Abstract
Purpose
The aim of the study was to determine the 5 year migratory and wear patterns, adverse events and clinical outcomes of a cementless, porous acetabular cup.
Methods
RSA imaging of a cohort of 11 patients was retrospective analysed at 5 years post Total Hip Arthroplasty (THA). Changes in pain, function and symptoms of the hip at 5 years post-THA were compared to preoperative and 2 year postoperative assessments on the Harris Hip Score (HHS) and Hip dysfunction and Osteoarthritis Outcome Score (HOOS).
Results
The majority of cup migration occurred up to 6 months and stabilised thereafter (6 months to 5 years, p = 0.091–0.866, Wilcoxon Signed Rank test). The direction of rotation around the 3 axes was evenly distributed among the cups between anterior-posterior rotation, internal-external rotation and increased-decreased inclination. The majority of the cups translated proximally, at an average migration of 0.36 mm (±95%CI 0.17) at 5-years post-THA. Following initial bedding in, up to 6 months, there was no detectable polyethylene wear between 6 months and 5 years. At 5 years postoperatively, a statistically significant difference was observed across all HOOS subscales in comparison to preoperative values, with higher means reported at 5 years (p < 0.001). The total mean HHS displayed a statistically significant improvement, increasing from ‘poor’ preoperatively to ‘good’ at 5 years post-THA.
Conclusion
Following initial migration between discharge and 6 months, the cementless porous acetabular cup demonstrated a tendency for stabilisation from 6 months up to 5 years post-THA, suggesting good mid-term fixation. Additionally, improvements in clinical outcome measures of pain, function and quality-of-life remained high following THA at 5 years post-surgery.
Keywords: Acetabular cup, Migration, Radiostereometric analysis, RSA, Total Hip Arthroplasty, THA
1. Introduction
Cementless acetabular components continue to grow as the fixation of choice for conventional Total Hip Arthroplasty (THA) in Australia1.
Revision of primary conventional THA was reported at 3.9% in 2014 by the Australian Orthopaedic Association National Joint Replacement Registry.1 Loosening and lysis (28.0%), followed by dislocation (24.2%), continue to identify as major causes of revision and THA failure.1 At 7 years post-THA, loosening/lysis was identified as the predominant cause for revision.1 Large and, in particular, continuously, increasing migration implies instability. As such, monitoring the longer term stability of prosthetic devices is imperative.
The R3 acetabular cementless cup (Smith & Nephew, Memphis, TN) is one of the most frequently used acetabular components for conventional THA.1 From 2011 to 2014, the R3 cup listed as the third most commonly utilised acetabular model in Australia.1 Given the continual use of this acetabular component, further clinical data is necessary to monitor the performance of this cementless prosthesis. The present study considered the stability of the R3 cup through assessment of Radiostereometric Analysis (RSA).
RSA2 is a technique used to accurately measure the true position of an object in three-dimensional space.3 RSA allows the quantitative assessment of in vivo migration of orthopaedic devices. Migratory patterns of orthopaedic prosthetics has been used to predict aseptic loosening and long term stability of the device. Pijls et al.4 conducted an RSA meta-analysis concluding a clinically relevant association between early migration of acetabular cups and late revision.
There are currently four acetabular articular surfaces in use in Australia, which include cross-linked Polyethylene (PE), Non Cross-linked PE, ceramic and metal.1 This R3 system can accommodate three bearings (PE, ceramic, metal), with the ceramic and PE currently in use. The present acetabular shell utilises a three-dimensional asymmetric titanium powder coating with 60% porosity (Stik Tite, Smith & Nephew). Porous coatings with high porosity and greater coefficients of friction have demonstrated good biological fixation.5, 6
In 2009, a prospective cohort study commenced to determine the safety and effectiveness of the R3 device. Participants were assessed pre operatively and at 6 months, 1 year and 2 years post-THA.7 Findings at 2 years post-THA were identified as acceptable, yet within the ‘at risk’ range for early proximal migration (0.2–1.0 mm), and recommendations for further investigation were advised.7 Current views in studies of fixation suggest that the pattern of migration, rather than that magnitude, is of greater importance, highlighting the need for longer term follow-up.8, 9 In the present study authors assessed the same participant cohort 5 years post-THA.
The aim of the study was to determine the 5 year migratory and wear patterns, adverse events and clinical outcomes of a R3 acetabular cup.
