Background:
Despite improvements in early detection of breast cancer, disparities persist in stage at diagnosis, which is an important prognostic factor.
Methods:
We used the space-time scan statistic in SaTScan to identify geographic areas and time periods with significantly elevated proportions of female breast cancer diagnosed at the in situ or distant stage in New Jersey. The analyses were conducted with census tracts as the geographic unit of analysis, elliptical spatial windows, 3-year temporal windows, and Poisson models. Statistical significance was determined by 999 Monte Carlo simulations (P < .05); significant clusters were mapped in ArcMap. Breast cancer cases within the clusters were compared with breast cancer cases outside the clusters on demographic, socioeconomic, and clinical factors using the Pearson chi-square test (P < .05). In addition, populations within the clusters were compared with the population outside the clusters on demographic and socioeconomic factors.
Results:
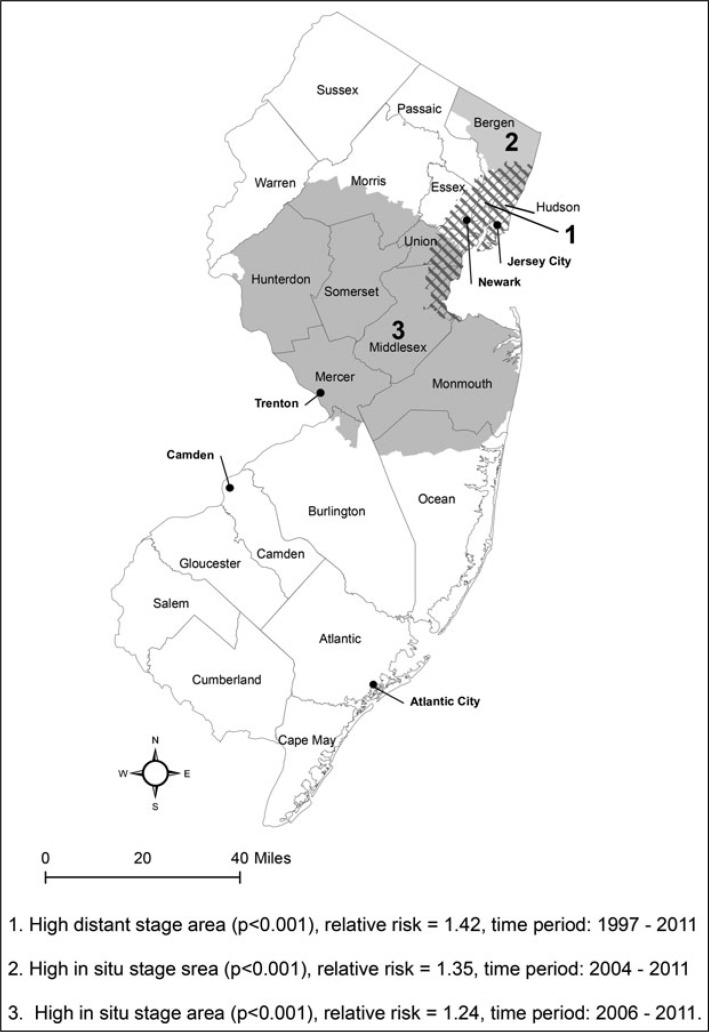
After exclusions, 126 756 cases of primary female breast cancer diagnosed in 1997 to 2011 from the New Jersey State Cancer Registry were included in the analysis. One distant stage breast cancer cluster was identified in northeastern New Jersey from 1997 through 2011 (n = 26 244, relative risk [RR] = 1.42, P < .001). Two in situ breast cancer clusters were found in northeastern New Jersey from 2004 through 2011 (n = 12 496, RR = 1.35, P < .001) and in central New Jersey from 2006 through 2011 (n = 29 319, RR = 1.24, P < .001). The distant stage cluster contained relatively high percentages of minority and lower socioeconomic status (SES) breast cancer cases and populations, whereas the in situ clusters had relatively low percentages of minority and lower SES breast cancer cases and populations.
Conclusion:
Although there have been improvements since an earlier study of distant stage breast cancer diagnosed in 1995 to 1997, disparities in stage at diagnosis continue. These findings can be used by our local cancer control partners to target specific populations for interventions such as breast cancer education and mammography screening, as well as by state legislative and public health authorities for resource allocation.
Keywords: breast cancer, disparities, GIS, spatial-temporal analysis, stage
Breast cancer continues to be the leading cancer diagnosis and second largest cause of cancer mortality among US women, with an estimated 247 000 new cases and 40 500 deaths in 2016.1 Although the age-adjusted incidence rate of breast cancer for non-Hispanic white women was higher than that for non-Hispanic black women, 128.1 versus 124.3 per 100 000 in 2008 to 2012, the mortality rate was 42% higher in black non-Hispanic women than in white non-Hispanic women (31.0 vs 21.9).1 Female breast cancer survival rates in the United States have improved greatly since 1975; however, for women diagnosed in 2005 to 2011, the 5-year relative survival rate was much lower for blacks (81%) than for whites (92%).1 Stage at diagnosis is an important prognostic factor with 5-year relative survival rates of 99%, 85%, and 26% for breast cancers diagnosed at the local, regional, and distant stages, respectively.1
In New Jersey, the 5-year (2009-2013) age-adjusted incidence rate for female breast cancer was 131.4 per 100 000. However, the rates varied greatly by race and ethnicity—135.5, 120.6, 89.8, and 96.2 among white, black, Asian and Pacific Islander (API), and Hispanic (of any race) women, respectively.2 As in the United States, NJ black women have a higher breast cancer age-adjusted mortality rate than white women, 30.4 per 100 000 compared with 23.7 per 100 000 in 2008 to 2012, despite their lower incidence rate.3 The 5-year relative survival rate for cancers diagnosed in 2001 to 2005 was lower for NJ black women (76.4%) than for white (89.7%), API (88.3%), and Hispanic (87.4%) women.4 This survival difference is related to a lower percentage of black women diagnosed at the local stage (49.5%) than women in the other race and ethnic groups (54%-59%) and to black women's lower survival at each stage (local, regional, distant)4 as well as to other factors.
