Abstract
Introduction
The previous studies have not reached on consensus as to the outcome of acetabular reconstruction with autogenous bone graft for dysplastic hips, especially in severe cases such as Crowe type IV. The current study aimed to determine the survivorship of the arthroplasty and the grafts as well as the change of hip joint center averagely 9.8 years (range, 5–19) after cementless total hip arthroplasty.
Materials and methods
We reviewed 52 cases including 19 cases of complete hip dislocation of which acetabular defects were augmented with autogenous bone grafts taken from the resected femoral heads. For radiographic evaluation, in addition to checking failures of THA, acetabular coverages of the grafts as well as lateral center-edge angles were measured and compared between two time points, immediately postoperative and the final evaluations. Those outcomes were also analyzed according to the degree of hip dysplasia, grouping the subjects by Crowe classification. Translations of the reconstructed hip joint center after THA were measured and checked if they affected clinical outcomes or caused any complications. To assess clinically, Harris hip score and visualized analogue pain scale were reviewed.
Results
Mean coverage ratio of the sockets with the grafts was 28.4% immediately after the surgery (range, 11.1%–65.0%) and 27.2% at the final follow-up (range, 11.1%–63.6%). When comparing high grade dysplasia (Crowe type III, IV) to low grade dysplasia (Crowe type I, II), there was no significant difference of the above outcomes (p = 0.476). As to the location of hip joint center, 14 outliers were located distally within the normal horizontal range especially in cases with Crowe type IV. Those outliers showed no difference on clinical outcome. The mean HHS was 52.2 (range, 19–87) and VAS was 7.2 (range, 5–9) preoperatively, each of which was improved to 92.9 (range, 63–100) and 1.4 (range, 0–4) postoperatively. No failures were experienced during the study period.
Conclusions
Acetabular augmentation using autogenous bone graft from the resected femoral head is found to be a successful method for dysplastic hip, even in severe cases such as Crowe type IV, showing favorable results in more than 8 years. When inevitable, a degree of compromise on hip joint center can be needed in dealing with severe hip dysplasia.
Keywords: Acetabulum, Hip dysplasia, Bone grafting, Total hip replacement
1. Introduction
Longevity becomes an issue especially when total hip arthroplasty (THA) is applied in dysplastic hip, since destruction of the joint frequently occurs in relatively early ages of the patients. At the same time, the more severe dysplasia of hip should we cope with, the more difficulty follows in obtaining the prosthetic stability that is necessary to long-term survivorship.1, 2 When it comes to complete dislocation, also referred to as Crowe type IV, some authors even denied it to be indication of THA.3, 4, 5 To date, various methods have been introduced to overcome high grade dysplasia,6, 7, 8, 9, 10, 11, 12, 13, 14, 15 which can be categorized according to whether they retain anatomic hip joint center or not.
Surgeons prefer to avoid non-anatomic hip joint center whenever possible because disadvantages following it have been well known from leg length discrepancy, dislocation, or impingement to early loosening.9, 16, 17 However, enough bony coverage should be guaranteed to obtain anatomic hip center, which necessitate bone graft. When grafted bone is incorporated, which reportedly takes from 16 months to 32 months,18, 19 resorption of it could compromise stability of the acetabular cup.10, 20 In this context, various reports about acetabular reconstruction in the dysplastic hip joint using bone graft have not reached consensus on the survivorship of THA. Several favorable short to mid-term results2, 12, 17, 21, 22, 23 as well as inconsistent long-term results were reported.24, 25, 26, 27, 28, 29, 30, 31 There are some variables regarding THA techniques in hip dysplasia, which makes direct comparison among the previous reports complicate. Moreover, different severities of acetabular dysplasia as well as demographics of each study group add more difficulty in drawing conclusions. As Delimar recently figured out in their study,32 autografts have superiority in terms of graft survival to allografts. Considering that in cases of dysplastic hip joints, unlike in revisional THA, femoral heads can be sources of bone grafts needed for the acetabular reconstruction, the techniques recently supported by Kim24 and Tsukada17 using bulk femoral head autografts seem to be a reasonable option. However, the subjects of their studies with a small number of high grade of hip dysplasia still leave a question that same favorable results could be achieved even in Crowe IV. In this study, we tried to figure out (1) reliability of the acetabular reconstruction technique using autogenous bone graft in high grade hip dysplasia, (2) influence of Crowe type on outcomes, and (3) acceptable range of reconstructed hip joint center that does not affect clinical results.
2. Materials and methods
We reviewed the patients who underwent total hip arthroplasties for hip dysplasia using autogenous bone grafts in acetabular reconstruction between 1995 and 2009. Patients with less than 5 years of follow-up or pathology of hip joint other than acetabular dysplasia were excluded. Thus, total 47 patients, consisting of 5 males and 42 females, including 5 bilateral cases met the criteria for inclusion. The subject had a mean age of 49.6 years old (Table 1). They were grouped according to Crowe classification,2 5 cases corresponding to grade I, and 20, 8, 19 cases to grade II, III, IV respectively, and then were evaluated on both clinical and radiographic outcomes. Demographic data and clinical outcomes were obtained by reviewing the electronic medical records, and serial radiographs of each patient were analyzed.
