Abstract
Disparities in infertility and access to infertility treatments, such as assisted reproductive technology (ART), by race/ethnicity, have been reported. However, identifying disparities in ART usage may have been hampered by missing race/ethnicity information in ART surveillance. We review infertility prevalence and treatment disparities, use recent data to examine ART use in the United States by race/ethnicity and residency in states with mandated insurance coverage for in vitro fertilization (IVF), and discuss approaches for reducing disparities. We used 2014 National ART Surveillance System (NASS) data to calculate rates of ART procedures per million women 15–44 years of age, a proxy measure of ART utilization, for Census-defined racial/ethnic groups in the United States; rates were further stratified by the presence of insurance mandates for IVF treatment. Missing race/ethnicity data (35.6% of cycles) were imputed. Asian/Pacific Islander (A/PI) women had the highest rates of ART utilization at 5883 ART procedures per million women 15–44 years of age in 2014, whereas American Indian/Alaska Native non-Hispanic women had the lowest rates at 807 per million, compared with other racial/ethnic groups. In each racial/ethnic category, ART utilization rates were higher for women in states with an insurance mandate for IVF treatment versus those without. In 2014, A/PI women had the highest rates of ART utilization. ART utilization for all racial/ethnic groups was higher in states with insurance mandates for IVF than those without, although disparities were still evident. Although mandates may increase access to infertility treatments, they are not sufficient to eliminate these disparities.
Keywords: infertility, racial/ethnic disparities, assisted reproductive technology, insurance mandate, in vitro fertilization
Approximately 12% of U.S. women 15–44 years of age have difficulty getting or staying pregnant, and disparities in infertility prevalence and service use by race/ethnicity have been noted.1–3 From 1982 to 2002, infertility, the inability to conceive after 12 months or more of unprotected intercourse, decreased in the United States among white non-Hispanic women, yet increased among black non-Hispanic women.4,5 Furthermore, black non-Hispanic women of reproductive age were 80% more likely to report infertility,3 but 20% less likely to receive infertility services than their white counterparts.6,7 Assisted reproductive technology (ART), procedures where eggs or embryos are handled outside of the body to establish a pregnancy, are costly infertility treatments seldom covered by health insurance and likely subject to disparities in access.8 This commentary reviews racial/ethnic differences in infertility prevalence and treatment, examines recent national ART utilization rates by race/ethnicity and presence of a state insurance mandate for infertility treatment, and discusses potential approaches for reducing disparities.
Racial/ethnic disparities in infertility prevalence have been documented and may be due to disparities in conditions known to cause infertility such as sexually transmitted infections (STIs). For instance, some racial/ethnic minorities report higher rates of STIs (including STIs leading to pelvic inflammatory disease) compared with non-Hispanic whites.5,9–12 Additionally, delays in accessing infertility care have been described for some racial/ethnic groups.11 For example, Asian/Pacific Islander (A/PI) and black non-Hispanic women reported longer durations of infertility4 and accessed ART at a later age compared with white non-Hispanic women.13,14
There are also differences in infertility service use, the highest proportion of use occurring among older, college-educated white non-Hispanic women with incomes >300% above the poverty level.15,16 In 1999–2000, the distribution of ART cycles in the United States varied by race/ethnicity with white non-Hispanic women accounting for 85.5% of cycles, followed by Hispanic (5.5%), black non-Hispanic (4.6%), and A/PI non-Hispanic (4.5%) women.16,17 While data from 2004 to 2006 showed a higher percentage of ART cycles for A/PI women (9.8%) compared with black and Hispanic (both at 6.5%),18 more recent estimates are lacking.
Race/ethnicity is often linked with socioeconomic disparities in healthcare access,19 especially in the United States, where certain racial/ethnic groups may experience residential segregation into neighborhoods with less economic and educational opportunities.20 Conversely, one study found that socioeconomic factors—but not race—were associated with use of fertility treatments, as women with higher levels of income and education spent more money on fertility treatments than those with lower levels.21 ART, the most costly infertility treatment, averages $12,400 per cycle and may require multiple cycles to achieve a live birth.8 With the median U.S. income at $53,657 in 2014,22 ART can impose a financial burden on couples, particularly if health insurance coverage is limited or nonexistent.23,24
Insurance coverage of in vitro fertilization (IVF), a common ART treatment, is associated with higher utilization and improvements in practice and outcomes such as the transfer of fewer embryos and lower percentages of multiple births.24 For instance, the difference in the proportion of women using IVF in the military between black non-Hispanic women and their white non-Hispanic counterparts was lower than the difference between the same two groups in the general U.S. population, suggesting that insurance coverage from the military may reduce disparities in access.16 Additionally, universal insurance coverage mandates requiring all private insurers provide coverage for IVF were found to expand access to IVF treatment, even after accounting for differences in socioeconomic status.25 Currently, 15 states adopted mandates requiring some level of private insurance coverage for infertility services in the United States; however, only 8 states mandate coverage for IVF. The mandates vary, with some states restricting coverage to select infertility diagnoses or ages and some implementing coverage caps.4 Additionally, employers that self-insure are exempt from state mandates and can comprise much of the employed population.
