Supplemental Digital Content is available in the text.
Background:
Oncoplastic breast-conserving surgery (OBCS) avoids mastectomy for larger tumors, but patient-reported outcomes are unknown.
Methods:
The BREAST-Q questionnaire was distributed to 333 women following therapeutic mammaplasty or latissimus dorsi (LD) miniflap since 1991 [tumor diameter, 32.5 (5–100) mm). QScore software generated scores/100 for breast appearance, physical, emotional, and sexual wellbeing. Outcomes following therapeutic mammaplasty and LD miniflap were compared and qualitative data analyzed to identify common themes relating to satisfaction.
Results:
One hundred fifty (45%) women responded [mammaplasty versus LD miniflap, 52% versus 42%; age, 52 (30–83) years; follow-up, 84 (4–281) months). Eighty-nine percent rated OBCS better than mastectomy, > 80% recommending it to others. Mean outcome scores for breast appearance, physical, and emotional wellbeing were high and persisted beyond 15 years. Therapeutic mammaplasty patients were significantly more satisfied than those undergoing LD miniflap with the shape (P < 0.05), the size (P < 0.005), and the natural feel of the treated breast (P = 0.01). They demonstrated similar scores for physical and emotional wellbeing and a lower score for sexual wellbeing than LD miniflap patients. More LD miniflap patients reported back/shoulder symptoms and were more likely to report upper back pain (P < 0.05), but very few (< 5%) were concerned about donor-site appearance. Overall satisfaction with surgical outcomes was high in both OBCS groups (82% “excellent/very good”) but greatest after therapeutic mammaplasty (P < 0.005).
Conclusions:
Patients report long-lasting satisfaction after OBCS and outcomes that compare very favorably with those reported following mastectomy and immediate autologous reconstruction.
INTRODUCTION
Surgery for breast cancer has contracted from radical procedures to breast conservation, which is now standard of care for early breast cancer.1,2 Breast-conserving surgery is increasingly used for larger tumors, some downsized by neoadjuvant treatment, but mastectomy is still indicated in about a third of patients. Data from the United Kingdom National Mastectomy and Breast Reconstruction Audit (UKNMBRA)3 disclosed high overall levels of satisfaction following mastectomy and breast reconstruction, with highest levels following complex techniques. This audit collected data prospectively on > 18,000 women treated by mastectomy with or without reconstruction, using the Breast-Q to assess patient-reported outcomes (PROMs) at 3 and 18 months. Over 2,000 underwent immediate autologous reconstruction.3
Resection volume:breast volume is a key factor influencing cosmesis after breast conserving surgery, with patients reporting higher satisfaction following limited volume loss.4 Oncoplastic breast-conserving surgery (OBCS) combines breast conservation with immediate reconstruction of the resection defect, allowing more extensive resections without compromising cosmetic outcomes or oncological safety.5–7 This allows breast conservation for patients requiring extensive resections previously necessitating mastectomy. Better quality of life has been reported following oncoplastic breast conservation compared with conventional breast conserving surgery,8,9 but longer term PROMs are unknown.
This unit has been performing OBCS using latissimus dorsi (LD) miniflaps and therapeutic mammaplasty for 25 and 15 years, respectively. We investigated this mature cohort of patients to establish PROMs. The UKNMBRA was used as a reference group, as most of our full reconstructions used either mixed implant/flap or implant-alone techniques, and the numbers of autologous procedures were insufficient to enable a useful comparison. The well-designed prospective UKNMBRA enjoyed a high response rate, allowing a valid comparison between our patients and a much larger group of patients undergoing immediate autologous reconstruction.
METHODS
The BREAST-Q10 is a validated, multidimensional questionnaire-based tool that assesses PROMs following breast reconstruction. It measures patient experience and quality of life using a hierarchy of questions exploring physical, psychological and sexual wellbeing, cosmetic appearance, and overall satisfaction, ranked using a simple Likert scale.
The BREAST-Q was distributed by mail to 333 women treated by either therapeutic mammaplasty or LD miniflap between September 1991 and November 2014. Patients were also asked about additional procedures undertaken, the pain, softness, and lumpiness of the treated and contralateral breast, the amount of help required with daily activities, and the overall results of surgery.
Results were analyzed using the Qscore software [Rasch Unidimensional Measurement Models Laboratory (https://webcore.mskcc.org/breastq/scoring.html)], giving a mean outcome score/100 for 4 domains: breast appearance, physical, emotional, and sexual wellbeing. Scores were compared with those from UKNMBRA following immediate autologous reconstruction, which utilized the same analysis methods.3 Both studies used data that was not adjusted for age, performance status, level of deprivation, and health-care provider.
Responses following therapeutic mammaplasty and LD miniflap were compared using chi-square analysis for categorical responses, and the unpaired Students’ t test for continuous data.
