Abstract
Rib fractures are a common injury resulting from blunt chest trauma. The most important complications associated with rib fractures include death, pneumonia, and the need for mechanical ventilation. The development of new osteosynthesis materials has stimulated increased interest in the surgical treatment of rib fractures. Surgical stabilisation, however, is not needed for every patient with rib fractures or for every patient with flail chest. This paper presents an easy-to-use evidence-based algorithm, developed by the authors, for the treatment of patients with flail chest and isolated rib fractures.
Keywords: Rib fractures, Morbidity, Mortality, Rib fixation, Algorithm
Introduction
Rib fractures are a common injury. They comprise 12% of all fractures seen in patients, particularly in the elderly [1], and approximately 10% of blunt trauma patients have rib fractures [2].
Several studies have revealed significant morbidity and mortality to be associated with rib fractures, even with rib fracture(s) as an isolated injury [3]. Tanaka et al. [4] described a mortality rate up to 51%. Twenty-five percent of trauma deaths are due to blunt thoracic trauma, with two-thirds of these patients having rib fractures [5,6]. In trauma deaths due to motor vehicle accidents, over 55% of the casualties aged 65 years or older only had rib fractures [3]. The most common complication of patients with rib fractures is pneumonia, with rates of up to 70% [4].
The major goal in the treatment of patients with rib fractures is reducing pain, thereby making the patient comfortable and subsequently improving respiration and preventing pneumonia. If pain control is not optimised, breathing excursions will diminish and coughing will be prevented, increasing the risk of pneumonia.
Several treatment modalities have been described, ranging from simple non-operative management with painkillers to extensive surgical treatments that stabilise rib fractures [7]. History has shown that stabilisation has been achieved using several different devices [8–10]. The introduction of dedicated new materials is again stimulating interest in the operative treatment of rib fractures. Surgical treatment has therefore experienced a boost, making it an interesting option within the spectrum of treatment modalities [3,11–15]. However, no real consensus has been reached for determining which patients require surgery and which do not. The challenge is to identify the right therapy for the right patient.
A treatment algorithm is proposed based on a combination of clinical experience and an analysis of the available literature that was conducted to identify the relevant risk factors.
Materials and methods
A literature search in Medline was performed using the key words: rib fracture, morbidity, mortality, and surgical stabilization. A total of 182 abstracts were found and analysed independently by 2 reviewers. For evaluating the clinical results, only abstracts published after 2000 were used.
Two subgroups of abstracts were created. The first group described the morbidity and mortality of patients with rib fractures, regardless of the therapy given. The second subgroup described the results of surgical stabilisation in patients with rib fractures, flail chest, and isolated rib fractures.
The first subgroup was analysed to establish a baseline for the morbidity and mortality in patients with rib fractures. Factors determining morbidity and mortality were identified. After defining specific morbidity and mortality levels relative to the risk factors, the reviewers analysed the second subgroup of abstracts in order to determine whether the operative stabilisation of rib fractures may have additional value in the treatment of patients with rib fractures.
The second subgroup was then analysed to determine whether the operative stabilization of rib fractures provided additional value in the treatment of patients with rib fractures.
Morbidity and mortality of patients with rib fractures
Significant morbidity and mortality was described in association with rib fractures. There was a significant association between the number of rib fractures and morbidity (p=0.027) [1,2,4,16,17].
The most commonly described complication was pneumonia, depending on which group of patients was analysed; in flail chest, a rate of up to 70% has been described [4]. Other frequently seen complications include increased hospital length of stay (HLOS), increased length of intensive care unit (ICU) stay, increased ventilator dependency, acute respiratory distress syndrome (ARDS), systemic inflammatory response syndrome (SIRS), prolonged pain (>2 months), prolonged disability (>2 months), and even the inability to return to work.