While many studies on treatment utilization focus on the frequency of ART cycles performed, limited national studies of the ART utilization rate by race/ethnicity exist. Furthermore, many of these studies used older data and were limited by the high percentage of missing race/ethnicity values in ART surveillance data.26 Therefore, we used 2014 data from the Centers for Disease Control and Prevention’s (CDC) National ART Surveillance System (NASS) to calculate the number of ART procedures per million women of reproductive age (15–44 years) (a proxy measure of ART utilization based on varying population sizes) for each racial/ethnic category of women. Denominators for these calculations were derived from U.S. Census data.27,28 To address the high proportion (35.6%) of missing information, multiple data imputation was performed for race/ethnicity using SUDAAN’s HOTDECK procedure, under the assumption of missing at random.29 We also calculated ART utilization by race/ethnicity for women living in eight states with mandated insurance coverage for IVF during 2014 (Arkansas, Connecticut, Hawaii, Illinois, Maryland, Massachusetts, New Jersey, and Rhode Island) and for states without such coverage.
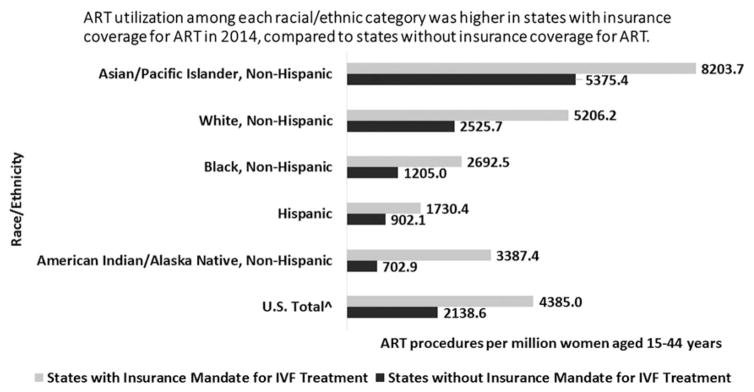
In 2014, A/PI women had the highest number of ART procedures per million women 15–44 years (5883.0) of age followed by white non-Hispanic women (2888.4), whereas black non-Hispanic, Hispanic, and American Indian/Alaska Native non-Hispanic women had lower than the average U.S. ART utilization rates (1434.0, 996.7, 806.8, respectively). ART usage rates were higher in states with insurance coverage mandates for IVF than in states without such mandates, regardless of race/ethnicity (Fig. 1).
FIG. 1.
ART procedures per million women 15–44 years of age by race/ethnicity and presence of insurance coverage mandate for IVF treatment in the United States, 2014. Two or more races not shown. U.S. Census racial/ethnic categories for each state in 2014 among women 15–44 years of age were used to calculate the ART procedures per million women rate. U.S. Territories, banking, research, and oocyte thaw cycles, as well as non-U.S. residents were excluded from the analysis. ^U.S. total of ART procedures does not include missing values. U.S. total number of ART procedures after exclusions = 154,876. ART, assisted reproductive technology; IVF, in vitro fertilization.
Affordability may help explain the higher ART utilization rate among A/PI women. According to 2014 U.S. income data, the A/PI population was the highest earning race/ethnic group with a median income of $74,29722 and had the highest educational attainment compared with other race/ethnic groups.30 Higher incomes may facilitate access to infertility services, and pursuit of higher education may contribute to childbearing later in life when fertility treatments are more likely to be needed.31,32 Additionally, some evidence suggests that A/PI women may be affected by premature ovarian aging at higher rates than white women.33
Although our results suggest that ART utilization was higher in states with IVF mandates regardless of race/ethnicity, in states with a mandate, utilization rates for black non-Hispanic and Hispanic women were still lower than the overall utilization rate for those states, a finding consistent with other studies.34,35 This disparity may be due to out-of-pocket costs such as deductibles and copayments or factors beyond economics that may also provide barriers to care.31,35 For example, certain racial/ethnic groups may delay accessing covered services due to cultural factors such as infertility stigma or fear of disappointing a partner.4,36
The need to address disparities in ART utilization was recognized in the National Public Health Action Plan for the Detection, Prevention, and Management of Infertility; it calls for the provision and monitoring of effective infertility treatment services and/or prevention of conditions leading to infertility disparities.37 Ensuring complete and accurate data collection on race/ethnicity in surveillance systems that monitor infertility and infertility treatments would aid future studies of disparities in risk factors for infertility and access to and utilization of safe and effective treatment.