Table 1.
Demographic characteristics.
| Characteristic | Value |
|---|---|
| Number of hips | 52 |
| Bilaterality | 5 |
| Follow-up duration (years)* | 9.83 (5–19) |
| Age (years)* | 49.6 (19–76) |
| Sex (F/M) | (47/5) |
| Crowe type (cases) | |
|---|---|
| I | 5 |
| II | 20 |
| III | 8 |
| IV | 19 |
Values are expressed as means, with ranges in parentheses.
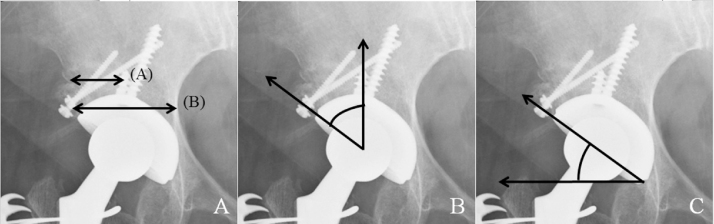
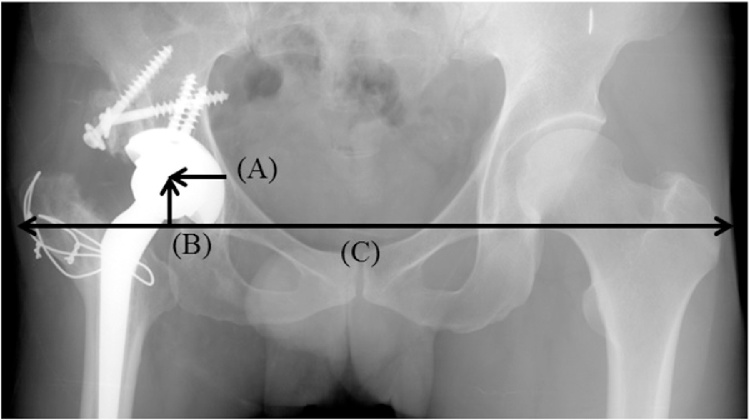
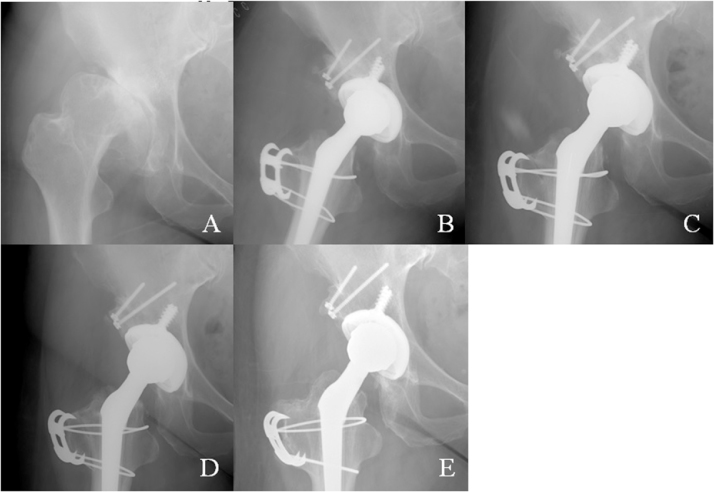
For radiographic evaluation, coverage by the graft on the socket was measured on anteroposterior pelvis plain radiograph and calibrated with the known socket diameter, being converted into the coverage ratio to compensate variable magnitudes of radiographic images (Fig. 1A). For another evaluation for the coverage, lateral center-edge (CE) angle was measured just after the surgery and at the final evaluation (Fig. 1B). We did not apply the coverage ratio or lateral CE angle preoperatively because they cannot reflect the severity of hip dysplasia arithmetically when both parameters are influenced by the location of the femoral head, for which some Crowe III cases could look worse on those parameters than Crowe IV cases. Positions of the acetabular sockets were expressed on 2 dimensions in the way introduced by Russotti33 (Fig. 2). For each case with translation of the hip joint center out of normal range, Crowe classification and possible complications were checked. The inclinations of the sockets (Fig. 1C) as well as any sign of loosening were looked into on serial plain radiographs. Radiographic changes of the grafts were also staged with the method introduced by Knight et al.19 (Fig. 3). The changes have three steps: (1) trabecular bridging, in which appeared the trabecular formation between the graft-host interface; (2) remodeling, in which disappeared the graft-host interface with change in graft density representing revascularization; (3) reorientation, in which the trabecular pattern of the graft was reformed as the acetabular dome.
Fig. 1.
(A) Coverage ratio: (the graft coverage A/the length of the acetabular cup B) × 100%, (B) Lateral center-edge angle and (C) Inclination of the acetabular cup.
Fig. 2.
Position of the acetabular socket, A: Horizontal location, B: Vertical location, C: Inter-teardrop line.
Fig. 3.