The primary objective was to evaluate the pattern of acetabular cup migration at 5 years post-THA.
Secondary objectives were to assess changes in pain, function and symptoms of the hip using the patient and clinician reported outcomes measures, the Hip dysfunction and Osteoarthritis Outcome Score (HOOS), 5 years post-THA
2. Material and methods
A cohort of 20 participants took part in a prospective cohort study registered on the Australian New Zealand Clinical Trials registry (Registration Number: ACTRN12608000234314). A retrospective analysis of prospectively conducted RSA imaging was approved by a Human Research Ethics Committee (HREC No. 263.15).
Patients requiring a primary THA due to non-inflammatory degenerative joint disease were invited to participant in the trial. Patients were excluded from participation if they presented with any of the following characteristics: active infection or sepsis; vascular insufficiency, muscular atrophy, or neuromuscular disease severe enough to compromise implant stability or postoperative recovery; females of child-bearing age and not taking contraceptive precautions; inadequate bone stock to support the device; known moderate to severe renal insufficiency; known or suspected metal sensitivity; immunosuppression or receiving high doses of corticosteroids; emotional or neurological condition that would pre-empt their ability or willingness to participate; Body Mass Index (BMI) > 40 kg/m2.
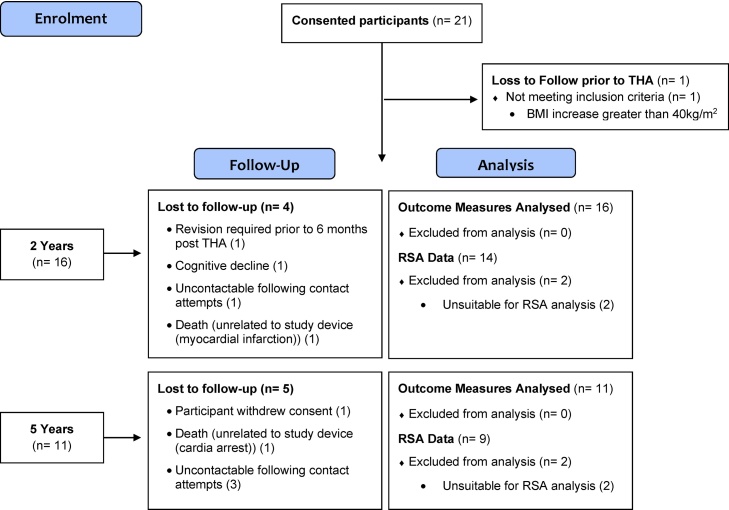
Initially, 21 patients consented for participation, however one participant was withdrawn due to a BMI increase of >40 at the time of surgery (Fig. 1). Patient demographics are listed in Table 1.
Fig. 1.
Recruitment and Follow-up Flow – Chart.
Table 1.
Baseline Participant Demographics.
| Preoperatively (n = 20) | 5 Year Follow − up (n = 11) | |
|---|---|---|
| Gender: n (%) | M: 8 (40.0); F: 12 (60.0) | M: 6 (54.5); F: 5 (45.5) |
| Age (Y): Mean (Range) | 69.5 (53 − 87) | 68.6 (57 − 84) |
| BMI (kg/m2): Mean (SD) | 28.47 (5.01) | 28.56 (5.20) |
| Primary Diagnosis: | Osteoarthritis | Osteoarthritis |
BMI Units: kg/m2; M: Male, F: Female; Y: Years; SD: Standard Deviation; n: number of participants.
Figures are based on demographic data gathered at time of recruitment.
2.1. Participant cohort: At 5 year follow-up
By 2 years post-surgery 4 participants were withdrawn from the study and an additional 2 participants were unable to be included in the 2 year RSA due to unsuitable imaging. Between the 2 and 5 year study follow-ups a further 2 participants were lost to follow-up due to withdrawal of consent and death, leaving a total of 14 participants available for follow-up at 5 years post-THA (Fig. 1).
2.2. Outcome measures
Patient and clinician reported outcome measures listed below are reported preoperatively, and at 2 years and 5 years post-THA.