In addition to the number of rib fractures, age is a relevant factor in relation to morbidity and mortality. Holcomb et al. [16] identified a significant (p<0.05) increase in both HLOS and ICU stay due to the age of the patient: 14.0±2.2 days and 7.5±1.8 days, respectively, for patients older than 45 years compared to 8.0±1.0 days and 2±1 days, respectively, for younger patients. Mechanical ventilation was necessary in 60% of patients for an average of 13 days, and ventilator days increased with age and the number of fractured ribs [16,17]. Unplanned intubation after hospital admission because of rib fractures was associated with increased rates of ARDS, pneumonia, and SIRS. Age over 45 years and having more than 4 rib fractures were identified as significant risk factors [3,5,16].
Prolonged pain and disability have been well described [18]. It was previously thought that pain and disability due to rib fractures would last no more than 6–8 weeks, but 59% of patients had prolonged (>6 weeks) pain and 76% of patients had a prolonged disability [18]. Up to 29% of patients were unable to return to work after rib fractures. Quality of life was significantly reduced in patients with rib fractures [11].
Mortality was found to be significant in patients with rib fractures. The overall mortality was 10%, and patients with flail chest exhibited a mortality of up to 51% [17]. Patients older than 65 years with more than 3 rib fractures had a triple or higher chance of dying due to the rib fractures [1]. Bergeron et al. [2] analysed 4,325 cases of blunt chest trauma and found that the mortality increased 8-fold with 6 or more rib fractures in patients older than 65. Holcomb et al. [16] performed a retrospective analysis of 171 chest trauma patients and reported that the morbidity was greater in patients with more than 4 rib fractures. Flagel et al. [17] performed a retrospective analysis of the national trauma database containing 731,823 patients. He found that 64,750 patients (9%) sustained rib fractures, which is similar to the previously mentioned figure of 10%. Flagel et al. [17] also found the following correlations between rib fractures and mortality: 4 rib fractures increased the mortality rate from 5.8% to 8.1%, 6 rib fractures increased the mortality rate to 11.8%, and if a patient had more than 8 rib fractures, the mortality increased to above 34%.
It is clear that age and the number of rib fractures are important factors concerning the prognosis of the patient.
Operative treatment of rib fractures
Analysing the literature reveals that there are 2 main groups of patients with rib fractures. The first group are patients with flail chest, defined as a chest injury with 3 or more, consecutive, ipsilateral, double-broken ribs. The second group are patients with multiple rib fractures with no flail component. The flail group has received the most attention from a scientific point of view. Many articles have been published describing the benefit of operative treatment of flail chest using different kinds of osteosynthesis materials [4,11–14,19–23].
A comparison of the morbidity outcomes of surgical versus non-operative management of patients with rib fractures reveals the following. A significant reduction in pneumonia rates was found in surgically treated patients: 90% versus 22% at 21 days after surgery (p<0.05) [4]. The HLOS and ICU stay were significantly reduced by up to 50% [11,19,20]. For example, Marasco et al. [11] found results of 359 hours compared to 285 hours, in favour of the surgically stabilized patients (p<0.03). Ventilator days were significantly reduced, not only in patients with flail chest, but also in patients with multiple rib fractures who were unresponsive to pain medication [4,15,20,21]. Other outcomes, such as unplanned intubation, tracheostomies, sepsis, and ARDS were significantly reduced in surgically treated flail chest patients. Lung capacity after surgical stabilization was found to be higher than after conservative management of flail chest (p<0.0002) [21,22]. Marasco et al. [11] found no difference in spirometry after 3 months. The number of patients returning to work after 6 months increased significantly after surgical stabilization [4], and their long-term quality of life improved significantly [20].
The most important outcome measure is perhaps mortality, which has also been found to be significantly reduced after surgical stabilization. Several publications have reported a reduction in mortality of up to 33% [4,20,21].
Some articles have mentioned a reduction of total healthcare costs for patients who undergo surgery to treat rib fractures, favouring surgical stabilisation despite the cost of surgery [4,11,22].