Radiographic changes of the bone graft applied in the case of a 61-year-old woman with Crowe type III hip dysplasia (A) Preoperative image, (B) immediately postoperative image, (C) 3 months after THA, showing trabecular bridging at the graft-host interface, (D) 1 years after THA, showing remodeling with blurring of the interface line and change in graft density, (E) 2 years after THA, showing reorientation with the same trabecular pattern of the graft as the acetabular dome.
For clinical evaluation, Visual analogue scale (VAS) and Harris hip score (HHS) were assessed both preoperatively and postoperatively, and compared between low grade dysplasia (Crowe I, II) and high grade dysplasia (Crowe type III, IV). Any postoperative complications or clinical symptoms related to failure of the arthroplasty were reviewed thoroughly on medical records.
Paired t-test was used in analyzing the outcomes over time progression, comparing preoperative or immediate postoperative results to those of the final follow-up. In analyzing according to Crowe classification, independent t-test was used, comparing between low grade dysplasia (Crowe I, II) and high grade dysplasia (Crowe type III, IV). Level of significance was set at p < 0.05.
2.1. Surgical technique
Posterolateral approach was used to get to the acetabulum and trochanteric osteotomy was applied unless enough operative field was secured. To achieve as much coverage as possible, acetabular cup was medialized within the extent not to penetrate the medial wall of pelvis, or ilioischial line on anteroposterior pelvis radiograph. Fitmore cups (47 cases, Zimmer, Warsaw, IN, USA) and Conical stems (46 cases, Zimmer, Warsaw, IN, USA) were the most commonly used prosthesis and Trilogy cups (5 cases, Zimmer, Warsaw, IN, USA) and CLS stems (6 cases Zimmer, Warsaw, IN, USA) were occasionally used in cases of severe dysplasia or high offset.
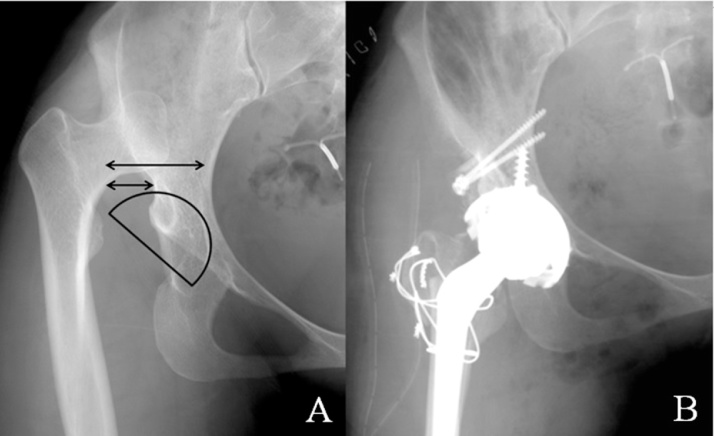
Autogenous bone grafts taken from the resected femoral heads were applied in the same manner introduced by former authors.17, 31, 34, 35 3.5 mm screws were usually applied to fix the grafts, after which initial secure fixation was considered as the basic principle. At the same time, we tried not to exceed the graft coverage more than 30–40% of the socket suggested by previous literatures.11, 20, 24, 27, 32 In dealing with severely dysplastic acetabulum such as Crowe type IV, we inevitably translated the hip joint center as shown in Fig. 4. In these cases, soft tissue tension and range of motion without impingement were checked intraoperatively. When neglected dislocation of the hip joint was too stiff to get reduction only with soft tissue release, femoral shortening was considered (Fig. 5). The shortening was made minimally to get reduction so that risk of leg length discrepancy was minimized.
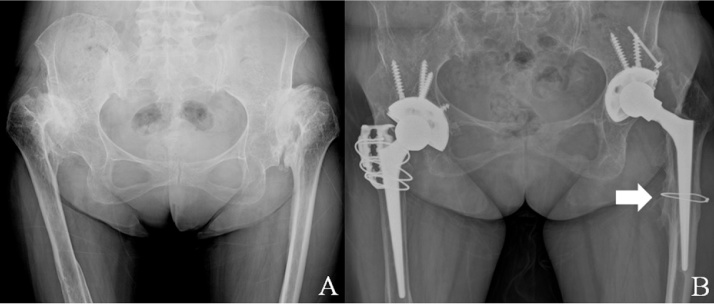
Fig. 4.
Preoperative and postoperative images of the case of a 39-year-old woman with Crowe type IV (A) when applying the same sized socket as actually done in THA, but at the routine hip joint center, the coverage ratio would be nearly 50%. (B) with the lower hip joint center than normal range, 12.5 mm from the inter-teardrop line for vertical location and 21.5 mm for horizontal location, the coverage ratio was measured to be 31%.
Fig. 5.
Preoperative and postoperative images of the case of a 40-year-old woman with neglected hip dislocations bilaterally (A) Neglected dislocations caused pain, which necessitated the surgical treatment. (B) Image taken at the final exam 7 years after THA, from difficulty to get reduction, 2 cm femoral shortening was made during the left side THA, after which 1 cm femoral shortening was made on the right side considering both reduction and leg length discrepancy. The arrow indicates cerclage wire for additional fixation after the shortening. Trochanteric osteotomy was applied on the right side.
