Background:
Plastic surgeons routinely see patients with complex or chronic wounds of all etiology. In a previous study, we found that up to 1 in 4 of these patients is at risk for malnutrition, which may be influencing their ability to heal. The goal of this study was to develop and validate a universal screening protocol that would be fast and accurate and allow for effective intervention and optimization of nutrition before plastic surgery.
Methods:
To accomplish these goals, we adopted a 2-part screening algorithm using the Canadian Nutritional Screening Tool (CNST) to triage patients in our outpatient clinics and then further screened those identified as being at risk using the Subjective Global Assessment (SGA) tool and blood work.
Results:
We screened 111 patients with diagnoses related to breast cancer (n = 10; 9.01%), elective surgery (n = 38; 34.23%), emergency surgery (n = 8; 7.21%), fractures (n = 15; 13.51%), and wounds (n = 40; 36.04%). Of the screened subjects, 15.32% (n = 17) were found to be at nutritional risk using the CNST, and 13 were confirmed to be moderately or severely malnourished using the SGA. Importantly, there were no positive correlations between nutritional status and smoking, diabetes, body mass index, or age, indicating that a universal screening protocol is needed to effectively screen a diverse plastic surgery population for malnutrition.
Conclusions:
Screening patients with both the CNST and the SGA is an effective way to identify patients before surgery to improve outcomes.
INTRODUCTION
Malnutrition is a well-recognized issue in the acute care setting with a prevalence ranging from 30% to 45%, and elderly individuals are recognized to be most at risk.1–3 The consequence of malnutrition is impaired wound healing, decreased cardiac and respiratory functions, and negative health outcomes that often result in prolonged length of hospital stays.4–9 In fact, it is estimated that malnourished patients account for approximately 27% of surgical patients admitted to hospitals.10 Identification of nutritional deficiency, especially within the surgical field, is crucial to improve outcomes,10 as malnourished patients are 60% more likely to be readmitted to hospital within 15 days and have increased mortality (50% versus 10% for well-nourished patients) in the first 3 years postdischarge.11 Significantly higher in-hospital costs have also been reported for malnourished patients.11,12
Because nutritional status is so important to outcomes, a number of different tools have been developed for universal screening purposes (the Mini Nutritional Assessment for the elderly, the Malnutrition Universal Screening Tool (MUST), and the Nutritional Risk Score among others13). However, these tools range in complexity and length, and there is currently no consensus in the Canadian Healthcare system as to the best screening tool for routine use. We recently used the Canadian Nutritional Screening Tool (CNST) to profile the nutritional status of the plastic surgery outpatient population at a busy urban tertiary care centre in Toronto, ON.14 In that study, we found that almost 1 in 4 of our patients were at nutritional risk, cementing the need for universal nutritional screening in our clinical practice. In that study, we found the CNST to be an easily implemented rapid screen for nutritional risk with the potential for universal implementation. However, we were concerned that this tool was not capturing enough information about a patient’s nutritional status if they were found to be at risk. As a next step, we have now created a routine nutritional screening algorithm based on the Integrated Nutrition Pathway for Acute Care and recommendations of the American Society for Parenteral and Enteral Nutrition.1,15 We now report the screening of an additional 111 patients by triaging first with the CNST and secondarily (in those at risk by CNST screen) with the more comprehensive Subjective Global Assessment (SGA) tool. The results of our SGA-based screening support the findings of the CNST, suggesting that universal screening using this easily implemented 2-part screening system would accurately identify those patients at nutritional in our plastic surgery population and allow us to improve outcomes through optimization of nutritional status.
METHODS
Setting
This cross-sectional study was approved by the St. Michael’s Hospital Research Ethics Board (REB16-266) before initiation of recruitment. Enrolment took place at St Michael’s Hospital, Toronto, from October until December 2016. Eligibility criteria included (1) referral to a plastic surgeon for assessment of a wound or other surgical concern, (2) ability and willingness to consent, and (3) age above 18 years. Informed and voluntary consent was obtained for all participants.