Early detection of breast cancer through mammography has been shown to decrease mortality and increase treatment options, and it is recommended by many organizations.1,5 In recognition of the importance of early detection in breast cancer control, “Healthy People 2020” and “Healthy New Jersey 2020” objectives relating to breast cancer include reducing late-stage female breast cancer, increasing the proportion of women who receive breast cancer screening, and reducing the female breast cancer mortality rate.6,7 Healthy People 2020 also includes increasing the proportion of women who are counseled by their providers about mammograms.6
Breast cancer and other cancers have been studied over space and time, including breast cancer incidence,8–10 breast cancer mortality,11 proportion of in situ or late-stage breast cancer,12,13 proportion of late-stage prostate cancer,14,15 and brain cancer incidence.16 The space-time scan statistic in SaTScan software was used in some of these cancer studies,11,13,16 as well as in studies of other health problems such as accidental poisoning17 and AIDS mortality.18,19
The purpose of this study was to identify geographic areas and time periods with significantly elevated proportions of female breast cancer diagnosed at the in situ or distant stage in New Jersey from 1997 through 2011 and then to map and characterize the geographic areas. A previous study using a spatial scan statistic found 2 geographic areas in northeastern New Jersey that had significantly elevated proportions of women with breast cancer diagnosed at the distant stage from 1995 through 1997.20 The present study expands upon the earlier study by adding 14 diagnosis years, the dimension of time as well as space, and a search for clusters of elevated proportions of women diagnosed with breast cancer in situ. The 2 outcomes of interest, distant stage breast cancer and in situ breast cancer, were chosen because survival with distant stage breast cancer is very low whereas survival with in situ breast cancer is extremely high. In addition, mammography use is strongly associated with the incidence of in situ breast cancer.21
Methods
Cases
Incident cases of breast cancer were obtained from the NJ State Cancer Registry (NJSCR), which is a high-quality population-based cancer incidence registry covering a diverse population of about 8.9 million people residing in New Jersey. It is a National Cancer Institute (NCI) Surveillance, Epidemiology and End Results (SEER) expansion registry and part of CDC's National Program of Cancer Registries. NJ regulations (N.J.A.C. 8:57A) require reporting of newly diagnosed cancer cases to the NJSCR by hospitals, diagnosing physicians, dentists, and independent clinical laboratories.
Demographic and clinical information about each newly diagnosed cancer case (eg, age, sex, race, ethnicity, date of diagnosis, stage at diagnosis, primary payer at diagnosis) is included. Primary site and histology are coded to the International Classification of Diseases for Oncology, third edition (ICD-O-3)22 and stage at diagnosis is coded according to SEER summary stage (in situ, local, regional, distant, unknown).23,24
Cases are geocoded to their address at diagnosis by SEER*DMS, the database management system used by NJSCR. Geocoding services within SEER*DMS are provided by the Automated Geospatial Geocoding Interface Environment System, developed and supported through collaborative efforts of the North American Association of Central Cancer Registries, Texas A&M University, and NCI.25 Additional details about case ascertainment, coding, case completeness, and other quality measures are included in NJSCR annual reports at http://nj.gov/health/ces/index.shtml.
Primary in situ and invasive female breast cancer cases in the NJSCR diagnosed from 1997 through 2011 were included in this study. Cases diagnosed in 1979 through 1994 were excluded because the proportion of unknown stage breast cancers was greater than 10% each year. Cases diagnosed in 1995 and 1996 were excluded because we included the most recent diagnosis year available (2011) and we needed 3-year time windows. The ICD-O-3 codes for breast cancer are those in the SEER site recode definition (site code C500-C509), except mesotheliomas and Kaposi's sarcomas were excluded.26 Cases ascertained by death certificate or autopsy report only or without a valid census tract were excluded. The 2000 census tract boundary centroid geocodes were used for all cases.
Statistical Methods
The space-time scan statistic in SaTScan software (version 9.3) was used to identify geographic areas and time periods with significantly elevated proportions of women with breast cancer diagnosed at the in situ or distant stage.16,27 The SaTScan analyses were conducted with census tracts as the geographic aggregation unit, elliptical spatial windows,28 Poisson model, maximum cluster size of 50% of the population at risk, and 3-year temporal windows. We used the Poisson model rather than the Bernouli model, which also is available in SaTScan, because we had population-based data and female breast cancer diagnosed at the in situ or distant stage is relatively rare. Statistical significance was determined by 999 Monte Carlo simulations (P < .05).
“Cases” were defined as women who were diagnosed with breast cancer at the in situ or distant stage from 1997 to 2011 (numerators) and the “population at risk” was all female breast cancer cases diagnosed from 1997 to 2011 (denominators). The relative risk (RR) for each cluster, that is, the risk of being diagnosed at the in situ or distant stage within the cluster versus the risk outside the cluster, was estimated in SaTScan. The RR is the ratio of the observed number of “cases” (cases diagnosed at the distant or in situ stage) divided by the expected number of “cases” within the cluster and the observed number of “cases” divided by the expected number of “cases” outside the cluster. The expected numbers of “cases” were calculated by applying the statewide proportion of distant or in situ diagnoses to the total number of cases inside and outside the clusters. The SaTScan results were exported to ArcGIS ArcMap version 10.0 for mapping.