2.2.1. Hip disability and Osteoarthritis Outcome Score 2.0 (HOOS)
The HOOS is a patient-reported outcome measure aimed to evaluate symptoms and functional limitations of the hip.10 It has been validated for patients with osteoarthritis pre- and post-THA.10 The HOOS consists of 40 items, subdivided into 5 subscales; Pain, Symptoms, Activity Limitations – Daily Living, Sports and Recreation Function, and Hip Related Quality of Life. Participants’ respond to each item on a 5-item Likert scale labelled none, mild, moderate, severe and extreme equating from 0 points to 4 points. Each subscale is then summed and standardised into a total out of 100, providing a 0–100 worst-to-best point scale.10
2.2.2. The Harris Hip Score (HHS)
The HHS is a clinician-administered outcome measure used for rating pain and functional capacity of the hip.11 It is widely adopted scoring system consisting of 4 domains totalling a maximum score of 0-to-100 points (pain (44), function (47), absence of deformity (5) and range of motion (4)).11, 12 The higher the HHS score achieved, the less hip dysfunction presented.12 The total HHS has been categorised as Poor (<70), Fair (70–79), Good (80–89) and Excellent (90–100).13, 14 The present paper compared the 5 year HHS to preoperative baseline HHS.
2.3. Operative details
Surgical procedures were performed at a single institution, by 9 orthopaedic surgeons. All participants underwent a posterolateral surgical approach, with the exception of 1 patient whose implant was inserted using a direct lateral approach.
Of the 11 participants analysed at the 5 year follow-up, 6 received the cemented Spectron femoral stem (Smith & Nephew), 4 received the cementless Anthology femoral stem (Smith & Nephew) and 1 received the CPCS cemented femoral stem (Smith & Nephew). Five patients received an oxidised zirconium (Oxinium, Smith & Nephew) femoral head, while 6 received a cobalt-chrome (CoCr) femoral head. A highly cross-linked polyethylene (XLPE) liner was used in 10 patients, however liner type was un-identifiable in 1 case.
2.4. Radiostereometric analysis technique
Ten tantalum markers (0.8 mm diameter; RSA Biomedical, Umea, Sweden) were placed in a standardised formation15 across the acetabulum whilst six tantalum markers (1.0 mm diameter; RSA Biomedical, Umea, Sweden) were placed in the outer rim of the polyethylene liner at the time of surgery.
Baseline RSA examinations were performed at discharge within 5 days of surgery and again at 6, 12, 24, and 60 months postoperatively. All RSA examinations were taken with patients in a supine position. A ceiling-mounted radiographic tube and a mobile radiographic tube were used simultaneously to take exposures of the hip with a calibration cage (Uniplanar Cage Number 43; RSA Biomedical). Acetabular migration was measured by movement of the acetabular cup relative to the acetabulum, whilst polyliner wear was measured by movement of the femoral head centre relative to the polyliner of the cup, using the UmRSA software (v6.0; RSA Biomedical). The accuracy of the technique was influenced by the stability and distribution of tantalum markers, determined by the mean error of rigid body fitting and the condition number, respectively. A cut-off level of 0.30 mm for the mean error of rigid body fitting and 120 for the condition number were used for exclusion of patients from the analysis.15 As this paper focused on magnitude and pattern of migration, absolute values for the different parameters were displayed.
2.5. Statistical analysis
Pijls et al.4 proposed that RSA studies of 10 to 60 participants followed for 2 years identified the same unsafe cups as data aggregated from thousands of patients captured at 10 years by joint registries. In consideration of this research, the study sample of 11 participants that remained at 5 years post-THA was anticipated to be sufficient in order to evaluate the migration of the R3 acetabular cup. The present research limited analysis to preoperative, 2 year and 5 year data as the remaining time-points have been published.7
Change in migration between 6 months and 5 years was analysed using the Wilcoxon Signed Rank test. This test was employed as the absolute values of the different migration parameters were not normally distributed.
All remaining analyses were conducted using Stata 14.1 (StataCorp, College Station, Texas). Means scores for the HHS and each HOOS subscale were obtained using separate random effects mixed models. The independent variables in each model were year (treated as a categorical), BMI, age and gender. A subject was entered in the model as a random effect. P-values for differences were obtained using Stata’s contrast command. A p-value of less than 0.05 (two-tailed) was deemed to be statistically significant.
3. Results
Of the 20 participants consented, 14 were contacted for follow-up at 5 years post-THA. Of these 14 participants, 3 were loss to follow-up following repeated contact attempts. Consequently, 11 participants were assessed using the HHS and HOOS questionnaires (Fig. 1).