Free text comments were encouraged within each domain. Qualitative responses were classified into thematic domains and analyzed in keeping with Miles et al.11 structure of qualitative analysis, then manually grouped by the authors using previously validated themes for patient satisfaction.12
RESULTS
Questionnaires were sent to 333 women (112 therapeutic mammoplasties, 221 LD miniflaps). One hundred and fifty (45%) returned questionnaires [58 mammoplasties (52%); 92 LD miniflaps (42%)], median age 52 years [mammaplasty 59 (39–83); LD miniflap 49 (30–70) years; P < 0.0001], follow-up 84 months [mammaplasty 53 (4–174); LD miniflap 112 (6–281) months; P < 0.0001; tumor diameter 32.5 (5–100) mm].
Patient-Reported Outcomes
Figure 1 compares the PROMs returned after OBCS with those returned after mastectomy and immediate autologous reconstruction.3 The trend toward decreasing scores for question items lower down the scale confirms the validity of the Breast-Q, as outcomes are increasingly difficult to achieve moving down the list. Women undergoing therapeutic mammaplasty were significantly more satisfied than those undergoing LD miniflap with the shape of their operated breast wearing a bra (P < 0.05), the size of their treated breast (P < 0.005), and the natural feel of the treated breast (P = 0.01). They were also significantly less likely to report upper back pain (P < 0.05).
Fig. 1.
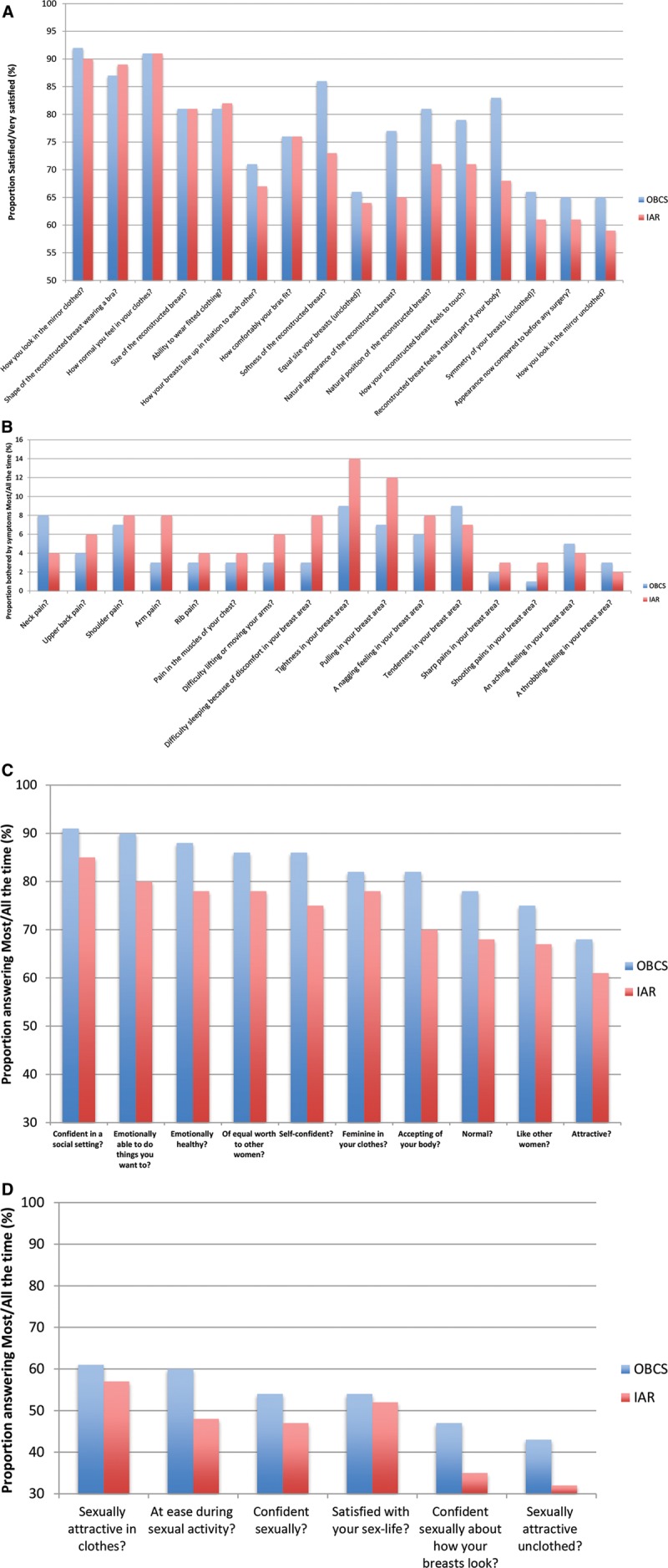
A, Satisfaction with the postoperative appearance of the breast following OBCS and immediate autologous reconstruction.3 B, Physical wellbeing following OBCS and immediate autologous reconstruction.3 C, Emotional wellbeing following OBCS and immediate autologous reconstruction.3 D, Sexual wellbeing following OBCS and immediate autologous reconstruction.3
Overall Satisfaction
When reporting overall satisfaction, most women stated that having OBCS was definitely preferable to mastectomy alone, would undergo it again, would encourage it to other women, and had no regrets about having the surgery (therapeutic mammaplasty versus LD miniflap: 91% versus 88%, 86% versus 73%, 90% versus 74%, and 88% versus 76%, respectively). Fewer felt that the surgery went exactly as planned or changed their lives for the better (therapeutic mammaplasty versus LD miniflap, 53% versus 42% and 61% versus 57%, respectively; P > 0.05).
