in minority groups compared to whites.(Coyle 1999; Garrett, Dickson et al. 2008) In our previous work using data from this same study, we found that African Americans and Mexican-Hispanics participants in this study have lower trust in health care compared to whites.(Schwei, Kadunc et al. 2014) Additionally, we have shown that patients who perceived that they had a negative health care experience in the past 5 years had lower institutional trust than patients who don’t.(Schwei, Kadunc et al. 2014) Taken in the context of this previous work, the findings we report in this analysis suggest that the experience of having or perceiving to have had a negative interaction in the health care setting does not vary by race/ethnicity, but is related to greater distrust of health care and subsequent disengagement from care.
We also found that individuals with a bachelor’s degree or more reported the perception of negative health care experiences more often than patients with less than a high school education. It is plausible that individuals with a bachelor’s degree or more education are more comfortable reporting that they perceived to have had negative health care experience as compared to individuals with a lower level of education or that they have higher expectations than other groups. Individuals who perceived to have had a previous negative health care experience may also have been hesitant to seek care for an illness for financial reasons until the illness or injury had progressed to a more serious state. Previous research has shown that worrying about cost is a commonly cited barrier for delaying care.(Strunk and Cunningham 2002) It is also possible, as shown in previous work, that a complicated medical history could contribute to the perception of a negative health care experience.(Coyle 1999)
Of note, the significantly lower odds of reporting a negative experience in health care for the highest income group was no longer significant in the fully adjusted model and the odds were higher. We conducted a number of follow-up analyses to try to better understand what might account for this change but could find no one single covariate that contributed to it. It appears that avoided health care due to cost and self-rated health, together, are providing information that is also represented in family income.
Similar to what has been found in other work,(Hsiung and Thomas 2001; Eriksson and Svedlund 2007; Martins 2008; Peek, Sayad et al. 2008; Nickasch and Marnocha 2009; Suurmond, Uiters et al. 2011) our study supports the idea that a perceived negative health care experience prompts individuals to change their care seeking behaviors. We specifically examined 10 behavior changes that can have negative consequences for an individual’s future health outcomes,(Weiss and Ramsey 1989; Altice, Mostashari et al. 2001; Benkert, Peters et al. 2006; Benkert, Hollie et al. 2009; Bickell, Weidmann et al. 2009; Lee and Lin 2009; van Walraven, Oake et al. 2010; Stefanacci and Guerin 2013) and we found that almost all individuals change at least one behavior. These changes in behavior have implications for the continuity of care an individual receives from an individual provider or a health care system in general and their ability to get the care they need.
The open-ended question at the end of the Negative Health Care Experiences Measure, allowed us to ask people why a negative health care experience resulted in individuals not going for health care even though they thought they needed it. Consistent with previous studies, our sample indicated that a previous negative experience often lead to an unwillingness to seek care for reasons such as lack of access,(Coyle 1999; Bankauskaite and Saarelma 2003; Martins 2008; Nickasch and Marnocha 2009; Lee, Moriarty et al. 2010) lack of compassion from health care workers,(Phillips 1996; Coyle 1999; Bankauskaite and Saarelma 2003; Martins 2008; Nickasch and Marnocha 2009; Lee, Moriarty et al. 2010; Suurmond, Uiters et al. 2011) and lack of quality care.(Coyle 1999; Bankauskaite and Saarelma 2003; Martins 2008; Nickasch and Marnocha 2009; Lee, Moriarty et al. 2010; Suurmond, Uiters et al. 2011) Our findings support this idea that a previous negative health care experience is a barrier to the utilization of the health care system for a variety of different reasons.