Approaches to reduce disparities in access to infertility treatment could include provider incentives to practice in lower resource settings, provider education on appropriate and timely referrals to fertility specialists, and patient education about treatment funding options and lower cost care.38,39 The American Society for Reproductive Medicine encourages providers to offer low-cost infertility treatments to reduce disparities in access.38 Furthermore, including infertility diagnosis and evaluation services within health department STI and Title X clinics40 may facilitate earlier diagnosis and infertility care seeking. Evaluation of infertility prevention programs, such as the CDC’s Infertility Prevention Project41 or educational efforts aimed at improving ART outcomes in cities and states,42 may identify effective evidence-based strategies that could help reduce disparities in infertility and its treatment. Additional studies could assess racial/ethnic disparities in cultural and social stigmas surrounding infertility, such as perceived bias from providers, and their impact on ART utilization.18,31,36,43,44 Burdens from the indirect costs of infertility treatment, such as missed work days and transportation to undergo treatments, could also be assessed.
In summary, recent 2014 data showing high ART utilization for A/PI women and lower ART utilization for other minority women point to continued disparities in infertility treatment. While insurance coverage may increase access and address some or all of the cost barriers, strategies that address other cost and noncost factors may be needed to help eliminate utilization disparities. It is important to continue to document, prevent, and reduce racial/ethnic disparities in infertility and access to care.
Footnotes
CDC Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Centers for Disease Control and Prevention, Division of Reproductive Health. [Accessed May 31, 2017];Infertility FAQs. Available at: www.cdc.gov/reproductivehealth/infertility.
- 2.Centers for Disease Control and Prevention, National Center for Health Statistics. [Accessed May 31, 2017];Infertility. Available at: www.cdc.gov/nchs/fastats/infertility.htm.
- 3.Chandra A, Copen C, Stephen EH. Infertility and impaired fecundity in the United States, 1982–2010: Data from the National Survey of Family Growth. Natl Health Stat Rep. 2013;67:16. [PubMed] [Google Scholar]
- 4.Quinn M, Fujimoto V. Racial and ethnic disparities in assisted reproductive technology access and outcomes. Fertil Steril. 2016;105:1119–1123. doi: 10.1016/j.fertnstert.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 5.Stephen EH, Chandra A. Declining estimates of infertility in the United States: 1982–2002. Fertil Steril. 2006;86:516–523. doi: 10.1016/j.fertnstert.2006.02.129. [DOI] [PubMed] [Google Scholar]
- 6.Kissin DM, Boulet SL, Jamieson DJ Assisted Reproductive Technology Surveillance and Research Team. Fertility treatments in the United States: Improving access and outcomes. Obstet Gynecol. 2016;128:387–390. doi: 10.1097/AOG.0000000000001419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chandra A, Copen C, Stephen EH. Infertility service use in the United States: Data from the National Survey of Family Growth, 1982–2010. Natl Health Stat Rep. 2014;73:1–21. [PubMed] [Google Scholar]
- 8.Resolve. The National Infertility Association. [Accessed May 31, 2017];The Costs of Infertility Treatment. Available at: www.resolve.org/family-building-options/making-treatment-affordable/the-costs-of-infertility-treatment.html.
- 9.Centers for Disease Control and Prevention. [Accessed May 31, 2017];2015 Sexually Transmitted Diseases Surveillance: STDs in Racial and Ethnic Minorities. 2015 Available at: https://www.cdc.gov/std/stats15/minorities.htm.