Hip motion including sitting position was allowed just after the operation and tolerable weight bearing was granted in 2 days postoperatively. Meanwhile, crutches were recommended for all patients until postoperative 3 months. Regular follow-up was made at 6 weeks, 3 months, 6 months after the operation, thereafter annual follow-up was made. Simple radiographs including anteroposterior and translateral images were gained at each follow-up.
3. Results
The mean period of follow-up was 9.8 years postoperatively (range, 5–19 years) with 25 cases of more than 10 years of follow-up. During that period, there were no cases of revision due to any causes, nor complications such as dislocation, osteolysis or loosening. Neither loosening of the sockets nor broken screws were detected on plain radiographs taken at the final follow-up. All cases, including 19 cases with complete dislocation (Crowe type IV), were able to be reducted into the true acetabulums, for which 1 patient with bilateral neglected dislocations needed to have femoral shortening by 2 cm and 1 cm respectively (Fig. 5).
3.1. Radiographic outcomes
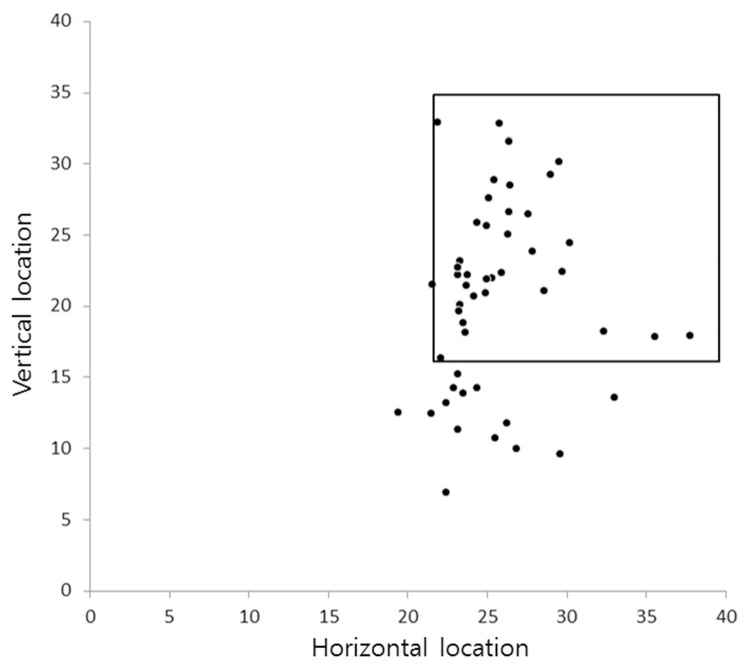
Mean coverage ratio of the sockets with the grafts was 28.4% immediately after the surgery (range, 11.1%–65.0%) and 27.2% at the final follow-up (range, 11.1%–63.6%) (Table 2). In terms of Crowe classification, there was no significant influence of the grade of hip dysplasia on the coverage ratio at immediately postoperative (p = 0.150) and the final follow-up (p = 0.476) (Table 3). Lateral CE angle was showed to be improved to 40.0° (range, 23°–55°) on radiographs taken just after the surgery and was checked to be 39.0° (range, 23°–55°) at the final evaluation (Table 2). There was no significant difference of postoperative CE angle between the groups of Crowe type I, II and Crowe type III, IV immediately postoperative (p = 0.931) and the final evaluation (p = 0.617) (Table 3). Mean inclination of the acetabular cups was 45.9° (range, 39°–61°) for low grade dysplasia group (Crowe type I, II) and 48.8° (range, 40°–60°) for high grade dysplasia group (Crowe type III, IV), showing no statistically significant difference (p = 0.051) (Table 3). There was no significant change of inclination over time progression (p = 0.322) (Table 2). As to the location of hip joint center, there were 14 outliers consisting of 3 cases with Crowe type II and 11 cases with Crowe type IV (Fig. 6). Most outliers were only outside the vertical normal range of THA rotation center but not outside the horizontal range. Time taken to show radiographic changes staged by the method of Knight et al. was found to be similar to that reported by Kim et al.24
Table 2.
Radiographic results.
| Parameter | Value | P value |
|---|---|---|
| Coverage ratio (%) | ||
| Immediate postoperation | 28.4 (11.1–65.0) | |
| Final evaluation | 27.2 (11.1–63.6) | P = 0.001 |
| Lateral CE angle (°) | ||
| Immediate postoperation | 40.0 (23–55) | |
| Final evaluation | 39.0 (23–55) | P = 0.000 |
| Inclination of socket (°) | ||
| Immediate postoperation | 47.4 (39–61) | |
| Final evaluation | 47.5 (39–61) | P = 0.322 |
| Hip joint center (mm) | ||
| Vertical location | 20.5 (6.9–33.0) | |
| Horizontal location | 25.9 (19.4–37.1) | |
| Radiographic change (months)* | ||
| Trabecular bridging | 3.6 (2–6) | |
| Remodeling | 7.7 (4–14) | |
| Reorientation | 17.1 (13–24) | |
| Loosening of socket | none | |
| Breakage of screw | none | |
All values are expressed as means, with range in parentheses.