Breast cancer cases in the clusters were compared with the cases in the rest of New Jersey on clinical, demographic, and socioeconomic status (SES) characteristics—stage (in situ, local, regional, distant, unknown), age (0-44, 45-64, 65 and older), race (white, black, API, other/unknown), ethnicity (non-Hispanic, Hispanic), marital status (married, not married, unknown), insurance status (private, Medicare, Medicaid, other government, not insured, unknown), and percentage of residents living in poverty in the census tract the case resided in at the time of diagnosis (0%-<5%, 5%-<10%, 10%-<20%, 20%-100%, unknown). Statistical significance of differences between cases in the clusters and the rest of New Jersey were determined with the Pearson chi-square test (P < .05).
Populations within the clusters were compared with the population in the rest of New Jersey for differences in demographic and socioeconomic characteristics including race, ethnicity, language spoken at home, education, marital status, unemployment, renter occupied housing, family income, and per capita income using data from the United States Census Bureau's 2005-2009 American Community Survey.29 The descriptive statistics of the cases and populations inside and outside the clusters were calculated using SAS version 9.4 (SAS Institute Inc, Cary, North Carolina).
Results
A total of 126 756 cases of in situ and invasive female breast cancer were included in the analyses, after excluding 602 cases ascertained only from death certificates and autopsy reports and 360 cases without a valid census tract. Of the 126 756 cases, 5 951 (4.7%) were diagnosed at the distant stage and 27 181 (21.4%) were diagnosed with in situ breast cancer.
Distant stage breast cancer
SaTScan identified a single cluster in northeastern New Jersey (Cluster 1) with a significantly elevated proportion of breast cancer diagnosed at the distant stage from 1997 through 2011 (RR = 1.42; P < .001) (Figure 1). It encompassed 1 entire county and sections of 4 counties (Figure 1) and included 1613 cases diagnosed at the distant stage, 6.1% of breast cancer cases in the cluster, and 27.1% of distant stage breast cancer cases diagnosed statewide (Table 1).
FIGURE 1.
Geographic Areas in New Jersey With Significantly Elevated Proportions of Breast Cancer Cases Diagnosed at the Distant Stage or In Situ The clusters were identified by SaTScan software as having a significantly higher proportion of distant stage breast cancers (cluster 1) or significantly higher proportions of in situ breast cancers (clusters 2 and 3) than the rest of New Jersey. Data are from the New Jersey State Cancer Registry, New Jersey Department of Health, 2014 analytic file.
TABLE 1. Characteristics of Breast Cancer Cases in the Geographic Area With a Significantly Elevated Proportion of Cases Diagnosed at the Distant Stage Versus Breast Cancer Cases in the Rest of New Jersey, 1997 to 2011 (N = 126 756)a.
| Cluster 1 (n = 26 244)b | Rest of New Jersey (n = 100 512) | New Jersey (N = 126 756) | ||||
|---|---|---|---|---|---|---|
| Characteristic | Number | % | Number | % | Number | % |
| Stage at diagnosisc | ||||||
| In situ | 4 966 | 18.9 | 22 215 | 22.1 | 27 181 | 21.4 |
| Local | 11 839 | 45.1 | 47 703 | 47.5 | 59 542 | 47.0 |
| Regional | 6 747 | 25.7 | 23 262 | 23.1 | 30 009 | 23.7 |
| Distant | 1 613 | 6.1 | 4 338 | 4.3 | 5 951 | 4.7 |
| Unknown | 1 079 | 4.1 | 2 994 | 3.0 | 4 073 | 3.2 |
| Age at diagnosisc | ||||||
| 0-44 y | 3 514 | 13.4 | 12 681 | 12.6 | 16 195 | 12.8 |
| 45-64 y | 11 951 | 45.5 | 47 267 | 47.0 | 59 218 | 46.7 |
| 65 y and older | 10 779 | 41.1 | 40 564 | 40.4 | 51 343 | 40.5 |
| Racec | ||||||
| White | 18 913 | 72.1 | 88 952 | 88.5 | 107 865 | 85.1 |
| Black | 5 660 | 21.6 | 7 649 | 7.6 | 13 309 | 10.5 |
| Asian and Pacific Islander | 1 419 | 5.4 | 3 448 | 3.4 | 4 867 | 3.8 |
| Other/unknownd | 252 | 1.0 | 463 | 0.5 | 715 | 0.6 |
| Ethnicityc | ||||||
| Non-Hispanic | 21 895 | 83.4 | 95 936 | 95.4 | 117 831 | 93.0 |
| Hispanic | 4 349 | 16.6 | 4 576 | 4.6 | 8 925 | 7.0 |
| Marital statusc | ||||||
| Married | 11 692 | 44.6 | 57 516 | 57.2 | 69 208 | 54.6 |
| Not marriede | 13 267 | 50.6 | 36 748 | 36.6 | 50 015 | 39.5 |
| Unknown | 1 285 | 4.9 | 6 248 | 6.2 | 7 533 | 5.9 |
| Insurance statusc | ||||||
| Private | 11 337 | 43.2 | 49 551 | 49.3 | 60 888 | 48.0 |
| Medicare | 8 616 | 32.8 | 31 822 | 31.7 | 40 038 | 31.9 |
| Medicaid | 995 | 3.8 | 1 561 | 1.6 | 2 556 | 2.0 |
| Other government | 14 | 0.1 | 173 | 0.2 | 187 | 0.1 |
| Not insured | 1 632 | 6.2 | 2.290 | 2.3 | 3 922 | 3.1 |
| Unknown | 3 650 | 13.9 | 15 115 | 15.0 | 18 765 | 14.8 |
| Neighborhood poverty levelc,f | ||||||
| 0%-<5% | 6 616 | 25.2 | 62 424 | 62.1 | 69 040 | 54.5 |
| 5%-<10% | 7 351 | 28.0 | 24 787 | 24.7 | 32 138 | 25.4 |
| 10%-<20% | 7 806 | 29.7 | 9 350 | 9.3 | 17 156 | 13.5 |
| 20%-100% | 4 465 | 17.0 | 3 918 | 3.9 | 8 383 | 6.6 |
| Unknown | 6 | <0.05 | 33 | <0.05 | 39 | <0.05 |
aData are from the New Jersey State Cancer Registry, New Jersey Department of Health, 2014, analytic file.
