Abstract
Cases of cerebrospinal fluid (CSF) rhinorrhea due to clival fracture are rare. We present a case of bacterial meningitis with CSF rhinorrhea after a clival fracture. Heavily T2-weighted images showed a bone flap in the thinned clivus and fluid collection in the sphenoid sinus. CSF rhinorrhea developed at 1 month after mild trauma. The fracture may have been caused by the trauma and/or by the pressure gradient between the intracranial CSF space and the sphenoid sinus. A detailed history to identify trauma and an examination to detect bone defects in the skull base are necessary when patients present with bacterial meningitis and persistent rhinorrhea.
Keywords: cerebrospinal fluid, rhinorrhea, clival fracture, bacterial meningitis
Introduction
Cerebrospinal fluid (CSF) rhinorrhea is a symptom caused by the leakage of CSF into the nasal sinus, resulting from a defect in the skull base. It is often caused by trauma (head trauma and iatrogenic insult), followed by idiopathic, congenital, and neoplastic lesions (1,2). CSF rhinorrhea is usually detected by nasal endoscopy and/or endonasal examination after fluorescein lumbar puncture, the detection of beta-2 transferrin, computed tomography (CT), or magnetic resonance imaging (MRI). Heavily T2-weighted fast spine echo (FSE), which highlights water signals better than conventional T2-weighted images, is useful for detecting CSF leaks in patients with rhinorrhea and intracranial hypotension syndrome (3,4). Moreover, in patients with CSF rhinorrhea, the location of a CSF fistula can be easily detected by magnetic resonance cisternography with contiguous 1-mm heavily T2-weighted FSE (TR 2000 ms; TE 200 ms) (3). A prospective study reported that 22% of patients with CSF rhinorrhea spontaneously recovered with conservative therapy (2). Patients with persistent CSF rhinorrhea may require surgical therapy such as endoscopic endonasal repair and sinus obliteration or cranialization because 20% of these cases will develop bacterial meningitis (2). The common sites of origin for CSF rhinorrhea after anterior skull-base trauma include the cribriform plate, the roof of the sphenoid sinus, and the posterior wall of the frontal sinus, because the dura mater is strictly adherent to the bone at these sites (5). The clivus is the deepest bone of the skull base and is rarely injured. The incidence of clival fracture among all patients admitted with traumatic brain injury is 1.2% (6). Clival fracture is classified based on its direction into the longitudinal, oblique, and transverse subtypes (6,7). It is further classified based on the quality of the fracture into the hairline, linear, diastatic, and displaced subtypes (6). We herein report the unusual case of a patient who developed bacterial meningitis caused by the leakage of CSF into the sphenoid sinus due to a clival fracture. The defect was a bone flap, which might have been caused by a similar mechanism to spontaneous CSF leakage after a limited longitudinal clival fracture.
Case Report
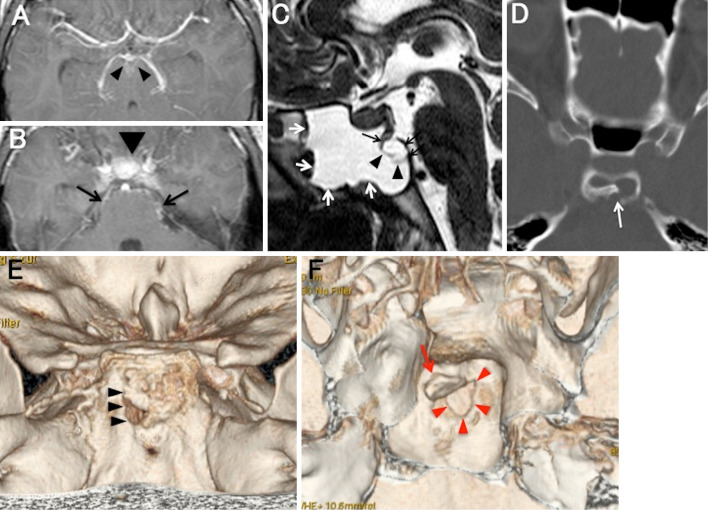
At one month before his admission, a 38-year-old man experienced two episodes of watery rhinorrhea, which spontaneously resolved within a week and a subsequent fever of 4 days in duration. He complained of severe headache on the day prior to his admission, and was transported to our hospital by ambulance. He had a history of mild trauma with a fall from a bicycle, which occurred 1 month before the first appearance of rhinorrhea. On arrival, he was disoriented and hyperactive. He vomited several times. Neck stiffness was observed, but no other neurological abnormalities were detected. A laboratory examination revealed an elevated C-reactive protein level (4.7 IU/mL) and a white blood cell count of 15,700/mm3. A CSF examination revealed an elevated intrathecal pressure (300 mmH2O), pleocytosis (1,381 white blood cells/mm3, 99% neutrophils), and total protein elevation (736 mg/dL); glucose was undetectable. Streptococcus