Staging of the radiographic change was based on the method of Knight et al.
Table 3.
Radiographic outcomes according to Crowe classification.
| Crowe type I, II | Crowe type III, IV | P value | |
|---|---|---|---|
| Number of hips | 25 | 27 | |
| Follow-up duration (years) | 7.85 (2–19) | 8.87 (2–16) | P = 0.381 |
| Age (years) | 52.8 (23–72) | 46.1 (19–76) | P = 0.042* |
| Revision case | none | none | |
| Coverage ratio (%) | |||
| Immediate postop. | 25.4 (11.3–65.0) | 31.2 (11.1–64.3) | P = 0.150 |
| Final evaluation | 24.3 (11.3–62.5) | 29.8 (11.1–63.6) | P = 0.476 |
| Lateral CE angle (°) | |||
| Immediate postop. | 40.8 (23–55) | 41.0 (25–55) | P = 0.931 |
| Final evaluation | 38.4 (23–55) | 39.6 (23–54) | P = 0.617 |
| Inclination of socket (°) | |||
| Immediate postop. | 45.9 (39–61) | 48.8 (40–60) | P = 0.051 |
| Final evaluation | 46.0 (39–61) | 48.8 (40–60) | P = 0.085 |
All results are expressed as means, with ranges in parentheses; there were no significant differences but * value.
Fig. 6.
Location of hip joint center is expressed on a graph in the same way as that of Kim et al.24 and Russotti et al.33 with the quadrangle representing the normal range of hip center of THA. The outliers tended to have lower vertical locations within normal horizontal range.
3.2. Clinical outcomes
HHS was 52.2 (range, 19–87) on average preoperatively, which was improved to 92.9 (range, 63–100) at the final follow-up. VAS was improved from 7.2 (range, 5–9) preoperatively to 1.4 (range, 0–4) postoperatively (Table 4). When comparing those figures between low grade dysplasia group (Crowe type I, II) and high grade dysplasia group (Crowe type III, IV), there was no difference in the postoperative states, showing consistent improvements (Table 5). There were no complaints of leg length discrepancy or dislocation.
Table 4.
Clinical results.
| Parameter | Value | P value |
|---|---|---|
| HHS | ||
| Preoperative | 52.2 (19–87) | |
| Postoperativeb | 92.9 (63–100) | P = 0.000 |
| VAS | ||
| Preoperative | 7.2 (5–9) | |
| Postoperativeb | 1.4 (0–4) | P = 0.000 |
| Complaint of LLDa | none | |
All values are expressed as means, with range in parentheses.
LLD = leg length discrepancy.
Values were at the final evaluation.
Table 5.
Clinical outcomes according to Crowe classification.
| Crowe type I, II | Crowe type III, IV | P value | |
|---|---|---|---|
| HHS | |||
| Preoperative | 57.6 (32–75) | 47.1 (19–87) | P = 0.014* |
| Postoperative† | 93.3 (65–100) | 92.5 (63–100) | P = 0.608 |
| VAS | |||
| Preoperative | 7.0 (5–9) | 7.4 (5–9) | P = 0.065 |
| Postoperative† | 1.3 (0–4) | 1.5 (0–4) | P = 0.433 |
All results are expressed as means, with ranges in parentheses; there were no significant differences but * value; † values were at the final evaluation.
4. Discussion
Augmentation of acetabular defect with bone graft in dysplastic hip allows enough coverage of the socket and anatomical positioning of the prosthetic joint, preventing too much high or medial hip center. In that case, retaining of the bone graft is one of the most significant prerequisite in long-term survivorship of the arthroplasty. As noted by Harris WH,20 success in shot to mid-term results do not guarantee longevity of the arthroplasty. For this, some authors regarded the graft resorption as a reason not to choose allogenous or autogenous bone for the augmentation material.3, 4, 5 Several reports with favorable mid to long-term results, however, were limited by their small number of subjects,36 or did not include enough severe dysplastic cases17, 24, 25, 28, 29, 34 to come into conclusions.
There have been several studies on factors that affect the graft resorption. First of all, allogenous bone was proved inferior to autogenous graft showing significantly more extensive resorption. Delimar et al. reported that allogenous bones were resorbed twice as fast as autogenous grafts.32 Thus, there seems to be no controversies to use autografts which can easily be obtained from the resected femoral head in THA for hip dysplasia. As to the extent of bone graft coverage, Shinar et al. recommended that graft should not exceed more than 30% of the entire socket for favorable result,11, 32 supported by similar results from other studies.20, 24, 27 A number of studies successfully applied bone grafts more than 30% of the socket coverage, but they did not mention the severity of hip dysplasia17 or only covered small proportion of Crowe IV cases.24 When it comes to cemented THA, contradictory results have been reported. Akiyama showed excellent long-term results of 96% survival at 15 years,31 attributing their success to improved surgical techniques. On the other hand, Delimar32 and Zahar37 reported multiple early or late failures, warning the use of bone grafts. Those discrepancies may be because of that cement use in THA is less reproducible than cementless THA and vulnerable to various factors. Making the future revision harder is another reason for surgeons to choose it especially when secondary osteoarthritis due to hip dysplasia needs THA in earlier age than other causes. Klapach et al. tried using cement instead of bone graft for the augmentation, reporting favorable survivorship.38 This has yet to be acknowledged as standard procedure.