Survey Instruments
The CNST is a 2-question validated nutritional screening tool, designed to allow rapid nutritional screening by nonspecialists.16 The CNST has been shown to have good sensitivity (91.7%) and specificity (74.8%) in Canadian adult inpatients.16 The SGA, our selected assessment tool, includes a history and physical examination and has a nonnumerical weighing scheme prioritizing certain elements like percentage weight loss and obvious physical signs of malnutrition.17 The SGA has been known for its relevance for predicting clinical outcome and previous use in surgical populations.13,18
Data Collection and Reporting
Data collection took place in the St Michael’s Hospital outpatient clinic. Two trained research assistants recruited patients to the study, obtained their informed, voluntary, and written consent, and collected the first nutritional screening data using the CNST. For purpose of standardization, 1 research assistant trained with a dietician and used the SGA to screen selected patients identified as being at nutritional risk by the CNST as per our study algorithm (Fig. 1). The algorithm selected for this study follows the recommendations developed from the Integrated Nutrition Pathway for Acute Care in that only patients identified at nutritional risk were further assessed with the SGA.1 Participants identified as being at nutritional risk were then invited to be evaluated with the SGA17 and were given blood work requisitions and asked to undergo micronutrient analysis (vitamin D, E, C, A, B12, selenium, zinc, rbc, folate, ferritin, iron stores, and prealbumin), and referred to a hospital dietician.
Fig. 1.
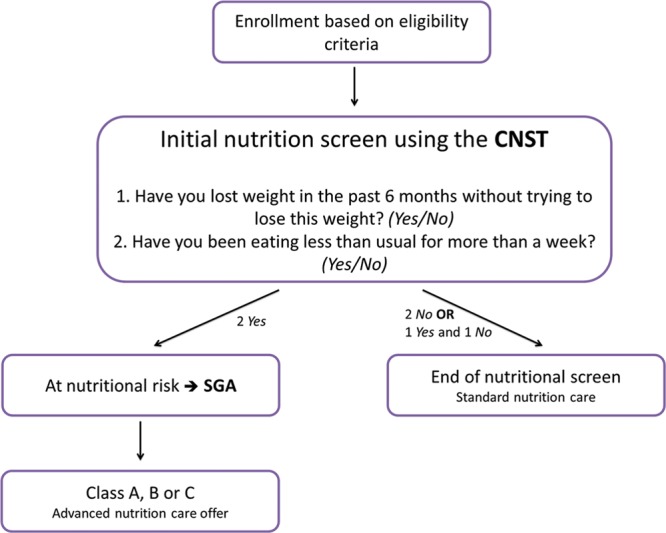
Nutritional screening algorithm used in our study.