3.1. Radiostereometric analysis
Of the 11 participants that underwent RSA imaging at 5 years post-THA, 9 were suitable for analysis. Radiographs of 2 study hips displayed poor marker visibility in the acetabulum, with condition numbers exceeding the acceptable range for inclusion, at >330 and >175.
3.1.1. Acetabular cup migration
The migration of the cups in the different directions up to 5 years is displayed in Table 2. The majority of the migration occurred up to 6 months, following which the cups stabilised (6 months to 5 years, p = 0.091–0.866, Wilcoxon Signed Rank test). The direction of rotation around the 3 axes was evenly distributed among the cups between anterior-posterior rotation, internal-external rotation and increased-decreased inclination. The majority of the cups translated proximally.
Table 2.
Migration (absolute values) of the cups up to 5-years.
| 6 months |
12 months |
24 months |
5 years |
6 months to 5 years |
|
|---|---|---|---|---|---|
| Mean (± 95% CI) | Mean (± 95% CI) | Mean (± 95% CI) | Mean (± 95% CI) | P* | |
| Rotations | |||||
| X axis (anterior-posterior rotation) | 0.98 (0.57) | 0.75 (0.57) | 0.68 (0.3) | 1.05 (0.58) | 0.612 |
| Y axis (internal-external rotation) | 0.96 (0.47) | 0.98 (0.86) | 0.99 (0.52) | 1.39 (1.14) | 0.091 |
| Z axis (increased-decreased inclination) | 0.86 (0.44) | 0.76 (0.52) | 0.77 (0.51) | 0.76 (0.65) | 0.345 |
| Translations | |||||
| X axis (medial-lateral) | 0.34 (0.15) | 0.36 (0.17) | 0.36 (0.17) | 0.26 (0.26) | 0.866 |
| Y axis (proximal-distal) | 0.35 (0.16) | 0.34 (0.20) | 0.39 (0.20) | 0.36 (0.17) | 0.398 |
| Z axis (anterior-posterior) | 0.26 (0.12) | 0.26 (0.14) | 0.35 (0.17) | 0.39 (0.29) | 0.176 |
3.1.2. Polyethylene wear
After the initial bedding in, up to 6 months, there was no detectable migration between 6 months and 5 years (Table 3). The annual migration (wear) from 6 months to 5 years was 0.002 mm (proximal wear) and 0.007 mm (2D wear).
Table 3.
Measurement of polyethylene liner wear up to 5 years (measured as femoral head penetration)
| 6 months |
12 months |
24 months |
5 years |
|||||
|---|---|---|---|---|---|---|---|---|
| mean | ± 95% CI | mean | ± 95% CI | mean | ± 95% CI | mean | ± 95% CI | |
| Proximal wear (y axis) | 0.12 | 0.15 | 0.12 | 0.18 | 0.09 | 0.16 | 0.13 | 0.17 |
| 2D wear (x and y axis) | 0.20 | 0.19 | 0.22 | 0.22 | 0.20 | 0.20 | 0.23 | 0.23 |
| 3D wear (x, y, and z axis) | 0.32 | 0.18 | 0.33 | 0.24 | 0.34 | 0.21 | 0.32 | 0.21 |
Mean (Confidence Interval).
3.2. Outcomes measures
3.2.1. HOOS
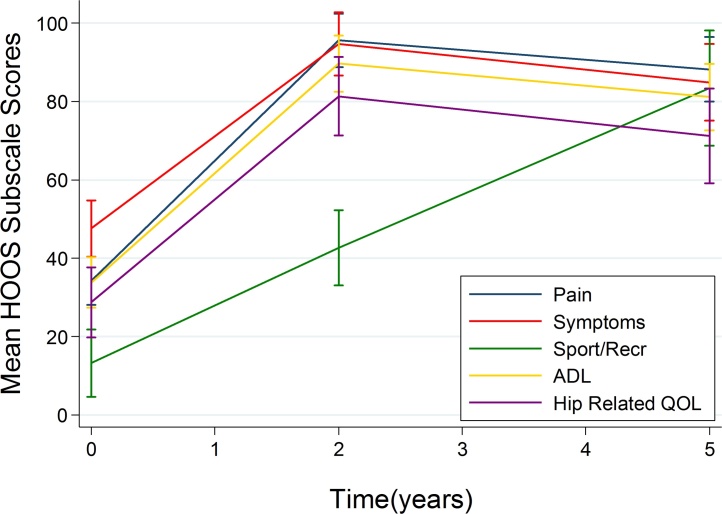
Mean and 95% Confidence Intervals (CI) of each HOOS subscale are reported in Table 4. A statistically significant difference was observed across all subscales at 5 years postoperatively in comparison to preoperative values, with higher means reported at 5 years (p < 0.001). No significant difference in HOOS subscales were present between 2 years and 5 years post-THA (p > 0.05), with the exception of the subscale, Sports and Recreation Function which displayed a significant mean increase between 2 and 5 years postoperatively (p < 0.001). Findings are graphically represented in the HOOS profile (Fig. 2).
