Abstract
Background
Increasing rates of cannabis use among emerging adults is a growing public health problem. Intensive longitudinal data can provide information on proximal motives for cannabis use, which can inform interventions to reduce use among emerging adults.
Method
As part of a larger longitudinal study, patients aged 18–25 years (N=95) recruited from an urban Emergency Department completed daily text message assessments of risk behaviors for 28 days, including daily cannabis quantity and motives. Using a mixed effects linear regression model, we examined the relationships between daily quantity of cannabis consumed and motives (i.e., enhancement, social, conformity, coping, and expansion).
Results
Participants were, on average, 22.0 years old (SD=2.2); 48.4% were male, 45.3% were African American, and 56.8% received public assistance. Results from the multi-level analysis (clustering day within individual), controlling for gender, race, and receipt of public assistance, indicated daily use of cannabis use for enhancement (β=.27), coping (β=.15), and/or social motives (β=.34) was significantly associated with higher quantities of daily cannabis use; whereas expansion and conformity motives were not.
Conclusions
Daily data show that emerging adults who use cannabis for enhancement, social, and coping motives reported using greater quantities of cannabis. Future research should examine more comprehensive cannabis motives (e.g., boredom, social anxiety, sleep) and test tailored interventions focusing on alternative cognitive/behavioral strategies to address cannabis motives.
Keywords: cannabis motives, text messaging, cannabis use, emerging adults
1. Introduction
Cannabis is the most frequently used substance of abuse other than alcohol and tobacco (Center for Behavioral Health Statistics and Quality, 2016). Cannabis is associated with many individual and public health consequences (Silins et al., 2014; Volkow et al., 2016). Recent U.S. state legislation has increased legal access to cannabis, shifting the national context surrounding cannabis use. Daily consumption and perceived approval of cannabis use are increasing while perceived risk is decreasing, particularly among young people (Azofeifa et al., 2016; Johnston et al., 2016). Emerging adults (usually ages 18–25 years) comprise the age group with the highest lifetime (46.9%), past-year (13.6%), and past-month (8.4%) prevalence of cannabis use (Center for Behavioral Health Statistics and Quality, 2016) and cannabis use disorders (Hasin et al., 2015). Emerging adults in urban areas are of particular concern given that urban versus rural areas have a higher prevalence of cannabis use and cannabis use disorders (Hasin et al., 2015). To inform policy and interventions, we need a deeper understanding of the determinants of cannabis use among emerging adults. Individual data captured daily or at the event-level can provide needed detail on proximal factors influencing cannabis use. Such data may prove useful in developing personalized, tailored, and/or just-in-time adaptive interventions (Nahum-Shani et al., 2016) to reduce cannabis consumption and negative consequences.
Although many factors across levels of social ecology influence substance use (Abadi et al., 2011; Keyes et al., 2011; Sallis et al., 2008; Tang and Orwin, 2009), motives (i.e., reasons for use) are an important individual-level characteristic because they are related to negative consequences (Blevins et al., 2016b; Lee et al., 2009), including developing cannabis use disorders (Benschop et al., 2015; Schlossarek et al., 2016). Motives may change as a result of cannabis interventions; in prior work, reductions in motives (particularly coping-related motives) predicted post-intervention reductions in consumption and consequences (Blevins et al., 2016a), underscoring the need to examine how cannabis-related motives affect consumption. Models of cannabis use motives were originally adapted from models of alcohol motives (Cooper, 1994; Cooper et al., 1995), and were characterized in five domains: enhancement (e.g., enjoyment), coping (e.g., reducing negative affect), social (e.g., making a social event more enjoyable), expansion (e.g., altering perceptual awareness), or conformity (e.g., fitting in) (Simons et al., 1998). Researchers later expanded cannabis motives to include others such as relaxation, social anxiety, and sleep (Lee et al., 2009; Lee et al., 2007).
In cross-sectional data, young people’s motives for cannabis use are associated with cannabis consumption, severity, and consequences, and other psychosocial outcomes (Benschop et al., 2015; Bonn-Miller et al., 2014; Bonn-Miller and Zvolensky, 2009a; Bonn-Miller and Zvolensky, 2009b; Bravo et al., 2017; Farris et al., 2016; Simons et al., 1998; Zvolensky et al., 2007). Among young adults, when adjusting for gender, age of cannabis initiation, and other substance use, greater enhancement and social motives positively correlated with recent cannabis use while conformity was negatively related to consumption (Zvolensky et al., 2007). In this same sample, higher coping motives were related to lower positive affect and higher negative affect, anxiety sensitivity, anxious arousal, and depression symptoms. Other motives were less consistently associated with outcomes: enhancement was positively associated with positive affect and negatively associated with anxious arousal and depression symptoms, whereas conformity was positively correlated with negative affect, and no relationships were observed for expansion or social motives. Among college students who used cannabis at least once in the previous month, social, coping, expansion, and enhancement motives positively correlated with frequency of cannabis use over the month, whereas conformity was non-significant (Bravo et al., 2017). Using the expanded motives list among high school students using cannabis regularly, coping motives were positively related to externalizing (Blevins et al., 2016b) and higher coping, alcohol-related, and availability motives, along with lower celebration motives were associated with stronger internalizing (Blevins et al., 2016b). Among Dutch young adults using cannabis regularly, motives regarding routine use (i.e., boredom, habit) and coping were related to cannabis dependence (Benschop et al., 2015). Data from other young adults found that those meeting criteria for cannabis dependence had higher levels of all five original motives dimensions than those not meeting criteria (Bonn-Miller and Zvolensky, 2009b).
Although cannabis use motives are generally correlated with consumption and other outcomes in cross-sectional research, motives are conceptualized as situational reasons for use that are expected to vary across time and contexts (Cooper, 1994). For example, event-level research demonstrated that perceived motivation for cannabis use can differ when measured just before and after consumption (Shrier and Scherer, 2014). Further, among high school students, motives for use changed across the course of a multi-session intervention, and such changes were predictive of treatment outcomes for up to 15 months, but were not measured at the daily level (Blevins et al., 2016a).