- 10.Sutton MY, Sternberg M, Zaidi A, St Louis ME, Markowitz LE. Trends in pelvic inflammatory disease hospital discharges and ambulatory visits, United States, 1985–2001. Sex Transm Dis. 2005;32:778–784. doi: 10.1097/01.olq.0000175375.60973.cb. [DOI] [PubMed] [Google Scholar]
- 11.Huddleston HG, Cedars MI, Sohn SH, Giudice LC, Fujimoto VY. Racial and ethnic disparities in reproductive endocrinology and infertility. Am J Obstet Gynecol. 2010;202:413–419. doi: 10.1016/j.ajog.2009.12.020. [DOI] [PubMed] [Google Scholar]
- 12.Kreisel K, Torrone E, Bernstein K, Hong J, Gorwitz R. Prevalence of pelvic inflammatory disease in sexually experienced women of reproductive age—United States, 2013–2014. MMWR Morb Mortal Wkly Rep. 2017;66:80–83. doi: 10.15585/mmwr.mm6603a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seifer DB, Frazier LM, Grainger DA. Disparity in assisted reproductive technologies outcomes in black women compared with white women. Fertil Steril. 2008;90:1701–1710. doi: 10.1016/j.fertnstert.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 14.Purcell K, Schembri M, Frazier LM, et al. Asian ethnicity is associated with reduced pregnancy outcomes after assisted reproductive technology. Fertil Steril. 2007;87:297–302. doi: 10.1016/j.fertnstert.2006.06.031. [DOI] [PubMed] [Google Scholar]
- 15.Chandra A, Stephen EH. Impaired fecundity in the United States: 1982–1995. Fam Plann Perspect. 1998;30:34–42. [PubMed] [Google Scholar]
- 16.Feinberg EC, Larsen FW, Catherino WH, Zhang J, Armstrong AY. Comparison of assisted reproductive technology utilization and outcomes between Caucasian and African American patients in an equal-access-to-care setting. Fertil Steril. 2006;85:888–894. doi: 10.1016/j.fertnstert.2005.10.028. [DOI] [PubMed] [Google Scholar]
- 17.Grainger DA, Seifer DB, Frazier LM, Rall MJ, Tjaden BL, Merrill JC. Racial disparity in clinical outcomes from women using advanced reproductive technologies (ART): Analysis of 80,196 ART cycles from the SART database 1999 and 2000. Fertil Steril. 2004;82(Suppl 2):S37–S38. [Google Scholar]
- 18.Fujimoto VY, Luke B, Brown MB, et al. Racial and ethnic disparities in assisted reproductive technology outcomes in the United States. Fertil Steril. 2010;93:382–390. doi: 10.1016/j.fertnstert.2008.10.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. CDC health disparities and inequalities report—United States, 2013. Morb Mortal Wkly Rep. 2013;62:7–32. [Google Scholar]
- 20.U.S. Department of Health and Human Services, Office of Disease Prevention & Health Promotion. [Accessed May 31, 2017];Healthy people 2020: An opportunity to address societal determinants of health in the United States. 2010 Available at: www.healthypeople.gov/2010/hp2020/advisory/SocietalDeterminantsHealth.htm.
- 21.Smith JF, Eisenberg ML, Glidden D, et al. Socioeconomic disparities in the use and success of fertility treatments: Analysis of data from a prospective cohort in the United States. Fertil Steril. 2011;96:95–101. doi: 10.1016/j.fertnstert.2011.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DeNavas-Walt C, Proctor BD. U.S. Census Bureau CPR, editor. Income and poverty in the United States: 2014. Washington, DC: U.S. Government Printing Office; 2015. pp. P60–P252. [Google Scholar]
- 23.Chambers GM, Hoang VP, Sullivan EA, et al. The impact of consumer affordability on access to assisted reproductive technologies and embryo transfer practices: An international analysis. Fertil Steril. 2014;101:191–198. e194. doi: 10.1016/j.fertnstert.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 24.Boulet SL, Crawford S, Zhang Y, et al. Embryo transfer practices and perinatal outcomes by insurance mandate status. Fertil Steril. 2015;104:403–409. e401. doi: 10.1016/j.fertnstert.2015.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hamilton BH, McManus B. The effects of insurance mandates on choices and outcomes in infertility treatment markets. Health Econ. 2012;21:994–1016. doi: 10.1002/hec.1776. [DOI] [PubMed] [Google Scholar]
- 26.Wellons MF, Fujimoto VY, Baker VL, et al. Race matters: A systematic review of racial/ethnic disparity in Society for Assisted Reproductive Technology reported outcomes. Fertil Steril. 2012;98:406–409. doi: 10.1016/j.fertnstert.2012.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.U.S. Census Bureau Population Division. [Accessed May 31, 2017];Annual estimates of the resident population by sex, age, race, and Hispanic origin for the United States and states: April 1, 2010 to July 1, 2014 2015. Available at: http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=PEP_2014_PEPASR6H&prodType=table.