In the current study, we experienced no failure out of 52 cases hip dysplasia about half of which were high grade dysplasia (Crowe type III, IV, 27 cases). Similar principles recommended by Kim24 including secure fixation of the grafts, press-fitting of the acetabular sockets, and use of the porous surfaced sockets were also applied in our cases. At the same time, to deal with high grade dysplasia especially Crowe IV cases, we accept some amount of changes in hip center not to exceed the extent of graft coverage more than suggested by the previous literatures.11, 20, 24, 27, 32 Russotti et al. reported that proximal hip joint center within normal range of vertical location could be clinically acceptable.33 Considering outliers of the current study tended to be within the normal vertical range, similar assumption can be made on distally located hip joint center. However, we could not suggest the landmarks or generally applicable principles on this, because morphology of pelvic wall was inconsistent particularly in cases of Crowe type IV. Preoperative templating in addition to intraoperative decision making should be remarked in dealing with severe hip dysplasia. In spite of the compromise of hip joint center, we had 2 cases with Crowe type II and 4 cases with Crowe type IV that showed the coverage ratio more than 50%. We did not find any difference of results in those 6 cases.
The current study has several limitations. Firstly, the nature of retrospective design is weakness, although it has as similar level of evidence as the previous studies. Secondly, the follow-up period may be not enough to determine survivorship of the arthroplasty. According to the study by Zahar,37 failure could increase even after 15 years postoperatively. Apart from that THA is not accepted as the permanent procedure yet, such disadvantageous circumstance as the defective acetabulum might well aggravate longevity of THA. Possible factors that could affect the survivorship include the graft incorporation, surgical techniques and use of cement, which makes all the differences among the results about the longevity of THA in hip dysplasia. Persistent observation of the study group should follow to determine our accurate survivorship. We focused on the change of the coverage ratio, considering major resorption of graft reportedly represented as trabecular reorientation on radiograph is showed to occur 2 or 3 years after the operation.18, 19 The results showed no significant difference between low and high grade dysplasia groups. Another problem of this study lied in that radiographic figures were only measured on 2 dimensions. However, we took the similar way most previous studies applied, which can make it easy to compare our results with others. Distinguishing radiographic changes of the grafts on plain radiographs was also complicate so that other observers, especially radiologists, could be helpful to get robust results. Anyhow, our results were similar to those of Kim et al.24 Lastly, we cannot give the exact guidelines or landmarks as to the acceptable extent of translation of hip joint center, because we did not experience complications that could originate from the translation. The compromise on THA rotation center was inevitably made to satisfy both the principle not to exceed the graft coverage more than recommended by many authors and to get the initial secure fixation of the sockets. We only made conclusions on possible acceptable range of hip center without complications. We also assumed that other variables like soft tissue tension or intraoperative range of motion also take important part in deciding the hip center. We gave up the anatomic center only when there were no other options and did not alter inclination or version of the cup for the coverage.
Acetabular augmentation with autogenous bone graft from the resected femoral head showed favorable outcomes in averagely 9.8 years follow-up. When inevitable, a degree of compromise on hip joint center can be needed in dealing with severe hip dysplasia.