Table 4.
HOOS Subscale Scores pre-operatively and at 2 years and 5 years following THA.
| HOOS Subscale | Pre-Operative (n = 20) | 2 Years (n = 16) | 5 Years (n = 11) | P-value Pre-Op Vs. 5 Yrs. | P-Value 2 Yrs. Vs. 5 Yrs. |
|---|---|---|---|---|---|
| Pain | 34.2 | 95.6 | 88.2 | <0.001 | 0.165 |
| (28.1, 40.3) | (88.8, 102.4) | (79.9, 96.5) | |||
| Symptoms | 47.6 | 94.7 | 84.9 | <0.001 | 0.130 |
| (40.4, 54.8) | (86.6, 102.7) | (75.1, 94.6) | |||
| ADL | 33.8 | 89.7 | 81.1 | <0.001 | 0.078 |
| (27.3, 40.3) | (85.5, 96.8) | (72.7, 89.5) | |||
| Sports/Recr | 13.3 | 42.6 | 83.4 | <0.001 | <0.001 |
| (4.7, 21.9) | (33.1, 52.2) | (68.7,98.1) | |||
| Hip Related QOL | 28.7 | 81.3 | 71.2 | <0.001 | 0.178 |
| (19.8, 37.7) | (71.3, 91.3) | (59.2,83.3) |
ADL: Activities of Daily Living; Sports/Recr.: Sports and Recreation Function; QOL: Quality of Life.
Fig. 2.
HOOS Profiles: Preoperatively and at 2 years and 5 years following THA.
ADL: Activities of Daily Living; Sports/Recr.: Sports and Recreation Function; QOL: Quality of Life.
3.2.2. HHS
The mean preoperative HHS was 46.3 (43.6, 55.0) in comparison to 80.5 (72.9, 88.1) at 5 year post-THA. A statistically significant improvement was observed between 5 years postoperatively and preoperative values (p < 0.001).
3.3. Adverse Events (AE)
Over the 5 year follow-up duration, 2 AE were identified as relating to the study device or operative site. The first related to the study device and involved a fractured calcar of the femur, intraoperatively. A second involved Cellulitis at the operative site, post-THA. A total of 29 AE were reported for 8 participants in this cohort, however the remaining 27 events were classified as not related to the study device, nor the operative site (Appendix A: Table A1).
4. Discussion
The aim of the study was to determine the 5 year migratory and wear patterns, adverse events and outcome measures of a R3 acetabular cup. Following initial migration between discharge and 6 months, the R3 acetabular cup demonstrated a tendency for stabilisation from 6 months up to 5 years post-THA.
The present study was primarily concerned with the pattern of migration rather than the magnitude of migration. Current views in RSA studies of fixation express that for cementless implants, the magnitude of migration from the initial postoperative RSA investigation to the following, i.e. 6 months, is not as significant as the pattern of migration from the second investigation onwards.8, 9 Such views arise as the magnitude of migration is dependent on many factors such as quality of the bone, initial fixation and most importantly, the time interval between surgery and initial RSA imaging. The R3 cup now demonstrates stabilisation over time to 5 years post-THA, suggesting good mid-term success in regards of fixation. Uncemented acetabular cups have demonstrated similar migration patterns in recent literature. Salemyr et al. assessed the migration of another porous, titanium cup, concluding no micromotion following initial migration which plateaued at 6 months.16
Several XLPE liners are available, however are developed using various manufacturing methods. Variations in manufacturing may include dose of radiation, type of radiation and the addition of vitamin E. Due to differing manufacturing processes it cannot be concluded that all XLPEs behave consistently in regards to wear, and as such are tested using RSA. The low annual wear rate for the XLPE of the R3 liner in the present study suggests that this variety of XLPE (Smith & Nephew) is an improvement compared to conventional polyethylene.