4.1 Strengths and Limitations
Several methodological issues may limit the generalizability of our findings. The data were collected from a convenience sample of Chicago residents shopping at selected supermarkets, and therefore we were not able to survey consumers who are home bound. In our sample, the average person has lower socioeconomic status and lower educational attainment than the average person in the United States and therefore these results may not be generalizable to the broader population. In addition, our measures of behavior change were self-reports and cross-sectional, making it difficult to establish the temporal ordering of events. Also, the perception of a negative health care experience was a single-item variable which could be interpreted in different ways. Finally, we do not have any specific details on the severity or number of negative encounters that individuals perceived to have experienced so it is likely that the negative health care experiences that people identified ranged from a provider being late to a misdiagnosis and they could range from one negative experience to many negative experiences.
There are also several strengths to this study. First, in addition to examining the perception of previous negative health care experiences in our population, we were able to examine the link between the perception of a previous negative health care experience and self-reported changes in health seeking behaviors. Secondly, we used a racially and ethnically diverse sample in which to examine this question. Finally, by surveying individuals in grocery stores, we inquired about the perception of having previous negative health care experiences outside of the health care system, and this may have allowed individuals to be more forthcoming about previous negative experiences without fears of compromising the quality of the health care they receive.
4.2 Conclusions
Our study provides evidence that many people report perceiving having had a negative health care encounter in the past five years, and that the perception of previous negative experiences does not vary appreciably across racial and ethnic groups. Further, for most people in our sample, the perception of a previous negative health care encounter lead to one or more clinically significant behavior changes that have the potential to impact the individual’s future health. Research should continue to explore how other factors such as trust or discrimination are related to the perception of a previous negative health care experience and how perceived severity of a negative health care experience relates to behavior changes in order to further the goal of decreasing the prevalence of these experiences and their consequences.
Contributor Information
Rebecca J. Schwei, Department of Medicine, University of Wisconsin School of Medicine and Public Health, Suite 210, 800 University Bay Drive, Madison, WI 53705, (608)262-8312 (phone), (888)263-2864 (fax).
Timothy Johnson, Institute for Health Research and Policy, University of Illinois at Chicago, Westside Research Office Bldg., 1747 West Roosevelt Road, Chicago, IL 60608-1264, (312) 996-5310 (phone), (312) 996-3358 (fax).
Alicia K. Matthews, Institute for Health Research and Policy, University of Illinois at Chicago, Westside Research Office Bldg., 1747 West Roosevelt Road, Chicago, IL 60608-1264, (312) 996-7885 (phone), (312) 996-9049 (fax).
Elizabeth A. Jacobs, Departments of Medicine & Population Health Sciences, University of Wisconsin School of Medicine and Public Health, Suite 210, 800 University Bay Drive, Madison, WI 53705, (608) 262-8302 (phone), (888) 263-2864 (fax).
References
- Altice FL, Mostashari F, et al. Trust and the acceptance of and adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2001;28(1):47–58. doi: 10.1097/00042560-200109010-00008. [DOI] [PubMed] [Google Scholar]