Satisfaction with Flap Donor-Site Appearance
Women following LD miniflap reconstruction were questioned about satisfaction with donor-site appearance. Few women expressed concern with donor-site appearance (2–7% for all questions). Therapeutic mammaplasty does not involve a donor site, therefore patients were asked to report satisfaction with scarring, symmetry, and contralateral scars. Most reported being satisfied/very satisfied with the appearance and scarring of the treated and contralateral breast (94% and 90%, 90% and 91%, respectively).
Functional Impairment
All OBCS patients were questioned specifically about back and shoulder function to compare the LD miniflap group with mammaplasty patients who, by avoiding LD harvest, acted as a “control.” For a range of daily activities, very few women reported back and shoulder dysfunction after LD miniflap (see figure, Supplemental Digital Content 1, which shows experience of back and shoulder functional impairment following OBCS compared with LD reconstruction with/without implant,3 http://links.lww.com/PRSGO/A485). Although fewer women reported symptoms after mammaplasty versus LD miniflap, differences were not significant for individual question items (P > 0.05).
Most respondents were able to carry out daily living tasks unaided with similar outcomes reported following mammaplasty versus LD miniflap (P > 0.05) (see figure, Supplemental Digital Content 2, which shows proportion of OBCS patients independent with daily living activities, http://links.lww.com/PRSGO/A486).
Mean Outcome Scores
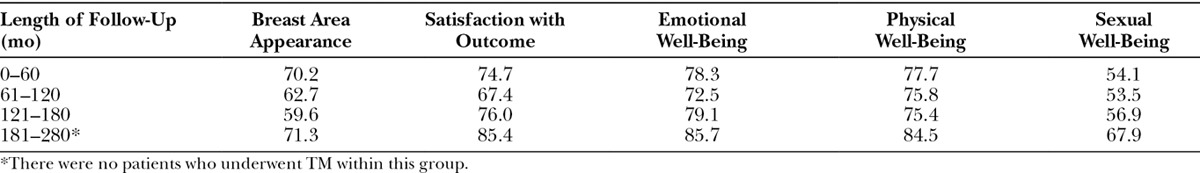
Both OBCS groups returned high aggregated mean outcome scores for breast appearance, overall satisfaction, emotional, and physical wellbeing (Fig. 2). Scores were lowest for sexual wellbeing. Cohort analysis confirmed persistence of outcomes with time, good scores being returned beyond 15 years (Table 1), but the generation of aggregated scores using an algorithm within the Qscore software prevented a meaningful statistical comparison.
Fig. 2.
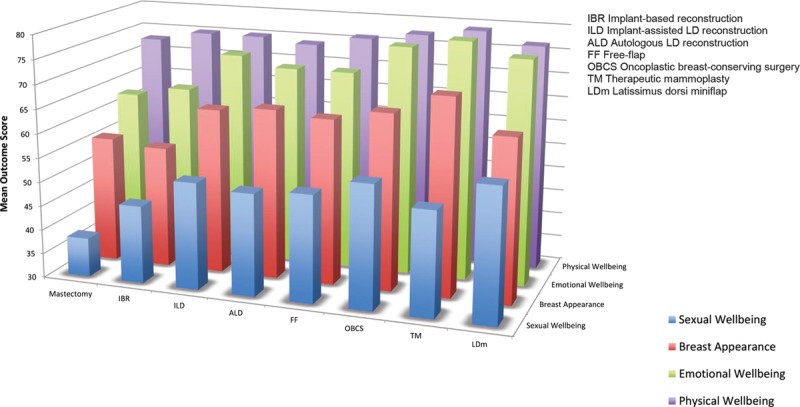
Mean outcome scores following mastectomy alone, immediate reconstruction,3 and OBCS.
Table 1.