Because of their changing nature, motives may be more accurately captured with event or daily-level methods, but few researchers have evaluated specific acute associations between motives and amount consumed consumption. For example, ecological momentary assessment (EMA) data of young people’s cannabis use indicated that 86% of use events involved enhancement, expansion, or social motives and 14% involved coping or conformity motives, but these motives were not associated with more hits consumed (Shrier et al., 2013). In a diverse community sample, primarily comprising college students, using EMAs over two weeks, most cannabis use episodes involved enhancement motives (77.7%), followed by coping (62.7%), expansion (22.8%), social (17.7%), and conformity (2.8%) (Buckner et al., 2015). Together, these studies (Buckner et al., 2015; Shrier et al., 2013) demonstrate that individuals can have multiple, simultaneous motives for acute cannabis use, but relationships between motives and level of consumption within days or events are under-investigated. Further, EMA data also suggest that acute motives relate to other contextual factors associated with cannabis use, such as withdrawal symptoms and negative affect (Buckner et al., 2015). Given that previous EMA studies demonstrate relationships between anxiety and cannabis craving and use, motives related to coping with negative affect may play an important role in determining acute consumption, at least for some individuals (Buckner et al., 2012; Buckner et al., 2011).
Although these previous studies provide a useful foundation for understanding daily motives and cannabis use, in the present study, we begin to address gaps in the literature by examining daily data collected via text messaging from a sample of emerging adults recruited from an urban healthcare setting. Most literature examining cannabis motives has focused on school samples, in particular college students, or medical cannabis patients, with limited attention to urban populations with higher prevalence. Further, previous research has often been cross-sectional in nature and lacks information on how motives influence quantity consumed using more fine-grained longitudinal approaches. Specifically, we examine daily relationships between perceived influence of five motive types and quantity of cannabis consumed. We hypothesized that, in general, higher motives would be associated with higher consumption at the daily level, but had no specific hypotheses about which motives would be more strongly associated with daily consumption, because few researchers have evaluated simultaneous relationships between motives and acute consumption at the daily level.
2. Method
2.1. Study Setting
From November 2014 through September 2015, we recruited emerging adults from the Emergency Department (ED) at Hurley Medical Center, a Level-One trauma center in urban Flint, Michigan. This mid-sized city has poverty and crime rates similar to other mid-size rust belt cities (U.S. Census Bureau, 2015a, b, c, d, e). We recruited from the ED because emerging adults attending EDs often have elevated rates of substance use and other risky behaviors (Bonar et al., 2016; Cunningham et al., 2006; Walton et al., 2011; Wilson and Klein, 2000). The Institutional Review Boards at both Hurley Medical Center and the University of Michigan approved the research, and a Certificate of Confidentiality was obtained from the National Institutes of Health.
2.2. Participants
Patients ages 18–25 years attending the ED were eligible for screening for a longitudinal 28-day survey study of substance use and sexual behaviors. We excluded patients from screening based on these criteria: insufficient cognition or physical/medical state that would preclude ability to provide informed consent, presenting for care involving intensive ED-based social work intervention (e.g., suicidality, acute sexual assault), having a live-in partner already participating in the study, significant hearing/visual impairment, illiteracy and/or inability to communicate in English, or enrolled in another longitudinal study.
Because the longitudinal study focused on substance use and sexual risk, participants were eligible for enrollment if they reported: illicit drug use/non-medical use of prescription drugs in the previous 4 weeks, sexual intercourse without a condom during the past 4 weeks, and having a cell phone with ability to text message (see Measures). After approaching 726 patients for screening, we screened 586 (80.7%) with 139 eligible (23.7%) for enrollment. A total of 111 participants enrolled (79.9%) and 106 completed at least one daily survey; 95 reported cannabis use on at least one daily survey (M=68.7%, SD=27.3% surveys completed) and are included in the analyses presented here. They were 48.4% male, 45.3% African American (39.0% European American and 15.8% other identity), and their mean age was 22.0 years (SD=2.2). Most (56.8%) received public assistance. Based on chart reviews, participants were categorized as visiting the ED for medical/psychiatric reasons (82.1%) or injury-related reasons (17.9%). Table 1 shows further demographic characteristics.
Table 1.
Descriptive and cannabis acquisition characteristics for N =95 participants reporting cannabis use on daily surveys
| Sample Characteristics | M (SD) or % (n) |
|---|---|
|
| |
| Age | 22.0 (2.2) |
|
| |
| Sex | |
| Female | 49 (51.6%) |
| Male | 46 (48.4%) |
|
| |
| Ethnicity | |
| African American | 43 (45.3%) |
| European American/Other | 52 (54.7%) |
|
| |
| Educational attainment | |
| Less than HS education | 26 (27.4%) |
| HS/GED or higher | 69 (72.6%) |
|
| |
| Currently in school | |
| Yes | 21 (22.1%) |
| No | 74 (77.9%) |
|
| |
| Marital status | |
| Married/Engaged | 17 (17.9%) |
| Single | 77 (81.1%) |
|
| |
| Currently receiving public assistance | |
| Yes | 54 (56.8%) |
| No | 41 (43.2%) |
|
| |
| Most frequent method of using cannabisa | |
| Blunt | 59 (63.4%) |
| Joint | 18 (19.4%) |
| Bowl | 13 (14.0%) |
| Bong | 3 (3.2%) |
|
| |
| How often purchased cannabis in past 28 daysa | |
| Not purchased | 16 (18.3%) |
| 1–3 times per month | 22 (23.7%) |
| Once per week | 15 (16.1%) |
| 2–6 times per week | 26 (28.0%) |
| Daily | 13 (14.0%) |
|
| |
| Typical source of cannabis in past 28 daysa | |
| Known dealer | 34 (36.6%) |
| Friend/roommate | 28 (30.1%) |
| Family member/spouse/partner | 18 (19.4%) |
| Dispensary | 9 (9.7%) |
| Stranger/unknown dealer | 3 (3.2%) |
| Grows own | 1 (1.1%) |
|
| |
| Typical quantity of cannabis obtaineda | |
| 1–2 joints worth | 33 (35.5%) |
| 1/8 oz. | 22 (23.7%) |
| 1/4 oz. | 18 (19.4%) |
| 1/2 oz. | 6 (6.5%) |
| 1 oz. | 5 (5.4%) |
| Other | 9 (9.7%) |
|
| |
| Ever trades goods/services for cannabisa | |
| Yes | 11 (11.8%) |
| No | 82 (88.2%) |
|
| |
| Been issued a medical cannabis card | 8 (8.4%) |
|
| |
| Mean cannabis use frequency per day of use on daily surveys | 3.20 (3.46) |
|
| |
| Reported quantity of cannabis on daily survey use daysb | |
| <0.5g (<1 joint) | 192 (17.9%) |
| 0.5g (1 joint) | 194 (18.0%) |
| 1g (2 joints) | 225 (20.9%) |
| 1.5g (3 joints) | 124 (11.5%) |
| 2g (4 joints) | 144 (13.4%) |
| 2.5g+ (5+ joints) | 196 (18.2%) |
|
| |
| Motives ratings across daily survey periodc | |
| Enhancement | 2.74 (1.15) |
| Coping | 1.83 (1.06) |
| Social | 1.69 (1.01) |
| Expansion | 1.67 (0.99) |
| Conformity | 1.18 (0.55) |
N=93 because these data were collected from the 93 people who had used cannabis in the 28 days prior to baseline, but 95 people are included in analyses because they used cannabis during the daily survey period. Purchased quantities assessed (responses shown above) were on a different scale than daily quantity to capture a range of purchasing behaviors.