bCluster 1 was identified by SaTScan software as having a significantly elevated proportion of distant stage breast cancer during 1997 through 2011 (P < .001).
cP < .001, P values are from Pearson chi-square tests comparing cluster 1 with the rest of New Jersey.
dIncludes American Indian/Alaskan Native.
eIncludes separated, divorced, widowed.
fNeighborhood poverty level of the residents in the census tracts the cases resided in at the time of diagnosis, for example, 0%-<5% means 0% to <5% of the residents lived in poverty. Cases diagnosed between 1997 and 2004 were assigned a neighborhood poverty level based on data from the 2000 US Census; cases diagnosed in 2005 and later were assigned a neighborhood poverty level based on data from the American Community Survey, US Census Bureau.
The comparison of breast cancer cases in cluster 1 to breast cancer cases in the rest of New Jersey revealed that the cluster contained significantly higher percentages of younger (0-44) and older (65 and older), black, API, Hispanic, not married, and uninsured or Medicaid-insured cases (P < .001; Table 1). Breast cancer cases in the cluster also were more likely to reside in high poverty census tracts. The population in this cluster had substantially higher percentages of blacks, Hispanics, and foreign-born persons than the population in the rest of New Jersey, as well as higher percentages of households with Spanish or an Indo-European language spoken at home and persons who speak English less than well (Table 2). The population within Cluster 1 also had higher percentages of people without a high school education, unmarried and unemployed, renter occupied housing, and families with incomes below poverty than the population in the rest of New Jersey. The cluster population had a lower per capita income (Table 2).
TABLE 2. Population Characteristics in the Geographic Area With a Significantly Elevated Proportion of Breast Cancer Cases Diagnosed at the Distant Stage Versus Breast Cancer Cases Diagnosed in the Rest of New Jerseya.
| Characteristic | Cluster 1b | Rest of New Jersey | New Jersey |
|---|---|---|---|
| Total population | 2 170 272 | 6 480 276 | 8 650 548 |
| Women 20 and older | 840 070 | 2 462 575 | 3 302 645 |
| Black racec | 24.8% | 11.0% | 14.4% |
| Hispanic ethnicity | 30.3% | 11.1% | 15.9% |
| Foreign-born persons | 33.3% | 15.1% | 19.7% |
| Language spoken at home (age 5 y and older) | |||
| Spanish | 19.6% | 7.1% | 9.4% |
| Other Indo-Europeand | 11.2% | 6.4% | 7.3% |
| Asian and Pacific Islandere | 4.7% | 3.4% | 3.6% |
| Speak English less than well | 15.7% | 6.7% | 8.3% |
| Education (age 25 y and older) | |||
| Less than high school education | 19.6% | 11.0% | 13.2% |
| Marital status (women age 15 y and older) | |||
| Now married | 40.1% | 51.4% | 48.5% |
| Economic status | |||
| Unemployed (age 16 and older) | 8.2% | 6.5% | 7.0% |
| Housing that is renter occupied | 55.8% | 25.0% | 32.9% |
| Family income below poverty | 11.4% | 5.5% | 7.0% |
| Per capita income | $27 760 | $36 853 | $34 571 |
aData are based on the American Community Survey 2005-2009, US Census Bureau.
bCluster 1 was identified by SaTScan software as having a significantly elevated proportion of distant stage breast cancer during 1997 through 2011 (P < .001).
cFrom 1 race or from 2 or more races.
dIncludes Greek, Russian, Polish, Serbo-Croatian, other Slavic languages, Hindi, and other Indic languages.
eIncludes Chinese, Japanese, Korean, other Asian languages, Tagalog, Hawaiian, and other Pacific Island languages.
In situ breast cancer
Two clusters with significantly high proportions of in situ breast cancer were identified, one in northeastern New Jersey from 2004 to 2011 (cluster 2, RR = 1.35, P < .001) and the other in central New Jersey from 2006 to 2011 (cluster 3, RR = 1.24, P < .001). Cluster 2 covered almost an entire county and had 3195 in situ cases, representing 25.6% of breast cancer cases in the cluster and 11.8% of in situ breast cancer cases diagnosed statewide. Cluster 3 included 4 counties, most of 2 counties, and parts of 3 other counties in central New Jersey (Figure 1) and had 6894 in situ cases, representing 23.5% of breast cancer cases in the cluster and 25.4% of in situ cases diagnosed statewide (Table 3).
TABLE 3. Characteristics of Breast Cancer Cases in the Geographic Areas With Significantly Higher Proportions Diagnosed In Situ Versus Breast Cancer Cases Diagnosed in the Rest of New Jersey (N = 126 756)a.