Mean Outcome Scores following OBCS Categorized by Length of Follow-Up
Twenty-eight respondents (13 mammaplasty, 15 LD miniflap) were categorized as having undergone “extreme” OBCS13 (tumors > 50 mm). Scores for these patients were higher in most domains than the overall cohort: breast appearance 71, overall satisfaction 73, emotional wellbeing 83, physical wellbeing 79, and sexual wellbeing 59.
Local Symptoms
Women rated the softness, pain, and lumpiness in their treated breast. Overall, most reported that the breast felt soft/normal (61%) and pain-free (60%) with no significant procedure-related differences (mammaplasty versus LD miniflap 71% versus 55% and 51% versus 66%, respectively; P > 0.05). Women having mammaplasty were more likely to describe lumpiness versus LD miniflaps (34% versus 24%; P < 0.05).
Twenty respondents (13%) did not receive adjuvant breast irradiation (DXT) usually as a result of patient choice and reported significantly less firmness (DXT versus no DXT, 4% versus 0%; P < 0.05) and less breast pain and/or lumpiness (DXT versus no DXT, 2.4% versus 0% and 4% versus 0%, respectively; P > 0.05).
Additional Procedures
Forty-nine patients (32.7%) underwent additional surgical procedures (mammaplasty, 29.3%; LD miniflap, 34.8%; mean, 1.7 procedures/patient), most commonly nipple reconstruction (9.4%) and contralateral mammaplasty (19.5%). Donor-site or wound complications and augmentation for asymmetry were uncommon (4.7%, 4%, and 3.3%, respectively).
Overall Experience
Eighty-two percent described the overall experience of their operation as “excellent” or “very good” (mammaplasty, 88%; LD miniflap, 78%; P < 0.005). Three quarters of our patients felt “very satisfied” with the OBCS options offered, a response that was independent of the type of surgery (mammaplasty, 83%; LD miniflap, 67%; P > 0.05).
Qualitative Data
Four hundred seventy-one free text comments were analyzed. Twelve domains were explored: communication, hospital staff, postoperative course, adjuvant treatment, adjunctive procedures, cosmetic appearance, symptoms, how natural the breast seems, clothing, relationships, confidence, and survivorship. These were each subdivided into themes to better represent the variety of comments, examples of which include information provision, radiotherapy and cosmesis, family support, and life after treatment. Factors within each theme that seemed to contribute to higher patient satisfaction were also explored (see figure, Supplemental Digital Content 3, which shows general dimensions, themes, and associated factors contributing to patient satisfaction, http://links.lww.com/PRSGO/A487). None of the previously established themes were added or removed in the process, and representative comments were summarized (see table, Supplemental Digital Content 4, which displays the summary of qualitative findings and representative comments, http://links.lww.com/PRSGO/A488).
DISCUSSION
OBCS involves reconstruction of the resection defect either by volume displacement or by volume replacement. It should be considered when > 10–15% breast volume loss is anticipated.4 Volume displacement involves either mobilization and transposition of local dermoglandular flaps to reconstruct resection defects of 10–20% breast volume or a more extensive mammaplasty procedure for larger resections14 to avoid cosmetic failure.6 Many different mammaplasty techniques have been described for specific tumor locations,14 using pedicle techniques evolved from breast reduction as well as secondary pedicles. Most patients choose an immediate contralateral procedure to avoid asymmetry.15 Two-thirds of our patients had an inferior pedicle mammaplasty, with the remainder undergoing a superolateral or medial pedicle technique depending on the tumor site.
During volume replacement, resection defects are reconstructed using a range of local or distant pedicled or free autologous flaps.14,16 This approach can restore the shape and size of the breast without the need for contralateral surgery. Options include myocutaneous, myosubcutaneous, perforator and adipose tissue flaps, lipomodelling, and implants.14,17 We first described volume replacement using a myosubcutaneous LD flap, the “LD miniflap” in 199718 and have reported fewer complications and better cosmetic and functional outcomes than skin-sparing mastectomy with immediate breast reconstruction.19 The myosubcutaneous miniflap is harvested via a lateral incision and is used to reconstruct defects when the overlying skin is preserved. The myocutaneous LD miniflap carries a skin island for resections removing skin, but this may lead to a color discrepancy between the donor skin paddle and native breast.14
The operation can be performed as a 1-stage procedure with intraoperative frozen section margin analysis20 or as a 2-stage procedure following formal margin analysis. Selection for volume displacement or replacement is based chiefly on breast volume and predicted volume loss. A breast size > 500 cc with ptosis is a common indication for therapeutic mammaplasty, while LD miniflap is more appropriate in younger patients with smaller nonptotic breasts. In practice, decisions about the type of OBCS or mastectomy with or without total reconstruction are based on a range of clinical and oncological factors and ultimately patient choice.