N = 1,075 days reporting quantity
Ns on motives variables range from 1,052 to 1,067 days due to missing responses on some daily motives items.
2.3. Design and Procedures
We recruited participants to complete baseline measures, 28 days of daily text message surveys, and an assessment at the conclusion of the daily surveys. The full protocol and procedures were previously described (Bonar et al., in press; Bonar et al., in press). Research assistants (RAs) recruited during days and evenings, using medical records to identify potential participants. Interested participants provided consent and received a gift valuing $1.00 for self-administering a computerized eligibility survey. RAs obtained a second written consent from eligible participants who then completed baseline measures, a urine drug screening (UDS), and orientation to the text message surveys. We provided $20 cash for the baseline assessment, $5 for the UDS, and a $10 credit card gift card to offset the cost of text messaging surveys.
For the 28 days following baseline, participants were automatically texted at 10:00 a.m. prompting the daily survey, with questions texted sequentially after participants replied “START”. They had until midnight to complete each day’s questions that assessed drug use and sexual behaviors for the previous day (Bonar et al., in press). On days when a participant did not report a target behavior (e.g., cannabis use) the survey branched to avoid sending related questions, instead sending an equal number of items querying other activities. Out of 3,108 possible surveys, we administered 19 by phone when participants had technical problems. Weekly, we added survey payments ($2 per survey; $5 bonus for each week they completed 6 out of 7 surveys) to participants’ gift cards. After the 28-day period, we invited participants to complete a final assessment mirroring the baseline assessment ($25 cash compensation, $5 for UDS). At the final assessment, most participants in the present analytic sample (76.1% of N = 84 responding) self-reported that text message surveys took less than 15 minutes to complete; time stamps were not reliable indicators because participants could respond to survey questions throughout the day (from 10am–12am). Participants who were compliant with all study procedures, from baseline through the final assessment could earn the equivalent of $142. The present analyses focus on data from the baseline enrollment and longitudinal daily surveys.
2.4. Measures
2.4.1. Eligibility criteria
At screening, we assessed drug use eligibility with items modified from the Substance Abuse Outcomes Module (SAOM; Smith et al., 1996; Smith et al., 2006) and the NIDA-Modified Alcohol Smoking and Substance Involvement Screening Test (ASSIST) version 2.0 (Humeniuk et al., 2008; WHO ASSIST Working Group, 2002). Participants indicated the number of days (0 to 28) in the past 4 weeks that they used: cannabis, cocaine/crack, street opioids, hallucinogens, inhalants, and methamphetamines. They reported the number of days of non-medical use of prescription sedatives, opioids, and stimulants. Participants reported lifetime sexual activity (Centers for Disease Control and Prevention (CDC), 2012), then the number of past 4-week main and/or casual partners and condom use with each partner type on items adapted from Monitoring the Future (Johnston et al., 2010b). For the cell-phone eligibility criterion, participants were asked (yes/no) if they had a cell phone and, if so, whether the phone had text messaging (Ranney et al., 2013).
2.4.2. Sample Demographics
For screening and baseline surveys we used items adapted from national studies and prior research (Cunningham et al., 2014; Harris, 2009; Johnston et al., 2010a; Smith et al., 1996; United States Department of Health and Human Services et al., 2008) to characterize participants’ demographics.
2.4.3. Baseline Timeline Follow-back (TLFB)
For the day of the ED visit and 28 days prior RAs administered a TLFB to assess substance use and sexual behaviors (Scott-Sheldon et al., 2010; Weinhardt et al., 1998). To assess daily cannabis quantity, we showed participants images depicting 0.5 grams of cannabis in joint and loose form to assist in estimating daily consumption (Collins et al., 2014). For analyses, we coded cannabis quantity on TLFB use days as follows: <1 joint (<0.5g) = 1 (representing any use, but not finishing a joint), 1 joint (0.5g) = 2, between 1 and 2 joints (between 0.5g and 1 g) = 3, 2 joints (1g) = 4, 3 joints (1.5g) = 5, and, so on, increasing in increments of 0.5 g/1 joint. During the TLFB, we asked about cannabis use and acquisition (e.g., typical source, amount purchased) (Collins et al., 2014). This TLFB interview helped train participants to estimate total daily cannabis quantity on the text surveys using approximately 0.5g = 1 joint.