References
- 1.Argenson J.N., Flecher X., Parratte S., Aubaniac J.M. Anatomy of the dysplastic hip and consequences for total hip arthroplasty. Clin Orthop Related Res. 2007;465:40–45. doi: 10.1097/BLO.0b013e3181576052. [DOI] [PubMed] [Google Scholar]
- 2.Crowe J.F., Mani V.J., Ranawat C.S. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg. Am Vol. 1979;61(1):15–23. [PubMed] [Google Scholar]
- 3.Charnley J., Feagin J.A. Low-friction arthroplasty in congenital subluxation of the hip. Clin Orthop Related Res. 1973;(91):98–113. doi: 10.1097/00003086-197303000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Anwar M.M., Sugano N., Masuhara K., Kadowaki T., Takaoka K., Ono K. Total hip arthroplasty in the neglected congenital dislocation of the hip. A five- to 14-year follow-up study. Clin Orthop Related Res. 1993;295:127–134. [PubMed] [Google Scholar]
- 5.Cameron H.U., Botsford D.J., Park Y.S. Influence of the Crowe rating on the outcome of total hip arthroplasty in congenital hip dysplasia. J Arthroplasty. 1996;11(5):582–587. doi: 10.1016/s0883-5403(96)80113-6. [DOI] [PubMed] [Google Scholar]
- 6.Kaneuji A., Sugimori T., Ichiseki T., Yamada K., Fukui K., Matsumoto T. Minimum ten-year results of a porous acetabular component for Crowe I to III hip dysplasia using an elevated hip center. J Arthroplasty. 2009;24(2):187–194. doi: 10.1016/j.arth.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Dorr L.D., Tawakkol S., Moorthy M., Long W., Wan Z. Medial protrusio technique for placement of a porous-coated, hemispherical acetabular component without cement in a total hip arthroplasty in patients who have acetabular dysplasia. J Bone Joint Surgery. Am Vol. 1999;81(1):83–92. doi: 10.2106/00004623-199901000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Hartofilakidis G., Stamos K., Karachalios T., Ioannidis T.T., Zacharakis N. Congenital hip disease in adults. Classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg. Am Vol. 1996;78(5):683–692. doi: 10.2106/00004623-199605000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Pagnano W., Hanssen A.D., Lewallen D.G., Shaughnessy W.J. The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty. J Bone Joint Surg. Am Vol. 1996;78(7):1004–1014. doi: 10.2106/00004623-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Hendrich C., Mehling I., Sauer U., Kirschner S., Martell J.M. Cementless acetabular reconstruction and structural bone-grafting in dysplastic hips. J Bone Joint Surg. Am Vol. 2006;88(2):387–394. doi: 10.2106/JBJS.D.02373. [DOI] [PubMed] [Google Scholar]
- 11.Shinar A.A., Harris W.H. Bulk structural autogenous grafts and allografts for reconstruction of the acetabulum in total hip arthroplasty. Sixteen-year-average follow-up. J Bone Joint Surg. Am Vol. 1997;79(2):159–168. doi: 10.2106/00004623-199702000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Gerber S.D., Harris W.H. Femoral head autografting to augment acetabular deficiency in patients requiring total hip replacement. A minimum five-year and an average seven-year follow-up study. J Bone Joint Surg. Am Vol. 1986;68(8):1241–1248. [PubMed] [Google Scholar]
- 13.Hooten J.P., Jr., Engh C.A., Heekin R.D., Vinh T.N. Structural bulk allografts in acetabular reconstruction. Analysis of two grafts retrieved at post-mortem. J Bone Joint Surg. Br Vol. 1996;78(2):270–275. [PubMed] [Google Scholar]
- 14.Delimar D., Cicak N., Klobucar H., Pecina M., Korzinek K. Acetabular roof reconstruction with pedicled iliac graft. Int Orthop. 2002;26(6):344–348. doi: 10.1007/s00264-002-0381-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Delimar D., Bohacek I., Pecina M., Bicanic G. Acetabular roof reconstruction with pedicled iliac graft: ten years later. Int Orthop. 2014;38(1):199–201. doi: 10.1007/s00264-013-2170-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Linde F., Jensen J., Pilgaard S. Charnley arthroplasty in osteoarthritis secondary to congenital dislocation or subluxation of the hip. Clin Orthop Relat Res. 1988;227:164–171. [PubMed] [Google Scholar]
- 17.Tsukada S., Wakui M. Bulk femoral head autograft without decortication in uncemented total hip arthroplasty: seven- to ten-year results. J Arthroplasty. 2012;27(3):437–444. doi: 10.1016/j.arth.2011.06.003. e431. [DOI] [PubMed] [Google Scholar]
- 18.Iida H., Matsusue Y., Kawanabe K., Okumura H., Yamamuro T., Nakamura T. Cemented total hip arthroplasty with acetabular bone graft for developmental dysplasia. Long-term results and survivorship analysis. J Bone Joint Surg Br. 2000;82(2):176–184. [PubMed] [Google Scholar]
- 19.Knight J.L., Fujii K., Atwater R., Grothaus L. Bone-grafting for acetabular deficiency during primary and revision total hip arthroplasty. A radiographic and clinical analysis. J Arthroplasty. 1993;8(4):371–382. doi: 10.1016/s0883-5403(06)80035-5. [DOI] [PubMed] [Google Scholar]
- 20.Mulroy R.D., Jr., Harris W.H. Failure of acetabular autogenous grafts in total hip arthroplasty: increasing incidence: a follow-up note. J Bone Joint Surg. Am Vol. 1990;72(10):1536–1540. [PubMed] [Google Scholar]