Oncological Considerations
Oncological safety is of prime concern with any emerging technique. Early reports of OBCS confirmed its oncological safety,6,21 with similar rates of recurrence, disease-free and overall survival compared with standard breast conserving surgery.5,22–24 A recent meta-analysis of > 8,000 patients comparing outcomes after OBCS and standard breast conserving surgery, reported significantly lower rates of positive margins, reexcision and local recurrence, and better cosmetic outcomes.7
Losken et al.25 found that therapeutic mammaplasty has no effect on the detection of local recurrence, in keeping with our experience following LD miniflap reconstruction,26 as flaps remain radiolucent, with a radiolucent rim and minimal local distortion.27,28 Reducing breast size by therapeutic mammaplasty may also facilitate adjuvant radiotherapy, as late radiotherapy changes are more common in larger breasts due to dose heterogeneity.29 We reported favorable outcomes following irradiation of LD miniflaps, suggesting that their robust blood supply is able to withstand the ischemic changes induced by radiotherapy.30
Overall Satisfaction following Breast-Conserving Surgery
With equivalent survival following breast-conserving surgery and mastectomy,1,2 interest in factors such as patient preference, aesthetic outcome, psychosocial adjustment, and long-term quality of life become more important in determining choice of procedure.31 The use of validated self-administered questionnaires is an established method to study this,32 and the popular Breast-Q10 has been used in almost 50 studies and with minor modifications in considerably more.33
There is little data regarding quality of life following OBCS, although several authors have demonstrated high levels of satisfaction with aesthetic outcome after therapeutic mammaplasty.34–36 Patel et al.37 used the Breast-Q to compare satisfaction and quality of life after immediate, staged-immediate, and delayed mammaplasty. No significant differences were reported between these 3 groups, but positive scores were returned in all domains. Santos et al.38 compared cosmetic outcome following breast conserving surgery versus mammaplasty in 122 women, reporting more “excellent” aesthetic results in the mammaplasty group. The study included T1/2 tumors, preventing a direct comparison with our patients [mean tumor diameter, 32.5 (5–100) mm].
Hernanz et al.39 reviewed the evidence for therapeutic mammaplasty from 10 studies, concluding clear oncological and cosmetic advantages, as well as improved quality of life in women with macromastia. Veiga et al.9 compared quality of life and self-esteem after breast-conserving surgery and OBCS using volume replacement, reporting higher quality of life following OBCS using the SF-36 questionnaire.
Fewer women expressed concern with donor-site appearance (2–7% for all questions) than UKNMBRA respondents following either LD with implant (6–14%) or autologous LD reconstruction (8–15%).3 More than 80% of our patients described the final results of their surgery as “excellent” or “very good,” compared with two-thirds of women after mastectomy and immediate autologous reconstruction, and a higher proportion (82%) described the overall experience of their operation as “excellent” or “very good,” compared with immediate autologous reconstruction (67%).3 Both OBCS groups returned high mean outcome scores in most domains, higher than those reported by the UKNMBRA following either mastectomy alone, or mastectomy and immediate reconstruction.3
This contrasts with other BREAST-Q data comparing mastectomy with and without reconstruction with standard breast-conserving surgery, finding lower physical and sexual wellbeing scores after breast conservation.40
Satisfaction with symmetry, breast size, and softness was higher after mammaplasty than after LD miniflap in our patients. This highlights the importance of symmetry, and the benefit of simultaneous reduction, and may reflect the longer follow-up of LD miniflap patients. LD miniflap patients were more satisfied with their scars than those choosing implant or autologous LD reconstruction.3 The use of a single lateral incision in 85% of cases for tumor resection, flap harvest, and reconstruction may explain these results.16
Physical Wellbeing and Functional Impairment
Higher levels of physical wellbeing were experienced by our patients than those reported in the UKNMBRA,3 possibly reflecting the preservation of a more “natural” breast. High functional scores following therapeutic mammaplasty (although not significantly higher than following LD miniflap) may reflect donor-site avoidance and the functional improvement experienced following breast reduction.41,42 The similar levels of emotional wellbeing observed after both types of OBCS suggests that anxiety about diagnosis and treatment influences emotional wellbeing more than the type of surgery.
Very few women undergoing OBCS experienced difficulties performing daily tasks, fewer than after LD reconstruction with or without implants,3 and slightly less following mammaplasty than LD miniflap. Limiting muscle dissection during LD miniflap harvest may reduce disability, as our patients reported less impairment than following more extensive LD harvest.3 Functional preservation is arguably even more important than good cosmesis because of the influence of disability on quality of life. Somewhat surprisingly, although pain in the treated breast was common, it had little impact on activities of daily living, satisfaction, or wellbeing scores.
