Abstract
Background
Excessive alcohol use among the homeless may contribute to their high rates of emergency department use. Survey-based studies have provided some information on the relation between alcohol and emergency department use among the homeless.
Methods
This study used an intensive schedule of random breath collections and self-report assessments to examine the relation between emergency department utilization and alcohol use in homeless alcohol-dependent adults. Data were from homeless alcohol-dependent adults (N = 116) who were participating in a therapeutic workplace that provided job-skills training every weekday for 26 weeks. Breath-sample collections and assessments of self-reported alcohol use were scheduled each week, an average of twice per week per participant, at random times between 9:00 AM and 5:00 PM. Participants received $35 for each breath sample collected. Self-reports of emergency department use were assessed throughout the study.
Results
Thirty-four percent of participants reported attending an emergency department and reported an average of 2.2 emergency department visits (range 1-10 visits). Alcohol intoxication was the most common reason for emergency department use. Participants who used the emergency department had significantly more alcohol-positive breath samples and more self-reported heavy alcohol use than participants who did not use the emergency department.
Conclusions
This study provided a rare intensive assessment of alcohol and emergency department use in homeless alcohol-dependent adults over an extended period. Emergency department use was high and was significantly related to indices of alcohol use.
Keywords: alcohol, emergency department, heavy drinking, homeless, therapeutic workplace
1. Introduction
People who are homeless face numerous barriers to accessing health care and use acute care services, such as emergency departments, at high rates (Kushel et al., 2001, 2002; Martinez and Burt, 2006; Larimer et al., 2009). Compared to the general population, people who are homeless are three to four times more likely to have at least one emergency department visit annually (Kushel et al., 2001, 2002), and are more likely to be repeat emergency department users (Doran et al., 2013, Ku et al., 2010; Mandelberg et al., 2000). Heavy use of the emergency department in general can be problematic because it contributes to high health care costs and inefficiency (Adams, 2013). Identification of the reasons for the high rates of emergency department use among the homeless could be used to guide interventions to reduce costs, improve quality of care, and address unmet health care needs.
One factor that may be particularly relevant to the high rates of emergency department use among the homeless is excessive alcohol use. Problematic alcohol use is common among the homeless; some estimates show that as many as half of homeless adults are dependent on alcohol (Fazel et al., 2008). Studies of emergency department use among the homeless have provided some information on the relation between alcohol and emergency department use. In a survey-based study with 2,578 homeless adults, repeated (4 or more visits in the previous year) emergency department use was associated with self-reported alcohol or drug problems (Kushel et al., 2002). In another study that examined Medicaid administrative data from 6,494 homeless adults, alcohol-related disorders were the most common reason for an emergency department visit (Lin et al., 2015). In contrast to these studies, a secondary analysis of survey data from 2,974 homeless adults did not find an association between alcohol abuse and emergency department use (Kushel et al., 2001). To further explore the relation between alcohol and emergency department use among the homeless, the present study focused on a sample of homeless adults with known alcohol use problems. The present study used an intensive longitudinal schedule of random breath-alcohol collections and self-report assessments to examine the relation between emergency department utilization and measures of alcohol use in homeless alcohol-dependent adults.
2. Material and methods
2.1. Design and description of the main trial
Data for this analysis were collected during a randomized clinical trial that evaluated whether a therapeutic workplace could promote alcohol abstinence in homeless and unemployed alcohol-dependent adults. The therapeutic workplace is an employment-based intervention designed to promote drug and alcohol abstinence and education and job skills in individuals with chronic unemployment and drug and alcohol addiction. Participants were invited to work in the therapeutic workplace for 26 weeks and were randomized to one of three conditions: a control condition that offered job-skills training in the therapeutic workplace and two experimental conditions – one assessing the impact of payment for participation in training and one assessing the impact of requiring alcohol abstinence to access paid training. The primary outcome measures and detailed methods have been reported previously (Koffarnus et al., 2011). Methods relevant to the present analysis are provided below.
2.2. Participants
Participants were recruited from an inpatient detoxification unit and community agencies that provided services to the homeless in Baltimore, MD. Participants were at least 18 years old, were unemployed, met DSM-IV criteria for alcohol dependence, and reported that they were currently homeless (i.e., stayed in a shelter, on the street, or in an abandoned house at least one night over the past 30 days; lost public housing assistance recently or were at risk of losing residence; or slept in more than two places over the past 30 days).
2.3. Breath sample collection and testing
Randomly-scheduled breath samples were collected and tested to provide a biological measure of alcohol use. On average, two breath samples were randomly scheduled per week for each participant during the hours of 9:00 AM to 5:00 PM. At scheduled times, research staff would call or page participants on cell phones or pagers that were assigned to them at the start of the study. If research staff were able to collect a breath sample from the participants within 60 minutes of phone or page contact, the participant received a $35 voucher that was exchangeable for goods and services. Community/field visits were used for some of the breath-sample collections if the participant was not attending the therapeutic workplace at the time the collection was scheduled. Breath samples were tested for alcohol using an Alco-Sensor III device.