- 28.U.S. Census Bureau Population Division. [Accessed May 31, 2017];Annual estimates of the resident population for selected age groups by sex for the United States, states, counties, and Puerto Rico commonwealth and municipios: April 1, 2010 to July 1, 2014. Available at: http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk.
- 29.Pedersen AB, Mikkelsen EM, Cronin-Fenton D, et al. Missing data and multiple imputation in clinical epidemiological research. Clin Epidemiol. 2017;9:157–166. doi: 10.2147/CLEP.S129785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ryan C, Bauman K. Educational attainment in the United States: 2015. [Accessed May 31, 2017];US Census Bureau Current Population Reports. 2016 Available at: https://www.census.gov/content/dam/Census/library/publications/2016/demo/p20-578.pdf.
- 31.Jain T. Socioeconomic and racial disparities among infertility patients seeking care. Fertil Steril. 2006;85:876–881. doi: 10.1016/j.fertnstert.2005.07.1338. [DOI] [PubMed] [Google Scholar]
- 32.The European Society of Human Reproduction and Embrology (ESHRE) Capri Workshop Group. Social determinants of human reproduction. Hum Reprod. 2001;16:1518–1526. [Google Scholar]
- 33.Gleicher N, Weghofer A, Li J, Barad D. Differences in ovarian function parameters between Chinese and Caucasian oocyte donors: Do they offer an explanation for lower IVF pregnancy rates in Chinese women? Hum Reprod. 2007;22:2879–2882. doi: 10.1093/humrep/dem289. [DOI] [PubMed] [Google Scholar]
- 34.Seifer DB, Zackula R, Grainger DA a Society for Assisted Reproductive Technology Writing Group. Report: Trends of racial disparities in assisted reproductive technology outcomes in black women compared with white women: Society for Assisted Reproductive Technology 1999 and 2000 vs. 2004–2006. Fertil Steril. 2010;93:626–635. doi: 10.1016/j.fertnstert.2009.02.084. [DOI] [PubMed] [Google Scholar]
- 35.Feinberg EC, Larsen FW, Wah RM, Alvero RJ, Armstrong AY. Economics may not explain Hispanic underutilization of assisted reproductive technology services. Fertil Steril. 2007;88:1439–1441. doi: 10.1016/j.fertnstert.2007.01.031. [DOI] [PubMed] [Google Scholar]
- 36.Missmer SA, Seifer DB, Jain T. Cultural factors contributing to health care disparities among patients with infertility in Midwestern United States. Fertil Steril. 2011;95:1943–1949. doi: 10.1016/j.fertnstert.2011.02.039. [DOI] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention. National public health action plan for the detection, prevention, and management of infertility. Atlanta, Georgia: Department of Health and Human Services; 2014. [Google Scholar]
- 38.Ethics Committee of the American Society for Reproductive Medicine. Disparities in access to effective treatment for infertility in the United States: An ethics committee opinion. Fertil Steril. 2015;104:1104–1110. doi: 10.1016/j.fertnstert.2015.07.1139. [DOI] [PubMed] [Google Scholar]
- 39.Letourneau JM, Smith JF, Ebbel EE, et al. Racial, socioeconomic, and demographic disparities in access to fertility preservation in young women diagnosed with cancer. Cancer. 2012;118:4579–4588. doi: 10.1002/cncr.26649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gavin L, Moskosky S, Carter M, et al. Providing quality family planning services: Recommendation of CDC and the U.S. Office of Population Affairs. Morb Mortal Wkly Rep. 2014;63:1–54. [Google Scholar]
- 41.Centers for Disease Control and Prevention. [Accessed May 31, 2017];Infertilty prevention project (IPP) Available at: www.cdc.gov/std/infertility/ipp-archive.htm.
- 42.Association of State and Territorial Health Organizations (ASTHO) [Accessed May 31, 2017];The role of state public health agencies in improving assisted reproductive technology. 2016 Available at: www.astho.org/Programs/Maternal-and-Child-Health/Documents/The-Role-of-State-Public-Health-Agencies-in-Improving-Assisted-Reproductive-Technology.
- 43.Bharadwaj A. Why adoption is not an option in India: The visibility of infertility, the secrecy of donor insemination, and other cultural complexities. Soc Sci Med. 2003;56:1867–1880. doi: 10.1016/s0277-9536(02)00210-1. [DOI] [PubMed] [Google Scholar]
- 44.Jain T, Hornstein MD. Disparities in access to infertility services in a state with mandated insurance coverage. Fertil Steril. 2005;84:221–223. doi: 10.1016/j.fertnstert.2005.01.118. [DOI] [PubMed] [Google Scholar]