2.4.4. Daily text message surveys
Our present analyses focus on 7 daily items assessing cannabis use and motives that were developed based on prior research, but adapted them to fit the character count parameters of text messaging that apply on some mobile phones. We queried daily cannabis frequency: “How many times did you use weed YESTERDAY, separated by at least 1 hour in between each use? Reply with a number: 0–24.” Those responding greater than 0 received items measuring quantity and motives. We assessed quantity with the item, “How much WEED did you have YESTERDAY?” Followed by response options: <0.5g (<1 joint), 0.5g (1 joint), 1g (2 joints), 1.5g (3 joints), 2g (4 joints), or 2.5g+ (5+ joints); coded 1 to 6, respectively, for analyses. To assist in reporting quantity, we provided participants with handouts including the images of cannabis used in the baseline TLFB. We assessed daily motives with items adapted from each subscale of the Marijuana Motives Measure (Simons et al., 1998), specifically selecting items with high factor loadings on each subscale and relevance to the study population. We asked “Did you use weed yesterday…” followed by: TO ENJOY THE FEELING? (enhancement); TO AVOID FEELING LEFT OUT? (conformity); TO EXPAND YOUR AWARENESS? (expansion); TO HELP YOU FEEL LESS DEPRESSED OR NERVOUS? (coping); and TO MAKE A SOCIAL GATHERING MORE FUN? (social). Response options were: “not at all,” “a little,” “somewhat,” or “a great deal,” coded 1 to 4, respectively to assess strength, or relevance, of motives on a specific day.
2.5. Data analyses
We calculated descriptive analyses (means, standard deviations, and proportions) to describe sample characteristics. To explore the relationship between daily motives for cannabis use and quantity consumed, we treated days as the unit of analysis and restricted focus to days where cannabis use was reported. We calculated variance inflation factors for each predictor, particularly due to concerns about the overlapping nature of some motives; none were larger than 1.27, indicating minimal impact of collinearity. We treated quantity of use as the outcome variable, and estimated the effects of enhancement, conformity, expansion, coping, and social motives as predictors, while controlling for indicators of ethnicity (dichotomized to African American vs. Other), gender (male/female), and receipt of public assistance (yes/no; as a proxy for socio-economic status) due to the higher rates of cannabis use among African Americans, men, and lower SES groups (Lanza et al., 2015; Redonnet et al., 2012). We only included cannabis use days (N=1,049) on which complete data for all independent variables were provided; thus missing data was not imputed for the primary analysis, consistent with prior studies (Buckner et al., 2015; Shrier and Scherer, 2014). To account for intra-class correlations arising from the nesting of days within individual, we used linear random effects regression models to estimate covariate effects, fit using the R (version 3.2.3) package lme4 (Bates et al., 2014). We used a single random intercept by individual to model intra-class correlations arising from stable within-individual characteristics. Although the outcome variable is discrete (a 6-point scale), all models presented showed excellent residual diagnostics, indicating approximately normal errors. Although with adequate sample sizes (as in this sample), the importance of the normal errors on the resulting inference about the regression coefficients has been shown to be minimal (Lumley et al., 2002).
3. Results
3.1. Baseline cannabis use
Descriptive TLFB data indicated that participants used cannabis on M=17.3 days (SD=10.6) of the 28 days preceding baseline. On use days, average quantity consumed was between 1.5 (coded 5) and 2.0g (coded 6; M=5.8, SD=6.4). Most participants (63.4%) reported blunts as their most frequent use method. There were a variety of purchasing patterns; the largest portion of participants reported purchasing 2–6 times per week (28.0%) and only 1 to 2 joints at a time (35.5%). Participants most often obtained cannabis from a known dealer (36.6%) or a friend/roommate (30.1%); 8.4% reported having a medical cannabis card. See Table 1 for additional details.
3.2. Daily reports of cannabis use
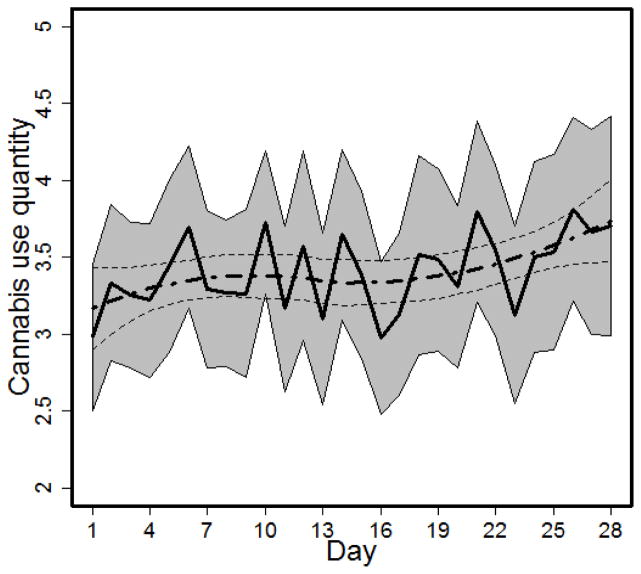
Participants reported using cannabis on 1,086 daily surveys (54.6% of 1,989 days participants provided responses) during the 28-day period. They used an average 3.2 times per use day (SD=3.5); the mean for daily quantity of use was 3.4 (SD=1.7) on the 6-point daily rating scale, reflecting between 1.0 grams and 1.5 grams (N=1,075 days due to missing responses), although the true mean may be higher because the upper response option was 2.5g+ (5+ joints)/ The breakdown for number of days participants reported different quantities of use, average daily frequency, and daily motives are shown in Table 1; enhancement was rated highest and conformity was rated lowest. Figure 1 displays the average quantity consumed per cannabis use day with pointwise 95% confidence intervals; which was not significantly time-varying (p=.32). Men (M=3.5, SD=1.8) and women (M=3.3, SD=1.7) and African Americans (M=3.4, SD=1.7) and individuals of other ethnic backgrounds (M=3.4, SD=1.8) did not significantly differ on mean daily quantity. Participants receiving public assistance reported significantly lower quantity than those not receiving public assistance (M=3.3, SD=1.7 vs. M=3.6, SD=1.7, p<.01), potentially reflecting less access to funds for purchasing cannabis
Figure 1.