2.4. Self-reports of alcohol and emergency department use
Self-reported alcohol use was assessed at each randomly-scheduled breath sample collection. Participants were asked whether they consumed any alcohol during the 24 hours prior to the collection and if so, whether they engaged in heavy drinking (≥ 4 drinks for women and ≥ 5 drinks for men). Self-report of a visit to the emergency department was collected and documented for adverse event reports. Adverse events were collected as a part of routine study assessments conducted each month and throughout the study, whenever therapeutic workplace staff had contact with participants. Because participants could attend the therapeutic workplace every weekday, workplace staff had frequent opportunities to monitor emergency department use.
2.5. Data Analyses
Breath samples with a blood alcohol level (BAL) greater than or equal to 0.004 g/dl were considered positive for alcohol. Heavy drinking was defined as 4 or more drinks for women and 5 or more drinks for men in a 24-hour period. Two methods of handling missing data were used, in which breath collections and self-report assessments that were scheduled but not collected were considered missing (missing missing) or were coded as the adverse outcome (missing positive). Unpaired t-tests were conducted to compare alcohol use among participants who did and did not use the emergency department. Mixed-effects longitudinal logistic regression was used to determine the odds of an emergency department visit as a function of alcohol use in the preceding week. Alcohol use across a week was used as the predictor in the longitudinal logistic regression because it allowed for the inclusion of both of the weekly randomly scheduled breath-sample collections. Statistically significant differences were assessed at a significance level of .05.
3. Results
3.1. Participant demographics
The sample was predominantly male (80%) and white (51%), with an average age of 43.0 (SD=8.7) years. At intake, all participants met DSM-IV criteria for alcohol dependence and reported an average of 23.7 (SD=8.1) drinking days out of the past 30 days and an average of 24.7 (SD=16.7) drinks per drinking day in the past 30 days. All participants were currently homeless and reported that they stayed or slept in a recovery house or homeless shelter on an average of 5.3 (SD=9.3) days out of the past 30 days and stayed or slept on the street an average of 13.6 (SD=12.1) days out of the past 30 days.
3.2. Frequency of and reasons for emergency department visits
A total of 39 out of the 116 participants (34%) reported receiving care in an emergency department. Of these 39 participants, 59% reported having had one emergency department visit, 21% reported 2 or 3 visits, and 21% reported 4 or more visits. On average, these participants made 2.2 emergency department visits (range 1-10 visits) during the study period. A total of 86 emergency department visits were made. Alcohol intoxication was the most common reason for an emergency department visit (number of visits = 25; 29.1%), followed by medical problems (n=16; 18.6%), seizure (n=15; 17.4%), rape or assault (n=14; 16.3%), psychological problems (n=10; 11.6%), alcohol withdrawal (n=4; 4.7%), and drug or medication overdose (n=2; 2.3%).
3.3. Emergency department visits and alcohol use
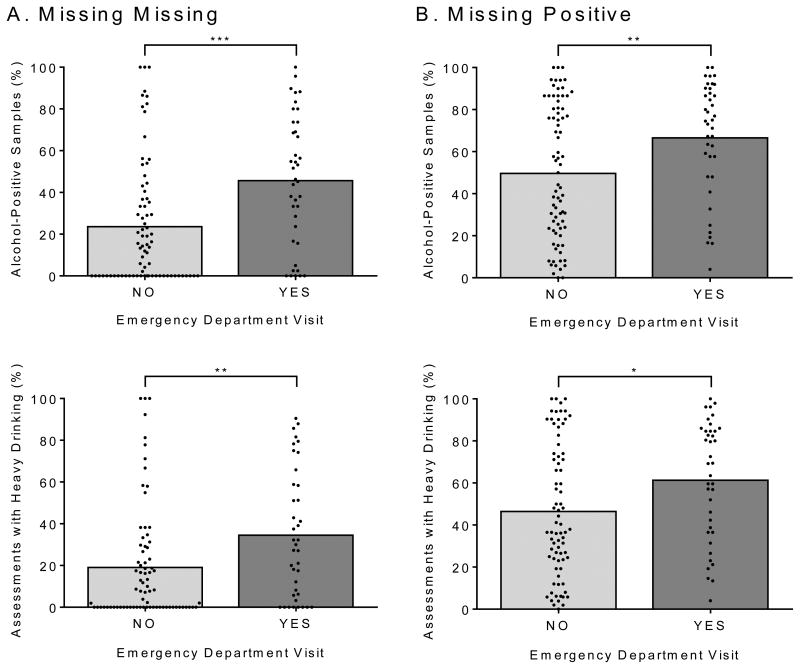
Figure 1 shows the relation between emergency department visits and measures of alcohol use for the missing-missing (A) and missing-positive (B) analyses. The percentage of alcohol-positive breath samples was significantly higher for participants who used the emergency department compared to participants who did not [missing missing: t(114) = 3.711, p < .001; missing positive: t(114) = 2.822, p = .006]. The percentage of randomly-scheduled assessments at which participants reported heavy drinking in the prior 24 hours was significantly higher for participants who used the emergency department compared to participants who did not [missing missing: t(114) = 2.762, p = .007; missing positive: t(114) = 2.482, p = .015]. Sixty-five percent of the scheduled breath samples were collected and 31% were positive for alcohol. The percentage of samples collected did not significantly differ between participants who did and did not use the emergency department [62.9% and 66.1%, respectively; t(114) = 0.544, p = .587].