Although most of the evidence available regarding rib fixation relates to the treatment of flail chest patients, some articles have only investigated patients with multiple rib fractures. These publications have also identified significant reductions in HLOS, ICU stay, ventilator days, pneumonia, and mortality, and an increase in vital capacity [13,20].
Discussion
Analysing the literature reveals that patients with rib fractures have considerable morbidity and mortality. However, one of the challenges in this analysis is that patients with flail chest and multiple rib fractures are often combined and regarded as one group. This makes interpreting these results difficult, as flail chest patients are obviously more seriously injured, and one would expect the morbidity and mortality rates to be higher in this group. Patients with multiple rib fractures, however, represent a far larger and more interesting group from an economic health perspective.
The available data concerning flail chest patients and surgical fixation is of a higher scientific level than the data on single and multiple rib fractures, as several randomised controlled trials have been published on flail chest patients. Only cohort studies are available for multiple rib fracture patients.
The injury patterns and effects of flail chest were well described even as far back as the early 20th century [10]. The physiological mechanism and effects resulting in pulmonary complications are well understood. Patients with flail chest have paradoxical movements of the flail part of the thorax, which reduces the efficiency of the ventilation in the lung. Less well known is that due to the pressure changes in the thoracic cavity, venous return of blood to the heart is reduced. This in turn has a negative effect on the cardiac output and thus the hemodynamic status of the patient. Apart from injuries of the chest, the prognosis of a flail chest patient is of course also determined by other injuries. These patients have sustained high-impact trauma, which generally results in multiple injuries.
Pulmonary complications are well known. All flail chest patients have some degree of lung contusion, which in combination with reduced movement and pain leads to an elevated risk of contracting pneumonia. The rates in the literature range from 10% and 70%, predominantly between 20% and 40% [3–5,24]. The risk factors for pneumonia are age, the number of rib fractures, and whether pain is persistent.
Apart from pneumonia, mortality is a significant issue with flail chest. Rates as high as 51% have been described [1,4]. Of course, this is not only determined by pulmonary-related problems, but also by the other injuries that a patient sustains. Nonetheless, it is interesting to note that mortality rates are reduced if the rib fractures of flail chest patients receive operative stabilisation [4,20,21].
Several studies have described considerable benefits of the surgical repair of flail chest. Patients treated surgically have shorter ICU stays, less need for ventilator support, reduced pneumonia, reduced HLOS, and reduced mortality.
The highest level of evidence (level 2) has been provided by the randomized studies of Tanaka et al. [4], Granetzny et al. [21], Marasco et al. [11], and Wu et al. [20]. They all describe a beneficial effect of the surgical fixation of flail chest on the length of ICU stay, ventilator support duration, and hospital length of stay with a reduction of 8 days on average. Tanaka et al. [4] and Granetzny et al. [21] describe a reduction in mortality and an average reduction of pneumonia of 46%. A recent Cochrane review was also based on these studies [23]. They conclude that surgical stabilization seems to be beneficial in flail chest patients, but the patient numbers are relatively small and studies do not indicate which flail chest patients to treat operatively and which conservatively.
The English National Institute of Clinical Excellence has decided that operative repair of flail chest injuries can be offered routinely, based on the current level 2 evidence in the literature.
However, not every case of flail chest is the same. It is important to understand the difference between the radiological definition of flail chest as stated above and the clinical definition of flail chest which is: “a chest wall injury with ipsilateral consecutive double broken ribs resulting in paradoxical movement of the chest wall.” A potential problem with a focus on the clinical definition is underestimating lateral and posterior flail chest injuries. These regions of the chest are covered with thick layers of muscle and the scapula, making it virtually impossible to see the paradoxical movement. When operating on posterior flail chest patients it becomes apparent that these lateral and posterior injuries are highly unstable. We therefore propose that the radiological definition be used when identifying patients with flail chest. It is important to understand that this is only possible using computed tomography (CT). A conventional X-ray for rib fractures may underestimate the amount and extent of rib fractures by as much as 50%, as well as missing other relevant intrathoracic injuries [25].