Sexual Wellbeing
Scores for sexual wellbeing following OBCS were lower than all other domains, reflecting the trend seen following immediate autologous reconstruction.3 Sheppard and Ely43 explored low sexual wellbeing following breast surgery using a series of in-depth interviews held with patients and spouses. They noted that women may wrongly perceive their partner to be disturbed by changes to their bodies and that despite being an important component of the breast cancer experience, sexuality and body image are not often discussed by health-care professionals.43
Limitations
Quality of life and satisfaction may be affected by a number of factors other than those measured in this survey, including tumor stage, adjuvant treatment, and fear of recurrence. Women undergoing breast-conserving surgery, including OBCS, are more prone to worry about ipsilateral recurrence than those undergoing mastectomy and breast reconstruction, and this may explain why others have failed to show better quality of life after breast conservation compared with mastectomy.34,44 Waljee et al.45 proposed that these patients may not receive the same level of counseling as mastectomy patients and are less informed about recovery and experience. This may help to explain the variety of comments we received regarding recovery, long-term symptoms, and cosmetic outcome.
A response rate of 45% is not unusual for this type of survey, but nonresponse bias cannot be ruled out. On the other hand, postal surveys confer several advantages, including limited cost, anonymity, and reproducibility.46 The effect of this response rate on our results is unknown and may have been improved by a second mailing or by the use of an incentive. Other sources of potential bias included differential response rates comparing this study with the UKNMBRA3 (45% versus > 80%), different methods of data collection (by treating unit versus national audit office3) and different lengths of follow-up (84 versus 18 months3), although the scores returned by patients in different time cohorts were similar.
CONCLUSIONS
OBCS is extending opportunities for breast conservation to patients previously treated by mastectomy. This study has confirmed the patient-reported benefits of these procedures, which continue beyond a median 7-year follow-up. Patients undergoing OBCS experienced better quality of life, higher levels of satisfaction and wellbeing, better donor-site appearance and function, less impact on daily activity, and better surgical outcomes than previously published evidence of women undergoing more major procedures.
OBCS offers a valuable new alternative to mastectomy and reconstruction for patients facing a high risk of unacceptable cosmetic deformity after standard breast-conserving surgery. Additionally, it achieves 2 increasingly important goals of modern breast cancer treatment: psychological wellbeing combined with good quality of life.
Supplementary Material
Footnotes
Presented at the Association of Breast Surgeons Annual Conference, May 2016, Manchester, United Kingdom; seventh Winchester Oncoplastic Masterclass, September 2016, Winchester, United Kingdom.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the Wessex Cancer Research Fund.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.van Dongen JA, Voogd AC, Fentiman IS, et al. Long-term results of a randomized trial comparing breast-conserving therapy with mastectomy: European Organization for Research and Treatment of Cancer 10801 trial. J Natl Cancer Inst. 2000;92:1143–1150.. Available at http://www.ncbi.nlm.nih.gov/pubmed/10904087. Accessed August 18, 2016. [DOI] [PubMed] [Google Scholar]
- 2.Jacobson JA, Danforth DN, Cowan KH, et al. Ten-year results of a comparison of conservation with mastectomy in the treatment of stage I and II breast cancer. N Engl J Med. 1995;332:907–911.. [DOI] [PubMed] [Google Scholar]
- 3.Jeevan R, Cromwell D, Browne J, van der Meulen J; National Mastectomy and Breast Reconstruction Audit; 2011. Available at https://www.rcseng.ac.uk/surgeons/research/surgical-research/docs/national-mastectomy-and-breast-reconstruction-audit-fourth-report-2011. Accessed August 19, 2016.