pneumonia was detected in a bacterial culture of the CSF sample. The patient was therefore treated with high-dose ceftriaxone. Four days later, the level of glucose in the patient's CSF increased (34 mg/dL). Because glucose in the persistent rhinorrhea was detected by N-multistixⓇ (Siemens Healthineers Japan, Tokyo, Japan) and biochemical tests, CSF leakage was strongly suspected as the cause of rhinorrhea. Axial T1-weighted MRI with contrast showed enhancement in the interpeduncular cistern and the basal cistern around the pons, which is compatible with a skull base abscess (Figure A and B). Sagittal heavily T2-weighted images with FSE (TR 1500; TE 250) showed a bone gap with a flap in the thinned clivus and an enlarged sphenoid sinus filled with collected CSF, due to a partial defect in the mucosa separating the sinus from the clivus (Figure C). A displaced longitudinal clival fracture in the bone window of CT was detected (Figure D). Three-dimensional CT of the skull base demonstrated a 3×4-mm circular bone defect with a flap on its edge in the middle of the clivus (Figure E and F). After antibiotic treatment, the patient's symptoms, including fever, headache, disorientation, and rhinorrhea, improved. Endoscopic endonasal transsphenoidal surgery was performed at month after the onset of meningitis. Fluid collection was not observed in the sphenoid sinus. There were no abscesses or cystic lesions inside the fractured bone fragment. Thus, the circular bone defect of the clivus was packed with gel foam and surrounding fat and covered with a nasoseptal bone flap. Although the gaps of the sphenoidal mucosa, dura and arachnoid membrane were not directly confirmed by endoscopic surgery, it is thought that inflammatory adhesion of the broken mucosa naturally closed the gap, because CSF leakage was not observed immediately before surgery. A spinal drain was inserted for one week, and an indwelling sphenoidal balloon was placed for 10 days. The CSF rhinorrhea stopped, and the patient was discharged at 2 weeks after surgery.
Figure.
A, B: Axial T1-weighted images with contrast showing enhancement in the interpeduncular cistern (arrowheads), the basal cistern around the pons (arrows), and the suprasellar cistern (arrowhead). C: Sagittal heavily T2-weighted images with FSE (TR 1500; TE 250) showing a bone gap with a flap (black arrows) in the thinned clivus and an enlarged sphenoid sinus filled with CSF (white arrows), due to a partial defect of the mucosa separating the sinus from the clivus (arrowheads). D, E: A displaced longitudinal clival fracture was observed in the bone window of head computed tomography (CT) (D; white arrow) and in the dorsal portion of the clivus on three-dimensional CT (E; black arrowheads). F: A 3-dimensional cranial base reconstruction of the clivus viewed from the sphenoid sinus showing a 3×4-mm circular bone defect (red arrowheads) with a flap on its edge in the center of the clivus (red arrow).
Discussion
We herein report the case of a patient with CSF rhinorrhea associated with an atypical clival fracture that was only detected after the development of bacterial meningitis, which was caused by Streptococcus pneumonia. CSF rhinorrhea is rare, with an incidence of 3% in all clival fracture patients (6). Heavily T2-weighted MRI contributed to the detection of the fracture site, the condition of the mucosal component, and the extent of the CSF leakage in this patient. Three-dimensional CT of the skull base was also useful for assessing the condition of the fracture in detail. We did not test the patient for beta-2 transferrin, which exists exclusively in the CSF. However, glucose was detected in the persistent rhinorrheal fluid at 4 days after the initiation of antibiotic therapy. There was no evidence of enhancement at the clivus, which is a characteristic MRI feature of osteomyelitis and clival cysts or ecchordosis physaliphora, both of which have the potential to cause CSF rhinorrhea (8).