Figure 1.
The relation between emergency department visits and measures of alcohol use from randomly-scheduled breath sample collections and self-report assessments. Two methods of handling missing data were used, in which breath collections and self-report assessments that were scheduled but not collected were considered missing (Panel A, Missing Missing) or were coded as the adverse outcome (Panel B, Missing Positive). The graphs in the top panel show the percentage of alcohol-positive breath samples and the graphs in the bottom panel show the percentage of self-report assessments with heavy drinking for participants who did and did not use the emergency department. The filled circles show percentages for individual participants and the bars show group means. *p < .05, **p < .01, and ***p < .001.
In the longitudinal logistic models, alcohol-positive breath samples in the preceding week significantly predicted emergency department visits in the following week in the missing-missing analyses (OR = 2.66, 95% CI: 1.186 – 5.953, p = .018). In the missing-positive analyses, the relation was attenuated and not statistically significant (OR = 1.60, 95% CI: 0.671 – 3.792, p = .291).
4. Discussion
This study provided a rare intensive assessment of alcohol use and emergency department utilization in homeless alcohol-dependent adults over an extended period of time. Emergency department use was high and concentrated in about one-third of the sample of homeless alcohol-dependent adults. Repeated emergency department use (more than 1 visit) was common. The high rate of and frequent emergency department use was similar to that reported in prior studies with homeless adults (Kushel et al., 2002; Lin et al., 2015). Alcohol intoxication was the most common reason for an emergency department visit. Furthermore, emergency department use was highest among those homeless adults who used alcohol as assessed by randomly-scheduled breath alcohol collections and self-report assessments. Those with the highest rates of emergency department use had more alcohol-positive breath samples and more self-reported heavy alcohol use. In the week preceding an emergency department visit, participants were likely to provide alcohol-positive breath samples. Taken together, these data suggest that alcohol is a key driver of emergency department use among homeless alcohol-dependent adults.
Prior research has suggested a number of reasons for high rates of emergency department use among people experiencing homelessness. These reasons include a high prevalence of unintentional injuries and exposure to violence while homeless, as well as a high prevalence of drug use and mental illness (Ku et al., 2010; Kushel et al., 2001, 2002; Padgett and Struening, 1992; Padgett et al., 1995). Similar to these prior studies, emergency department use in the present study occurred for a variety of reasons, including medical problems or seizure, rape or assault, psychological problems, and drug or medication overdose. Most emergency department visits in the present study were directly attributable to alcohol use (i.e., alcohol intoxication and withdrawal); however, given the high rates of excessive alcohol use in the present sample, it is possible that alcohol use may have contributed to other conditions that required medical care in the emergency department.
A few study limitations should be noted. First, data for this analysis were collected during a three-condition randomized trial that evaluated whether a therapeutic workplace could promote alcohol abstinence in homeless alcohol-dependent adults. The present results may or may not generalize to the overall population of homeless adults with alcohol use disorders. However, conducting the present study in the context of the trial did allow for an intensive assessment of the relation between alcohol and emergency department use. Second, our conclusions are limited by the correlational nature of the data. We cannot know for certain whether alcohol use led to emergency department visits, or whether visits to the emergency department are associated with some unknown factor, such as insurance status or the ability to access primary care in ambulatory settings. Third, the collection rate of the random breath samples was 65%; it is possible that some alcohol use was not captured by these assessments. The rate of missing data may have influenced results of the mixed-effects longitudinal logistic regression as results were significant for the missing-missing but not the missing-positive analyses. Obtaining accurate measures of alcohol use in general can be challenging due to the short detection window (several hours) of blood alcohol levels. Future research may benefit from the use of transdermal alcohol monitors to continuously and objectively monitor alcohol use (Dougherty et al., 2014).