Mean cannabis use quantity by survey day (range 1 to 28).
Note. Quantity was assessed using the following response options: <0.5g (<1 joint), 0.5g (1 joint), 1g (2 joints), 1.5g (3 joints), 2g (4 joints), or 2.5g+ (5+ joints); coded 1 to 6, respectively, for analyses. The solid black line represents cross-sectional estimates at each day, with point-wise confidence intervals in the gray shaded regions; the smooth curve estimates generated by a generalized additive model, with corresponding point-wise 95% CIs, are shown in dashed lines.
3.3. Daily associations between motives and cannabis use
Univariate correlations between daily reports of motives and quantity were statistically significant: enhancement (r=0.15, p<.001), conformity (r=0.09, p<.01), expansion (r=0.15, p<.001), coping (r=0.09, p<.01), and social (r=0.25, p<.001). Table 2 displays results from the multi-level linear regression analysis (clustering day within individual) including standardized and unstandardized coefficients, controlling for gender, ethnicity, and receipt of public assistance, (Model R2=.50). Using cannabis for enhancement (β=0.27), coping (β=0.15), and social motives (β=0.34) was significantly associated with higher quantities of cannabis used within a given day. Notably, expansion (β= 0.08) and conformity motives (β=−0.03) were not significantly associated with quantity. The estimated residual intra-class correlation (i.e., within-individual correlations between repeated measurements) was 0.43.
Table 2.
Associations between daily cannabis use motives and quantity consumed
| Predictors | Adjusted effects β (SE) | Adjusted effects Standardized β |
|---|---|---|
| Male (vs. Female) | 0.29 (0.27) | n/aa |
| African American (vs. Other) | 0.19 (0.26) | n/a |
| Receipt of Public Assistance (vs. no) | −0.16 (0.28) | n/a |
| Enhancement | 0.27 (0.05)*** | 0.31 |
| Coping | 0.15 (0.05)*** | 0.16 |
| Social | 0.34 (0.06)*** | 0.34 |
| Expansion | 0.08 (0.06) | 0.08 |
| Conformity | −0.04 (0.09) | −0.02 |
p<.001
Binary variables are were not standardized. The analytic sample size was N=1,049 days from 93 individuals because 37 daily reports were excluded due to missing variables (N=11 days were missing responses on quantity of cannabis consumption, and N=19 to 34 responses were missing across daily motive items).
4. Discussion
This study demonstrates same-day relationships between the strength of specific motives for using cannabis and self-reported quantity consumed, among at-risk emerging adults. When accounting for the strength and co-occurrence of multiple motives, on days when participants reported greater enhancement, social, and/or coping motives they reported using larger quantities of cannabis. Conformity and expansion motives were not associated with daily quantity when controlling for these other factors, unlike in prior cross-sectional work with other samples (Bravo et al., 2017; Zvolensky et al., 2007). However, similar to these prior cross-sectional studies, we found positive relationships between social, enhancement, and coping motives and quantity. Although these and other prior studies show higher motives are positively associated with cannabis consumption, severity, and psychosocial outcomes (e.g., anxiety, depression; not measured in the current analyses) at broader levels of measurement (Benschop et al., 2015; Bonn-Miller and Zvolensky, 2009b; Schlossarek et al., 2016; Simons et al., 1998; Zvolensky et al., 2007), this is one of the first studies to examine acute same-day relationships between cannabis motives and quantity.
In comparing our daily data to other event-based work we note that Shrier and colleagues previously found no significant relationships between positive (i.e., expansion, enhancement, and social) or negative (i.e., conformity and coping) motives and cannabis use at the event-level when measuring quantity based on number of hits (Shrier et al., 2013). Of note, these researchers asked participants their “main” reason for use and combined “positive” and “negative” motives, whereas we asked about the strength of five separate motive constructs simultaneously and measured total cannabis quantity throughout the day, as opposed to number of hits which could be more difficult to recall. These methodological differences, in addition to sample characteristics (e.g., Shrier and colleagues focused on adolescents, the current sample included emerging adults), may help explain our different results. Our findings are relatively consistent with work by Buckner and colleagues’ (2015) among emerging adults. They reported that most cannabis use episodes involved enhancement and coping motives, the most strongly endorsed motives by our participants, followed by social and expansion motives. Conformity was rarely involved in cannabis use episodes in this prior work and, similarly, we found conformity had the lowest daily ratings.
Our findings show small-to-medium associations between same-day motives and quantity of cannabis use, thereby further supporting the need to address motives explicitly in cannabis use interventions for young people. Tailoring interventions to identify alternative ways to satisfy motives related to enhancement, social, and coping-related cannabis use could enhance efficacy by reducing use, potentially preventing the associated negative consequences. For example, individuals who use cannabis to cope may benefit from psychosocial treatment or strategies to manage negative affective experiences. Individuals with social and enhancement motives may benefit from strategies to help identify alternative leisure activities, positive social supports, and/or refusal and harm reduction strategies to use in social situations. Further, because previous research has shown that cannabis use motives can change as a result of interventions (Blevins et al., 2016a), the presence of same-day relationships in our data suggests more research is needed to develop interventions that help individuals address their specific motives. Effective interventions may include face-to-face sessions (Blevins et al., 2016a) that are supplemented with just-in-time or ecological momentary interventions to send intervention prompts in contexts when these motivations are increasingly acute to provide adaptive and immediate strategies (Shrier et al., 2014).