As would be expected, the HOOS demonstrated statistically significant improvements in pain, symptoms, function and quality of life 5 years post-THA in comparison to the patient’s preoperative state. This finding is consistent with scores at 2 years,7 with the exception of even further improvements in Sports and Recreation Function at 5 years post-THA. It is speculated that the greater score may be attributable to increased strength of the gluteal muscle or patient confidence, over time.
Similarly, the total mean HHS increased from a poor score preoperatively to a good score 5 years postoperatively, as classified by Harris et al.11 and Nilsdotter and Bremander12 The two adverse events identified as relating to the study device or operative site were reportedly resolved.
An important limitation of the study is the small sample available for analysis at 5 years post-THA, 9 of the 20 participants were analysed which may have influenced results. Additionally, given the 5 year follow-up time period, different researchers were required to analyse the 5 year clinical and RSA data. This may have influenced RSA analysis when considering the subjective nature of marker identification. Nevertheless, conclusions drawn from the migration data of the R3 cup at 2 years post-THA7 highlighted the need for longitudinal analysis, addressed in this work.
5. Conclusion
Following initial migration between discharge and 6 months, the R3 cementless porous acetabular cup demonstrated a tendency for stabilisation from 6 months up to 5 years post-THA, suggesting good mid-term fixation. Additionally, improvements in clinical outcomes measures of pain, function and quality of life remained high following THA at 5 years post-surgery.
Funding
No funding was provided for the 5 year retrospective review.
The prospective cohort from which the present 5 year data was compared was identified from an established study funded and designed by Smith & Nephew, Memphis, TN.
The company had no involvement in the study conduct, data analysis, manuscript preparation or any aspect of the 5 year retrospective review reported in this paper.
Authors do not have any proprietary interests in the materials described in the article.
Author contribution
Ms. Annika Theodoulou: Literature review, collection of patient data, manuscript write-up and preparation for publication.
Professor Kjell G. Nilsson: Analysis, interpretation and write-up of Radiostereometric analysis findings.
Associate Professor Graham Mercer: Study development and interpretation of clinical findings.
Dr. Stephen J. Quinn: Statistical analysis and statistical interpretation and write-up of clinical outcome measures.
Professor Jeganath Krishnan: Study development and interpretation of clinical findings.
Conflict of interest
None.
Acknowledgement
The authors gratefully acknowledge and thank Mr Pawel Skuza for preliminary statistical advice.
Appendix A
Table A1.
Adverse Events.
| Participant ID | Adverse Event | Severity | Involves Operative Site/Hip | Relationship to study device |
|---|---|---|---|---|
| 001 | Intraoperative fractured calcar of left femur | Mild | Yes | Definitely related |
| Elective TKA | Mild | No | Not related | |
| First Seizure | Mild | No | Not related | |
| Excision of recurrent squamous cell carcinoma in parotid with Level LN clearance and Tonsillectomy | Mild | No | Not related | |
| 003 | Urinary tract infection | Mild | No | Not related |
| Anaemia | Moderate | No | Not related | |
| Worsening bowel cancer | Moderate | No | Not related | |
| Moderately differentiated caecal adenocarcinoma requiring right hemicolectomy | Moderate | No | Not related | |
| 004 | Right Cellulitis post-Right THA | Mild | Yes | Not related |
| 006 | Severe left osteoarthritic hip with early changes of osteonecrosis | Mild | No | Not related |
| 008 | Left THA − elective | Moderate | No | Not related |
| Cardiac arrest. | Severe | No | Not related | |
| 010 | THA | Mild | No | Not related |
| Right benign obturator lesion | Mild | No | Not related | |
| 012 | NSTEMI Myocardial Infarction | Severe | No | Not related |
| 013 | Left hip pain post- THA | Mild | No | Not related |
| Left hip greater trochanteric bursitis | Mild | No | Not related | |
| Left THA | Mild | No | Not related | |
| Left Hip Acetabular Revision (not the study Hip) | Mild | No | Not related | |
| 015 | Osteoarthritis left hip | No | ||
| 017 | Mallory Weiss Tear | Mild | No | Not related |
| Benign prostatic Hypertrophy | Mild | No | Not related | |
| Febrile Illness | Mild | No | Not related | |
| 019 | Osteoarthritis left hip THA | Mild | No | Not related |
| Diffuse large B cell lymphoma and follicular lymphoma | Mild | No | Not related | |
| Palpitations for Investigation | Mild | No | Not related | |
| 020 | Possible cardiac small vessel ischaemia secondary to T2DM | Mild | No | Not related |
| Elective angiogram with PCI | Mild | No | Not related | |
| 021 | Admission to hospital with AF and delirium following slow cognitive decline | Severe | No | Not related |
TKA: Total Knee Arthroplasty; THA: Total Knee Arthroplasty.