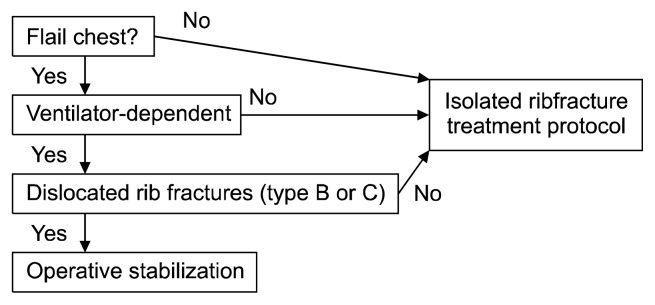
Using the radiological definition in turn poses the risk of identifying too many patients eligible for surgical treatment of flail chest, resulting in over-treatment. The subgroup of patients who need surgical treatment are those with an unstable chest causing pulmonary insufficiency. Identifying these patients can be done by first choosing the patients who clearly exhibit pulmonary insufficiency ( i.e., those who are ventilator-dependent). The next step is to look for radiological evidence of instability, as shown by some form of dislocation of the rib fractures on a CT scan. Dislocation is defined as displacement of 2 mm or more (“in the algorithm, these are referred to as B or C fractures”). These factors are incorporated into the following algorithm for patients with flail chest (Fig. 1).
Fig. 1.
Algorithm for patients with flail chest.
In the above algorithm, patients can be shunted to the isolated rib fracture treatment protocol. The next algorithm for this protocol can be used for patients with rib fractures that have no flail component.
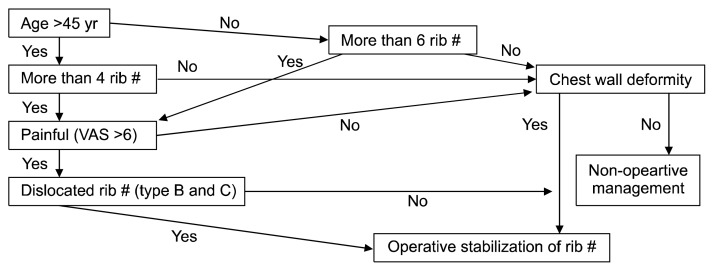
As stated previously, a review of the literature demonstrated a substantially larger number of publications on the flail group compared to the scientific evidence concerning patients with multiple rib fractures. An analysis of the literature regarding the latter group has revealed several factors predictive of the prognosis of a patient. The first factor is age. There is a significant relationship between the age of a patient and the risk of rib fracture complications. Several articles have described the age of 45 years as a threshold between a relatively good prognosis and a poorer prognosis [3,5,16]. The second factor is the number of rib fractures. An exponential relationship has been observed between the number of rib fractures and the risk of complications due to the fractures, pneumonia, mortality, and so on. The third factor is pain, which is often underestimated. A substantial number of rib fracture patients have prolonged pain, defined as a period greater than 6 weeks [18]. Pain itself causes decreased respiratory motion and decreased coughing, putting the patient at risk for developing pneumonia. In general, a visual analogue scale (VAS) score >6 is recognized in the scientific literature as substantial. As the fourth and final factor, the authors have included the amount of dislocation of the rib fractures. A dislocation of 2 mm or more is considered substantial, because such dislocation is similar to that observed in flail chest patients. Dislocated rib fractures imply that there is a degree of instability, which in turn will have an effect on chest movement and pain, putting the patient at risk for pulmonary complications. Combining the above factors results in the following algorithm (Fig. 2).
Fig. 2.
Algorithm for rib fracture management. VAS, visual analogue scale.