- 4.Cochrane RA, Valasiadou P, Wilson ARM, et al. Cosmesis and satisfaction after breast-conserving surgery correlates with the percentage of breast volume excised. Br J Surg. 2003;90:1505–1509.. [DOI] [PubMed] [Google Scholar]
- 5.Rietjens M, Urban CA, Rey PC, et al. Long-term oncological results of breast conservative treatment with oncoplastic surgery. Breast. 2007;16:387–395.. [DOI] [PubMed] [Google Scholar]
- 6.Clough KB, Lewis JS, Couturaud B, et al. Oncoplastic techniques allow extensive resections for breast-conserving therapy of breast carcinomas. Ann Surg. 2003;237:26–34.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Losken A, Dugal CS, Styblo TM, et al. A meta-analysis comparing breast conservation therapy alone to the oncoplastic technique. Ann Plast Surg. 2014;72:145–149.. [DOI] [PubMed] [Google Scholar]
- 8.Kaviani A, Sodagari N, Sheikhbahaei S, et al. From radical mastectomy to breast-conserving therapy and oncoplastic breast surgery: a narrative review comparing oncological result, cosmetic outcome, quality of life, and health economy. ISRN Oncol. 2013;2013:742462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Veiga DF, Veiga-Filho J, Ribeiro LM, et al. Quality-of-life and self-esteem outcomes after oncoplastic breast-conserving surgery. Plast Reconstr Surg. 2010;125:811–817.. [DOI] [PubMed] [Google Scholar]
- 10.Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124:345–353.. [DOI] [PubMed] [Google Scholar]
- 11.Miles MB, Huberman AM, Saldaña J. Qualitative Data Analysis : A Methods Sourcebook. 20133rd ed California: SAGE Publications. [Google Scholar]
- 12.Anderson R, Barbara A, Feldman S. What patients want: a content analysis of key qualities that influence patient satisfaction. J Med Pract Manage. 22:255–261.. Available at http://www.ncbi.nlm.nih.gov/pubmed/17494478. Accessed August 18, 2016. [PubMed] [Google Scholar]
- 13.Silverstein MJ, Savalia N, Khan S, et al. Extreme oncoplasty: breast conservation for patients who need mastectomy. Breast J. 21:52–59.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rainsbury RM, Clough KB, Kaufman GJ, et al. Dixon J. In: Breast Surgery: A Companion to Specialist Surgical Practice. 20145th ed Edinburgh, Scotland: Saunders Elsevier. [Google Scholar]
- 15.Losken A, Hamdi M. Partial breast reconstruction: current perspectives. Plast Reconstr Surg. 2009;124:722–736.. [DOI] [PubMed] [Google Scholar]
- 16.Rusby J, Rainsbury R. Urban C de A, Rietjens M. Distant Volume Flaps for Conservative Surgery. In: Oncoplastic and Reconstructive Breast Surgery. 2013Milano, Italy: Springer. [Google Scholar]
- 17.Rainsbury RM, Clough KB, Kaufman GJ, Nos C, Dixon JM. Dixon JM. Oncoplastic procedures to allow breast conservation and a satisfactory cosmetic outcome. Breast Surgery: In: A Companion to Specialist Surgical Practice. 20145th ed Elsevier Saunders. [Google Scholar]
- 18.Raja MA, Straker VF, Rainsbury RM. Extending the role of breast-conserving surgery by immediate volume replacement. Br J Surg. 1997;84:101–105.. [PubMed] [Google Scholar]
- 19.Gendy RK, Able JA, Rainsbury RM. Impact of skin-sparing mastectomy with immediate reconstruction and breast-sparing reconstruction with miniflaps on the outcomes of oncoplastic breast surgery. Br J Surg. 2003;90:433–439.. [DOI] [PubMed] [Google Scholar]
- 20.Rusby JE, Paramanathan N, Laws SAM, et al. Immediate latissimus dorsi miniflap volume replacement for partial mastectomy: use of intra-operative frozen sections to confirm negative margins. Am J Surg. 2008;196:512–518.. [DOI] [PubMed] [Google Scholar]
- 21.Cothier-Savey I, Otmezguine Y, Calitchi E, et al. [Value of reduction mammoplasty in the conservative treatment of breast neoplasms. Apropos of 70 cases]. Ann Chir Plast esthétique. 1996;41:346–353.. Available at http://www.ncbi.nlm.nih.gov/pubmed/9183883. Accessed August 18, 2016. [PubMed] [Google Scholar]
- 22.De Lorenzi F, Hubner G, Rotmensz N, et al. Oncological results of oncoplastic breast-conserving surgery: long term follow-up of a large series at a single institution: a matched-cohort analysis. Eur J Surg Oncol. 2016;42:71–77.. [DOI] [PubMed] [Google Scholar]
- 23.Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347:1227–1232.. [DOI] [PubMed] [Google Scholar]
- 24.Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–1241.. [DOI] [PubMed] [Google Scholar]
- 25.Losken A, Schaefer TG, Newell M, et al. The impact of partial breast reconstruction using reduction techniques on postoperative cancer surveillance. Plast Reconstr Surg. 2009;124:9–17.. [DOI] [PubMed] [Google Scholar]
- 26.Banerjee D, Paramanathan N, Summerhayes C, et al. Local recurrence following skin-sparing oncoplastic techniques: a 10-year Winchester experience. Eur J Cancer. 2003;1:38. [Google Scholar]