- 21.Harris W.H., Crothers O., Oh I. Total hip replacement and femoral-head bone-grafting for severe acetabular deficiency in adults. J Bone Joint Surg. Am Vol. 1977;59(6):752–759. [PubMed] [Google Scholar]
- 22.Marti R.K., Schuller H.M., van Steijn M.J. Superolateral bone grafting for acetabular deficiency in primary total hip replacement and revision. J Bone Joint Surg. Br Vol. 1994;76(5):728–734. [PubMed] [Google Scholar]
- 23.Schofer M.D., Pressel T., Schmitt J., Heyse T.J., Boudriot U. Reconstruction of the acetabulum in THA using femoral head autografts in developmental dysplasia of the hip. JClin Orthop Related Res. 2011;6:32. doi: 10.1186/1749-799X-6-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim M., Kadowaki T. High long-term survival of bulk femoral head autograft for acetabular reconstruction in cementless THA for developmental hip dysplasia. Clin Orthop Relat Res. 2010;468(6):1611–1620. doi: 10.1007/s11999-010-1288-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Jong P.T., Haverkamp D., van der Vis H.M., Marti R.K. Total hip replacement with a superolateral bone graft for osteoarthritis secondary to dysplasia: a long-term follow-up. J Bone Joint Surg. Br Vol. 2006;88(2):173–178. doi: 10.1302/0301-620X.88B2.16769. [DOI] [PubMed] [Google Scholar]
- 26.Inao S., Matsuno T. Cemented total hip arthroplasty with autogenous acetabular bone grafting for hips with developmental dysplasia in adults: the results at a minimum of ten years. J Bone Joint Surg. Br Vol. 2000;82(3):375–377. doi: 10.1302/0301-620x.82b3.10465. [DOI] [PubMed] [Google Scholar]
- 27.Rodriguez J.A., Huk O.L., Pellicci P.M., Wilson P.D., Jr. Autogenous bone grafts from the femoral head for the treatment of acetabular deficiency in primary total hip arthroplasty with cement. Long-term results. J Bone Joint Surg. 1995;77(8):1227–1233. doi: 10.2106/00004623-199508000-00013. [DOI] [PubMed] [Google Scholar]
- 28.Masui T., Iwase T., Kouyama A., Shidou T. Autogenous bulk structural bone grafting for reconstruction of the acetabulum in primary total hip arthroplasty: average 12-year follow-up. Nagoya J Med Sci. 2009;71(3–4):145–150. [PMC free article] [PubMed] [Google Scholar]
- 29.Saito S., Ishii T., Mori S., Hosaka K., Nemoto N., Tokuhashi Y. Long-term results of bulk femoral head autograft in cementless THA for developmental hip dysplasia. Orthopedics. 2011;34(2):88. doi: 10.3928/01477447-20101221-15. [DOI] [PubMed] [Google Scholar]
- 30.Busch V.J., Clement N.D., Mayer P.F., Breusch S.J., Howie C.R. High survivorship of cemented sockets with roof graft for severe acetabular dysplasia. Clin Orthop Related Res. 2012;470(11):3032–3040. doi: 10.1007/s11999-012-2346-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Akiyama H., Kawanabe K., Iida H., Haile P., Goto K., Nakamura T. Long-term results of cemented total hip arthroplasty in developmental dysplasia with acetabular bulk bone grafts after improving operative techniques. J Arthroplasty. 2010;25(5):716–720. doi: 10.1016/j.arth.2009.05.017. [DOI] [PubMed] [Google Scholar]
- 32.Delimar D., Aljinovic A., Bicanic G. Failure of bulk bone grafts after total hip arthroplasty for hip dysplasia. Arch Orthop Trauma Surg. 2014;134(8):1167–1173. doi: 10.1007/s00402-014-2006-8. [DOI] [PubMed] [Google Scholar]
- 33.Russotti G.M., Harris W.H. Proximal placement of the acetabular component in total hip arthroplasty. A long-term follow-up study. J Bone Joint Surg. Am Vol. 1991;73(4):587–592. [PubMed] [Google Scholar]
- 34.Spangehl M.J., Berry D.J., Trousdale R.T., Cabanela M.E. Uncemented acetabular components with bulk femoral head autograft for acetabular reconstruction in developmental dysplasia of the hip: results at five to twelve years. J Bone Joint Surg. Am Vol. 2001;83-a(10):1484–1489. doi: 10.2106/00004623-200110000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Yamaguchi M., Bauer T.W., Hashimoto Y. Deformation of the acetabular polyethylene liner and the backside gap. J Arthroplasty. 1999;14(4):464–469. doi: 10.1016/s0883-5403(99)90102-x. [DOI] [PubMed] [Google Scholar]
- 36.Yamaguchi T., Naito M., Asayama I., Shiramizu K. Cementless total hip arthroplasty using an autograft of the femoral head for marked acetabular dysplasia: case series. J Orthop Surg (Hong Kong) 2004;12(1):14–18. doi: 10.1177/230949900401200104. [DOI] [PubMed] [Google Scholar]
- 37.Zahar A., Papik K., Lakatos J., Cross M.B. Total hip arthroplasty with acetabular reconstruction using a bulk autograft for patients with developmental dysplasia of the hip results in high loosening rates at mid-term follow-up. Int Orthop. 2014;38(5):947–951. doi: 10.1007/s00264-014-2280-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Klapach A.S., Callaghan J.J., Miller K.A. Total hip arthroplasty with cement and without acetabular bone graft for severe hip dysplasia. A concise follow-up, at a minimum of twenty years, of a previous report. J Bone Joint Surg. Am Vol. 2005;87(2):280–285. doi: 10.2106/JBJS.D.02130. [DOI] [PubMed] [Google Scholar]