- Avis M, Bond M, et al. Exploring patient satisfaction with out-patient services. J Nurs Manag. 1995;3(2):59–65. doi: 10.1111/j.1365-2834.1995.tb00082.x. [DOI] [PubMed] [Google Scholar]
- Bankauskaite V, Saarelma O. Why are people dissatisfied with medical care services in Lithuania? A qualitative study using responses to open-ended questions. Int J Qual Health Care. 2003;15(1):23–9. doi: 10.1093/intqhc/15.1.23. [DOI] [PubMed] [Google Scholar]
- Barr DA. Race/ethnicity and patient satisfaction. Using the appropriate method to test for perceived differences in care. J Gen Intern Med. 2004;19(9):937–43. doi: 10.1111/j.1525-1497.2004.30415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benkert R, Hollie B, et al. Trust, mistrust, racial identity and patient satisfaction in urban African American primary care patients of nurse practitioners. J Nurs Scholarsh. 2009;41(2):211–9. doi: 10.1111/j.1547-5069.2009.01273.x. [DOI] [PubMed] [Google Scholar]
- Benkert R, Peters RM, et al. Effects of perceived racism, cultural mistrust and trust in providers on satisfaction with care. J Natl Med Assoc. 2006;98(9):1532–40. [PMC free article] [PubMed] [Google Scholar]
- Bickell NA, Weidmann J, et al. Underuse of breast cancer adjuvant treatment: patient knowledge, beliefs, and medical mistrust. J Clin Oncol. 2009;27(31):5160–7. doi: 10.1200/JCO.2009.22.9773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulware LE, Cooper LA, et al. Race and trust in the health care system. Public Health Rep. 2003;118(4):358–65. doi: 10.1016/S0033-3549(04)50262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyle J. Exploring the meaning of ‘dissatisfaction’ with health care: the importance of ‘personal identity threat’. Sociology of Health & Illness. 1999;21(1):95–124. [Google Scholar]
- Coyle J. Understanding dissatisfied users: developing a framework for comprehending criticisms of health care work. J Adv Nurs. 1999;30(3):723–31. doi: 10.1046/j.1365-2648.1999.01137.x. [DOI] [PubMed] [Google Scholar]
- DeSalvo KB, Fisher WP, et al. Assessing measurement properties of two single-item general health measures. Qual Life Res. 2006;15(2):191–201. doi: 10.1007/s11136-005-0887-2. [DOI] [PubMed] [Google Scholar]
- DeSalvo KB, Jones TM, et al. Health care expenditure prediction with a single item, self-rated health measure. Med Care. 2009;47(4):440–7. doi: 10.1097/MLR.0b013e318190b716. [DOI] [PubMed] [Google Scholar]
- Doescher MP, Saver BG, et al. Racial and ethnic disparities in perceptions of physician style and trust. Arch Fam Med. 2000;9(10):1156–63. doi: 10.1001/archfami.9.10.1156. [DOI] [PubMed] [Google Scholar]
- Eriksson U, Svedlund M. Struggling for confirmation--patients’ experiences of dissatisfaction with hospital care. J Clin Nurs. 2007;16(3):438–46. doi: 10.1111/j.1365-2702.2005.01544.x. [DOI] [PubMed] [Google Scholar]
- Garrett PW, Dickson HG, et al. “The Happy Migrant Effect”: perceptions of negative experiences of healthcare by patients with little or no English: a qualitative study across seven language groups. Qual Saf Health Care. 2008;17(2):101–3. doi: 10.1136/qshc.2007.022426. [DOI] [PubMed] [Google Scholar]
- Hsiung PC, Thomas V. Coping strategies of people with HIV/AIDS in negative health care experiences. AIDS Care. 2001;13(6):749–62. doi: 10.1080/09540120120076913. [DOI] [PubMed] [Google Scholar]
- Johnson RL, Saha S, et al. Racial and ethnic differences in patient perceptions of bias and cultural competence in health care. J Gen Intern Med. 2004;19(2):101–10. doi: 10.1111/j.1525-1497.2004.30262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Permanente Division of Research. Distance Diabetes Study of Northern California. 2005–2006 from https://www.dor.kaiser.org/external/uploadedFiles/content/research/distance/DISTANCE_Survey_FINAL_2006.pdf.