| Characteristic | Cluster 2 (n = 12 496)b | Cluster 3 (n = 29 319)b | Rest of New Jersey (n = 84 941) | New Jersey (N = 126 756) |
|---|---|---|---|---|
| Stage at diagnosisc | ||||
| In situ | 3 195 (25.6%) | 6 894 (23.5%) | 17 092 (20.1%) | 27 181 (21.4%) |
| Local | 5 861 (46.9%) | 13 701 (46.7%) | 39 980 (47.1%) | 59 542 (47.0%) |
| Regional | 2 619 (21.0%) | 6 708 (22.9%) | 20 682 (24.4%) | 30 009 (23.7%) |
| Distant | 504 (4.0%) | 1 225 (4.2%) | 4 222 (5.0%) | 5 951 (4.7%) |
| Unknown | 317 (2.5%) | 791 (2.7%) | 2 965 (3.5%) | 4 073 (3.2%) |
| Age at diagnosisc | ||||
| 0-44 y | 1 531 (12.3%) | 4 046 (13.8%) | 10 618 (12.5%) | 16 195 (12.8%) |
| 45-64 y | 5 947 (47.6%) | 14 312 (48.8%) | 38 959 (45.9%) | 59 218 (46.7%) |
| 65 y and older | 5 018 (40.2%) | 10 961 (37.4%) | 33 364 (41.6%) | 51 343 (40.5%) |
| Racec | ||||
| White | 10 810 (86.5%) | 24 923 (85.0%) | 72 132 (84.9%) | 107 865 (85.1%) |
| Black | 692 (5.5%) | 2 578 (8.8%) | 10 039 (11.8%) | 13 309 (10.5%) |
| Asian and Pacific Islander | 903 (7.2%) | 1 675 (5.7%) | 2 289 (2.7%) | 4 867 (3.8%) |
| Other/unknownd | 91 (0.7%) | 143 (0.5%) | 481 (0.6%) | 715 (0.6%) |
| Ethnicityc | ||||
| Non-Hispanic | 11 752 (94.1%) | 27 921 (95.2%) | 78 158 (92.0%) | 117 831 (93.0%) |
| Hispanic | 744 (6.0%) | 1 398 (4.8%) | 6 783 (8.0%) | 8 925 (7.0%) |
| Marital statusc | ||||
| Married | 7 556 (60.5%) | 17 592 (60.0%) | 44 060 (51.9%) | 69 208 (54.6%) |
| Not marriede | 4 452 (35.6%) | 10 488 (35.8%) | 35 075 (41.3%) | 50 015 (39.5%) |
| Unknown | 488 (3.9%) | 1 239 (4.2%) | 5 806 (6.8%) | 7 533 (5.9%) |
| Insurance statusc | ||||
| Private | 6 414 (51.3%) | 15 738 (53.7%) | 38 736 (45.6%) | 60 888 (48.0%) |
| Medicare | 4 158 (33.3%) | 8 709 (29.7%) | 27 571 (32.5%) | 40 438 (31.9%) |
| Medicaid | 182 (1.5%) | 388 (1.3%) | 1 986 (2.3%) | 2 556 (2.0%) |
| Other government | 7 (0.1%) | 38 (0.1%) | 142 (0.2%) | 187 (0.2%) |
| Not insured | 363 (2.9%) | 760 (2.6%) | 2 799 (3.3%) | 3 922 (3.1%) |
| Unknown | 1 372 (11.0%) | 3 686 (12.6%) | 13 707 (16.1%) | 18 765 (14.8%) |
| Neighborhood poverty levelc,f | ||||
| 0%-<5% | 8 410 (67.3%) | 20 737 (70.7%) | 39 893 (47.0%) | 69 040 (54.5%) |
| 5%-<10% | 2 795 (22.4%) | 5 682 (19.4%) | 23 661 (27.9%) | 32 138 (25.4%) |
| 10%-<20% | 1 218 (9.8%) | 1 998 (6.8%) | 13 940 (16.4%) | 17 156 (13.5%) |
| 20%-100% | 73 (0.6%) | 892 (3.0%) | 7 418 (8.7%) | 8 383 (6.6%) |
| Unknown | 0 | 10 (<0.05%) | 29 (<0.05%) | 39 (<0.05%) |
aData are from the New Jersey State Cancer Registry, New Jersey Department of Health, 2014 analytic file.
bClusters 2 and 3 were identified by SaTScan software as having significantly elevated proportions of in situ breast cancers during 2004 to 2011 for cluster 2 and during 2006 to 2011 for cluster 3 (P < .001).
cP < .001, P values are from Pearson chi-square tests comparing the clusters with the rest of New Jersey.
dIncludes American Indian/Alaskan Native.
eIncludes separated, divorced, widowed.
fNeighborhood poverty level of the residents of the census tracts the cases resided in at the time of diagnosis, for example, 0%-<5% means 0% to <5% of the residents lived in poverty. Cases diagnosed between 1997 and 2004 were assigned a neighborhood poverty level based on data from the 2000 US Census; cases diagnosed in 2005 and later were assigned a neighborhood poverty level based on data from the American Community Survey, US Census Bureau.
The in situ breast cancer clusters (clusters 2 and 3) had lower percentages of cases 65 and older, black, Hispanic, not married, uninsured or Medicaid-insured, as well as much lower percentages of cases living in a high poverty level census tract than the rest of New Jersey (P < .001; Table 3). The clusters also contained higher percentages of API cases than the rest of New Jersey. The populations in clusters 2 and 3 had lower percentages of blacks, Hispanics, persons with less than a high school education, unmarried persons, unemployed persons, renter occupied housing, and families with incomes below poverty than the population in the rest of New Jersey. The percentages of foreign-born persons, people speaking an Indo-European or API language at home, and persons who speak English less than well was higher, as was the per capita income, in these 2 clusters compared with the population in the rest of New Jersey (Table 4).