Limitations of our study include potential concerns about generalizability and representativeness. Data were obtained from a larger study involving a clinical sample with inclusion criteria based on drug use and sexual risk, thus results may not fully reflect those of other emerging adults. While longitudinal data are a strength of this investigation, participants’ reports may still be biased by retrospective recall for past-day cannabis use, social desirability, or demand characteristics. Further, missing data for incomplete daily surveys could potentially reflect different patterns of motives and cannabis use. No gold standard measurement for quantity of cannabis consumption exists, although we trained participants in a procedure to estimate their daily quantity of use, measuring quantity remains a challenge in the field given varying potency and methods of administration (see van der Pol et al., 2013). Estimates may be also complicated when individuals share joints or blunts with others or are estimating consumption when intoxicated. Differences in baseline daily cannabis quantity estimates determined via the interviewer-administered TLFB and those obtained from self-report longitudinal text message daily surveys further highlight the challenges in measuring cannabis quantity via multiple methods, but may also reflect changes in use patterns after baseline, assessment reactivity, or lack of daily survey reporting on high consumption days. In addition, there may be possible ceiling effects in the daily survey estimates given our highest response option was 2.5g+. However, there may be strengths in our quantity measure; we conducted the adjusted model substituting daily frequency as the dependent measure and found the same pattern of results; due to problematic residual diagnostics in the daily frequency model, we feel more confident in the use quantity model results. Future research using similar quantity-based items may benefit from expanding the upper limit assessed, given that the highest response choice (2.5g+) was chosen in about 1 in 5 daily reports of quantity. Finally, although we did not include a method for assessing careless responding in our daily surveys, we note that the texting system was set to only allow for valid responses (e.g., Y or N for yes/no responses, restricted range for numeric responses), which could inhibit some careless responding.
Although our study begins to address a gap in the literature regarding daily-level cannabis use, our data do not represent all possible motives for cannabis use. Because we were mindful of participant burden in completing daily assessments, we chose to focus on the five-factor model of cannabis motives. Future daily and event level research should incorporate more expansive lists of motives (Lee et al., 2009), which could further inform the tailoring of interventions. In addition, advancing technology (e.g., increasing use of smartphones, mobile applications, passive data collection) may support more extensive motives assessments and/or EMAs, particularly as the digital divide closes and more individuals have access to such technologies (Anderson and Rainie, 2015). In particular, emerging adults continue to represent a population where cannabis use reaches its peak. Although many will not experience significant consequences of cannabis use or need for treatment (Center for Behavioral Health Statistics and Quality, 2016), understanding proximal factors influencing decisions to use cannabis may be a critical next step in harm reduction focused cognitive-behavioral approaches to reduce use and prevent cannabis-related consequences.
Acknowledgments
We wish to thank the patients and staff at Hurley Medical Center.
Funding Source: National Institute on Drug Abuse
References
- Abadi MH, Shamblen SR, Thompson K, Collins DA, Johnson K. Influence of risk and protective factors on substance use outcomes across developmental periods: a comparison of youth and young adults. Subst use misuse. 2011;46:1604–1612. doi: 10.3109/10826084.2011.598598. [DOI] [PubMed] [Google Scholar]
- Anderson M, Rainie L. Pew Research Center. Technology Device Ownership. 2015;2015:29. [Google Scholar]
- Azofeifa A, Mattson ME, Schauer G, McAfee T, Grant A, Lyerla R. National estimates of marijuana use and related indicators - National Survey on Drug Use and Health, United States, 2002–2014. Morb Mortal Wkly Rep Surveill Summ. 2016;65:1–25. doi: 10.15585/mmwr.ss6511a1. [DOI] [PubMed] [Google Scholar]
- Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. 2014 arXiv preprint arXiv:1406.5823. [Google Scholar]
- Benschop A, Liebregts N, van der Pol P, Schaap R, Buisman R, van Laar M, van den Brink W, de Graaf R, Korf DJ. Reliability and validity of the Marijuana Motives Measure among young adult frequent cannabis users and associations with cannabis dependence. Addict Behav. 2015;40:91–95. doi: 10.1016/j.addbeh.2014.09.003. [DOI] [PubMed] [Google Scholar]
- Blevins CE, Banes KE, Stephens RS, Walker DD, Roffman RA. Change in motives among frequent cannabis-using adolescents: Predicting treatment outcomes. Drug Alcohol Depend. 2016a;167:175–181. doi: 10.1016/j.drugalcdep.2016.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins CE, Banes KE, Stephens RS, Walker DD, Roffman RA. Motives for marijuana use among heavy-using high school students: an analysis of structure and utility of the comprehensive marijuana motives questionnaire. Addict Behav. 2016b;57:42–47. doi: 10.1016/j.addbeh.2016.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonar EE, Cunningham RM, Collins RL, Cranford JA, Chermack ST, Zimmerman MA, Blow FC, Walton MA. Feasibility and Acceptability of Text Messaging to Assess Daily Substance Use and Sexual Behaviors among Urban Emerging Adults. Addiction Research & Theory. doi: 10.1080/16066359.2017.1310205. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonar EE, Koocher GP, Benoit MF, Collins RL, Cranford JA, Walton MA. Perceived risks and benefits in a text message study of substance abuse and sexual behavior. Ethics & Behavior. doi: 10.1080/10508422.2017.1293541. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonar EE, Whiteside LK, Walton MA, Zimmerman MA, Booth BM, Blow FC, Cunningham RM. Prevalence and correlates of HIV risk among adolescents and young adults reporting drug use: Data from an urban emergency department in the United States. Journal of HIV/AIDS & Social Services. 2016;15:3–28. [PMC free article] [PubMed] [Google Scholar]