The clivus is composed of the upper sphenoidal bone and the lower occipital bone (9). The bones are bound by spheno-occipital synchondrosis during childhood, with complete ossification in adults (9). There are two types of traumatic clival fracture: one is caused by severe head trauma resulting in brainstem injury or brain herniation, which is associated with a high mortality rate of 38.5% (6,10); the other is caused by mild contusion due to a constructive vulnerability between the middle and superior portions of the clivus (1,9). The former type is sometimes accompanied by vertebrobasilar artery occlusion adjacent to the clivus (with a longitudinal fracture) or by multiple cranial nerve palsies (with a transverse fracture) (6,10). Nakamura et al. reported the case of a 58-year-old man who presented with coma, rhinorrhea, a longitudinal clival fracture (a midline linear fracture in the occipital bone), and subsequent acute subdural hematoma from a severe head injury (10). The latter type occurs due to clival vulnerability associated with the following: the insufficient ossification of the spheno-occipital synchondrosis and/or a thinned clivus because of a well-developed sphenoid sinus; benign intracranial hypertension with empty sella syndrome and/or arachnoid pits; repeated basilar artery pulsations; or repetitive increased intracranial pressure following repeated Valsalva maneuvers (for example, while playing the saxophone) (9). These anatomical and functional factors also play a role in spontaneous CSF leaks (9). Hirayama et al. recently reported a case that was similar to ours. It involved an alert 89-year-old man who presented after a traffic accident, who only had CSF leakage through a clival defect (1). In our patient, a clival flap fracture was detected, extending from the middle to the superior thinner portion, which may have been fragile to external force (1). However, the patient did not develop CSF rhinorrhea until 1 month after trauma. Even after the limited prolapse of the clival bone flap with the dural and arachnoid tear following the initial trauma, the sphenoidal mucosa was thought to have remained intact for some time. It is thought to have gradually separated and detached from the clivus into the sphenoid sinus due to the pressure gradient between the intracranial and the sinus spaces. In our patient, the mucosal structure was eventually broken to cause the leakage of CSF into the sphenoid sinus. This mechanism is similar to that observed in spontaneous transclival CSF leaks (9).
When a patient with bacterial meningitis has persistent watery rhinorrhea, it is important to obtain a detailed history of trauma, to test for glucose and to examine the patient for clival fractures or a bone defects of the skull base. Fractures in the vulnerable clival area can occur even with mild trauma. The occurrence of subsequent bacterial meningitis decreases to 3.4% after surgical repair in patients with traumatic CSF leakage (2). Our patient had no rhinorrhea after surgery; however, a long period of observation is required to ensure that a relapse of meningitis does not occur in the future.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Hirayama A, Komatsu F, Hotta K, et al. Endoscopic endonasal repair of cerebrospinal fluid leakage caused by a rare traumatic clival fracture. Neurol Med Chir (Tokyo) 56: 81-84, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Daudia A, Biswas D, Jones NS. Risk of meningitis with cerebrospinal fluid rhinorrhea. Ann Otol Rhinol Laryngol 116: 902-905, 2007. [DOI] [PubMed] [Google Scholar]
- 3. Vimala LR, Jasper A, Irodi A. Non-invasive and minimally invasive imaging evaluation of CSF rhinorrhea-a retrospective study with review of literature. Pol J Radiol 81: 80-85, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wang YF, Lirng JF, Fuh JL, Hseu SS, Wang SJ. Heavily T2-weighted MR myelography vs CT myelography in spontaneous intracranial hypotension. Neurology 73: 1892-1898, 2009. [DOI] [PubMed] [Google Scholar]
- 5. Komatsu M, Komatsu F, Cavallo LM, et al. Purely endoscopic repair of traumatic cerebrospinal fluid rhinorrhea from the anterior skull base: case report. Neurol Med Chir (Tokyo) 51: 222-225, 2011. [DOI] [PubMed] [Google Scholar]
- 6. Winkler-Schwartz A, Correa JA, Marcoux J. Clival fractures in a level I trauma center. J Neurosurg 122: 227-235, 2015. [DOI] [PubMed] [Google Scholar]
- 7. Ochalski PG, Spiro RM, Fabio A, Kassam AB, Okonkwo DO. Fractures of the clivus: a contemporary series in the computed tomography era. Neurosurgery 65: 1063-1069, 2009. [DOI] [PubMed] [Google Scholar]
- 8. Chihara C, Korogi Y, Kakeda S, et al. Ecchordosis physaliphora and its variants: proposed new classification based on high-resolution fast MR imaging employing steady-state acquisition. Eur Radiol 23: 2854-2860, 2013. [DOI] [PubMed] [Google Scholar]
- 9. Van Zele T, Kitice A, Vellutini E, Balsalobre L, Stamm A. Primary spontaneous cerebrospinal fluid leaks located at the clivus. Allergy Rhinol (Providence) 4: e100-e104, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nakamura F, Tama N, Kuga Y, Kojima T, Waga S. Traumatic cerebrospinal fluid rhinorrhea caused by a longitudinal fracture of the clivus: A case report. Jpn J Neurosurg 7: 699-702, 1998. [Google Scholar]