The primary objective of this study was to validate the diagnostic accuracy of the CNST in our patient population using the SGA. The secondary objective was to describe the characteristics of the plastic surgery patient population identified as being at nutritional risk. In that regard, categorical and continuous variables were presented as means (%).
RESULTS
Accuracy of the CNST
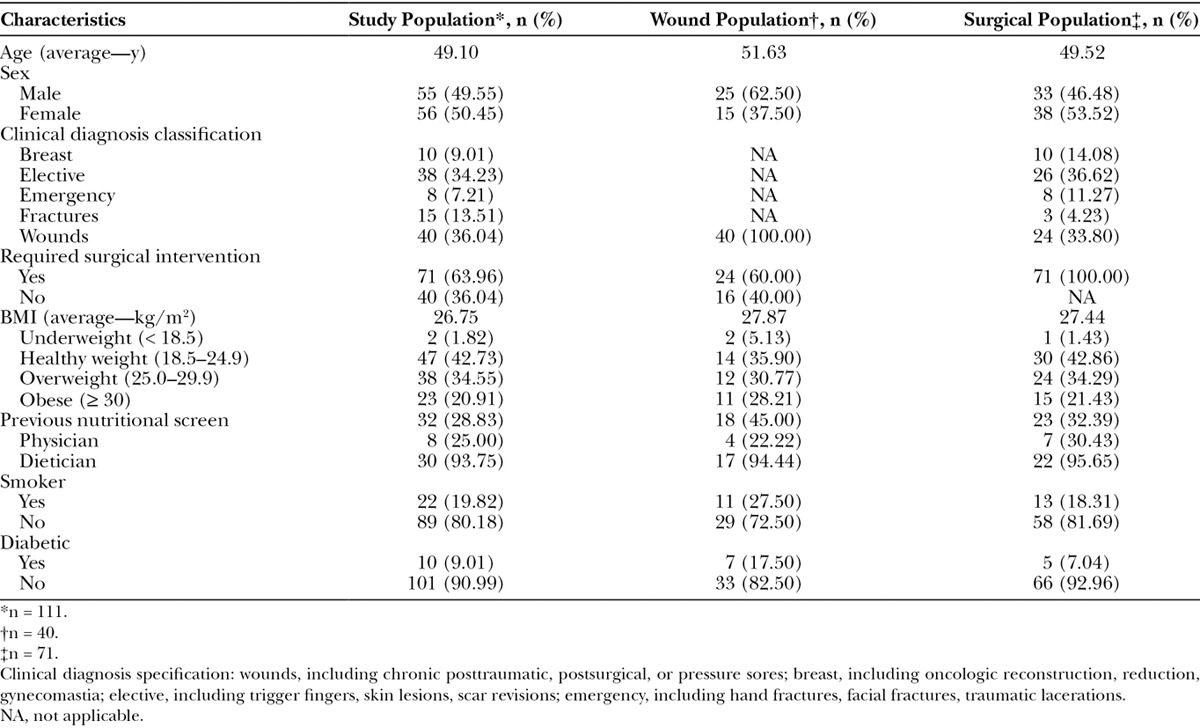
We adopted a 2-part screening protocol for this study, using the CNST to triage patients and the SGA to validate outcome. A total of 111 patients were surveyed with this protocol over a period of 3 months, with an average age of 49 years and average body mass index (BMI) of 26.75 kg/m2 (Table 1). There were a total of 55 men and 56 women. Of the enrolled participants, 71 (63.97%) had a surgical diagnosis and had undergone or were planning to undergo a surgical procedure. The remaining 40 (36.04%) patients were seeing a plastic surgeon because of a subacute or chronic wound diagnosis. This patient population differed from that in our previous study,14 which was more heavily weighted with diabetic foot wounds. Instead, this study focused on including a more medically diverse patient population.
Table 1.
Demographic and Clinical Characteristics of Patients Assessed in the Plastic Surgery Outpatient by Subgroups
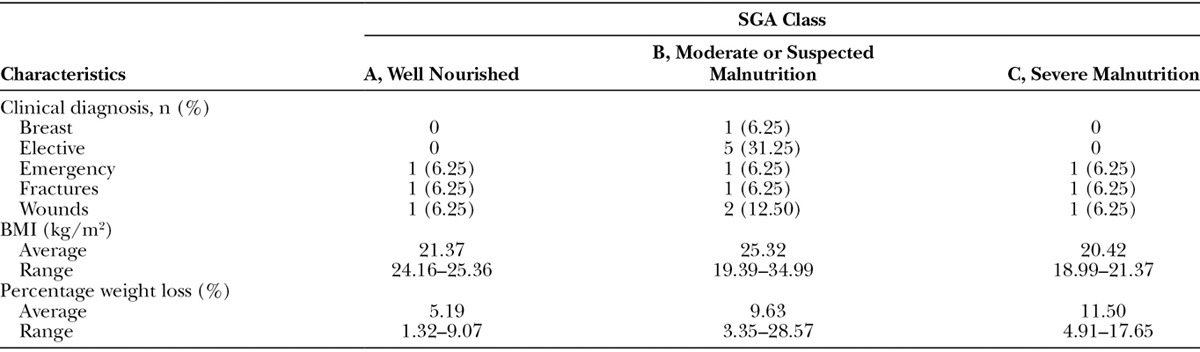
The CNST identified 17 (15.32%) patients from our sample of 111 at nutritional risk (Table 2). The SGA was performed on 16 of these patients, with 1 refusal. The SGA confirmed the nutritional diagnosis in 13/16 patients: 10 were found to be moderately malnourished (SGA class B) and 3 were found to be severely malnourished (SGA class C; Table 3). These results suggest that the CNST overpredicts nutritional risk in 18.75% of cases but is generally an accurate predictor of macronutrient deficiency in a diverse plastic surgery patient population.
Table 2.
Canadian Nutritional Screening Tool Responses, *n = 111
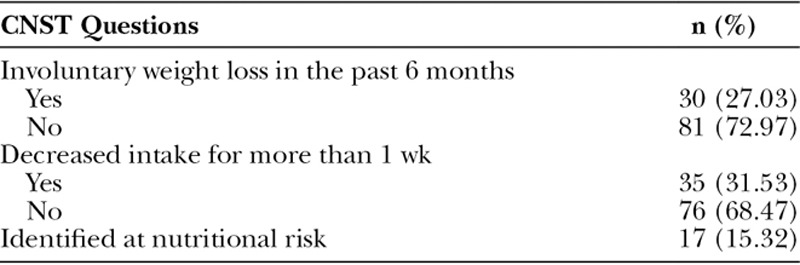
Table 3.