References
- 1.Australian Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide: AOA; 2015.
- 2.Selvik G. Roentgen stereophotogrammetry: a method for the study of the kinematics of the skeletal system. Acta Orthop Scand Suppl. 1989;232:1–51. [PubMed] [Google Scholar]
- 3.Karrholm J., Herberts P., Hultmark P., Malchau H., Nivbrant B., Thanner J. Radiostereometry of hip prostheses. Review of methodology and clinical results. Clin Orthop Relat Res. 1997;344:94–110. [PubMed] [Google Scholar]
- 4.Pijls B.G., Nieuwenhuijse M.J., Fiocco M. Early proximal migration of cups is associated with late revision in THA: a systematic review and meta-analysis of 26 RSA studies and 49 survivalstudies. Acta Orthop. 2012;83(6):583–591. doi: 10.3109/17453674.2012.745353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bourne R.B., McCalden R.W., Naudie D., Charron K.D., Yuan X., Holdsworth D.W. The next generation of acetabular shell design and bearing surfaces. Orthopedics. 2008;31(Suppl. 2 (12)) [PubMed] [Google Scholar]
- 6.Naudie D.D., Somerville L., Korczak A. A randomized trial comparing acetabular component fixation of two porous ingrowth surfaces using RSA. J Arthroplasty. 2013;28(Suppl. (8)):48–52. doi: 10.1016/j.arth.2013.06.041. [DOI] [PubMed] [Google Scholar]
- 7.Grosser D., Benveniste S.H., Bramwell D., Krishnan J. Early migration of the R3 uncemented acetabular component: a prospective 2 year radiostereometric analysis. J Surgery. 2013;1(2) [Google Scholar]
- 8.Callary S.A., Campbell D.G., Mercer G.E., Nilsson K.G., Field J.R. The 6-year migration characteristics of a hydroxyapatite-coated femoral stem: a radiostereometric analysis study. J Arthroplasty. 2012;27(7) doi: 10.1016/j.arth.2011.12.002. 1344-1348 e1341. [DOI] [PubMed] [Google Scholar]
- 9.Henricson A., Nilsson K.G. Trabecular metal tibial knee component still stable at 10 years. Acta Orthop. 2016;87(5):504–510. doi: 10.1080/17453674.2016.1205169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nilsdotter A.K., Lohmander L.S., Klassbo M., Roos E.M. Hip disability and osteoarthritis outcome score (HOOS)–validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;4:10. doi: 10.1186/1471-2474-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harris W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 12.Nilsdotter A., Bremander A. Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care Res (Hoboken) 2011;63(Suppl. 11):S200–207. doi: 10.1002/acr.20549. [DOI] [PubMed] [Google Scholar]
- 13.Kavanagh B.F., Fitzgerald R.H., Jr. Clinical and roentgenographic assessment of total hip arthroplasty. A new hip score. Clin Orthop Relat Res. 1985;193:133–140. [PubMed] [Google Scholar]
- 14.Marchetti P., Binazzi R., Vaccari V. Long-term results with cementless fitek (or fitmore) cups. J Arthroplasty. 2005;20(6):730–737. doi: 10.1016/j.arth.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 15.Valstar E.R., Gill R., Ryd L., Flivik G., Borlin N., Karrholm J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop. 2005;76(4):563–572. doi: 10.1080/17453670510041574. [DOI] [PubMed] [Google Scholar]
- 16.Salemyr M., Muren O., Eisler T. Porous titanium construct cup compared to porous coated titanium cup in total hip arthroplasty: a randomised controlled trial. Int Orthop. 2015;39(5):823–832. doi: 10.1007/s00264-014-2571-z. [DOI] [PubMed] [Google Scholar]