TABLE 4. Population Characteristics in the Geographic Areas With Significantly Higher Proportions of Breast Cancer Cases Diagnosed In Situ Versus the Rest of New Jerseya.
| Characteristic | Cluster 2b | Cluster 3b | Rest of New Jersey | New Jersey |
|---|---|---|---|---|
| Total population | 669 428 | 1 942 511 | 6 038 609 | 8 650 548 |
| Women 20 and older | 260 746 | 725 315 | 2 316 584 | 3 302 645 |
| Black racec | 7.4% | 11.8% | 16.1% | 14.4% |
| Hispanic ethnicity | 12.9% | 12.1% | 17.5% | 15.9% |
| Foreign-born persons | 28.0% | 21.0% | 18.3% | 19.7% |
| Language spoken at home (age 5 y and older) | ||||
| Spanish | 9.7% | 8.2% | 9.7% | 9.4% |
| Indo-Europeand | 9.2% | 9.3% | 6.4% | 7.3% |
| Asian or Pacific Islandere | 10.0% | 5.1% | 2.5% | 3.6% |
| Speak English less than well | 10.7% | 8.8% | 7.9% | 8.3% |
| Education (age 25 y and older) | ||||
| Less than high school education | 8.3% | 9.9% | 14.8% | 13.2% |
| Marital status (women age 15 y and older) | ||||
| Now married | 54.8% | 52.3% | 46.6% | 48.5% |
| Economic status | ||||
| Unemployed (age 16 y and older) | 5.1% | 5.9% | 7.5% | 7.0% |
| Housing that is renter occupied | 29.4% | 26.4% | 35.2% | 32.9% |
| Family income below poverty | 3.8% | 4.3% | 8.2% | 7.0% |
| Per capita income | $44 664 | $40 519 | $31 541 | $34 571 |
aData are based on the American Community Survey 2005-2009, US Census Bureau.
bClusters 2 and 3 were identified by SaTScan software as having significantly elevated proportions of in situ breast cancers during 2004 to 2011 for cluster 2 and during 2006 to 2011 for cluster 3 (P < .001).
cFrom 1 race or from 2 or more races.
dIncludes Greek, Russian, Polish, Serbo-Croatian, other Slavic languages, Hindi, and other Indic languages.
eIncludes Chinese, Japanese, Korean, other Asian languages, Tagalog, Hawaiian, and other Pacific Island languages.
Discussion
This study identified an area in northeastern New Jersey (cluster 1) with a significantly elevated proportion of breast cancer diagnosed at the distant stage, which occurred over the entire 15-year study period (1997-2011). This is consistent with the results of our previous study that found 2 significant clusters with high proportions of breast cancer cases diagnosed at the distant stage from 1995 through 1997, also in northeastern New Jersey (parts of Bergen, Hudson, and Essex counties).20 The current cluster includes these same 3 counties and extends into 2 additional counties to the south. In 1995 to 1997, 13% and 9% of the cases in the 2 clusters were diagnosed at the distant stage versus 5% in the rest of New Jersey.20 Later, in 1997 to 2011, 6.1% of the cases in the cluster compared with 4.7% of the cases in the rest of New Jersey were diagnosed at the distant stage. The apparent narrowing gap suggests improvement in screening and early detection of breast cancer. It is not likely due to large demographic and SES changes in the cases and populations, as the demographic and SES characteristics in the 2 studies' cluster areas were similar with high percentages of minority (black, Hispanic) and low SES breast cancer cases and populations.
This study also identified 2 clusters with significantly elevated proportions of in situ breast cancer, 1 in northeastern New Jersey from 2004 through 2011 (cluster 2) and the other in central New Jersey from 2006 through 2011 (cluster 3). The demographic and SES characteristics of the cases and populations in these 2 clusters also are very different from the rest of New Jersey, but with fewer blacks and Hispanics and higher SES. The proportion of female breast cancer cases diagnosed in situ increased statewide from 16.8% in 1997 to 23.9% in 2011.30 However, our findings show that in large areas of the state the percentage of breast cancer diagnosed in situ has not increased as much as in the 2 in situ cluster areas (clusters 2 and 3) in recent years (2004-2011). The disparity in stage at diagnosis is especially noticeable in the parts of the 3 counties in which the in situ breast cancer clusters overlap with the distant stage breast cancer cluster. Perhaps a better understanding of why women in clusters 2 and 3 have experienced higher rates of in situ breast cancer diagnosis can be applied to increasing early diagnosis of breast cancer in the other areas of the state.
A previous study with space-time analysis (SaTScan) of 1988-1997 data in Massachusetts found one significant cluster with a high proportion of breast cancer diagnosed at the distant stage in a mostly urban area south of Boston during 1988 to 1990.13 When adjusted for SES alone or adjusted for SES and urban/rural status together, this cluster was significant only in 1989. The cluster was no longer significant when adjusted only for urban/rural status and there were no clusters of high proportions of distant stage breast cancer after 1990. Another study analyzed the proportion of in situ breast cancer in four 5-year time periods between 1981 and 2000 in a Wisconsin county. From 1986 to 1990, significantly higher percentages of cases with urban and suburban zip codes were diagnosed in situ compared with cases in rural zip codes.12 By 1996 to 2000, urban, suburban, and rural zip codes throughout the county had similar percentages of in situ breast cancer cases. Both of these studies found no significant geographic disparities in breast cancer stage at diagnosis in their more recent study years, that is, the 1990s. In this NJ study, however, geographic disparities in breast cancer stage at diagnosis proportions persisted into the 2000s for distant stage and began in the 2000s for in situ.
Also noticeable is that while the populations in the distant stage cluster and 2 in situ stage clusters in this study all have higher proportions of foreign-born persons, persons who speak a language other than English at home, and persons who speak English less than well compared with the population in the rest of New Jersey, the specific racial and ethnic population compositions differ. The population in the distant stage cluster has a much higher proportion of Hispanics and people who speak Spanish at home than the populations in the in situ clusters, while the populations in the in situ clusters have much higher percentages of persons speaking an API language at home than the distant stage cluster population. This suggests that other factors associated with specific races and ethnicities are more important to being diagnosed with breast cancer at the in situ or distant stage than simply being foreign born or not speaking English well. Other research has shown that inability to pay for screening, lack of knowledge about or provider recommendations for screening, no routine health care, and unavailability of culturally acceptable services may be involved.20
Strengths and limitations
Strengths of this study include the use of a population-based, high-quality cancer registry, a large data set covering 15 years, and a well-established approach to spatial-temporal analysis. The SaTScan software is free, easy to use, well-maintained, and supported and widely used. Thus, our methodology can be replicated, with some caveats,31 in other states and jurisdictions with population-based cancer registries to better identify priority areas for breast cancer control efforts.