Classification of Subjective Global Assessments, *n = 16
Malnourished Population
The patients identified as at risk for malnutrition by the CNST ranged in age from 24 to 86 years (mean, 46.2 years) and were equally split between genders (8 males and 9 females). The average BMI of at risk individuals was 21.37 (± 4.76). Of note, 3 individuals had BMIs of > 30 (classified as obese), 2 patients had BMIs of 25–30 (classified as overweight), and the remainder had BMIs in the 18.5–24.99 range (classified as normal; Table 3). This result suggests that preconceived notions as to how a malnourished individual looks should be challenged—these patients were not underweight (and some were in fact obese). Also of note, only 2 of our at-risk patients were diabetics, and there was no correlation between smoking status and malnutrition.
We also examined our at-risk population by subcategorizing patients according to clinical diagnosis. Patients were categorized as breast (including oncologic reconstructions, reductions, gynecomastia), elective (including trigger fingers, skin lesions, scar revisions), emergency (including traumatic lacerations, amputations, foreign bodies), fractures (including craniofacial and hands), and wounds (including pressure sores, subacute to chronic posttraumatic, subacute to chronic postsurgical). The number of patients per subcategory identified by the CNST as being at nutritional risk was variable (Table 1), with surprisingly few patients at nutritional risk in the wound cohort (4/40; 10%). Of those wound patients, only 1 was a diabetic. Importantly, examining the breakdown of patients according to clinical diagnosis suggests that 14 patients were seeing the plastic surgeon for wounds or elective surgeries could have benefitted from a nutritional program leading up to their clinic visit, and 3 could have benefitted from optimized nutrition following trauma.
Micronutrient Analysis
The CNST and SGA both screen for macronutrient (protein, carbohydrate, and fats) deficiencies, but wound healing is also affected by deficiencies in micronutrients (vitamins and minerals). Of the patients with confirmed macronutrient deficiencies, we found 1 patient who also had iron deficient anemia (iron low (3 µmol/L), RBC low (3.36 × 1012/L), Hg low (103 g/L), vitamin A low (0.8 µmol/L), 1 patient with selenium borderline low (1.3 µmol/L), and low vitamin C (17 µmol/L), and a final patient with low vitamin C (15 µmol/L). We also identified a patient who is likely oversupplementing their diet, as they had elevated levels of folate and vitamins E, A, and B12. We unfortunately had a response rate of only 8/16 patients given requisitions for blood work, and therefore the number of patients with micronutrient deficiencies may have been higher. Regardless, these results suggest that patients identified as being at risk for macronutrient deficiencies are also at risk for micronutrient deficiencies and should be screened accordingly.
Age
Nutritional status often declines with age,19,20 and we therefore also subdivided our patient population by age (< 50 years and ≥ 50 years). We found no age-related increase in nutritional risk: the frequency of malnutrition in patients < 50 years was 16.1% (14/87 patients) and in those ≥ 50 years 12.5% (3/24 patients). Interestingly, the 3 patients ≥ 50 years identified at nutritional risk were all seeing the plastic surgeon as a result of pressure sores on the sacrum, ischium, or coccyx. Although this sample size is too small to evaluate the significance of this finding, it is of note that other studies have shown that nutritional variables can predict the development of pressure sores.21 Albumin levels were one of the most significant independent predictors of poor wound healing outcomes in chronic wounds.4,22 However, we did not identify any individuals who had albumin levels outside the normal range (3.0–51.0 g/L).
DISCUSSION
Patients being referred to the plastic and reconstructive surgery outpatient clinics present with diverse diagnoses. It is well established that optimizing perioperative patients’ healing involves addressing nutritional deficiencies, but there is little consensus as to what screening tool should be used for routine assessment. Our study was designed to follow up on previous work indicating that we have high rates of malnutrition in our plastic surgery population, with the goal of defining a nutritional screening system for routine use in all our outpatients. To be of use for universal screening, our tool must be (1) rapid to administer, translating into universal implementation and (2) accurate, such that few false-positives/negatives would waste clinical resources. Given the success we had using the CNST in our first study, we triaged patients in the current study using the CNST first and then classified those at nutritional risk more thoroughly using a secondary tool (the SGA) and micronutrient analysis. Such a 2-part screen is supported by the American Society for Parenteral and Enteral Nutrition15 and offers both good screening accuracy and ease of implementation. Our experience in both our previous study and the current study suggests that the CNST can be completed in less than 1 minute and therefore fulfills our first criteria. The SGA has been previously validated in surgical populations13,18 and in our hands confirmed the CNST’s findings in approximately 80% of cases (satisfying the second criteria). Adding blood work for micronutrient analysis to the workup of patients at risk adds depth to our nutritional assessment and allows for tailored and specific optimization before surgery. Our experience in this study confirms that nutritional screening in the outpatient clinic setting is feasible, innovative, and necessary for holistic patient care.