- Bonn-Miller MO, Boden MT, Bucossi MM, Babson KA. Self-reported cannabis use characteristics, patterns and helpfulness among medical cannabis users. Am J Drug Alcohol Abuse. 2014;40:23–30. doi: 10.3109/00952990.2013.821477. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ. An evaluation of the nature of marijuana use and its motives among young adult active users. Am J Addict. 2009a;18:409–416. doi: 10.3109/10550490903077705. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ. An evaluation of the nature of marijuana use and its motives among young adult active users. Am J Addict. 2009b;18:409–416. doi: 10.3109/10550490903077705. [DOI] [PubMed] [Google Scholar]
- Bravo AJ, Prince MA, Pearson MR. Can I Use Marijuana Safely? An Examination of Distal Antecedents, Marijuana Protective Behavioral Strategies, and Marijuana Outcomes. J Stud Alcohol Drugs. 2017;78:203–212. doi: 10.15288/jsad.2017.78.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Crosby RD, Wonderlich SA, Schmidt NB. Social anxiety and cannabis use: an analysis from ecological momentary assessment. J Anxiety Disord. 2012;26:297–304. doi: 10.1016/j.janxdis.2011.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Zvolensky MJ, Crosby RD, Wonderlich SA, Ecker AH, Richter A. Antecedents and consequences of cannabis use among racially diverse cannabis users: an analysis from Ecological Momentary Assessment. Drug Alcohol Depend. 2015;147:20–25. doi: 10.1016/j.drugalcdep.2014.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Zvolensky MJ, Smits JA, Norton PJ, Crosby RD, Wonderlich SA, Schmidt NB. Anxiety sensitivity and marijuana use: an analysis from ecological momentary assessment. Depress Anxiety. 2011;28:420–426. doi: 10.1002/da.20816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. 2015 National Survey on Drug Use and Health: Detailed tables. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2016. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) 2011 Behavioral Risk Factor Surveillance System Survey Questionnaire. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, Georgia: 2012. [Google Scholar]
- Collins RL, Vincent PC, Yu J, Liu L, Epstein LH. A behavioral economic approach to assessing demand for marijuana. Exp Clin Psychopharmacol. 2014;22:211–221. doi: 10.1037/a0035318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychol Assess. 1994;6:117. [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: a motivational model of alcohol use. J Pers Soc Psychol. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Cunningham RM, Ranney M, Newton M, Woodhull W, Zimmerman M, Walton MA. Characteristics of youth seeking emergency care for assault injuries. Pediatrics. 2014;133:e96–e105. doi: 10.1542/peds.2013-1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Walton MA, Trowbridge M, Weber J, Outman R, Benway A, Maio R. Correlates of violent behavior among adolescents presenting to an urban emergency department. J Pediatr. 2006;149:770–776. doi: 10.1016/j.jpeds.2006.08.073. [DOI] [PubMed] [Google Scholar]
- Farris SG, Metrik J, Bonn-Miller MO, Kahler CW, Zvolensky MJ. Anxiety Sensitivity and Distress Intolerance as Predictors of Cannabis Dependence Symptoms, Problems, and Craving: The Mediating Role of Coping Motives. J Stud Alcohol Drugs. 2016;77:889–897. doi: 10.15288/jsad.2016.77.889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris KM. [accessed on April 16, 2017];The National Longitudinal Study of Adolescent to Adult Health (Add Health), Waves I & II, 1994–1996; Wave III, 2001–2002; Wave IV, 2007–2009 [machine-readable data file and documentation] 2009 http://www.cpc.unc.edu/projects/addhealth/codebooks/wave1.
- Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, Jung J, Pickering RP, Ruan WJ, Smith SM, Huang B, Grant BF. Prevalence of Marijuana Use Disorders in the United States Between 2001–2002 and 2012–2013. JAMA Psychiatry. 2015;72:1235–1242. doi: 10.1001/jamapsychiatry.2015.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humeniuk R, Ali R, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J, de Lacerda RB, Ling W, Marsden J, Monteiro M, Nhiwatiwa S, Pal H, Poznyak V, Simon S. Validation of the Alcohol, Smoking And Substance Involvement Screening Test (ASSIST) Addiction. 2008;103:1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- Johnston LD, Bachman JG, O’Malley PM, Schulenberg JE. Monitoring the future: A continuing study of American youth (12th-grade survey), 2010: Core data codebook. Inter-university consortium for political and social research; Ann Arbor. 2010a. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Miech RA. Monitoring the Future national survey results on drug use, 1975–2015: Volume 2, College students and adults ages 19–55. Institute for Social Research, The University of Michigan; Ann Arbor: 2016. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. HIV/AIDS: Risk & Protective Behaviors among American Young Adults, 2004–2008. National Institutes of Health; 2010b. [Google Scholar]
- Keyes KM, Schulenberg JE, O’Malley PM, Johnston LD, Bachman JG, Li G, Hasin D. The social norms of birth cohorts and adolescent marijuana use in the United States, 1976–2007. Addiction. 2011;106:1790–1800. doi: 10.1111/j.1360-0443.2011.03485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Vasilenko SA, Dziak JJ, Butera NM. Trends Among U.S. High School Seniors in Recent Marijuana Use and Associations With Other Substances: 1976–2013. J Adolesc Health. 2015;57:198–204. doi: 10.1016/j.jadohealth.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CM, Neighbors C, Hendershot CS, Grossbard JR. Development and preliminary validation of a comprehensive marijuana motives questionnaire. J Stud Alcohol Drugs. 2009;70:279–287. doi: 10.15288/jsad.2009.70.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CM, Neighbors C, Woods BA. Marijuana motives: young adults’ reasons for using marijuana. Addict Behav. 2007;32:1384–1394. doi: 10.1016/j.addbeh.2006.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health data sets. Annu Rev Public Health. 2002;23:151–169. doi: 10.1146/annurev.publhealth.23.100901.140546. [DOI] [PubMed] [Google Scholar]