Potential limitations of this type of study include exclusions due to an inability to geocode cases to a census tract and errors in geocoding. Relatively few cases (n = 360; 0.3%) were excluded because of geocoding problems and, although geocoding errors may have occurred, they would not have significantly affected the results if the errors involved small distances because the clusters are relatively large.
Another limitation was the lack of data at the individual level on demographic and SES factors of interest, such as education, income, employment, and language, as they are not routinely collected by population-based cancer registries. To compensate, we compared populations in the clusters with the rest of New Jersey using US Census 2005-2009 American Community Survey demographic and SES data. However, the populations' demographic and SES factors may have changed over time, especially in cluster 1, the distant stage cluster, which included 15 years of cases (1997-2011). To address this potential bias, we compared the race and ethnic distributions in cluster 1 between the 2000 Census and the 2005-2009 American Community Survey. We found that the percentages of the cluster population that were black and Hispanic increased between the 2000 US Census (23.6% and 26.5%, respectively) and the 2005-2009 American Community Survey (24.8% and 30.3%, respectively). However, the proportion of blacks and Hispanics in the rest of New Jersey's population also increased between 2000 and 2005-2009, blacks from 9.8% to 11.0%, and Hispanics from 8.6% to 11.1%.
We did not investigate changes in insurance status during the study period (1997-2011) and between the earlier study20 and this study, a potential question for future research, especially given recent changes due to the Affordable Care Act. Another factor of interest is the screening history of the breast cancer cases, particularly those diagnosed at the distant stage. The NJSCR does not include mammography screening information, and publicly available screening data are not available at the census tract level (for example, Behavioral Risk Factor Surveillance System data). Identification of screening data to link with breast cancer cases is another potential research topic.
Breast cancer molecular subtype, that is, hormone receptor/human growth factor-neu receptor (HR/HER2) expression, is another factor that we were unable to account for in this study. There is a growing body of research suggesting that non-Hispanic black women are at higher risk for a more aggressive type of breast cancer, ER-/HER2- (triple negative),32,33 which may not be detected at as early a stage as less aggressive types. Thus, higher rates of triple negative breast cancers among non-Hispanic black women also may have contributed to the elevated proportion of distant stage disease in cluster 1. More research is needed to assess this possibility.
Implications for Policy & Practice
Our findings show that more attention to breast cancer education and screening are needed throughout New Jersey to increase the proportion of in situ and decrease the proportion of distant stage breast cancer diagnosed statewide.
These services are especially needed in the geographic area with a significantly higher proportion of breast cancer diagnosed at the distant stage, as well as in the geographic areas outside the clusters with significantly high proportions of breast cancer diagnosed in situ.
We have begun to share our findings with cancer control partners within the New Jersey Department of Health– for example, Office of Cancer Control and Prevention and Cancer Education and Early Detection (CEED) Program, partially funded by CDC's National Breast and Cervical Cancer Education and Detection Program.
Through these partners, we hope to reach the county-based Chronic Disease Coalitions, CEED Lead Agencies, and other health agencies and professionals to inform breast cancer education and screening programs at the local level.
On a policy level, these findings can be used by legislative and public health authorities in resource allocation– for example, for the CEED Program.
They may also be used by Office of Cancer Control and Prevention to evaluate New Jersey's progress on “Healthy New Jersey 2020”7 objectives relating to breast cancer stage at diagnosis and screening.
Footnotes
Cancer Epidemiology Services, including the New Jersey State Cancer Registry, receives financial support from Surveillance, Epidemiology, and End Results Program of the National Cancer Institute, National Institutes of Health, under contract HHSN 261201300021I and control No. N01-PC-2013-00021; National Program of Cancer Registries, Centers for Disease Control and Prevention, under cooperative agreement 5U58DP003931; Preventive Health and Health Services Block Grant, Centers for Disease Control and Prevention, under grant 4230-215-037140-12; the State of New Jersey and Rutgers Cancer Institute of New Jersey.
The authors declare no conflicts of interest.
References
- 1.American Cancer Society. Cancer Facts & Figures 2016. Atlanta, GA: American Cancer Society; 2016. [Google Scholar]
- 2.New Jersey State Cancer Registry, Cancer Epidemiology Services, New Jersey Department of Health. Invasive cancer incidence rates by county in New Jersey, female breast, 2009-2013. http://nj.gov/health/ces/. Accessed May 16, 2016.
- 3.New Jersey State Cancer Registry, Cancer Epidemiology Services, New Jersey Department of Health. Cancer mortality rates by county in New Jersey, female breast, 2008-2012. http://nj.gov/health/ces/. Accessed May 16, 2016.
- 4.Niu X, Roche LM, Pawlish K, Stroup A. Cancer Survival in New Jersey, 1979-2005. Trenton: Cancer Epidemiology Services, New Jersey Department of Health; September 2014. http://nj.gov/health/ces/index.shtml. Accessed November 5, 2014. [Google Scholar]
- 5.US Preventive Services Task Force; Breast cancer: screening, recommendation summary. September 2014. http://www.uspreventiveservicestaskforce.org. Accessed November 17, 2014. [Google Scholar]
- 6.Office of Disease Prevention and Health Promotion, Centers for Disease Control and Prevention. Healthy People 2020—Cancer. http://www.healthypeople.gov/2020/topics-objectives/topic/cancer. Accessed November 17, 2014.
- 7.New Jersey Department of Health. Healthy New Jersey 2020—cancer. http://nj.gov/health/chs/hnj2020/documents/objectives/. Accessed November 17, 2014.