Beyond validating the nutritional screen itself, we were interested in identifying characteristics of our patient population at nutritional risk. Of the patients participating in this study, 71 (63.96%) were in clinic for a surgical intervention and 40 (36.04%) had a wound diagnosis. The CNST identified 17 patients at nutritional risk, the majority of who were moderately or severely malnourished (10 patients SGA class B and 3 SGA class C). Most of these patients were seeing the plastic surgeon for an elective procedure, which indicates an opportunity for optimization before surgery. Importantly, only 2 patients of our entire patient cohort (1.82%) were found to be underweight (< 18.5) as per the World Health Organization’s classification but were not found to be at nutritional risk. This discrepancy between BMI and nutritional status underscores the importance of universal nutritional screening in an outpatient setting, as overt signs of malnutrition are easily missed.
Even more easily missed are micronutrient imbalances that can impact cellular functions including immunity and wound healing.23 The antioxidant vitamins A, E, K, and C have roles in eliminating prooxidants, scavenging free radicals and maintaining an essential balance between oxidative stress and antioxidants.23,24 Vitamin C is also a catalyst required in the synthesis of collagen part of new tissue creation and wound healing processes.23 Micronutrient deficiencies impact the elderly most often and are usually deficiencies in vitamin D, zinc, and vitamin B12 (cobalamine)25,26 in that population. Unfortunately, our study was limited by sample size and we did not have a sufficient response rate to compare the micronutrient status of our patients according to age. We did however identify 3 patients with deficiencies in micronutrients important to wound healing, including vitamin C. In a follow-up study, we aim to profile the micronutrient status of more patients undergoing outpatient plastic surgeries in a multicenter setting.
CONCLUSIONS
Screening all patients attending plastic surgery outpatient clinics for nutritional status has the potential to improve patient outcomes significantly. In our case, we identified 15% of our patients who were at risk for poor healing due to nutrient deficiency and could have benefitted from nutritional coaching/intervention before surgery. By screening patients with both the CNST and the SGA, we captured the nutritional status of a large number of patients and carefully profiled those at risk. This screening system will be validated in a follow-up multicenter study in a larger patient population to allow us to draw further conclusions about micronutrient deficiencies in our population.
Footnotes
Disclosure: Supported by a research grant from the AFP Innovation Fund (Ontario, Canada). The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Keller HH, McCullough J, Davidson B, et al. The Integrated Nutrition Pathway for Acute Care (INPAC): building consensus with a modified Delphi. Nutr J. 2015;14:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vanderwee K, Clays E, Bocquaert I, et al. Malnutrition and nutritional care practices in hospital wards for older people. J Adv Nurs. 2011;67:736–746.. [DOI] [PubMed] [Google Scholar]
- 3.Allard JP, Keller H, Jeejeebhoy KN, et al. Malnutrition at hospital admission-contributors and effect on length of stay: a prospective cohort study from the Canadian Malnutrition Task Force. JPEN J Parenter Enteral Nutr. 2016;40:487–497.. [DOI] [PubMed] [Google Scholar]
- 4.Molnar JA, Underdown MJ, Clark WA. Nutrition and chronic wounds. Adv Wound Care (New Rochelle). 2014;3:663–681.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Webb JG, Kiess MC, Chan-Yan CC. Malnutrition and the heart. CMAJ. 1986;135:753–758.. [PMC free article] [PubMed] [Google Scholar]