- Nahum-Shani I, Smith SN, Spring BJ, Collins LM, Witkiewitz K, Tewari A, Murphy SA. Just-in-Time Adaptive Interventions (JITAIs) in Mobile Health: Key Components and Design Principles for Ongoing Health Behavior Support. Ann Behav Med. 2016 doi: 10.1007/s12160-016-9830-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranney ML, Choo EK, Spirito A, Mello MJ. Adolescents’ Preference for Technology-Based Emergency Department Behavioral Interventions: Does It Depend on Risky Behaviors? Pediatr Emerg Care. 2013;29:475–481. doi: 10.1097/PEC.0b013e31828a322f. [DOI] [PubMed] [Google Scholar]
- Redonnet B, Chollet A, Fombonne E, Bowes L, Melchior M. Tobacco, alcohol, cannabis and other illegal drug use among young adults: the socioeconomic context. Drug Alcohol Depend. 2012;121:231–239. doi: 10.1016/j.drugalcdep.2011.09.002. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. John Wiley & Sons; 2008. pp. 43–64. [Google Scholar]
- Schlossarek S, Kempkensteffen J, Reimer J, Verthein U. Psychosocial Determinants of Cannabis Dependence: A Systematic Review of the Literature. Eur Addict Res. 2016;22:131–144. doi: 10.1159/000441777. [DOI] [PubMed] [Google Scholar]
- Scott-Sheldon LA, Carey MP, Carey KB. Alcohol and risky sexual behavior among heavy drinking college students. AIDS Behav. 2010;14:845–853. doi: 10.1007/s10461-008-9426-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrier LA, Rhoads A, Burke P, Walls C, Blood EA. Real-time, contextual intervention using mobile technology to reduce marijuana use among youth: A pilot study. Addict Behav. 2014;39:173–180. doi: 10.1016/j.addbeh.2013.09.028. [DOI] [PubMed] [Google Scholar]
- Shrier LA, Scherer EB. It depends on when you ask: motives for using marijuana assessed before versus after a marijuana use event. Addict Behav. 2014;39:1759–1765. doi: 10.1016/j.addbeh.2014.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrier LA, Walls C, Rhoads A, Blood EA. Individual and contextual predictors of severity of marijuana use events among young frequent users. Addict Behav. 2013;38:1448–1456. doi: 10.1016/j.addbeh.2012.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silins E, Horwood LJ, Patton GC, Fergusson DM, Olsson CA, Hutchinson DM, Spry E, Toumbourou JW, Degenhardt L, Swift W, Coffey C, Tait RJ, Letcher P, Copeland J, Mattick RP. Young adult sequelae of adolescent cannabis use: an integrative analysis. Lancet Psychiatry. 2014;1:286–293. doi: 10.1016/S2215-0366(14)70307-4. [DOI] [PubMed] [Google Scholar]
- Simons J, Correia CJ, Carey KB, Borsari BE. Validating a five-factor marijuana motives measure: Relations with use, problems, and alcohol motives. J Couns Psychol. 1998;45:265. [Google Scholar]
- Smith GR, Babor TF, Burnam MA, Mosley CL, Rost KM, Burns B. Substance Abuse Outcomes Module: User’s Manual. University of Arkansas for Medical Sciences; Little Rock, AR: 1996. [Google Scholar]
- Smith GR, Burnam MA, Mosley CL, Hollenberg JA, Mancino M, Grimes W. Reliability and validity of the substance abuse outcomes module. Psychiatr Serv. 2006;57:1452–1460. doi: 10.1176/ps.2006.57.10.1452. [DOI] [PubMed] [Google Scholar]
- Tang Z, Orwin RG. Marijuana initiation among American youth and its risks as dynamic processes: Prospective findings from a national longitudinal study. Subst Use Misuse. 2009;44:195–211. doi: 10.1080/10826080802347636. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. 2010–2014 5-Year American Community Survey. Camden, New Jersey: 2015a. [accessed on April 6 2016]. http://factfinder.census.gov. [Google Scholar]
- U.S. Census Bureau. 2010–2014 5-Year American Community Survey. Flint, Michigan: 2015b. [accessed on April 6 2016]. http://factfinder.census.gov. [Google Scholar]
- U.S. Census Bureau. 2010–2014 5-Year American Community Survey. Hartford, Connecticut: 2015c. [accessed on April 6 2016]. http://factfinder.census.gov. [Google Scholar]
- U.S. Census Bureau. 2010–2014 5-Year American Community Survey. United States: 2015d. [accessed on April 6 2016]. http://factfinder.census.gov. [Google Scholar]
- U.S. Census Bureau. State and County QuickFacts. Flint, Michigan: 2015e. [accessed on February 15 2016]. http://quickfacts.census.gov/qfd/states/26/2629000.html. [Google Scholar]
- United States Department of Health and Human Services, National Institutes of Health, National Institute on Drug Abuse. Drug Abuse Treatment Outcome Study--Adolescent (DATOS-A), 1993–1995: [United States]. ICPSR03404-v3 Inter-university Consortium for Political and Social Research [distributor]; Ann Arbor, MI. 2008. [Google Scholar]
- van der Pol P, Liebregts N, de Graaf R, Korf DJ, van den Brink W, van Laar M. Validation of self-reported cannabis dose and potency: an ecological study. Addiction. 2013;108:1801–1808. doi: 10.1111/add.12226. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Swanson JM, Evins AE, DeLisi LE, Meier MH, Gonzalez R, Bloomfield MA, Curran HV, Baler R. Effects of Cannabis Use on Human Behavior, Including Cognition, Motivation, and Psychosis: A Review. JAMA Psychiatry. 2016;73:292–297. doi: 10.1001/jamapsychiatry.2015.3278. [DOI] [PubMed] [Google Scholar]
- Walton MA, Resko S, Whiteside L, Zimmerman MA, Chermack ST, Cunningham RM. Sexual risk behaviors among teens at an inner city emergency department: Relationship to Violent Behaviors and Substance Use. J Adolesc Health. 2011;48:303–305. doi: 10.1016/j.jadohealth.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinhardt LS, Carey MP, Maisto SA, Carey KB, Cohen MM, Wickramasinghe SM. Reliability of the timeline follow-back sexual behavior interview. Ann Behav Med. 1998;20:25–30. doi: 10.1007/BF02893805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002;97:1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- Wilson KM, Klein JD. Adolescents who use the emergency department as their usual source of care. Arch Pediatr Adolesc Med. 2000;154:361–365. doi: 10.1001/archpedi.154.4.361. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Vujanovic AA, Bernstein A, Bonn-Miller MO, Marshall EC, Leyro TM. Marijuana use motives: A confirmatory test and evaluation among young adult marijuana users. Addict Behav. 2007;32:3122–3130. doi: 10.1016/j.addbeh.2007.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]