- 8.Jafari-Koshki T, Schmid VJ, Mahaki B. Trends of breast cancer incidence in Iran during 2004-2008: a Bayesian space-time model. Asian Pac J Cancer Prev. 2014;15:1557–1561. [DOI] [PubMed] [Google Scholar]
- 9.Vieira VM, Webster TF, Weinberg JM, Aschengrau A. Spatial-temporal analysis of breast cancer in upper Cape Cod, Massachusetts. Int J Health Geogr. 2008;7:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crabbe JCF, Gregorio DI, Samocluk H, Swede H. Secular trends, race, and geographic disparity of early-stage breast cancer incidence: 25 years of surveillance in Connecticut. Am J Public Health. 2015;105(suppl 3):e64–e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hsu CE, Jacobson H, Mas FS. Evaluating the disparity of female breast cancer mortality among racial groups—a spatiotemporal analysis. Int J Health Geogr. 2004:3:4 http://www.ij-healthgeographics.com/contents/3/1/4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McElroy JA, Remington PL, Gangnon RE, Hariharan L, Andersen LD. Identifying geographic disparities in the early detection of breast cancer using a geographic information system. Prev Chronic Dis. January 2006:3(1):A10 http://www.cdc.gov/pcd/issues/2006/jan/05_0065.htm. [PMC free article] [PubMed] [Google Scholar]
- 13.Sheehan TJ, DeChello LM. A space-time analysis of the proportion of late stage breast cancer in Massachusetts, 1988 to 1997. Int J Health Geogr. 2005;4:15 http://www.ij-healthgeographics.com/content/4/1/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goovaerts P. Analysis of geographical disparities in temporal trends of health outcomes using space-time joinpoint regression. Int J Appl Earth Obs Geoinf. 2013;22:75–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goovaerts P, Xiao H. The impact of place and time on the proportion of late-stage diagnosis: the case of prostate cancer in Florida, 1981-2007. Spat Spatiotemporal Epidemiol. 2012;3:243–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kulldorff M, Athas WF, Feuer EJ, Miller BA, Key CR. Evaluating cluster alarms: a space-time scan statistic and brain cancer in Los Alamos, New Mexico. Am J Public Health. 1998;88:1377–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nkhoma ET, Hsu CE, Hunt VI, Harris AM. Detecting spatiotemporal clusters of accidental poisoning mortality among Texas counties, U.S., 1980-2001. Int J Health Geogr. 2004;3:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chiu Y-W, Hsu CE, Wang M-Q, Nkhoma ET. Examining geographic and temporal variations of AIDS mortality: evidence of racial disparities. J Natl Med Assoc. 2008;100:788–796. [DOI] [PubMed] [Google Scholar]
- 19.Chiu Y-W, Wang M-Q, Chuang H-Y, Hsu CE, Nkhoma ET. A new application of spatiotemporal analysis for detecting demographic variations in AIDS mortality: an example from Florida. Kaohsiung J Med Sci. 2008;24:568–575. [DOI] [PubMed] [Google Scholar]
- 20.Roche LM, Skinner R, Weinstein RB. Use of a geographic information system to identify and characterize areas with high proportions of distant stage breast cancer. J Public Health Manage Pract. 2002;8:26–32. [DOI] [PubMed] [Google Scholar]
- 21.Tarlov E, Zenk SN, Campbell RT, Warnecke RB, Block R. Characteristics of mammography facility locations and stage of breast cancer at diagnosis in Chicago. J Urban Health. 2008;86:196–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fritz A, Percy C, Jack A, et al. , eds. International Classification of Diseases for Oncology, 3rd ed. Geneva, Switzerland: World Health Organization; 2000. [Google Scholar]
- 23.Young JL, Jr, Roffers SD, Ries LAG, et al. SEER Summary Staging Manual—2000: Codes and Coding Instructions, NIH Publication Number 01-4969. Bethesda, MD: National Cancer Institute; 2001. [Google Scholar]
- 24.Adamo MB, Johnson CH, Ruhl JL, et al. , eds. SEER Program Coding and Staging Manual, NIH Publication number 10-5581. Bethesda, MD: National Cancer Institute; 2010. [Google Scholar]
- 25.SEER*DMS tutorials. http://seer.cancer.gov/seerdms/tutorials/geocoding.seerdms.V13.pdf. Accessed November 10, 2014.
- 26.SEER Site Recode ICD-O-3 (1/27/2003) Definition, Surveillance Epidemiology and End Results. http://seer.cancer.gov/siterecode/icdo3-d01272003/. Accessed May 30, 2012.
- 27.Kulldorff M. A spatial scan statistic. Comm Stat Theory Methods. 1997;26:1481–1496. [Google Scholar]
- 28.Kulldorff M, Huang L, Pickle L, et al. An elliptical spatial scan statistic. Stat Med. 2006;25:3929–3943. [DOI] [PubMed] [Google Scholar]
- 29.2005-2009 American Community Survey 5-Year Estimates. http://factfinder2.census.gov/.
- 30.New Jersey State Cancer Registry, New Jersey Department of Health. September 2014. Analytic File. Trenton, New Jersey. Accessed October 20, 2014. [Google Scholar]
- 31.Sherman RL, Henry KA, Tannenbaum SL, Feaster DJ, Kobetz E, Lee DJ. Applying spatial analysis tools in public health: an example using SaTScan to detect geographic targets for colorectal cancer screening interventions. Prev Chronic Dis. 2014;11:130264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kohler BA, Sherman RL, Howlader N, et al. Annual report to the nation on the status of cancer, 1975-2011, featuring incidence of breast cancer subtypes by race/ethnicity, poverty and state. J Natl Cancer Institute. 2015;107:djvo48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parise CA, Caggiano V. Disparities in race/ethnicity and socioeconomic status: risk of mortality of breast cancer patients in the California Cancer Registry, 2000-2010. BMC Cancer. 2013;13:449. [DOI] [PMC free article] [PubMed] [Google Scholar]