- 27.Tan VK, Cornford EJ, McCulley SJ, et al. Qualitative mammographic findings and outcomes of surveillance mammography after partial breast reconstruction with an autologous flap. J Surg Oncol. 2015;111:377–381.. [DOI] [PubMed] [Google Scholar]
- 28.Monticciolo DL, Ross D, Bostwick J, 3rd, et al. Autologous breast reconstruction with endoscopic latissimus dorsi musculosubcutaneous flaps in patients choosing breast-conserving therapy: mammographic appearance. AJR Am J Roentgenol. 1996;167:385–389.. [DOI] [PubMed] [Google Scholar]
- 29.Moody AM, Mayles WP, Bliss JM, et al. The influence of breast size on late radiation effects and association with radiotherapy dose inhomogeneity. Radiother Oncol. 1994;33:106–112.. Available at http://www.ncbi.nlm.nih.gov/pubmed/7708953. Accessed August 18, 2016. [DOI] [PubMed] [Google Scholar]
- 30.Laws SAM, Cheetham J, Rainsbury RM. Volume changes after latissimus dorsi “miniflap” breast reconstruction. Breast Cancer Res Treat. 2001;69:232. [Google Scholar]
- 31.Conde DM, Pinto-Neto AM, Cabello C, et al. Quality of life in Brazilian breast cancer survivors age 45-65 years: associated factors. Breast J. 2005;11:425–432.. [DOI] [PubMed] [Google Scholar]
- 32.Fehlauer F, Tribius S, Mehnert A, et al. Health-related quality of life in long term breast cancer survivors treated with breast conserving therapy: impact of age at therapy. Breast Cancer Res Treat. 2005;92:217–222.. [DOI] [PubMed] [Google Scholar]
- 33.Cohen WA, Mundy LR, Ballard TN, et al. The BREAST-Q in surgical research: a review of the literature 2009-2015. J Plast Reconstr Aesthet Surg. 2016;69:149–162.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.D’Aniello C, Grimaldi L, Barbato A, et al. Cosmetic results in 242 patients treated by conservative surgery for breast cancer. Scand J Plast Reconstr Surg Hand Surg. 1999;33:419–422.. Available at http://www.ncbi.nlm.nih.gov/pubmed/10614751. Accessed August 18, 2016. [DOI] [PubMed] [Google Scholar]
- 35.Fitoussi A, Berry M, Fama F, et al. Oncoplastic breast surgery for cancer: analysis of 540 consecutive cases [outcomes article]. - PubMed - NCBI. Plast Reconstr Surg. 2010;125:454–462.. [DOI] [PubMed] [Google Scholar]
- 36.Spear SL, Pelletiere CV, Wolfe AJ, et al. Experience with reduction mammaplasty combined with breast conservation therapy in the treatment of breast cancer. Plast Reconstr Surg. 2003;111:1102–1109.. [DOI] [PubMed] [Google Scholar]
- 37.Patel KM, Hannan CM, Gatti ME, et al. A head-to-head comparison of quality of life and aesthetic outcomes following immediate, staged-immediate, and delayed oncoplastic reduction mammaplasty. Plast Reconstr Surg. 2011;127:2167–2175.. [DOI] [PubMed] [Google Scholar]
- 38.Santos G, Urban C, Edelweiss MI, et al. Long-term comparison of aesthetical outcomes after oncoplastic surgery and lumpectomy in breast cancer patients. Ann Surg Oncol. 2014:2500–2508.. [DOI] [PubMed] [Google Scholar]
- 39.Hernanz F, Regaño S, Vega A, et al. Reduction mammaplasty: an advantageous option for breast conserving surgery in large-breasted patients. Surg Oncol. 2010;19:e95–e102.. [DOI] [PubMed] [Google Scholar]
- 40.Howes BH, Watson DI, Xu C, et al. Quality of life following total mastectomy with and without reconstruction versus breast-conserving surgery for breast cancer: a case-controlled cohort study. J Plast Reconstr Aesthet Surg. 2016;69:1184–1191.. [DOI] [PubMed] [Google Scholar]
- 41.Sabino Neto M, Demattê MF, Freire M, et al. Self-esteem and functional capacity outcomes following reduction mammaplasty. Aesthet Surg J. 2008;28:417–420.. [DOI] [PubMed] [Google Scholar]
- 42.Blomqvist L, Eriksson A, Brandberg Y. Reduction mammaplasty provides long-term improvement in health status and quality of life. Plast Reconstr Surg. 2000;106:991–997.. Available at http://www.ncbi.nlm.nih.gov/pubmed/11039369. Accessed August 18, 2016. [DOI] [PubMed] [Google Scholar]
- 43.Sheppard LA, Ely S. Breast cancer and sexuality. Breast J. 2008;14:176–181.. [DOI] [PubMed] [Google Scholar]
- 44.Nano MT, Gill PG, Kollias J, et al. Psychological impact and cosmetic outcome of surgical breast cancer strategies. ANZ J Surg. 2005;75:940–947.. [DOI] [PubMed] [Google Scholar]
- 45.Waljee JF, Hu ES, Ubel PA, et al. Effect of esthetic outcome after breast-conserving surgery on psychosocial functioning and quality of life. J Clin Oncol. 2008;26:3331–3337.. [DOI] [PubMed] [Google Scholar]
- 46.Cartwright A. Interviews or postal questionnaires? Comparisons of data about women’s experiences with maternity services. Milbank Q. 1988;66:172–189.. [PubMed] [Google Scholar]