- LaVeist TA. Disentangling race and socioeconomic status: a key to understanding health inequalities. J Urban Health. 2005;82(2 Suppl 3):iii26–34. doi: 10.1093/jurban/jti061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist TA, Nickerson KJ, et al. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev. 2000;57(Suppl 1):146–61. doi: 10.1177/1077558700057001S07. [DOI] [PubMed] [Google Scholar]
- Lee AV, Moriarty JP, et al. What can we learn from patient dissatisfaction? An analysis of dissatisfying events at an academic medical center. J Hosp Med. 2010;5(9):514–20. doi: 10.1002/jhm.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee YY, Lin JL. The effects of trust in physician on self-efficacy, adherence and diabetes outcomes. Soc Sci Med. 2009;68(6):1060–8. doi: 10.1016/j.socscimed.2008.12.033. [DOI] [PubMed] [Google Scholar]
- Lovgren G, Engstrom B, et al. Patients’ narratives concerning good and bad caring. Scand J Caring Sci. 1996;10(3):151–6. doi: 10.1111/j.1471-6712.1996.tb00328.x. [DOI] [PubMed] [Google Scholar]
- Martins DC. Experiences of homeless people in the health care delivery system: a descriptive phenomenological study. Public Health Nurs. 2008;25(5):420–30. doi: 10.1111/j.1525-1446.2008.00726.x. [DOI] [PubMed] [Google Scholar]
- Matthews A, Johnson T, et al. Emotional Distress and Reduction in Health Care Utilization Following a Negative Experience in Health Care 2007 [Google Scholar]
- Nickasch B, Marnocha SK. Healthcare experiences of the homeless. J Am Acad Nurse Pract. 2009;21(1):39–46. doi: 10.1111/j.1745-7599.2008.00371.x. [DOI] [PubMed] [Google Scholar]
- O’Malley AS, Mandelblatt J, et al. Continuity of care and the use of breast and cervical cancer screening services in a multiethnic community. Arch Intern Med. 1997;157(13):1462–70. [PubMed] [Google Scholar]
- Peek ME, Sayad JV, et al. Fear, fatalism and breast cancer screening in low-income African-American women: the role of clinicians and the health care system. J Gen Intern Med. 2008;23(11):1847–53. doi: 10.1007/s11606-008-0756-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips D. Medical professional dominance and client dissatisfaction. A study of doctor-patient interaction and reported dissatisfaction with medical care among female patients at four hospitals in Trinidad and Tobago. Soc Sci Med. 1996;42(10):1419–25. doi: 10.1016/0277-9536(95)00290-1. [DOI] [PubMed] [Google Scholar]
- Rogers A, Karlsen S, et al. ‘All the services were excellent. It is when the human element comes in that things go wrong’: dissatisfaction with hospital care in the last year of life. J Adv Nurs. 2000;31(4):768–74. doi: 10.1046/j.1365-2648.2000.01347.x. [DOI] [PubMed] [Google Scholar]
- Schout G, de Jong G, et al. Establishing contact and gaining trust: an exploratory study of care avoidance. J Adv Nurs. 2010;66(2):324–33. doi: 10.1111/j.1365-2648.2009.05171.x. [DOI] [PubMed] [Google Scholar]
- Schwei RJ, Kadunc K, et al. Impact of sociodemographic factors and previous interactions with the health care system on institutional trust in three racial/ethnic groups. Patient Educ Couns. 2014;96(3):333–8. doi: 10.1016/j.pec.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley B, Stith A, et al. Unequal treatment: Confronting racial and ethnic disparities in health care. Institute of Medicine of the National Academies; Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- Stefanacci RG, Guerin S. Why medication adherence matters to patients, payers, providers. Manag Care. 2013;22(1):37–9. [PubMed] [Google Scholar]
- Strunk BC, Cunningham PJ. Treading water: Americans’ access to needed medical care, 1997–2001. Track Rep. 2002;(1):1–6. [PubMed] [Google Scholar]
- Suurmond J, Uiters E, et al. Negative health care experiences of immigrant patients: a qualitative study. BMC Health Serv Res. 2011;11:10. doi: 10.1186/1472-6963-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Walraven C, Oake N, et al. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract. 2010;16(5):947–56. doi: 10.1111/j.1365-2753.2009.01235.x. [DOI] [PubMed] [Google Scholar]
- Weiss GL, Ramsey CA. Regular source of primary medical care and patient satisfaction. QRB Qual Rev Bull. 1989;15(6):180–4. doi: 10.1016/s0097-5990(16)30289-5. [DOI] [PubMed] [Google Scholar]
- Wen CK, Hudak PL, et al. Homeless people’s perceptions of welcomeness and unwelcomeness in healthcare encounters. J Gen Intern Med. 2007;22(7):1011–7. doi: 10.1007/s11606-007-0183-7. [DOI] [PMC free article] [PubMed] [Google Scholar]