In this algorithm, the operative stabilisation of rib fractures only occurs under the following conditions: (1) if a patient is older than 45 years of age and has more than 4 rib fractures that are painful, as shown by a VAS >6 (regardless of adequate painkillers), and has dislocated rib fractures; or (2) if a patient is younger than 45, has more than 6 rib fractures (which poses a risk for pulmonary complications, as described by Bergeron et al. [2] and Flagel et al. [17]) and the rib fractures are painful (VAS >6) and dislocated; or (3) if a patient is younger than 45 and has fewer than 6 rib fractures, but with substantial displacement causing a deformity/impalement. This pathway is also offered for older patients (>45 years) with either a few fractures and a substantial deformity/impalement or low pain level (VAS <6) and a substantial deformity.
In all other cases, non-operative treatment is offered to the patient.
Conclusion
The pathology surrounding patients with rib fractures is substantial. Ten percent of cases of blunt chest trauma have rib fractures. Rib fractures are correlated with significant morbidity and mortality, and both age and the number of rib fractures are key prognostic factors.
Surgical therapy has proven to be beneficial for patients with rib fractures in reducing pulmonary complications. The level of evidence is greater for flail chest patients than for patients with isolated rib fractures. Depending on how aggressive the therapeutic regime is, being >45 years of age and having more than 4 rib fractures can be considered a cut-off point for surgical therapy to be beneficial.
This paper has presented a powerful and easy-to-use clinical tool to assist in deciding between the surgical and conservative treatment of patients with rib fractures.
Footnotes
Conflict of interest
No potential conflicts of interest relevant to this article are reported.
References
- 1.Barnea Y, Kashtan H, Skornick Y, Werbin N. Isolated rib fractures in elderly patients: mortality and morbidity. Can J Surg. 2002;45:43–6. [PMC free article] [PubMed] [Google Scholar]
- 2.Bergeron E, Lavoie A, Clas D, et al. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J Trauma. 2003;54:478–85. doi: 10.1097/01.TA.0000037095.83469.4C. [DOI] [PubMed] [Google Scholar]
- 3.Kent R, Woods W, Bostrom O. Fatality risk and the presence of rib fractures. Ann Adv Automot Med. 2008;52:73–82. [PMC free article] [PubMed] [Google Scholar]
- 4.Tanaka H, Yukioka T, Yamaguti Y, et al. Surgical stabilization of internal pneumatic stabilization?: a prospective randomized study of management of severe flail chest patients. J Trauma. 2002;52:727–32. doi: 10.1097/00005373-200204000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Todd SR, McNally MM, Holcomb JB, et al. A multidisciplinary clinical pathway decreases rib fracture-associated infectious morbidity and mortality in high-risk trauma patients. Am J Surg. 2006;192:806–11. doi: 10.1016/j.amjsurg.2006.08.048. [DOI] [PubMed] [Google Scholar]
- 6.Shorr RM, Rodriguez A, Indeck MC, Crittenden MD, Hartunian S, Cowley RA. Blunt chest trauma in the elderly. J Trauma. 1989;29:234–7. doi: 10.1097/00005373-198902000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Unsworth A, Curtis K, Asha SE. Treatments for blunt chest trauma and their impact on patient outcomes and health service delivery. Scand J Trauma Resusc Emerg Med. 2015;23:17. doi: 10.1186/s13049-015-0091-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones TB, Richardson EP. Traction on the sternum in the treatment of multiple fractured ribs. Surg Gynecol Obstet. 1926;42:283–5. [Google Scholar]
- 9.Jaslow IA. Skeletal traction in the treatment of multiple fractures of the thoracic cage. Am J Surg. 1946;72:753–5. doi: 10.1016/0002-9610(46)90358-3. [DOI] [PubMed] [Google Scholar]