The number of annual emergency department visits increased from 103 million visits in 1999 to 136 million visits in 2009 in the US. This increase in emergency department use has led to overcrowding, increased wait times for both minor and serious problems, and increased health care costs (National Center for Health Statistics, 2011). It has been suggested that efforts aimed at reducing overuse of the emergency department would benefit from focusing on those patients who use the emergency department most frequently (Adams, 2013). The present findings and other similar studies suggest that the homeless are a patient population that frequently uses the emergency department at high rates (Doran et al., 2013; Kushel et al., 2001, 2002; Mandelberg et al., 2000). Furthermore, alcohol-related problems and alcohol use may be key drivers of emergency department use among homeless alcohol-dependent adults. The development of effective interventions for homeless adults who use alcohol persistently may be helpful in reducing emergency department use and associated costs.
Highlights.
Alcohol intoxication was the most common reason for emergency department use
Homeless adults with emergency department use had more alcohol-positive breath samples
Homeless adults with emergency department use had higher rates of heavy alcohol use
Acknowledgments
Role of Funding Source: This work was supported by the National Institutes of Health grant numbers R01 AA12154, R01 DA037314, and T32 DA07209. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. These funding sponsors were not involved in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Footnotes
Contributions: All authors contributed to the conceptualization and design of the analyses. AH and CW conducted the analyses. AH and KS managed the literature search. AH wrote the first draft of the manuscript. BJ, SS, CW, MF, GB, and KS provided substantive and conceptual feedback on all drafts. All authors contributed to and have approved the final manuscript.
Conflict of Interest: Dr. Bigelow has received research support from Orexo Pharmaceuticals and consulted for Transcept Pharmaceuticals. All other authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adams JG. Emergency department overuse: perceptions and solutions. JAMA. 2013;309:1173–1174. doi: 10.1001/jama.2013.2476. [DOI] [PubMed] [Google Scholar]
- Doran KM, Raven MC, Rosenheck RA. What drives frequent emergency department use in an integrated health system? National data from the Veterans Health Administration. Ann Emerg Med. 2013;62:151–159. doi: 10.1016/j.annemergmed.2013.02.016. [DOI] [PubMed] [Google Scholar]
- Dougherty DM, Hill-Kapturczak N, Liang Y, Karns TE, Cates SE, Lake SL, Mullen J, Roache JD. Use of continuous transdermal alcohol monitoring during a contingency management procedure to reduce excessive alcohol use. Drug Alcohol Depend. 2014;142:301–306. doi: 10.1016/j.drugalcdep.2014.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5:1670–1681. doi: 10.1371/journal.pmed.0050225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffarnus MN, Wong CJ, Diemer K, Needham M, Hampton J, Fingerhood M, Silverman K. A randomized clinical trial of a therapeutic workplace for chronically unemployed, homeless, alcohol-dependent adults. Alcohol Alcohol. 2011;46:561–569. doi: 10.1093/alcalc/agr057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ku BS, Scott KC, Kertesz SG, Pitts SR. Factors associated with use of urban emergency departments by the US homeless population. Public Health Rep. 2010;125:398–405. doi: 10.1177/003335491012500308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: Results from a community-based study. Am J Public Health. 2002;92:778–784. doi: 10.2105/ajph.92.5.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285:200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Malone DK, Garner MD, Atkins DC, Burlingham B, Lonczak HS, Tanzer K, Ginzler J, Clifasefi SL, Hobson WG, Marlatt GA. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301:1349–1357. doi: 10.1001/jama.2009.414. [DOI] [PubMed] [Google Scholar]
- Lin WC, Bharel M, Zhang J, O'Connell E, Clark RE. Frequent emergency department visits and hospitalizations among homeless people with Medicaid: Implications for Medicaid expansion. Am J Public Health. 2015;105:S716–S722. doi: 10.2105/AJPH.2015.302693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandelberg JH, Kuhn RE, Kohn MA. Epidemiologic analysis of an urban, public emergency department's frequent users. Acad Emerg Med. 2000;7:637–646. doi: 10.1111/j.1553-2712.2000.tb02037.x. [DOI] [PubMed] [Google Scholar]
- Martinez TE, Burt MR. Impact of permanent supportive housing on the use of acute care health services by homeless adults. Psychiatr Serv. 2006;57:992–999. doi: 10.1176/ps.2006.57.7.992. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. National Hospital Ambulatory Medical Care Survey: 2011. Emergency Department Summary Tables. 2011 Retrieved from http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2011_ed_web_tables.pdf.
- Padgett DK, Struening EL, Andrews H, Pittman J. Predictors of emergency room use by homeless adults in New York City: The influence of predisposing, enabling and need factors. Soc Sci Med. 1995;41:547–556. doi: 10.1016/0277-9536(94)00364-y. [DOI] [PubMed] [Google Scholar]
- Padgett DK, Struening EL. Victimization and traumatic injuries among the homeless: Associations with alcohol, drug, and mental problems. Am J Orthopsychiat. 1992;62:525–534. doi: 10.1037/h0079369. [DOI] [PubMed] [Google Scholar]