- 6.Ghignone M, Quintin L. Malnutrition and respiratory function. Int Anesthesiol Clin. 1986;24:65–74.. [DOI] [PubMed] [Google Scholar]
- 7.Neumayer LA, Smout RJ, Horn HG, et al. Early and sufficient feeding reduces length of stay and charges in surgical patients. J Surg Res. 2001;95:73–77.. [DOI] [PubMed] [Google Scholar]
- 8.Studley HO. Percentage of weight loss: a basic indicator of surgical risk in patients with chronic peptic ulcer. 1936. Nutr Hosp. 2001;16:141–143; discussion 140.. [PubMed] [Google Scholar]
- 9.Bistrian BR, Blackburn GL, Hallowell E, et al. Protein status of general surgical patients. JAMA. 1974;230:858–860.. [PubMed] [Google Scholar]
- 10.Ho JW, Wu AH, Lee MW, et al. Malnutrition risk predicts surgical outcomes in patients undergoing gastrointestinal operations: results of a prospective study. Clin Nutr. 2015;34:679–684.. [DOI] [PubMed] [Google Scholar]
- 11.Lim SL, Ong KC, Chan YH, et al. Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin Nutr. 2012;31:345–350.. [DOI] [PubMed] [Google Scholar]
- 12.Curtis LJ, Bernier P, Jeejeebhoy K, et al. Costs of hospital malnutrition. Clin Nutr. 2016; Sep 19. pii: S0261–5614(16)31247X.. [DOI] [PubMed] [Google Scholar]
- 13.van Bokhorst-de van der Schueren MA, Guaitoli PR, Jansma EP, et al. Nutrition screening tools: does one size fit all? A systematic review of screening tools for the hospital setting. Clin Nutr. 2014;33:39–58.. [DOI] [PubMed] [Google Scholar]
- 14.Yu J, Hunter PJ, Perry JA, et al. Plastic surgery patients are malnourished: utilizing the Canadian malnutrition screening tool. Plast Reconstr Surg Glob Open. 2016;4:e1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mueller C, Compher C, Ellen DM; American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Board of Directors. A.S.P.E.N. clinical guidelines: nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enteral Nutr. 2011;35:16–24.. [DOI] [PubMed] [Google Scholar]
- 16.Laporte M, Keller HH, Payette H, et al. Validity and reliability of the new Canadian Nutrition Screening Tool in the ‘real-world’ hospital setting. Eur J Clin Nutr. 2015;69:558–564.. [DOI] [PubMed] [Google Scholar]
- 17.Detsky AS, McLaughlin JR, Baker JP, et al. What is subjective global assessment of nutritional status? JPEN J Parenter Enteral Nutr. 1987;11:8–13.. [DOI] [PubMed] [Google Scholar]
- 18.Baker JP, Detsky AS, Wesson DE, et al. Nutritional assessment: a comparison of clinical judgement and objective measurements. N Engl J Med. 1982;306:969–972.. [DOI] [PubMed] [Google Scholar]
- 19.Forster S, Gariballa S. Age as a determinant of nutritional status: a cross sectional study. Nutr J. 2005;4:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gaggiotti G, Orlandoni P, Ambrosi S, et al. The influence of age and sex on nutritional parameters in subjects aged 60 years and over. Arch Gerontol Geriatr. 1995;20:117–128.. [DOI] [PubMed] [Google Scholar]
- 21.Hengstermann S, Fischer A, Steinhagen-Thiessen E, et al. Nutrition status and pressure ulcer: what we need for nutrition screening. JPEN J Parenter Enteral Nutr. 2007;31:288–294.. [DOI] [PubMed] [Google Scholar]
- 22.Stechmiller JK. Understanding the role of nutrition and wound healing. Nutr Clin Pract. 2010;25:61–68.. [DOI] [PubMed] [Google Scholar]
- 23.Demling RH. Nutrition, anabolism, and the wound healing process: an overview. Eplasty. 2009;9:e9. [PMC free article] [PubMed] [Google Scholar]
- 24.High KP. Micronutrient supplementation and immune function in the elderly. Clin Infect Dis. 1999;28:717–722.. [DOI] [PubMed] [Google Scholar]
- 25.Wakimoto P, Block G. Dietary intake, dietary patterns, and changes with age: an epidemiological perspective. J Gerontol A Biol Sci Med Sci. 2001;56 Spec No 2:65–80.. [DOI] [PubMed] [Google Scholar]
- 26.Sandstead HH, Henriksen LK, Greger JL, et al. Zinc nutriture in the elderly in relation to taste acuity, immune response, and wound healing. Am J Clin Nutr. 1982;36:1046–1059.. [DOI] [PubMed] [Google Scholar]