- 10.Bemelman M, Poeze M, Blokhuis TJ, Leenen LP. Historic overview of treatment techniques for rib fractures and flail chest. Eur J Trauma Emerg Surg. 2010;36:407–15. doi: 10.1007/s00068-010-0046-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marasco SF, Davies AR, Cooper J, et al. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg. 2013;216:924–32. doi: 10.1016/j.jamcollsurg.2012.12.024. [DOI] [PubMed] [Google Scholar]
- 12.Bottlang M, Long WB, Phelan D, Fielder D, Madey SM. Surgical stabilization of flail chest injuries with MatrixRIB implants: a prospective observational study. Injury. 2013;44:232–8. doi: 10.1016/j.injury.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 13.Wiese MN, Kawel-Boehm N, Moreno de la Santa P, et al. Functional results after chest wall stabilization with a new screwless fixation device. Eur J Cardiothorac Surg. 2015;47:868–75. doi: 10.1093/ejcts/ezu318. [DOI] [PubMed] [Google Scholar]
- 14.Doben AR, Eriksson EA, Denlinger CE, et al. Surgical rib fixation for flail chest deformity improves liberation from mechanical ventilation. J Crit Care. 2014;29:139–43. doi: 10.1016/j.jcrc.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 15.Wada T, Yasunaga H, Inokuchi R, et al. Effectiveness of surgical rib fixation on prolonged mechanical ventilation in patients with traumatic rib fractures: a propensity score-matched analysis. J Crit Care. 2015;30:1227–31. doi: 10.1016/j.jcrc.2015.07.027. [DOI] [PubMed] [Google Scholar]
- 16.Holcomb JB, McMullin NR, Kozar RA, Lygas MH, Moore FA. Morbidity from rib fractures increases after age 45. J Am Coll Surg. 2003;196:549–55. doi: 10.1016/S1072-7515(02)01894-X. [DOI] [PubMed] [Google Scholar]
- 17.Flagel BT, Luchette FA, Reed RL, et al. Half-a-dozen ribs: the breakpoint for mortality. Surgery. 2005;138:717–23. doi: 10.1016/j.surg.2005.07.022. [DOI] [PubMed] [Google Scholar]
- 18.Fabricant L, Ham B, Mullins R, Mayberry J. Prolonged pain and disability are common after rib fractures. Am J Surg. 2013;205:511–5. doi: 10.1016/j.amjsurg.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 19.Jayle CP, Allain G, Ingrand P, et al. Flail chest in poly-traumatized patients: surgical fixation using Stracos reduces ventilator time and hospital stay. Biomed Res Int. 2015;2015:624723. doi: 10.1155/2015/624723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu WM, Yang Y, Gao ZL, Zhao TC, He WW. Which is better to multiple rib fractures, surgical treatment or conservative treatment? Int J Clin Exp Med. 2015;8:7930–6. [PMC free article] [PubMed] [Google Scholar]
- 21.Granetzny A, Abd El-Aal M, Emam E, Shalaby A, Boseila A. Surgical versus conservative treatment of flail chest: evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg. 2005;4:583–7. doi: 10.1510/icvts.2005.111807. [DOI] [PubMed] [Google Scholar]
- 22.Lardinois D, Krueger T, Dusmet M, Ghisletta N, Gugger M, Ris HB. Pulmonary function testing after operative stabilisation of the chest wall for flail chest. Eur J Cardiothorac Surg. 2001;20:496–501. doi: 10.1016/S1010-7940(01)00818-1. [DOI] [PubMed] [Google Scholar]
- 23.Cataneo AJ, Cataneo DC, de Oliveira FH, Arruda KA, El Dib R, de Oliveira Carvalho PE. Surgical versus nonsurgical interventions for flail chest. Cochrane Database Syst Rev. 2015;(7):CD009919. doi: 10.1002/14651858.CD009919.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sirmali M, Turut H, Topcu S, et al. A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management. Eur J Cardiothorac Surg. 2003;24:133–8. doi: 10.1016/S1010-7940(03)00256-2. [DOI] [PubMed] [Google Scholar]
- 25.Livingston DH, Shogan B, John P, Lavery RF. CT diagnosis of Rib fractures and the prediction of acute respiratory failure. J Trauma. 2008;64:905–11. doi: 10.1097/TA.0b013e3181668ad7. [DOI] [PubMed] [Google Scholar]